Summary
Collaboration between gastroenterologists and rheumatologists is recommended for the correct management of patients with associated spondyloarthritis (SpA) and inflammatory bowel disease (IBD). We aimed to establish the appropriateness of several red flags for a prompt specialist referral. A systematic review of the literature was performed using the GRADE method to describe the prevalence of co‐existing IBD‐SpA and the diagnostic accuracy of red flags proposed by a steering committee. Then, a consensus among expert gastroenterologists and rheumatologists (10 in the steering committee and 13 in the expert panel) was obtained using the RAND method to confirm the appropriateness of each red flag as ‘major’ (one sufficient for patient referral) or ‘minor’ (at least three needed for patient referral) criteria for specialist referral. The review of the literature confirmed the high prevalence of co‐existing IBD‐SpA. Positive and negative predictive values of red flags were not calculated, given the lack of available data. A consensus among gastroenterology and rheumatology specialists was used to confirm the appropriateness of each red flag. Major criteria to refer patients with SpA to the gastroenterologist included: rectal bleeding, chronic abdominal pain, perianal fistula or abscess, chronic diarrhoea and nocturnal symptoms. Major criteria to refer patients with IBD to the rheumatologist included: chronic low back pain, dactylitis, enthesitis and pain/swelling of peripheral joints. Several major and minor red flags have been identified for the diagnosis of co‐existing IBD‐SpA. The use of red flags in routine clinical practice may avoid diagnostic delay and reduce clinic overload.
Keywords: inflammatory bowel disease, red flag, spondyloarthritis
Introduction
Inflammatory bowel diseases (IBD, including Crohn's disease (CD) and ulcerative colitis (UC) and spondyloarthritis (SpA), are chronic disorders which may co‐exist in the same subject, worsening the disability and the quality of life of the patient and making the clinical management of the diseases more complicated. It is noteworthy that SpA is reported in the literature as the most common extra‐intestinal manifestation in IBD patients 1, 2, 3, 4, 5. However, this still represents an underestimated clinical problem, as demonstrated by Stolwijk et al. in a Dutch study: among 350 IBD patients, 129 (39·6%) reported articular symptoms suggestive of SpA, but only half of them were referred to a rheumatologist 5. A prompt and correct diagnosis of these disorders may have a significant impact on their therapeutic management, influencing the type and duration of therapies 6, 7 and possibly preventing the complications related to progressive and potentially irreversible intestinal and articular tissue damage. Conversely, symptoms not specifically related to inflammatory conditions may induce inappropriate referral, causing clinic overload. Therefore, direct collaboration between gastroenterologists and rheumatologists is fundamental, and may benefit from the identification of ‘red flags’ (disease‐specific signs and symptoms) for easier and more appropriate patient referral.
Recently, several red flags have been proposed to facilitate early referral of patients with Crohn's disease from primary to specialist care and thus avoid diagnostic delay 8. Moreover, a six‐item questionnaire (DETAIL) has been developed to screen patients with IBD for the diagnosis of SpA, but it needs to be validated in larger cohorts of patients 9.
This study aimed to obtain a consensus among gastroenterology and rheumatology specialists on the adequateness of several ‘red flags’ for a correct referral of patients with IBD and SpA from the gastroenterologist to the rheumatologist (and vice versa).
Methods
The entire process was developed throughout several meetings, from December 2016 to October 2017. ‘Red flags’ were defined as signs or symptoms which may alert to a possible diagnosis of IBD in a patient with axial or peripheral SpA, or (analogously) may alert to a possible diagnosis of axial or peripheral SpA in a patient with IBD, allowing a prompt referral to the relevant clinical specialist (Table 1).
Table 1.
Definition of gastrointestinal and rheumatological red flags selected by the Steering Committee
| ‘Red flag’: sign or symptom suggestive of a specific disease | |
|---|---|
| Red flags for IBD | Red flags for SpA |
| Chronic diarrhoea (change in the bowel habit with loose stools and/or increase of bowel movements per day lasting >4 weeks) | Chronic low back pain (>3 months) |
| Chronic abdominal pain (>3 months) 8 | Family history of SpA (presence in first‐degree or second‐degree relatives of any of the following: AS, psoriasis, acute uveitis, reactive arthritis, IBD 73 |
| Rectal bleeding (not from haemorrhoids) | Peripheral joint pain*/swelling |
| Weight loss (>5% in the last 3 months 8, involuntarily) | Dactylitis (past or present, diagnosed by a doctor) 73 |
| Fever (no otherwise explained and associated to raised inflammatory markers) | Enthesitis (heel enthesitis: past or present spontaneous pain or tenderness at examination at the site of the insertion of the Achilles tendon or plantar fascia at the calcaneus) 73 |
| Family history of IBD | Psoriasis (past or present, diagnosed by a doctor) 73 |
| Anaemia (no otherwise explained) | Anterior uveitis (past or present, and confirmed by an ophthalmologist) 73 |
| Perianal fistula or abscess (past or current) | Urethritis/cervicitis (within 1 month before the onset of arthritis/enthesitis/dactylitis) 73 |
| Nocturnal symptoms (diarrhoea or abdominal pain) | Chest pain |
| Oral aphtosis (recurrent) | |
IBD = inflammatory bowel disease; SpA = spondyloarthritis; AS = ankylosing spondylitis.
Recurrent or lasting >3 months.
Project management
The steering committee was the same as previous projects already published concerning the management of this particular clinical setting 6, 7 and included 10 Italian rheumatologists and gastroenterologists with definitive expertise in the field of SpA and IBD identified according to their publication record, participation in national meetings and clinical trials and/or senior academic rank. Two clinical fellows (C.F. and P.L.) performed the systematic review of the literature. The expert panel was composed of 13 gastroenterologists and rheumatologists from different Italian regions (Supporting information, Appendix 1). A clinical epidemiologist with expertise in the GRADE framework and consensus methods was also involved (L.S.), as well as an experienced medical librarian.
Systematic literature review
The GRADE framework for diagnostic tests was used to formulate the search questions (Table 2), with the definition of patients, diagnostic test (in our case, ‘red flag’), comparison (in our case, the absence of ‘red flag’) and outcomes of interest 10.
Table 2.
GRADE model for diagnostic tests used for the literature search
| Population | Rheumatological patient | Gastroenterological patient |
|---|---|---|
|
|
|
| Diagnostic test (‘red flag’) | Gastrointestinal signs or symptoms | Rheumatological signs or symptoms |
|
|
|
| Control (absence of ‘red flag’) | Absence of gastrointestinal symptoms | Absence of rheumatological symptoms |
| Outcome | Diagnosis of gastrointestinal disease | Diagnosis of rheumatological disease: |
|
|
IBD = inflammatory bowel disease; CD = Crohn's disease; UC = ulcerative colitis; SpA = spondyloarthritis; AxSpA = axial spondyloarthritis; pSpA = peripheral spondyloarthritis.
To estimate the positive and negative predictive value (post‐test probability) of each red flag, information about the prevalence of the disease (pre‐test probability) and test accuracy (sensitivity and specificity) would be needed. Therefore, different systematic reviews were performed to address the following issues:
the prevalence of SpA in patients with an established diagnosis of IBD;
the prevalence of IBD in patients with an established diagnosis of SpA;
the diagnostic accuracy of rheumatological red flags in IBD patients; and
the diagnostic accuracy of gastrointestinal red flags in SpA patients.
PubMed and EMBASE were interrogated for the search, without initial date limit, until January 2017. Only English papers were included, and abstracts without full text were excluded. Details of search terms for prevalence data are available in the Supporting information.
Statistical analyses
Abstract and full texts were assessed for eligibility, and data were extracted by the clinical fellows (C.F. and P.L.) in two dedicated spreadsheets (one for SpA and one for IBD), in duplicate. The metan suite of commands in stata version 14 was used for data synthesis, using random effect models. Heterogeneity was assessed by means of the I 2 statistic. The sources of heterogeneity that were explored were specific diagnosis (AxSpA/pSpA, CD/UC/IBD) in all population/outcome combinations (i.e. all possible scenarios) and (for diagnostic accuracy) in each individual red flag.
To obtain a rough estimate of the positive and negative predictive value of each red flag for the population/outcome combination of interest, the Bayes formula was applied, informed with estimates obtained in the meta‐analysis.
RAND method
Given the results of the systematic review (see Results), the RAND method 11 was used to define the appropriateness of patient referral from the gastroenterologist to the rheumatologist and vice versa, when specific signs or symptoms (red flags) suggest co‐existing IBD‐SpA in a number of clinical scenarios.
Expert opinion
Based on the results of the systematic review of the literature and their personal opinion, the gastroenterology and rheumatology specialists participated in two rounds of an online survey (the first in June 2017 and the second in August 2017) to define the appropriateness of gastroenterology or rheumatology referral for each red flag. A procedure (in this case: referral to a clinical specialist) should be considered appropriate when ‘the expected health benefit […] exceeds the expected negative consequences […] by a sufficiently wide margin that the procedure is worth doing, exclusive of cost’ 11, 12, 13.
A nine‐point scale was used to quantify appropriateness of referral, considering ‘1’ as absolutely inappropriate, ‘5’ as uncertain and ‘9’ as absolutely appropriate. The median score was used to classify appropriateness (1–3 inappropriate, 4–6 probably appropriate, 7–9 always appropriate), and the 30–70th interpercentile range corrected for asymmetry (IPRAS) was used to assess disagreement. After viewing the results of the first round, in which their responses were highlighted, panel members were asked to review their choices in the second round.
Final consensus
The final meeting was held on 10 October 2017 in Rome, Italy. The goal was to reach consensus on the final classification of each red flag as ‘major’ (1 red flag sufficient for patient referral) or ‘minor’ (>1 red flag needed for patient referral) and to establish how many minor red flags are required to justify patient referral in both gastroenterological and rheumatological settings. All questions were formulated as: ‘Do you agree to consider this red flag as “major” criteria for referral in this scenario?’ or ‘do you agree that a minimum of three minor red flags are needed for referral?’, allowing ‘yes’, ‘no’ or ‘no opinion’ as responses. All votes were expressed electronically and anonymously. Consensus was defined as >70% of the panel agreeing for ‘yes’ with <15% of the panel responding ‘no’.
Results
Systematic review
A total of 28 384 non‐duplicate records were screened at the abstract level: 939 for the prevalence of co‐existing IBD‐SpA (Fig. 1); 15 954 for the diagnostic accuracy of gastrointestinal red flags; and 11 491 for rheumatological red flags (Supporting information, Figs. S1 and S2). Then, 378 full texts were assessed for eligibility and, finally, 78 papers were included in the qualitative and quantitative analysis: 67 for the analysis of the prevalence of co‐existing IBD‐SpA 2, 3, 4, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77 (Tables 3 and 4) and only 11 for the diagnostic accuracy of red flags 8, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87.
Figure 1.
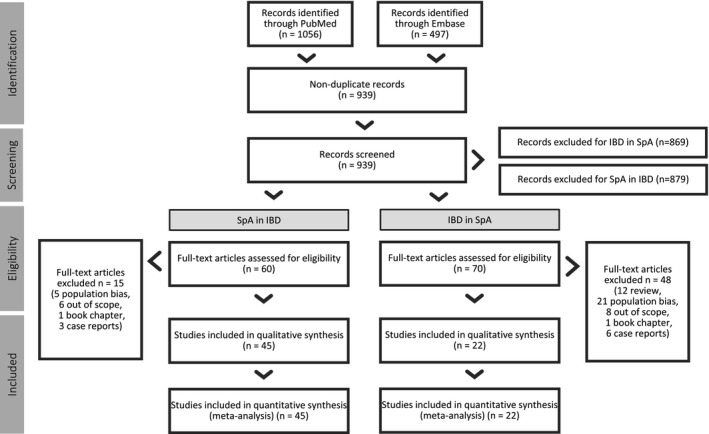
Flowchart of study selection for prevalence of co‐existing inflammatory bowel diseases (IBD) and spondyloarthritis (SpA) (‘SpA in IBD’: prevalence of SpA among patients with a diagnosis of IBD; ‘IBD in SpA’: prevalence of IBD in patients with a diagnosis of SpA).
Table 3.
Characteristics of studies included in the analysis of prevalence of SpA in IBD patients
| Author (year) | Study design | Country | Population (n diagnosis) | SpA (n diagnosis) | Prevalence SpA (%) |
|---|---|---|---|---|---|
| Al‐Jarallah (2013) 14 | Prospective cross‐sectional | Kuwait | 130 IBD (45 UC, 85 CD) | 41 PSpA | 31·5 |
| 15 AxSpA | 11·5 | ||||
| 4 SA | 3·1 | ||||
| 7 Entesopathy | 5·4 | ||||
| 2 Dactylitis | 1·5 | ||||
| Bandinelli (2014) 15 | Prospective cohort | Italy | 81 IBD (26 UC, 55 CD) | 22 Radiological SA | 27·1 |
| Bandyopadhyay (2015) 16 | Prospective cross‐sectional | India | 120 IBD (58 UC, 62 CD) | AS | 18 |
| PA | 23 | ||||
| Bardazzi (1997) 17 | Prospective cross‐sectional | Italy | 68 UC | 4 AS | 5·8 |
| 9 SA | 13·2 | ||||
| 6 unclassified SpA | 8·8 | ||||
| Barreiro‐De Acosta (2007) 18 | Prospective cross‐sectional | Spain | 173 CD | 31 PA | 17·9 |
| 12 SA | 6·9 | ||||
| 4 AS | 2·3 | ||||
| Bernstein (2001) 19 | Population‐based registry | Canada | 4454 IBD | AS | 0·8 (female) |
| 2·1 (male) | |||||
| Beslek (2009) 20 | Prospective cross‐sectional | Turkey | 122 IBD (94 UC, 28 CD) | 35 SpA | 28·7 |
| 10 AS | 8·2 | ||||
| Bhat (2009) 21 | Registry | USA/Canada | 1489 IBD | PA | 7 |
| SA | 4 | ||||
| AS | 2 | ||||
| Bruining (2008) 22 | Retrospective | USA | 357 CD | 8 Radiological SA | 2·2 |
| Christodoulou (2002) 23 | Retrospective | Greece | 215 UC | 9 SA | 4·2 |
| 5 oligo‐PA | 2·3 | ||||
| 18 poly‐PA | 8·3 | ||||
| 37 CD | 6 SA | 16·2 | |||
| 2 oligo‐PA | 5·4 | ||||
| 3 poly‐PA | 8·1 | ||||
| Dekker‐Saeys (1978) 25 | Prospective cross‐sectional | The Netherlands | 109 IBD | 4 AS | 3·7 |
| PA | 12·8 | ||||
| Radiological SA | 10·1 | ||||
| D'Incà (2009) 24 | Prospective cohort | Italy | 385 UC | 8 SA | 2·1 |
| 4 AS | 1 | ||||
| 8 Oligo‐PA | 2·1 | ||||
| 7 Poly‐PA | 1·8 | ||||
| 266 CD | 15 SA | 5·6 | |||
| 5 AS | 1·9 | ||||
| 2 Oligo‐PA | 0·7 | ||||
| 7 Poly‐PA | 2·6 | ||||
| Van Erp (2016) 4 | Prospective cohort | The Netherlands | 510 IBD | 155 SpA | 30·4 |
| Enthesitis | 0·7 | ||||
| Dactylitis | 0·7 | ||||
| Hyla (1976) 26 | Prospective cross‐sectional | USA | 89 IBD | 11 Radiological SA | 12·4 |
| 4 AS | 4·5 | ||||
| Jalan (1970) 27 | Retrospective | Scotland | 399 UC | 17 AS | 4·2 |
| 27 Arthropathy | 6·8 | ||||
| 20 Dactylitis | 5 | ||||
| Karreman (2016) 28 | Meta‐analysis | NA | IBD | SpA | 13 |
| PA | 13 | ||||
| SA | 10 | ||||
| AS | 3 | ||||
| Enthesitis | 1 | ||||
| Dactylitis | 6 | ||||
| Kochhar (1991) 29 | Prospective cross‐sectional | India | 150 UC | 16 SA | 10·7 |
| 21 PA | 14 | ||||
| Lanna (2008) 30 | Prospective cross‐sectional | Brasil | 130 IBD | 8 AS | 6·2 |
| 7 Enthesitis | 5·4 | ||||
| 12 Radiological SA | 9·2 | ||||
| 21 PA | 16·2 | ||||
| 59 UC | AS | 0 | |||
| 2 Enthesitis | 3·4 | ||||
| Radiological SA | 3·4 | ||||
| PA | 11·9 | ||||
| 71 CD | AS | 11·3 | |||
| 5 Enthesitis | 7 | ||||
| Radiological SA | 14·1 | ||||
| PA | 19·7 | ||||
| Leclerc‐Jacob (2014) 31 | Retrospective | France | 186 IBD | 31 Radiological SA | 16·7 |
| Liu (2016) 32 | Retrospective | China | 195 CD | 8 AS | 4·12 |
| McEniff (1994) 33 | Prospective case series | USA | 65 IBD | 21 Radiological SA | 32 |
| Mocelin (2015) 34 | Retrospective | Brasil | 100 CD | 6 SpA | 6 |
| Modena (1988) 35 | Prospective case series | Italy | 51 CD | 6 AS | 11·7 |
| 8 oligo‐PA | 15·7 | ||||
| 2 poly‐PA | 3·9 | ||||
| 6 Radiological SA | 11·7 | ||||
| Münch (1986) 36 | Prospective cross‐sectional | Germany | 167 CD | 73 SpA | 44 |
| 15 AS | 9 | ||||
| 24 SA | 14 | ||||
| 23 PA | 14 | ||||
| 11 SA + arthritis | 7 | ||||
| Orchard (2008) 37 | Prospective case series | UK | 44 CD | 17 Radiological SA | 39 |
| Palm (2002) 38 | Population‐based cohort | Norway | 521 IBD | 15 AS | 3·7 |
| 2 Dactylitis | |||||
| 1 Enthesitis | |||||
| SpA | 22 | ||||
| Radiological SA | 2 | ||||
| Paparo (2012) 39 | Retrospective | Italy | 221 CD | 53 Radiological SA | 24 |
| Peeters (2004) 40 | Prospective cross‐sectional | Belgium | 102 CD | 23 Radiological SA | 23 |
| 9 AS | 8·8 | ||||
| 17 PA | 16·6 | ||||
| 11 Enthesopathy | 10·4 | ||||
| Peeters (2008) 41 | Prospective cross‐sectional | Belgium | 244 CD | 65 Radiological SA | 27 |
| 16 AS | 6·5 | ||||
| Pezerović (2013) 42 | Retrospective population‐based | Croatia | 150 IBD | 32 PA | 21·3 |
| 6 SA | 4 | ||||
| 8 AS | 5·3 | ||||
| 119 UC | 24 PA | 20·2 | |||
| 3 SA | 2·5 | ||||
| 4 AS | 3·4 | ||||
| 31 CD | 8 PA | 25·8 | |||
| 3 SA | 9·7 | ||||
| 4 AS | 12·9 | ||||
| Pokharna (2004) 43 | Prospective cross‐sectional | India | 46 UC | 1 PA | 2 |
| Queiro (2000) 44 | Prospective cross‐sectional | Spain | 62 IBD | 15 Radiological SA | 24 |
| 19 PA | 30 | ||||
| 2 AS | 3 | ||||
| Rodriguez (2008) 45 | Prospective cross‐sectional | Puerto Rico | 100 IBD | 42 SpA | 42 |
| 2 AS | 2 | ||||
| 13 SA | 13 | ||||
| 5 PA | 5 | ||||
| 3 Dactylitis | 3 | ||||
| 2 Enthesitis | 2 | ||||
| Salvarani (2001) 2 | Population‐based inception cohort | Italy, the Netherlands | 160 IBD | 29 SpA | 18·1 |
| 5 AS | 3·1 | ||||
| 23 Unclassified SpA | 14·4 | ||||
| Scarpa (1992) 46 | Prospective cross‐sectional | Italy | 79 UC | 20 AS | 25·3 |
| 15 PA | 19 | ||||
| 14 Unclassified SpA | 17·7 | ||||
| Scott (1990) 47 | Prospective cross‐sectional | USA | 86 CD | 25 Radiological SA | 29 |
| Sofia (2014) 49 | Retrospective | USA | 513 Caucasian UC | 10 AS/SA | 1·6 |
| 28 African American UC | 2 AS/SA | 7·1 | |||
| 1127 Caucasian CD | 2.9 AS/SA | 2·9 | |||
| 108 African American CD | 3 AS/SA | 2·8 | |||
| Steer (2003) 50 | Prospective cross‐sectional | UK | 134 CD | 31 Radiological SA | 23 |
| Suh (1998) 51 | Retrospective | Korea | 129 IBD | 20 PA | 15 |
| Radiological SA | 6·2 | ||||
| AS | 1·6 | ||||
| 77 UC | 15 PA | 19·6 | |||
| 52 CD | 5 PA | 9·6 | |||
| Sung (1994) 52 | Retrospective | China | 15 CD | 2 AS | 13·3 |
| 1 SA | 6·6 | ||||
| 1 Colitic arthritis | 6·6 | ||||
| Turkcapar (2006) 3 | Prospective cross‐sectional | Turkey | 162 IBD | 74 SpA | 45·7 |
| 16 AS | 9·9 | ||||
| 24 PA | 14·8 | ||||
| 81 Enthesitis | 50 | ||||
| 74 Bilateral SA | 45·7 | ||||
| 22 Radiological SA | 13·6 | ||||
| 84 UC | 36 SpA | 42·8 | |||
| 7 AS | 8·3 | ||||
| 12 PA | 14·3 | ||||
| 39 Enthesitis | 46·4 | ||||
| 36 Bilateral SA | 42·8 | ||||
| 12 Radiological SA | 14·3 | ||||
| 78 CD | 38 SpA | 48·7 | |||
| 9 AS | 11·5 | ||||
| 12 PA | 15·4 | ||||
| 42 Enthesitis | 53·8 | ||||
| 38 Bilateral SA | 48·7 | ||||
| 10 Radiological SA | 12·8 | ||||
| Vavricka (2011) 53 | Prospective cohort | Swiss | 950 IBD | 272 Arthritis | 28·6 |
| 39 AS | 4·1 | ||||
| 370 UC | 79 Arthritis | 21·3 | |||
| 6 AS | 1·6 | ||||
| 580 CD | 193 Arthritis | 33·3 | |||
| 33 AS | 5·7 | ||||
| Vavricka (2015) 54 | Registry | Swiss | 1249 IBD | 60 AS/SA | 16·4 |
| 256 Arthritis | 70 | ||||
| 483 UC | 14 AS/SA | 13·4 | |||
| 62 Arthritis | 59·1 | ||||
| 735 CD | 45 AS/SA | 18·2 | |||
| 184 Arthritis | 74·2 | ||||
| de Vlam (2000) 48 | Prospective cross‐sectional | 103 IBD | 10 AS | 10 | |
| 10 Synovitis | 10 | ||||
| 7 Enthesopathy | 7 | ||||
| 33 SA | 32 | ||||
| 36 SpA | 35 | ||||
| 25 UC | 3 AS | 12 | |||
| 3 Synovitis | 12 | ||||
| 2 Enthesopathy | 4 | ||||
| 6 SA | 24 | ||||
| 11 SpA | 44 | ||||
| 78 CD | 7 AS | 9 | |||
| 7 Synovitis | 9 | ||||
| 5 Enthesopathy | 8 | ||||
| 27 SA | 35 | ||||
| 25 SpA | 32 | ||||
| Yi (2012) 55 | Retrospective | China | 153 CD | 7 Arthritis | 4·6 |
| 1 AS | 0·65 |
IBD = inflammatory bowel disease; CD = Crohn's disease; UC = ulcerative colitis; SpA = spondyloarthritis; AxSpA = axial spondyloarthritis; pSpA = peripheral spondyloarthritis; PA = peripheral arthritis; AS = ankylosing spondylitis; SA = sacroiliitis.
Table 4.
Characteristics of studies included in the analysis of prevalence of IBD in SpA patients
| Author (year) | Study design | Country | Population (n diagnosis) | IBD (n diagnosis) | Prevalence IBD (%) |
|---|---|---|---|---|---|
| Mitulescu (2015) 68 | Retrospective | Romania | 70 SA | 1 IBD | 1·4 |
| 39 PsA | 0 IBD | 0 | |||
| 17 USPA | 2 IBD | 11·8 | |||
| Rudwaleit (2011) 73 | Prospective cohort | Multi‐national | 176 pSpA | 6 IBD | 3·4 |
| Essers et al. (2015) 66 | Prospective cohort | The Netherlands | 216 SA | 15 IBD | 23·6 |
| Belgium | |||||
| France | |||||
| Dougados (2015) 63 | Prospective cohort | France | 708 AxSpA | 35 IBD | 4·9 |
| Deesomchok (1985) 61 | Retrospective cohort | Thailand | 46 SA | 0 | 0 |
| Eliakim (2005) 65 | Prospective cross‐sectional | Israel | 20 SpA | 6 CD‐like lesions endoscopic findings | 30 |
| Dean (2016) 60 | Registry | Scotland | 1964 AS primary care | 118 IBD | 6 |
| 1700 secondary care | 204 IBD | 12 | |||
| Perez Alamino (2011) 70 | Retrospective | Multi‐national | 1274 AS | 45 IBD | 3·6 |
| Collantes (2007) 58 | Registry | Spain | 1385 SpA | 13 IBD | 0·3 |
| Buschiazzo (2011) 57 | Prospective cohort | Argentina | 402 SpA | 10 IBD | 2·5 |
| Sampaio‐Barros (2011) 75 | Prospective cohort | Italy | 1036 SpA | 10 IBD | 1 |
| Peluso (2015) 69 | Retrospective | Italy | 387 PsA | 63 IBD | 16·2 |
| 15 CD | 3·8 | ||||
| 10 UC | 2·5 | ||||
| 38 Non‐specific colitis | 9·8 | ||||
| Rojas‐Vargas (2009) 71 | Retrospective | Spain | 150 SpA | 4 IBD | 2·6 |
| Costello (1980) 59 | Prospective | USA | 55 SA | 9 IBD | 16·3 |
| 3 CD | 5·45 | ||||
| 6 UC | 10·9 | ||||
| Edmunds (1981) 64 | Prospective | UK | 1331 SA | 82 IBD | 6 |
| Tayel (2012) 77 | Registry | Egypt | 75 SpA | 1 IBD | 1·3 |
| del Río‐Martínez (2016) 62 | Registry | Spain | 291 AxSpA | 9 IBD | 3·1 |
| 86 pSpA | 1o IBD | 11·6 | |||
| Stolwijk (2015) 76 | Registry | UK | 4101 SA | 151 IBD | 3·7 |
| Said‐Nahal (2000) 74 | Retrospective | France | 329 SpA | 17 IBD | 5 |
| 10 CD | 3 | ||||
| 7 UC | 2 | ||||
| García‐Vicuña (2016) 67 | Prospective cohort | Spain | 513 SpA | 13 IBD | 2·5 |
IBD = inflammatory bowel disease; CD = Crohn's disease; UC = ulcerative colitis; SpA = spondyloarthritis; AxSpA = axial spondyloarthritis; pSpA = peripheral spondyloarthritis; USpA = unclassified SpA; AS = ankylosing spondylitis; SA = sacroiliitis; PsA = psoriatic arthritis.
Results of this exercise indicated high heterogeneity of prevalence estimates across studies and clinical scenarios (I 2 statistics: 90·3% for prevalence of IBD in AxSpA, 89·1% in pSpA, 96·3% for SpA in CD, 94·7% in UC, 98·1% in IBD, all P < 0·001) and low reliability in the estimates of accuracy due to poor quality of evidence. Therefore, the results were not pooled into a summary estimate but used only in a qualitative manner.
There were no studies specifically focused on the diagnostic accuracy of gastroenterological red flags in rheumatological patients, and vice versa. Therefore, the review and the subsequent data analysis included the sensitivity and specificity of red flags in the general population as the best surrogate. For some red flags, there were no specific data on diagnostic accuracy. Considering the impossibility to pool results, and to obtain a reliable summary estimate of the prevalence of co‐existing IBD‐SpA and diagnostic accuracy of individual red flags, positive and negative predictive values were not calculated.
RAND online surveys
The response rate to the online survey was 100% in both rounds. Nno disagreement was reported after the second round, and all red flags were judged as ‘absolutely appropriate’ or ‘probably appropriate’. Moreover, there was a general overlap between rheumatological (axial and peripheral SpA) and gastrointestinal (IBD, UC and CD) scenarios.
Based on the results of the online survey, red flags were categorized into two possible clinical scenarios: gastrointestinal or rheumatological signs or symptoms in patients with SpA and IBD, respectively. In fact, a more accurate diagnosis (axial or peripheral SpA and CD or UC) is the result of the process guided by the specialist after patient referral and, therefore, was considered out of the scope of this paper.
Final consensus
A total of 22 specialists participated in this final session of the consensus (attendance rate 92%).
The participants were called to vote on the appropriateness of each red flag to confirm the classification as minor or major criteria. Major criteria for the referral of a patient with SpA to the gastroenterologist included: rectal bleeding, chronic abdominal pain, perianal fistula or abscess, chronic diarrhoea and nocturnal symptoms. Major criteria for the referral of a patient with IBD to the rheumatologist included: chronic low back pain, dactylitis, enthesitis and pain/swelling of peripheral joints. All remaining red flags were confirmed to be minor criteria (Table 5). Urethritis/cervicitis was removed from the list of red flags due to its inclusion in other three major criteria (arthritis/enthesitis/dactylitis) 86.
Table 5.
Classification of red flags as ‘major’ or ‘minor’ criteria for specialist referral
| Red flags in SpA | Criteria classification | Red flags in IBD | Criteria classification |
|---|---|---|---|
| Chronic diarrhoea | Major | Chronic low back pain | Major |
| Rectal bleeding | Major | Dactylitis | Major |
| Perianal fistula/abscess | Major | Enthesitis | Major |
| Chronic abdominal pain | Major | Peripheral joint pain/swelling | Major |
| Nocturnal symptoms | Major | Family history of SpA | Minor |
| Oral aphtosis | Minor | Psoriasis | Minor |
| Fever | Minor | Anterior uveitis | Minor |
| Anaemia | Minor | Chest pain | Minor |
| Family history of IBD | Minor | Urethritis/cervicitis | Removed |
| Weight loss | Minor |
IBD = inflammatory bowel disease; SpA = spondyloarthritis.
The participants also approved the need for at least three minor criteria for specialist referral in both cases (rheumatological referral of patients with IBD to, and gastroenterological referral of, patients with SpA).
Discussion
The identification of patients with co‐existing IBD and SpA may have important implications for their clinical management by influencing treatment, preventing possible complications and, thus, improving clinical outcomes and quality of life. Multi‐disciplinary collaboration between gastroenterologists and rheumatologists represents the best way to improve the therapeutic approach to such complex clinical scenarios.
This study identified several red flags for prompt and appropriate referral between gastroenterologists and rheumatologists, which might potentially facilitate the diagnosis of co‐existing IBD‐SpA.
The results from our systematic review first confirmed the high prevalence of co‐existing IBD‐SpA, particularly in the gastroenterological population (Table 3). The impact of this association is particularly relevant for the clinical management of IBD patients because articular involvement often requires more expensive or aggressive therapeutic approaches, including biological agents or combination treatment with immunosuppressants (i.e. methotrexate). Moreover, van der Have and colleagues recently showed that the presence of joint pain might significantly and negatively affect the quality of life and the work productivity of IBD patients 88. The prevalence of IBD in the rheumatological setting seems to be lower, but clinically significant even so (Table 4). The importance of identifying co‐existing IBD among these patients also derives from the possibility of developing chronic intestinal inflammation during treatment with etanercept, a tumour necrosis factor (TNF) inhibitor specifically used in rheumatology and dermatology 89. Moreover, the diagnosis of co‐existing IBD‐SpA may influence the dosage and infusion regimen of most biological agents, because gastroenterological diseases require higher doses in comparison with those used for the treatment of isolated SpA 7.
Very scarce evidence emerged from the literature search concerning the diagnostic accuracy of red flags. No studies could be found specifically in the gastroenterological or rheumatological setting, and a very limited number of studies performed in the general population were identified. In particular, sensitivity and specificity of gastrointestinal red flags for the diagnosis of IBD have been described in only three papers 8, 78, 79. Ford et al. 78 prospectively enrolled 1981 consecutive patients attending the gastroenterological clinic of two Canadian hospitals because of gastrointestinal symptoms. All subjects underwent a full colonoscopy and were invited to describe their intestinal symptoms among a list selected from the Rome III diagnostic questionnaire 90. Three hundred and two patients were diagnosed with IBD, whereas all the others (n = 1679) served as controls. The items that resulted in independent predictors of IBD were: positive family history, younger age, the passage of stools more than four times a day >75% of the time, urgency most of the time and anaemia. However, the authors concluded that individual items were not useful to predict a diagnosis of IBD, because most of them had low sensitivity and specificity values 78. Danese and colleagues 8 identified several red flags to be included in a 21‐item questionnaire and administered it to 85 CD patients, 80 subjects with IBS (irritable bowel syndrome) and 36 healthy controls, asking to select the symptoms they had had during the 12 months before the diagnosis (for CD) or at the time of the visit (for IBS and controls). Interestingly, all red flags included in our study were significantly more frequent in the CD patients evaluated by Danese et al. 8 Finally, the authors proposed an index with high predictive value for CD diagnosis, based on the eight items that resulted independent at the multivariate analysis, to be validated in prospective studies 8. The study published by Lisciandrano et al. described the pattern of oral lesions in IBD patients and controls, without showing any statistically significant difference among groups 79.
The ASAS (Assessment of SpondyloArthritis International Society Group) developed sets of criteria for the classification of peripheral and axial (with and without definite radiographic sacroiliitis) SpA. The clinical history included features of inflammatory back pain (IBP) and extraspinal manifestations such as arthritis, enthesitis, uveitis, dactylitis, psoriasis, Crohn's/ulcerative colitis, good response to non‐steroidal anti‐inflammatory drugs (NSAIDs), family history for SpA, human leucocyte antigen (HLA)‐B27 and elevated C‐reactive protein (CRP). In accordance with these criteria, a patient with chronic back pain (>3 months) and age at onset less than 45 years can be classified in the presence of sacroiliitis plus at least one typical SpA feature, or in the presence of HLA‐B27 plus at least two other SpA features. Patients with arthritis and/or enthesitis and/or dactylitis plus one or more of the following parameters – psoriasis, inflammatory bowel disease, preceding infection, HLA‐B27, uveitis, sacroiliitis on imaging – or two or more other parameters – arthritis, enthesitis, dactylitis, inflammatory back pain in the past, family history of SpA – can be classified as ‘peripheral SpA’. In the entire ASAS population of 975 patients, sensitivity and specificity of the combined use of the two sets of criteria for peripheral SpA were 79·5 and 83·3%, respectively 86. Tomero et al. analysed the performance of the ASAS criteria for the classification of SpA in early SpA clinics. The sensitivity and specificity of the ASAS criteria set were 65 and 93%, respectively, suggesting how these criteria are limited to detection of early SpA forms, especially in populations in which magnetic resonance imaging (MRI) is not routinely available or in populations with a low prevalence of HLA‐B27 87.
For the early diagnosis of axSpA, the Berlin diagnostic algorithm has been proposed in patients with IBP. This algorithm is completely based on the sensitivity and specificity of typical SpA features and considers the probability of SpA by calculating the likelihood ratio‐product of SpA features for each patient. Although the algorithm consists of different steps, the presence of IBP is mandatory. It means that this algorithm is not helpful in the detection of the disease in patients with axSpA but without IBP 85, 91. For this reason, Van der Berg et al. validated a modified algorithm for diagnosing axSpA in which IBP is excluded as obligatory entry criterion and added as an SpA feature 80.
Although such scarce data represent an important limitation for any possible evidence‐based recommendation, the appropriateness of each red flag was assessed by expert opinion and expressed and quantified using the RAND/UCLA method 11. After the two rounds of the online survey, there was no disagreement among the participants. However, the interspecialist referral was judged as always appropriate for some red flags and possibly appropriate for others, leading to their classification as ‘major’ or ‘minor’ criteria, respectively. In fact, the establishment of some rules for referral may avoid diagnostic delay, improve quality of care and decrease the possibility of complications, but it is also fundamental to avoid clinic overflow with unnecessary referrals and the possible consequent increase of health‐care costs. In this regard, we recognize as a limitation of this study the inclusion of some general symptoms in the list of red flags: in particular, our definition of low back pain intentionally excluded any inflammatory characteristic (such as onset before the age of 45, morning stiffness, pain relieved by movements), as well as peripheral joint pain without swelling. However, patients should be referred to the rheumatologist only when these symptoms recur or last for at least 3 months (Table 1). In fact, IBD patients with back/joint pain have a significantly lower quality of life and work productivity 88, therefore these symptoms, when persistent, are worthy of referral to a rheumatologist, regardless of the presence of articular inflammation.
During the last meeting, it was established that at least three minor criteria are required for specialist referral. However, most of the participants argued that some minor red flags have different importance in clinical practice. For example, the family history of IBD is not enough to refer a patient with SpA to the gastroenterologist, but it should be considered more clinically relevant than isolated fever or oral aphthosis; in this case, non‐invasive tests such as fecal calprotectin or bowel ultrasound may be indicated to investigate the presence of intestinal inflammation, with subsequent referral to the gastroenterologist only in the case of altered test results.
Similar considerations emerged from minor criteria for rheumatological referral. Non‐infectious anterior uveitis, confirmed by the ophthalmologist, may be itself an extra‐intestinal manifestation in patients with IBD, regardless of the presence of SpA, and thus should be considered with more caution in comparison with family history of SpA or chest pain.
The strength of our project was the joint involvement of rheumatologists and gastroenterologists in the management of patients with both diseases, and a structured method to collect expert opinion. The main limitation is the lack of reliable evidence to elaborate a solid decision strategy: prospective and multi‐centre studies are needed to formally validate these symptoms and signs as diagnostic tools and to combine individual red flags into a ‘diagnostic score’. Moreover, the participants in our project came from an Italian setting only; the appropriateness of these criteria may be different in other populations and health‐care systems. In this regard, a Spanish study has been published recently, describing some major or minor criteria for diagnosis of SpA or IBD 92: the results differ slightly from ours. However, this confirms the need for a shared strategy to diagnose such complicated diseases early.
In conclusion, our study suggests that several signs and symptoms should be closely monitored to improve the clinical management of patients with a suspected association of IBD and SpA. Prospective validation of these red flags is necessary before their routine use in clinical practice.
Author contributions
C. F. and P. L. performed the literature review. L. S. performed the statistical analysis. C. F., P. L. and L. S. wrote the manuscript. E. L., F. C., F.Cast., P. G., A. O., C. S., R. S., M. V., I. O. and A. A. are members of the steering committee of the Italian SpA‐IBD Expert Panel Group and critically reviewed the manuscript. All authors approved the final version of the manuscript.
Dedication
We remember with fondness Professor Ignazio Olivieri for his professionalism and compassion.
Disclosures
C. F. has served as a consultant or advisory member for AbbVie and MSD. F. Cast. has served as a consultant or advisory member for AbbVie, Ferring, Janssen, MSD, Sofar and Takeda. P. G. received honoraria or consultation fees from Janssen, Abbvie, Pfizer, Celgene, Takeda, Ferring, MSD, Alfa Wasserman and Amgen; and participated in a company‐sponsored speaker's bureau for Abbvie, Janssen, Takeda, Ferring, Msd, Sofar and Chiesi. A. O. served as advisory board member for AbbVie, Janssen‐Cilag, MSD, Pfizer and Takeda Pharmaceuticals, and received lecture grants from AbbVie, Chiesi, Janssen‐Cilag, MSD, Sofar and Takeda Pharmaceuticals. M. V. participated in the Advisory Board and received lecture fees or support for research from MSD, Hospira, Mundipaharma, Takeda, Abbvie, Chiesi, Zambon, Amgen, Biogen, Jannsen, Pfizer, Sofar and Giuliani. A. A. has served as a consultant or advisory member for AbbVie, Allergan, Amgen, Biogen, Celgene, Celltrion, Ferring, Hospira, Janssen, Lilly, MSD, Mundipharma, Pfizer, Samsung Bioepis, Sofar and Takeda, has received lecture fees from AbbVie, AstraZeneca, Chiesi, Ferring, Hospira, Medtronic, MSD, Mitsubishi Tanabe, Mundipharma, Nikkiso, Otsuka, Pfizer, Samsung Bioepis, Takeda, Tigenix, and Zambon, and has received research funding from MSD and Takeda. All other authors have no conflicts of interest to declare.
Supporting information
Fig. S1. Flowchart of study selection for diagnostic accuracy of gastrointestinal red flags.
Fig. S2. Flowchart of study selection for diagnostic accuracy of rheumatologic red flags.
Acknowledgements
Funding of the project was provided by an unrestricted contribution from MSD Italia Srl. The funding source had no role in selecting the participants, reviewing the literature, defining consensus statements, drafting or reviewing the paper, or in the decision to submit the manuscript. All views expressed are solely those of the authors. The authors thank Editamed Srl – Torino for technical support during all stages of this project and Chiara Formigoni, the medical librarian, for the help with the literature search.
Appendix 1.
Collaborators
Italian SpA‐IBD Expert Panel Group:
-
‐
Marina Beltrami, Department of Internal Medicine, Arcispedale Santa Maria Nuova‐IRCCS, Reggio Emilia, Italy
-
‐
Fabrizio Bossa, Division of Gastroenterology, ‘Casa Sollievo della Sofferenza’ Hospital, IRCCS, San Giovanni Rotondo, Foggia, Italy
-
‐
Francesco Costa, Gastroenterology Unit, Department of Gastroenterology, University of Pisa, Pisa, Italy
-
‐
Walter Fries, Inflammatory Bowel Disease Unit, A.O.U. Policlinico ‘G. Martino’, Messina, Italy
-
‐
Mauro Galeazzi, Department of Medical Sciences, Surgery and Neurosciences, Rheumatology Unit, University of Siena, Siena, Italy
-
‐
Roberto Giacomelli, Division of Rheumatology, Department of Biotechnological and Applied Clinical Science, University of L'Aquila, L'Aquila, Italy
-
‐
Giovanni Lapadula, Rheumatology Unit, Department of Emergency and Transplantation, University of Bari, Bari, Italy
-
‐
Nazzarena Malavolta, Departmental Program of Rheumatology, Cardio‐Thoraco‐Vascular Department, Azienda Ospedaliera Universitaria di Bologna, Bologna, Italy
-
‐
Mariabeatrice Principi, Gastroenterology Unit, Department of Emergency and Organ Transplantation (D.E.T.O.), University of Bari, Italy
-
‐
Roberta Ramonda, Rheumatology Unit, Department of Medicine‐DIMED, University Hospital of Padova , Padova , Italy
-
‐
Gabriele Riegler, U.O.S.D. of Gastroenterology ‐ ‘Luigi Vanvitelli’ Campania University, Naples, Italy
-
‐
Giovanni Triolo, Rheumatology Section, Department of Internal Medicine, University of Palermo, Palermo. Italy
-
‐
Giorgio Zoli, Department of Internal Medicine, SS Annunziata Hospital, Cento, Ferrara, Italy
Contributor Information
A. Armuzzi, Email: alearmuzzi@yahoo.com.
the Italian SpA‐IBD Expert Panel Group:
Marina Beltrami, Fabrizio Bossa, Francesco Costa, Walter Fries, Mauro Galeazzi, Roberto Giacomelli, Giovanni Lapadula, Nazzarena Malavolta, Mariabeatrice Principi, Roberta Ramonda, Gabriele Riegler, Giovanni Triolo, and Giorgio Zoli
References
- 1. Orchard TR, Wordsworth BP, Jewell DP. Peripheral arthropathies in inflammatory bowel disease: their articular distribution and natural history. Gut 1998; 42:387–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Salvarani C, Vlachonikolis IG, van der Heijde DM et al Musculoskeletal manifestations in a population‐based cohort of inflammatory bowel disease patients. Scand J Gastroenterol 2001; 36:1307–13. [DOI] [PubMed] [Google Scholar]
- 3. Turkcapar N, Toruner M, Soykan I et al The prevalence of extraintestinal manifestations and HLA association in patients with inflammatory bowel disease. Rheumatol Int 2006; 26:663–8. [DOI] [PubMed] [Google Scholar]
- 4. van Erp SJ, Brakenhoff LK, van Gaalen FA et al Classifying back pain and peripheral joint complaints in inflammatory bowel disease patients: a prospective longitudinal follow‐up study. J Crohns Colitis 2016; 10:166–75. [DOI] [PubMed] [Google Scholar]
- 5. Stolwijk C, Pierik M, Landewe R, Masclee A, van Tubergen A. Prevalence of self‐reported spondyloarthritis features in a cohort of patients with inflammatory bowel disease. Can J Gastroenterol 2013; 27:199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Olivieri I, Cantini F, Castiglione F et al Italian Expert Panel on the management of patients with coexisting spondyloarthritis and inflammatory bowel disease. Autoimmun Rev 2014; 13:822–30. [DOI] [PubMed] [Google Scholar]
- 7. Armuzzi A, Felice C, Lubrano E et al Multidisciplinary management of patients with coexisting inflammatory bowel disease and spondyloarthritis: a Delphi consensus among Italian experts. Dig Liver Dis 2017; 49:1298–305. [DOI] [PubMed] [Google Scholar]
- 8. Danese S, Fiorino G, Mary JY et al Development of red flags index for early referral of adults with symptoms and signs suggestive of Crohn's disease: an IOIBD initiative. J Crohns Colitis 2015; 9:601–6. [DOI] [PubMed] [Google Scholar]
- 9. Di Carlo M, Luchetti MM, Benfaremo D et al The DETection of Arthritis in Inflammatory boweL diseases (DETAIL) questionnaire: development and preliminary testing of a new tool to screen patients with inflammatory bowel disease for the presence of spondyloarthritis. Clin Rheumatol 2018; 37:1037–1077. [DOI] [PubMed] [Google Scholar]
- 10. Schunemann HJ, Oxman AD, Brozek J et al Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ 2008; 336:1106–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fitch K, Bernstein SJ, Aguilar MD et al The RAND/UCLA appropriateness method user's manual. Santa Monica, CA: RAND Corporation; 2001. [Google Scholar]
- 12. Brook RH, Chassin MR, Fink A, Solomon DH, Kosecoff J, Park RE. A method for the detailed assessment of the appropriateness of medical technologies. Int J Technol Assess Health Care 1986; 2:53–63. [DOI] [PubMed] [Google Scholar]
- 13. Park RE, Fink A, Brook RH et al Physician ratings of appropriate indications for six medical and surgical procedures. Am J Public Health 1986; 76:766–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Al‐Jarallah K, Shehab D, Al‐Attiyah R et al Antibodies to mutated citrullinated vimentin and anti‐cyclic citrullinated peptide antibodies in inflammatory bowel disease and related arthritis. Inflamm Bowel Dis 2012; 18:1655–62. [DOI] [PubMed] [Google Scholar]
- 15. Bandinelli F, Terenzi R, Giovannini L et al Occult radiological sacroiliac abnormalities in patients with inflammatory bowel disease who do not present signs or symptoms of axial spondylitis. Clin Exp Rheumatol 2014; 32:949–52. [PubMed] [Google Scholar]
- 16. Bandyopadhyay D, Bandyopadhyay S, Ghosh P et al Extraintestinal manifestations in inflammatory bowel disease: prevalence and predictors in Indian patients. Ind J Gastroenterol 2015; 34:387–94. [DOI] [PubMed] [Google Scholar]
- 17. Bardazzi G, Mannoni A, d'Albasio G et al Spondyloarthritis in patients with ulcerative colitis. Ital J Gastroenterol Hepatol 1997; 29:520–4. [PubMed] [Google Scholar]
- 18. Barreiro‐De Acosta M, Enrique Domínguez‐Muñoz J, Concepcion Núñez‐Pardo De Vera et al. Relationship between clinical features of Crohn's disease and the risk of developing extraintestinal manifestations. Eur J Gastro Hepatol 2007; 19:73–8. [DOI] [PubMed] [Google Scholar]
- 19. Bernstein CN, Blanchard JF, Rawsthorne P, Yu N. The prevalence of extraintestinal diseases in inflammatory bowel disease: a population‐based study. Am J Gastroenterol 2001; 96:1116–22. [DOI] [PubMed] [Google Scholar]
- 20. Beslek A, Onen F, Birlik M et al Prevalence of spondyloarthritis in Turkish patients with inflammatory bowel disease. Rheumatol Int 2009; 29:955–7. [DOI] [PubMed] [Google Scholar]
- 21. Bhat M, Nguyen GC, Pare P et al Phenotypic and genotypic characteristics of inflammatory bowel disease in French Canadians: comparison with a large North American repository. Am J Gastroenterol 2009; 104:2233–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bruining DH, Siddiki HA, Fletcher JG, Tremaine WJ, Sandborn WJ, Loftus EV Jr. Prevalence of penetrating disease and extraintestinal manifestations of Crohn's disease detected with CT enterography. Inflamm Bowel Dis 2008; 14:1701–6. [DOI] [PubMed] [Google Scholar]
- 23. Christodoulou DK, Katsanos KH, Kitsanou M, Stergiopoulou C, Hatzis J, Tsianos EV. Frequency of extraintestinal manifestations in patients with inflammatory bowel disease in Northwest Greece and review of the literature. Dig Liver Dis 2002; 34:781–6. [DOI] [PubMed] [Google Scholar]
- 24. D'Inca R, Podswiadek M, Ferronato A, Punzi L, Salvagnini M, Sturniolo GC. Articular manifestations in inflammatory bowel disease patients: a prospective study. Dig Liver Dis 2009; 41:565–9. [DOI] [PubMed] [Google Scholar]
- 25. Dekker‐Saeys BJ, Meuwissen SG, Van Den Berg‐Loonen EM, De Haas WH, Agenant D, Tytgat GN. Ankylosing spondylitis and inflammatory bowel disease. II. Prevalence of peripheral arthritis, sacroiliitis, and ankylosing spondylitis in patients suffering from inflammatory bowel disease. Ann Rheum Dis 1978; 37:33–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hyla JF, Franck WA, Davis JS. Lack of association of HLA B27 with radiographic sacroiliitis in inflammatory bowel disease. J Rheumatol 1976; 3:196–200. [PubMed] [Google Scholar]
- 27. Jalan KN, Prescott RJ, Walker RJ, Sircus W, McManus JP, Card WI. Arthropathy, ankylosing spondylitis, and clubbing of fingers in ulcerative colitis. Gut 1970; 11:748–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Karreman MC, Luime JJ, Hazes JMW, Weel AEAM. The prevalence and incidence of axial and peripheral spondyloarthritis in inflammatory bowel disease: a systematic review and meta‐analysis. J Crohns Colitis 2017;11:631–42. [DOI] [PubMed] [Google Scholar]
- 29. Kochhar R, Mehta SK, Nagi B, Bhatia V, Goenka MK, Malik AK. Extraintestinal manifestations of idiopathic ulcerative colitis. Ind J Gastroenterol 1991; 10:88–9. [PubMed] [Google Scholar]
- 30. Lanna CCD, Ferrari et al. A cross‐sectional study of 130 Brazilian patients with Crohn's disease and ulcerative colitis: analysis of articular and ophthalmologic manifestations. Clin Rheumatol 2008; 27:503–9. [DOI] [PubMed] [Google Scholar]
- 31. Leclerc‐Jacob S, Lux G, Rat AC et al The prevalence of inflammatory sacroiliitis assessed on magnetic resonance imaging of inflammatory bowel disease: a retrospective study performed on 186 patients. Aliment Pharmacol Ther 2014; 39:957–62. [DOI] [PubMed] [Google Scholar]
- 32. Liu S, Ding J, Wang M, Zhou W, Feng M, Guan W. Clinical features of Crohn disease concomitant with ankylosing spondylitis: a preliminary single‐center study. Medicine 2016; 95:e4267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. McEniff N, Eustace S, McCarthy C, O'Malley M, O'Morain CA, Hamilton S. Asymptomatic sacroiliitis in inflammatory bowel disease. Assessment by computed tomography. Clin Imaging 1995; 19:258–62. [DOI] [PubMed] [Google Scholar]
- 34. Mocelin V, Nisihara RM, Utiyama SRR, Kotze LMS, Ramos O, Messias‐Reason I. Anti‐CCP antibodies and rheumatological findings in Brazilian patients with Crohn's disease. Digestion 2015; 91:303–6. [DOI] [PubMed] [Google Scholar]
- 35. Modena V, Amoroso A, Frattasio C et al HLA antigens and clinical manifestations in Crohn's disease. Clin Exp Rheumatol 1988; 6:221–5. [PubMed] [Google Scholar]
- 36. Münch H, Purrmann J, Reis HE et al Clinical features of inflammatory joint and spine manifestations in Crohn's disease. Hepatogastroenterology 1986; 33:123–7. [PubMed] [Google Scholar]
- 37. Orchard TR, Holt H, Bradbury L et al The prevalence, clinical features and association of HLA‐B27 in sacroiliitis associated with established Crohn's disease. Aliment Pharmacol Ther 2009; 29:193–7. [DOI] [PubMed] [Google Scholar]
- 38. Palm O, Moum B, Ongre A, Gran JT. Prevalence of ankylosing spondylitis and other spondyloarthropathies among patients with inflammatory bowel disease: a population study (the IBSEN study). J Rheumatol 2002; 29:511–5. [PubMed] [Google Scholar]
- 39. Paparo F, Bacigalupo L, Garello I et al Crohn's disease: prevalence of intestinal and extraintestinal manifestations detected by computed tomography enterography with water enema. Abdom Imaging 2012; 37:326–37. [DOI] [PubMed] [Google Scholar]
- 40. Peeters H, Vander Cruyssen B, Laukens D et al Radiological sacroiliitis, a hallmark of spondylitis, is linked with CARD15 gene polymorphisms in patients with Crohn's disease. Ann Rheum Dis 2004; 63:1131–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Peeters H, Vander Cruyssen B, Mielants H et al Clinical and genetic factors associated with sacroiliitis in Crohn's disease. J Gastroenterol Hepatol 2008; 23:132–7. [DOI] [PubMed] [Google Scholar]
- 42. Pezerović D, Zulj M, Klarin I, Majnarić L, Vcev I, Vcev A. Clinical expression of inflammatory bowel diseases – a retrospective population‐based cohort study; Vukovarsko‐Srijemska County, Croatia, 2010. Coll Antropol 2013; 37:919–27. [PubMed] [Google Scholar]
- 43. Pokharna RK, Kabra PK, Sharma R, Kochar DK. Extraintestinal manifestations of idiopathic ulcerative colitis in northwestern India. Ind J Gastroenterol 2004; 23:89–90. [PubMed] [Google Scholar]
- 44. Queiro R, Maiz O, Intxausti J et al Subclinical sacroiliitis in inflammatory bowel disease: a clinical and follow‐up study. Clin Rheumatol 2000; 19:445–9. [DOI] [PubMed] [Google Scholar]
- 45. Rodriguez VE, Costas PJ, Vazquez M et al. Prevalence of spondyloarthropathy in Puerto Rican patients with inflammatory bowel disease. Ethn Dis 2008; 18:S2–225‐9. [PubMed] [Google Scholar]
- 46. Scarpa R, del Puente A, D'Arienzo A et al The arthritis of ulcerative colitis: clinical and genetic aspects. J Rheumatol 1992; 19:373–7. [PubMed] [Google Scholar]
- 47. Scott WW, Fishman EK, Kuhlman JE et al Computed tomography evaluation of the sacroiliac joints in Crohn disease. Radiologic/clinical correlation. Skeletal Radiol 1990; 19:207–10. [DOI] [PubMed] [Google Scholar]
- 48. de Vlam K, Mielants H, Cuvelier C, De Keyser F, Veys EM, De Vos M. Spondyloarthropathy is underestimated in inflammatory bowel disease: prevalence and HLA association. J Rheumatol 2000; 27:2860–5. [PubMed] [Google Scholar]
- 49. Sofia MA, Rubin DT, Hou N, Pekow J. Clinical presentation and disease course of inflammatory bowel disease differs by race in a large tertiary care hospital. Dig Dis Sci 2014; 59:2228–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Steer S, Jones H, Hibbert J et al Low back pain, sacroiliitis, and the relationship with HLA‐B27 in Crohn's disease. J Rheumatol 2003; 30:518–22. [PubMed] [Google Scholar]
- 51. Suh CH, Lee CH, Lee J et al Arthritic manifestations of inflammatory bowel disease. J Korean Med Sci 1998; 13:39–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sung JJ, Hsu RK, Chan FK, Liew CT, Lau JW, Li AK. Crohn's disease in the Chinese population. An experience from Hong Kong. Dis Colon Rectum 1994; 37:1307–9. [DOI] [PubMed] [Google Scholar]
- 53. Vavricka SR, Brun L, Ballabeni P et al Frequency and risk factors for extraintestinal manifestations in the Swiss inflammatory bowel disease cohort. Am J Gastroenterol 2011; 106:110–9. [DOI] [PubMed] [Google Scholar]
- 54. Vavricka SR, Rogler G, Gantenbein C et al Chronological order of appearance of extraintestinal manifestations relative to the time of IBD diagnosis in the Swiss inflammatory bowel disease cohort. Inflamm Bowel Dis 2015; 21:1794–800. [DOI] [PubMed] [Google Scholar]
- 55. Yi F, Chen M, Huang M et al The trend in newly diagnosed Crohn's disease and extraintestinal manifestations of Crohn's disease in central China: a retrospective study of a single center. Eur J Gastro Hepatol 2012; 24:1424–9. [DOI] [PubMed] [Google Scholar]
- 56. Bakland G, Nossent HC, Gran JT. Incidence and prevalence of ankylosing spondylitis in Northern Norway. Arthritis Rheum 2005; 53:850–5. [DOI] [PubMed] [Google Scholar]
- 57. Buschiazzo E, Maldonado‐Cocco JA, Arturi P et al Epidemiology of spondyloarthritis in Argentina. Am J Med Sci 2011; 341:289–92. [DOI] [PubMed] [Google Scholar]
- 58. Collantes E, Zarco P, Muñoz E et al Disease pattern of spondyloarthropathies in Spain: description of the first national registry (REGISPONSER) extended report. Rheumatology (Oxf) 2007; 46:1309–15. [DOI] [PubMed] [Google Scholar]
- 59. Costello PB, Alea JA, Kennedy AC, McCluskey RT, Green FA. Prevalence of occult inflammatory bowel disease in ankylosing spondylitis. Ann Rheum Dis 1980; 39:453–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Dean LE, Macfarlane GJ, Jones GT. Differences in the prevalence of ankylosing spondylitis in primary and secondary care: only one‐third of patients are managed in rheumatology. Rheumatology (Oxf) 2016; 55:1820–5. [DOI] [PubMed] [Google Scholar]
- 61. Deesomchok U, Tumrasvin T. Clinical study of Thai patients with ankylosing spondylitis. Clin Rheumatol 1985; 4:76–82. [DOI] [PubMed] [Google Scholar]
- 62. del Río‐Martínez P, Navarro‐Compán V, Díaz‐Miguel C et al Similarities and differences between patients fulfilling axial and peripheral ASAS criteria for spondyloarthritis: results from the Esperanza Cohort. Semin Arthritis Rheum 2016; 45:400–3. [DOI] [PubMed] [Google Scholar]
- 63. Dougados M, Etcheto A, Molto A et al Clinical presentation of patients suffering from recent onset chronic inflammatory back pain suggestive of spondyloarthritis: The DESIR cohort. Joint Bon, Spine 2015; 82:345–51. [DOI] [PubMed] [Google Scholar]
- 64. Edmunds L, Elswood J, Kennedy LG, Calin A. Primary ankylosing spondylitis, psoriatic and enteropathic spondyloarthropathy: a controlled analysis. J Rheumatol 1991; 18:696–8. [PubMed] [Google Scholar]
- 65. Eliakim R, Karban A, Markovits D et al Comparison of capsule endoscopy with ileocolonoscopy for detecting small‐bowel lesions in patients with seronegative spondyloarthropathies. Endoscopy 2005; 37:1165–9. [DOI] [PubMed] [Google Scholar]
- 66. Essers I, Ramiro S, Stolwijk C et al Characteristics associated with the presence and development of extra‐articular manifestations in ankylosing spondylitis: 12‐year results from OASIS. Rheumatology (Oxf) 2015; 54:633–40. [DOI] [PubMed] [Google Scholar]
- 67. García‐Vicuña R, Zarco P, González CM, Vanaclocha F, Marín‐Jiménez I, Cea‐Calvo L. Two‐year incidence of psoriasis, uveitis and inflammatory bowel disease in patients with spondyloarthritis: a study in the AQUILES cohort. Reumatologia Clinica 2016; 12:22–6. [DOI] [PubMed] [Google Scholar]
- 68. Mitulescu TC, Popescu C, Naie A et al Acute anterior uveitis and other extra‐articular manifestations of spondyloarthritis. J Med Life 2015; 8:319–25. [PMC free article] [PubMed] [Google Scholar]
- 69. Peluso R, Iervolino S, Vitiello M, Bruner V, Lupoli G, Di Minno MND. Extra‐articular manifestations in psoriatic arthritis patients. Clin Rheumatol 2015; 34:745–53. [DOI] [PubMed] [Google Scholar]
- 70. Pérez Alamino R, Maldonado Cocco JA, Citera G et al Differential features between primary ankylosing spondylitis and spondylitis associated with psoriasis and inflammatory bowel disease. J Rheumatol 2011; 38:1656–60. [DOI] [PubMed] [Google Scholar]
- 71. Rojas‐Vargas M, Muñoz‐Gomariz E, Escudero A et al First signs and symptoms of spondyloarthritis – data from an inception cohort with a disease course of two years or less (REGISPONSER‐Early). Rheumatology (Oxf) 2009; 48:404–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Roussou E, Sultana S. Early spondyloarthritis in multiracial society: differences between gender, race, and disease subgroups with regard to first symptom at presentation, main problem that the disease is causing to patients, and employment status. Rheumatol Int 2012; 32:1597–604. [DOI] [PubMed] [Google Scholar]
- 73. Rudwaleit M, van der Heijde D, Landewé R et al The assessment of SpondyloArthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis 2011; 70:25–31. [DOI] [PubMed] [Google Scholar]
- 74. Said‐Nahal R, Miceli‐Richard C, Berthelot JM et al The familial form of spondylarthropathy: a clinical study of 115 multiplex families. Groupe Français d'Etude Génétique des Spondylarthropathies. Arthritis Rheum 2000; 43:1356–65. [DOI] [PubMed] [Google Scholar]
- 75. Sampaio‐Barros PD. Epidemiology of spondyloarthritis in Brazil. Am J Med Sci 2011; 341:287–8. [DOI] [PubMed] [Google Scholar]
- 76. Stolwijk C, Essers I, van Tubergen A et al The epidemiology of extra‐articular manifestations in ankylosing spondylitis: a population‐based matched cohort study. Ann Rheum Dis 2015; 74:1373–8. [DOI] [PubMed] [Google Scholar]
- 77. Tayel MY, Soliman E, El Baz WF, El Labaan A, Hamaad Y, Ahmed MH. Registry of the clinical characteristics of spondyloarthritis in a cohort of Egyptian population. Rheumatol Int 2012; 32:2837–42. [DOI] [PubMed] [Google Scholar]
- 78. Ford AC, Moayyedi P, Bercik P et al Lack of utility of symptoms and signs at first presentation as predictors of inflammatory bowel disease in secondary care. Am J Gastroenterol 2015; 110:716–24. [DOI] [PubMed] [Google Scholar]
- 79. Lisciandrano D, Ranzi T, Carrassi A et al Prevalence of oral lesions in inflammatory bowel disease. Am J Gastroenterol 1996; 91:7–10. [PubMed] [Google Scholar]
- 80. van den Berg R, de Hooge M, Rudwaleit M et al ASAS modification of the Berlin algorithm for diagnosing axial spondyloarthritis: results from the SPondyloArthritis Caught Early (SPACE)‐cohort and from the Assessment of SpondyloArthritis international Society (ASAS)‐cohort. Ann Rheum Dis 2013; 72:1646–53. [DOI] [PubMed] [Google Scholar]
- 81. Sieper J, van der Heijde D, Landewe R et al New criteria for inflammatory back pain in patients with chronic back pain: a real patient exercise by experts from the Assessment of SpondyloArthritis international Society (ASAS). Ann Rheum Dis 2009; 68:784–8. [DOI] [PubMed] [Google Scholar]
- 82. Bakland G, Alsing R, Singh K, Nossent JC. Assessment of SpondyloArthritis International Society criteria for axial spondyloarthritis in chronic back pain patients with a high prevalence of HLA‐B27. Arthritis Care Res (Hoboken) 2013; 65:448–53. [DOI] [PubMed] [Google Scholar]
- 83. Hermann J, Giessauf H, Schaffler G, Ofner P, Graninger W. Early spondyloarthritis: usefulness of clinical screening. Rheumatology (Oxf) 2009; 48:812–6. [DOI] [PubMed] [Google Scholar]
- 84. Lin Z, Liao Z, Huang J et al Evaluation of Assessment of Spondyloarthritis International Society classification criteria for axial spondyloarthritis in Chinese patients with chronic back pain: results of a 2‐year follow‐up study. Int J Rheum Dis 2014; 17:782–9. [DOI] [PubMed] [Google Scholar]
- 85. Rudwaleit M, Landewe R, van der Heijde D et al The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal. Ann Rheum Dis 2009; 68:770–6. [DOI] [PubMed] [Google Scholar]
- 86. Rudwaleit M, van der Heijde D, Landewe R et al The Assessment of SpondyloArthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis 2011; 70:25–31. [DOI] [PubMed] [Google Scholar]
- 87. Tomero E, Mulero J, de Miguel E et al Performance of the Assessment of Spondyloarthritis International Society criteria for the classification of spondyloarthritis in early spondyloarthritis clinics participating in the ESPERANZA programme. Rheumatology (Oxf) 2014; 53:353–60. [DOI] [PubMed] [Google Scholar]
- 88. van der Have M, Brakenhoff LK, van Erp SJ et al Back/joint pain, illness perceptions and coping are important predictors of quality of life and work productivity in patients with inflammatory bowel disease: a 12‐month longitudinal study. J Crohns Colitis 2015; 9:276–83. [DOI] [PubMed] [Google Scholar]
- 89. O'Toole A, Lucci M, Korzenik J. Inflammatory Bowel disease provoked by Etanercept: report of 443 possible cases combined from an IBD referral center and the FDA. Dig Dis Sci 2016; 61:1772–4. [DOI] [PubMed] [Google Scholar]
- 90. Whitehead WE. The Validation Working Team Committee in association with the Rome Questionnaire C. Development and validation of the Rome III diagnostic questionnaire. In: III. DDAeR, ed. Funct Gastrointest Dis 2006:835‐53. [Google Scholar]
- 91. Rudwaleit M, van der Heijde D, Khan MA, Braun J, Sieper J. How to diagnose axial spondyloarthritis early. Ann Rheum Dis 2004; 63:535–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Sanz Sanz J, Juanola Roura et al Screening of inflammatory bowel disease and spondyloarthritis for referring patients between rheumatology and gastroenterology. Gastroenterol Hepatol 2018; 41:54–62. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig. S1. Flowchart of study selection for diagnostic accuracy of gastrointestinal red flags.
Fig. S2. Flowchart of study selection for diagnostic accuracy of rheumatologic red flags.


