Abstract
Background: The limited success of conventional anticraving interventions encourages research into new treatment strategies. Heart rate variability biofeedback (HRVB), which is based on slowed breathing, was shown to improve symptom severity in various disorders. HRVB, and certain rates of controlled breathing (CB), may offer therapeutic potential as a complementary drug-free treatment option to help control substance craving.
Methods: This review evaluated current evidence on the effectiveness of HRVB and CB training as a complementary anticraving intervention, based on guidelines from the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols. Studies that assessed a cardiorespiratory feedback or CB intervention with substance craving as an outcome were selected. Effect sizes were calculated for each study. The Scale for Assessing Scientific Quality of Investigations in Complementary and Alternative Medicine was used to evaluate the quality of each study reviewed.
Results: A total of eight articles remained for final review, including controlled studies with or without randomization, as well as noncontrolled trials. Most studies showed positive results with a variety of methodological quality levels and effect size. Current HRVB studies rated moderately on methodological rigor and showed inconsistent magnitudes of calculated effect size (0.074–0.727) across populations. The largest effect size was found in a nonclinical college population of high food cravers utilizing the most intensive HRVB training time of 240 min.
Conclusions: Despite the limitations of this review, there is beginning evidence that HRVB and CB training can be of significant therapeutic potential. Larger clinical trials are needed with methodological improvements such as longer treatment duration, adequate control conditions, measures of adherence and compliance, longitudinal examination of craving changes, and more comprehensive methods of craving measurement.
Keywords: : craving, heart rate variability biofeedback, substance use disorder, complementary, anticraving intervention
Introduction
Recovery from substance use disorder (SUD) is difficult to maintain. Within the first year of SUD treatment, relapse occurs in 50%–70% of recovering patients.1,2 While many factors may be associated, craving is one of the strongest and most distressing predictors of relapse.3–5 Recent research advancements showed that craving can still be experienced years after abstinence.6 Currently, craving is a criterion for SUD diagnoses,7 and anticraving intervention is an essential component of recovery maintenance and relapse prevention.8,9
Craving is a highly subjective experience with virtually no universal definition. Although craving has inspired thousands of articles in the literature, components of the craving construct remain controversial.9,10 Advances in neuroimaging research resulted in novel views of craving as a phenomenon of psychobiologic origins, highlighting biologic factors of craving with an emphasis on motivational components.10,11 Specifically, changes in the mesolimbic dopamine pathways have been recognized as sites for the reinforcing properties of addictive drugs.12,13 Substance craving is associated with increased activity in limbic, striatal, and cortical brain systems.13,14 The most prominent theory from this view is the incentive-sensitization theory, which explains the mechanism of craving by neurobiologic adaptations of brain circuits regulating motivated behavior and cognitive decision-making.15 Repeated drug exposure sensitizes the brain to drug stimuli resulting in pathologic incentive salience, a motivational “wanting” attribute given by the brain to reward predicting stimuli ascribed to the drug.15,16 Dysregulation in dopamine, serotonin, gamma-aminobutyric acid, endogenous opioid peptides, and noradrenalin functions has been associated with activation of the brain's reward center resulting in incentive salience.6,14,15,17 From this neurobiologic standpoint, craving is defined as an intense abnormal desire and physiologic need for a particular drug or food.14,18 Current pharmacologic, behavioral, and combination treatments for substance craving are based on these premises.19
Conventional substance craving treatments
Treatment for substance craving is generally integrated within every stage of recovery from SUD starting with detoxification through maintenance of abstinence. Available treatment approaches include pharmacologic interventions, behavioral counseling, support groups, and evaluation and treatment for co-occurring mental health issues.8 Studies show that no single approach to recovery is effective alone.20 Combinations of pharmacologic and behavioral interventions have been found more effective than a single approach in terms of long-term recovery outcomes.8 Despite treatment advancements, patient outcomes have not changed much, and maintaining recovery is still a major challenge.1,21–23 Given that craving is one of the strongest predictors of relapse,11,24 the need to identify additional and effective anticraving interventions is evident.
Complementary and alternative medicine in craving control
The limitations of conventional therapies in maintaining abstinence and preventing relapse resulted in attempts at using complementary and alternative medicine (CAM) practices.25 CAM therapies such as mind–body practices, biofeedback and neurofeedback, auricular acupuncture, homeopathic and naturopathic medicine, ayurvedic preparations, and bioelectromagnetic therapies have been used in the treatment of SUD.21 Anecdotal evidence of the effectiveness of CAM therapies in SUD treatment has existed for more than 25 years although research evidence has been limited.25 However, available evidence supports the use of mind–body practices, biofeedback, neurofeedback, and acupuncture as adjuvant therapies in the treatment of SUD. Acupuncture is widely used as a CAM treatment for opioid addiction in both Western and Asian countries.25 Yet, a meta-analysis of 14 published acupuncture trials showed that treatment and control groups did not differ on opioid craving although symptoms of anxiety and depression were improved in treatment groups.26 Positive results of greater craving reduction have been reported when acupuncture was used as an adjuvant treatment to methadone maintenance.27 Furthermore, mind–body therapies are widely used to reduce stress effects and have been used to reduce cravings. Such therapies focus on the interactions among brain, mind, body, and behavior. A review of 14 smoking cessation trials showed that yoga and meditation-based interventions were effective in reducing nicotine craving intensity.20 Qigong meditation also led to significantly greater substance craving reduction than did stress management and relaxation training, when used as an adjuvant to residential treatment for SUD.28,29 In addition, there is growing evidence on the efficacy of mindfulness meditation,30 which was shown to reduce brain activity in regions related to craving.24 Mindfulness-based interventions showed reductions in craving for smoking,31 alcohol,32 and binge drinking in college students.33,34 Although mindfulness shows very positive postintervention craving outcomes, more evidence is needed on its long-term effectiveness.35 Along with mind–body practices, biofeedback is a therapeutic procedure that facilitates mind–body interaction.36 Different biofeedback techniques, including neurofeedback training37,38 and heart rate variability biofeedback (HRVB),39,40 showed promise in reducing drug and food18,41 craving. In this review the authors focus on HRVB that is based on slowed breathing.
The HRVB perspective
Biofeedback research has shown that humans can be trained, through operant conditioning, to control certain autonomic nervous system functions, such as cardiac responses, gastrointestinal contractions, and vasomotor activity.36,42 The objectives of biofeedback are to (1) help persons acquire awareness of the mind–body interaction, highlighting the interaction between thoughts and automatic physiologic responses; (2) acquire methods to control maladaptive physiologic responses with the help of physiologic monitoring; and (3) learn to regulate their thoughts and physiology in everyday life without the use of instrumentation.36,43 The goal is to improve autonomic regulation by engaging the parasympathetic nervous system and recovering from stress-induced sympathetic responses.44 Autonomic imbalances in sympathetic and parasympathetic systems have been reported with increased craving.14 Experiences of craving are often associated with physiologic responses such as increased salivation, heart rate, and blood pressure, as well as psychologic responses such as depression and anxiety.12,45 The experience of craving is therefore associated with moment-to-moment changes in physiologic states which contribute to the person's behavior.45–47 A flexible autonomic system provides the ability for rapid modulation of physiologic states in accordance with situational demands.43,48 Neurocardiac dynamics, such as heart rate variability (HRV), underlie the heart-brain feedback loop that contributes to behavioral flexibility.49,50 HRV is the variability in R- to R-spike intervals of the electrocardiogram that is regulated by neural mechanisms of the autonomic nervous system, reflecting efferent vagus and sympathetic nerve activity and afferent nerve activity mediated by the baroreceptors. High-frequency HRV reflects high-frequency heart rate oscillations (0.15–0.4 Hz) mediated by vagal activity.51 According to polyvagal theory, primary emotions are related to the vagal regulation of the heart, and different types of vagal activity (e.g., withdrawal or activation) support different behaviors. In line with this theory, evidence shows that HRV provides insight into the neural mechanisms of the flexible regulation of affective states and cognition.48,49,52 Research suggests that low HRV predicts craving in individuals with SUD.39,47 Increasing HRV may therefore improve autonomic homeostasis and behavioral flexibility48,49,53 and, thus, enhance craving control. HRVB is a form of cardiorespiratory feedback training that aims to increase HRV and enhance vagal heart rate control.50,54,55 In HRVB, users are trained to breathe at their own resonance frequency, which maximizes HRV by eliciting high-amplitude heart rate oscillations. In one empirically supported training approach, users are asked to breath slowly at a rate of 4.5–6.5 breaths per minute with frequencies ranging from 0.075 to 0.108 Hz.54 Resonance frequency is identified when respirations and heart rate oscillations occur in a phase (i.e., heart rate rises simultaneously with inhalation and decreases simultaneously with exhalation).45,56 Users are then trained to practice breathing at their own resonance frequency with the help of visual pacers and electronic monitoring of the heart rate. HRVB was shown to improve symptom severity of various disorders such as asthma, depression, anxiety, fibromyalgia, and hypertension.44,53,57,58 Controlled breathing (CB) paced at about 0.1 Hz (i.e., approximately five to six breaths per minute) provides a close proxy to the resonance breathing rate achieved in HRVB.56 The effectiveness of HRVB and CB in reducing substance craving will be discussed in this review.
Materials and Methods
Rationale and objectives
The limited success of current anticraving interventions encourages research into new treatment strategies. Because craving is a biobehavioral phenomenon that is modulated by physiologic, as well as cognitive processes, biobehavioral interventions, such as HRVB, offer therapeutic potential to aid substance craving control as a complementary or alternative drug-free treatment option. This review reports current evidence on the effectiveness of HRVB in reducing craving and the challenges of research in this area, using the Preferred reporting items for systematic review and meta-analysis protocols 2015.59 Due to the limited number of studies investigating HRVB and craving, the authors expanded their review to include research studying CB as an intervention to reduce craving. Although HRVB and CB use different training methodologies, both approaches are based on slowed rhythmic breathing at about five-to-six breaths per minute. The major difference between HRVB and CB is that during HRVB users receive feedback about their physiologic responses such as respirations and heart rate. Therefore, evidence from CB studies may help support the relationship between HRVB and craving. The purpose of this review is as follows: (1) to assess current evidence on the effectiveness of HRVB and other CB strategies in reducing craving and (2) to outline current methodological challenges and future directions for research examining HRVB as an anticraving intervention.
Literature search and article selection
A review of the existing literature was performed using combinations of the search terms: craving, urge, desire, HRVB, respiratory sinus arrhythmia biofeedback, cardiorespiratory feedback, and breathing. Databases searched included Social Sciences Citation Index, MEDLINE, PsycINFO, PubMed, Scopus, and Google Scholar. Only peer-reviewed articles were considered and abstracts were used to determine article relevance. No publication time or language limits were used. Literature searches ended in August 2017.
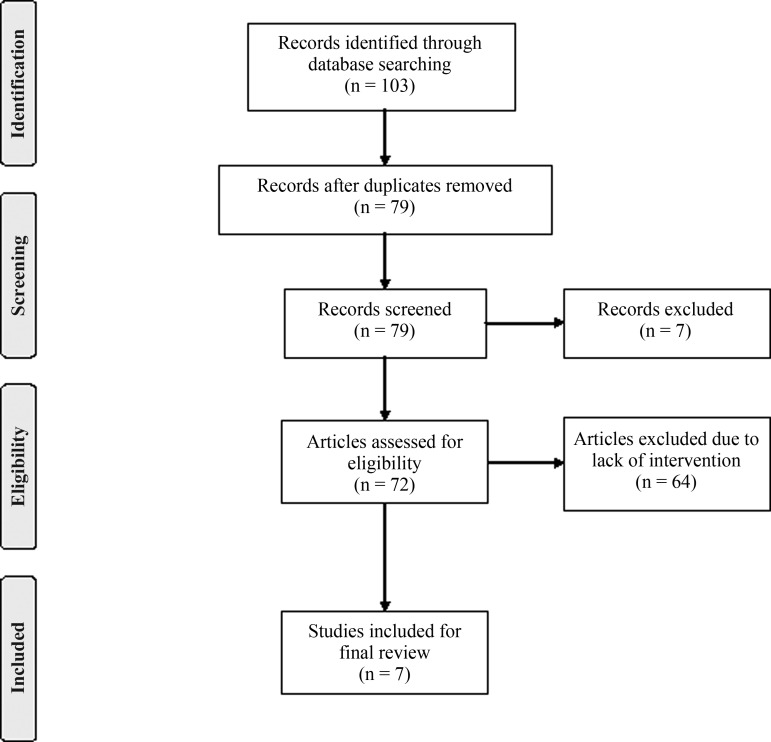
To be selected, studies had to address their primary research question by assessing a cardiorespiratory feedback or CB intervention with substance craving as a primary or secondary outcome, whether in a sample of persons with addictive disorders or other nonclinical samples. The initial search yielded 103 records of which 7 conference proceedings and book chapters were excluded. After abstract and full-text evaluation, a total of 95 articles were excluded due to duplication, observational and/or cross-sectional data, or lack of intervention, yielding a total of 8 articles for final review. Finally, the study protocol by Sarkar et al.60 was excluded because the study results were not found in the literature and communication with the authors failed. The final sample for review included seven research studies (Fig. 1), including controlled studies with or without randomization, as well as noncontrolled trials. The main features of the studies included in this review are shown in Tables 1 and 2.
FIG. 1.
PRISMA 2015 Flow Diagram.59 N.B.: “The PRISMA Statement document is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.”
Table 1.
Features of Studies Investigating Heart Rate Variability Biofeedback and Substance Craving
| Reference | Sample | Substance/diagnosis | HRVB training | Control | Craving measure | Findings |
|---|---|---|---|---|---|---|
| Eddie et al.39 | 20–25 years 100% male 28-day intensive inpatient United States |
Polysubstance SUD + Co-occurring Axis-I and Axis-II diagnoses |
n = 20; one 60–75 min session/week over 3 weeks (Total: 180–225 min) Handheld emWave device (20 min twice daily practice) |
n = 21 Rehabilitative treatment as usual (TAU) |
Adjusted PACS | HRVB intervention vs. control comparison Larger mean craving reduction (35.8% vs. 27.3%; t(39) = 0.99, p > 0.05) No chronic HRV changes at post-treatment baseline HRVB dose–response effect was not reported |
| Meule et al.18 | 18–40 years 11% male Nonclinical University setting Germany |
None; High food cravers selected |
n = 14; Twelve 20-min sessions over 4 weeks (Total: 240 min) No home practice |
Non-craving-control (NCC; n = 28) Craving-control (CC; n = 14) No treatments provided |
FCQ-T | HRVB intervention vs. control comparison Larger mean craving reduction in the HRVB group (13%; t(13) = 2.81, p < 0.05) vs. the NCC (7%; t(27) = 2.90, p < 0.01). No changes in CC. Stronger standard effect sizes in HRVB group (0.95) than in CC (0.01) and NCC (0.32) Vagal-cardiac control: No changes in HRVB group vs. decrease in CC |
| Penzlin et al.40 | 25–59 years 71% male Inpatient rehabilitation Germany |
Alcohol use disorder |
n = 24; Three 20-min sessions/week over 2 weeks (Total: 120 min) No home practice |
n = 24 Rehabilitative TAU |
OCDS | HRVB intervention vs. control comparison Larger mean craving reduction at week 2 (37.2%, p < 0.05 vs. nonsignificant change), smaller craving reduction at week 3 (45.2% vs. 68.9%; p < 0.05) and week 6 (44.5% vs. 72.4%; p < 0.05) Nonsignificant trend toward increase in CVNN following HRVB compared to baseline and control |
| Zucker et al.66 | 18–60 years 55% male Urban residential program (6 months to 1 year); United States |
Polysubstance SUD + elevated PTSD symptoms |
n = 19; 30-min StressEraser device training preintervention 20 min daily home practice over 4 weeks |
n = 19; Progressive Muscle Relaxation (PMR) 20 min daily over 4 weeks |
1 item (10-point scale); no craving to extreme craving | HRVB intervention vs. control comparison Larger mean craving reduction trend (40.9% vs. −1.6%; F(1, 34) = 2.52, p = 0.2) Increases in SDNN* at postintervention baseline (t(15) = −2.4, p = 0.03) vs. no changes in PMR group No dose–response effect found with no differences between high and low users of the StressEraser |
CC, craving-control; CVNN, coefficient of variation of normal-to-normal intervals; FCQ-T, food craving questionnaire-trait; HRV, heart rate variability; HRVB, heart rate variability biofeedback; NCC, non-craving-control; OCDS, obsessive compulsive drinking scale; PACS, Pennsylvania alcohol craving scale; PMR, Progressive Muscle Relaxation; SDNN, standard deviation of normal-to-normal intervals; SUD, substance use disorder; TAU, treatment as usual.
Table 2.
Features of Studies Investigating Controlled Breathing Interventions and Substance Craving
| Reference | Sample | Diagnosis | CB intervention | Control | Craving measure | Findings |
|---|---|---|---|---|---|---|
| De Zeni and Araujo69 | 18–40 years 100% male Detoxification unit Brazil |
Cocaine dependence |
n = 32; Deep breathing Total time: 10 min |
None | CCQB VAS |
Pre–post comparison Mean craving reduction of 32.1% in CCQB scores (t(32) = 4.55, p < 0.001) and 65.4% in VAS scores (t(32) = 6.32, p < 0.001) immediately after deep breathing |
| McClernon et al.67 | 18–60 years 33% male Community sample United States |
Nicotine dependence |
n = 21*; Controlled breathing over 12 sec every 30 min over 4 h Total time: 240 min |
n = 21*; Stayed in quiet room (light reading) | SJWQ - craving subscale | CB intervention vs. control comparison Larger mean craving reduction (F(1, 7) = 22.44, p = 0.002). Means and SDs were not reported. |
| Shahab et al.68 | 18–55 years 54% male Community sample United States |
Nicotine dependence |
n = 48; Yogic breathing (Total time: 15 min) Over 24 h Average yogic breathing of 7.7 times outside laboratory over 24 h |
n = 48; 10 min video about yogic breathing | Single item + SJWQ craving subscale | CB intervention vs. control comparison Immediately post-intervention, larger reduction in ‘strength of urges to smoke’ (F(1, 96) = 16.1, p < 0.001), “craving a cigarette now” (F(1, 96) = 16.1, p < 0.001), and “desire to smoke now” (F(1, 96) = 6.6, p = 0.012). Means and SDs were not reported. At 24 h follow-up, no craving reductions found except for participants who reported practicing yogic breathing “often” or “very often” (F(1, 46) = 4.0, p = 0.048) |
Same participants were randomized to control and treatment conditions. CB, controlled breathing; CCQB, cocaine craving questionnaire-brief; D, Cohen's d; dppc2, effect size based on pooled pretest standard deviation; SJWQ, Shiffman and Jarvik smoking withdrawal symptom questionnaire; VAS, visual analog scale.
Quality assessment
Due to the limited number of published studies addressing their research question, a formal meta-analysis of the literature was not possible. However, effect sizes were calculated, using the pooled pretest standard deviation to estimate the differences of the pre–post means, to provide a quantitative measure of the magnitude of observed effect for each study.61,62 This method provides an unbiased estimate of the population effect size and handles violations of assumptions of independence and homogeneity of variance.63 In addition, a qualitative systematic approach was used to further explore challenges and future directions of research studying HRVB as an anticraving intervention. The Scale for Assessing Scientific Quality of Investigations in CAM (SASQI-CAM) was used to evaluate the quality of each article, resulting in a numerical score between zero and 21. Satisfactory scientific quality has been attributed to studies with SASQI scores greater than 9. The SASQI approach takes into consideration challenges in CAM research such as establishing control conditions and blinding group assignment.20,64 The reviewed articles were rated independently by two authors on the SASQI. Interrater reliability for the seven SASQI scores rated by two authors was determined by an intraclass correlation, using a two-way random effects model.65
Results
HRV biofeedback studies
To date, four studies investigated the relationship between HRVB and craving using different populations, settings, and training methods, without yielding a definite conclusion on the effectiveness of HRVB in reducing substance craving. Two of those studies showed a trend in craving reductions with no statistical significance.39,66 Both studies were conducted in a residential SUD treatment setting and used relatively brief HRVB interventions (3–4 weeks). Zucker et al.66 investigated substance craving changes in a controlled pilot study of 38 patients with elevated post-traumatic stress disorder symptoms, following a home-based HRVB intervention. Participants were trained for 30 min on the use of a portable biofeedback device and were asked to practice slowed breathing for 20 min daily over the course of 4 weeks. Participants in the control group were asked to listen to a 20-min progressive muscle relaxation recording on daily basis. No substance craving differences were found between the biofeedback group and the progressive muscle relaxation group. However, the biofeedback group showed a trend of craving reduction following the intervention compared to no craving changes in the progressive muscle relaxation group.66 In this study, craving was only measured twice (before and after the intervention) using a single item. Poor measurement validity of craving may have therefore contributed to the lack of statistical significance in the results. In addition, the home-based nature of the intervention does not allow an assessment of adherence to the intervention. In contrast, the study by Eddie et al.39 administered formal three-session HRVB training over 3 weeks to young men (N = 41) receiving inpatient SUD treatment. A larger craving reduction trend was found in the HRVB group compared to the control group receiving treatment as usual. This finding was not statistically significant despite a medium effect size (Cohen's d = 0.35). The three-session HRVB training may have been insufficient to produce statistically significant craving reductions.39 Studies using longer interventions showed more promising results although more evidence is needed on the dose necessary to produce craving changes. In a nonclinical (N = 56) sample of high food cravers from a German university, participants showed statistically significant reduced food cravings following a 12-session HRVB intervention over 4 weeks.18 This study used an experimental group of high food cravers (craving-biofeedback group) and two control groups, a craving-control group of high food cravers and a low-craving control group of participants who reported low food cravings. Craving reductions were noted in the low-craving controls, while no changes occurred in the craving-control group. Notably, standardized effect sizes were consistently higher in the craving-biofeedback group than in both control groups. Biofeedback practice was limited to laboratory sessions, excluding home practice.18 Despite the promising evidence from this study, results may not be generalizable to clinical populations of substance users. A recent randomized controlled trial showed similar results in a sample of alcohol dependent persons from an inpatient rehabilitation center in Germany.40 Craving reductions occurred immediately following six 20-min HRVB training sessions given over 2 weeks in addition to standard rehabilitation treatment, compared to no craving changes in the control group. However, participants in the control group showed larger craving reductions, than the experimental group, at three and 6 weeks after the intervention. These findings suggest that HRVB contributed to earlier craving reduction than standard treatment alone, but the lack of HRVB effect and superiority of standard treatment at follow-up could not be explained.40 In conclusion, overall evidence suggests that HRVB is a promising adjunct to conventional craving treatment. Larger trials are needed to confirm its effectiveness and provide evidence about treatment duration and the amount of daily biofeedback practice that are necessary to produce immediate and long-term craving reductions in persons with SUD.
Biofeedback training methods and practice time
The aforementioned studies used different biofeedback training methods ranging from a 30-min handheld device training to a total of 240 min of laboratory-based HRVB training either with or without home breathing practice. An average 20-min daily breathing practice did not seem to produce statistically significant craving reductions in two of the studies although both found craving reduction trends.39,66 In addition, in one study no craving differences were found between high and low users of daily breathing practice.66 It is however difficult to assess whether these results were due to incorrect breathing practice or unreliable reports of daily practice time. In contrast, the use of a total 120 min HRVB formal training over 2 weeks40 and 240 min over 4 weeks18 with no daily breathing practice showed statistically significant craving reductions postintervention. Training session duration did not seem to affect craving reductions as much as the total amount of training in minutes regardless of the number of weeks. The exact amount and duration of HRVB training needed to produce craving reductions are still unclear. Future studies are needed to provide more evidence on the efficacy of daily breathing practice versus formal laboratory-based training. Identifying a specific training amount is essential to ensure a cost-effective intervention.
CB studies
Their search yielded a total of three studies investigating CB interventions in the treatment of substance craving (Table 2). These studies did not report the rate at which CB was conducted, except for McClernon et al.67 that used a breathing rate of five breaths per minute (i.e., similar to HRVB). Two of the CB studies used community samples of cigarette smokers who were asked to abstain from smoking for 12–24 h before the intervention. CB interventions were mostly based on relatively brief CB training, and results were limited to acute craving changes immediately postintervention. Two studies of different CB techniques showed significantly larger craving reductions in cigarette smokers immediately after the intervention compared to control groups not receiving CB training.67,68 Both studies used the craving subscale from the Shiffman and Jarvik Smoking Withdrawal Questionnaire to measure craving pre- and postbreathing training. Craving reductions were evident with both short (15 min)68 and long (240 min)67 CB breathing training although different breathing techniques were used. Shahab et al.68 reported a significant amount (average of 7.7 times) of CB practice outside laboratory hours over a period of 24 h after training. At 24 h follow-up, no craving reductions were found except for participants who reported practicing yogic breathing “often” or “very often.” Similarly, McClernon et al.67 concluded that craving reductions were related to continued use of deep breathing. Craving levels fluctuated over the course of 4 h before and after each breathing exercise, showing that craving reductions after the first breathing exercise were only maintained with continued use of deep breathing.67 Based on these results, a dose–effect relationship between CB and craving reduction may be evident in cigarette smokers abstaining from smoking for a short period of time. Similar postintervention craving reductions were reported in a sample of crack cocaine dependent persons (N = 32) who were offered 10 min of deep breathing training.69 However, the deep breathing intervention was accompanied with soft music, and no control group was used for comparison. It is therefore difficult to discern whether the craving reductions resulted from the breathing intervention or the calming effect of soft music or both. In conclusion, brief CB exercises showed effectiveness in acutely reducing craving immediately after the breathing exercise. A limitation of this research is that information was not provided about the temporal pacing of the CB interventions in most studies. More detailed methodological information is required to understand if underlying mechanisms of respiratory sinus arrhythmia and baroreceptor activation involved in HRVB are also active in the CB intervention. Evidence also is needed on the long-term effectiveness of CB in terms of craving reduction and the amount of practice needed for this relationship to hold. Although the mechanism of CB was not assessed in the reviewed studies, CB, depending on its rate, may share the same HRVB mechanism in terms of parasympathetic activation and restoration of autonomic balance.
Discussion
Effectiveness of HRVB and CB in reducing cravings
The literature supports HRVB training and CB as potential candidates to assist craving reduction in persons recovering from SUD, although a definitive conclusion was not possible. Their review yielded a varied range of methodological quality levels and effect size (Table 3). The reviewed HRVB articles were rated moderately on methodological rigor (SASQI = 11–14.5). CB articles showed a lower but wider range of SASQI scores (SASQI = 8–15). Interrater reliability for the seven articles showed high intraclass correlation of the SASQI scores rated independently by two authors. The single measure intraclass correlation was 0.92, and the average measure intraclass correlation was 0.96. Furthermore, the reviewed studies showed inconsistent magnitudes of calculated effect size (0.074–0.727) across populations. The largest effect size was found in a nonclinical college population of high food cravers utilizing the longest HRVB training time of 240 min. A small-to-moderate effect size was found in SUD populations from inpatient/residential settings except for the Penzlin et al.40 study which showed nearly zero effect of the 2-week HRVB on craving. In contrast, two of the three CB studies indicated modest methodological quality due to the lack of control and randomization, while one CB study was rated highly. Notwithstanding quality, all CB studies showed moderate-to-large effect size ranging from 0.413 to 1.498. The largest effect size was found in smoking cessation studies testing the same persons repeatedly67 and without control.69 Effect size may have been inflated due to dependency which usually yields a higher power62 or to differences in substance type (cigarettes vs. alcohol vs. other drugs). In general, CB studies were limited to brief pre–post assessment of craving which did not provide evidence on the long-term effectiveness of CB treatment. Taken together, of the seven studies reviewed, three HRVB and all three CB studies showed positive results with inconsistent effect size. The reasons behind this wide range of effect size may include cultural differences with 50% non-U.S. studies, treatment setting variations (which may impose various lengths of abstinence and treatment options), substance type, individual variations and comorbidities, treatment protocol and duration, and other methodological and validity related discrepancies. Although CB studies provided additional supportive evidence to the effectiveness of cardiorespiratory training in acutely reducing craving, more clinical trials with carefully monitored interventions are required to rigorously determine the long-term effects of HRVB as an anticraving treatment.
Table 3.
Effect Size and Quality Ratings Using the Scale for Assessing Scientific Quality of Investigations
| Reference | Study design | Intervention/duration | Effect size | SASQI score (average)* |
|---|---|---|---|---|
| De Zeni and Araujo69 | Pre–post | Deep breathing (10 min) | dCCQB = 1.026 | 8/21 |
| dVAS = 0.968 | ||||
| Eddie et al.39 | Controlled trial | HRVB (3 weeks) | dppc2 = 0.232 | 14.5/21 |
| McClernon et al.67 | Crossover trial | Controlled breathing (4 h) | d = 1.498 | 8/21 |
| Meule et al.18 | RCT | HRVB (4 weeks) | dppc2 = 0.727 | 14/21 |
| Penzlin et al.40 | RCT | HRVB (2 weeks) | dppc2 = 0.074 | 14/21 |
| Shahab et al.68 | RCT | Yogic breathing (24 h) | dpost = 0.728 | 15/21 |
| d24hr = 0.413 | ||||
| Zucker et al.66 | RCT | Portable HRVB (4 weeks) | dppc2 = 0.329 | 11.5/21 |
Average SASQI scores rated independently by two authors.
CCQB, cocaine craving questionnaire-brief; D, Cohen's d; dppc2, effect size based on pooled pretest standard deviation; HRVB, heart rate variability biofeedback; RCT, randomized controlled trial; SASQI, The Scale for Assessing Scientific Quality of Investigations; VAS, visual analog scale.
Mechanism of action
The physiologic or psychophysiologic mechanisms through which HRVB may lead to a reduction in craving are not known. More generally, mechanisms that underlie the empirically supported clinical benefit of HRVB in other populations (e.g., asthma, depression) are not well understood. In contrast, acute physiologic effects of HRVB and CB are clearly observable. For example, large increases in HRV and baroreflex sensitivity occur acutely during both HRVB and CB paced at approximately five to six breaths per minute.54,70,71 Recent laboratory studies further suggest that the active ingredient of HRVB may be CB paced at 0.1 Hz.56,72 Laboratory studies also have demonstrated that a brief practice of HRVB or CB paced at 0.1 Hz, performed in anticipation of psychosocial stress, or during induced stress, helped to control physiologic arousal and state anxiety and improved cognitive performance.70,73 These results lead to the hypothesis that both HRVB and CB may diminish a psychophysiologic component of craving “in-the-moment” and perhaps set the stage for enhanced cognitive control of behavior. However, one study did not find that CB reduced momentary food craving.74 This may be due to methodological issues such as exposing the participants to food cues throughout the slowed breathing period. There is a clear need for further laboratory studies and clinical trials to uncover the mediators of HRVB and CB effects on craving. Both experimental and observational studies are needed to determine whether changes in craving are driven by cumulative physiologic effects of repeated HRBV and CB, whether individuals consciously implement CB into their daily life to counter stimuli that induce craving, and whether consistent mapping of CB to stimuli that instigate craving may result, over time, in an automatic CB rate near 0.1 Hz that dampens craving in-the-moment without relying on effortful cognitive processes.
Challenges of HRVB studies
Craving measurement
In the reviewed HRVB articles, craving was examined with different types of assessments (Table 1) that are based on dissimilar conceptualizations of the craving construct, ranging from single-item to multidimensional assessments. The adjusted Pennsylvania Alcohol Craving Scale is a five-item single-factor scale that measures characteristics of craving without asking about factors associated with craving, such as emotional states or incentives.75 In contrast, the Obsessive Compulsive Drinking Scale is a multidimensional instrument that assesses the cognitive aspects of craving, including thoughts and compulsions, as well as addiction severity.76 Similarly, the Food Craving Questionnaire–Trait is a multidimensional instrument that measures various aspects of food cravings such as food triggers, relief anticipation, and preoccupation/control over eating. From a validity perspective, the variety of theoretical assumptions underlying each of these instruments may have resulted in the measurement of different aspects of craving creating inconsistencies in trial outcomes such as those revealed in this review. Given the relatively rudimentary understanding of the phenomenon of craving, it is not yet possible to accurately assess what experiencing craving means to the patient, clinician, and researcher. Despite the advantages of single-item ratings of drug craving and how highly they correlate with many multi-item questionnaires, this type of craving assessment may fail to assess urges and cravings if drug takers attribute such feelings to another psychologic or physiologic state, such as anxiety, excitement, or drug withdrawal.77 Components of the construct of craving, including emotional, cognitive, physiologic, and behavioral responses, remain the subject of considerable debate,10 suggesting the need for using multiple types of craving measurement and perhaps for more grounded theory or phenomenologic studies in this area.
Training protocols and personal practice
Despite the limited number of HRVB studies, various training protocols were used employing different session allocations and treatment durations. The study with the longest standardized training time (240 min) and treatment duration (4 weeks)18 among the three other studies had the strongest effect in terms of craving reduction, regardless of home practice. This observation is also supported by previous clinical trials of HRVB that have produced clinically significant changes in fibromyalgia, depression, and post-traumatic stress disorder symptoms with longer interventions of 8–10 weeks, although these studies included home practice of up to 20 min twice daily.57,78,79 Yet, it is unknown whether this dose–effect relationship holds in clinical SUD populations. In addition, the usefulness of personal HRVB practice outside training hours remains unknown. Although positive anecdotal reports have been conveyed,39 a relationship between personal practice and craving has not been found, and participant reports of daily practice have not been independently verified.
Methods and statistical analysis
Because craving is a highly subjective and temporal phenomenon, observed changes in craving may be either undirected fluctuations or systematic changes. Erroneous conclusions about craving changes are likely therefore when only pre–post measurements are used. A minimum of three observations is usually required to differentiate error from real change, supporting the need for longitudinal data. The primary advantage of a longitudinal study lies in its capacity to inform about within-person in addition to between-person relationships.80 The discrepancies found in the literature highlight the predominance of individual differences in craving assessments and the necessity of interpreting craving changes as a function of intra- and interindividual sources of variance. General linear models, such as the analyses of variance and regression analyses, used by all reviewed studies, fail to distinguish intra- and interindividual differences because they do not examine sources of dependency (or strong correlations between residuals).80,81 The use of multilevel modeling (also known as general linear mixed models) and potentially structural equation modeling in analyzing longitudinal data allows for the simultaneous examination of between- and within-person relationships.82,83 With repeated measures, dependency is expected between the individual's responses over time, which violates the assumption of independence of data that is required for repeated measures analyses of variance and regression analyses. Multilevel modeling overcomes this shortcoming by partitioning the outcome's residual variance into within- and between-person components. The covariance between residual components is therefore explored to identify sources of dependency and accurately distinguish individual and time-specific differences. Furthermore, multilevel modeling handles missing and unbalanced data while preserving statistical power and the generalizability of results, which overcomes the problem of listwise deletion with general linear models.80,82,84
Strengths and limitations
Strengths of this review include the use of a quantitative assessment of effect size across studies, a qualitative systematic review approach, and an exploration of study attributes that were associated with craving reductions. Nonetheless, this review has several limitations. First, the limited volume of HRVB and CB studies investigating craving does not provide material for a systematic review. Second, CB and HRVB interventions used different training methods and may not share the same mechanisms, which make comparison difficult across studies. However, CB studies were informative and worthy of examination and provided additional support to the evidence from HRVB studies. Third, the reliability and validity of the SASQI have not been empirically evaluated, and SASQI ratings cannot be considered completely unbiased.
Future directions
Further study of HRVB and CB as anticraving interventions for persons recovering from SUD is required, but would benefit from improved methodology addressing the aforementioned challenges. Based on this review, the following considerations are recommended: (1) use of reproducible HRVB and CB training protocols; for HRVB, the minimum treatment duration should be 8–10 weeks, (2) longitudinal examination of craving changes over time, (3) examination of the effects of personal practice outside HRVB and CB training using accurate measurements of practice time and treatment fidelity, (4) further examination of confounding variables (such as substance type, comorbidity, length of abstinence, and treatment setting) and other predictors of craving, (5) use of multiple craving instruments to ensure measurement validity of the craving phenomenon, and (6) use of appropriate statistical analyses to differentiate between- and within-person variations, such as multilevel modeling and structural equation modeling.
Conclusions
The impact of craving as a frequently experienced and strong predictor of relapse underscores the need for investigating innovative anticraving interventions. Biobehavioral interventions, such as HRVB and CB, are advantageous because craving is modulated by physiologic, as well as cognitive, processes. HRVB training seems to be of significant therapeutic potential, and CB interventions warrant further study. Most reviewed studies showed positive results and a relatively moderate effect size across the studied populations. However, due to the scarcity and limitations of the studies available, larger clinical trials are required with methodological improvements such as longer treatment duration, adequate control conditions, measures of adherence and compliance, longitudinal examination of craving changes differentiating undirected fluctuation from systematic change, and more comprehensive methods to measure the craving phenomenon.
Acknowledgment
The authors thank Dr. Barbara Caldwell, Rutgers University, for her input on this work.
Author Disclosure Statement
This work was supported in part by NIAAA grant K24 AA021778. No competing financial interests exist. The funding source had no role in the study design, collection, analysis, or interpretation of the data, writing of the manuscript, or the decision to submit the article for publication.
References
- 1. NIDA. Principles of Drug Addiction Treatment: A Research-Based Guide. Third ed. Rockville, MD: National Institute of Health, 2009 [Google Scholar]
- 2. SAMHSA. The TEDS Report: Treatment Outcomes among Clients Discharged from Outpatient Substance Abuse Treatment. Rockville, MD: SAMHSA, 2009 [Google Scholar]
- 3. Fatseas M, Serre F, Alexandre JM, et al. Craving and substance use among patients with alcohol, tobacco, cannabis or heroin addiction: A comparison of substance- and person-specific cues. Addiction 2015;110:1035–1042 [DOI] [PubMed] [Google Scholar]
- 4. Paliwal P, Hyman SM, Sinha R. Craving predicts time to cocaine relapse: Further validation of the Now and Brief versions of the cocaine craving questionnaire. Drug Alcohol Depend 2008;93:252–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sinha R. New findings on biological factors predicting addiction relapse vulnerability. Curr Psychiatry Rep 2011;13:398–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Addolorato G, Leggio L, Abenavoli L, Gasbarrini G. Neurobiochemical and clinical aspects of craving in alcohol addiction: A review. Addict Behav 2005;30:1209–1224 [DOI] [PubMed] [Google Scholar]
- 7. APA. Diagnostic and Statistical Manual of Mental Disorders 5th ed. Arlington, VA: American Psychiatric Publishing, 2013 [Google Scholar]
- 8. NIDA. DrugFacts: Treatment Approaches for Drug Addiction. Rockville, MD: National Institute on Drug Abuse, 2016 [Google Scholar]
- 9. Tiffany ST, Wray JM. The clinical significance of drug craving. Ann N Y Acad Sci 2012;1248:1–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kavanagh DJ, Statham DJ, Feeney GF, et al. Measurement of alcohol craving. Addict Behav 2013;38:1572–1584 [DOI] [PubMed] [Google Scholar]
- 11. Drummond DC. Theories of drug craving, ancient and modern. Addiction 2001;96:33–46 [DOI] [PubMed] [Google Scholar]
- 12. Haass-Koffler CL, Leggio L, Kenna GA. Pharmacological approaches to reducing craving in patients with alcohol use disorders. CNS Drugs 2014;28:343–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Westbrook C, Creswell JD, Tabibnia G, et al. Mindful attention reduces neural and self-reported cue-induced craving in smokers. Soc Cogn Affect Neurosci 2013;8:73–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sinha R. The clinical neurobiology of drug craving. Curr Opin Neurobiol 2013;23:649–654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Robinson TE, Berridge KC. Review. The incentive sensitization theory of addiction: Some current issues. Philos Trans R Soc Lond B Biol Sci 2008;363:3137–3146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Robinson TE, Berridge KC. The neural basis of drug craving: An incentive-sensitization theory of addiction. Brain Res Brain Res Rev 1993;18:247–291 [DOI] [PubMed] [Google Scholar]
- 17. Skinner MD, Aubin HJ. Craving's place in addiction theory: Contributions of the major models. Neurosci Biobehav Rev 2010;34:606–623 [DOI] [PubMed] [Google Scholar]
- 18. Meule A, Freund R, Skirde AK, et al. Heart rate variability biofeedback reduces food cravings in high food cravers. Appl Psychophysiol Biofeedback 2012;37:241–251 [DOI] [PubMed] [Google Scholar]
- 19. Konova AB, Moeller SJ, Goldstein RZ. Common and distinct neural targets of treatment: Changing brain function in substance addiction. Neurosci Biobehav Rev 2013;37(10 Pt 2):2806–2817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Carim-Todd L, Mitchell SH, Oken BS. Mind-body practices: An alternative, drug-free treatment for smoking cessation? A systematic review of the literature. Drug Alcohol Depend 2013;132:399–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Behere RV, Muralidharan K, Benegal V. Complementary and alternative medicine in the treatment of substance use disorders-a review of the evidence. Drug Alcohol Rev 2009;28:292–300 [DOI] [PubMed] [Google Scholar]
- 22. Miller WR, Walters S, Bennett ME. How Effective Is Alcoholism Treatment in the United States? J Stud Alcohol 2001;62:211–220 [DOI] [PubMed] [Google Scholar]
- 23. O'Brien CP. Anticraving medications for relapse prevention: A possible new class of psychoactive medications. Am J Psychiatry 2005;162:1423–1431 [DOI] [PubMed] [Google Scholar]
- 24. Witkiewitz K, Bowen S, Douglas H, Hsu SH. Mindfulness-based relapse prevention for substance craving. Addict Behav 2013;38:1563–1571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Baird C. Complementary and alternative therapies in addictions treatment. J Addict Nurs 2014;25:214–216 [Google Scholar]
- 26. Boyuan Z, Yang C, Ke C, et al. Efficacy of acupuncture for psychological symptoms associated with opioid addiction: A systematic review and meta-analysis. Evid Based Complement Alternat Med 2014;2014:313549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chan YY, Lo WY, Li TC, et al. Clinical efficacy of acupuncture as an adjunct to methadone treatment services for heroin addicts: A randomized controlled trial. Am J Chin Med 2014;42:569–586 [DOI] [PubMed] [Google Scholar]
- 28. Chen KW, Comerford A, Shinnick P, Ziedonis DM. Introducing qigong meditation into residential addiction treatment: A pilot study where gender makes a difference. J Altern Complement Med 2010;16:875–882 [DOI] [PubMed] [Google Scholar]
- 29. Smelson D, Chen KW, Ziedonis D, et al. A pilot study of Qigong for reducing cocaine craving early in recovery. J Altern Complement Med 2013;19:97–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Black DS. Mindfulness-based interventions: An antidote to suffering in the context of substance use, misuse, and addiction. Subst Use Misuse 2014;49:487–491 [DOI] [PubMed] [Google Scholar]
- 31. Ruscio AC, Muench C, Brede E, Waters AJ. Effect of Brief Mindfulness Practice on Self-Reported Affect, Craving, and Smoking: A Pilot Randomized Controlled Trial Using Ecological Momentary Assessment. Nicotine Tob Res 2016;18:64–73 [DOI] [PubMed] [Google Scholar]
- 32. Murphy CM, MacKillop J. Mindfulness as a strategy for coping with cue-elicited cravings for alcohol: An experimental examination. Alcohol Clin Exp Res 2014;38:1134–1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mermelstein LC, Garske JP. A brief mindfulness intervention for college student binge drinkers: A pilot study. Psychol Addict Behav 2015;29:259–269 [DOI] [PubMed] [Google Scholar]
- 34. Vinci C, Peltier MR, Shah S, et al. Effects of a brief mindfulness intervention on negative affect and urge to drink among college student drinkers. Behav Res Ther 2014;59:82–93 [DOI] [PubMed] [Google Scholar]
- 35. Penberthy JK, Konig A, Gioia CJ, et al. Mindfulness-Based Relapse Prevention: History, Mechanisms of Action, and Effects. Mindfulness 2015;6:151–158 [Google Scholar]
- 36. Calderon KS, Thompson WW. Biofeedback relaxation training: A rediscovered mind-body tool in public health. Am J Health Stud 2004;19:185–194 [Google Scholar]
- 37. Dehghani-Arani F, Rostami R, Nadali H. Neurofeedback training for opiate addiction: Improvement of mental health and craving. Appl Psychophysiol Biofeedback 2013;38:133–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hartwell KJ, Hanlon CA, Xingbao L, et al. Individualized real-time fMRI neurofeedback to attenuate craving in nicotine-dependent smokers. J Psychiatry Neurosci 2016;41:48–55 48p [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Eddie D, Kim C, Bates ME, et al. A pilot study of brief heart rate variability biofeedback to reduce craving in young adult men receiving inpatient treatment for substance use disorders. Appl Psychophysiol Biofeedback 2014;39:181–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Penzlin AI, Siepmann T, Illigens BMW, et al. Heart rate variability biofeedback in patients with alcohol dependence: A randomized controlled study. Neuropsychiatr Dis Treat 2015;11:2619–2627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Imperatori C, Valenti EM, Della Marca G, et al. Coping food craving with neurofeedback. Evaluation of the usefulness of alpha/theta training in a non-clinical sample. Int J Psychophysiol 2017;112:89–97 [DOI] [PubMed] [Google Scholar]
- 42. Glick RM, Greco CM. Biofeedback and primary care. Prim Care 2010;37:91–103 [DOI] [PubMed] [Google Scholar]
- 43. Lehrer P, Eddie D. Dynamic processes in regulation and some implications for biofeedback and biobehavioral interventions. Appl Psychophysiol Biofeedback 2013;38:143–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gevirtz R. The promise of heart rate variability biofeedback: Evidence-based applications. Biofeedback 2013;41:110–120 [Google Scholar]
- 45. Eddie D, Vaschillo E, Vaschillo B, Lehrer P. Heart rate variability biofeedback Theoretical basis, delivery, and potential for treating sud. Addict Res Theory 2015;23:266–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kemp AH, Quintana DS. Review: The relationship between mental and physical health: Insights from the study of heart rate variability. Int J Psychophysiol 2013;89:288–296 [DOI] [PubMed] [Google Scholar]
- 47. Quintana DS, Kemp AH, Guastella AJ, et al. Heart rate variability predicts alcohol craving in alcohol dependent outpatients: Further evidence for HRV as a psychophysiological marker of self-regulation. Drug Alcohol Depend 2013;132:395–398 [DOI] [PubMed] [Google Scholar]
- 48. Porges SW. The polyvagal perspective. Biol Psychol 2007;74:116–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bates ME, Buckman JF. Integrating Body and Brain Systems in Addiction Neuroscience. Biological Research on Addiction Vol 2 First ed. San Diego: Elsevier, Inc., 2013 [Google Scholar]
- 50. Lehrer PM, Gevirtz R. Heart rate variability biofeedback: How and why does it work? Front Psychol 2014;5:1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Berntson GG, Bigger JT, Jr., Eckberg DL, et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology 1997;34:623–648 [DOI] [PubMed] [Google Scholar]
- 52. Thayer JF, Lane RD. Review: Claude Bernard and the heart–brain connection: Further elaboration of a model of neurovisceral integration. Neurosci Biobehav Rev 2009;33:81–88 [DOI] [PubMed] [Google Scholar]
- 53. Lehrer PM, Vaschillo E, Vaschillo B, et al. Biofeedback treatment for asthma. CHEST 2004;126:352–361 [DOI] [PubMed] [Google Scholar]
- 54. Lehrer PM, Vaschillo E, Vaschillo B. Resonant frequency biofeedback training to increase cardiac variability: Rationale and manual for training. Appl Psychophysiol Biofeedback 2000;25:177–191 [DOI] [PubMed] [Google Scholar]
- 55. Nolan RP, Kamath MV, Floras JS, et al. Heart rate variability biofeedback as a behavioral neurocardiac intervention to enhance vagal heart rate control. Am Heart J 2005;149:1137. [DOI] [PubMed] [Google Scholar]
- 56. Vaschillo EG, Vaschillo B, Lehrer PM. Characteristics of Resonance in Heart Rate Variability Stimulated by Biofeedback. Appl Psychophysiol Biofeedback 2006;31:129–142 [DOI] [PubMed] [Google Scholar]
- 57. Karavidas MK, Lehrer PM, Vaschillo E, et al. Preliminary Results of an Open Label Study of Heart Rate Variability Biofeedback for the Treatment of Major Depression. Appl Psychophysiol Biofeedback 2007;32:19–30 [DOI] [PubMed] [Google Scholar]
- 58. Lin G, Xiang Q, Fu X, et al. Heart rate variability biofeedback decreases blood pressure in prehypertensive subjects by improving autonomic function and baroreflex. J Altern Complement Med 2012;18:143–152 [DOI] [PubMed] [Google Scholar]
- 59. Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- 60. Sarkar BK, Shahab L, Arora M, et al. A cluster randomized controlled trial of a brief tobacco cessation intervention for low-income communities in India: Study protocol. Addiction 2014;109:371–378 [DOI] [PubMed] [Google Scholar]
- 61. Field A, Gillet R. How to do a meta-analysis. Br J Math Stat Psychol 2010;63:665–694 [DOI] [PubMed] [Google Scholar]
- 62. Lenhard W, Lenhard A. Calculation of Effect Sizes. Psychometrica 2016. Online document at: www.psychometrica.de/effect_size.html#cohc, accessed August12, 2016
- 63. Morris SB. Estimating effect sizes from pretest-posttest-control group designs. Organ Res Methods 2008;11:364–386 [Google Scholar]
- 64. Meeks T, Wetherell J, Irwin M, et al. Complementary and alternative treatments for late-life depression, anxiety, and sleep disturbance: A review of randomized controlled trials. J Clin Psychiatry 2007;68:1461–1471 [DOI] [PubMed] [Google Scholar]
- 65. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15:155–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Zucker TL, Samuelson KW, Muench F, et al. The effects of respiratory sinus arrhythmia biofeedback on heart rate variability and posttraumatic stress disorder symptoms: A pilot study. Appl Psychophysiol Biofeedback 2009;34:135–143 [DOI] [PubMed] [Google Scholar]
- 67. McClernon FJ, Westman EC, Rose JE. The effects of controlled deep breathing on smoking withdrawal symptoms in dependent smokers. Addict Behav 2004;29:765–772 [DOI] [PubMed] [Google Scholar]
- 68. Shahab L, Sarkar BK, West R. The acute effects of yogic breathing exercises on craving and withdrawal symptoms in abstaining smokers. Psychopharmacology (Berl) 2013;225:875–882 [DOI] [PubMed] [Google Scholar]
- 69. De Zeni TC, Araujo RB. Deep breathing in the management of craving and anxiety symptoms of crack-cocaine-dependent patients. Rev Psiquiatr Rio Gd Sul 2009;31:116–119 [Google Scholar]
- 70. Wells R, Outhred T, Heathers JAJ, et al. Matter over mind: A randomised-controlled trial of single-session biofeedback training on performance anxiety and heart rate variability in musicians. PLoS One 2012;7:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Buckman JF, Vaschillo EG, Fonoberova M, Mezic I, Bates ME. The translational value of psychophysiology methods and mechanisms: multi-level, dynamic, personalized. J Stud Alcohol Drugs 2018;79:229–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Fonoberova M, Mezic I, Buckman JF, et al. A computational physiology approach to personalized treatment models: The beneficial effects of slow breathing on the human cardiovascular system. Am J Physiol Heart Circ Physiol 2014;307:H1073–H1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Prinsloo GE, Rauch HGL, Lambert MI, et al. The effect of short duration heart rate variability (HRV) biofeedback on cognitive performance during laboratory induced cognitive stress. Appl Cogn Psychol 2011;25:792–801 [Google Scholar]
- 74. Meule A, Kübler A. A pilot study on the effects of slow paced breathing on current food craving. Appl Psychophysiol Biofeedback 2017;42:59–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcohol Clin Exp Res 1999;23:1289–1295 [PubMed] [Google Scholar]
- 76. Anton R, Moak D, Latham P. The obsessive compulsive drinking scale: A new method of assessing outcome in alcoholism treatment studies. Arch Gen Psychiatry 1996;53:225–231 [DOI] [PubMed] [Google Scholar]
- 77. Rosenberg H. Clinical and laboratory assessment of the subjective experience of drug craving. Clin Psychol Rev 2009;29:519–534 [DOI] [PubMed] [Google Scholar]
- 78. Tan G, Dao TK, Farmer L, et al. Heart rate variability (HRV) and posttraumatic stress disorder (PTSD): A pilot study. Appl Psychophysiol Biofeedback 2011;36:27–35 [DOI] [PubMed] [Google Scholar]
- 79. Hassett AL, Radvanski DC, Vaschillo EG, et al. A pilot study of the efficacy of heart rate variability (HRV) biofeedback in patients with fibromyalgia. Appl Psychophysiol Biofeedback 2007;32:1–10 [DOI] [PubMed] [Google Scholar]
- 80. Hoffman L. Longitudinal Analysis: Modeling Within-Person Fluctuation and Change. 1st ed. New York: Routledge, 2015 [Google Scholar]
- 81. Holden JE, Kelley K, Agarwal R. Analyzing change: A primer on multilevel models with applications to nephrology. Am J Nephrol 2008;28:792–801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Hox JJ. Multilevel Analysis: Techniques and Applications. Second ed. Mahwah, NJ: Lawrence Erlbaum Associates, 2010 [Google Scholar]
- 83. Hoffman L, Stawski RS. Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Res Hum Dev 2009;6:97–120 [Google Scholar]
- 84. Kwok OM, Underhill AT, Berry JW, et al. Analyzing longitudinal data with multilevel models: An example with individuals living with lower extremity intra-articular fractures. Rehabil Psychol 2008;53:370–386 [DOI] [PMC free article] [PubMed] [Google Scholar]