Abstract
Schwannoma or neurilemmoma is a benign, slow-growing nerve sheath tumor arising from Schwann cells of the cranial, peripheral or autonomic nerves. Approximately 25%–40% of schwannomas occur in the head and neck region. Occurrences of intraoral schwannomas are rare with reported prevalence being 1%. Intraorally, schwannomas occur in the tongue, palate, buccal mucosa, lips and gingiva. This article provides an insight into a rare case of palatal schwannoma with literature review.
Keywords: Antoni A, Antoni B, S100, schwannoma, soft palate
INTRODUCTION
Schwannoma also called as neurilemmoma, neurinoma and perineural fibroblastoma is a solitary, slow-growing, benign neural tumor. It was first described by Verocay in 1908.[1,2,3,4] They can arise from cranial, peripheral or autonomic nerves.[5] Extracranial schwannoma is common in the head-and-neck region with the rate of occurrence of 25%–40% whereas intraoral occurrence is only about 1%.
CASE REPORT
A 43-year-old man presented to the outpatient clinic with complaints of swelling in the oral cavity and discomfort during swallowing for the past 1 month. He complained of pain only when the lesion was poked. There was no history of paraesthesia. Medical history was noncontributory. Inspection of the oral cavity revealed a solitary sessile swelling of size 2 × 2 cm and oval in shape in the region of the right soft palate extending into the hard palate. Surface of the mucosa over the swelling was smooth, with mild erythema on the superior surface. The margins were well defined with no evidence of any secondary changes. On palpation, it was nontender and firm in consistency [Figure 1]. The regional lymph nodes were not palpable. A provisional diagnosis of benign salivary gland neoplasm probably adenoma was made. The probable differential diagnoses considered were fibroma, neurofibroma, retention cyst and infected palatal cyst. Further investigations were done. Intraoral radiograph in the region of the left upper posterior teeth did not reveal any significant pathology [Figure 2]. Occlusal radiograph [Figure 3] and orthopantomograph [Figure 4] showed the presence of a periapical radiolucent lesion in relation to nonvital left upper central incisor. No features of erosion of the palatal cortex were noticed in the occlusal radiograph and orthopantomograph. Contrast computed tomography (CT) revealed enhanced soft tissue density with attenuation of +30 Hounsfield units in the left posterior palate region suggestive of a soft tissue mass probably of muscular or neuronal origin [Figure 5]. Incisional biopsy was done, and the tissue was sent for histopathological examination. Histopathological examination revealed the presence of characteristic Antoni A and Antoni B areas blending imperceptibly [Figures 6 and 7]. Antoni A areas were composed of compact spindle cells with wavy nuclei and indistinct cytoplasmic borders. They were arranged in short bundles or interlacing fascicles. Highly differentiated Antoni A areas with nuclear palisading, whorling of cells and Verocay bodies were also observed, Verocay bodies are two compact rows of cells with well-aligned nuclei separated by homogeneous eosinophilic areas. Antoni B areas were less orderly and less cellular. The spindle or oval cells were arranged haphazardly in the loosely textured matrix composed of delicate collagen fibers. Mild, diffuse inflammatory cell infiltrate is seen. An immunohistochemical examination of the tumor showed strong and uniform positivity with S100 antigen [Figure 8]. Clinical behavior, histopathological findings and immunohistochemistry confirmed the diagnosis of schwannoma.
Figure 1.

Swelling involving the left hard and soft palate
Figure 2.

Intraoral radiograph on 25, 26 and 27 regions showing no significant periapical pathology
Figure 3.

Periapical radiolucent lesion in relation to nonvital 21 and no features of erosion of the palatal cortex were noticed in the occlusal radiograph
Figure 4.

Orthopantomograph showed the presence of a periapical radiolucent lesion in relation to nonvital 21
Figure 5.

Enhanced soft tissue density with attenuation of +30 Hounsfield units in the left posterior palate region (arrow) suggestive of a soft tissue mass probably of muscular or neuronal origin
Figure 6.
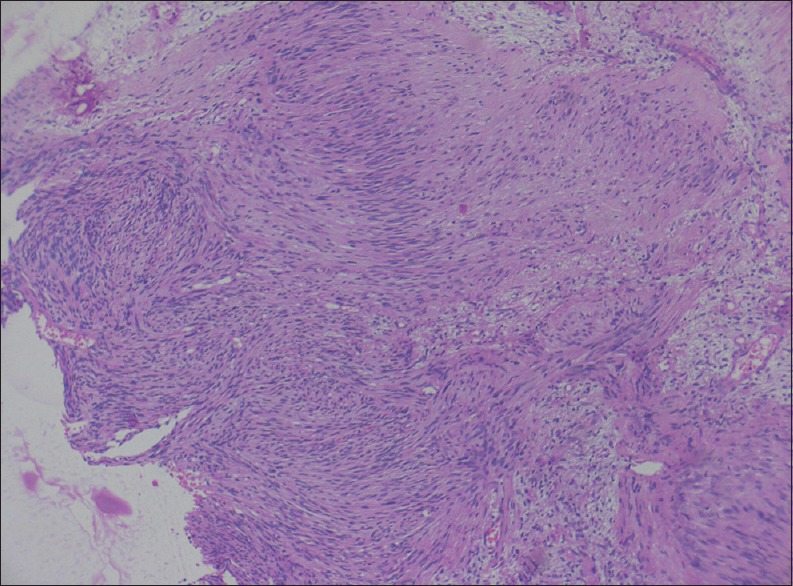
Antoni A and Antoni B areas (H&E, ×10)
Figure 7.
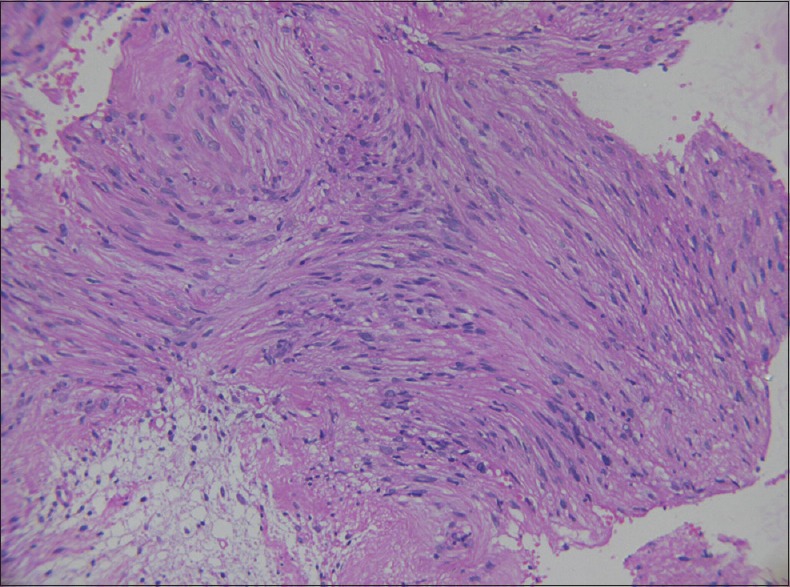
Antoni A areas with Verocay bodies (×40)
Figure 8.
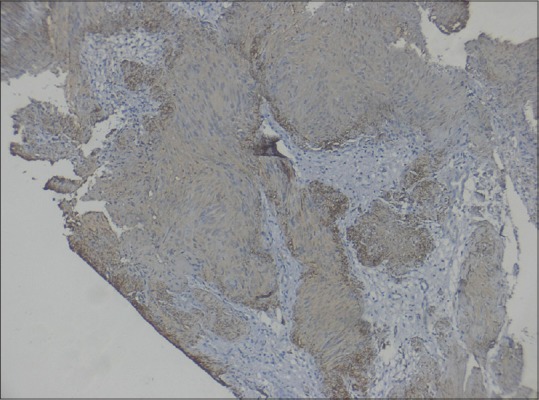
Antoni A and Antoni B areas showing diffuse S100 positivity (immunostain-S100)
The lesion was removed under general anesthesia [Figure 9]. Gross inspection of the lesion revealed a grayish, well-circumscribed mass, approximately 3 cm × 2 cm × 2 cm in size [Figure 10]. Histopathology of the excised specimen also confirmed as schwannoma. After 6 months of follow-up, no evidence of recurrence was detected.
Figure 9.

Intraoperative image
Figure 10.
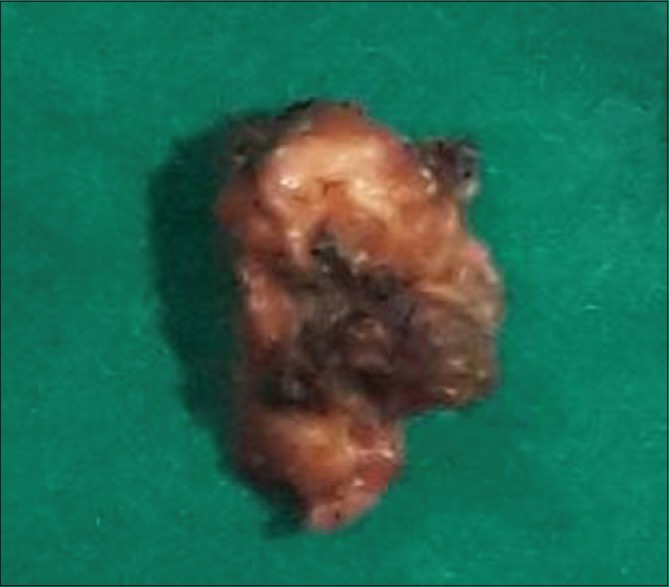
Excised specimen
DISCUSSION
Schwannoma also called as neurilemmoma, neurinoma and perineural fibroblastoma is a solitary, slow-growing, benign neural tumor. It was first described by Verocay in 1908.[1,2,3,4] The tumor is derived from Schwann cells which produce the myelin sheath covering the peripheral nerve. They can arise from cranial, peripheral or autonomic nerves.[5] They are usually encapsulated, generally asymptomatic and composed of Schwann cells. Schwannomas are present outside the nerve. As the tumor enlarges, it causes displacement and compression of the nerve of origin.[6,7] Although it can occur at any age, they are more common around the second to the third decade of life. Literature shows more female predilection, but the present case was occurred in a male patient.
Extracranial schwannoma is common in the head-and-neck region with the rate of occurrence of 25%–40% whereas intraoral occurrence is only about 1%.[8] Oral schwannomas are usually present in the soft tissue, more commonly the tongue, followed by palate and buccal mucosa and may have clinical features similar to other benign lesions such as mucocele, fibroma, neurofibroma, lipoma and benign salivary gland tumor.[6,9] On occasion, if the tumor arises centrally within the bone, they may produce bony expansion. Intraosseous schwannomas are most common in the posterior mandible and usually appear as either unilocular or multilocular radiolucencies on radiographs. Pain and paresthesia are not unusual for intrabony tumors. Patients with multiple nerve schwannomas should be evaluated for von Recklinghausen's disease. Asaumi et al.,[10] in their study, described that ultrasonography, CT and magnetic resonance imaging may be helpful as a diagnostic and treatment tool, for the estimation of tumor margins and the determination of infiltration to surrounding structures. In this case, contrast CT revealed enhanced soft tissue density with an attenuation value of +30 Hounsfield units in the palate with no infiltration into the surrounding tissues. Schwannomas are histopathologically characterized by a mixture of two patterns of tissue growth, namely, Antoni type A and B. Antoni A type is made up of spindle-shaped Schwann cells which are aligned to form a characteristic palisading around Verocay bodies. Verocay bodies are central acellular eosinophilic, hyaline structures which consist of reduplicated basement membrane and cytoplasmic processes.[11] Mitotic figures are occasionally present. Antoni B tissue does not exhibit this characteristic palisading. It demonstrates disorderly arrangement of cells and fibers in a loose myxomatous stroma. Ancient schwannoma is a rare type of schwannoma in which degenerative changes can be noted. These changes consist of cyst formation, necrosis, hyalinization, hemorrhage, hemosiderin deposits, inflammation, fibrosis and nuclear atypia.[12] The immunohistochemical markers S100 are used in most cases to confirm the Schwann cell origin of these tumors and confirm diagnosis.[13] Local excision is the treatment of choice. The nonencapsulated form requires a margin of normal tissue, and careful separation from the involved nerve is also necessary to preserve normal function.[2,7,9,14] Although recurrence is rare, malignant transformation of a benign schwannoma is also reported.[15,16] The prognosis is good.
CONCLUSION
Schwannoma is present as a slow-growing painless swelling in the oral cavity not often encountered in clinical practice. This submucosal lesion must be differentiated from other benign lesions that also appear in the same region. Prognosis is good and recurrence is rare.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chi AC, Carey J, Muller S. Intraosseous schwannoma of the mandible: A case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:54–65. doi: 10.1016/s1079-2104(03)00228-2. [DOI] [PubMed] [Google Scholar]
- 2.Parikh RN, Desai N. Intraoral schwannoma (neurilemmoma): An unusual anterior palatal swelling-a case report. J. Int Oral Health. 2010;2:87–91. [Google Scholar]
- 3.Shafer GW, Hine KM, Levy B. A Textbook of Oral Pathology. 4th ed. Bangalore: Prism books (PVT.) LDT; 1993. Benign and Malignant Tumors of the Oral Cavity; pp. 208–10. [Google Scholar]
- 4.Naidu GS, Sinha SM. Schwannoma of the tongue: An unusual presentation in a child. Indian J Dent Res. 2010;21:457–9. doi: 10.4103/0970-9290.70790. [DOI] [PubMed] [Google Scholar]
- 5.Lollar KW, Pollak N, Liess BD, Miick R, Zitsch RP., 3rd Schwannoma of the hard palate. Am J Otolaryngol. 2010;31:139–40. doi: 10.1016/j.amjoto.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 6.Martins MD, Anunciato de Jesus L, Fernandes KP, Bussadori SK, Taghloubi SA, Martins MA, et al. Intra-oral schwannoma: Case report and literature review. Indian J Dent Res. 2009;20:121–5. doi: 10.4103/0970-9290.49059. [DOI] [PubMed] [Google Scholar]
- 7.Zachariades N, Skoura C, Papageorgiou G, Chrissomali E. Giant ancient neurilemmoma of the cervical region: Report of case. J Oral Maxillofac Surg. 2001;59:668–72. doi: 10.1053/joms.2001.23399. [DOI] [PubMed] [Google Scholar]
- 8.Pfeifle R, Baur DA, Paulino A, Helman J. Schwannoma of the tongue: Report of 2 cases. J Oral Maxillofac Surg. 2001;59:802–4. doi: 10.1053/joms.2001.24298. [DOI] [PubMed] [Google Scholar]
- 9.Baliga M, Uppal N, Ramanathan A. Schwannomas of the head and neck: A case series. J Maxillofac Oral Surg. 2009;8:283–6. doi: 10.1007/s12663-009-0069-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asaumi J, Konouchi H, Kishi K. Schwannoma of the upper lip: Ultrasound, CT, and MRI findings. J Oral Maxillofac Surg. 2000;58:1173–5. doi: 10.1053/joms.2000.9584. [DOI] [PubMed] [Google Scholar]
- 11.Yaga US, Mengji AK, Besta R, Gollamudi N. Rare case of palatal schwannoma: Case report and review of literature. J Indian Acad Oral Med Radiol. 2015;27:484–7. [Google Scholar]
- 12.Kargahi N, Razavi SM, Hasheminia D, Keshani F, Safaei M, Hashemzadeh Z. Mandibular intraosseous schwannoma in a child: Report of a rare case. Dent Res J (Isfahan) 2012;9(Suppl 1):S119–22. [PMC free article] [PubMed] [Google Scholar]
- 13.Lira RB, Gonçalves Filho J, Carvalho GB, Pinto CA, Kowalski LP. Lingual schwannoma: Case report and review of the literature. Acta Otorhinolaryngol Ital. 2013;33:137–40. [PMC free article] [PubMed] [Google Scholar]
- 14.Yamazaki H, Kaneko A, Ota Y, Tsukinoki K. Schwannoma of the mental nerve: Usefulness of preoperative imaging: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:122–6. doi: 10.1016/s1079-2104(03)00462-1. [DOI] [PubMed] [Google Scholar]
- 15.Dicerbo M, Sciubba JJ, Sordill WC, Deluke MD. Malignant schwannoma of the palate: A case report and review of the literature. J Oral Maxillofac Surg. 1992;50:1217–21. doi: 10.1016/0278-2391(92)90157-u. [DOI] [PubMed] [Google Scholar]
- 16.Hatziotis JC, Asprides H. Neurilemoma (schwannoma) of the oral cavity. Oral Surg Oral Med Oral Pathol. 1967;24:510–26. doi: 10.1016/0030-4220(67)90431-8. [DOI] [PubMed] [Google Scholar]


