Abstract
Background
Non-small-cell lung cancer (NSCLC) is a global public health problem, and brain is a common metastatic site in advanced NSCLC. Currently, whole-brain radiotherapy (WBRT) remains a major treatment for brain metastases, while EGFR-tyrosine kinase inhibitor (TKI) is the standard treatment for advanced NSCLC harboring EGFR mutations, which is also effective for brain metastases. However, whether EGFR-TKIs plus radiotherapy is superior to EGFR-TKIs alone for the treatment of advanced EGFR-mutant NSCLS with brain metastases remains controversial. This study aimed to compare the efficacy of concurrent EGFR-TKIs and WBRT vs EGFR-TKI alone in a retrospective cohort of advanced EGFR-mutant NSCLS with brain metastases.
Patients and methods
The medical records of 104 treatment-naïve, advanced EGFR-mutant NSCLC patients with brain metastases were retrospectively reviewed, and there were 56 patients undergoing concurrent EGFR-TKI and WBRT, and 48 patients given EGFR-TKI alone, including 20 cases with salvage WBRT upon brain metastasis progression. The survival prognosis was compared between the two cohorts.
Results
The baseline clinicopathologic factors were balanced between the two cohorts. After a median follow-up of 23 months, 35.6% of the study subjects survived. Concurrent EGFR-TKI and WBRT significantly improved the median intracranial PFS (iPFS) compared with EGFR-TKI alone (17.7 vs 11.0 months, P=0.015); however, no significant difference was seen in median overall survival between the two cohorts (28.1 vs 24.0 months, P=0.756). In addition, the median iPFS was found to significantly vary in the number of brain metastases (≤3 vs>3 metastases: 18.0 vs 12.5 months, P=0.044). Subgroup analysis showed that concurrent EGFR-TKI and WBRT improved median iPFS compared with EGFR-TKI alone in patients with more than three brain metastases (P=0.001); however, no significant difference was observed between the two regimens in patients with three or less brain metastases (P=0.526).
Conclusion
Our data demonstrate that concurrent EGFR-TKI and WBRT achieves longer iPFS than EGFR-TKI alone in advanced EGFR-mutant NSCLC with brain metastases. In advanced EGFR-mutant NSCLC with three or less brain metastases, EGFR-TKI alone may be an option as a first-line therapy.
Keywords: non-small-cell lung cancer, brain metastasis, epidermal growth factor receptor, tyrosine kinase inhibitor, whole-brain radiotherapy
Introduction
Lung cancer, the most common type of cancer and the leading cause of cancer-related deaths worldwide, remains a great threat to public health across the world.1 Each year, >1 million new cases are diagnosed with lung cancer, and over 1 million deaths are attributed to this malignancy.2 As a major type of lung cancer, non-small-cell lung cancer (NSCLC) accounts for ~85% of all lung cancers.3
Metastasis determines the design of the treatment regimen and prognosis in NSCLC patients.4,5 Brain is a common metastatic site in patients with NSCLC, and ~20%–25% of the NSCLC patients at initial diagnosis are estimated to have brain metastasis.6,7 It has been shown that the NSCLC patients with brain metastases have a poor prognosis, low quality of life, and short survival, with a median survival period of only 1–2 months in untreated patients.8–11
Currently, the treatment options for NSCLC with brain metastasis mainly include stereotactic radiosurgery (SRS), whole-brain radiotherapy (WBRT), surgery, chemotherapy, targeted therapy, and symptomatic and supportive treatment.12–14 WBRT and SRS remain the standard treatment for brain metastases in NSCLC; however, such treatments exhibit limited effects on patients’ survival, which only prolong the survival period of 4–6 months.15,16 Conventional therapies, such as chemotherapy, have shown an unsatisfactory efficacy in the treatment of brain metastases in NSCLC due to the presence of blood–brain barrier (BBB).17 A search for treatments that may greatly prolong the survival and improve the prognosis has, therefore, been paid much attention in NSCLC patients with brain metastases.
Driver gene-targeted therapy achieves better survival benefits for the patients with advanced NSCLC, and EGFR is a predominant driver oncogene in NSCLC.18 EGFR-tyrosine kinase inhibitors (TKIs) have been accepted as the initial therapy for advanced NSCLC patients with EGFR-sensitive mutations, and EGFR-TKI treatment was reported to achieve an overall response rate (ORR) of 55%–85%, progression-free survival (PFS) of ~12 months, and overall survival (OS) of 24–36 months in advanced EGFR-mutant NSCLC patients.19–21 Data from Phase 3 clinical trials have shown that EGFR-TKI treatment may increase the objective response rate (RR), prolong the PFS, and cause significantly lower incidence of adverse reactions in NSCLC patients relative to in platinum-containing double-drug chemotherapy.22,23
It has been found that the NSCLC patients harboring an EGFR mutation have a higher incidence of brain metastasis (30%–70%) than those without EGFR mutations, and the management of brain metastasis is, therefore, critical to antitumor therapy in NSCLC patients harboring an EGFR mutation.24–27 Data from clinical trials have demonstrated that EGFR-TKIs may cause regression of established brain metastases from NSCLC, with an intracranial RR of 75% in treatment-naïve, advanced EGFR-mutant NSCLC patients.28–30 To date, the optimal timing of brain radiotherapy, however, remains controversial in EGFR-mutant lung cancer patients with brain metastasis in the presence of well-controlled intracranial and extracranial lesions by EGFR-TKIs. The present study was, therefore, designed to compare the efficacy of concurrent EGFR-TKIs and WBRT vs EGFR-TKI alone in a retrospective cohort of advanced EGFR-mutant NSCLS with brain metastases, so as to provide insights into the optimal timing of brain radiotherapy.
Patients and methods
Study subjects
The medical records of 104 treatment-naïve, advanced EGFR-mutant NSCLC patients with brain metastases admitted to Fujian Provincial Cancer Hospital (Fuzhou, People’s Republic of China) during the period from January 1, 2012 to June 30, 2017 were retrospectively reviewed. All NSCLCs were definitively diagnosed with pathologic examinations, and EGFR mutation analysis was performed using amplification refractory mutation system PCR or next-generation sequencing. There were 56 patients undergoing concurrent EGFR-TKI and WBRT, and 48 patients given EGFR-TKI alone, including 20 cases with salvage WBRT upon brain metastasis progression.
Treatment regimens
All patients received an initial MRI scan of the brain prior to administration of EGFR-TKIs and every 2–3 months post-treatment with EGFR-TKIs. All subjects were given 150 mg erlotinib (Roche, Basel, Switzerland) once a day (QD), 250 mg gefitinib (AstraZeneca Pharmaceuticals, Waltham, MA, USA) QD or 150 mg icotinib (Betta Pharmaceuticals Co., Ltd., Hangzhou, People’s Republic of China) three times a day, and WBRT was delivered at a dose of 30 Gy divided in ten fractions for 5 days a week, given at a total of 2 weeks. The response to therapy was evaluated according to the Response Evaluation Criteria in Solid Tumor version 1.1, 1 month after the initial treatment with EGFR-TKIs,31 followed by once every 2–3 months, and the adverse events were assessed according to the Common Terminology Criteria for Adverse Events version 4.0.32
Survival analysis
Intracranial PFS (iPFS) was defined as the survival from initial EGFR-TKIs treatment to intracranial progression following WBRT. OS was estimated from the date of initial diagnosis until the date of death or the last follow-up.
Statistical analysis
All data were entered into Microsoft Excel 2007 (Microsoft, Inc., Redmond, WA, USA), and all statistical analyses were performed using the statistical software SPSS version 23.0 (IBM Corporation, Armonk, NY, USA). Chi-squared test or Fisher’s exact test was used to compare the clinicopathologic characteristics between the two cohorts. Survival curves were generated using the Kaplan–Meier method, and the survival probability was compared with the log-rank test. A Cox regression model was employed for univariate and multivariate analyses to evaluate the corresponding 95% CIs and HRs. A P value of <0.05 was considered statistically significant.
Informed consent
All participants signed the informed consent pertaining to targeted therapy or brain radiotherapy. All subjects involved in this study agreed to publish related demographic and clinical features.
Ethical approval
The study protocol was reviewed and approved by the Ethical Review Committee of Fujian Provincial Cancer Hospital (approval no. FJZLYY2015-00179). All experimentations described in this study were conducted in accordance with the Declaration of Helsinki.
Results
Clinicopathologic characteristics of the study subjects
The study subjects included 45 men and 59 women, and had a median age of 59 years (range, 23–79 years) at diagnosis. Of all subjects, 97.1% were diagnosed with adenocarcinoma and 88.5% had an Eastern Cooperative Oncology Group (ECOG) Performance Status score of 0 or 1. There were 83 cases with extracranial metastases and 48 cases with symptomatic brain metastases initially. In addition, there were 39 cases harboring an EGFR exon 19 deletion mutation, 39 cases harboring an EGFR exon 21L858R mutation, 5 cases harboring an EGFR exon 21L861Q mutation, 4 cases harboring an EGFR exon 18G719X mutation, 4 cases harboring combined EGFR exon 21L858R and exon 20 T790M mutations, 4 cases harboring combined EGFR exon 19 deletion mutation and exon 20 T790M mutation, while the mutation sites of the other 9 cases were unclear. The baseline clinicopathologic features were balanced between the two cohorts (Table 1).
Table 1.
Clinicopathologic characteristics of the study subjects
| Characteristics | Total subjects (N=104) | EGFR-TKI plus WBRT (n=56) | EGFR-TKI (n=48) | P-value | ||
|---|---|---|---|---|---|---|
|
| ||||||
| No. of patients | % | No. of patients | % | |||
|
| ||||||
| Gender | ||||||
| Male | 45 | 25 | 55.6 | 20 | 44.4 | 0.843 |
| Female | 59 | 31 | 52.5 | 28 | 47.5 | |
| Age (years) | ||||||
| >60 | 37 | 19 | 51.2 | 18 | 48.6 | 0.837 |
| ≤60 | 67 | 37 | 30 | |||
| ECOG-PS score | ||||||
| 0–1 | 92 | 48 | 52.2 | 44 | 47.8 | 0.377 |
| ≥2 | 12 | 8 | 66.7 | 4 | 33.3 | |
| Symptomatic brain metastasis | ||||||
| Yes | 48 | 29 | 60.4 | 19 | 39.6 | 0.241 |
| No | 56 | 27 | 48.2 | 29 | 51.8 | |
| Smoking status | ||||||
| Never | 77 | 41 | 53.2 | 36 | 46.8 | 0.836 |
| Former | 27 | 15 | 55.6 | 12 | 44.4 | |
| EGFR mutations | ||||||
| 19 del | 39 | 18 | 46.2 | 21 | 53.8 | 0.173 |
| L858R | 39 | 20 | 51.3 | 19 | 48.7 | |
| Others | 26 | 18 | 69.2 | 8 | 30.8 | |
| Extracranial metastasis initially | ||||||
| Yes | 83 | 45 | 54.2 | 38 | 45.8 | 0.880 |
| No | 21 | 11 | 52.3 | 10 | 47.6 | |
| Number of brain metastases, n | ||||||
| >3 | 70 | 30 | 42.9 | 40 | 57.1 | 0.403 |
| ≤3 | 34 | 16 | 47.1 | 18 | 52.9 | |
| Histology | ||||||
| Adenocarcinoma | 101 | 56 | 55.4 | 45 | 44.6 | 0.095 |
| Others | 3 | 0 | 0 | 3 | 100 | |
Abbreviations: ECOG-PS, Eastern Cooperative Oncology Group Performance Status; TKI, tyrosine kinase inhibitor; WBRT, whole-brain radiotherapy.
Intracranial progression
The subjects received follow-up for a median period of 23 months (range, 5–82 months). At the end of the follow-up period (June 30, 2017), 36 subjects remained alive and 66 cases were dead due to disease progression. Of all subjects, 86 cases (82.7%) had an intracranial progressive disease, with a median iPFS of 14.5 months (95% CI, 11.924–17.076 months). Intracranial progression developed in 76.8% (43/56) of the patients receiving EGFR-TKIs plus and WBRT, while intracranial progression occurred in 89.6% (43/48) of the cases given EGFR-TKIs alone. The median iPFS was 17.7 months (95% CI, 16.288–22.212 months) in the patients receiving concurrent EGFR-TKIs and WBRT, which was significantly longer than that of those given EGFR-TKIs alone (median iPFS, 11.0 months; 95% CI, 8.067–13.933 months; P=0.015), as shown in Table 2 and Figure 1.
Table 2.
iPFS and OS according to subgroups
| n | Median iPFS (months) | 95% CI | P-value | Median OS (months) | 95% CI | P-value | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Gender | |||||||
| Male | 45 | 14.2 | 9.362–19.038 | 0.584 | 25.5 | 17.718–33.282 | 0.380 |
| Female | 59 | 15.1 | 13.683–16.517 | 28.0 | 21.150–34.850 | ||
| Age (years) | |||||||
| >60 | 37 | 17.6 | 11.421–16.579 | 0.649 | 28.3 | 21.815–34.785 | 0.326 |
| ≤60 | 67 | 14.0 | 13.037–22.163 | 25.5 | 29.575–31.425 | ||
| ECOG-PS | |||||||
| 0–1 | 92 | 14.5 | 11.291–17.709 | 0.952 | 25.4 | 20.760–30.040 | 0.198 |
| ≥2 | 12 | 14.5 | 4.316–24.684 | 25.5 | 2.705–48.295 | ||
| Symptomatic of BM | |||||||
| Yes | 36 | 17.6 | 13.787–21.413 | 0.218 | 28.0 | 24.122–31.878 | 0.953 |
| No | 68 | 14.0 | 10.780–17.220 | 25.4 | 19.988–30.812 | ||
| Smoking status | |||||||
| Never | 77 | 14.5 | 11.882–17.118 | 0.996 | 27.3 | 22.842–31.758 | 0.761 |
| Former | 27 | 16.1 | 9.124–23.076 | 25.5 | 16.953–34.047 | ||
| EGFR mutations | |||||||
| 19 del | 39 | 14.5 | 11.634–16.214 | 0.915 | 27.5 | 17.050–38.365 | 0.356 |
| L858R | 39 | 15.1 | 13.852–16.786 | 22.1 | 17.552–26.865 | ||
| Other | 26 | 17.2 | 12.466–21.756 | 28.2 | 23.678–32.986 | ||
| Extracranial metastasis initially | |||||||
| Yes | 83 | 14.5 | 11.031–17.969 | 0.362 | 24.0 | 18.579–29.421 | 0.203 |
| No | 21 | 15.1 | 6.179–24.021 | 28.4 | 24.543–32.257 | ||
| Number of BMs | |||||||
| >3 | 70 | 12.5 | 12.952–17.432 | 0.044 | 27.3 | 21.633–32.967 | 0.696 |
| ≤3 | 34 | 18.0 | 16.142–23.554 | 30.0 | 21.027–38.973 | ||
| Therapy method | |||||||
| EGFR-TKI plus WBRT | 56 | 17.7 | 16.288–22.212 | 0.015 | 28.1 | 23.975–32.225 | 0.756 |
| EGFR-TKI alone | 48 | 11.0 | 8.067–13.933 | 24.0 | 17.428–30.572 | ||
Abbreviations: ECOG-PS, Eastern Cooperative Oncology Group Performance Status; iPFS, intracranial progression-free survival; OS, overall survival; PFS, progression-free survival; TKI, tyrosine kinase inhibitor; WBRT, whole-brain radiotherapy.
Figure 1.
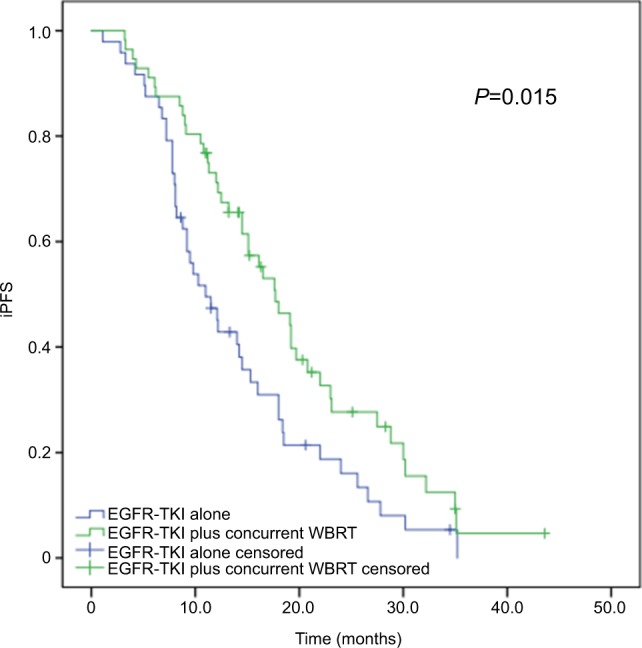
Kaplan–Meier curves for iPFS in advanced EGFR-mutant NSCLC patients.
Notes: The median iPFS is significantly longer in patients receiving concurrent EGFR-TKIs and WBRT than in those given EGFR-TKIs alone (17.7 vs 11.0 months, P=0.015).
Abbreviations: iPFS, intracranial progression-free survival; NSCLC, non-small-cell lung cancer; TKI, tyrosine kinase inhibitor; WBRT, whole-brain radiotherapy.
The 70 patients with more than three brain metastases had a median iPFS of 12.5 months (95% CI, 12.952–17.432 months), which was significantly shorter than that of 34 cases with three or less brain metastases (median iPFS, 18.0 months; 95% CI, 16.142–23.554 months; P=0.044), as shown in Figure 2.
Figure 2.
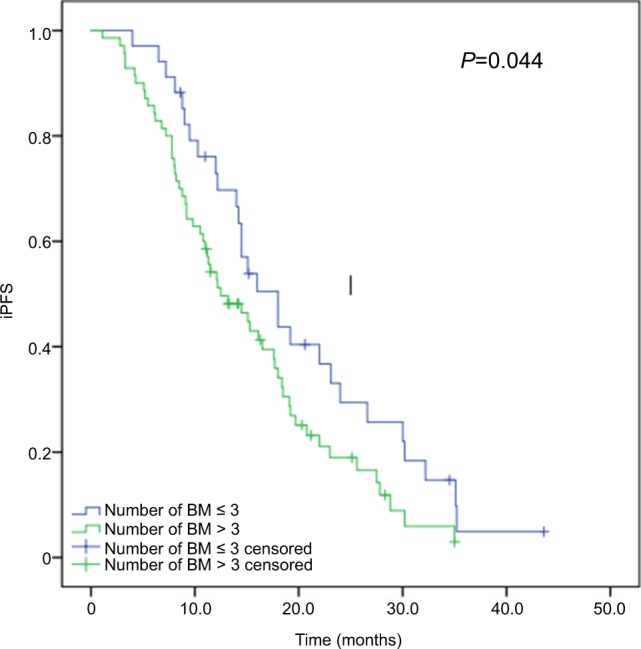
Kaplan–Meier curves for iPFS in advanced EGFR-mutant NSCLC patients with various number of brain metastases.
Note: Patients with more than three brain metastases had significantly shorter median iPFS than those with three or less brain metastases (12.5 vs 18.0 months, P=0.044).
Abbreviations: iPFS, intracranial progression-free survival; NSCLC, non-small-cell lung cancer.
Among the study subjects, there were 6 patients (5.8%) with complete response and 42 patients (40.4%) with partial response, yielding an ORR of 46.2%. In addition, there were 52 patients (50.0%) with stable disease. The ORR was comparable between the patients receiving concurrent EGFR-TKIs and WBRT and EGFR-TKIs alone (48.2% vs 54.2%, P=0.562; Table 3). Cox multivariate regression analysis revealed that concurrent EGFR-TKIs and WBRT was an independent predictor of iPFS (P=0.004) and more than three brain metastases was a potential independent predictor unfavorably affecting iPFS in advanced EGFR-mutant NSCLC patients (P=0.017; Table 4).
Table 3.
Response to therapy in the two study cohorts
| Response | EGFR-TKI plus WBRT (n=48) | EGFR-TKI alone (n=56) | Total n (%) |
|---|---|---|---|
|
| |||
| CR | 2 | 4 | 6 (5.8%) |
| PR | 25 | 22 | 47 (45.2%) |
| SD | 25 | 20 | 45 (43.2%) |
| PD | 2 | 2 | 4 (3.8%) |
| ORR | 48.2% | 54.2% | 104 (100%) |
Abbreviations: CR, complete response; ORR, overall response rate; PD, progressive disease; PR, partial response; SD, stable disease; TKI, tyrosine kinase inhibitor; WBRT, whole-brain radiotherapy.
Table 4.
Univariable and multivariable analyses of covariables associated with intracranial progression-free survival
| Characteristics | n | Univariate | Multivariate | ||
|---|---|---|---|---|---|
|
| |||||
| HR (95% CI) | P-value | HR (95% CI) | P-value | ||
|
| |||||
| Number of brain metastasis | |||||
| >3 | 70 | 1.533 (0.969–2.427) | 0.068 | 1.785 (1.110–2.871) | 0.017 |
| ≤3 | 34 | ||||
| Therapy method | |||||
| EGFR-TKI + WBRT | 56 | 0.590 (0.385–0.903) | 0.015 | 0.504 (0.336–0.807) | 0.004 |
| EGFR-TKI | 48 | ||||
Abbreviations: TKI, tyrosine kinase inhibitor; WBRT, whole-brain radiotherapy.
Survival outcomes
Thirty-six patients survived until the end of the followup period. Among all study subjects, the median OS was 27.3 months (95% CI, 23.109–31.491 months), and no significant difference was found in the median OS between the patients receiving concurrent EGFR-TKIs and WBRT (median OS, 28.1 months; 95% CI, 23.975–32.225 months) and EGFR-TKIs alone (median OS, 24.0 months; 95% CI, 17.428–30.572 months), with a P-value of 0.756. Among the 48 patients given EGFR-TKIs alone, there were 20 cases with salvage WBRT upon brain metastasis progression, and the median OS did not significantly differ in patients receiving concurrent EGFR-TKIs and WBRT (median OS, 28.1 months; 95% CI, 23.975–32.225 months), salvage WBRT (median OS, 36.1 months; 95% CI, 19.678–52.622 months), and EGFR-TKIs alone (median OS, 22.5 months; 95% CI, 14.990–30.010 months), with a P-value of 0.366 (Figure 3).
Figure 3.
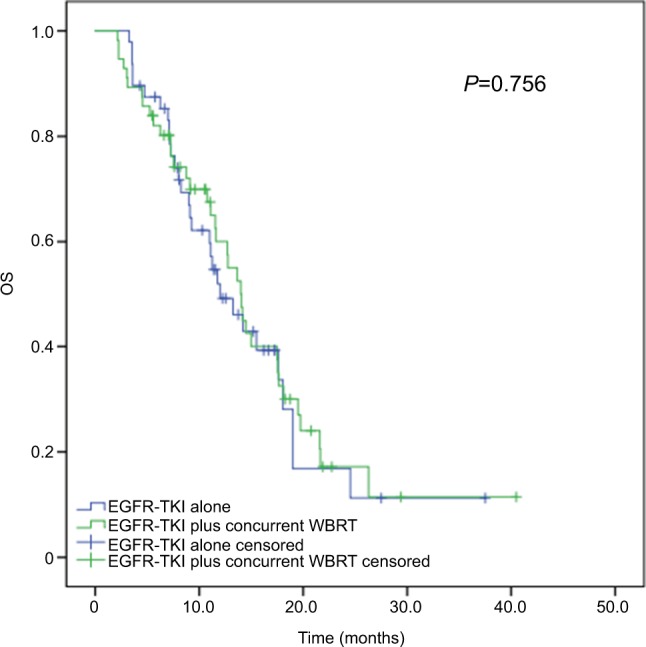
Kaplan–Meier curves for OS in advanced EGFR-mutant NSCLC patients receiving various treatment regimens.
Note: The median OS did not significantly differ in patients receiving concurrent EGFR-TKIs and WBRT (median OS, 28.1 months; 95% CI, 23.975–32.225 months) and EGFR-TKIs alone (median OS, 24.0 months; 95% CI, 17.428–30.572 months), with the P-value being 0.756.
Abbreviations: NSCLC, non-small-cell lung cancer; OS, overall survival; TKI, tyrosine kinase inhibitor; WBRT, whole-brain radiotherapy.
Subgroup analyses
Subgroup analyses revealed that of the 70 patients with more than three brain metastases, the median iPFS was significantly longer in cases receiving concurrent EGFR-TKIs and WBRT (median iPFS, 17.6 months; 95% CI, 14.176–21.024 months) than in those given EGFR-TKIs alone (median iPFS, 9.2 months; 95% CI, 6.924–11.476 months; P=0.001), as shown in Figure 4. Among the 34 patients with three or less brain metastases, however, no significant difference was detected in the median iPFS between the patients receiving concurrent EGFR-TKIs and WBRT and EGFR-TKIs alone (P=0.526; Figure 5).
Figure 4.
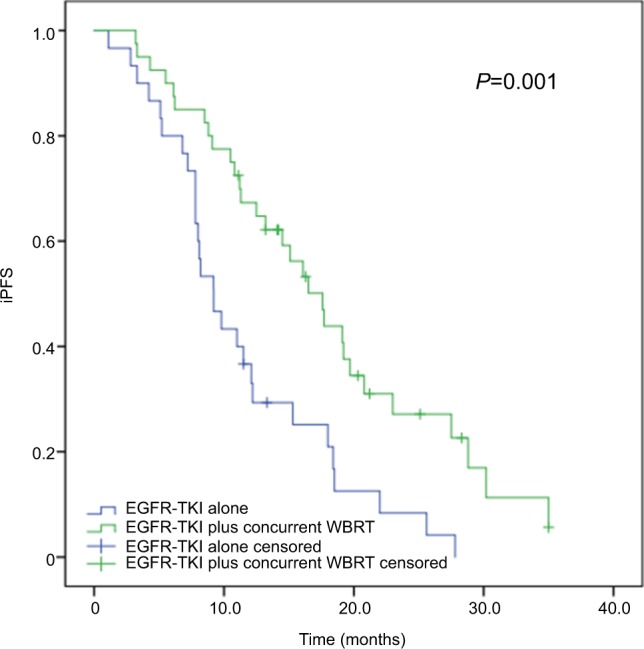
Subgroup analysis of iPFS in advanced EGFR-mutant NSCLC patients with more than three brain metastases.
Note: The median iPFS was significantly longer in patients receiving concurrent EGFR-TKIs and WBRT than in those given EGFR-TKIs alone (17.6 vs 9.2 months, P=0.001).
Abbreviations: iPFS, intracranial progression-free survival; NSCLC, non-small-cell lung cancer; TKI, tyrosine kinase inhibitor; WBRT, whole-brain radiotherapy.
Figure 5.
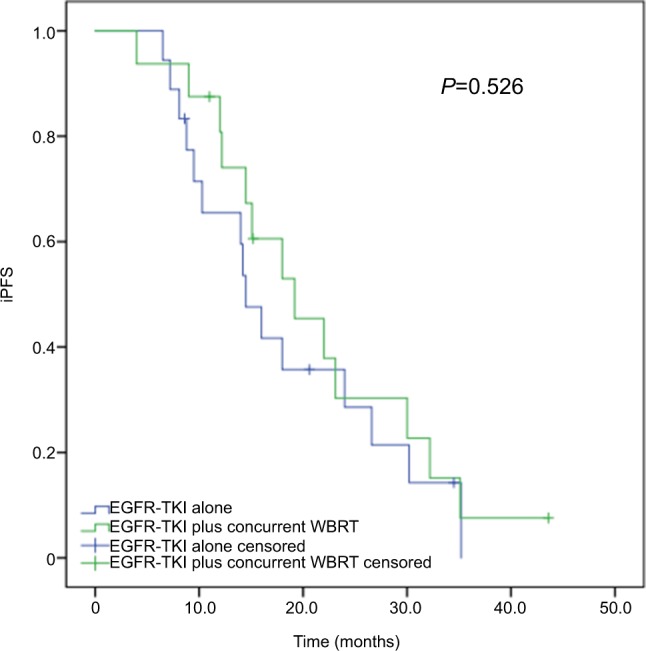
Subgroup analysis of iPFS in advanced EGFR-mutant NSCLC patients with three or less brain metastases.
Note: The median iPFS was comparable between the patients receiving concurrent EGFR-TKIs and WBRT and EGFR-TKIs alone (19.2 vs 14.5 months, P=0.526).
Abbreviations: iPFS, intracranial progression-free survival; NSCLC, non-small-cell lung cancer; TKI, tyrosine kinase inhibitor; WBRT, whole-brain radiotherapy.
Toxicity
During the treatment period, the incidence of adverse events was 85.7% and 83.3% in the subjects receiving concurrent EGFR-TKIs and WBRT and EGFR-TKIs alone. In cases given EGFR-TKIs alone, the incidence of grade 3 and higher adverse events was 2.1%, and in the cases receiving concurrent EGFR-TKIs and WBRT, the incidence of grade 3 and higher adverse events was 8.9%, including a case with reduced drug doses due to the development of grade 3 diarrhea. The WBRT-related adverse events mainly included dizziness and headache, which were alleviated following dehydration treatment, as well as neurocognitive impairment (grade 1 and 2 in three cases and grade 3 in one case), as shown in Table 5.
Table 5.
Treatment-related toxicities
| EGFR-TKI concurrent WBRT (n=56) | EGFR-TKI alone (n=48) | |||
|---|---|---|---|---|
|
| ||||
| Grade 1 or 2 | Grade 3 or worse | Grade 1 or 2 | Grade 3 or worse | |
|
| ||||
| Total adverse events | 48/56 (85.7%) | 40/48 (83.3%) | ||
| Elevated ALT/AST | 15 (26.8%) | 1 (1.8%) | 11 (22.9%) | 0 |
| Elevated bilirubin | 6 (10.7%) | 0 | 5 (10.4%) | 0 |
| Rash | 15 (26.8%) | 2 (3.6%) | 17 (35.4%) | 1 (2.1%) |
| Fatigue | 8 (14.3%) | 0 | 10 (20.8%) | 0 |
| Nausea | 7 (12.5%) | 0 | 5 (10.4%) | 0 |
| Vomiting | 4 (7.1%) | 0 | 3 (6.3%) | 0 |
| Diarrhea | 3 (5.4%) | 1 (1.8%) | 5 (10.4%) | 0 |
| Dizziness | 15 (26.8%) | 0 | 0 | 0 |
| Headache | 11 (19.6) | 0 | 0 | 0 |
| Cognitive disorder | 3 (5.4%) | 1 (1.8%) | 0 | 0 |
Abbreviations: TKI, tyrosine kinase inhibitor; WBRT, whole-brain radiotherapy.
Discussion
Currently, the treatment of advanced NSCLC with brain metastasis remains a great challenge,8–10 and EGFR-mutant NSCLC has been found to be more likely to present brain metastases.24–27 Prior to the introduction of EGFR-TKI, WBRT, surgical resection of the metastatic lesions, and SRS were the standard treatments of brain metastasis; however, radiotherapy and surgery cause non-ignorable brain damages, which may seriously affect patients’ survival and quality of life.12–16 EGFR-TKI is an emerging effective treatment option for EGFR-mutant lung cancer patients with brain metastasis.33 Results from the CTONG-0803 Phase 2 clinical trial showed that the single-agent erlotinib at a daily dose of 150 mg was active and well tolerated as a second-line therapy in NSCLC patients with brain metastasis, which achieved 10.1 months iPFS.34 Another multicenter, Phase 3, open-label, parallel, randomized controlled trial to compare the efficacy of icotinib vs whole-brain irradiation with or without chemotherapy revealed that icotinib treatment (median iPFS, 10.1 months) achieved significantly longer iPFS than WBI plus chemotherapy (median iPFS, 4.8 months) in patients with EGFR-mutant NSCLC and multiple brain metastases.35 Since brain radiotherapy may cause brain injuries, the optimal timing of brain radiotherapy remains in dispute until now. In EGFR-mutant NSCLC patients with brain metastasis, is the first-line brain radiotherapy is required? Does brain radiotherapy serve as a salvage therapy upon intracranial tumor progression? These questions remain to be answered. Previous studies have shown that concurrent EGFR-TKI and brain radiotherapy (WBRT or SRS) may increase the intracra-nial disease control rate and extend the OS in EGFR-mutant NSCLC patients.36–38 In addition, a recent multi-institutional analysis demonstrated that SRS followed by EGFR-TKI resulted in the longest OS and allowed patients to avoid the potential neurocognitive sequelae of WBRT in EGFR-mutant NSCLC patients with brain metastases.39
Our data showed that concurrent EGFR-TKIs and WBRT achieved significantly longer iPFS than EGFR-TKIs alone (median iPFS, 17.7 vs 11.0 months, P=0.015), which was similar to a previous study reporting that concurrent early brain radiotherapy with EGFR-TKI may improve intracranial disease control in EGFR-mutant NSCLC with brain metastasis.38 Results from a Phase 2 clinical trial showed that erlotinib in combination with WBRT was well tolerated with a favorable objective RR in patients with brain metastases from NSCLC.40 Due to the protection of the BBB, the drug concentration is not high in the central nervous system (CNS).41 Therefore, optimal CNS penetration is a critical issue for patients with brain metastases.42 Brain radiotherapy is found to destroy the BBB and increase the TKIs concentration in the cerebrospinal fluid.43,44 In addition, it has been shown that EGFR mutation is a radiosensitive NSCLC genotype and EGFR-TKI is supposed to be a radiosensitizer.43,45,46 It is, therefore, hypothesized that EGFR-TKI and WBRT may have a synergistic effect, and the combination of EGFR-TKI and WBRT may result in better intracranial tumor control in NSCLC harboring EGFR mutations. Taking these findings together, it is considered that concurrent EGFR-TKIs with WBRT may achieve better intracranial tumor control in NSCLC harboring EGFR mutations.
In the current study, concurrent EGFR-TKIs with WBRT (median OS, 28.1 months) achieved extension of the OS relative to EGFR-TKIs alone (median OS, 24 months), although no significant difference was seen between these two regimens in terms of the median OS (P=0.756). Of the 48 patients initially treated with EGFR-TKI alone, there were 20 cases receiving salvage WBRT upon brain metastasis progression, and 58.3% of the cases lost the timing for WBRT due to physical intolerance and treatment abandonment. Our data showed no significant difference in the OS between the patients receiving concurrent EGFR-TKIs with WBRT and EGFR-TKIs alone. Follow-up revealed that the majority of the patients were well tolerant to WBRT, with only a case developing grade 3 neurocognitive impairment, who had a 4.5 OS. Further studies to examine the effect of WBRT-induced neurocognitive impairment on survival in EGFR-mutant NSCLC patients with brain metastasis are required. We, therefore, recommend concurrent EGFR-TKI with brain radiotherapy as an initial therapy for EGFR-mutant NSCLC patients with brain metastasis. A retrospective multi-institutional analysis showed that SRS followed by EGFR-TKI (46 months) achieved longer median OS than WBRT followed by EGFR-TKI (30 months) and EGFR-TKI followed by SRS or WBRT (25 months) at intracranial progression in EGFR-mutant NSCLC patients with brain metastases (P<0.001).39 In addition, SRS was found to have less toxicity and avoided the potential neurocognitive sequelae from WBRT.47,48 EGFR-TKI plus brain radiotherapy, notably SRS, as an initial therapy, may improve the survival and avoid losing the timing for radiotherapy, which may be an optimal option for the treatment of EGFR-mutant NSCLC with brain metastasis. However, a prospective, randomized clinical trial is urgently needed to confirm the findings.
In this study, a Cox multivariate regression analysis revealed that the number of brain metastasis was an independent predictor of iPFS, and advanced EGFR-mutant NSCLC patients with three or less brain metastases at initial diagnosis affected iPFS favorably. Previous studies have demonstrated that ECOG performance status, EGFR mutation subtype, and absence of extracranial metastases are independent predictors of iPFS and OS in NSCLC patients with brain metastasis,39,49 which was not found in the present study. Our data report a single-institution experience and the study sample is small. Further large-scale, multicenter, retrospective studies to identify the factors affecting iPFS and OS in NSCLC patients with brain metastasis are warranted.
Currently, neurosurgery or radiosurgery is the standard option for the radical therapy of locally intracranial metastatic tumors, and SRS is accepted as the first choice for the local treatment of locally intracranial metastatic tumors.50,51 However, either surgery or radiotherapy is invasive and has side effects, while EGFR-TKI shows a high response and few adverse effects for intracranial metastatic tumors.50,51 To defer or avoid neurocognitive sequelae from WBRT, it is necessary to identify the patient population given EGFR-TKI alone as the initial therapy. Our subgroup analysis showed that concurrent EGFR-TKI and WBRT improved median iPFS compared with EGFR-TKI alone in patients with more than three brain metastases (P=0.001); however, no significant difference was observed between the two regimens in patients with three or less brain metastases (P=0.526). It is hypothesized that, in EGFR-mutant NSCLC with three or less brain metastases, EGFR-TKI alone may be an option as a first-line therapy; however, this requires further investigations to test such a hypothesis. Osimertinib, an oral, CNS-active, third-generation EGFR-TKI, was found to be effective in crossing the BBB and penetrating the CNS.52 Data from the FLAURA study revealed that osimertinib achieved a significantly higher CNS objective RR (66%) than the first-generation EGFR-TKI and remarkably reduced the risk of intracranial progression in advanced NSCLC patients with EGFR-TKI-sensitizing mutation.53 In Asian patients with previously untreated advanced NSCLC harboring exon 19 deletion (Ex19del)/L858R EGFR-TKI-sensitizing mutations, first-line osimertinib demonstrated a clinically meaningful improvement in PFS over the standard of care EGFR-TKI (gefitinib or erlotinib) (median PFS, 16.5 vs 11.0 months, HR =0.54, 95% CI, 0.41–0.72; P<0.0001).54 However, more investigations are required to demonstrate the likelihood of osimertinib as an alternative of brain radiotherapy in EGFR-mutant, advanced NSCLC patients with brain metastases. In addition, prospective studies are needed to identify the patient population given EGFR-TKI alone in whom brain radiotherapy is not needed, in order to protect them against radiation-induced neurocognitive sequelae from WBRT.
Conclusion
The results of the present study demonstrate that concurrent EGFR-TKI and WBRT may improve intracranial disease control in advanced EGFR-mutant NSCLC with brain metastasis. Initial treatment with EGFR-TKI alone may cause a loss of timing for WBRT, and concurrent EGFR-TKI with WBRT may be an optimal option for EGFR-mutant NSCLC with brain metastasis at the initial diagnosis. However, EGFR-TKI alone may be an option as the first-line therapy in patients with three or less brain metastases, which may defer or avoid neurocognitive sequelae from WBRT. Further multi-institutional, prospective, randomized clinical trials to validate our findings and determine the optimal treatment for EGFR-mutant NSCLC with brain metastasis seem justified.
Data sharing statement
All data reported in this study are available upon request by contacting the corresponding author.
Acknowledgments
This study was supported by grants from the Fujian Provincial Medical Innovative Project (grant no. 2017-CX-7), Fujian Provincial Sci & Tech Innovative Joint Fund (grant no. 2017Y9080), and Fujian Provincial Sci & Tech Guiding Project (grant no. 2018Y0017).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Herbst RS, Heymach JV, Lippman SM. Lung cancer. N Engl J Med. 2008;359(13):1367–1380. doi: 10.1056/NEJMra0802714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gouvinhas C, De Mello RA, Oliveira D, et al. Lung cancer: a brief review of epidemiology and screening. Future Oncol. 2018;14(6):567–575. doi: 10.2217/fon-2017-0486. [DOI] [PubMed] [Google Scholar]
- 3.Goldstraw P, Ball D, Jett JR, et al. Non-small-cell lung cancer. Lancet. 2011;378(9804):1727–1740. doi: 10.1016/S0140-6736(10)62101-0. [DOI] [PubMed] [Google Scholar]
- 4.Berhoune M, Banu E, Scotte F, Prognon P, Oudard S, Bonan B. Therapeutic strategy for treatment of metastatic non-small cell lung cancer. Ann Pharmacother. 2008;42(11):1640–1652. doi: 10.1345/aph.1L200. [DOI] [PubMed] [Google Scholar]
- 5.Herbst RS, Morgensztern D, Boshoff C. The biology and management of non-small cell lung cancer. Nature. 2018;553(7689):446–454. doi: 10.1038/nature25183. [DOI] [PubMed] [Google Scholar]
- 6.Riihimäki M, Hemminki A, Fallah M, et al. Metastatic sites and survival in lung cancer. Lung Cancer. 2014;86(1):78–84. doi: 10.1016/j.lungcan.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 7.Quint LE, Tummala S, Brisson LJ, et al. Distribution of distant metastases from newly diagnosed non-small cell lung cancer. Ann Thorac Surg. 1996;62(1):246–250. doi: 10.1016/0003-4975(96)00220-2. [DOI] [PubMed] [Google Scholar]
- 8.D’Antonio C, Passaro A, Gori B, et al. Bone and brain metastasis in lung cancer: recent advances in therapeutic strategies. Ther Adv Med Oncol. 2014;6(3):101–114. doi: 10.1177/1758834014521110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dawe DE, Greenspoon JN, Ellis PM. Brain metastases in non-small-cell lung cancer. Clin Lung Cancer. 2014;15(4):249–257. doi: 10.1016/j.cllc.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 10.Taimur S, Edelman MJ. Treatment options for brain metastases in patients with non-small-cell lung cancer. Curr Oncol Rep. 2003;5(4):342–346. doi: 10.1007/s11912-003-0077-8. [DOI] [PubMed] [Google Scholar]
- 11.Waqar SN, Samson PP, Robinson CG, et al. Non-small-cell lung cancer with brain metastasis at presentation. Clin Lung Cancer. 2018;19(4):e373–e379. doi: 10.1016/j.cllc.2018.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ulahannan D, Khalifa J, Faivre-Finn C, Lee SM. Emerging treatment paradigms for brain metastasis in non-small-cell lung cancer: an overview of the current landscape and challenges ahead. Ann Oncol. 2017;28(12):2923–2931. doi: 10.1093/annonc/mdx481. [DOI] [PubMed] [Google Scholar]
- 13.Mulvenna PM. The management of brain metastases in patients with non-small cell lung cancer – is it time to go back to the drawing board? Clin Oncol (R Coll Radiol) 2010;22(5):365–373. doi: 10.1016/j.clon.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 14.Tsakonas G, De Petris L, Ekman S. Management of brain metastasized non-small cell lung cancer (NSCLC) – from local treatment to new systemic therapies. Cancer Treat Rev. 2017;54:122–131. doi: 10.1016/j.ctrv.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Won YK, Lee JY, Kang YN, et al. Stereotactic radiosurgery for brain metastasis in non-small cell lung cancer. Radiat Oncol J. 2015;33(3):207–216. doi: 10.3857/roj.2015.33.3.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khuntia D, Brown P, Li J, Mehta MP. Whole-brain radiotherapy in the management of brain metastasis. J Clin Oncol. 2006;24(8):1295–1304. doi: 10.1200/JCO.2005.04.6185. [DOI] [PubMed] [Google Scholar]
- 17.Zimmermann S, Dziadziuszko R, Peters S. Indications and limitations of chemotherapy and targeted agents in non-small cell lung cancer brain metastases. Cancer Treat Rev. 2014;40(6):716–722. doi: 10.1016/j.ctrv.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 18.Tabchi S, Kourie HR, Klastersky J. Concurrent driver mutations/rearrangements in non-small-cell lung cancer. Curr Opin Oncol. 2017;29(2):118–122. doi: 10.1097/CCO.0000000000000353. [DOI] [PubMed] [Google Scholar]
- 19.Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin–paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–957. doi: 10.1056/NEJMoa0810699. [DOI] [PubMed] [Google Scholar]
- 20.Brown T, Boland A, Bagust A, et al. Gefitinib for the first-line treatment of locally advanced or metastatic non-small cell lung cancer. Health Technol Assess. 2010;14(Suppl 2):71–79. doi: 10.3310/hta14suppl2/10. [DOI] [PubMed] [Google Scholar]
- 21.Maemondo M, Inoue A, Kobayashi K, et al. North-East Japan Study Group Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362(25):2380–2388. doi: 10.1056/NEJMoa0909530. [DOI] [PubMed] [Google Scholar]
- 22.Mitsudomi T, Morita S, Yatabe Y, et al. West Japan Oncology Group Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised Phase 3 trial. Lancet Oncol. 2010;11(2):121–128. doi: 10.1016/S1470-2045(09)70364-X. [DOI] [PubMed] [Google Scholar]
- 23.Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (optimal, CTONG-0802): a multicentre, open-label, randomised, Phase 3 study. Lancet Oncol. 2011;12(8):735–742. doi: 10.1016/S1470-2045(11)70184-X. [DOI] [PubMed] [Google Scholar]
- 24.Heon S, Yeap BY, Britt GJ, et al. Development of central nervous system metastases in patients with advanced non-small cell lung cancer and somatic EGFR mutations treated with gefitinib or erlotinib. Clin Cancer Res. 2010;16(23):5873–5882. doi: 10.1158/1078-0432.CCR-10-1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee YJ, Choi HJ, Kim SK, et al. Frequent central nervous system failure after clinical benefit with epidermal growth factor receptor tyrosine kinase inhibitors in Korean patients with nonsmall-cell lung cancer. Cancer. 2010;116(5):1336–1343. doi: 10.1002/cncr.24877. [DOI] [PubMed] [Google Scholar]
- 26.Bhatt VR, Kedia S, Kessinger A, Ganti AK. Brain metastasis in patients with non-small-cell lung cancer and epidermal growth factor receptor mutations. J Clin Oncol. 2013;31(25):3162–3164. doi: 10.1200/JCO.2013.49.8915. [DOI] [PubMed] [Google Scholar]
- 27.Shin DY, Na II, Kim CH, Park S, Baek H, Yang SH. EGFR mutation and brain metastasis in pulmonary adenocarcinomas. J Thorac Oncol. 2014;9(2):195–199. doi: 10.1097/JTO.0000000000000069. [DOI] [PubMed] [Google Scholar]
- 28.Heon S, Yeap BY, Lindeman NI, et al. The impact of initial gefitinib or erlotinib versus chemotherapy on central nervous system progression in advanced non-small cell lung cancer with EGFR mutations. Clin Cancer Res. 2012;18(16):4406–4414. doi: 10.1158/1078-0432.CCR-12-0357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iuchi T, Shingyoji M, Sakaida T, et al. Phase II trial of gefitinib alone without radiation therapy for Japanese patients with brain metastases from EGFR-mutant lung adenocarcinoma. Lung Cancer. 2013;82(2):282–287. doi: 10.1016/j.lungcan.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 30.Han JY, Park K, Kim SW, et al. First-SIGNAL: first-line single-agent Iressa versus gemcitabine and cisplatin trial in never-smokers with adenocarcinoma of the lung. J Clin Oncol. 2012;30(10):1122–1128. doi: 10.1200/JCO.2011.36.8456. [DOI] [PubMed] [Google Scholar]
- 31.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45(2):228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 32.Chen AP, Setser A, Anadkat MJ, et al. Grading dermatologic adverse events of cancer treatments: the common terminology criteria for adverse events version 4.0. J Am Acad Dermatol. 2012;67(5):1025–1039. doi: 10.1016/j.jaad.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 33.Simoff MJ, Lally B, Slade MG, et al. Symptom management in patients with lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e455S–e497S. doi: 10.1378/chest.12-2366. [DOI] [PubMed] [Google Scholar]
- 34.Wu YL, Zhou C, Cheng Y, et al. Erlotinib as second-line treatment in patients with advanced non-small-cell lung cancer and asymptomatic brain metastases: a Phase II study (CTONG-0803) Ann Oncol. 2013;24(4):993–999. doi: 10.1093/annonc/mds529. [DOI] [PubMed] [Google Scholar]
- 35.Yang JJ, Zhou C, Huang Y, et al. Icotinib versus whole-brain irradiation in patients with EGFR-mutant non-small-cell lung cancer and multiple brain metastases (brain): a multicentre, Phase 3, open-label, parallel, randomised controlled trial. Lancet Respir Med. 2017;5(9):707–716. doi: 10.1016/S2213-2600(17)30262-X. [DOI] [PubMed] [Google Scholar]
- 36.Chen Y, Yang J, Li X, et al. First-line epidermal growth factor receptor (EGFR)-tyrosine kinase inhibitor alone or with whole-brain radiotherapy for brain metastases in patients with EGFR-mutated lung adenocarcinoma. Cancer Sci. 2016;107(12):1800–1805. doi: 10.1111/cas.13079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Magnuson WJ, Yeung JT, Guillod PD, Gettinger SN, Yu JB, Chiang VL. Impact of deferring radiation therapy in patients with epidermal growth factor receptor-mutant non-small cell lung cancer who develop brain metastases. Int J Radiat Oncol Biol Phys. 2016;95(2):673–679. doi: 10.1016/j.ijrobp.2016.01.037. [DOI] [PubMed] [Google Scholar]
- 38.Liu Y, Deng L, Zhou X, et al. Concurrent brain radiotherapy and EGFR-TKI may improve intracranial metastases control in non-small cell lung cancer and have survival benefit in patients with low DS-GPA score. Oncotarget. 2017;8(67):111309–111317. doi: 10.18632/oncotarget.22785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Magnuson WJ, Lester-Coll NH, Wu AJ, et al. Management of brain metastases in tyrosine kinase inhibitor-naïve epidermal growth factor receptor-mutant non-small-cell lung cancer: a retrospective multi-institutional analysis. J Clin Oncol. 2017;35(10):1070–1077. doi: 10.1200/JCO.2016.69.7144. [DOI] [PubMed] [Google Scholar]
- 40.Welsh JW, Komaki R, Amini A, et al. Phase II trial of erlotinib plus concurrent whole-brain radiation therapy for patients with brain metastases from non-small-cell lung cancer. J Clin Oncol. 2013;31(7):895–902. doi: 10.1200/JCO.2011.40.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Banks WA. From blood–brain barrier to blood–brain interface: new opportunities for CNS drug delivery. Nat Rev Drug Discov. 2016;15(4):275–292. doi: 10.1038/nrd.2015.21. [DOI] [PubMed] [Google Scholar]
- 42.Upadhyay RK. Drug delivery systems, CNS protection, and the blood brain barrier. Biomed Res Int. 2014;2014:869269. doi: 10.1155/2014/869269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khalifa J, Amini A, Popat S, Gaspar LE, Faivre-Finn C, International Association for the Study of Lung Cancer Advanced Radiation Technology Committee Brain metastases from NSCLC: radiation therapy in the era of targeted therapies. J Thorac Oncol. 2016;11(10):1627–1643. doi: 10.1016/j.jtho.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 44.Zhang J, Yu J, Sun X, Meng X. Epidermal growth factor receptor tyrosine kinase inhibitors in the treatment of central nerve system metastases from non-small cell lung cancer. Cancer Lett. 2014;351(1):6–12. doi: 10.1016/j.canlet.2014.04.019. [DOI] [PubMed] [Google Scholar]
- 45.Johung KL, Yao X, Li F, et al. A clinical model for identifying radio-sensitive tumor genotypes in non-small cell lung cancer. Clin Cancer Res. 2013;19(19):5523–5532. doi: 10.1158/1078-0432.CCR-13-0836. [DOI] [PubMed] [Google Scholar]
- 46.Spano JP, Fagard R, Soria JC, Rixe O, Khayat D, Milano G. Epidermal growth factor receptor signaling in colorectal cancer: preclinical data and therapeutic perspectives. Ann Oncol. 2005;16(2):189–194. doi: 10.1093/annonc/mdi057. [DOI] [PubMed] [Google Scholar]
- 47.Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009;10(11):1037–1044. doi: 10.1016/S1470-2045(09)70263-3. [DOI] [PubMed] [Google Scholar]
- 48.Habets EJ, Dirven L, Wiggenraad RG, et al. Neurocognitive functioning and health-related quality of life in patients treated with stereotactic radiotherapy for brain metastases: a prospective study. Neuro Oncol. 2016;18(3):435–444. doi: 10.1093/neuonc/nov186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yang WC, Xiao F, Shih JY, et al. Epidermal growth factor receptor mutation predicts favorable outcomes in non-small cell lung cancer patients with brain metastases treated with stereotactic radiosurgery. Radiother Oncol. 2018;126(2):368–374. doi: 10.1016/j.radonc.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 50.Lin X, DeAngelis LM. Treatment of brain metastases. J Clin Oncol. 2015;33(30):3475–3484. doi: 10.1200/JCO.2015.60.9503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lin J, Jandial R, Nesbit A, Badie B, Chen M. Current and emerging treatments for brain metastases. Oncology (Williston Park) 2015;29(4):250–257. [PubMed] [Google Scholar]
- 52.Malapelle U, Ricciuti B, Baglivo S, et al. Osimertinib. Recent Results Cancer Res. 2018;211:257–276. doi: 10.1007/978-3-319-91442-8_18. [DOI] [PubMed] [Google Scholar]
- 53.Vansteenkiste J, Reungwetwattana T, Nakagawa K, et al. CNS response to osimertinib vs standard of care (SoC) EGFR-TKI as first-line therapy in patients (pts) with EGFR-TKI sensitising mutation (EGFRm)-positive advanced non-small cell lung cancer (NSCLC): data from the FLAURA study. Ann Oncol. 2017;28(suppl_10):mdx782. [Google Scholar]
- 54.Cho BC, Chewaskulyong B, Lee KH, et al. Osimertinib versus standard of care EGFR TKI as first-line treatment in patients with EGFRm advanced NSCLC: FLAURA Asian subset. J Thorac Oncol. 2019;14(1):99–106. doi: 10.1016/j.jtho.2018.09.004. [DOI] [PubMed] [Google Scholar]


