Abstract
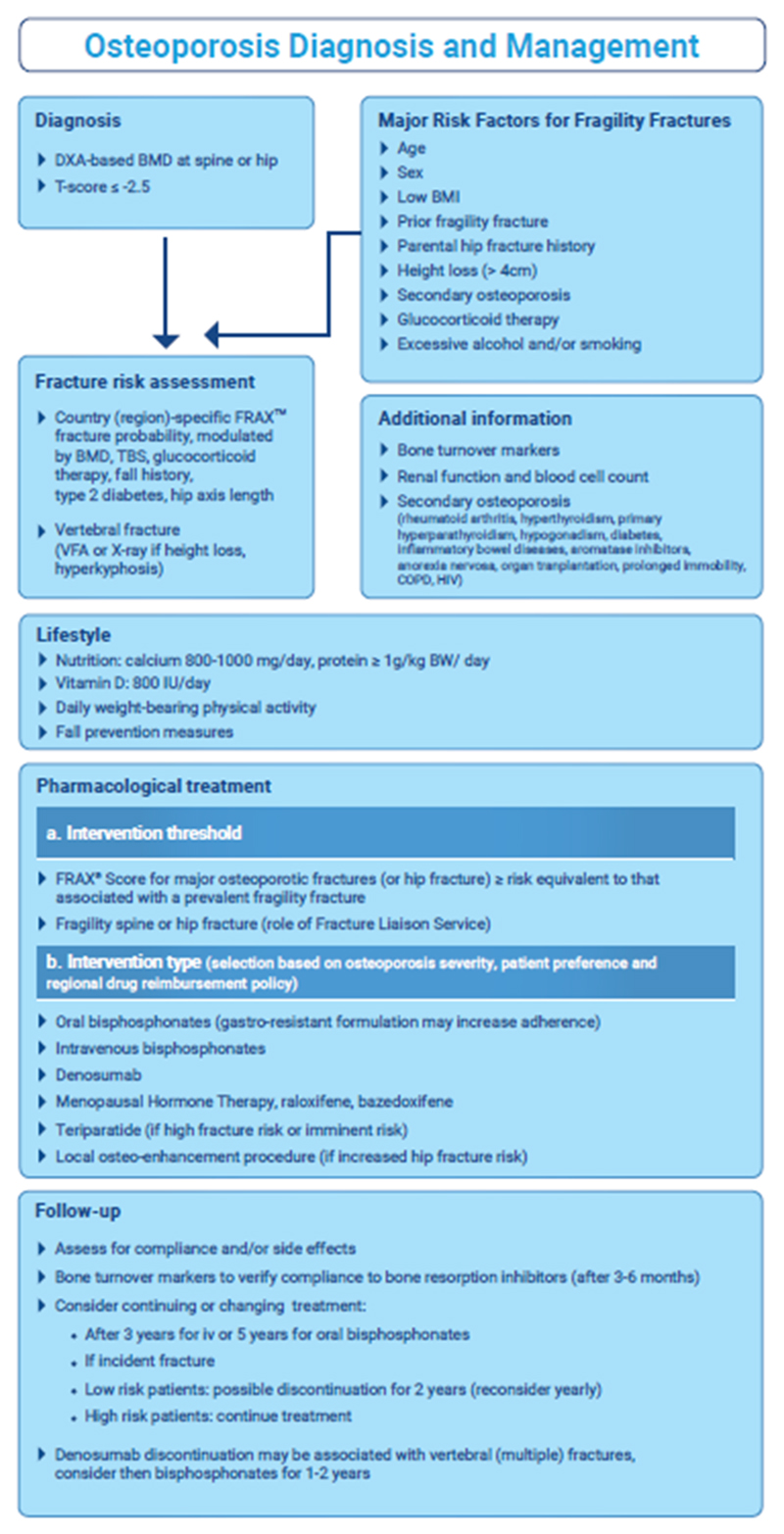
A guidance on the assessment and treatment of postmenopausal women at risk from fractures due to osteoporosis was recently published in Osteoporosis International as a joint effort of the International Osteoporosis Foundation and European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (1) This manuscript updates the previous guidelines document, published in 2013 (2) and is written in a European perspective. The present article reports and summarizes the main recommendations included in this 2018 guidance document (Figure 1).
Keywords: Bone mineral density, Diagnosis of osteoporosis, Fracture risk assessment, FRAX, Health economics, Treatment of osteoporosis
Summary of main recommendations
Diagnosis of osteoporosis
The operational definition of osteoporosis is based on the T-score for BMD assessed by DXA at the femoral neck or spine and is defined as a value for BMD 2.5 SD or more below the young female adult mean.
For clinical purposes, other sites and techniques can be used for diagnosis.
Low bone mass (osteopenia) should not be considered a disease category but is intended solely for purpose of epidemiological description.
Risk factors for fragility fractures
Several factors contribute significantly to fracture risk over and above that provided by bone mineral density measurements. These include age, sex, low body mass index, previous fragility fracture, parental history of hip fracture, glucocorticoid treatment, current smoking, alcohol intake of 3 or more units daily and causes of secondary osteoporosis.
Additional risk factors that are of use in case finding include height loss (>4 cm) and thoracic kyphosis.
Bone markers (serum procollagen type I N propeptide (s-PINP) and serum C-terminal cross-linking telopeptide of type I collagen (s-CTX) as markers of bone formation and bone resorption, respectively) have some prognostic significance for fracture in situations where BMD is unavailable.
Assessment of fracture risk
Country-specific FRAX® should be used to assess fracture probability in postmenopausal women who have risk factors for fracture. In individuals at intermediate risk, bone mineral density (BMD) measurement should be performed using dual energy X-ray absorptiometry and FRAX fracture probability re-estimated.
Where BMD testing is unavailable, FRAX can be used without the input of BMD
Trabecular bone score (TBS) may be used as an adjunct to BMD measurements and FRAX.
Interpretation of FRAX scores may be influenced by exposure to glucocorticoids, information on lumbar spine BMD, trabecular bone score, hip axis length, falls history, immigration status and type 2 diabetes mellitus.
Vertebral fracture assessment should be considered if there is a history of ≥4cm height loss, kyphosis, recent or current long-term oral glucocorticoid therapy, or a BMD T-score ≤ -2.5.
Lifestyle and dietary measures
Recommendations should include a daily calcium intake of between 800 and 1200mg and sufficient dietary protein, ideally achieved through dairy products.
A daily dose of 800IU cholecalciferol should be advised for postmenopausal women at increased risk of fracture.
Calcium supplementation is appropriate if the dietary intake is below 800 mg/day, and vitamin D supplementation considered in patients at risk of, or showing evidence of, vitamin D insufficiency.
Regular weight-bearing exercise should be advised, tailored to the needs and abilities of the individual patient.
A history of falls should be obtained in individuals at increased risk of fracture with further assessment and appropriate measures undertaken in those at increased risk.
Pharmacological intervention in postmenopausal women
The oral bisphosphonates (alendronate, risedronate and ibandronate) may be used as initial treatments in the majority of cases. In women intolerant to oral bisphosphonates (or in those for whom they are contraindicated), intravenous bisphosphonates or denosumab provide the most appropriate alternatives, with raloxifene, or menopause hormone therapy as additional options. Teriparatide is preferentially recommended for patients at high risk of fracture.
Treatments should be reviewed after 3 - 5 years treatment with bisphosphonate. Fracture risk should be reassessed after a new fracture, regardless of when it occurs. The risk of new clinical and vertebral fractures increases in patients who stop treatment.
Withdrawal of denosumab therapy is associated with a rebound in vertebral fracture rate. Bisphosphonate therapy can be considered after discontinuation of denosumab.
There is little evidence to guide decision-making beyond 10 years of treatment and management options in such patients should be considered on an individual basis.
Intervention thresholds for pharmacological intervention
The thresholds recommended for decision-making are based on probabilities of major osteoporotic and hip fracture derived from FRAX. These vary in different healthcare systems with variation in “willingness to pay”.
Women aged over 65 years with a prior fragility fracture can be considered for treatment without the need for further assessment; BMD measurement may be felt more appropriate in younger postmenopausal women.
Age-dependent intervention thresholds provide clinically appropriate and equitable access to treatment and have been shown to be cost-effective.
Systems of care
The utility of age-dependent FRAX thresholds in population screening approach has recently been validated as feasible, effective and health economically viable.
Coordinator-based Fracture Liaison Services (FLS) should be used to systematically identify men and women with fragility fracture. Their effectiveness and cost-effectiveness have been established recently.
Figure 1.
Algorithm for the diagnosis and management of osteoporosis in postmenopausal women
References
- 1.Kanis JA, Cooper C, Rizzoli R, Reginster JY, on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors and the Committee of National Societies of the International Osteoporosis Foundation (IOF) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporosis International. 2018 doi: 10.1007/s00198-018-4704-5. [Epub ahead of print] [DOI] [Google Scholar]
- 2.Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster J-Y, on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporosis International. 2018;24:23–57. doi: 10.1007/s00198-012-2074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]