ABSTRACT
Rising environmental temperatures represent a major threat to human health. The activation of heat advisories using evidence-based thresholds for high-risk outdoor ambient temperatures have been shown to be an effective strategy to save lives during hot weather. However, although the relationship between weather and human health has been widely defined by outdoor temperature, corresponding increases in indoor temperature during heat events can also be harmful to health especially in vulnerable populations. In this review, we discuss our current understanding of the relationship between outdoor temperature and human health and examine how human health can also be adversely influenced by high indoor temperatures during heat events. Our assessment of the existing literature revealed a high degree of variability in what can be considered an acceptable indoor temperature because there are differences in how different groups of people may respond physiologically and behaviorally to the same living environment. Finally, we demonstrate that both non-physiological (e.g., geographical location, urban density, building design) and physiological (e.g., sex, age, fitness, state of health) factors must be considered when defining an indoor temperature threshold for preserving human health in a warming global climate.
KEYWORDS: Climate change, extreme heat events, elderly, chronic disease, heat-related mortality, heat stress, overheating, urban heat island, air conditioning, sleep
Introduction
A 2017 report in Nature Climate Change concluded that the threat to human life from excess heat now is inevitable [1]. Heat exposure, especially for several consecutive days, can cause potentially deadly heat-related illnesses such as heat exhaustion and heat stroke [2]. Children, the elderly, and individuals with chronic health conditions are particularly vulnerable [3–12]. However, at present, there are only few recommendations on how best to help and protect heat-vulnerable populations who are exposed to hot weather especially in their homes where high indoor temperature can threaten their health, thermal comfort and/or quality of life.
Climate change is not only associated with rising outdoor temperatures, but also increases in the air temperature of the indoor environment (i.e., buildings, houses) [13], particularly during prolonged periods of hot weather (e.g., heat waves) [14]. Factors such as modern building design and insulation (buildings being more air tight, more efficient window designs, etc.) [15–17], increased urbanization [18–20] as well as urban form and sprawl [18,20–22] have led to elevations in indoor temperature and a subsequent rise in mortality risk from heat exposure in recent years. In fact, most heat-related fatalities occur in an indoor environment (i.e., home) [5,23,24], with exposure to high indoor temperatures forming an underlying cause of many heat-related fatalities during extreme heat events [11,25,26].
It is well established that a strong relationship exists between rising outdoor temperature and mortality, whereby mortality begins to rise above a specific temperature threshold – the heat threshold [27–29]. However, indoor temperature patterns can vary markedly from those measured outdoors during heat waves [16,30–33] which could affect this relationship. For example, while outdoor temperatures at nighttime typically decrease from peak daytime levels during hot weather, indoor temperatures tend to remain elevated [13,32]. Moreover, indoor temperature can rise progressively over consecutive days of extreme outdoor heat exposing dwelling occupants to a sustained heat stress [32]. Consequently, in the absence of adequate protective measures (e.g., operable windows to enhance air exchange, mechanical ventilation, air conditioning, etc.) and/or appropriate behavioral strategies to implement these measures (e.g., ability to turn on air conditioner, open window, close window blinds, etc.), a continuous exposure to high indoor temperature conditions can lead to heat-related injuries, and in extreme situations death in the most vulnerable individuals [11,25,26]. Even short periods of heat exposure can reduce functional ability [34,35], quality of life (including sleep quality) [31,36] and thermal comfort [31,37,38]. Furthermore, exposure to heat can exacerbate existing health conditions such cardiovascular and respiratory disease, resulting in increased hospital admissions and mortality [6,39,40].
To date, only few studies have investigated indoor temperature in dwellings of heat vulnerable occupants and even fewer have assessed the impact of rising indoor temperature on heat-related morbidity and mortality [16,17,31,41,42]. Many countries, regions, and/or cities have instituted heat action plans, with a purpose to reduce heat-related mortality and morbidity [28,43–49]. These heat action plans are activated when a specific outdoor ambient temperature that is considered to be high-risk is exceeded. However, recent findings indicate that indoor temperature that is likely to better represent heat exposure of vulnerable populations [31] especially given that they spend almost 90% of their time indoors [50,51].
In this review, we examine our current understanding of the relationship between outdoor temperature and human health during hot weather and discuss how exposure to high indoor temperatures can mediate this response. We also discuss the consequences of overheating in dwellings and evaluate how factors such as geographical location, urban sprawl, building design and other factors can influence this temperature response. Additionally, we assess how physiological adaptations and behavioural adjustments to hot weather play a role in mitigating an individual's susceptibility to indoor heat stress. Finally, we discuss the need to establish indoor temperature thresholds during hot weather and the directions that have been taken to define and implement these limits.
Heat waves and human health
Extreme heat events produce the highest death tolls when compared with all natural weather hazards [52,53], resulting in an unexpected quick and dramatic increase in short-term mortality among vulnerable populations [6,54]. For this reason, it is viewed as a silent killer. The most vulnerable populations are children [55–57] as well as older adults and individuals with type 2 diabetes [6,25,58] especially those with associated co-morbidities such as obesity [6,59–62] and/or cardiovascular disease [6,8,25,63,64]. In the case of euhydrated older adults and individuals with type 2 diabetes, recent studies show that this vulnerability is attributed to an age- and disease-mediated reduction in whole-body heat dissipation leading to greater body heat storage (Figure 1) [65–72]. In addition to the above groups, people living alone as well as deprived individuals show increased mortality rates during heat waves [3–12], which highlights the key roles of isolation and socioeconomic factors on the vulnerability to heat waves [7]. Overall, it is important to underline that, although there are groups that are particularly vulnerable during heat waves, no segment of the population can be considered to be protected from the risks associated with hot weather [5,58].
Figure 1.
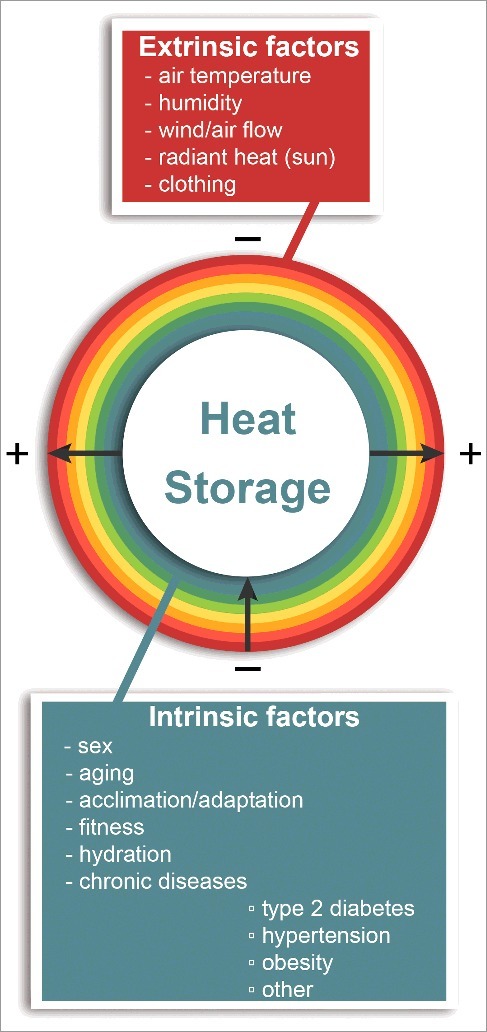
Environmental (extrinsic) and non-environmental (intrinsic) factors affecting whole-body (-, reduction; + increase) heat exchange and the amount of heat stored in the body during rest and physical activity in the heat.
Epidemiological evidence demonstrates a 2–5% increase in all-cause mortality in the elderly for every 1°C increase in the average daily outdoor temperature during the warm summer period [73]. Although heat-related mortality increases rapidly from the start of a heat wave, the impact on human health and the health care system extends beyond the heat event. In fact, the adverse effects of extreme heat are evident for as long as three to four days after the maximum outdoor temperature peak [64,74], albeit the greatest effects typically occur for temperature on the same or following day [39,75–77]. The dramatic effect of heat on human health was revealed during a major heat wave in Chicago in 1995. Record high temperatures of 41°C resulted in 739 heat-related deaths over a 5-day period [11]. In 2003, a large-scale catastrophic effect of extreme heat on population health occurred when ∼70,000 excess deaths were recorded in Europe during a two-month heat wave (average temperature ≥30°C; peak temperatures >40°C) [26]. The death toll is purported to have exceeded 70,000 by the end of the nearly two month long heat wave in 2010 [78]. These catastrophic events also highlight the fact that people living in temperate climates (e.g., northern temperate Asia, the northern United States, southern Canada, and parts of northeastern Europe) are not immune from the serious health impacts associated that extreme heat events can cause.
Recent reports also show that health care costs associated with extreme heat events are rising dramatically [79] and will place an insurmountable strain on health care systems worldwide [80]. Between 2000 and 2009, extreme heat events resulted in nearly $5.4 billion in additional health care costs in the United States [80] representing 37% of the $14 billion in health care costs associated with climate change related events including infectious disease outbreaks, hurricanes, wildfire, and floods. In Canada, it is estimated that the impact on the Québec health care system alone and Québec society in general would exceed $33 billion over the next 50 years [81]. However, the health impacts of heat waves and the associated cost on the health care system are likely to rise beyond these estimates as the rapidly aging population [82] relocates to urban areas to be closer to essential services like health and social care [52,83,84]. These large, highly-dense, urban centres experience some of the highest temperatures during hot weather periods [74,85,86] (i.e., due to the heat island effect – area that is significantly warmer than its surrounding rural areas due to human activities). In the absence of any adaptation of the population or infrastructure, heat-related mortality will rise dramatically over the next few decades [87].
At present there is an alarming scarcity of guidance about how to respond to extreme heat events and how to address heat-related health risks [88]. International evidence suggests that appropriate public health programs can dramatically limit heat-related mortality [89–91]. Unfortunately, the most recent meta-analysis on the topic reported that knowledge on the effects of heat exposure on heat vulnerable populations remains incomplete [92]. This limits our ability to define evidence-based thresholds and/or limits (i.e., high-risk ambient conditions) for the activation of short-term (e.g., work/exercise exposure limits, heat advisories, maximum indoor temperature standards, others) and long-term (e.g., heat adaptation strategies for individuals) heat protection measures and prevention strategies to alleviate the level of thermal strain during heat waves. In the absence of adequate mitigation measures, human mortality due to extreme heat events will increase in a warmer climate. Even acclimatization may not protect humans from unprecedented or intolerable heat stress under severe warming scenarios due to human physiological limits [93].
Urbanization and heat stress
Urbanization continues at a high pace in many countries. For example, in highly developed industrialized countries with temperate climates like Canada, large cities such as Montreal, Toronto and Vancouver are experiencing a rapid population growth and increased urban development [94]. The latter is noteworthy because the urban environment, and therefore temperature, is strongly affected by the design and density of buildings and by other manmade changes (e.g., addition of asphalt roads and pathways, removal of trees, elimination of open green space areas, others) [84]. Indeed, some of these large Canadian metropolitan cities have experienced some of the largest urban-mediated increases in the number of high heat stress days and nights comparable to those in large cities with hotter climates like Phoenix, Houston and New York in the United States [95]. As global average surface temperatures are predicted to rise and heat waves are expected to increase in intensity, frequency and duration [1,87,96,97], dense urban environments will be most impacted because of the urban heat island effect [98–102].
The term “heat island” describes built-up areas that are hotter than nearby rural areas. Heat islands can form over any built-up area, but especially occurs over large cities where surfaces (e.g., asphalt roads, buildings, other) have a tendency to absorb large quantities of solar radiation during the day and transfer that thermal energy to the environment during the night, resulting in higher ambient temperatures and intensifying the effects of heat waves [39,52]. The lack of green space exacerbates the effect such that peak temperatures vary across the city depending on the type of land cover [103]. In fact, green spaces are associated with decreased heat-related morbidity and mortality in urban areas [10,104].
Urbanization and the associated urban heat island effect can cause the ambient temperature within a city to be as much as 10°C hotter than surrounding rural regions [105–107]. Furthermore, the heat island effect prevents the cooling of buildings at night such that night-to-day difference is reduced. In such situations, the decline in outdoor temperature during the evening is insufficient to provide urban dwellers with adequate opportunity to cool [108]. Further, urban areas have a distinct asymmetry in their daily temperature cycle compared to rural areas. High heat stress days and nights occur more frequently in urban areas when compared with rural areas [95]. Consequently, the urban heat island can lead to earlier mortality and morbidity during heat waves in urban areas as compared to rural areas [87,109–111]. This is especially the case in urban areas located in temperate climates [111]. While epidemiological studies of urban populations reveal that daily mortality increases as ambient temperature rises above a specific-city threshold (as typically defined by a central outdoor temperature measured at an airport or other central location) [75,112], there is spatial heterogeneity in the mortality response to high ambient temperatures [62,99]. Higher mortality rates occur in denser, and potentially warmer areas within cities, while other locations in those cities are less affected [99,113,114].
Increasingly, research has been directed at characterizing the urban heat island effect through different weather research and forecasting models to simulate the metropolitan climate to better understand how urban form and design may affect temperature patterns during extreme heat events [106,124]. Combined with the development of building energy models, the knowledge acquired from this research is used to facilitate the development and implementation of new protective measures and construction standards for the protection of human health against the potentially deadly effects of high-risk outdoor temperature extremes. In recent years, this research has also included work directed at understanding how outdoor weather patterns affect indoor temperature conditions and how factors such as dwelling characteristics may affect this response.
Outdoor temperature and human health
The relationship between weather (e.g., outdoor ambient temperature) and human health typically exhibits a U- or J-shaped curve wherein the heat-related morbidity and mortality rises exponentially when temperatures exceed a threshold value [101,115]. The assessment of the thermal environment on temperature-attributable mortality has served as a valuable tool to assess the acute health effects of heat exposure over time [20,102,115–121]. The consistency of this heat-mortality relationship has spawned heat management strategies to protect health, which have included heat warning systems for entire metropolitan areas or regions [28,43–49,122]. However, there are a number of factors such as geographical location and climate type, seasonal influences (i.e., time of year when the heat wave occurs such as early in the summer versus late in the summer) and others (Figure 2) that have been shown to affect human health during heat waves and, therefore, the temperature-attributable mortality [20,99,102,115–121,123–127]. Humidity is an equally important factor in defining when climatic conditions become fatal. The threshold at which temperature becomes deadly decreases with increasing relative humidity [1]. This is because air saturated with water vapour prevents sweat evaporation, which is our primary heat loss mechanism [128]. Consequently, as the body dissipates less heat, a greater amount of heat is stored in the body leading to potentially dangerous increases in body core temperature paralleled by a progressive state of dehydration and therefore elevated level of cardiovascular strain [129].
Figure 2.

Defining an indoor temperature threshold and the factors that can influence the response.
Studies show that there is a marked variation in the outdoor temperature threshold at which increases in heat-related mortality occurs between locations (e.g., cities, regions, countries, others) [115,118,120,125,126,130–135]. This is due to the fact that heat-related mortality and morbidity are strongly influenced by regional climate and human adaptation. People residing in hotter climates tend to cope better in extreme heat [121,127] and in general, the temperature threshold for heat-related mortality is lower in cooler climates and higher in warmer climates [20,115,120,125,126,136,137]. However, the largest effects of heat on human health are especially observed in regions with milder summers where hot weather may be severe but infrequent in occurrence [20,133,138]. Irrespective of the absolute temperature threshold, risk increases proportionally to rises in temperature. Additionally, temperatures exceeding these thresholds are also associated with increased emergency room visits and hospital admission rates [74,139,140] albeit the threshold is higher in those regions or countries with hotter weather demonstrating that human adaptation is an important mediator.
In addition to geographical variations, the heat-threshold can differ for different health outcomes [20,141]. For example, studies show that increases in heat-related risks occur at different outdoor temperature thresholds for cardiovascular-related mortality and all-cause mortality [11,20,102,115–121,123–125,132,142,143]. Moreover, studies show that a lower threshold for heat-related mortality can occur for a relatively lower air temperature if the exposure occurs over successive days. Loughan et al. [139] identified a different threshold for daily (30°C) versus a 3-day average (27°C) temperature above which a significant increase in hospital myocardial infarction occurred. Specifically, they showed that days exceeding these thresholds resulted in markedly different outcomes in terms of increases in hospital admission that were estimated at 10% and 38% respectively for the daily and 3-day average conditions respectively.
Physiological factors such as those associated with sex, age, fitness and others can also alter the temperature threshold of heat-related mortality and morbidity and, therefore, the absolute temperature at which rapid increases in mortality occur during hot weather [144]. Moreover, individuals who lack access or the ability to access appropriate protective measures during extreme heat conditions such as air conditioning, cooling centres, etc. and/or who live in densely populated areas (i.e., urban centres) are especially vulnerable to temperature extremes [11]. Consequently, a lower temperature threshold for heat-related mortality and morbidity is observed [11,20]. Short-term acclimatization, as can occur over the summer period for example [145], can also influence this response such that the threshold temperature for increases in heat-related mortality is increased when hot weather occurs in late summer or early fall as compared to the late spring/early summer [125]. While this downward shift in heat-related mortality is associated with physiological adaptations, behavioural adjustments also play an important role [146].
Although temperature-attributable mortality data provides important information, caution must be used when applying this information to define threshold limits for high-risk ambient conditions. The marked variability in the temperature threshold at which increases in heat-related mortality occur underscores an important limitation of defining a single temperature from which to protect human health. This is because the thresholds above which heat stress conditions become sufficiently hazardous to human health to warrant a health warning varies between locations depending on their climate as well as between population groups (e.g., older adults, individuals with chronic health conditions). As such, defining a single heat-threshold from which to implement a broad based heat management strategy or advisory (e.g., heat alert) to protect health for a broader region or country may under-protect some populations while over-protecting others [134]. Ultimately however, identifying a specific threshold is an important challenge that must be addressed as the identification of heat-thresholds play an important role in the management of public health during heat waves as well as the implementation of heat alert systems [28,147].
Given that heat-related mortality and morbidity are strongly influenced by regional climate and human adaptation, it may be more appropriate to represent the impact of hot weather on human health as a relative change from the ‘normal’ conditions as opposed to using a given absolute ambient temperature. Using this approach would take into account spatial and group variability in the response to hot weather potentially leading to an enhanced ability to plan and respond to extreme heat events and protect the health of vulnerable people. For example, emergency managers can reprioritize allocation of medical resources to those areas most likely to be affected by extreme heat conditions [99]. Unfortunately, however, evidence on the utility of this approach as a means to mitigate heat-related illnesses during extreme heat events is currently unavailable.
Another important consideration is whether the use of a single or central site (e.g., using airport temperature) measure of outdoor ambient conditions (e.g., temperature and/or humidity) is sufficient to broadly define vulnerability to heat of a population or group. An over- or under-estimation of outdoor temperature can lead to a misclassification of exposure, which can have catastrophic consequences in the most vulnerable people. The challenge remains in quantifying heat exposure levels that can be highly variable between individuals. This is because individuals are not uniformly exposed to the high heat conditions during hot weather (including other heat sources), especially within cities where outdoor temperature can vary markedly between neighborhoods [15,99]. Furthermore, individual differences in daily activity patterns as well as the type, duration and intensity of the heat exposure (e.g., indoor versus outdoor exposure, source heat – radiant or self-generated during increase physical activity, other) [148] are also important factors (Figure 2).
Various heat stress indices are used to establish heat thresholds and some combine temperature, humidity and/or wind to give a better estimate of the temperature equivalent perceived by the individual [149]. These are generally described or classified as simple and complex indices of heat stress. One of these simple indices is the apparent temperature that combines mean temperature, relative humidity and air velocity. Of note, it has been shown that outdoor temperature and apparent temperature (but not relative humidity) are strongly correlated to indoor temperatures only when outdoor temperatures are warm [41]. Maximum or minimum apparent temperature [120,150] can also be used in place of mean temperature [121]. It is a measure of relative discomfort from combined heat and high humidity [151] and it is a way of measuring how hot the ambient condition feels when relative humidity is factored with the actual air temperature. Simply, the apparent, or “feels-like” temperature, considers the real air temperature in addition to other weather conditions that can modify what the air feels like (i.e., humidity and wind). This measure was used in a number of studies to assess heat effects on mortality [120,121].
In addition to the apparent temperature, the heat index (or mean heat index; United States National Oceanic and Atmospheric Administration issues heat warnings for the entire United States based on the mean heat index) or humidex (developed in Canada and used by Canadian meteorologists) are widely used. They measure the effect of humidity on the perception of temperatures above 27°C [109]. As humidity increases, the air is perceived to be hotter due to the reduction in evaporation of sweat [128]. Humidex differs from the heat index in that it is derived from the dew point rather than the relative humidity. Complex indices consider numerous meteorological and physiological parameters that assess the heat load for a particular place or area. These parameters include air temperature, water vapour pressure, wind velocity and short- and long-wave radiant fluxes. These can be divided into two categories, synoptic weather classifications (derived solely from observed meteorological parameters) and heat budget models (which use meteorological parameters to predict physiological heat load). The latter is also widely used for the assessment of indoor thermal comfort.
Despite the development of complex methods to estimate heat exposure and our growing knowledge about the consequences of temperature on human health, there is no consensus on what measure of temperature is the best predictor of mortality [152]. Maximum, minimum or mean temperatures have typically been used as simple and effective methods to estimate the exposure. Typically, daily maximum temperature represents peak day time temperatures at a time when people are more active, whereas minimum temperatures reflect night time conditions when most people are less active (i.e., resting, sleeping). In contrast, mean temperature provides a more representative measure of the hour-to-hour changes in ambient temperature conditions (typically the estimate is based on multiple observations over the day) and is thought to be less prone to measurement error compared with the temperature extremes. Among the various weather indices, maximum heat index has been shown to be better than models using other simple indices such as maximum, minimum or average temperature, as well as more complex models such as spatial synoptic classification of weather type for assessing public health risk due to hot weather [153,154]. Barnett and colleagues [155] examined mean, minimum and maximum temperature with and without humidity, as well as apparent temperature and the Humidex. They showed that no temperature measure was consistently the best at predicting mortality in all age groups, seasons or regions; rather they observed marked variations in the best temperature measure across all the aforementioned parameters. However, a strong correlation between different measures of temperatures were measured leading the authors to conclude that the choice of temperature measurement to use should come down to one of practical convenience [155]. It has been argued that using daily data might miss the very short-term heat effects that are especially important in heat vulnerable populations. In this context, it has been suggested that examining the effects by hour (time of day), rather than using more conventional metrics (i.e., maximum, minimum or average temperature) would allow a more specific identification of high-risk periods when health would be negatively impacted [99,156,157].
The interrelationship between indoor and outdoor temperature on human health
It is estimated that people, especially the most vulnerable (i.e., older adults and individuals with chronic disease) spend the majority (80-90%) of their time indoors [50,51]. This raises important concerns about the validity of employing outdoor measures to define heat-related risks for human health. During heat waves, high outdoor temperatures can persist for several consecutive days and, when night temperatures do not decrease enough to allow buildings to cool down, overheating in homes can occur (characterized as the unintended rise in internal building temperature) [13]. As mentioned earlier, exposure to high indoor temperature was an underlying cause of many heat-related fatalities in the 2003 European heat wave [26]. Moreover, during the 1995 Chicago heat wave, those who did not leave their homes at least once a day and did not have access to transportation had higher mortality [11,25]. Similar trends were found in the 1999 Chicago heat wave [9].
While there has been limited research examining the relationship between indoor and outdoor temperature, some studies show this relationship to be linear especially in buildings that are naturally ventilated [158] regardless of how hot ambient temperatures may become [15]. Nevertheless, this may not always be the case. In the United Kingdom, it has been estimated that overheating affects more than 20% of households, underlying a potential danger that extreme heat events may have in vulnerable dwellings [159]. Wright and colleagues [33] were perhaps the first to actually measure indoor temperatures during a heat wave (part of the European heat wave of 2003) in five occupied houses in London and four in Manchester of diverse ages, sizes and construction. They reported large differences in indoor temperatures between homes, as well as between rooms within homes that included different peak temperatures and levels of discomfort. For homes in London, indoor temperatures exceeding 25ºC occurred more than 90% of the time, with six out of nine rooms above 25ºC for an entire week, and displaying a temperature higher than 28ºC between 22% and 80% of the time.
The Passivhaus Institute defines overheating in homes as temperatures exceeding 25ºC for more than 10% of the year [160]. The Chartered Institution of Building Services Engineers (CIBSE) in London, England recommends an operative summer temperature of 23–25ºC for living spaces whereby residents should not be exposed to ambient temperatures in excess of 25ºC for more than 5% of the occupied time and no more than 1% of occupied time above a threshold temperature of 28ºC [161]. The latter is considered an overheating criterion that is commonly used by industry. Healthcare Technical Memorandum 03-01 from the United Kingdom Department of Health [162] contains a similar criterion for overheating as employed by the CIBSE, though rather than 1% of occupied time, this guide refers to 50 hours occupied time above 28°C. For bedrooms, this threshold is lower with exceedance limits set at 5% of occupied hours over 24°C and 1% over 26°C [161]. This is based on the premise that temperatures above 24ºC can compromise sleep [163]. However, the underlying rationale for these aforementioned limits is unclear. Moreover, while the use of a fixed threshold temperature offers a method to establish the occurrence of overheating, it does not provide an indication of its severity.
In recent years, an increasing number of studies comprising monitoring [13,30,164–166] or modelling [166–171] approaches have assessed the heat risk in homes. These studies reveal that heat stress due to global warming is inevitable in many existing buildings if no adaptive measures (e.g., changes in building design, type of insulation, use of air conditioning, etc.) are taken. Consequently, occupants are likely to experience significant thermal discomfort from extended periods of elevated indoor temperatures during outdoor temperature extremes. This is supported by the findings of Mavrogianni et al. [30] who showed that in 36 homes monitored in London during a brief 5 day heat wave in the summer of 2009 (June 29 to July 3; maximum of 31ºC, minimum of 15ºC), approximately 33% of the bedrooms monitored reached uncomfortable nighttime temperatures with air temperature of 26ºC or greater. These indoor temperature extremes occurred despite the fact that average outdoor temperatures for the summer were below normal with a number of cold periods interspersed.
A recent report by Vellei and colleagues [172] showed that overheating occurs frequently in households with vulnerable occupants in the United Kingdom, even when protective measures are available such as air conditioning [172]. Similarly, White-Newsome et al. [16] (see additional details below) reported that homes with vulnerable residents in Detroit Michigan who had central air conditioning demonstrated similar high indoor temperatures to those homes without (i.e., 34.8°C and 34.4°C respectively). Interestingly, Vellei and co-workers [172] also found that vulnerable occupants reported feeling cooler when compared to their non-vulnerable counterparts. This may in part explain why similar indoor temperatures are measured in homes with vulnerable occupants with and without air conditioners. Elderly people may not feel the need to use the air conditioner which can be attributed to age-related attenuation in thermal sensation (i.e., ability to sense increased heat in the body) [173]. Ultimately, this decrease in thermal sensitivity could place heat-vulnerable people at a high risk of heat-related injury or death since it could potentially make them less likely to undertake behavioural actions for heat mitigation.
van Loenhout et al. [31] demonstrated that even small elevations above normal summer time outdoor temperature conditions can cause indoor temperature to reach levels that can negatively impact the health of heat vulnerable elderly living in a temperate climate (i.e., Netherlands). During the warmest week of the study period (August 14th to 20th, 2012), outdoor air temperature (mean temperature: 23.6ºC) was approximately 5ºC above normal conditions with the majority of the residents reporting indoor ambient conditions as being excessively warm. Many reported symptoms of thirst (43%) and excessive sweating (40%), as well as sleep disturbances (41%). Noteworthy, these symptoms were found to be exacerbated with each degree Celsius increase in indoor temperature. As the authors reported that “for an increase in 1ºC of indoor temperature, annoyance due to heat and sleep disturbance increased by 33% and 24% respectively. Outdoor temperature was associated with smaller increases: 13% and 11% for annoyance due to heat and sleep disturbances” [31]. Based on their findings, the authors surmised that indoor temperature may be a stronger predictor of health problems than outdoor temperature.
Sakka et al. [32] showed that the intensity, frequency and the length of heat waves as well as the period of time the heat event occurs (e.g., early spring versus late summer) can affect the transient changes in indoor temperatures. Their findings are based on the assessment of fifty naturally ventilated low-income dwellings (characterized by low thermal protection standards) in Athens, Greece during three brief heat waves occurring in the late spring and summer periods of 2007 (i.e., June: 5 days, June 24th to 28th, average/maximum outdoor: 34.3/41.5ºC, average/maximum indoor: 31.5/34.1ºC; July: 9 days, July 19th to 27th; average/maximum outdoor: 33.3/41.4ºC; average/maximum indoor: 31.7/33.0ºC; August: 3 days, August 22nd to 24th, average/maximum outdoor: 32.3/41.5ºC, average/maximum indoor: 31.3/34.1ºC). While they showed that increases in the intensity and/or the length of the heat event were associated with greater increases in indoor temperatures paralleled by a longer duration of peak indoor temperature. However, time of year (or seasonal effect) when the heat event occurs was shown to be an important determinant. Specifically, they showed while the August heat wave was shorter and cooler, indoor temperature reached levels similar to those measured in June due to the natural and progressive build-up of heat over the summer period.
Day-to-day variations in outdoor temperatures also play an important role in the evolution of indoor temperatures [15]. Smargiassi et al. [15] showed that outdoor temperature during the preceding hours had a larger influence on the indoor temperature than the actual (real time) outdoor temperature. Specifically, they showed that a 1ºC increment in the average temperature of the 24 preceding hours was associated with 0.36ºC increase in indoor temperatures. This influence was more than seven times greater than the near negligible influence of the current outdoor temperature (0.05ºC). Their findings were based on the hourly measurement of indoor temperature over 31 consecutive days in 75 dwellings in Montréal, Canada in the summer period (July 2005). Mean outdoor temperature recorded at Pierre-Elliott Trudeau airport located in Montréal was 22.7ºC with a maximum and minimum temperature of 32.3ºC and 10.2ºC respectively. In contrast, mean indoor temperature was nearly 4ºC higher (26.7ºC) and was paralleled by a greater recorded minimum (16.4ºC) and maximum (34.4ºC) temperature. In keeping with their observation, a prior study by Wright et al. [174] reported that the 72 hour moving average of outdoor temperatures to be highly related to indoor temperatures, albeit as noted above, Smargiassi et al. [15] showed a stronger relationship with a 24 hour moving average. This disparity may be attributable to climate variations as well as differences in building construction (e.g., type, design) between study regions. The study by Wright et al. [174] was conducted in nine dwellings in the United Kingdom (during the August 2003 heat wave; four homes in South Manchester and five in London) whereas Smargiassi examined 75 dwellings in North America (Montréal, Canada).
A growing number of studies reveal that buildings act as an important modifier of exposure to external climate, and therefore indoor temperature, thereby playing a key role in modulating the impact of heat waves on human health [16,30,33,159]. Building characteristics, such as the thermal capacity and conductivity of the construction material, type and number of windows, orientation of the house, number of floors (i.e., multi-level dwelling versus bungalows), building size and others, are important determinants of building heat gain and retention thereby modulating the outdoor to indoor temperature relationship (Figure 3) [16,30,33,159]. Indeed, as described above, studies demonstrate that for a given external ambient temperature recorded at a single or central point, indoor temperatures can vary markedly across neighborhoods and homes. As stated by the Zero Carbon Hub “this ability of the building to modify temperatures implies that the relationship between outdoor temperature and mortality cannot be simply extrapolated to indoor temperature” [159] (Note: The Zero Carbon Hub was established in 2008, as a non-profit organisation, to take day-to-day operational responsibility for achieving the government's target of delivering zero carbon homes in England from 2016. The Hub reports directly to the 2016 Taskforce).
Figure 3.
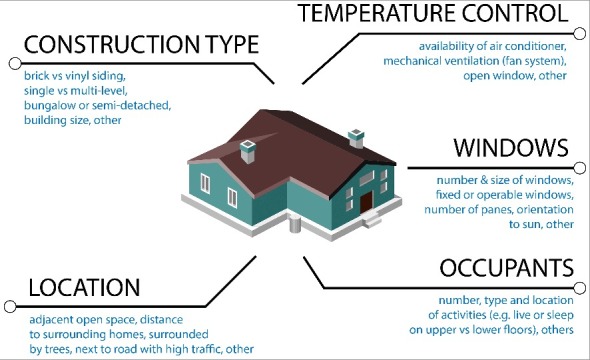
Building characteristics affecting heat gain and retention.
Recently, White-Newsome et al. [16] examined the relationship between ambient and indoor temperatures in homes (n = 55) occupied by elderly individuals (> 65 years) in metropolitan Detroit, Michigan in the summer of 2009. This assessment was conducted in context of home-specific characteristics that can influence indoor temperature and included: (i) the type of exterior construction (brick/asphalt, vinyl paneling or wood siding), (ii) the date of construction (1912–1939, 1940–1970, or after 1970), and (iii) the housing type (single family, high-rise, two-family flat). During this measurement period, a few homes achieved peak average temperatures above 32°C despite below-average ambient temperatures recorded over the measurement period. For a majority of the homes, a maximum temperature in excess of 34°C was observed. Mean outdoor temperature for the study period as recorded at the Detroit Metropolitan Airport was 21.0°C, ranging from 7.2 to 34.3°C. Across all homes, the highest daily temperature recorded ranged from 16.7 to 34.8°C with individual rooms for some dwellings reaching a maximum value of 35ºC. However, the authors reported that older non-high rise dwellings, and in particular, older houses constructed with relatively lower levels of insulation (e.g., vinyl paneling or wood siding), demonstrated the greatest indoor temperatures whereas houses constructed of higher insulating materials (e.g., brick) were more heat resilient. Furthermore, they showed that in addition to the building itself, the surrounding green coverage played a critical role in affecting indoor temperature balance.
While improving home construction (e.g., insulation, windows, etc.) and modifying home surroundings could mitigate indoor heat exposure among heat vulnerable populations, overheating is still reported in recently-refurbished and newly-built homes including those located in relatively temperate climates [13,165,166,175]. A meta-analysis of indoor temperatures in selected low-energy contemporary housing in the United Kingdom (measurement period 2012–2014) revealed that based on the CIBSE threshold of 5% annual occupied hours above 25°C (see details above for additional information), 57% of bedrooms and 75% of living rooms were classified as being overheated. The underlying reasons for such overheating remains unclear, although a number of studies have used dynamic thermal simulation to assess how different energy refurbishments might affect building overheating during hot weather [165,166,176].
It has been suggested that summer overheating may be an unintended consequence of the rapid change in the construction industry, specifically the poorly-applied energy-efficiency principles in building construction [177]. While governments have established new energy-efficient standards for new and retrofitted homes, these may not be sufficient to eliminate or alleviate the risk of overheating in homes. In fact, the need for more energy efficiency is resulting in highly insulated and air-tight dwellings that may inadvertently increase the risk of uncomfortable or excessive summer indoor temperatures [175]. In the absence of appropriate climate-change adaptation strategies (i.e., shading, natural ventilation and other passive cooling measures), as well as occupant behavioural actions (e.g., occupancy density, duration and patterns and the generation of casual loads from cooking, use of appliances, lighting, etc.), increases in indoor temperatures can be excessively high [178] potentially compromising the health of vulnerable occupants.
Ultimately, the protection of vulnerable populations to the adverse effects of extreme heat to human health will involve the assessment of structural quality of dwellings. This is supported by the findings of Oikonomou et al. [169] which determined that the thermal characteristics and qualities of a home accounts for a greater variation in indoor temperature than the effect of location within the urban environment (i.e., the urban heat island effect) itself during hot weather. In the context of the structural/design characteristics of the home, it has been shown that upper stories, a southern orientation, and an elevated glazing-to-wall ratio is associated with a greater increase in solar heat gain [179] and increased insulation and air-tightness and a reduced wall area-to-volume ratio prevent the release of accumulated heat [180].
The fact that the dwelling itself is a key determinant of indoor temperature transient highlights the need for greater efforts to ensure the effective implementation of strategies to minimize overheating and therefore unsafe elevations in indoor temperatures. In addition to improving the thermal quality of dwellings, research would need to be conducted to identify effective strategies to mitigate outdoor temperature extremes through modification of the urban environment (e.g., plant more trees, reduce building size, use of windows, others) where the risks of overheating in homes is greatest. Given that exposure to higher temperatures is more likely in urban areas, work must also be done to assess how the balance between the effects of the urban heat island and indoor temperatures (and therefore overheating) might change as a function of newer construction approaches and types. This need is especially important in context of the intensification of the urban heat island that is likely to occur with climate change and the increase in urban sprawl and urban density over the next decade. Finally, despite our growing knowledge on the effects of extreme heat on indoor temperature, there remains limited information regarding the role that ambient temperatures, housing and other environmental characteristics may play in personal temperature exposure among heat vulnerable populations.
Threshold for indoor thermal comfort
An individual's thermal comfort, health and wellbeing are negatively impacted by high indoor temperature. Interestingly however, there is very little research available on links between thermal comfort and health, particularly in vulnerable population groups such as children, the elderly, individuals with chronic health conditions, those living alone, and deprived people. Multiple factors can affect an individual's thermal comfort and include environmental and personal factors. Consequently, establishing a definition of thermal comfort that applies to everyone represents a difficult challenge. An environment that is comfortable for one person may be too hot for someone else. The ANSI/ASHRAE Standard 55 [181] defines thermal comfort (also known as human comfort) as “the state of mind that expresses satisfaction with the thermal environment” and is assessed by subjective evaluation (Note: The American Society of Heating, Refrigerating and Air-Conditioning Engineers, Inc. (ASHRAE) develops standards for both its members and others professionally concerned with refrigeration processes and the design and maintenance of indoor environments. ASHRAE is accredited by the American National Standards Institute (ANSI) and follows ANSI's requirements for due process and standards development).
In a home environment, various thermal comfort models have been developed to anticipate the range of conditions most comfortable for occupants. The most commonly used model for evaluating thermal comfort is the PMV-model (Predicted Mean Vote) as defined by Fanger [182]. Based on the model, a thermo-neutral ambient condition is one wherein the individual does not prefer either a colder or warmer environment. The model has been used to define standards of thermal comfort [183,184] and has been widely employed by heating and air conditioning engineers to prescribe and design the thermal environment [185]. The CIBSE has adopted the adaptive thermal model to define thermal comfort which represents an important paradigm shift from the heat-balance approach [186]. The adaptive thermal comfort model is based on the principle that an individual's thermal expectations and preferences are determined by their experience of recent (outdoor) temperatures such as seasonal variations in environmental conditions, and a range of other dependent factors, such as their access to environmental controls. The adaptive thermal comfort model allows for the natural physiological adaptation associated with extended periods of excessive heat (and cold). It is stated that, by using the adaptive thermal comfort model, contrary to the use of static comfort temperatures, the periods of discomfort are less likely to be overestimated.
In practice, the sensation of comfort responds to the changing conditions that are experienced during each day. However, thermal comfort is difficult to interpret because it is highly influenced by individual objective and subjective factors as well as environmental conditions (e.g., air temperature, humidity, radiant temperature, air velocity) (Figure 1). Moreover, each individual experiences these sensations differently based on the individual's state of well-being, age, sex, level of adaptation (acclimatization), hydration status, level of fatigue, and others (Figure 1). For example, people who live in areas with frequent high heat and humidity are better able to tolerate such conditions than those who do not [187]. Additionally, relative to their younger counterparts, older adults are less sensitive to thermal stimuli and have a tendency to feel cooler during exposure to heat [173,188]. As the body ages, changes in the body's capacity to dissipate heat causes the body to store more heat during exposure to hot environments [189] with differences becoming apparent in adults as young as 40 years [190], while substantial differences are detected in most individuals after their mid 50's [191]. As mentioned above, the perception and physiological response to high temperature change with age [192,193]. Thus, it is possible that an older person may perceive an environment to be thermally comfortable when in fact it may pose threats to their health. Notably, it is generally considered that older people prefer higher air temperatures for comfort than do younger, more active people [193]. Vellei and co-workers [172] showed that thermal comfort differs between vulnerable (defined as older than 65 years old, disabled or with long-term illness) and non-vulnerable home occupants during the summer period such that the vulnerable residents felt cooler despite experiencing similar levels of overheating in their homes.
Radiant heat transfer from surrounding objects also affects thermal comfort (Figure 1). People near hot or cold surfaces feel warmer or cooler independently of the air temperature. Comfort can also be influenced by whether a building has adequate ventilation (air flow) as well as air conditioning and whether occupants have control over the temperature [194]. Other factors such as the number of occupants in a home will also have an influence as overcrowding is associated with greater internal heat gains [180]. Vellei et al. [172] showed that rooms in vulnerable and overcrowded homes were found to have significantly higher mean temperatures, about 0.6°C higher than rooms in non-vulnerable and non-overcrowded homes as measured during the summer period. Since none of these factors remain stable, thermal comfort may vary both for the individual and among members of the household during the day and over time. Ultimately, this makes it difficult to view thermal comfort as a valid and/or reliable indicator of an individual's level of thermal strain from which safe indoor temperature limits can be defined.
Numerous studies have assessed human thermal comfort levels under indoor conditions, albeit these have been primarily conducted by building and engineering industries. Luo et al. [195] wrote “what kind of indoor climate should be created and how to create it are questions closely correlated with building energy consumption”, which highlights the impetus for examining indoor thermal comfort by these industries. As briefly discussed earlier, there are a number of factors that can affect indoor temperature including season, building type, outdoor temperature, etc. ASHRAE's Thermal Environmental Conditions for Human Occupancy Standard 55–2004 characterizes the indoor summer thermal comfort range as about 23–28°C [181] depending on the relative humidity (this assumes occupants are dressed in clothing typically worn when the outdoor environment is warm). These recommended temperature ranges are considered to meet the needs of at least 80% of individuals. However, it implies that some people may feel uncomfortable even if these values are achieved. The Canadian Standards Association recommends maintaining indoor temperatures within offices below approximately 26°C under conditions of typical relative humidity (CAN/CSA Z412-00), with adjustments required for low and high humidity conditions.
For the general population, it has been suggested that to maintain thermal comfort, sedentary activities in a room with limited air movement should not exceed 28°C [196]. Of concern however, is the fact that thermal comfort temperatures may not reflect the temperatures at which people experience health impacts from heat such as children, the elderly and individuals with chronic health conditions. The World Health Organization (WHO) guidance on thermal comfort in housing has been used to define groups that may be more susceptible to low and high indoor temperatures than others. It examines different methods for measuring thermal comfort, such as air temperature measurement, assessing resident's perception, and predicting satisfaction. As noted by Ormandy and Ezratty [197], “the World Health Organization's guidance on thermal comfort is not just about ensuring a sensation of satisfaction with the ambient temperature, it is inextricably linked to health. It is guidance for the home environment, and aimed at protecting health, particularly the health of those most susceptible and fragile to temperatures outside that range, such as the very young, and older people”. However, these recommendations should be interpreted with caution. The indoor temperature range (i.e., between 18 and 24°C on the basis that it is considered to be associated with minimal risk to health) appears to be defined solely from research on relatively healthy individuals under controlled conditions. Thus, the extent to which the WHO recommendations would protect the most vulnerable remains in question.
To the best of our knowledge, there are no studies that have systematically validated the WHO upper temperature threshold (i.e., 24ºC) for different heat-vulnerable groups (i.e., children, older adults, individuals with chronic health conditions, people living at home alone, and deprived individuals). In fact, there has been little in the way of strong scientific evidence to support the WHO recommendations. Moreover, the origins of these guidelines are somewhat ambiguous and appear to originate from a WHO Public Health Report published in 1968 titled ‘The Physiological Basis of Health Standards for Dwellings’ [198]. The authors identified an optimal temperature range of 15 to 25°C which was defined on the basis of earlier work by researchers [199–201] who showed that human energy expenditure is minimal within this range and that “within this narrow range of 7–10°C the body always reacts very sensitively to comparatively small changes in atmospheric conditions”. In 1982, a revised range of 18–24°C was subsequently introduced by the WHO albeit the underlying reasons for these revisions are unclear [202]. These guidelines remained in place and, to the best of our knowledge, have remained unchallenged. While the WHO guidance on thermal comfort in dwellings and the temperature range are frequently referred to and have been acknowledged as the range with which health is optimally protected, the evidence supporting this is still lacking.
Other approaches to define indoor thresholds
While there have been an increasing number of studies directed at assessing indoor temperature in homes during hot weather, there has been a lack of work directed at examining the corresponding physiological responses. To the best of our knowledge, Basu and Samet's study [42] is one of the few to assess the physiological responses in free-living elderly people. They measured skin temperature (as a proxy of body core temperature) and heart rate responses in 42 elderly adults within Baltimore over a 48-hour period between May and September 2000. In parallel, ambient temperature was recorded continuously with a sensor placed on the outer layer of the individual's clothing, to measure the miocroenvironmental condition. Additionally, outdoor temperature data for Baltimore corresponding to that monitoring period were acquired from the database of the National Climatic Data Center. They observed a positive association between ambient temperature, as assessed by the clothing temperature, and skin temperature with an increase in average skin temperature (i.e., a 0.15°F/0.08°C for every 1°F/0.56°C increase). No association was found between body temperature and Baltimore temperatures. While heart rate was shown to be related to activity level, no relationship was found between heart rate and ambient temperature. However, caution must be used when interpreting these findings. It has been shown that body temperature can underestimate the level of thermal strain (i.e., body heat storage) during exposure to extreme heat [72].
A recent report showed older euhydrated adults stored 1.8-times more heat as compared to their younger counterparts during exposure to high heat conditions (44ºC) (Figure 4) [72]. Body heat storage was measured by direct calorimetry (i.e., using an air calorimeter), which is the gold standard method for quantifying the heat loss from the human body [203]. However, the greater increase in body heat storage was only paralleled by a modest non-significant increase in body core temperature of 0.4-0.5°C; an increase in core temperature equivalent to a non-pathological sign of heat stress according to current guidelines for responding to extreme heat events and addressing heat-related health risks [204]. Irrespective of the shortcomings of their study, the findings by Basu and Samet [42] highlight the need to explore how physiological monitoring may provide important information to help identify risk to health during exposure to hot weather.
Figure 4.
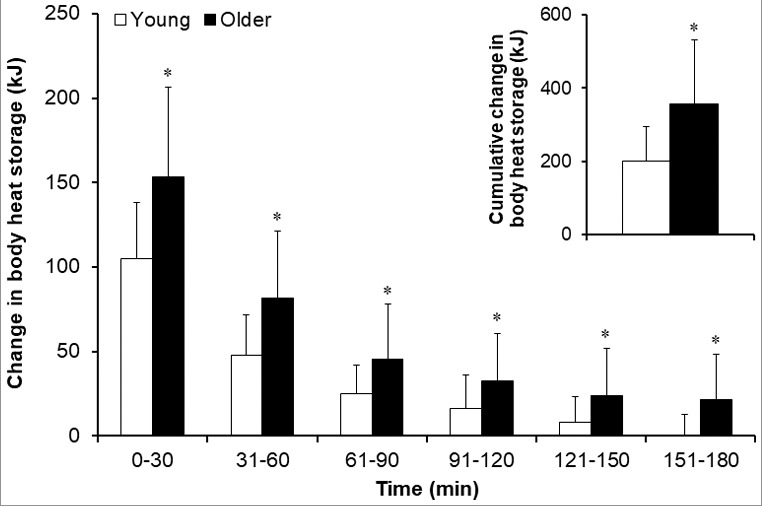
Body heat storage (mean ± SD) during a passive 3-hour extreme heat exposure in young and older adults. Note: * = comparison against the young group for the same time point statistically significant at p < 0.05; the white bars indicate the young group (19–28 y of age) and the black bars indicate the older group (55–73 y of age). Inset figure shows older adults stored 1.8-times more heat over the 3-hour exposure. Reproduced with permission (see ref. [72]).
Indoor temperature and sleep
During extreme heat events, night time outdoor temperatures can remain elevated causing indoor temperatures to also remain high. Human sleep is sensitive to the individual's environment and elevated ambient temperature can lead to frequent sleep disruptions, reduced sleep time and increased wakefulness [205–208], which is especially pronounced in the elderly [205,206]. Humidity is also considered a key factor that increases heat stress during sleep [207,209,210]. Poor sleep quality is associated with increased risk for mortality [211]. Insomnia was associated with a three-fold risk of mortality over 13–15 years follow-up especially in men and when insomnia was combined with short sleep duration [211]. A similar pattern of response has been observed in older people with a high mortality reported in those with nighttime insomnia, daytime sleepiness, and sleep-onset delay [212]. Moreover, poor sleep quality has been associated with obesity, depression, anxiety, diabetes mellitus, and cardiovascular disease [213,214]. While a direct relationship between sleep quality and heat-related mortality remains to be assessed, it is well established that elevated temperature and humidity can affect thermal comfort [215]. In turn, thermal comfort has been shown to be highly correlated with sleep quality [216]. Van Loenhout and colleagues [31] showed that elderly people experienced significant heat-related health problems during a brief heat wave (Netherlands, August 14th to 20th, 2010), which caused mean indoor temperatures to exceed 25°C. More than 40% of the monitored residents reported symptoms of heat stress (i.e., increased thirst, excessive sweating) paralleled by significant sleep disturbance and mental fatigue.
The CIBSE in the United Kingdom suggested thermal comfort and quality of sleep is affected when bedroom temperatures exceed 24°C [36]. On this basis, they recommend that bedroom temperatures at night should not exceed 26°C unless ceiling fans are available [36]. However, it is important to note that while the use of fans would be beneficial under moderate levels of heat, employing fans at more extreme ambient temperature and humidity conditions may actually cause greater heat storage in heat vulnerable older individuals [217,218].
Use of air conditioners
Mortality may be preventable by measures taken during episodes of extreme heat such as the use of air conditioners. In fact, a number of studies have shown that air conditioning diminishes the risk of heat-related mortality [9,11,25,219–221]. While health authorities recommend the use of air conditioners, surprisingly a large number of heat vulnerable adults do not have access to them or use them during a heat wave. Disparities in air-conditioning access contributed to the difference in heat wave mortality, which was nearly twice as high in minority-group residents in Los Angeles relative to the general population [47]. In the Chicago 1995 heat wave, some elderly people with air conditioning restricted ventilation in their homes by not opening windows for fear of crime which led to extreme increases in indoor temperatures and resulted in a substantial increase in mortality [222]. However, as discussed earlier access to air conditioning may not always prevent overheating in homes in elderly adults [16].
Kosatsky et al. [223] interviewed 238 patients with chronic health conditions at Montreal University hospital clinics over the 2005 summer period. Of the 173 (73%) participants who had a home air conditioning, 2% indicated that they never used their air conditioners during the day, while 17% indicated that they do not use them at night. Just over a third of the respondents (38%) ran the air conditioner all day. The average number of hours spent per 24-hour period in air-conditioned spaces during heat waves was 14.5 [224]. Of those who did not have an air conditioner, 14% spent time in a cool environment during hot weather. In a survey conducted in residents of New York City following a severe July 2011 heat wave where heat indices reached 46.1°C, Lane et al. [225] showed that a large majority of the seniors owned an air conditioner (79%). However, in contrast to the findings of Kosatsky et al., [223] of those who had an air conditioner, many never or rarely used it on hot days. Reasons for not using it included “not liking the feel, the cost of electricity, and energy conversation”. Moreover, some seniors preferred the use of fans while others felt that the use of air conditioners would worsen their health conditions (i.e., arthritis, asthma). Others indicated that they do not feel hot or that they were accustomed to the heat. Hwang and Chen [226] also showed that although air-conditioning was available in most homes, the elderly adapted to a warmer indoor condition by opening windows, adjusting clothing and using fans as opposed to employing air-conditioning.
Residents in nursing homes are particularly vulnerable to extreme heat events given their advanced age and presence of chronic health conditions. While the use of air conditioning could be effective at preventing heat-related deaths in these individuals, many long-term care facilities do not have air conditioning. Klenk et al. [227] showed that mortality rates in nursing home residents in Baden-Wurttemberg, Germany were the lowest when ambient temperatures were maintained below 26°C. In light of the fact that residents of nursing homes spend most of their time inside the facilities, an increasing number of government agencies mandate that hospitals and/or long-term care facilities have a central cooling system. For example, as a consequence of the 2003 heat wave, air conditioning equipment for nursing homes was included in the National Heat Wave Plan in France [228]. As outlined in the Long-Term Care Home Design Manual published by the Ontario Ministry of Health and Long-Term Care in 2015 [229], long-term care facilities must be equipped with “a mechanical system to cool air temperatures in all corridors, lounges, program/activity areas, all dining areas, the kitchen and the laundry space. The remaining areas of the long-term care home, including resident bedrooms, resident bath and shower rooms and resident washrooms, must have a system for tempering the air to keep air temperatures at a level that considers resident needs and comfort”.
While air conditioning may serve as an effective tool to prevent heat-related injuries or death, research demonstrates that the long term use of air-conditioning systems may itself pose a hazard to people's health [230–232]. For example, workers who had an air conditioned building versus a building with natural ventilation, experienced greater absences due to sickness and this was paralleled by an increase in medical-services (i.e., doctor visits) use, as well as hospital stays [231]. Another study showed that office workers who had home air conditioning were more likely to have visited a medical specialist in the previous year than those who had naturally ventilated homes [232]. In light of the fact that temperatures are likely to rise in the next decades and the intensity and frequency of temperature extremes will increase, there will likely be an increased exposure to air conditioning to keep vulnerable individuals protected from overheating. This will be especially necessary if indoor temperature thresholds are mandated.
A recent report showed that the demand for cooling energy increases by 5–20% for every 1°C increase in outdoor temperature [233]. A greater reliance on air conditioning may potentially lead to increases in the magnitude and frequency of peak electricity demand during extreme heat events and may contribute to heat island effects. This led to major power outages in the past; most notable of these was the 1995 heat wave in Chicago [222]. The massive power outages left people without sources of conditioned air which ultimately played a role in the death of over 739 [222]. This also raises important concerns about fuel poverty and the increasing difficulty that vulnerable populations may face in paying for the energy needed to maintain cool indoor temperatures to maintain health.
Defining an indoor temperature limit: where do we start?
As recently reported [1], about 30% of the world's population currently experiences at least 20 days per year of extreme heat conditions that can be considered deadly. However, it is expected that by the year 2100, three out of four people could be subject to this same threat which includes the most vulnerable. The need to define appropriate heat thresholds to protect human health is therefore paramount. However, to date there remains a paucity of research directed at defining ‘high risk’ ambient conditions for the most vulnerable. Some direction may be obtained from a recent report published by Toronto Public Health that suggested a maximum indoor temperature limit for multi-unit residential buildings should be set at 26°C. However, much of the evidence used to support this threshold is largely indirect. Their report notes that a City of Toronto by-law (Chapter 629, property standards), requires that apartments with air conditioning systems should be operated to maintain a maximum indoor temperature of 26°C. A recent report [85] evaluating the effects of hot temperatures on mortality across selected cities in Ontario, Canada, showed that daily mortality increased by up to ∼3% with a 5°C increase above daily mean temperature. However, the risk of mortality increases as outdoor temperature increases (i.e., ∼4-5% at 30°C). Since the median ambient temperature for the warm-temperature months in Toronto is ∼21°C, maintaining an indoor temperature limit of 26°C would substantially reduce the risk of heat-related mortality. A lower temperature however, would likely be required to ensure that all vulnerable people who have an impaired capacity to dissipate heat are protected.
The National Health Services (NHS) in England has also recommended that indoor temperatures should not exceed 26°C. This provision however, which is part of the NHS heat wave plan for England [234], is specifically recommended for rooms or areas (cool zones) where people in long-term care, nursing, and residential facilities can relocate during heat waves to keep cool. During heat emergencies, New York City's Office of Emergency Management which coordinates a multi-agency response that incorporates widely recommended best practices for protecting health during extreme heat events recommends that at-risk individuals visit a cooling centre or use air conditioning set at 78°F (∼25.5°C). Interestingly, this recommendation is in part defined by the need to lessen the strain on the energy grid while providing an environment that is protective to health [235]. Ultimately, it is important to note that the range of acceptable temperatures can differ between population groups (e.g., children, the elderly, individuals with chronic disease, etc.). This is because there are differences in how groups of people may respond to the same living environment [57,226]. Moreover, there is high degree of variability related to thermal comfort of indoor temperatures between and within groups [226].
Summary
The predicted temperature threshold whereby the climatic conditions can become lethal varies across countries, regions and cities; a pattern of response which can be ascribed to factors such as time of year, level of adaptation, behaviour and others. Moreover, marked differences may also occur between and within households due to the variations in microenvironment temperature.
While our knowledge on the effects of extreme heat events on outdoor temperature patterns is extensive, there remains limited information on the physiological strain associated with excessive indoor temperatures. Translating this information into definable indoor temperature thresholds above which heat stress conditions become sufficiently hazardous to human health remains a challenge. Beyond the numerous environmental factors, personal factors such as sex, age, and state of health can influence an individual's ability to thermoregulate, and must therefore be considered when defining evidence-based thresholds for high-risk indoor ambient conditions. Furthermore, work directed at the development of heat wave vulnerability indices for high-risk urban environments must be encouraged as this will allow the mapping of overheating risk and identification of prioritization areas by public health policy-makers.
Acknowledgments
This work was supported by Health Canada.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed
References
- [1].Mora C. Dousset B, Caldwell IR, et al. Global risk of deadly heat. Nat Clim Change. 2017;7:501–506. doi: 10.1038/NCLIMATE3322. [DOI] [Google Scholar]
- [2].Glazer JL. Management of heatstroke and heat exhaustion. Am Fam Physician. 2005;71(11):2133–2140. PMID:15952443 [PubMed] [Google Scholar]
- [3].Rey G, Jougla E, Fouillet A, et al. The impact of major heat waves on all-cause and cause-specific mortality in France from 1971 to 2003. Int Arch Occup Environ Health. 2007;80(7):615–626. doi: 10.1007/s00420-007-0173-4. PMID:17468879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Rey G, Fouillet A, Bessemoulin P, et al. Heat exposure and socio-economic vulnerability as synergistic factors in heat-wave-related mortality. Eur J Epidemiol. 2009;24(9):495–502. doi: 10.1007/s10654-009-9374-3. PMID:19642001 [DOI] [PubMed] [Google Scholar]
- [5].Fouillet A, Rey G, Laurent F, et al. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health. 2006;80(1):16–24. doi: 10.1007/s00420-006-0089-4. PMID:16523319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kenny GP, Yardley J, Brown C, et al. Heat stress in older individuals and patients with common chronic diseases. CMAJ. 2010;182(10):1053–1060. doi: 10.1503/cmaj.081050. PMID:19703915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Yardley J, Sigal RJ, Kenny GP. Heat health planning: the importance of social and community factors. Global Environ Chang. 2011;21:670–679. doi: 10.1016/j.gloenvcha.2010.11.010. [DOI] [Google Scholar]
- [8].Ishigami A, Hajat S, Kovats RS, et al. An ecological time-series study of heat-related mortality in three European cities. Environ Health. 2008;7(1):5. doi: 10.1186/1476-069X-7-5. PMID:18226218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Naughton MP, Henderson A, Mirabelli MC, et al. Heat-related mortality during a 1999 heat wave in Chicago. Am J Prev Med. 2002;22(4):221–227. doi: 10.1016/S0749-3797(02)00421-X. PMID:11988377 [DOI] [PubMed] [Google Scholar]
- [10].Kilbourne EM, Choi K, Jones TS, et al. Risk factors for heatstroke. A case-control study. JAMA. 1982;247(24):3332–3336. doi: 10.1001/jama.1982.03320490030031. PMID:7087076 [DOI] [PubMed] [Google Scholar]
- [11].Semenza JC, Rubin CH, Falter KH, et al. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med. 1996;335(2):84–90. doi: 10.1056/NEJM199607113350203. PMID:8649494 [DOI] [PubMed] [Google Scholar]
- [12].Rey G, Jougla E, Fouillet A, et al. Ecological association between a deprivation index and mortality in France over the period 1997 – 2001: variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health. 2009;9:33. doi: 10.1186/1471-2458-9-33. PMID:19161613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Morgan C, Foster JA, Poston A, et al. Overheating in Scotland: contributing factors in occupied homes. Build Res Inf. 2017;45(1-2):143–156. doi: 10.1080/09613218.2017.1241472. [DOI] [Google Scholar]
- [14].McGill G, Sharpe T, Robertson R, et al. Meta-analysis of indoor temperatures in new-build housing. Build Res Inf. 2017;45(1-2):19–39. doi: 10.1080/09613218.2016.1226610. [DOI] [Google Scholar]
- [15].Smargiassi A, Fournier M, Griot C, et al. Prediction of the indoor temperatures of an urban area with an in-time regression mapping approach. J Expo Sci Environ Epidemiol. 2008;18(3):282–288. doi: 10.1038/sj.jes.7500588. [DOI] [PubMed] [Google Scholar]
- [16].White-Newsome JL, Sanchez BN, Jolliet O, et al. Climate change and health: indoor heat exposure in vulnerable populations. Environ Res. 2012;112:20–27. doi: 10.1016/j.envres.2011.10.008. PMID:22071034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Franck U, Kruger M, Schwarz N, et al. Heat stress in urban areas: Indoor and outdoor temperatures in different urban structure types and subjectively reported well-being during a heat wave in the city of Leipzig. Meteorologische Zeitschrift. 2013;22(2):167–177. doi: 10.1127/0941-2948/2013/0384. [DOI] [Google Scholar]
- [18].Smoyer KE, Rainham DG, Hewko JN. Heat-stress-related mortality in five cities in Southern Ontario: 1980–1996. Int J Biometeorol. 2000;44(4):190–197. doi: 10.1007/s004840000070. PMID:11131291 [DOI] [PubMed] [Google Scholar]
- [19].Stone B, Rodgers MO. Urban form and thermal efficiency: How the design of cities influences the urban heat island effect. J Am Plan Assoc. 2001;67(2):186–198. doi: 10.1080/01944360108976228. [DOI] [Google Scholar]
- [20].Medina-Ramon M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatisation and effect modification in 50 US cities. Occup Environ Med. 2007;64(12):827–833. doi: 10.1136/oem.2007.033175. PMID:17600037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Stone B. A review of methods for estimating anthropogenic heat and moisture emissions in the urban environment. Int J Climatol. 2012;31:189–199. [Google Scholar]
- [22].Giridharan R, Lau SSY, Ganesan S, et al. Urban design factors influencing heat island intensity in high-rise high-density environments of Hong Kong. Build Environ. 2007;42(10):3669–3684. doi: 10.1016/j.buildenv.2006.09.011. [DOI] [Google Scholar]
- [23].Centers for Disease Control and Prevention Heat illness and deaths–New\sYork City, 2000–2011. MMWR. Morbidity and Mortality Weekly Report. 2013;62(31):617–621. [PMC free article] [PubMed] [Google Scholar]
- [24].New York City Department of Health and Mental Hygiene Heat waves and heat illness. New York (NY); 2013. [Google Scholar]
- [25].Semenza JC, McCullough JE, Flanders WD, et al. Excess hospital admissions during the July 1995 heat wave in Chicago. Am J Prev Med. 1999;16(4):269–277. doi: 10.1016/S0749-3797(99)00025-2. PMID:10493281 [DOI] [PubMed] [Google Scholar]
- [26].Robine JM, Cheung SL, Le Roy S Van Oyen H, et al. Death toll exceeded 70,000 in Europe during the summer of 2003. Comptes Rendus Biologies. 2008;331(2):171–178. doi: 10.1016/j.crvi.2007.12.001. PMID:18241810 [DOI] [PubMed] [Google Scholar]
- [27].Auliciems A, Skinner JL. Cardiovascular deaths and temperature in subtropical Brisbane. Int J Biometeorol. 1989;33(4):215–221. doi: 10.1007/BF01051080. PMID:2613364 [DOI] [PubMed] [Google Scholar]
- [28].Nicholls N, Skinner C, Loughnan M, et al. A simple heat alert system for Melbourne, Australia. Int J Biometeorol. 2008;52(5):375–384. doi: 10.1007/s00484-007-0132-5. PMID:18058138 [DOI] [PubMed] [Google Scholar]
- [29].Saez S, Sunyer J, Castlesague J, et al. Relationship between weather, temperature and mortality: a time series approach in Barcelona. Int J Epidemiol. 1995;24:576–582. doi: 10.1093/ije/24.3.576. PMID:7672899 [DOI] [PubMed] [Google Scholar]
- [30].Mavrogianni A, Davies M, Wilkinson P, et al. London housing and climate change: impact on comfort and health – preliminary results of a summer overheating study. Open House Int. 2010;35(2):49–59. [Google Scholar]
- [31].van Loenhout JA, le Grand A, Duijm F, et al. The effect of high indoor temperatures on self-perceived health of elderly persons. Environ Res. 2016;146:27–34. doi: 10.1016/j.envres.2015.12.012. PMID:26710340 [DOI] [PubMed] [Google Scholar]
- [32].Sakka A, Santamouris M, Livada I, et al. On the thermal performance of low income housing during heat waves. Energy Build. 2012;(49):69–77. doi: 10.1016/j.enbuild.2012.01.023. [DOI] [Google Scholar]
- [33].Wright AJ, Young A, Natarajan S. Dwelling temperatures and comfort during the August 2003 heat wave. Build Serv Eng Res Technol. 2005;26(4):285–300. doi: 10.1191/0143624405bt136oa. [DOI] [Google Scholar]
- [34].Lindemann U, Stotz A, Beyer N, et al. Effect of indoor temperature on physical performance in older adults during days with normal temperature and heat waves. Int J Environ Res Public Health. 2017;14(2):186–195. doi: 10.3390/ijerph14020186. PMID:28216585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Tham KW, Willem HC. Room air temperature affects occupants' physiology, perceptions and mental alertness. Build Environ. 2010;45:40–44. doi: 10.1016/j.buildenv.2009.04.002. [DOI] [Google Scholar]
- [36].Environmental Design. 7th ed. London: Chartered Institution of Building Services Engineers; 2006. ISBN 978190387668. © 2017 The Author(s). Published by Elsevier Ltd. [Google Scholar]
- [37].van Hoof J, Kort HSM, Hensen JLM, et al. Thermal comfort and the integrated design of homes for older people with dementia. Build Environ. 2010;2(45):358–370. doi: 10.1016/j.buildenv.2009.06.013. [DOI] [Google Scholar]
- [38].van Hoof J, Schellen L, Soebarto V, et al. Ten questions concerning thermal comfort and ageing. Build Environ. 2017;120:123–133. doi: 10.1016/j.buildenv.2017.05.008. [DOI] [Google Scholar]
- [39].Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiologic reviews. 2002;24(2):190–202. doi: 10.1093/epirev/mxf007. PMID:12762092 [DOI] [PubMed] [Google Scholar]
- [40].Michelozzi P, Accetta G, De Sario M D'Ippoliti D, et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. American journal of respiratory and critical care medicine. 2009;179(5):383–389. doi: 10.1164/rccm.200802-217OC. PMID:19060232 [DOI] [PubMed] [Google Scholar]
- [41].Nguyen JL, Schwartz J, Dockery DW. The relationship between indoor and outdoor temperature, apparent temperature, relative humidity, and absolute humidity. Indoor air. 2014;24(1):103–112. doi: 10.1111/ina.12052. PMID:23710826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Basu R, Samet JM. An exposure assessment study of ambient heat exposure in an elderly population in Baltimore, Maryland. Environmental health perspectives. 2002;110(12):1219–1224. doi: 10.1289/ehp.021101219. PMID:12460801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Lowe D, Ebi KL, Forsberg B. Heatwave early warning systems and adaptation advice to reduce human health consequences of heatwaves. Int J Environ Res Public Health. 2011;8(12):4623–4648. doi: 10.3390/ijerph8124623. PMID:22408593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Toloo G, FitzGerald G, Aitken P, et al. Evaluating the effectiveness of heat warning systems: systematic review of epidemiological evidence. Int J Environ Res Public Health. 2013;58(5):667–681. doi: 10.1007/s00038-013-0465-2. [DOI] [PubMed] [Google Scholar]
- [45].Toloo GS, Fitzgerald G, Aitken P, et al. Are heat warning systems effective? Environmental Health. 2013;12:27. doi: 10.1186/1476-069X-12-27. PMID:23561265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Bernard SM, McGeehin MA. Municipal heat wave response plans. American journal of public health. 2004;94(9):1520–1522. doi: 10.2105/AJPH.94.9.1520. PMID:15333307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Kovats RS, Hajat S. Heat stress and public health: a critical review. Annu Rev Public Health. 2008;29:41–55. doi: 10.1146/annurev.publhealth.29.020907.090843. PMID:18031221 [DOI] [PubMed] [Google Scholar]
- [48].Smoyer-Tomic KE, Kuhn R, Hudson A. Heat wave hazards: an overview of heat wave impacts in Canada. Nat Hazard. 2003;28(2):465–486. doi: 10.1023/A:1022946528157. [DOI] [Google Scholar]
- [49].Pascal M, Laaidi K, Ledrans M, et al. France's heat health watch warning system. Int J Biometeorol. 2006;50(3):144–153. doi: 10.1007/s00484-005-0003-x. PMID:16328399 [DOI] [PubMed] [Google Scholar]
- [50].Klepeis NE, Nelson WC, Ott WR, et al. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Expo Anal Environ Epidemiol. 2001;11(3):231–252. doi: 10.1038/sj.jea.7500165. PMID:11477521 [DOI] [PubMed] [Google Scholar]
- [51].Leech JA, Nelson WC, Burnett RT, et al. “It's about time: A Comparison of Canadian and American time – Activity Patterns. J Expo Anal Environ Epidemiol. 2002;12:427–432. doi: 10.1038/sj.jea.7500244. PMID:12415491 [DOI] [PubMed] [Google Scholar]
- [52].Luber G, McGeehin M. Climate change and extreme heat events. Am J Prev Med. 2008;35(5):429–435. doi: 10.1016/j.amepre.2008.08.021. PMID:18929969 [DOI] [PubMed] [Google Scholar]
- [53].Borden KA, Cutter SL. Spatial patterns of natural hazards mortality in the United States. International Journal of Health Geographics. 2008;7:64. doi: 10.1186/1476-072X-7-64. PMID:19091058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Government of Canada Canada in a changing climate: Sector perspective on impacts and adaptation. Ottawa: National Resources Canada; 2014. [Google Scholar]
- [55].Gomes LH, Carneiro-Junior MA, Marins JC. Thermoregulatory responses of children exercising in a hot environment. Rev Paul Pediatr. 2013;31(1):104–110. doi: 10.1590/S0103-05822013000100017. PMID:23703052 [DOI] [PubMed] [Google Scholar]
- [56].Bytomski JR, Squire DL. Heat illness in children. Curr Sports Med Rep. 2003;2(6):320–324. doi: 10.1249/00149619-200312000-00007. PMID:14583161 [DOI] [PubMed] [Google Scholar]
- [57].Tsuzuki-Hayakawa K, Tochihara Y, Ohnaka T. Thermoregulation during heat exposure of young children compared to their mothers. Eur J Appl Physiol Occup Physiol. 1995;72(1-2):12–17. doi: 10.1007/BF00964108. PMID:8789564 [DOI] [PubMed] [Google Scholar]
- [58].Yardley JE, Stapleton JM, Sigal RJ, et al. Do heat events pose a greater health risk for individuals with type 2 diabetes? Diabetes Technol Ther. 2013;15(6):520–529. doi: 10.1089/dia.2012.0324. PMID:23530578 [DOI] [PubMed] [Google Scholar]
- [59].Bar-Or O, Lundegren HM, Buskirk ER. Heat tolerance of exercising obese and lean women. J Appl Physiol. 1969;26(4):403–409. doi: 10.1152/jappl.1969.26.4.403. PMID:5775324 [DOI] [PubMed] [Google Scholar]
- [60].Havenith G, Coenen JM, Kistemaker L, et al. Relevance of individual characteristics for human heat stress response is dependent on exercise intensity and climate type. Eur J Appl Physiol Occup Physiol. 1998;77(3):231–241. doi: 10.1007/s004210050327. PMID:9535584 [DOI] [PubMed] [Google Scholar]
- [61].Koppe C, Kovats S, Jendritzky G, et al. The impact of heat on human health (Chapter 3). In: David J Breuer, editor. Health and global environmental changes, Series 2. World Health Organization; 2004. P. 17–34. [Google Scholar]
- [62].Vandentorren S, Bretin P, Zeghnoun A, et al. August 2003 heat wave in France: risk factors for death of elderly people living at home. Eur J Public Health. 2006;16(6):583–591. doi: 10.1093/eurpub/ckl063. PMID:17028103 [DOI] [PubMed] [Google Scholar]
- [63].Semenza JC, Rubin CH, Falter KH, et al. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med. 1996;335(2):84–90. doi: 10.1056/NEJM199607113350203. PMID:8649494 [DOI] [PubMed] [Google Scholar]
- [64].Hoffmann B, Hertel S, Boes T, et al. Incrased cause-specific mortality associated with 2003 heatwave in Essen, Germany. J Toxicol Environ Health A. 2008;71:759–765. doi: 10.1080/15287390801985539. PMID:18569574 [DOI] [PubMed] [Google Scholar]
- [65].Larose J, Wright HE, Sigal RJ, et al. Do older females store more heat than younger females during exercise in the heat? Med Sci Sports Exerc. 2013;45(12):2265–2276. doi: 10.1249/MSS.0b013e31829d24cc. PMID:23715429 [DOI] [PubMed] [Google Scholar]
- [66].Larose J, Wright HE, Stapleton J, et al. Whole-body heat loss is reduced in older males during short bouts of intermittent exercise. Am J Physiol. 2013;305(6):R619–629. doi: 10.1152/ajpregu.00157.2013. [DOI] [PubMed] [Google Scholar]
- [67].Stapleton JM, Poirier MP, Flouris AD, et al. Aging impairs heat loss, but when does it matter? J Appl Physiol (1985). 2015;118(3):299–309. doi: 10.1152/japplphysiol.00722.2014. PMID:25505030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Stapleton JM, Poirier MP, Flouris AD, et al. At what level of heat load are age-related impairments in the ability to dissipate heat evident in females? PLoS One. 2015;10(3):e0119079. doi: 10.1371/journal.pone.0119079. PMID:25790024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Kenny GP, Flouris AD, Dervis S, et al. Older adults experience greater levels of thermal and cardiovascular strain during extreme heat exposures. Med Sci Sports Exerc. 2015;46(5):S396. [Google Scholar]
- [70].Kenny GP, Sigal RJ, McGinn R. Body temperature regulation in diabetes. Temperature. 2016;3(1):119–145. doi: 10.1080/23328940.2015.1131506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Kenny GP, Stapleton JM, Yardley JE, et al. Older adults with type 2 diabetes store more heat during exercise. Med Sci Sports Exerc. 2013;45(10):1906–1914. doi: 10.1249/MSS.0b013e3182940836. PMID:23542894 [DOI] [PubMed] [Google Scholar]
- [72].Kenny GP, Poirier MP, Metsios GS, et al. Hyperthermia and cardiovascular strain during an extreme heat exposure in young versus older adults. Temperature. 2016;4(1):79–88. doi: 10.1080/23328940.2016.1230171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Yu W, Mengersen K, Wang X, et al. Daily average temperature and mortality among the elderly: a meta-analysis and systematic review of epidemiological evidence. Int J Biometeorol. 2012;56(4):569–581. doi: 10.1007/s00484-011-0497-3. PMID:21975970 [DOI] [PubMed] [Google Scholar]
- [74].Bustinza R, Lebel G, Gosselin P, et al. Health impacts of the July 2010 heat wave in Quebec, Canada. BMC public health. 2013;13:56. doi: 10.1186/1471-2458-13-56. PMID:23336593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Braga AL, Zanobetti A, Schwartz J. The time course of weather-related deaths. Epidemiology. 2001;12(6):662–667. doi: 10.1097/00001648-200111000-00014. PMID:11679794 [DOI] [PubMed] [Google Scholar]
- [76].Stafoggia M, Forastiere F, Agostini D, et al. Vulnerability to heat-related mortality: a multicity, population-based, case-crossover analysis. Epidemiology. 2006;17(3):315–323. .doi: 10.1097/01.ede.0000208477.36665.34. PMID:16570026 [DOI] [PubMed] [Google Scholar]
- [77].Gasparrini A, Armstrong B. The impact of heat waves on mortality. Epidemiology. 2011;22(1):68–73. doi: 10.1097/EDE.0b013e3181fdcd99. PMID:21150355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Barriopedro D, Fischer EM, Luterbacher J, et al. The hot summer of 2010: redrawing the temperature record map of Europe. Science. 2011;332(6026):220–224. doi: 10.1126/science.1201224. PMID:21415316 [DOI] [PubMed] [Google Scholar]
- [79].Natural Resources Defense Council Health and climate change: accounting for costs. New York City, NY: Natural Resources Defense Council; 2011. [Google Scholar]
- [80].Knowlton K, Rotkin-Ellman M, Geballe L, et al. Six climate change-related events in the United States accounted for about $14 billion in lost lives and health costs. Health Aff (Millwood). 2011;30(11):2167–2176. doi: 10.1377/hlthaff.2011.0229. PMID:22068410 [DOI] [PubMed] [Google Scholar]
- [81].Larrivée C, Sinclair-Desgagné N, Da Silva L, et al. Évaluation des impacts des changements climatiques et de leurs coûts pour le Québec et l’État québécois. Québec: Ouranos; 2015. [Google Scholar]
- [82].Jackson T, Clemens J, Palacios M. Canada's aging population and implications for government finances. Vancouver, British Columbia: Frasier Institute; 2017. [Google Scholar]
- [83].Canada goes urban Statistics Canada; 2015.. [assesed http://www.statcan.gc.ca/pub/11-630-x/11-630-x2015004-eng.htm. [Google Scholar]
- [84].Census in Brief Municipalities in Canada with the largest and fastest-growing populations between 2011 and 2016. Statistics Canada; 2016.. [assesed http://www12.statcan.gc.ca/census-recensement/2016/as-sa/98-200-x/2016001/98-200-x2016001-eng.cfm. [Google Scholar]
- [85].Chen H, Wang J, Li Q, et al. Assessment of the effect of cold and hot temperatures on mortality in Ontario, Canada: a population-based study. CMAJ open. 2016;4(1):E48–58. doi: 10.9778/cmajo.20150111. PMID:27280114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Kosatsky T. Hot day deaths, summer 2009. BCMJ. 2010;52:261. [Google Scholar]
- [87].Hajat S, Vardoulakis S, Heaviside C, et al. Climate change effects on human health: projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. J Epidemiol Community Health. 2014;68(7):641–648. doi: 10.1136/jech-2013-202449. PMID:24493740 [DOI] [PubMed] [Google Scholar]
- [88].Health professionals: be prepared for heatwaves. Lancet. 2015;386(9990):219. doi: 10.1016/S0140-6736(15)61261-2. PMID:26194505 [DOI] [PubMed] [Google Scholar]
- [89].World Health Organisation – Europe Heat-health action plans: guidance. Copenhagen, Denmark: World Health Organisation; 2008. [Google Scholar]
- [90].Fouillet A, Rey G, Wagner V, et al. De Crouy-Chanel P, et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int J Epidemiol. 2008;37(2):309–317. doi: 10.1093/ije/dym253. PMID:18194962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Boyson C, Taylor S, Page L. The national heatwave plan – a brief evaluation of issues for frontline health staff. PLoS Curr. 2014;6. doi: 10.1371/currents.dis.aa63b5ff4cdaf47f1dc6bf44921afe93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Benmarhnia T, Deguen S, Kaufman JS, et al. Review article: Vulnerability to heat-related mortality: a systematic review, meta-analysis, and meta-regression analysis. Epidemiology. 2015;26(6):781–793. doi: 10.1097/EDE.0000000000000375. PMID:26332052 [DOI] [PubMed] [Google Scholar]
- [93].Sherwood SC, Huber M. An adaptability limit to climate change due to heat stress. Proc Natl Acad Sci USA. 2010;107(21):9552–9555. doi: 10.1073/pnas.0913352107. PMID:20439769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Population and dwelling count highlight tables, 2016 Census Statistics Canada; 2017. [assesed http://www12.statcan.gc.ca/census-recensement/2016/dp-pd/hlt-fst/pd-pl/Table.cfm?Lang = Eng&T = 205&S = 3&RPP = 100.
- [95].Oleson KW, Monaghan A, Wilhelmi O, et al. Interactions between urbanization, heat stress, and climate change. Climate Change. 2015;129:525–541. doi: 10.1007/s10584-013-0936-8. [DOI] [Google Scholar]
- [96].Jones GS, Stott PA, Christidis N. Human contribution to rapidly increasing frequency of very warm northern hemisphere summers. J Geophys Res. 2008;113:D02109. doi: 10.1029/2007JD008914. [DOI] [Google Scholar]
- [97].Meehl GA, Tebaldi C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science. 2004;305(5686):994–997. doi: 10.1126/science.1098704. PMID:15310900 [DOI] [PubMed] [Google Scholar]
- [98].Gabriel KM, Endlicher WR. Urban and rural mortality rates during heat waves in Berlin and Brandenburg, Germany. Environ Pollut. 2011;159(8-9):2044–2050. doi: 10.1016/j.envpol.2011.01.016. PMID:21295389 [DOI] [PubMed] [Google Scholar]
- [99].Hondula DM, Davis RE, Leisten MJ, et al. Fine-scale spatial variability of heat-related mortality in Philadelphia County, USA, from 1983–2008: a case-series analysis. Environ Health. 2012;11:16. doi: 10.1186/1476-069X-11-16. PMID:22443423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Laaidi K, Zeghnoun A, Dousset B, et al. The impact of heat islands on mortality in Paris during the August 2003 heat wave. Environ Health Perspect. 2012;120(2):254–259. doi: 10.1289/ehp.1103532. PMID:21885383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Smargiassi A, Goldberg MS, Plante C, et al. Variation of daily warm season mortality as a function of micro-urban heat islands. J Epidemiol Community Health. 2009;63(8):659–664. doi: 10.1136/jech.2008.078147. PMID:19366997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].McMichael AJ, Wilkinson P, Kovats RS, et al. International study of temperature, heat and urban mortality: the 'ISOTHURM' project. Int J Epidemiol. 2008;37(5):1121–1131. doi: 10.1093/ije/dyn086. PMID:18522981 [DOI] [PubMed] [Google Scholar]
- [103].Kolokotroni M, Giannitsaris I, Watkins R. The effect of the London urban heat island on building summer cooling demand and night ventilation strategies. Solar Energy. 2006;80(4):383–392. doi: 10.1016/j.solener.2005.03.010. [DOI] [Google Scholar]
- [104].Reid CE, O'Neill MS, Gronlund CJ, et al. Mapping community determinants of heat vulnerability. Environ Health Perspect. 2009;117(11):1730–1736. doi: 10.1289/ehp.0900683. PMID:20049125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Aniello C. Mapping micro-urban heat islands using landsat TM and a GIS. Comput Geosci. 1995;21:965–969. doi: 10.1016/0098-3004(95)00033-5. [DOI] [Google Scholar]
- [106].Lo CP. Application of high-resolution thermal infrared remote sensing and GIS to assess the urban heat island effect. Int J Remote Sens. 1997;18:287–304. doi: 10.1080/014311697219079. [DOI] [Google Scholar]
- [107].Vogt JA, Oke TR. Thermal remote sensing of urban climates. Remote Sens Environ. 2003;86:370–384. doi: 10.1016/S0034-4257(03)00079-8. [DOI] [Google Scholar]
- [108].Rogot E, Sorlie PD, Backlund E. Air-conditioning and mortality in hot weather. Am J Epidemiol. 1992;136(1):106–116. doi: 10.1093/oxfordjournals.aje.a116413. PMID:1415127 [DOI] [PubMed] [Google Scholar]
- [109].Conti S, Meli P, Minelli G, et al. Epidemiologic study of mortality during the Summer 2003 heat wave in Italy. Environmental Res. 2005;98(3):390–399. doi: 10.1016/j.envres.2004.10.009. [DOI] [PubMed] [Google Scholar]
- [110].Martinez BF, Annest JL, Kilbourne EM, et al. Geographic distribution of heat-related deaths among elderly persons. Use of county-level dot maps for injury surveillance and epidemiologic research. JAMA. 1989;262(16):2246–2250. doi: 10.1001/jama.1989.03430160068032. PMID:2795805 [DOI] [PubMed] [Google Scholar]
- [111].Clarke JF. Some effects of the urban structure on heat mortality. Environmental Res. 1972;5(1):93–104. doi: 10.1016/0013-9351(72)90023-0. [DOI] [PubMed] [Google Scholar]
- [112].Fouillet A, Rey G, Jougla E, et al. A predictive model relating daily fluctuations in summer temperatures and mortality rates. BMC public health. 2007;7:114. doi: 10.1186/1471-2458-7-114. PMID:17578564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Harlan SL, Brazel AJ, Prashad L, et al. Neighborhood microclimates and vulnerability to heat stress. Soc Sci Med. 2006;63:2847-2863. PMID:16996668 [DOI] [PubMed] [Google Scholar]
- [114].Smoyer KE. Putting risk in its place: methodological considerations for investigating extreme event health risk. Soc Sci Med. 1998;47:1809–1824. doi: 10.1016/S0277-9536(98)00237-8. PMID:9877350 [DOI] [PubMed] [Google Scholar]
- [115].Curriero FC, Heiner KS, Samet JM, et al. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155(1):80–87. doi: 10.1093/aje/155.1.80. PMID:11772788 [DOI] [PubMed] [Google Scholar]
- [116].D'Ippoliti D, Michelozzi P, Marino C, et al. The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Environ Health. 2010;9:37. doi: 10.1186/1476-069X-9-37. PMID:20637065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [117].Son JY, Lee JT, Anderson GB, et al. The impact of heat waves on mortality in seven major cities in Korea. Environmental health perspectives. 2012;120(4):566–571. doi: 10.1289/ehp.1103759. PMID:22266672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118].Tong S, Wang XY, Barnett AG. Assessment of heat-related health impacts in Brisbane, Australia: comparison of different heatwave definitions. PLoS One. 2010;5(8):e12155. doi: 10.1371/journal.pone.0012155. PMID:20730050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Ye X, Wolff R, Yu W, et al. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. 2012;120(1):19–28. doi: 10.1289/ehp.1003198. PMID:21824855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Baccini M, Biggeri A, Accetta G, et al. Heat effects on mortality in 15 European cities. Epidemiology. 2008;19(5):711–719. doi: 10.1097/EDE.0b013e318176bfcd. PMID:18520615 [DOI] [PubMed] [Google Scholar]
- [121].Zanobetti A, Schwartz J. Temperature and mortality in nine US cities. Epidemiology. 2008;19(4):563–570. doi: 10.1097/EDE.0b013e31816d652d. PMID:18467963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122]. Health Canada, Extreme Heat Events Guidelines: Technical Guide for Health Care Workers. Ottawa, Ontario. p. 149. ISBN: 978-1-100-18172-1. [Google Scholar]
- [123].Hajat S, Kovats RS, Lachowycz K. Heat-related and cold-related deaths in England and Wales: who is at risk? Occup Environ Med. 2007;64(2):93–100. doi: 10.1136/oem.2006.029017. PMID:16990293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124].Bhaskaran K, Hajat S, Haines A, et al. Effects of ambient temperature on the incidence of myocardial infarction. Heart. 2009;95(21):1760–1769. doi: 10.1136/hrt.2009.175000. PMID:19635724 [DOI] [PubMed] [Google Scholar]
- [125].Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20(2):205–213. doi: 10.1097/EDE.0b013e318190ee08. PMID:19194300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [126].Chestnut LG, Breffle WS, Smith JB, et al. Analysis of diferences in hot-weather-related mortality across 44 U.S. metropolitan areas. Environ Sci Policy. 1998;1:59–70. doi: 10.1016/S1462-9011(98)00015-X. [DOI] [Google Scholar]
- [127].Keatinge WR, Donaldson GC, Cordioli E, et al. Heat related mortality in warm and cold regions of Europe: observational study. BMJ. 2000;321(7262):670–673. doi: 10.1136/bmj.321.7262.670. PMID:10987770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [128].Kenny GP, Jay O. Thermometry, calorimetry, and mean body temperature during heat stress. Compr Physiol. 2013;3:1–31. PMID:23720280 [DOI] [PubMed] [Google Scholar]
- [129].Stapleton JM, Larose J, Simpson C, et al. Do older adults experience greater thermal strain during heat waves? Appl Physiol Nutr Metab. 2014;39(3):292–298. doi: 10.1139/apnm-2013-0317. PMID:24552369 [DOI] [PubMed] [Google Scholar]
- [130].Hajat S, Kovats RS, Atkinson RW, et al. Impact of hot temperatures on death in London: a time series approach. J Epidemiol Community Health. 2002;56(5):367–372. doi: 10.1136/jech.56.5.367. PMID:11964434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [131].Vaneckova P, Hart MA, Beggs PJ, et al. Synoptic analysis of heat-related mortality in Sydney, Australia, 1993–2001. Int J Biometeorol. 2008;52(6):439–451. doi: 10.1007/s00484-007-0138-z. PMID:18210167 [DOI] [PubMed] [Google Scholar]
- [132].Harlan SL, Chowell G, Yang S, et al. Heat-related deaths in hot cities: estimates of human tolerance to high temperature thresholds. Int J Environ Res Public Health. 2014;11(3):3304–3326. doi: 10.3390/ijerph110303304. PMID:24658410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [133].Kalkstein LS, Greene JS. An evaluation of climate/mortality relationships in large U.S. cities and the possible impacts of a climate change. Environ Health Perspect. 1997;105(1):84–93. doi: 10.1289/ehp.9710584. PMID:9074886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [134].Loughnan M, Nicholls N, Tapper N. Mortality-temperature thresholds for ten major population centres in rural Victoria, Australia. Health & Place. 2010;16(6):1287–1290. doi: 10.1016/j.healthplace.2010.08.008. [DOI] [PubMed] [Google Scholar]
- [135].Michelozzi P, de' Donato FK, Bargagli AM, et al. Surveillance of summer mortality and preparedness to reduce the health impact of heat waves in Italy. Int J Environ Res Public Health. 2010;7(5):2256–2273. doi: 10.3390/ijerph7052256. PMID:20623023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Armstrong BG, Chalabi Z, Fenn B, et al. Association of mortality with high temperatures in a temperate climate: England and Wales. J Epidemiol Community Health. 2011;65(4):340–345. doi: 10.1136/jech.2009.093161. PMID:20439353 [DOI] [PubMed] [Google Scholar]
- [137].Henderson SB, Victoria W, Kosatsky T. Differences in heat-related mortality across four ecological regions with diverse urban, rural and remote populations in British Columbia, Canada. Health & Place. 2013;23:48–53. doi: 10.1016/j.healthplace.2013.04.005. [DOI] [PubMed] [Google Scholar]
- [138].Sheridan SC, Kalkstein LS. Heat watch-warning systems in urban areas. World Resource Reviews. 1988;10:375–383. [Google Scholar]
- [139].Loughnan ME, Nicholls N, Tapper NJ. When the heat is on: Threshold temperatures for AMI admissions to hospital in Melbourne Australia. Applied Geography. 2010;30:63–69. doi: 10.1016/j.apgeog.2009.08.003. [DOI] [Google Scholar]
- [140].Knowlton K, Rotkin-Ellman M, King G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117(1):61–67. doi: 10.1289/ehp.11594. PMID:19165388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Williams S, Nitschke M, Sullivan T, et al. Heat and health in Adelaide, South Australia: assessment of heat thresholds and temperature relationships. Sci Total Environ. 2012;414:126–133. doi: 10.1016/j.scitotenv.2011.11.038. PMID:22169392 [DOI] [PubMed] [Google Scholar]
- [142].Bell ML, O'Neill MS, Ranjit N, et al. Vulnerability to heat-related mortality in Latin America: a case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol. 2008;37(4):796–804. doi: 10.1093/ije/dyn094. PMID:18511489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143].Egondi T, Kyobutungi C, Kovats S, et al. Time-series analysis of weather and mortality patterns in Nairobi's informal settlements. Global Health Action. 2012;5(1):19065. doi: 10.3402/gha.v5i0.19065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Yu W, Vaneckova P, Mengersen K, et al. Is the association between temperature and mortality modified by age, gender and socio-economic status? Sci Total Environ. 2010;408(17):3513–3518. doi: 10.1016/j.scitotenv.2010.04.058. PMID:20569969 [DOI] [PubMed] [Google Scholar]
- [145].Poirier M, Dervis S, Flouris AD, et al. Whole-body heat loss is enhanced in older adults following a summer in a humid continental climate. FASEB J. 2016;30:1290.1213. [Google Scholar]
- [146].Taylor NA. Human heat adaptation. Compr Physiol. 2014;4(1):325–365. doi: 10.1002/cphy.c130022. PMID:24692142 [DOI] [PubMed] [Google Scholar]
- [147].Weisskopf MG, Anderson HA, Foldy S, et al. Heat wave morbidity and mortality, Milwaukee, Wis, 1999 vs 1995: an improved response? Am J Public Health. 2002;92(5):830–833. doi: 10.2105/AJPH.92.5.830. PMID:11988455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [148].Rhomberg LR, Chandalia JK, Long CM, et al. Measurement error in environmental epidemiology and the shape of exposure-response curves. Crit Rev Toxicol. 2011;41(8):651–671. doi: 10.3109/10408444.2011.563420. PMID:21823979 [DOI] [PubMed] [Google Scholar]
- [149].Epstein Y, Moran DS. Thermal comfort and the heat stress indices. Ind Health. 2006;44(3):388–398. doi: 10.2486/indhealth.44.388. PMID:16922182 [DOI] [PubMed] [Google Scholar]
- [150].Analitis A, Katsouyanni K, Biggeri A, et al. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol. 2008;168(12):1397–1408. doi: 10.1093/aje/kwn266. PMID:18952849 [DOI] [PubMed] [Google Scholar]
- [151].Steadman RG. The assessment of sultriness. Part I: A temperature-humidity index based on human physiology and clothing science. J Appl Meteorol. 1979;18:861–873. doi:. [DOI] [Google Scholar]
- [152].Barnett AG, Astrom C. Commentary: What measure of temperature is the best predictor of mortality? Environmental Res. 2012;118:149–151. doi: 10.1016/j.envres.2012.05.008. [DOI] [PubMed] [Google Scholar]
- [153].Metzger KB, Ito K, Matte TD. Summer heat and mortality in New York City: how hot is too hot? Environ Health Perspect. 2010;118(1):80–86. doi: 10.1289/ehp.0900906. PMID:20056571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [154].Hajat S, Armstrong B, Baccini M, et al. Impact of high temperatures on mortality: is there an added heat wave effect? Epidemiology. 2006;17(6):632–638. doi: 10.1097/01.ede.0000239688.70829.63. PMID:17003686 [DOI] [PubMed] [Google Scholar]
- [155].Barnett AG, Tong S, Clements AC. What measure of temperature is the best predictor of mortality? Environmental Res. 2010;110(6):604–611. doi: 10.1016/j.envres.2010.05.006. [DOI] [PubMed] [Google Scholar]
- [156].Guo Y. Hourly associations between heat and ambulance calls. Environ Pollut. 2017;220(Pt B):1424–1428. doi: 10.1016/j.envpol.2016.10.091. PMID:27825842 [DOI] [PubMed] [Google Scholar]
- [157].Bhaskaran K, Hajat S, Armstrong B, et al. The effects of hourly differences in air pollution on the risk of myocardial infarction: case crossover analysis of the MINAP database. BMJ. 2011;343:d5531. doi: 10.1136/bmj.d5531. PMID:21933824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].de Dear R Brager GS. The adaptive model of thermal comfort and energy conservation in the built environment. Int J Biometeorol. 2001;45(2):100–108. doi: 10.1007/s004840100093. PMID:11513046 [DOI] [PubMed] [Google Scholar]
- [159].Zero Carbon Hub Overheating in homes, The big picture, Full report. London; 2015. http://www.zerocarbonhub.org/sites/default/files/resources/reports/ZCH-OverheatingInHomes-TheBigPicture-01.1.pdf [Google Scholar]
- [160].Passivhaus Institut The passive house planning package (PHPP). Victoria, British Columbia; 2012. [Google Scholar]
- [161].Chartered Institution of Building Services Engineers, CIBSE Guide A: Environmental Design. CIBSE; 2015. p. 402. ISBN: 9781906846541 . [Google Scholar]
- [162].Government of the United Kingdom Heating and ventilation of health sector buildings (HTM 03-01). Department of Health; 2007. [Google Scholar]
- [163].Chartered Institution of Building Services Engineers Guide A, environmental design. 7th ed London: The Stationery Office (TSO); 2006. [Google Scholar]
- [164].Baborska-Narozny M, Stevenson F, Chatterton P. Temperture in housing: Stratification and contextual factors. Engineering Sustainability. 2015;9:1–17. [Google Scholar]
- [165].Ji Y, Fitton R, Swan W, et al. Assessing overheating of the UK existing dwellings – A case study of replica Victorian end terrace house. Build Environ. 2014;7:1–11. doi: 10.1016/j.buildenv.2014.03.012. [DOI] [Google Scholar]
- [166].Tillson AA, Oreszczyn T, Palmer J. Assessing impacts of summertime overheating: some adaptation strategies. Build Res Inf. 2013;41(6):652–661. doi: 10.1080/09613218.2013.808864. [DOI] [Google Scholar]
- [167].Gul MS, Jenkins D, Patidar S, et al. Communicating future overheating risks to building design practitioners: Using the low carbon futures tool. Build Serv Eng Res Technol. 2015;36(2):182–195. doi: 10.1177/0143624414566475. [DOI] [Google Scholar]
- [168].Taylor J, Davies M, Mavrogianni A, et al. Mapping indoor overheating and air pollution risk modification across Great Britain: A modelling study. Build Environ. 2016;99:1–12. doi: 10.1016/j.buildenv.2016.01.010. [DOI] [Google Scholar]
- [169].Oikonomou E, Davies M, Mavrogianni A, et al. Modelling the relative importance of the urban heat island and the thermal quality of dwellings for overheating in London. Build Environ. 2012;57:223–238. doi: 10.1016/j.buildenv.2012.04.002. [DOI] [Google Scholar]
- [170].Symonds P, Taylor J, Mavrogianni A, et al. Overheating in English dwellings: comparison modelled and monitored large-scale. Build Res Inf. 2017;45(1-2):195–208. doi: 10.1080/09613218.2016.1224675. [DOI] [Google Scholar]
- [171].Mirzaei PA, Haghighat F, Nakhaie AA, et al. Indoor thermal condition in urban heat island – Development of a predictive tool. Build Environ. 2012;57:7–17. doi: 10.1016/j.buildenv.2012.03.018. [DOI] [Google Scholar]
- [172].Vellei M, Ramallo-Gonzalez AP, Coley D, et al. Overheating in vulnerable and non-vulnerable households. Build Res Inf. 2017;45(1-2):102–118. doi: 10.1080/09613218.2016.1222190. [DOI] [Google Scholar]
- [173].Dufour A, Candas V. Ageing and thermal responses during passive heat exposure: sweating and sensory aspects. Eur J Appl Physiol. 2007;100(1):19–26. doi: 10.1007/s00421-007-0396-9. PMID:17242944 [DOI] [PubMed] [Google Scholar]
- [174].Wright AJ, Young AN, Natarajan S. Dwelling temperatures and comfort during the 2003 heat wave. Build Serv Eng. 2005;26:285–300. doi: 10.1191/0143624405bt136oa. [DOI] [Google Scholar]
- [175].Dengel A, Swainson M. Overheating in new homes: a review of the evidence. London: HS BRE Press on behalf of NHBC Foundation, London; 2012. [Google Scholar]
- [176].Barbosa R, Vicente R, Santos R. Climate change and thermal comfort in Southern Europe housing: a case study from Lisbon. Build Environ. 2015;92:440–451. doi: 10.1016/j.buildenv.2015.05.019. [DOI] [Google Scholar]
- [177].Shrubsole C, MacMillan A, Davies M, et al. 100 Unintended consequences of policies to improve the energy efficiency of the UK housing stock Indoor and Built Environment. 2014;23(3):340–352. doi: 10.1177/1420326X14524586. [DOI] [Google Scholar]
- [178].Mavrogianni A, Pathan A, Oikonomou E, et al. Inhabitant actions and summer overheating risk in London dwellings. Build Res Inf. 2017;45(1-2):119–142. doi: 10.1080/09613218.2016.1208431. [DOI] [Google Scholar]
- [179].McLoed RS, Hopfe CJ, Kwan A. An investigation into future performance and overheating risks in Passivhaus dwellings. Build Environ. 2013;70:189-209. [Google Scholar]
- [180].Beizaee A, Lomas KJ, Firth SK. National survey of summertime temperatures and overheating risk in English homes. Build Environ. 2013;65:1–17. doi: 10.1016/j.buildenv.2013.03.011. [DOI] [Google Scholar]
- [181].American Society of Heating, Refrigeration and Air-Conditioning Engineers NSI/ASHRA Standard 55–2004: Thermal environmental conditions for human occupancy. Atlanta, GA; 2004. Available from: http://www.ashrae.org [Google Scholar]
- [182].Fanger PO. Thermal comfort: Analysis and applications in environmental engineering. Copenhagen: Danish Technical Press; 1970. [Google Scholar]
- [183].American Society of Heating, Refrigeration and Air-Conditioning Engineers ANSI/ASHRAE. Standard 55–2010 – thermal environmental conditions for human occupancy. Atlanta, GA; 2010. Available from: http://www.ashrae.org [Google Scholar]
- [184].International Standards Organisation ISO 7730 – Moderate Thermal Environments – Determination of the PMV and PPD indicies and specification of the conditions for thermal comfort. Geneva: ISO Copyright Office; 1994. [Google Scholar]
- [185].van Hoof J. Forty years of Fanger's model of thermal comfort: comfort for all? Indoor air. 2008;18(3):182–201. doi: 10.1111/j.1600-0668.2007.00516.x. PMID:18363685 [DOI] [PubMed] [Google Scholar]
- [186].de Dear RJ Akimoto T, Arens EA, Brager G, et al. Progress in thermal comfort research over the last twenty years. Indoor Air. 2013;23(6):442–461. doi: 10.1111/ina.12046. doi: 10.1111/ina.12046. PMID:23590514 [DOI] [PubMed] [Google Scholar]
- [187].de Dear R, Brager GS. Developing an adaptive model of thermal comfort and preference. ASHRAE Transactions. 1998;104(1):145–167. [Google Scholar]
- [188].Dujic Z, Ivancev V, Valic Z, et al. Postexercise hypotension in moderately trained athletes after maximal exercise. Med Sci Sports Exerc. 2006;38(2):318–322. doi: 10.1249/01.mss.0000187460.73235.3b. PMID:16531901 [DOI] [PubMed] [Google Scholar]
- [189].Kenny GP, Groeller H, McGinn R, et al. Age, human performance, and physical employment standards. Appl Physiol Nutr Metab. 2016;41(6 Suppl 2):S92–S107. doi: 10.1139/apnm-2015-0483. PMID:27277571 [DOI] [PubMed] [Google Scholar]
- [190].Larose J, Boulay P, Sigal RJ, et al. Age-related decrements in heat dissipation during physical activity occur as early as the age of 40. PLoS One. 2013;8(12):e83148. doi: 10.1371/journal.pone.0083148. PMID:24349447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [191].Flouris AD, McGinn R, Poirier M, et al. Screening criteria for increased susceptibility to heat stress during work or leisure in hot environments in healthy individuals aged 31–70 years. Temperature. 2017;79–88. doi: 10.1080/23328940.2017.1381800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [192].Flouris AD, Schlader ZJ. Human behavioral thermoregulation during exercise in the heat. Scand J Med Sci Sports. 2015;25(Suppl 1):52–64. doi: 10.1111/sms.12349. PMID:25943656 [DOI] [PubMed] [Google Scholar]
- [193].Collins KJ, Hoinville E. Temperature requirements in old age. Build Serv Eng Res Technol. 1980;1(4):165–172. doi: 10.1177/014362448000100401. [DOI] [Google Scholar]
- [194].Nicol JF, Humphreys MA. Adaptive thermal comfort and sustainable thermal standards for buildings. Energy Build. 2002;34(6):563–572. doi: 10.1016/S0378-7788(02)00006-3. [DOI] [Google Scholar]
- [195].Luo M, de Dear R, Ji W, et al. The dynamics of thermal comfort expectations: The problem challenge and implication. Build Environ. 2016;95:322–329. doi: 10.1016/j.buildenv.2015.07.015. [DOI] [Google Scholar]
- [196].Evans JM. Evaluating comfort with varying temperatures: a graphic design tool. Energy Build. 2003;35(1):87–93. doi: 10.1016/S0378-7788(02)00083-X. [DOI] [Google Scholar]
- [197].Ormandy D, Veronique E. Health and thermal comfort: from WHO guidance to housing strategies. Energy Policy. 2012;49:116–121. doi: 10.1016/j.enpol.2011.09.003. [DOI] [Google Scholar]
- [198].Goromosov MS. The Physiological Basis for Health Standards for Dwellings. Geneva: World Health Organization; 1968. [Google Scholar]
- [199].Rubner M. Lehrbuch der Hygiene. Wien; 1907. [Google Scholar]
- [200].Marsak ME. The meteorological factor in industrial hygiene. Moscow; 1931. [Google Scholar]
- [201].Slonim AD. Animals heat and its regulation in mammal organism. Moscow — Leningrad: Academic Press (Russian); 1952. [Google Scholar]
- [202].World Health Organization The effects of the indoor housing climate on the health of the elderly: Report on a WHO working group. Copenhagen: World Health Organization, Regional Office for Europe; 1984. [Google Scholar]
- [203].Kenny GP, Notley SR, Gagnon D. Direct calorimetry: a brief historical review of its use in the study of human metabolism and thermoregulation. Eur J Appl Physiol. 2017;117(9):1765–1785. doi: 10.1007/s00421-017-3670-5. PMID:28689303 [DOI] [PubMed] [Google Scholar]
- [204].World Meteorological Organization, World Health Organization Heatwaves and health: guidance on warning-system development. In: McGregor GR, Bessemoulin P, Ebi K, et al., editors. Geneva: World Meteorological Organization; 2015. [Google Scholar]
- [205].Ohnaka T, Tochihara Y, Kanda K. Body movements of the elderly during sleep and thermal conditions in bedrooms in summer. Appl Human Sci. 1995;14(2):89–93. doi: 10.2114/ahs.14.89. PMID:7749989 [DOI] [PubMed] [Google Scholar]
- [206].Okamoto-Mizuno K, Tsuzuki K. Effects of season on sleep and skin temperature in the elderly. Int J Biometeorol. 2010;54(4):401–409. doi: 10.1007/s00484-009-0291-7. PMID:20041336 [DOI] [PubMed] [Google Scholar]
- [207].Okamoto-Mizuno K, Mizuno K, Michie S, et al. Effects of humid heat exposure on human sleep stages and body temperature. Sleep. 1999;22(6):767–773. PMID:10505822 [PubMed] [Google Scholar]
- [208].Haskell EH, Palca JW, Walker JM, et al. The effects of high and low ambient temperatures on human sleep stages. Electroencephalogr Clin Neurophysiol. 1981;51(5):494–501. doi: 10.1016/0013-4694(81)90226-1. PMID:6165549 [DOI] [PubMed] [Google Scholar]
- [209].Okamoto-Mizuno K, Tsuzuki K, Mizuno K, et al. Effects of partial humid heat exposure during different segments of sleep on human sleep stages and body temperature. Physiol Behav. 2005;83(5):759–765. doi: 10.1016/j.physbeh.2004.09.009. PMID:15639161 [DOI] [PubMed] [Google Scholar]
- [210].Okamoto-Mizuno K, Tsuzuki K, Mizuno K. Effects of humid heat exposure in later sleep segments on sleep stages and body temperature in humans. Int J Biometeorol. 2005;49(4):232–237. doi: 10.1007/s00484-004-0237-z. PMID:15578234 [DOI] [PubMed] [Google Scholar]
- [211].Sivertsen B, Pallesen S, Glozier N, et al. Midlife insomnia and subsequent mortality: the Hordaland health study. BMC public health. 2014;14:720. doi: 10.1186/1471-2458-14-720. PMID:25024049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [212].Manabe K, Matsui T, Yamaya M, et al. Sleep patterns and mortality among elderly patients in a geriatric hospital. Gerontology. 2000;46(6):318–322. doi: 10.1159/000022184. PMID:11044786 [DOI] [PubMed] [Google Scholar]
- [213].Liu Y, Wheaton AG, Chapman DP, et al. Sleep duration and chronic diseases among U.S. adults age 45 years and older: evidence from the 2010 Behavioral Risk Factor Surveillance System. Sleep. 2013;36(10):1421–1427. doi: 10.5665/sleep.3028. PMID:24082301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [214].Altman NG, Izci-Balserak B, Schopfer E, et al. Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes. Sleep medicine. 2012;13(10):1261–1270. .doi: 10.1016/j.sleep.2012.08.005. PMID:23141932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [215].Parsons KC. Human thermal environments. London: Taylor & Francis; 2003. [Google Scholar]
- [216].Azmoon H, Dehghan H, Akbari J, et al. The relationship between thermal comfort and light intensity with sleep quality and eye tiredness in shift work nurses. J Environ Public Health. 2013;2013:639184. doi: 10.1155/2013/639184. PMID:23476674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [217].Gagnon D, Crandall CG. Electric fan use during heat waves: Turn off for the elderly? Temperature. 2017;4(2):104–106. doi: 10.1080/23328940.2017.1295833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [218].Gagnon D, Romero SA, Cramer MN, et al. Age Modulates Physiological Responses during Fan Use under Extreme Heat and Humidity. Med Sci Sports Exerc. 2017; Med Sci Sports Exerc. 2017 Nov;49(11):2333–2342. doi: 10.1249/MSS.0000000000001348. PMID:28609330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [219].Kilbourne EM. The spectrum of illness during heat waves. Am J Prev Med. 1999;16(4):359–360. PMID:10493296 [DOI] [PubMed] [Google Scholar]
- [220].Kaiser R, Rubin CH, Henderson AK, et al. Heat-related death and mental illness during the 1999 Cincinnati heat wave. The American journal of forensic medicine and pathology. 2001;22(3):303–307. doi: 10.1097/00000433-200109000-00022. PMID:11563746 [DOI] [PubMed] [Google Scholar]
- [221].Marmor M. Heat wave mortality in nursing homes. Environ Res. 1978;17(1):102–115. doi: 10.1016/0013-9351(78)90065-8. PMID:318500 [DOI] [PubMed] [Google Scholar]
- [222].Klinenberg E. Heat wave: a social autopsy of disaster in Chicago. Chicago, IL: Chicago University Press; 2002. [DOI] [PubMed] [Google Scholar]
- [223].Kosatsky T, Dufresne J, Richard L, et al. Heat awareness and response among Montreal residents with chronic cardiac and pulmonary disease. Can J Public Health. 2009;100(3):237–240. PMID:19507730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [224].Richard L, Kosatsky T, Renouf A. Correlates of hot day air-conditioning use among middle-aged and older adults with chronic heart and lung diseases: the role of health beliefs and cues to action. Health Edu Res. 2011;26(1):77–88. doi: 10.1093/her/cyq072. [DOI] [PubMed] [Google Scholar]
- [225].Lane K, Wheeler K, Charles-Guzman K, et al. Extreme heat awaraness and protective behaviors. J Urban Health. 2013;91(3):403–414. doi: 10.1007/s11524-013-9850-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [226].Hwang RL, Chen CP. Field study on behaviors and adaptation of elderly people and their thermal comfort requirements in residential environments. Indoor air. 2010;20(3):235–245. doi: 10.1111/j.1600-0668.2010.00649.x. PMID:20573123 [DOI] [PubMed] [Google Scholar]
- [227].Klenk J, Becker C, Rapp K. Heat-related mortality in residents of nursing homes. Age and ageing. 2010;39(2):245–252. doi: 10.1093/ageing/afp248. PMID:20093248 [DOI] [PubMed] [Google Scholar]
- [228].Michelon T, Magne P, Simon-Delavelle F. Lessons of the 2003 heat-wave in France and Action taken to limit the effects of future heat-waves. In: Kirch W, Menne B, Bertollini R, editors. Extreme weather events. Heidelberg: Springer-Verlag; 2005. p. 131–140. [Google Scholar]
- [229].Ministry of Health and Long-Term Care Long-Term Care Home Design Manual. Government of Ontario; 2015. Available from: HealthCapitalInvestmentBranch@ontario.ca [Google Scholar]
- [230].Mendell MJ, Lei-Gomez Q, Mirer AG, et al. Risk factors in heating, ventilating, and air-conditioning systems for occupant symptoms in US office buildings: the US EPA BASE study. Indoor Air. 2008;18(4):301–316. doi: 10.1111/j.1600-0668.2008.00531.x. PMID:18492050 [DOI] [PubMed] [Google Scholar]
- [231].Preziosi P, Czernichow S, Gehanno P, et al. Workplace air-conditioning and health services attendance among French middle-aged women: a prospective cohort study. Int J Epidemiology. 2004;33(5):1120–1123. doi: 10.1093/ije/dyh136. [DOI] [PubMed] [Google Scholar]
- [232].Sahakian N, Park JH, Cox-Ganser J. Respiratory morbidity and medical visits associated with dampness and air-conditioning in offices and homes. Indoor Air. 2009;19(1):58–67. doi: 10.1111/j.1600-0668.2008.00561.x. PMID:19076249 [DOI] [PubMed] [Google Scholar]
- [233].Scott MJ, Huang YJ. Effects of climate change on energy use in the United States. In: Wilbanks TJ, Bhatt V, Bilello DE, et al., editors. Synthesis and assessment product 4.5.. Washington, DC: Climate Change Science Program; 2007. p. 8–44. [Google Scholar]
- [234].Public Health England Heatwave plan for England. London, UK: Public Health England; 2015. p. 46. [Google Scholar]
- [235].US Environmental Protection Agency Excessive heat events guidebook. Washington (DC): United States Environmental Protection Agency; 2006. [Google Scholar]


