Abstract
The burden of uncontrolled asthma in children and adolescents is high. Treatment options for pediatric patients (aged under 18 years) with asthma are largely influenced by the Global Initiative for Asthma recommendations. Algorithms for adolescents (12–18 years) and adults are identical, but recommendations for children aged under 6 years and 6–11 years differ. Although the goals of treatment for pediatric patients with asthma are similar to those for adults, relatively few new therapies have been approved for this patient population within the last decade. Designing clinical trials involving children presents several challenges, notably that children are often less able to perform lung function tests, and traditional endpoints used in clinical trials with adults, such as forced expiratory volume in 1 second, asthma exacerbations and questionnaires, have limitations associated with their use in children. There are also ethical considerations related to the performance of longer placebo-controlled exacerbation trials. This review considers additional clinical endpoints to those traditionally reported, including forced expiratory flow at 25%–75% of forced vital capacity, which may help shed light on which treatments are most effective for use in pediatric patients with asthma. The pros and cons of specific and potentially clinically relevant endpoints are considered, along with device considerations and patient preferences that may enhance adherence and quality of life. Recent advances in the management of children and adolescents, including the US Food and Drug Administration and European Medicines Agency approval of tiotropium in patients with asthma aged 6 years and over, are also discussed.
Keywords: asthma, anticholinergic, tiotropium, pediatric, children, adolescents
Video abstract
Introduction
Asthma remains one of the most common chronic diseases of childhood and adolescence.1,2 Much of the understanding of the epidemiology of pediatric asthma is derived from data collected in the International Study of Asthma and Allergies in Childhood (ISAAC).3,4 Phase III of ISAAC involved around 1.2 million children from 233 centers in 98 countries, and found that the global prevalence of asthma was 14% and 12% in 13- to 14-year-olds and 6- to 7-year-olds, respectively.5 ISACC has, however, reported substantial differences (of up to 13-fold) between countries in the prevalence of asthma symptoms (specifically wheeze in the past 12 months) in children.6 The 2014 Global Asthma Report described an increase in the frequency of asthma symptoms in children in many low- and middle-income countries between 1993 and 2003, while prevalence remained the same or decreased in high-income countries.7
The burden associated with asthma in children and adolescents is considerable. In 2010, asthma was the eighth highest ranked cause of disability-adjusted life years in children aged 5–9 years and the third highest for children aged 10–14 years worldwide.6,8 Recurrent symptoms such as wheeze, cough and shortness of breath can also have a marked negative impact on the quality of life of children.9 Furthermore, asthma exacerbations are the leading cause of hospitalization in children10 and of the children who attend an emergency department with an asthma exacerbation, more than half are aged between 2 and 7 years old.11 These findings make asthma a leading cause of childhood morbidity from chronic diseases.12 The global socioeconomic burden of pediatric asthma is further increased by school absences9 and the relatively high cost of asthma care.6
Alarmingly, it is estimated that asthma control is inadequate in more than half of pediatric patients with asthma despite currently available treatment and guidelines.9,13 Clearly, there is a pressing need to alleviate the burden of uncontrolled asthma in pediatric patients, and effective treatment is paramount to achieving this. As will be discussed, treatment recommendations outlined by the Global Initiative for Asthma (GINA) consist of an inhaled corticosteroid (ICS) backbone with or without additional reliever therapy.13 Evidence has recently emerged supporting the use of anti-cholinergics in asthma,14 and tiotropium has become the first long-acting muscarinic receptor antagonist (LAMA) to be approved for the treatment of asthma.15 The aim of this review is to report on the use of anticholinergic therapies in pediatric patients with asthma and to discuss the difficulties in investigating new therapies for this population.
GINA Report recommendations
The GINA Report is intended to be a useful resource for the management of asthma, and provides recommendations that should be adjusted in line with local practices and available health care resources.13 The principle aims of these treatment recommendations are control of asthma symptoms and the minimization of future risk of exacerbations, fixed airflow limitation and treatment side effects. In pediatric patients, additional consideration is given to avoiding reduced lung growth and minimizing adverse effects, given the potential capacity of ICS treatment to negatively impact development.14,16 The GINA strategy recommends a stepwise approach towards asthma treatment, building on a framework of ICS controller medication with or without a reliever therapy.13
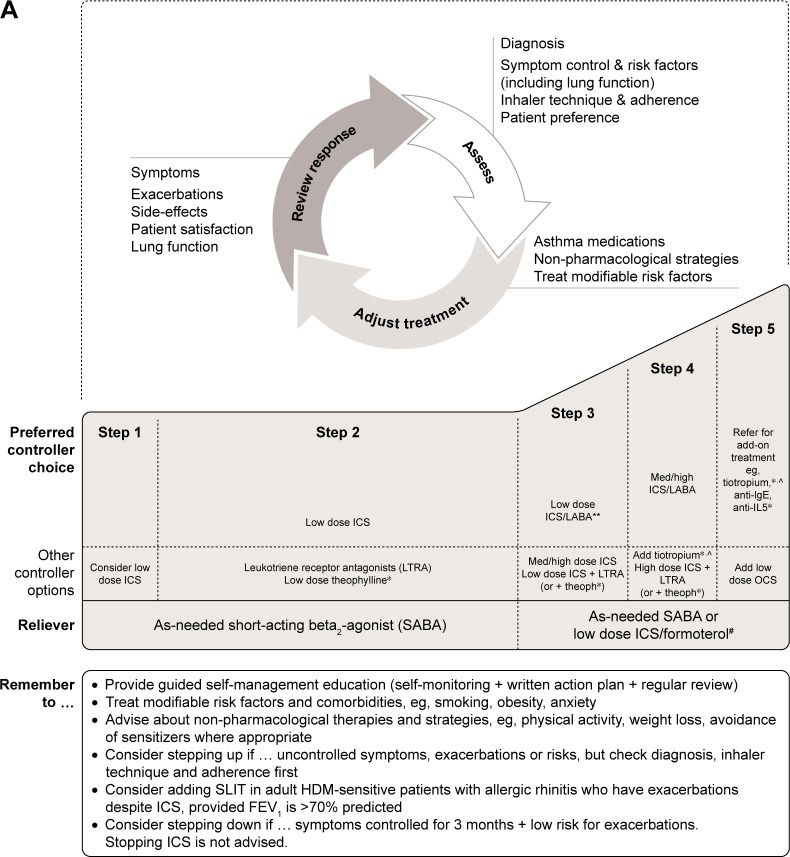
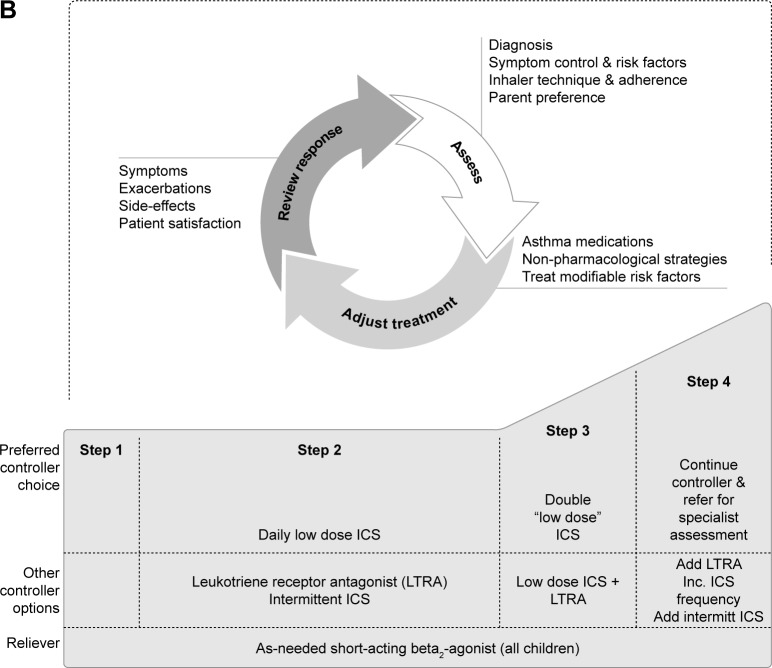
Algorithms for treatment of adult and adolescent (12–18 years) patients with asthma are the same (Figure 1A). For adolescents, the current GINA recommendations are low-dose ICS treatment followed by a stepwise increase in ICS dose and/or additional (or a second class of) maintenance therapy, such as a long-acting β2-agonist (LABA) or leukotriene receptor antagonist (LTRA), if control has not been achieved. Add-on treatment (eg, with tiotropium) is then suggested if control is still not attained. There are key differences in the recommendations for children. In children aged 6–11 years, increasing the ICS dose is preferred over combination ICS/LABA. If this is ineffective, then it is suggested that the child be referred for expert assessment and advice. In children under 6 years of age, the preferred asthma control medication is low-dose ICS, such as 200 µg budesonide or equivalent (Figure 1B). Due to lack of data, treatment options are limited in children under 6 years of age whose asthma symptoms are poorly controlled with ICS monotherapy.13 Therefore, data for additional second-line controller medications, such as theophylline, oral corticosteroids and anticholinergics, are particularly valuable to this patient subset.
Figure 1.
Stepwise approach for the treatment of asthma in (A) patients aged 6 years and over and (B) children under 6 years of age, as recommended in the GINA Report.
Notes: *Not for children <12 years; **for children 6–11 years, the preferred Step 3 treatment is medium-dose ICS; #low-dose ICS/formoterol is the reliever medication for patients prescribed low-dose budesonide/formoterol maintenance and reliever therapy; ^tiotropium by mist inhaler is an add-on treatment for patients with a history of exacerbations; it is not indicated in children <12 years. Copyright ©2018. Reproduced from Global Initiative for Asthma. GINA Report, Global strategy for asthma management and prevention.13
Abbreviations: FEV1, forced expiratory volume in 1 second; GINA, Global Initiative for Asthma; HDM, house dust mite; ICS, inhaled corticosteroids; IgE, immunoglobulin E; Inc., increase; intermitt, intermittent; LABA, long-acting β2-agonist; LTRA, leukotriene receptor antagonist; med, medium dose; OCS, oral corticosteroids; SABA, short-acting β2-agonist; SLIT, sublingual immunotherapy; theoph, theophylline.
While the GINA Report and its recommendations are regularly updated (most recently in 2018), there have been no updated recommendations from the National Heart, Lung and Blood Institute on asthma diagnosis/management since 2007.
Anticholinergic therapies
Anticholinergic agents target the function of acetylcholine, a neurotransmitter that plays a key role in the pathophysiology of asthma by way of driving bronchial smooth muscle contraction, mucus secretion, vasodilation and increasing airway tone. Further, cholinergic activity is believed to be the predominant driver of bronchoconstriction.14,17 There are two categories of acetylcholine receptors: nicotinic and muscarinic. Of these, the muscarinic M1, M2 and M3 subtypes are believed to be primarily involved in regulating broncho-constriction.14 Better understanding of muscarinic receptor agonists over the past two decades has led to investigation of both short- and long-acting anticholinergics in asthma. Several studies in children with severe asthma exacerbations suggest that the addition of the short-acting anticholinergic agent ipratropium to a β2-agonist may reduce hospital admissions and improve lung function.18–21 A 2012 meta-analysis of short-acting anticholinergics as bronchodilators in children aged $2 years with acute asthma exacerbations suggested that short-acting anticholinergics were less efficacious than β2-agonists.22 However, the safety of anticholinergics in children, combined with the lack of additional controller medications licensed for this population, has sustained an interest in developing anticholinergics for use in this patient population.
In recent years, evidence has emerged supporting the use of long-acting anticholinergic agents.14 Of note, not all LAMAs have equivalent potency as bronchodilators due to their differential effects on the muscarinic receptor subtypes M1–M3.23 The different biological functions of M1–M3 receptors in the airways distinguish their potential as therapeutic targets in asthma. M3 is the primary receptor subtype involved in bronchial and tracheal muscle contraction, and acts alongside M1 to increase smooth muscle tone in the airways.24,25 Conversely, M2 receptors inhibit the release of acetylcholine from parasympathetic nerves and decrease smooth muscle tone. Consequently, LAMAs that primarily mediate blockade of the M1 and M3 receptors are the most attractive candidate therapies for asthma treatment.23,26
Tiotropium for pediatric asthma
Evidence of tiotropium efficacy in pediatric patients with asthma
Tiotropium is a once-daily LAMA that has been approved for the treatment of chronic obstructive pulmonary disease for over a decade.27 Of note, tiotropium dissociates slowly from the M1 and M3 muscarinic receptors, but does so rapidly from the M2 receptor, making it a highly potent bronchodilator.28 A number of Phase III clinical trials in adult patients with symptomatic asthma recently led to tiotropium becoming the first LAMA to be approved for the treatment of asthma.29–32 These studies demonstrated that tiotropium improves lung function and asthma control in patients with a range of asthma severities, with a safety profile similar to that of placebo. The 2018 GINA Report recommends tiotropium as an add-on therapy in patients aged $12 years with a history of asthma exacerbations at Steps 4 and 5 of the stepwise approach (Figure 1A).13
Further investigation of tiotropium in asthma has demonstrated the effectiveness of tiotropium add-on therapy across all age groups.33 In Phase II dose-escalation studies of tiotropium in children and adolescents with symptomatic asthma, similar safety and tolerability profiles to placebo were observed, with early indications of efficacy.34,35 As a consequence of these positive early findings, five Phase III, randomized, double-blind, placebo-controlled, parallel-group trials in children and adolescents have recently investigated the efficacy and safety of once-daily tiotropium as an add-on therapy to ICS with or without other controllers (Table 1).36–43
Table 1.
Key results of Phase III studies with 2.5 and 5 µg tiotropium in children and adolescents with asthma
| Study | Patients (asthma severity and age) | Baseline therapy | Treatment duration, weeks | N | Primary and key secondary endpoint | Difference from placebo | |
|---|---|---|---|---|---|---|---|
| 2.5 µg tiotropium | 5 µg tiotropium | ||||||
| RubaTinA-asthma®37 | Moderate symptomatic 12- to 17-year-olds | At least ICS | 48 | 398 | Peak FEV1,a Week 24 | 134 (34, 234) (P<0.01) | 174 (76, 272) (P<0.001) |
| Trough FEV1, Week 24 | NS | 117 (10, 223) (P=0.03) | |||||
| PensieTinA-asthma®41 | Severe symptomatic 12- to 17-year-olds | ICS + $1 controller | 12 | 392 | Peak FEV1, Week 12 | 111 (2, 220) (P=0.046) | NS |
| Trough FEV1, Week 12 | NS | NS | |||||
| CanoTinA- asthma®38,42 | Moderate symptomatic 6- to 11-year-olds | At least ICS | 48 | 401 | Peak FEV1, Week 24 | 170 (108, 231) (P<0.001) | 164 (103, 225) (P<0.001) |
| Trough FEV1, Week 24 | 116 (46, 186) (P=0.001) | 118 (48, 188) (P=0.001) | |||||
| VivaTinA- asthma®39 | Severe symptomatic 6- to 11-year-olds | At least ICS + $1 controller | 12 | 401 | Peak FEV1, Week 12 | 35 (-28, 99) (P=0.27) | 139 (75, 203) (P<0.001) |
| Trough FEV1, Week 12 | 18 (-48, 85) (P=0.59) | 87 (19, 154) (P=0.01) | |||||
| NinoTinA- asthma®40, 43 | Symptomatic 1- to 5-year-olds | At least ICS | 12 | 101 | AE frequency | −17.9% | −15.4% |
| PACD, weekly frequency (%) of worsening asthma symptoms at Week 12, adjusted mean (CI) | −0.658 (−2.413, −1.098) (P=0.46) | −1.063 (−2.897, 0.772) (P=0.25) | |||||
| Risk of asthma exacerbations (reported as AEs) | Reduced risk (HR 0.46; 95% CI: 0.22, 0.98) (P=0.044) | Reduced risk (HR 0.42; 95% CI: 0.19, 0.94) (P=0.035) | |||||
Note:
FEV1 values are mean (CI) mL.
Abbreviations: AE, adverse event; CI, confidence interval; FEV1, forced expiratory volume in 1 second; HR, hazard ratio; ICS, inhaled corticosteroids; NS, not significant; PACD, pediatric asthma caregiver diary.
Two of these trials were performed in adolescents aged 12–17 years (Table 1).37,41 The first of these, RubaTinA-asthma® (NCT01257230), was performed in patients with moderate symptomatic asthma. Here, the efficacy and safety of once-daily tiotropium (5 or 2.5 µg) or placebo administered via Respimat® (Boehringer Ingelheim Pharma, Ingelheim am Rhein, Germany) were assessed as an add-on therapy to ICS (200–800 µg or 400–800 µg budesonide or equivalent/day for patients aged 12–14 years or 15–17 years, respectively) with or without an LTRA over 48 weeks. Both doses of tiotropium were safe and well tolerated, and conferred a significantly greater improvement in peak forced expiratory volume in 1 second (FEV1) within 3 hours after dosing (FEV1(0–3h)) at Week 24 compared with placebo.37 At Week 24, both doses were associated with significant improvements in forced expiratory flow between 25% and 75% of forced vital capacity (FEF25–75) compared with placebo at most time points.37
PensieTinA-asthma® (NCT01277523) was a Phase III study in adolescent patients with severe symptomatic asthma. Once-daily tiotropium (5 or 2.5 µg) or placebo, both administered by the Respimat®, was added to high-dose ICS (>400 µg or 800–1,600 µg budesonide or equivalent/day for patients aged 12–14 years or 15–17 years, respectively) plus at least one controller therapy (LABA or LTRA) or medium-dose ICS (200–400 µg budesonide or equivalent in patients aged 12–14 years and 400–800 µg budesonide or equivalent in patients aged 15–17 years) plus two or more other controller therapies (LABA and/or LTRA and/or sustained-release theophylline) over 12 weeks. In this study of adolescents with severe asthma, numerical improvements in measures of lung function and asthma control were reported with once-daily tiotropium add-on therapy, while the safety and tolerability of tiotropium were comparable with those of placebo.41
Two Phase III trials were performed in children aged 6–11 years (Table 1).38,39 In the first of these, VivaTinA-asthma® (NCT01634152), participants had severe symptomatic asthma. The efficacy and safety of tiotropium (5 or 2.5 µg) or placebo, both administered via the Respimat®, were assessed as an add-on therapy to high-dose ICS (>400 µg budesonide or equivalent per day) with one or more controller medications (LABA or LTRA) or medium-dose ICS (200–400 µg budesonide or equivalent per day) with two or more controller medications (LABA and/or LTRA and/or sustained-release theophylline) over 12 weeks. Compared with placebo, 5 µg tiotropium had a similar safety and tolerability profile and significantly improved peak FEV1(0–3h) at Week 12; both doses were associated with a significant improvement in FEF25–75 at Weeks 12 and 24.39 Add-on tiotropium in children aged 6–11 years was also evaluated in moderate symptomatic asthma in the CanoTinA-asthma® trial. Tiotropium (5 or 2.5 µg) versus placebo, both delivered via the Respimat®, was evaluated as an add-on therapy to medium-dose ICS (200–400 µg budesonide or equivalent/day) with or without an LTRA over 48 weeks. Both doses of tiotropium were well tolerated, and the 5 µg dose conferred a statistically significant improvement in FEV1(0–3h) at Week 24; both doses were associated with a significant improvement in FEF25–75 at the majority of time points throughout the 48-week study period.38 Finally, the NinoTinA-asthma® (NCT01634113) trial was conducted in preschool children aged 1–5 years with persistent asthma symptoms (Table 1). Once-daily tiotropium (5 or 2.5 µg) or placebo, delivered via the Respimat®, was given as an add-on therapy to ICS at a stable dose with or without additional controller medication for 12 weeks. In this study, tiotropium was shown to be safe and reduced the risk of asthma exacerbations reported as adverse events by more than 50% in very young patients.43
Overall, these studies demonstrate tiotropium to be efficacious in children and adolescents with asthma, irrespective of disease severity. In support of this, a pooled analysis of the RubaTinA-asthma® and CanoTinA-asthma® studies supported the use of tiotropium as an add-on therapy to the usual background medication of pediatric patients aged 6–11 years with symptomatic persistent asthma.44 Furthermore, in a systematic review of three studies of tiotropium in school-age symptomatic asthmatics, tiotropium was associated with significant improvements in FEV1 peak responses and a reduction in asthma exacerbation frequency compared with placebo. This review concluded tiotropium to be an efficacious and well-tolerated add-on to ICS plus one or more controller medications in this population.45
Efficacy of tiotropium in allergic asthma
Allergic asthma is the most common asthma phenotype.46 In childhood, asthma is frequently associated with atopy, a condition that predisposes individuals to develop immunoglobulin E (IgE) against specific allergens.47 Studies have been performed to investigate whether baseline IgE levels or blood eosinophil counts can influence response to tiotropium add-on therapy in patients aged 6–17 years with asthma. Data were pooled from moderate symptomatic patients in the CanoTinA-asthma®38 and RubaTinA-asthma®37 trials and from severe symptomatic patients in the VivaTinA-asthma®39 and PensieTinA-asthma®41 trials.36,48,49 In these pooled studies, tiotropium improved lung function irrespective of baseline IgE levels and blood eosinophil counts. Overall, these data demonstrate that tiotropium is effective in children and adolescents without the need for phenotyping of allergic status according to IgE levels and blood eosinophil counts.
Pharmacokinetics and pharmacogenomics of tiotropium
Age and developmental status are major influences on numerous factors, including anatomy, physiology and pathology, that could affect pharmacodynamics, kinetics and drug metabolism.47 Therefore, it is pertinent to compare the pharmacokinetics of tiotropium when administered to patients with asthma from different age groups. The pharmacokinetic properties of tiotropium are well established in adult patients with symptomatic asthma. Pharmacokinetic parameters of tiotropium demonstrate its fast absorption and long elimination time, with maximum plasma concentrations reached within 5 minutes of post-inhalation and a half-life of approximately 30 hours.50 Furthermore, pharmacokinetics of tiotropium in adult patients with asthma are dose proportional up to 5 µg once daily.51
Plasma and urine samples from subsets of symptomatic patients with asthma aged 6–11 years35 and 12–17 years34 treated with tiotropium in Phase II trials were used to evaluate the pharmacokinetic properties of tiotropium in these age groups.52,53 These studies found the pattern of absorption, exposure and clearance of tiotropium at steady state to be consistent with those reported in adults. The pharmacokinetic characteristics of tiotropium in children aged 1–5 years were also studied in the Phase III NinoTinA-asthma® study. Here, exposure to tiotropium, when normalized for body surface area, was comparable to older age groups based on urinary excretion data.40,43
Tiotropium pharmacokinetic data from patients with asthma of different ages were summarized in a clinical pharmacology review carried out by the US Food and Drug Administration (Table 2).54 In agreements with the aforementioned analyses, exposure of tiotropium in urine and plasma samples from patients with asthma is comparable in children aged 6–11 years, adolescents and adults.
Table 2.
Pharmacokinetics of tiotropium in asthma patients across age groups
| Age group | Fe0–3,ss (%) | Fe0–24,ss (%) | C0.083,ss (pg/mL) |
|---|---|---|---|
| 1–5 years40,43 | 1.08 (N=12, CV=66%) | NA | NA |
| 6–11 years35 | 2.88 (N=11, CV=48%) | 10.3 (N=11, CV=63%) | 2.42 (N=6, CV=49%) |
| 12–18 years34 | 2.42 (N=10, CV=80%) | 14.3 (N=12, CV=70%) | 2.19 (N=3, CV=88%) |
| $18 years | 2.61 (N=49, CV=111%) | 12.7 (N=102, CV=84%) | 2.38 (N=89, CV=54%) |
Note: Data from US Food and Drug Administration. Tiotropium bromide clinical pharmacology review. 2016. Available from: https://www.fda.gov/downloads/drugs/developmentapprovalprocess/developmentresources/ucm549091.pdf.54
Abbreviations: C0.083,ss, tiotropium plasma concentration at 5 minutes post-dose at steady state; CV, coefficient of variation; Fe0–3,ss, urine excretion fraction of unchanged tiotropium within 3 hours post-dose at steady state; Fe0–24,ss, urine excretion fraction of unchanged tiotropium within 24 hours post-dose at steady state; NA, not applicable.
Although no formal drug interaction studies have been conducted, tiotropium has been used with other drugs without clinical evidence of interactions.55 Concomitant treatment with other asthma medications such as LABA, ICS+LABA, oral corticosteroids and leukotriene modifiers does not affect exposure to tiotropium.54
Pharmacogenomics is another factor that may impact response to therapy. In this respect, a study performed in adults with severe asthma found that the presence of Arg16Gly in ADRB2 may predict response to tiotropium.56 However, similar studies are yet to be performed in children and adolescents.
Clinical trials with other LAMAs in asthma
Of the clinical trials assessing the safety and efficacy of LAMAs in the treatment of asthma, the tiotropium program has thus far been the most advanced across all age groups.27 A number of studies evaluating the potential of umeclidinium bromide and glycopyrronium in adult asthma have been completed or are ongoing (Table 3), although neither agent is approved for the treatment of asthma.27,57–63 Aside from tiotropium, other LAMAs are yet to be studied in children or adolescents with asthma. These pediatric trials are unlikely to be conducted unless their efficacy and safety are first demonstrated in adults. At the time of this publication, no studies are known to be completed or ongoing with aclidinium bromide in asthma.
Table 3.
Asthma clinical trials in adults with LAMAs other than tiotropium
| Study drugs | Patients | Treatment duration | Baseline therapy | N (enrolled) | Study findings |
|---|---|---|---|---|---|
| Umeclidinium bromide 31.25 and 62.5 µg57 | Symptomatic inadequately controlled | Variable 24–52 weeks | ICS/LABA | 2,250 | Trial ongoing |
| Umeclidinium bromide 15.6, 31.25, 62.5, 125 and 250 µg58 | Symptomatic | 14 weeks | Non-ICS controller | 350 | No significant dose response |
| Umeclidinium bromide 15.6, 31.25, 62.5, 125 and 250 µg58,59 | Symptomatic | 14 weeks | At least ICS/LABA | 421 | Combination treatment significantly increased trough FEV1 compared with ICS alone |
| Glycopyrronium MDI 1.9, 3.6, 7.2, 14.4 and 28.8 µg60 | Symptomatic | 14 days | ICS or non-ICS maintenance | 249 | Study complete Awaiting publication |
| Glycopyrrolate bromide 12.5 µg61 | Uncontrolled | 6 weeks | ICS | 98 | Study complete Awaiting publication |
| Glycopyrronium 50 µg62 | Symptomatic | 96 hours | NS | 13 | Tiotropium provided statistically superior bronchoprotection compared with glycopyrronium |
| Glycopyrronium 50 µg63 | Symptomatic mild-to-moderate | 24–48 hours | NS | 30 | Study complete awaiting publication |
Note: Copyright ©2017. The Korean Academy of Asthma, Allergy and Clinical Immunology. Reproduced from Aalbers R, Park HS. Positioning of long-acting muscarinic antagonists in the management of asthma. Allergy Asthma Immunol Res. 2017;9(5):386–393.27
Abbreviations: FEV1, forced expiratory volume in 1 second; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; MDI, metered-dose inhaler; NS, not specified.
Umeclidinium is a potent anticholinergic that demonstrates slow functional reversibility at the human M3 muscarinic receptor compared with the M2 receptor.64 Once-daily umeclidinium bromide combined with fluticasone furoate, administered via a dual-strip dry powder inhaler (DPI), has been investigated in adults with asthma who were symptomatic despite maintenance ICS treatment. This study reported significant increases in trough FEV1 in response to combination treatment, but not with fluticasone furoate alone.59 Furthermore, umeclidinium monotherapy (delivered via DPI) in patients with asthma not requiring ICS treatment did not provide a therapeutic benefit, given that it conferred modest, inconsistent, dose-independent improvements in trough FEV1.65 Other ongoing and completed studies in adult patients are summarized in Table 3.
As with tiotropium, glycopyrronium is an anticholinergic with higher selectivity for M3 receptors than for M2 receptors, and dissociates more slowly from the M3 receptors than from the M2 receptors.66 The only study of glycopyrronium to be published thus far compared the effects of glycopyrronium (administered via Breezhaler) and tiotropium (administered via Respimat®) on methacholine-induced bronchoconstriction in adults with symptomatic asthma. Here, tiotropium provided statistically superior bronchoprotection at both 24 and 72 hours compared with glycopyrronium.62 An additional study of glycopyrronium in adults has been completed and results are awaited (Table 3).
Challenges for future clinical trials in pediatric asthma
Several challenges are posed by the design of clinical trials in asthma involving children as participants, particularly the choice of endpoints to measure clinical efficacy. The endpoints traditionally used to measure drug efficacy in clinical trials of asthma in adults may not be the most appropriate for use with pediatric patients. These challenges need to be carefully considered in future trials in pediatric patients with asthma.
Clinical trial endpoints
The three attainable objectives of drug development across all age groups in asthma are 1) prevention and treatment of symptoms, 2) exacerbations, and 3) further complications.47 Clinical trials to investigate candidate drugs therefore have endpoints designed to quantify achievement of these goals (Table 4). To demonstrate the symptom-modifying effect of a reliever drug, there must be an improvement in an objective measure of airflow. For a drug to be registered as a symptom-preventing agent, there must be a demonstration of benefit in symptomatology, disease control, lung function, exacerbations and/or quality of life.47
Table 4.
Traditional and alternative clinical trial endpoints
| Endpoint | Definition | Advantages | Disadvantages |
|---|---|---|---|
| Traditional endpoints | |||
| FEV1 | Forced expiratory volume in 1 second | Robust, repeatable, standardized and simple measurement47 | Does not indicate disease processes such as hyperinflation or airway plugging;69 does not correlate with severity;47,68,70 difficult to perform in younger children71 |
| PEF | Peak expiratory flow | Portable PEF meters allow self-monitoring at home73 | Does not correlate with severity;72 many patients do not use PEF meters correctly73 |
| Frequency of asthma exacerbations | “Worsening of asthma requiring the use of systemic corticosteroids to prevent serious outcomes”78 | Commonly used endpoint;67 prevention of exacerbations is an important aspect of asthma control75,76 | Definition is subjective, leading to variations between studies and investigators;74,77 ethical considerations relating to use of exacerbations in placebo-controlled pediatric trials79 |
| Questionnaires: ACQ, ACT | Asthma Control Questionnaire, Asthma Control Test | Commonly used to assess asthma control;80 allow quantification of composite scores for outcome measures80 | Difficult for children to complete74,80 (although an interviewer-administered ACQ has been used in some pediatric studies39,42); caregiver assistance can alter outcome;74,80 episodic nature of pediatric asthma confounds use of questionnaires81 |
| cACT | Childhood ACT (recommended for baseline characterization of children aged 4–11 years67) | Completed by children and caregivers; recommended by the asthma outcomes workshop as a core baseline and observational outcome, and as a supplemental outcome for efficacy67 | Episodic nature of pediatric asthma confounds use of questionnaires81 |
| TRACK | Test for respiratory and asthma control in kids | In development82 | Difficulties associated with language and capabilities of the respondent74,80 |
| Alternative endpoints | |||
| FEF25–75 | Forced expiratory flow at 25%–75% of forced vital capacity | Sensitive measure of small airway obstruction;85 linked with acute wheezing, response to bronchodilators and ventilation defects;85 predictive of asthma severity85 | |
| IOS | Impulse oscillometry (mechanical measurement of the airway performed by non-invasive superimposing of pressure fluctuations on the airway during spontaneous breathing87) | Suitable for patients who cannot perform spirometry;87 complements information gained from FEV1 measurement;88 offers insights into alterations in airway mechanics in response to therapy88 | Cost |
| Biomarkers | Naturally occurring characteristic, molecule or gene that identifies a disease or a physiological/pathological process | Objective measure of asthma control | Research is lacking in children;89 unlikely to be used as a broad measure of asthma control across ages and phenotypes |
It is widely recognized that clinical research in asthma lacks standardization in outcomes.67 To address this, an Asthma Outcomes workshop was convened with the specific purpose of stratifying core, supplemental and emerging asthma outcomes.67 Importantly, this workshop differentiated between recommended endpoints in adult and pediatric patients. As will be discussed, measures of asthma outcomes frequently used in adult patients are often less appropriate for use in pediatric patients. Alternative endpoints to those traditionally reported in clinical trials may help to shed light on which treatments are most effective in children. More details on these traditional and alternative endpoints are provided in the following text and in Table 4.
Traditional endpoints
Objective measurements such as FEV1 and peak expiratory flow (PEF) play an important role in the evaluation of airflow in patients with asthma during clinical trials.47 In the assessment of efficacy of potential bronchodilators, FEV1 is the gold standard measurement of lung function.68 Although FEV1 has numerous advantages, including robustness, repeatability, standardization and ease of measurement,47 there are limitations to its use as a clinical endpoint. For example, FEV1 does not always confer a complete representation of the disease processes that occur in asthma, such as hyperinflation and airway plugging.69 In clinical trials with pediatric patients, the suitability of FEV1 as an endpoint has been questioned given that FEV1 does not correlate with asthma severity in children. In fact, FEV1 values fall within the normal range in the majority of pediatric patients with asthma, even when patients are markedly symptomatic.47,68,70 Also, efficient and reliable spirometry testing can be difficult in preschool children, especially in the younger age groups. In a study involving 355 children aged 3–5 years, only around half were able to perform effective spirometry.71 Another traditional endpoint – PEF – has also been shown not to correlate with asthma severity in children. Instead, PEF correlates with FEV1, suggesting this test may also have limitations as an asthma outcome measurement in children with asthma.72 In addition, portable PEF meters allow for self-monitoring at home, which can be beneficial for children, although all patients need to be observed carefully, as it has been reported that many patients, both adults and children, do not use the PEF meters correctly.73
Frequency of asthma exacerbations is a commonly used subjective measurement, and is recommended as both a core and supplemental asthma outcome in children.67 These episodes of airway narrowing are most common in infants and young children.74 Of note in children, their recurrence in early years is associated with progressive loss of lung function, making the prevention of exacerbations an especially important aspect of asthma control.75,76 However, the exact definition of what constitutes an exacerbation in a clinical trial has remained elusive. Most clinicians are able to identify asthma exacerbations through the observation of symptoms and medication changes, but the subjective nature of this assessment can lead to variations between studies and investigators.74,77 To rectify this issue, experts in the Asthma Outcomes workshop coined a cross-age definition of asthma exacerbations as “worsening of asthma requiring the use of systemic corticosteroids to prevent serious outcomes”.78 There are also ethical considerations around the use of exacerbations as an endpoint in placebo-controlled trials conducted in children. The chance of being assigned to the placebo group could deter parents from enrolling their child onto such a trial.79
Questionnaires also play a role in asthma control by quantifying composite scores for outcome measures. The Asthma Control Questionnaire (ACQ) and Asthma Control Test (ACT) are commonly employed to assess asthma control.80 There are obvious difficulties in completion of questionnaires by children, and assistance given by caregivers can prevent a true representation of the patient’s disease state.74,80 The episodic nature of asthma in young children also confounds the use of questionnaires.81 There are no core questionnaires recommended for efficacy studies in children. The Childhood ACT (cACT), completed by children and caregivers, is recommended for baseline characterization of children aged 4–11 years.80 cACT was recommended by the Asthma Outcomes workshop both as a core baseline and observational outcome, and as a supplemental outcome for efficacy.67 Further questionnaires for use in pediatric patients with asthma, such as the Test for Respiratory and Asthma Control in Kids instrument for infants aged 0–4 years,82 are in development but face ongoing challenges associated with language and the capabilities of the respondent.74,80 An interviewer-administered ACQ test has been used in some studies with children.38,39
Alternative endpoints
Objective measurements of asthma control are at the center of clinical trials testing the efficacy of asthma medications.68 Spirometry plays an important part in this, and is recommended as a core asthma outcome for children across all aspects of prospective clinical trials.67 However, the limitations of traditional spirometrical measurements (eg, FEV1) in children highlight a need for alternatives. One such alternative, FEF25–75, is a sensitive measure of small airway obstruction that quantifies the maximum mid-expiratory flow rate. FEF25–75 has been purported as more reflective of small airways function than FEV183 and in a large cohort of patients it was significantly associated with asthma control.84 Unlike FEV1, FEF25–75 has been linked with acute wheezing, response to bronchodilators and ventilation defects, and is predictive of asthma severity in children.85 However, some investigators have questioned its contribution to clinical decision making; one database study found that although abnormally low FEF25–75 values were more prevalent in children than in adults, only in a very small number of patients did FEF25–75 detect an impairment that FEV1 and FVC measures did not.86
There is a keen interest in the use of alternative acceptable measures of lung function in children who cannot perform spirometry, such as impulse oscillometry (IOS). IOS is a type of airway mechanic measurement performed by non-invasively superimposing pressure fluctuations on the airway during spontaneous breathing of the subject.87 A comparison of IOS and spirometry as measures of pediatric asthma control found that IOS complemented information gained by FEV1. Furthermore, IOS offered some additional insights into alterations in airway mechanics in response to therapy.88 However, there are cost considerations associated with IOS due to the high cost of the machines.
Biomarkers are another non-invasive objective measurement of asthma control, but are lacking in children, and utility as a broad measure of asthma control across ages and phenotypes seems unlikely.89
Patient considerations when choosing an anticholinergic for pediatric asthma
In children with asthma, poor adherence to medication has been shown to lead to increased morbidity.90 When selecting a treatment for pediatric asthma, patient preferences must be considered to help maintain therapeutic adherence. In children, a particularly relevant aspect of this is drug delivery, which poses significant challenges in young patients.74 Inhalers are the main device used in asthma treatment, and the GINA Report recommends they should reproducibly deliver a predetermined dose to the lungs with minimal deposition elsewhere in the body.13 Administration of ICS is most commonly performed using a pressured metered-dose inhaler (pMDI) device connected to a spacer, yet only a small fraction of the dose from these devices reach the distal airways.74 Anticholinergics can also be administered by inhalation, using pMDIs, nebulizers and DPIs.91
Patient satisfaction was a priority in the development of the inhaler used to administer tiotropium in pediatric clinical trials (Respimat® Soft Mist™ Inhaler, Boehringer Ingelheim Pharma). This pocket-sized inhaler has been shown to reproducibly deliver a single-breath, metered dose of inhalable aerosol from an aqueous drug solution in an environmentally friendly manner.92 Optimization of delivery to the lungs and minimal inspiratory effort were key in the design of this device,93 and likely explain why patients favored this inhaler over the commonly used Turbuhaler® (AstraZeneca UK Ltd, Luton, UK) DPI in a clinical trial. The two devices were compared in a randomized, placebo-controlled study, which found that 74% of patients preferred Respimat® compared with 17% who preferred Turbuhaler® and 9% who had no preference.94 Among pediatric patients with asthma, the benefits and ease of use of this innovative tiotropium inhaler could help to maximize patient adherence.
Conclusion
Pediatric asthma is a chronic disease leading to significant morbidity and health care utilization. As many as 50% of patients remain uncontrolled despite national and international guidelines designed to improve control. As this review reveals, new add-on therapy options to ICS/LABA are required, particularly for children and adolescents. However, developing such treatments is challenging. There are limitations to the conclusions that we can draw from the data sources used in this review, for example to the paucity of pediatric trials, the smaller sample sizes than in adult trials and the lack of information on LAMAs other than tiotropium in pediatric populations. It is also clearly essential that clinical trial design continues to consider alternative clinical endpoints, such as FEF25–75 and IOS, that are likely to be more suitable for use in clinical trials of pediatric asthma.
Tiotropium Respimat® is approved in asthma for adult patients (aged $18 years) in Singapore, patients aged $15 years in Japan and, most recently, approved for patients aged $6 years in the US and EU.27,95 The clinical trials of tiotropium in pediatric asthma summarized in this review support the safety and efficacy of tiotropium in children and adolescents, irrespective of disease severity and phenotype. At present, tiotropium is considered as an option for add-on to ICS/LABA combination. However, data suggest that it could be considered as an alternative to adding a LABA to ICS, and this may prove an attractive option for future therapeutic strategies.
Acknowledgments
Editorial support (writing assistance, assembling tables and figures, collating author comments, grammatical editing and referencing) was provided by Wemimo Omotosho, PhD (MediTech Media, London, UK) and was funded by Boehringer Ingelheim. The author would like to thank Kjeld Hansen, a member of the Patient Ambassador Group for the European Lung Foundation, for his input to the video summary for this manuscript.
Footnotes
Disclosure
The author reports no conflicts of interest in this work.
References
- 1.Centres for Disease Control and Prevention National Health Interview Survey, US children. 2015. [Accessed August 31, 2017]. Available from: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2015_SHS_Table_C-1.pdf.
- 2.Asthma UK Asthma facts and statistics. 2017. [Accessed August 26, 2017]. Available from: https://www.asthma.org.uk/about/media/facts-and-statistics/
- 3.Asher MI, Keil U, Anderson HR, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J. 1995;8(3):483–491. doi: 10.1183/09031936.95.08030483. [DOI] [PubMed] [Google Scholar]
- 4.Ellwood P, Asher MI, Beasley R, Clayton TO, Stewart AW, ISAAC Steering Committee The international study of asthma and allergies in childhood (ISAAC): phase three rationale and methods. Int J Tuberc Lung Dis. 2005;9(1):10–16. [PubMed] [Google Scholar]
- 5.Mallol J, Crane J, von Mutius E, Odhiambo J, Keil U, Stewart A, ISAAC Phase Three Study Group The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three: a global synthesis. Allergol Immunopathol (Madr) 2013;41(2):73–85. doi: 10.1016/j.aller.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Asher I, Pearce N. Global burden of asthma among children. Int J Tuberc Lung Dis. 2014;18:1269–1278. doi: 10.5588/ijtld.14.0170. [DOI] [PubMed] [Google Scholar]
- 7.The Global Asthma Network The Global Asthma Report 2014. [Accessed August 26, 2017]. Available from: http://www.globalasthmareport.org/resources/Global_Asthma_Report_2014.pdf.
- 8.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 9.Schmier JK, Manjunath R, Halpern MT, Jones ML, Thompson K, Diette GB. The impact of inadequately controlled asthma in urban children on quality of life and productivity. Ann Allergy Asthma Immunol. 2007;98(3):245–251. doi: 10.1016/S1081-1206(10)60713-2. [DOI] [PubMed] [Google Scholar]
- 10.Murray CS, Poletti G, Kebadze T, et al. Study of modifiable risk factors for asthma exacerbations: virus infection and allergen exposure increase the risk of asthma hospital admissions in children. Thorax. 2006;61(15):376–382. doi: 10.1136/thx.2005.042523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guttmann A, Zagorski B, Austin PC, et al. Effectiveness of emergency department asthma management strategies on return visits in children: a population-based study. Pediatrics. 2007;120(6):e1402–e1410. doi: 10.1542/peds.2007-0168. [DOI] [PubMed] [Google Scholar]
- 12.Pedersen SE, Hurd SS, Lemanske RF, Jr, et al. Global Initiative for Asthma Global strategy for the diagnosis and management of asthma in children 5 years and younger. Pediatr Pulmonol. 2011;46(1):1–17. doi: 10.1002/ppul.21321. [DOI] [PubMed] [Google Scholar]
- 13.Global Initiative for Asthma GINA Report, Global strategy for asthma management and prevention. 2018. [Accessed March 25, 2018]. Available from: http://ginasthma.org/2018-gina-report-global-strategy-for-asthma-management-and-prevention/
- 14.Price D, Fromer L, Kaplan A, van der Molen T, Román-Rodríguez M. Is there a rationale and role for long-acting anticholinergic bronchodilators in asthma? NPJ Prim Care Respir Med. 2014;24:14023. doi: 10.1038/npjpcrm.2014.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McIvor ER, McIvor RA. The evolving role of tiotropium in asthma. J Asthma Allergy. 2017;10:231–236. doi: 10.2147/JAA.S140577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Philip J. The effects of inhaled corticosteroids on growth in children. Open Respir Med J. 2014;8:66–73. doi: 10.2174/1874306401408010066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barnes PJ. Neural mechanisms in asthma. Br Med Bull. 1992;48(1):149–168. doi: 10.1093/oxfordjournals.bmb.a072531. [DOI] [PubMed] [Google Scholar]
- 18.Qureshi F, Zaritsky A, Lakkis H. Efficacy of nebulized ipratropium in severely asthmatic children. Ann Emerg Med. 1997;29(2):205–211. doi: 10.1016/s0196-0644(97)70269-5. [DOI] [PubMed] [Google Scholar]
- 19.Griffiths B, Ducharme FM. Combined inhaled anticholinergics and short-acting beta2-agonists for initial treatment of acute asthma in children. Cochrane Database Syst Rev. 2013;8:CD000060. doi: 10.1002/14651858.CD000060.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schuh S, Johnson DW, Callahan S, Canny G, Levison H. Efficacy of frequent nebulized ipratropium bromide added to frequent high-dose albuterol therapy in severe childhood asthma. J Pediatr. 1995;126(4):639–645. doi: 10.1016/s0022-3476(95)70368-3. [DOI] [PubMed] [Google Scholar]
- 21.Zorc JJ, Pusic MV, Ogborn CJ, Lebet R, Duggan AK. Ipratropium bromide added to asthma treatment in the pediatric emergency department. Pediatrics. 1999;103(4 Pt 1):748–752. doi: 10.1542/peds.103.4.748. [DOI] [PubMed] [Google Scholar]
- 22.Teoh L, Cates CJ, Hurwitz M, Acworth JP, van Asperen P, Chang AB. Anticholinergic therapy for acute asthma in children. Cochrane Database Syst Rev. 2012;4:CD003797. doi: 10.1002/14651858.CD003797.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barnes PJ. Muscarinic receptor subtypes in airways. Eur Respir J. 1993;6:328–331. [PubMed] [Google Scholar]
- 24.Gosens R, Zaagsma J, Meurs H, Halayko AJ. Muscarinic receptor signaling in the pathophysiology of asthma and COPD. Respir Res. 2006;7:73. doi: 10.1186/1465-9921-7-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Busse WW, Dahl R, Jenkins C, Cruz AA. Long-acting muscarinic antagonists: a potential add-on therapy in the treatment of asthma? Eur Respir Rev. 2016;25(139):54–64. doi: 10.1183/16000617.0052-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Belmonte KE. Cholinergic pathways in the lungs and anticholinergic therapy for chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005;2(4):297–304. doi: 10.1513/pats.200504-043SR. discussion 311–312. [DOI] [PubMed] [Google Scholar]
- 27.Aalbers R, Park HS. Positioning of long-acting muscarinic antagonists in the management of asthma. Allergy Asthma Immunol Res. 2017;9(5):386–393. doi: 10.4168/aair.2017.9.5.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barnes PJ. The pharmacological properties of tiotropium. Chest. 2000;117(2 Suppl):63S–66S. doi: 10.1378/chest.117.2_suppl.63s. [DOI] [PubMed] [Google Scholar]
- 29.Kerstjens HA, Engel M, Dahl R, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med. 2012;367(13):1198–1207. doi: 10.1056/NEJMoa1208606. [DOI] [PubMed] [Google Scholar]
- 30.Kerstjens HA, Casale TB, Bleecker ER, et al. Tiotropium or salmeterol as add-on therapy to inhaled corticosteroids for patients with moderate symptomatic asthma: two replicate, double-blind, placebo-controlled, parallel-group, active-comparator, randomised trials. Lancet Respir Med. 2015;3(5):367–376. doi: 10.1016/S2213-2600(15)00031-4. [DOI] [PubMed] [Google Scholar]
- 31.Ohta K, Ichinose M, Tohda Y, et al. Long-term once-daily tiotropium Respimat® is well tolerated and maintains efficacy over 52 weeks in patients with symptomatic asthma in Japan: a randomised, placebo-controlled study. PLoS One. 2015;10(4):e0124109. doi: 10.1371/journal.pone.0124109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paggiaro P, Halpin DM, Buhl R, et al. The effect of tiotropium in symptomatic asthma despite low- to medium-dose inhaled corticosteroids: a randomized controlled trial. J Allergy Clin Immunol Pract. 2016;4(1):104.e2–113.e2. doi: 10.1016/j.jaip.2015.08.017. [DOI] [PubMed] [Google Scholar]
- 33.Raissy HH, Kelly HW. Tiotropium bromide in children and adolescents with asthma. Paediatr Drugs. 2017;19(6):533–538. doi: 10.1007/s40272-017-0258-9. [DOI] [PubMed] [Google Scholar]
- 34.Vogelberg C, Engel M, Moroni-Zentgraf P, et al. Tiotropium in asth matic adolescents symptomatic despite inhaled corticosteroids: a randomised dose-ranging study. Respir Med. 2014;108(9):1268–1276. doi: 10.1016/j.rmed.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 35.Vogelberg C, Moroni-Zentgraf P, Leonaviciute-Klimantaviciene M, et al. A randomised dose-ranging study of tiotropium Respimat® in children with symptomatic asthma despite inhaled corticosteroids. Respir Res. 2015;16:20. doi: 10.1186/s12931-015-0175-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hamelmann E, Vogelberg C, Voelker B, et al. Tiotropium add-on therapy improves lung function in children and adolescents with moderate and severe symptomatic asthma, independent of markers of allergic status. Allergy. 2017;72:S103:413. [Google Scholar]
- 37.Hamelmann E, Bateman ED, Vogelberg C, et al. Tiotropium add-on therapy in adolescents with moderate asthma: a 1-year randomized controlled trial. J Allergy Clin Immunol. 2016;138(2):441–450. doi: 10.1016/j.jaci.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 38.Vogelberg C, Engel M, Laki I, et al. Tiotropium add-on therapy improves lung function in children with symptomatic moderate asthma. J Allergy Clin Immunol Pract. 2018;6(6):2160–2162.e9. doi: 10.1016/j.jaip.2018.04.032. [DOI] [PubMed] [Google Scholar]
- 39.Szefler SJ, Murphy K, Harper T, 3rd, et al. A phase III randomized controlled trial of tiotropium add-on therapy in children with severe symptomatic asthma. J Allergy Clin Immunol. 2017;140(5):1277–1287. doi: 10.1016/j.jaci.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 40.Bisgaard H, Vandewalker M, Graham LM, et al. Safety of tiotropium in pre-school children with symptomatic persistent asthma. Eur Respir J. 2016;48(Suppl 60):PA315. [Google Scholar]
- 41.Hamelmann E, Bernstein JA, Vandewalker M, et al. A randomised controlled trial of tiotropium in adolescents with severe symptomatic asthma. Eur Respir J. 2017;49(1) doi: 10.1183/13993003.01100-2016. pii: 1601100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vogelberg C, Engel M, Laki I, et al. Tiotropium add-on therapy improves lung function in children with symptomatic moderate asthma. J Allergy Clin Immunol Pract. 2018 doi: 10.1016/j.jaip.2018.04.032. [DOI] [PubMed] [Google Scholar]
- 43.Vrijlandt EJLE, El Azzi G, Vandewalker M, et al. Safety and efficacy of tiotropium in children aged 1–5 years with persistent asthmatic symptoms: a randomised, double-blind, placebo-controlled trial. Lancet Respir Med. 2018;6(2):127–137. doi: 10.1016/S2213-2600(18)30012-2. [DOI] [PubMed] [Google Scholar]
- 44.Vogelberg C, Hamelmann E, Szefler S, et al. Once-daily tiotropium respimat add-on therapy improves lung function and control in adolescents and children with moderate symptomatic asthma. J Allergy Clin Immunol. 2017;139(2):AB95. [Google Scholar]
- 45.Rodrigo GJ, Neffen H. Efficacy and safety of tiotropium in school-age children with moderate–to-severe symptomatic asthma: a systematic review. Pediatr Allergy Immunol. 2017;28(6):573–578. doi: 10.1111/pai.12759. [DOI] [PubMed] [Google Scholar]
- 46.Schatz M, Rosenwasser L. The allergic asthma phenotype. J Allergy Clin Immunol Pract. 2014;2(6):645–648. doi: 10.1016/j.jaip.2014.09.004. quiz 649. [DOI] [PubMed] [Google Scholar]
- 47.Holgate ST, Bousquet J, Chung KF, et al. Group for the Respect of Ethics and Excellence in Science: Asthma section Summary of recommendations for the design of clinical trials and the registration of drugs used in the treatment of asthma. Respir Med. 2004;98(6):479–487. doi: 10.1016/j.rmed.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 48.Vandewalker M, Vogelberg C, Hamelmann E, et al. Tiotropium Respimat® add-on therapy improves lung function in adolescents and children with moderate symptomatic asthma, irrespective of IgE levels and eosinophil count. Poster P521 presented at: the American Thoracic Society International Conference; May 19–24; 2016; Washington, DC. [Google Scholar]
- 49.Goldstein S, Vogelberg C, Hamelmann E, et al. Tiotropium Respimat® add-on therapy is effective in children and adolescents with severe symptomatic asthma, irrespective of immunoglobulin E levels and eosinophil count. Poster P520 presented at: the American Thoracic Society International Conference; May 19–24; 2016; Washington, DC. [Google Scholar]
- 50.Beeh KM, Kirsten AM, Dusser D, et al. Pharmacodynamics and pharmacokinetics following once-daily and twice-daily dosing of tiotropium Respimat® in asthma using standardized sample-contamination avoidance. J Aerosol Med Pulm Drug Deliv. 2016;29(5):406–415. doi: 10.1089/jamp.2015.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sharma A, Kerstjens HA, Aalbers R, Moroni-Zentgraf P, Weber B, Dahl R. Pharmacokinetics of tiotropium administered by Respimat((R)) in asthma patients: analysis of pooled data from Phase II and III clinical trials. Pulm Pharmacol Ther. 2017;42:25–32. doi: 10.1016/j.pupt.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 52.Sharma A, Weise S, Szefler S. Pharmacokinetics of tiotropium in patients aged 6–11 years with moderate asthma following administration via the Respimat® inhaler. Abstract presented at EAACI PAAM Eur Acad Allergy Clin Immunol Cong; October 26–28, 2017; London, UK. [Google Scholar]
- 53.Sharma A, Aalbers R, Hamelmann E, et al. Pharmacokinetics of tiotropium administered by Respimat® in adolescent asthma patients. Eur Resp J. 2017;50:S61:PA585. [Google Scholar]
- 54.US Food and Drug Administration Tiotropium bromide clinical pharmacology review. 2016. [Accessed August 30, 2017]. Available from: https://www.fda.gov/downloads/drugs/developmentapprovalprocess/developmentresources/ucm549091.pdf.
- 55.Boehringer Ingelheim Limited Spiriva Respimat 2.5 microgram, inhalation solution – Summary of Product Characteristics. 2017 [Google Scholar]
- 56.Park HW, Yang MS, Park CS, et al. Additive role of tiotropium in severe asthmatics and Arg16Gly in ADRB2 as a potential marker to predict response. Allergy. 2009;64(5):778–783. doi: 10.1111/j.1398-9995.2008.01876.x. [DOI] [PubMed] [Google Scholar]
- 57.GlaxoSmithKline A phase III parallel group study, comparing the efficacy, safety and tolerability of the fixed dose combination (FDC) of fluticasone furoate+umeclidinium bromide+vilanterol (FF/UMEC/VI) with the FDC of FF/VI in subjects with inadequately controlled asthma. [Accessed August 30, 2017]. (NLM identifier: NCT02924688). Available from: https://clinicaltrials.gov/ct2/show/NCT02924688.
- 58.Yang S, Goyal N, Beerahee M, Trivedi R, Lee L, Pascoe S. Dose-response modelling of umeclidinium and fluticasone furoate/umeclidinium in asthma. Eur J Clin Pharmacol. 2015;71(9):1051–1058. doi: 10.1007/s00228-015-1894-z. [DOI] [PubMed] [Google Scholar]
- 59.Lee LA, Yang S, Kerwin E, Trivedi R, Edwards LD, Pascoe S. The effect of fluticasone furoate/umeclidinium in adult patients with asthma: a randomized, dose-ranging study. Respir Med. 2015;109(1):54–62. doi: 10.1016/j.rmed.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 60.Pearl Therapeutics, Inc Chronic dosing cross-over study to assess the efficacy and safety of glycopyrronium (PT001) in adult subjects with intermittent asthma or mild to moderate persistent asthma. [Accessed August 30, 2017]. (NLM identifier: NCT02433834). Available from: https://clinicaltrials.gov/ct2/show/results/NCT02433834.
- 61.Chiesi Farmaceutici S.p.A. Efficacy of LAMA added to ICS in treatment of asthma (ELITRA) [Accessed August 30, 2017]. (NLM identifier: NCT02296411). Available from: https://clinicaltrials.gov/ct2/show/NCT02296411.
- 62.Blais CM, Davis BE, Cockcroft DW. Duration of bronchoprotection of the long-acting muscarinic antagonists tiotropium & glycopyrronium against methacholine-induced bronchoconstriction in mild asthmatics. Respir Med. 2016;118:96–101. doi: 10.1016/j.rmed.2016.07.017. [DOI] [PubMed] [Google Scholar]
- 63.University of Saskatchewan Effect of a LAMA and a uLABA on the methacholine dose-response curve. [Accessed August 30, 2017]. (NLM identifier: NCT02953041). Available from: https://clinical-trials.gov/ct2/show/NCT02953041.
- 64.Salmon M, Luttmann MA, Foley JJ, et al. Pharmacological characterization of GSK573719 (umeclidinium): a novel, long-acting, inhaled antagonist of the muscarinic cholinergic receptors for treatment of pulmonary diseases. J Pharmacol Exp Ther. 2013;345(2):260–270. doi: 10.1124/jpet.112.202051. [DOI] [PubMed] [Google Scholar]
- 65.Lee LA, Briggs A, Edwards LD, Yang S, Pascoe S. A randomized, three-period crossover study of umeclidinium as monotherapy in adult patients with asthma. Respir Med. 2015;109(1):63–73. doi: 10.1016/j.rmed.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 66.Alagha K, Palot A, Sofalvi T, et al. Long-acting muscarinic receptor antagonists for the treatment of chronic airway diseases. Ther Adv Chronic Dis. 2014;5(2):85–98. doi: 10.1177/2040622313518227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Busse WW, Morgan WJ, Taggart V, Togias A. Asthma outcomes workshop: overview. J Allergy Clin Immunol. 2012;129(3 Suppl):S1–S8. doi: 10.1016/j.jaci.2011.12.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Spahn J. Clinical trial efficacy: what does it really tell you? J Allergy Clin Immunol. 2003;112(5 Suppl):S102–S106. doi: 10.1016/j.jaci.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 69.Ståhl E. Correlation between objective measures of airway calibre and clinical symptoms in asthma: a systematic review of clinical studies. Respir Med. 2000;94(8):735–741. doi: 10.1053/rmed.2000.0814. [DOI] [PubMed] [Google Scholar]
- 70.Yawn BP, Brenneman SK, Allen-Ramey FC, Cabana MD, Markson LE. Assessment of asthma severity and asthma control in children. Pediatrics. 2006;118(1):322–329. doi: 10.1542/peds.2005-2576. [DOI] [PubMed] [Google Scholar]
- 71.Crenesse D, Berlioz M, Bourrier T, Albertini M. Spirometry in children aged 3 to 5 years: reliability of forced expiratory maneuvers. Pediatr Pulmonol. 2001;32(1):56–61. doi: 10.1002/ppul.1089. [DOI] [PubMed] [Google Scholar]
- 72.Fonseca AC, Fonseca MT, Rodrigues ME, Lasmar LM, Camargos PA. Peak expiratory flow monitoring in asthmatic children. J Pediatr (Rio J) 2006;82(6):465–469. doi: 10.2223/JPED.1566. [DOI] [PubMed] [Google Scholar]
- 73.Self TH, George CM, Wallace JL, Patterson SJ, Finch CK. Incorrect use of peak flow meters: are you observing your patients? J Asthma. 2014;51(6):566–572. doi: 10.3109/02770903.2014.914218. [DOI] [PubMed] [Google Scholar]
- 74.Szefler SJ, Chmiel JF, Fitzpatrick AM, et al. Asthma across the ages: knowledge gaps in childhood asthma. J Allergy Clin Immunol. 2014;133(1):3–13. doi: 10.1016/j.jaci.2013.10.018. quiz 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.O’Brian AL, Lemanske RF, Jr, Evans MD, Gangnon RE, Gern JE, Jackson DJ. Recurrent severe exacerbations in early life and reduced lung function at school age. J Allergy Clin Immunol. 2012;129(4):1162–1164. doi: 10.1016/j.jaci.2011.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.O’Byrne PM, Pedersen S, Lamm CJ, Tan WC, Busse WW, START Investigators Group Severe exacerbations and decline in lung function in asthma. Am J Respir Crit Care Med. 2009;179(1):19–24. doi: 10.1164/rccm.200807-1126OC. [DOI] [PubMed] [Google Scholar]
- 77.Cabana MD, Kunselman SJ, Nyenhuis SM, Wechsler ME. Researching asthma across the ages: insights from the National Heart, Lung, and Blood Institute’s Asthma Network. J Allergy Clin Immunol. 2014;133(1):27–33. doi: 10.1016/j.jaci.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fuhlbrigge A, Peden D, Apter AJ, et al. Asthma outcomes: exacerbations. J Allergy Clin Immunol. 2012;129(3 Suppl):S34–S48. doi: 10.1016/j.jaci.2011.12.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Caldwell PH, Murphy SB, Butow PN, Craig JC. Clinical trials in children. Lancet. 2004;364(9436):803–811. doi: 10.1016/S0140-6736(04)16942-0. [DOI] [PubMed] [Google Scholar]
- 80.Cloutier MM, Schatz M, Castro M, et al. Asthma outcomes: composite scores of asthma control. J Allergy Clin Immunol. 2012;129(3 Suppl):S24–S33. doi: 10.1016/j.jaci.2011.12.980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bacharier LB, Guilbert TW. Diagnosis and management of early asthma in preschool-aged children. J Allergy Clin Immunol. 2012;130(2):287–296. doi: 10.1016/j.jaci.2012.04.025. quiz 297–298. [DOI] [PubMed] [Google Scholar]
- 82.Murphy KR, Zeiger RS, Kosinski M, et al. Test for respiratory and asthma control in kids (TRACK): a caregiver-completed questionnaire for preschool-aged children. J Allergy Clin Immunol. 2009;123(4):833.e9–839.e9. doi: 10.1016/j.jaci.2009.01.058. [DOI] [PubMed] [Google Scholar]
- 83.Lipworth B. Targeting the small airways asthma phenotype: if we can reach it, should we treat it? Ann Allergy Asthma Immunol. 2013;110(4):233–239. doi: 10.1016/j.anai.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 84.Ciprandi G, Cirillo I, Pasotti F, Ricciardolo FL. FEF25-75: a marker for small airways and asthma control. Ann Allergy Asthma Immunol. 2013;111(3):233. doi: 10.1016/j.anai.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 85.Gibb E, Kaplan D, Thyne SM, Ly NP. Fef 25-75 as a predictor of asthma severity in children. Paper presented at: American Thoracic Society International Conference; May 21; 2012; San Francisco, CA. [Google Scholar]
- 86.Quanjer PH, Weiner DJ, Pretto JJ, Brazzale DJ, Boros PW. Measurement of FEF25–75% and FEF75% does not contribute to clinical decision making. Eur Respir J. 2014;43(4):1051–1058. doi: 10.1183/09031936.00128113. [DOI] [PubMed] [Google Scholar]
- 87.Komarow HD, Myles IA, Uzzaman A, Metcalfe DD. Impulse oscillometry in the evaluation of diseases of the airways in children. Ann Allergy Asthma Immunol. 2011;106(3):191–199. doi: 10.1016/j.anai.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Larsen GL, Morgan W, Heldt GP, et al. Childhood Asthma Research and Education Network of the National Heart, Lung, and Blood Institute Impulse oscillometry versus spirometry in a long-term study of controller therapy for pediatric asthma. J Allergy Clin Immunol. 2009;123(4):861.e1–867.e1. doi: 10.1016/j.jaci.2008.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.James A, Hedlin G. Biomarkers for the phenotyping and monitoring of asthma in children. Curr Treat Options Allergy. 2016;3(4):439–452. doi: 10.1007/s40521-016-0106-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.McQuaid EL, Kopel SJ, Klein RB, Fritz GK. Medication adherence in pediatric asthma: reasoning, responsibility, and behavior. J Pediatr Psychol. 2003;28(5):323–333. doi: 10.1093/jpepsy/jsg022. [DOI] [PubMed] [Google Scholar]
- 91.Palo Alto Medical Foundation Inhaled medications: anticholinergics. 2015. [Accessed August 30, 2017]. Available from: http://www.pamf.org/asthma/medications/inhaled/atrovent.html.
- 92.Dalby RN, Eicher J, Zierenberg B. Development of Respimat(®) Soft Mist™ Inhaler and its clinical utility in respiratory disorders. Med Devices (Auckl) 2011;4:145–155. doi: 10.2147/MDER.S7409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wachtel H, Kattenbeck S, Dunne S. The Respimat® development story: Patient-centered innovation. Pulm Ther. 2017;3(1):19–30. [Google Scholar]
- 94.Hodder R, Reese PR, Slaton T. Asthma patients prefer Respimat Soft Mist Inhaler to Turbuhaler. Int J Chron Obstruct Pulmon Dis. 2009;4:225–232. doi: 10.2147/copd.s3452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Boehringer Ingelheim Asthma: Expanded indication for SPIRIVA Respimat for people 6 years and older. [Accessed May 24, 2018]. Available at: https://www.boehringer-ingelheim.com/press-release/expanded-asthma-indication-spiriva-respimat-eu.