Abstract
Chronic inflammation is one of the most evident and common pathological conditions leading to deregulated osteoclastogenesis and bone remodeling. Tumor necrosis factor (TNF) as a pleiotropic cytokine plays a key role, not only in inflammation, but also in bone erosion in diseases associated with bone loss. TNF can stimulate the proliferation of osteoclast precursors and, in most conditions, act together with other cytokines and growth factors such as receptor activator of nuclear factor (NF)-[kappa]B ligand (RANKL), interleukin-6, and transforming growth factor beta to synergistically promote osteoclast formation and bone resorption in vivo. A longstanding enigma in the field is why TNF alone is not able to induce osteoclast differentiation as effectively as the same superfamily member RANKL, a physiological master osteoclastogenic cytokine. Recent studies have highlighted several lines of evidence showing the intrinsic mechanisms through RBP-J, NF-[kappa]B p100/TNF receptor-associated factor 3, or interferon regulatory factor-8 that restrain TNF-induced osteoclast differentiation and bone resorption. These feedback inhibitory mechanisms driven by TNF shed light into the current paradigm of osteoclastogenesis and would provide novel therapeutic implications on controlling inflammatory bone resorption.
Keywords: TNF, osteoclasts, bone resorption, inflammation
I. INTRODUCTION
Osteoimmunology is an emerging interdisciplinary field linking immunology and bone biology. Recent studies from the osteoimmunology field highlight the important roles of the immune system in the regulation of bone homeostasis in both physiological and pathological conditions.1–5 The adult skeleton undergoes constant and dynamic remodeling in order to maintain a healthy bone mass that is appropriately regulated by osteoclast-mediated bone resorption and associated osteoblast/osteocyte-mediated bone formation.6–8 Osteoclasts, derived from monocyte/macrophage precursors, are the exclusive cell type responsible for bone resorption. Osteoclast differentiation is effectively induced by the major osteoclastogenic cytokine receptor activator of nuclear factor (NF)-[kappa]B ligand (RANKL), which acts in concert with macrophage colony-stimulating factor (M-CSF) and immunoreceptor tyrosine-based activation motif (ITAM)-mediated co-stimulatory signals. Binding of RANKL to its receptor RANK activates a broad range of signaling cascades, including canonical and non-canonical NF-[kappa]B pathways, mitogen-activated kinase pathways leading to the activation of AP-1 and CREB transcription factors, and calcium signaling, to induce the expression of key transcription factors Blimp1 and NFATc1 for osteoclast differentiation.9–13 Chronic inflammation such as that occurs in rheumatoid arthritis, periodontitis, and periprosthetic osteolysis is one of the most common pathological conditions associated with excessive bone resorption. In these diseases, abnormally enhanced generation and/or function of osteoclasts results in inflammatory bone erosion.14–17
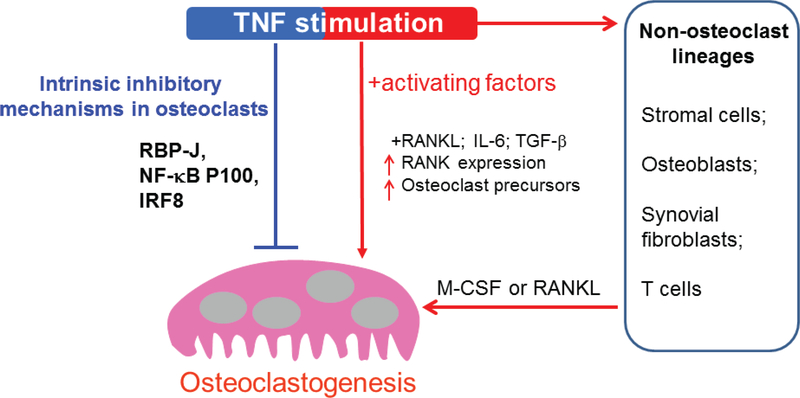
Tumor necrosis factor (TNF) is a pleiotropic cytokine important for immunity and inflammation. In addition to driving chronic inflammation, TNF plays a key role in inflammatory bone destruction observed in inflammatory arthritis, periodontitis, and periprosthetic osteolysis. The importance of TNF in the pathogenesis of rheumatoid arthritis and the resounding success of TNF blockade therapy in the treatment of rheumatoid arthritis and its associated bone erosion provide clinical evidence that TNF promotes pathologic bone resorption. Interestingly, however, compared with RANKL, TNF alone does not effectively induce osteoclast precursors to differentiate to osteoclasts directly, which has been demonstrated by both genetic evidence and osteoclastogenesis in human CD14-positive cells.18–20 TNF acts directly on osteoclast precursors, mostly in synergy with RANKL, to promote pathologic osteoclastogenesis and bone resorption.16–17,21–26 TNF may function in vivo to increase osteoclast precursors.27–30 In certain circumstances, transforming growth factor-beta may prime osteoclast precursors, which potentiates TNF to induce osteoclast differentiation.24 Other than the direct effects on osteoclast linage, TNF executes their indirect osteoclastogenic effect through augmentation of RANK expression on osteoclast precursors, M-CSF, and RANKL expression in stromal cells such as osteoblasts and synovial fibroblasts16,31–32 (Fig. 1).
FIG. 1:
Model showing a dual role of TNF in osteoclastogenesis. TNF can stimulate proliferation of osteoclast precursors, increase RANK expression, and in most conditions act together with other cytokines and growth factors such as RANKL, IL-6, and TGF-β to synergistically promote osteoclast formation and bone resorption in vivo. TNF also indirectly promotes osteoclastogenesis by targeting other cell populations such as osteoblastic/stromal cells, synovial cells, and T-cells by stimulating M-CSF or RANKL production from these cells. Recent studies have highlighted several lines of evidence showing that TNF restrains osteoclastogenesis through intrinsic feedback mechanisms such as via RBP-J, NF-[kappa]B p100/TRAF3, or IRF-8.
TNF and RANKL belong to the same TNF super family, but their osteoclastogenic capacity differs drastically. The intrinsic mechanisms that restrain TNF-induced osteoclastogenesis are much less understood than those that promote osteoclastogenesis in response to RANKL. In this review, we focus on and highlight recent discoveries (Fig. 1) by our group and others of several key feedback mechanisms that control the direct osteoclastogenic properties of TNF.33–36
II. RBP-J
RBP-J was originally identified as a master transcription factor in the canonical Notch signaling pathway,37 in which the Notch intracellular domains translocate to the nucleus after activation by Notch ligands, bind to RBP-J, and induce RBP-J-mediated transcriptional activation of Notch target genes such as Hes1 and Hey1. Accumulating evidence recently showed that RBP-J also functions as a critical transcriptional regulator in many other signaling pathways, such as the TNF,34 Toll-like receptor (TLR),38–39 Wnt-β-catenin,40 NF-[kappa]B,41–42 TAK1,43 and ITAM signaling pathways,35 and is also targeted by viral proteins42,44 and cellular proteins of unknown function.45–46 Therefore, RBP-J is a central transcription factor that receives inputs from various signaling pathways. Most cell types express a basic level of RBP-J that acts as either a transcriptional repressor or activator depending on the partner proteins with which it interacts.37 RBP-J regulates cell proliferation, differentiation, cell fate decisions, and diverse cellular functions, including neurogenesis, stem cell maintenance, and lymphocyte development.37,47 In myeloid lineage cells, RBP-J has been implicated in inflammatory macrophage activation and function,38–39,48 dendritic cell (DC) differentiation, and maintenance of CD8− DC populations.49–50 Although many of these functions are related to its role in Notch signaling, RBP-J function is context dependent and, under inflammatory conditions, RBP-J plays a key role in expression of immune response genes unrelated to canonical Notch signaling.39
We found that RBP-J expression level was suppressed in the synovial fluid macrophages isolated from rheumatoid arthritis (RA) patients, supporting a pathological relevance of RBP-J to RA. Indeed, RBP-J allelic variants have been linked with RA.51–52 The synovial fluid macrophages can function as osteoclast precursors. However, the role of RBP-J signaling in pathological osteoclastogenesis and bone resorption is not well understood. Notch-RBP-J signaling in osteoclasts plays a minor role in homeostatic bone resorption based on genetic evidence that mice with a myeloid-specific deletion of RBP-J (RBP-Jf/f LysM-Cre), deletion of Notch 1/2/3, or constitutively active NICD1 expression in the myeloid compartment (NICD1M) do not exhibit significant bone defects under physiological conditions.34,53 Consistent with these phenotypes, RBP-J modestly suppresses RANKL-induced osteoclastogenesis in vitro.34,54 In striking contrast, myeloid-specific deletion of RBP-J driven by LysMCre dramatically increases TNF-induced osteoclast differentiation to a level comparable to that induced by RANKL in control cells.34 Furthermore, this enhanced osteoclastogenesis leads to severe bone destruction in a TNF-induced inflammatory bone resorption model. TNF is able to induce osteoclast differentiation and inflammatory bone resorption in RBP-J-deficient cells and mice even in the absence of RANK signaling. Therefore, RBP-J deletion reveals the full osteoclastogenic potential of TNF. Complementary evidence shows that forced activation of RBP-J suppresses inflammatory arthritic bone resorption. Mechanistically, RBP-J suppresses NFATc1 transcription by attenuating c-Fos activation and Blimp1 induction, thereby preventing the downregulation of the transcriptional repressor IFN regulatory factor-8 (IRF-8) that blocks osteoclast differentiation.34 These studies shed insight into a poorly characterized field, in which RBP-J functions as a critical transcriptional repressor to suppress inflammatory and TNF-mediated osteoclastogenesis and bone resorption.
Our results revealed a predominant role of RBP-J in suppressing TNF-induced osteoclastogenesis compared with that induced by RANKL. Subsequent studies found an important clue for the relatively modest regulation of RANKL-induced osteoclastogenesis by RBP-J, which is likely attributed to the endogenously presence of ITAM-mediated calcium signaling.35 The ITAM-mediated signaling pathways play important roles in various cellular activities, including immune response and cancer activation. The main ITAM-containing adaptors expressed by myeloid osteoclast precursors are DNAX-activating protein 12 (DAP12) and Fc receptor common γ subunit (FcRγ). These adaptors associate with and mediate signaling by various receptors, including DAP12-associated triggering receptor expressed in myeloid cells 2 (TREM2) and signal-regulatory protein β 1 (SIRPβ1), FcRγ-associated osteoclastassociated receptor (OSCAR), paired immunoglobulin-like receptor-A (PIR-A) and FcRs. Osteoclasts require ITAM-mediated co-stimulation of RANK signaling for their appropriate differentiation during bone homeostasis.55 RBP-J deficiency almost completely reverses the defects of osteoclast differentiation program and significantly rescues the osteopetrotic bone phenotype of Dap12 knockout (KO) or Dap12/Fcrg double-KO mice by bypassing the requirement for costimulation of osteoclastogenesis during bone homeostasis.35 In inflammatory conditions, RBP-J restrains ITAM signaling and limits cross-talk between RANK or TNFR- and ITAM-associated receptors by suppressing PLCγ2 expression and keeping PLCγ2-calcium signaling in a repressed basal state. RBP-J deficiency enables TNF to induce osteoclast formation and bone resorption in Dap12 KO mice.35 These data show that RBP-J deficiency allows osteoclast differentiation to occur independently of ITAM-mediated costimulation during homeostatic bone remodeling and inflammatory bone destruction. Therefore, RBP-J imposes the requirement for ITAM-mediated co-stimulation. Our data suggests a model in which the balance between ITAM-mediated induction and RBP-J-mediated suppression determines the level of basal PLCγ2/calcium signaling, which further determines whether stimulation of osteoclast precursors with factors such as RANKL or TNF induces sufficient calcium signaling to cross the threshold required to effectively induce osteoclast differentiation.
These studies provided an important inhibitory mechanism mediated by RBP-J that can at least partially to explain the longstanding enigma in the field of why TNF alone is not able to induce osteoclast differentiation as effectively as the same superfamily member RANKL. The balance between the activating and inhibitory pathways fine tunes osteoclastogenesis and determines the strength of activating signals required for osteoclastogenesis in physiological and pathological settings. The expression and function of RBP-J can be altered in response to environmental cues in pathological states. For example, RBP-J expression level was significantly decreased in synovial fluid macrophages derived from RA patients.35 The lower RBP-J level could contribute to the excessive osteoclastic bone resorption in RA.
A question plaguing the field is whether upstream Notch signaling plays a similar role as RBP-J in controlling TNF-mediated osteoclastogenesis. Interestingly, deficiency of Notch1/2/3 or ADAM metallopeptidase domain 10 (ADAM10) in osteoclast precursors does not promote TNF-induced osteoclastogenesis (author’s unpublished data), suggesting that the canonical Notch-mediated osteoclastogenesis does not recapitulate RBP-J-suppressed osteoclastogenesis in response to TNF signaling. The pan inhibition of canonical Notch signaling may compromise the function of each specific Notch receptor. Although we cannot exclude the possibility that specific individual Notch receptors may function upstream of RBP-J to inhibit TNF-induced osteoclastogenesis, RBP-J may also act in a Notch-independent manner in this scenario. Furthermore, we did not find that TNF was able to induce osteoclast differentiation in the Hes1- and/or Hey1-deficient osteoclast precursors (author’s unpublished data). This suggests that the targets of RBP-J other than the canonical Notch targets presumably control the negative regulation of TNF-induced osteoclastogenesis. Indeed, modern genome-wide analysis using RBP-J or NICD chromatin immunoprecipitation sequencing identifies a distinct set of sites where RBP-J recruits neither NICD nor Histone acetyltransferase p300 and binds DNA statically irrespective of Notch activity.56–58 These findings significantly modify the current paradigm of canonical Notch/RBP-J signaling pathway and provide genomic evidence of a Notch-independent RBP-J signaling pathway. Appropriate manipulation of RBP-J activity in inflammatory arthritis mouse models has a significant impact on bone, but no discernable effects on TNF-mediated inflammation,34,59 suggesting a possibility of selective control of RBP-J activity in inflammatory bone destruction without affecting inflammation induced by TNF. Identification of RBP-J targets induced by TNF would provide a selective therapeutic strategy to prevent TNF-mediated bone resorption associated with inflammatory diseases without a significant impact on physiological bone remodeling.
III. NF-[KAPPA]B P100 AND TRAF3
The NF-[kappa]B family is comprised of RelA (p65), RelB, c-Rel, NF-[kappa]B1 (p50 and its precursor p105), and NF-[kappa]B2 (p52 and its precursor p100). NF-[kappa]B activation is induced by two major signaling pathways; the classical pathway mainly involves IKKβ-induced I[kappa]Bα degradation and subsequent RelA/p50 activation and the alternative pathway involves NIK-induced p100 processing to p52 and RelB/p52 activation. RelB is not only required for RANKL-induced osteoclast maturation, but is also important for TNF-induced bone resorption.60 Activation of IKKβ is sufficient for RANK-independent osteoclast differentiation and osteolysis.61 There are cross-talks between these two pathways and NF-[kappa]B activation from these two pathways plays important positive roles in inducing osteoclastogenesis.9,60,62–63 Conversely, clear evidence shows that NF-[kappa]B p100 functions as a negative regulator of osteoclastogenesis by binding to NF-[kappa]B complexes and preventing their nuclear translocation. Cytosolic accumulation of p100 impairs osteoclastogenesis, whereas p100 deficiency leads to enhanced osteoclastogenesis that contributes to an osteopenic phenotype in vivo.60,62–65 TNF does not seem to activate the alternative NF-[kappa]B pathway as efficiently as RANKL because it induces an accumulation of p100 in osteoclast precursors via induction of TRAF3, thus limiting TNF-induced osteoclastogenesis.64 TNF-Tg mice lacking NF-[kappa]B p100 exhibit more severe joint erosion than do their TNF-Tg littermates.64 These data suggest that inhibition of NF-[kappa]B p100 processing may represent a novel therapeutic strategy for inflammatory bone loss such as that occurs in RA, periodontitis, or periprosthetic osteolysis.
IV. IRF-8
In addition to activating positive signaling pathways, RANKL needs to overcome the “brakes” imposed on osteoclast differentiation by transcriptional repressors that include inhibitors of differentiation/DNA binding (Ids),49,66 Eos,27 v-maf musculoaponeurotic fibrosarcoma oncogene family protein B (MafB),67 IRF-8,36 and B-cell lymphoma 6 (Bcl6).68 Among these transcriptional repressors, IRF-8 deficiency dramatically promotes TNF-induced osteoclastogenesis and results in increased NFATc1 expression, indicating that IRF-8 has a suppressive role in TNF-induced osteoclastogenesis. IRF-8 deficiency also significantly attenuates TLR-induced inhibition of osteoclastogenesis, suggesting that IRF-8 plays an important part in the inhibitory mechanisms of TLRs. In a lipopolysaccharide-induced inflammatory bone resorption model, IRF-8-deficient mice exhibit enhanced osteoclast formation and more dramatic bone destruction than their wild-type littermates. These data indicate that this homeostatic role of IRF-8 may be important to limit bone resorption during acute infections and also in chronic inflammatory conditions such as RA. Identification of signaling pathways, additional factors, and mechanisms that regulate IRF-8 expression and function represents a promising approach to control inflammatory bone loss. The mechanisms by which the expression of these repressors is downregulated are largely unknown. Recently, inspiring studies highlighted novel epigenetic regulatory mechanisms that control IRF-8 downregulation,69–70 which moved the field one step ahead. Epigenetic regulation is universal in cellular processes that require transcription dynamics and genetic stability. Epigenetic modifications contribute to regulation of gene expression by transcriptional activation or repression. There are two main types of epigenetic modulation: DNA methylations such as via de novo DNA methyltransferase (DNMTs) DNMT3a and DNMT3b and histone post-translational modifications (histone tail modifications) such as acetylation, methylation, phosphorylation, ubiquitylation, and sumoylation of histones. Epigenetic repressors generally include DNMTs, histone deacetylases (HDACs) and polycomb group proteins (PcGs). Epigenetic repression of IRF-8 by Dnmt3a-mediated DNA hypermethylation leads to decreased IRF-8 expression and enhanced osteoclastogenesis and bone resorption.69 Our group found that EZH2 directly silences IRF-8 expression.70 EZH2 is the catalytic subunit of polycomb repressive complex 2 (PRC2) that catalyzes the addition of methyl groups to lysine 27 of histone 3 (H3K27me). EZH2 binds to the IRF-8 promoter and induces the transcriptional repressor marker H3K27me3 at the IRF-8 locus in response to RANKL.70 There are functional links among PRC2, HDACs, and DNMTs.71 It is thus likely that the regulation of IRF-8 expression can be controlled by both DNA methylation and histone modification in a synergistic manner. It would be of great interest to investigate whether these regulatory mechanisms also apply to TNF-induced osteoclastogenesis and if inflammatory conditions would alter the action between these mechanisms.
V. CONCLUSIONS
Osteoclastogenesis in vivo is mediated by various factors including cytokines, growth factors, signaling molecules, and transcription factors that directly target osteoclast precursors and affect their differentiation and/or indirectly mediate osteoclastogenesis by targeting other cell populations such as osteoblastic/stromal cells, synovial cells, and T-cells. In the latter case, for example, TNF stimulates RANKL production from these cells. Both direct and indirect effects are integrated together to regulate osteoclastogenesis. The extent of inflammatory bone resorption is often determined by the balance between opposing factors. This includes not only balance between positive osteoclastogenic factors and negative regulators, but also different effects of individual factors on different cell types. For example, TNF does not induce effective osteoclast differentiation directly, but at the same time it promotes osteoclastogenesis indirectly by activating RANKL expression on stromal, osteoblastic, and T-cells. A recent finding showed that Lgr4 is a new receptor for RANKL and the signal through Lgr4 suppresses osteoclastogenesis.72 It would be of interest to investigate whether TNF stimulates Lgr4 expression and TNF interacts with Lgr4-mediated signaling pathways to restrain osteoclast differentiation. In acute infection or chronic inflammatory diseases such as RA, TNF is often predominantly expressed. Osteoclast precursors in the inflammatory microenvironment are refractory to inhibitors of osteoclastogenesis such as IL-27,73 leading to excessive bone resorption. Therefore, the identification of additional mechanisms and factors that increase the potency of intrinsic repressors or restore cellular responses to suppressive factors may represent effective therapies for pathologic bone loss.
ACKNOWLEDGMENTS
This work was supported by grants from the National Institutes of Health (NIH R01 AR068970 and R01 AR071463 to B.Z.). The content of this manuscript is solely the responsibility of the author and does not necessarily represent the official views of the NIH.
ABBREVIATIONS:
- DAP12
TYRO protein tyrosine kinase-binding protein
- FasL
Fas ligand
- FcRg
Fc receptor g
- GM-CSF
granulocyte M-CSF
- IFN
interferon
- IL
interleukin
- IRF
interferon regulatory factor
- ITAM
immunoreceptor tyrosine-based activation motif
- M-CSF
macrophage colony-stimulating factor
- MITF
microphthalmia-associated transcription factor
- NFATc1
Nuclear factor of activated T-cells, cytoplasmic 1
- NF-[kappa]B
nuclear factor [kappa]B
- OPG
osteoprotegerin
- OSCAR
osteoclast-associated receptor
- PI3K
phosphatidylinositide-3-kinase
- RANK
receptor activator of NF-[kappa]B
- RANKL
RANK ligand
- RBP-J
Recombination Signal Binding Protein For Immunoglobulin Kappa J Region
- TNF
tumor necrosis factor
- TRAF
TNF receptor-associated factor
- TREM-2
triggering receptor expressed by myeloid cells-2
REFERENCES
- 1.Takayanagi H SnapShot: Osteoimmunology. Cell Metab. 2015;21(3):502.e1. [DOI] [PubMed] [Google Scholar]
- 2.Goldring SR. Osteoimmunology and bone homeostasis: relevance to spondyloarthritis. Curr Rheumatol Rep. 2013;15(7):342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schett G Osteoimmunology in rheumatic diseases. Arthritis Res Ther. 2009;11(1):210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lorenzo J, Choi Y. Osteoimmunology. Immunol Rev. 2005;208:5–6. [DOI] [PubMed] [Google Scholar]
- 5.Pacifici R. Osteoimmunology and its implications for transplantation. Am J Trans. 2013;13(9):2245–54. [DOI] [PubMed] [Google Scholar]
- 6.Sims NA, Martin TJ. Coupling the activities of bone formation and resorption: a multitude of signals within the basic multicellular unit. BoneKEy reports. 2014;3:481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matsuo K, Irie N. Osteoclast-osteoblast communication. Arch Biochem Biophys. 2008;473(2):201–9. [DOI] [PubMed] [Google Scholar]
- 8.Raggatt LJ, Partridge NC. Cellular and molecular mechanisms of bone remodeling. J Biol Chem. 2010;285(33):25103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asagiri M, Takayanagi H. The molecular understanding of osteoclast differentiation. Bone. 2007;40(2):251–64. [DOI] [PubMed] [Google Scholar]
- 10.Zhao B, Ivashkiv LB. Negative regulation of osteoclastogenesis and bone resorption by cytokines and transcriptional repressors. Arthritis Res Ther. 2011;13(4):234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Humphrey MB, Lanier LL, Nakamura MC. Role of ITAM-containing adapter proteins and their receptors in the immune system and bone. Immunol Rev. 2005;208:50–65. [DOI] [PubMed] [Google Scholar]
- 12.Boyce BF. Advances in the regulation of osteoclasts and osteoclast functions. J Dent Res. 2013;92(10):860–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Novack DV, Teitelbaum SL. The osteoclast: friend or foe? Annu Rev Pathol. 2008;3:457–84. [DOI] [PubMed] [Google Scholar]
- 14.Schett G, Gravallese E. Bone erosion in rheumatoid arthritis: mechanisms, diagnosis and treatment. Nat Rev Rheumatol. 2012;8(11):656–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldring SR, Purdue PE, Crotti TN, Shen Z, Flannery MR, Binder NB, Ross FP, McHugh KP. Bone remodelling in inflammatory arthritis. Ann Rheum Dis. 2013;72 (Suppl 2):ii52–5. [DOI] [PubMed] [Google Scholar]
- 16.Teitelbaum SL. Osteoclasts; culprits in inflammatory osteolysis. Arthritis Res Ther. 2006;8(1):201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boyce BF, Schwarz EM, Xing L. Osteoclast precursors: cytokine-stimulated immunomodulators of inflammatory bone disease. Curr Opin Rheumatol. 2006;18(4):427–32. [DOI] [PubMed] [Google Scholar]
- 18.Dougall WC, Glaccum M, Charrier K, Rohrbach K, Brasel K, De Smedt T, Daro E, Smith J, Tometsko ME, Maliszewski CR, Armstrong A, Shen V, Bain S, Cosman D, Anderson D, Morrissey PJ, Peschon JJ, Schuh J. RANK is essential for osteoclast and lymph node development. Genes Dev. 1999;13(18):2412–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pettit AR, Ji H, von Stechow D, Muller R, Goldring SR, Choi Y, Benoist C, Gravallese EM. TRANCE/RANKL knockout mice are protected from bone erosion in a serum transfer model of arthritis. Am J Pathol. 2001;159(5):1689–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yarilina A, Xu K, Chen J, Ivashkiv LB. TNF activates calcium–nuclear factor of activated T cells (NFAT)c1 signaling pathways in human macrophages. Proc Natl Acad Sci U S A. 2011;108(4):1573–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lam J, Takeshita S, Barker JE, Kanagawa O, Ross FP, Teitelbaum SL. TNF-alpha induces osteoclastogenesis by direct stimulation of macrophages exposed to permissive levels of RANK ligand. J Clin Invest. 2000;106(12): 1481–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li J, Sarosi I, Yan XQ, Morony S, Capparelli C, Tan HL, McCabe S, Elliott R, Scully S, Van G, Kaufman S, Juan SC, Sun Y, Tarpley J, Martin L, Christensen K, McCabe J, Kostenuik P, Hsu H, Fletcher F, Dunstan CR, Lacey DL, Boyle WJ. RANK is the intrinsic hematopoietic cell surface receptor that controls osteoclastogenesis and regulation of bone mass and calcium metabolism. Proc Natl Acad Sci U S A. 2000;97(4):1566–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schett G, Teitelbaum SL. Osteoclasts and arthritis. J Bone Mineral Res. 2009;24(7):1142–6. [DOI] [PubMed] [Google Scholar]
- 24.Kim N, Kadono Y, Takami M, Lee J, Lee SH, Okada F, Kim JH, Kobayashi T, Odgren PR, Nakano H, Yeh WC, Lee SK, Lorenzo JA, Choi Y. Osteoclast differentiation independent of the TRANCE–RANK–TRAF6 axis. J Exp Med. 2005;202(5):589–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kobayashi K, Takahashi N, Jimi E, Udagawa N, Takami M, Kotake S, Nakagawa N, Kinosaki M, Yamaguchi K, Shima N, Yasuda H, Morinaga T, Higashio K, Martin TJ, Suda T. Tumor necrosis factor alpha stimulates osteoclast differentiation by a mechanism independent of the ODF/RANKL-RANK interaction. J Exp Med. 2000;191(2):275–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Azuma Y, Kaji K, Katogi R, Takeshita S, Kudo A. Tumor necrosis factor-alpha induces differentiation of and bone resorption by osteoclasts. J Biol Chem. 2000;275(7): 4858–64. [DOI] [PubMed] [Google Scholar]
- 27.Anandarajah AP, Schwarz EM, Totterman S, Monu J, Feng CY, Shao T, Haas-Smith SA, Ritchlin CT. The effect of etanercept on osteoclast precursor frequency and enhancing bone marrow oedema in patients with psoriatic arthritis. Ann Rheum Dis. 2008;67(3):296–301. [DOI] [PubMed] [Google Scholar]
- 28.Yao Z, Li P, Zhang Q, Schwarz EM, Keng P, Arbini A, Boyce BF, Xing L. Tumor necrosis factor-alpha increases circulating osteoclast precursor numbers by promoting their proliferation and differentiation in the bone marrow through up-regulation of c-Fms expression. J Biol Chem. 2006;281(17):11846–55. [DOI] [PubMed] [Google Scholar]
- 29.Li P, Schwarz EM, O’Keefe RJ, Ma L, Looney RJ, Ritchlin CT, Boyce BF, Xing L. Systemic tumor necrosis factor alpha mediates an increase in peripheral CD11bhigh osteoclast precursors in tumor necrosis factor alpha-transgenic mice. Arthritis Rheum. 2004;50(1):265–76. [DOI] [PubMed] [Google Scholar]
- 30.Zhang Q, Guo R, Schwarz EM, Boyce BF, Xing L. TNF inhibits production of stromal cell-derived factor 1 by bone stromal cells and increases osteoclast precursor mobilization from bone marrow to peripheral blood. Arthritis Res Ther. 2008;10(2):R37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kitaura H, Kimura K, Ishida M, Kohara H, Yoshimatsu M, Takano-Yamamoto T. Immunological reaction in TNF-alpha-mediated osteoclast formation and bone resorption in vitro and in vivo. Clin Dev Immunol. 2013;2013:181849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walsh MC, Choi Y. Biology of the RANKL-RANK-OPG system in immunity, bone, and beyond. Front Immunol. 2014;5:511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boyce BF, Xiu Y, Li J, Xing L, Yao Z. NF-kappaB-mediated regulation of osteoclastogenesis. Endocrinol Metab (Seoul). 2015;30(1):35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao B, Grimes SN, Li S, Hu X, Ivashkiv LB. TNF-induced osteoclastogenesis and inflammatory bone resorption are inhibited by transcription factor RBP-J. J Exp Med. 2012;209(2):319–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li S, Miller CH, Giannopoulou E, Hu X, Ivashkiv LB, Zhao B. RBP-J imposes a requirement for ITAM-mediated costimulation of osteoclastogenesis. J Clin Invest. 2014;124(11):5057–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao B, Takami M, Yamada A, Wang X, Koga T, Hu X, Tamura T, Ozato K, Choi Y, Ivashkiv LB, Takayanagi H, Kamijo R. Interferon regulatory factor-8 regulates bone metabolism by suppressing osteoclastogenesis. Nat Med. 2009;15(9):1066–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kopan R, Ilagan MX. The canonical Notch signaling pathway: unfolding the activation mechanism. Cell. 2009;137(2):216–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu H, Zhu J, Smith S, Foldi J, Zhao B, Chung AY, Outtz H, Kitajewski J, Shi C, Weber S, Saftig P, Li Y, Ozato K, Blobel CP, Ivashkiv LB, Hu X. Notch-RBP-J signaling regulates the transcription factor IRF-8 to promote inflammatory macrophage polarization. Nat Immunol. 2012;13(7):642–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu X, Chung AY, Wu I, Foldi J, Chen J, Ji JD, Tateya T, Kang YJ, Han J, Gessler M, Kageyama R, Ivashkiv LB. Integrated regulation of Toll-like receptor responses by Notch and interferon-gamma pathways. Immunity. 2008;29(5):691–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shimizu T, Kagawa T, Inoue T, Nonaka A, Takada S, Aburatani H, Taga T. Stabilized beta-catenin functions through TCF/LEF proteins and the Notch/RBP-Jkappa complex to promote proliferation and suppress differentiation of neural precursor cells. Mol Cell Biol. 2008;28(24):7427–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Plaisance S, Vanden Berghe W, Boone E, Fiers W, Haegeman G. Recombination signal sequence binding protein Jkappa is constitutively bound to the NF-kappaB site of the interleukin–6 promoter and acts as a negative regulatory factor. Mol Cell Biol. 1997;17(7):3733–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Izumiya Y, Izumiya C, Hsia D, Ellison TJ, Luciw PA, Kung HJ. NF-kappaB serves as a cellular sensor of Kaposi’s sarcoma–associated herpesvirus latency and negatively regulates K-Rta by antagonizing the RBP-Jkappa coactivator. J Virol. 2009;83(9):4435–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Swarnkar G, Karuppaiah K, Mbalaviele G, Chen TH, Abu-Amer Y. Osteopetrosis in TAK1-deficient mice owing to defective NF-kappaB and NOTCH signaling. Proc Natl Acad Sci U S A. 2015;112(1):154–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hayward SD. Viral interactions with the Notch pathway. Semin Cancer Biol. 2004;14(5):387–96. [DOI] [PubMed] [Google Scholar]
- 45.Taniguchi Y, Furukawa T, Tun T, Han H, Honjo T. LIM protein KyoT2 negatively regulates transcription by association with the RBP-J DNA-binding protein. Mol Cell Biol. 1998;18(1):644–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Beres TM, Masui T, Swift GH, Shi L, Henke RM, MacDonald RJ. PTF1 is an organ-specific and Notch-independent basic helix-loop-helix complex containing the mammalian Suppressor of Hairless (RBP-J) or its paralogue, RBP-L. Mol Cell Biol. 2006;26(1):117–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maillard I, Fang T, Pear WS. Regulation of lymphoid development, differentiation, and function by the Notch pathway. Annu Rev Immunol. 2005;23:945–74. [DOI] [PubMed] [Google Scholar]
- 48.Foldi J, Shang Y, Zhao B, Ivashkiv LB, Hu X. RBP-J is required for M2 macrophage polarization in response to chitin and mediates expression of a subset of M2 genes. Protein Cell. 2016;7(3):201–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Caton ML, Smith-Raska MR, Reizis B. Notch-RBP-J signaling controls the homeostasis of CD8– dendritic cells in the spleen. J Exp Med. 2007;204(7):1653–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shang Y, Smith S, Hu X. Role of Notch signaling in regulating innate immunity and inflammation in health and disease. Protein Cell. 2016;7(3):159–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stahl EA, Raychaudhuri S, Remmers EF, Xie G, Eyre S, Thomson BP, Li Y, Kurreeman FA, Zhernakova A, Hinks A, Guiducci C, Chen R, Alfredsson L, Amos CI, Ardlie KG, Consortium B, Barton A, Bowes J, Brouwer E, Burtt NP, Catanese JJ, Coblyn J, Coenen MJ, Costenbader KH, Criswell LA, Crusius JB, Cui J, de Bakker PI, De Jager PL, Ding B, Emery P, Flynn E, Harrison P, Hocking LJ, Huizinga TW, Kastner DL, Ke X, Lee AT, Liu X, Martin P, Morgan AW, Padyukov L, Posthumus MD, Radstake TR, Reid DM, Seielstad M, Seldin MF, Shadick NA, Steer S, Tak PP, Thomson W, van der Helm–van Mil AH, van der Horst–Bruinsma IE, van der Schoot CE, van Riel PL, Weinblatt ME, Wilson AG, Wolbink GJ, Wordsworth BP, Consortium Y, Wijmenga C, Karlson EW, Toes RE, de Vries N, Begovich AB, Worthington J, Siminovitch KA, Gregersen PK, Klareskog L, Plenge RM. Genome-wide association study meta-analysis identifies seven new rheumatoid arthritis risk loci. Nat Genet. 2010;42(6):508–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eyre S, Bowes J, Diogo D, Lee A, Barton A, Martin P, Zhernakova A, Stahl E, Viatte S, McAllister K, Amos CI, Padyukov L, Toes RE, Huizinga TW, Wijmenga C, Trynka G, Franke L, Westra HJ, Alfredsson L, Hu X, Sandor C, de Bakker PI, Davila S, Khor CC, Heng KK, Andrews R, Edkins S, Hunt SE, Langford C, Symmons D, Biologics in Rheumatoid Arthritis G, Genomics Study S, Wellcome Trust Case Control C, Concannon P, Onengut-Gumuscu S, Rich SS, Deloukas P, Gonzalez-Gay MA, Rodriguez-Rodriguez L, Arlsetig L, Martin J, Rantapaa-Dahlqvist S, Plenge RM, Raychaudhuri S, Klareskog L, Gregersen PK, Worthington J. High-density genetic mapping identifies new susceptibility loci for rheumatoid arthritis. Nat Genet. 2012;44(12):1336–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bai S, Kopan R, Zou W, Hilton MJ, Ong CT, Long F, Ross FP, Teitelbaum SL. NOTCH1 regulates osteoclastogenesis directly in osteoclast precursors and indirectly via osteoblast lineage cells. J Biol Chem. 2008;283(10):6509–18. [DOI] [PubMed] [Google Scholar]
- 54.Ma J, Liu YL, Hu YY, Wei YN, Zhao XC, Dong GY, Qin HY, Ding Y, Han H. Disruption of the transcription factor RBP-J results in osteopenia attributable to attenuated osteoclast differentiation. Mol Biol Rep. 2013;40(3): 2097–105. [DOI] [PubMed] [Google Scholar]
- 55.Long CL, Humphrey MB. Osteoimmunology: the expanding role of immunoreceptors in osteoclasts and bone remodeling. Bonekey Rep. 2012;1:pii:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hamidi H, Gustafason D, Pellegrini M, Gasson J. Identification of novel targets of CSL-dependent Notch signaling in hematopoiesis. PLoS One. 2011;6(5):e20022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Castel D, Mourikis P, Bartels SJ, Brinkman AB, Tajbakhsh S, Stunnenberg HG. Dynamic binding of RBPJ is determined by Notch signaling status. Genes Dev. 2013;27(9):1059–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang H, Zou J, Zhao B, Johannsen E, Ashworth T, Wong H, Pear WS, Schug J, Blacklow SC, Arnett KL, Bernstein BE, Kieff E, Aster JC. Genome-wide analysis reveals conserved and divergent features of Notch1/RBPJ binding in human and murine T-lymphoblastic leukemia cells. Proc Natl Acad Sci U S A. 2011;108(36):14908–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang H, Hilton MJ, Anolik JH, Welle SL, Zhao C, Yao Z, Li X, Wang Z, Boyce BF, Xing L. NOTCH inhibits osteoblast formation in inflammatory arthritis via noncanonical NF-kappaB. J Clin Invest. 2014;124(7):3200–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vaira S, Johnson T, Hirbe AC, Alhawagri M, Anwisye I, Sammut B, O’Neal J, Zou W, Weilbaecher KN, Faccio R, Novack DV. RelB is the NF-kappaB subunit downstream of NIK responsible for osteoclast differentiation. Proc Natl Acad Sci U S A. 2008;105(10):3897–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Otero JE, Dai S, Alhawagri MA, Darwech I, Abu-Amer Y. IKKbeta activation is sufficient for RANK-independent osteoclast differentiation and osteolysis. J Bone Mineral Res. 2010;25(6):1282–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Novack DV, Yin L, Hagen-Stapleton A, Schreiber RD, Goeddel DV, Ross FP, Teitelbaum SL. The IkappaB function of NF-kappaB2 p100 controls stimulated osteoclastogenesis. J Exp Med. 2003;198(5):771–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Maruyama T, Fukushima H, Nakao K, Shin M, Yasuda H, Weih F, Doi T, Aoki K, Alles N, Ohya K, Hosokawa R, Jimi E. Processing of the NF-kappa B2 precursor p100 to p52 is critical for RANKL-induced osteoclast differentiation. J Bone Miner Res. 2010;25(5):1058–67. [DOI] [PubMed] [Google Scholar]
- 64.Yao Z, Xing L, Boyce BF. NF-kappaB p100 limits TNF-induced bone resorption in mice by a TRAF3-dependent mechanism. J Clin Invest. 2009;119(10):3024–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Soysa NS, Alles N, Weih D, Lovas A, Mian AH, Shimokawa H, Yasuda H, Weih F, Jimi E, Ohya K, Aoki K. The pivotal role of the alternative NF-kappaB pathway in maintenance of basal bone homeostasis and osteoclastogenesis. J Bone Miner Res. 2010;25(4):809–18. [DOI] [PubMed] [Google Scholar]
- 66.Barros P, Jordan P, Matos P. Rac1 signaling modulates BCL-6-mediated repression of gene transcription. Mol Cell Biol. 2009;29(15):4156–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kim K, Kim JH, Lee J, Jin HM, Kook H, Kim KK, Lee SY, Kim N. MafB negatively regulates RANKL-mediated osteoclast differentiation. Blood. 2007;109(8):3253–9. [DOI] [PubMed] [Google Scholar]
- 68.Miyauchi Y, Ninomiya K, Miyamoto H, Sakamoto A, Iwasaki R, Hoshi H, Miyamoto K, Hao W, Yoshida S, Morioka H, Chiba K, Kato S, Tokuhisa T, Saitou M, Toyama Y, Suda T, Miyamoto T. The Blimp1-Bcl6 axis is critical to regulate osteoclast differentiation and bone homeostasis. J Exp Med. 2010;207(4):751–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nishikawa K, Iwamoto Y, Kobayashi Y, Katsuoka F, Kawaguchi S, Tsujita T, Nakamura T, Kato S, Yamamoto M, Takayanagi H, Ishii M. DNA methyltransferase 3a regulates osteoclast differentiation by coupling to an S-adenosylmethionine-producing metabolic pathway. Nat Med. 2015;21(3):281–7. [DOI] [PubMed] [Google Scholar]
- 70.Fang C, Qiao Y, Mun SH, Lee MJ, Murata K, Bae S, Zhao B, Park-Min KH, Ivashkiv LB. Cutting Edge: EZH2 promotes osteoclastogenesis by epigenetic silencing of the negative regulator IRF-8. J Immunol. 2016;196(11): 4452–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Marchesi I, Bagella L. Role of enhancer of zeste homolog 2 polycomb protein and its significance in tumor progression and cell differentiation In: Radzioch D, editor. Chromatin remodelling. Rijeka: InTech; 2013. p. 119–52. [Google Scholar]
- 72.Luo J, Yang Z, Ma Y, Yue Z, Lin H, Qu G, Huang J, Dai W, Li C, Zheng C, Xu L, Chen H, Wang J, Li D, Siwko S, Penninger JM, Ning G, Xiao J, Liu M. LGR4 is a receptor for RANKL and negatively regulates osteoclast differentiation and bone resorption. Nat Med. 2016;22(5):539–46. [DOI] [PubMed] [Google Scholar]
- 73.Kalliolias GD, Zhao B, Triantafyllopoulou A, Park-Min KH, Ivashkiv LB. Interleukin-27 inhibits human osteoclastogenesis by abrogating RANKL-mediated induction of nuclear factor of activated T cells c1 and suppressing proximal RANK signaling. Arthritis Rheum. 2010;62(2):402–13. [DOI] [PMC free article] [PubMed] [Google Scholar]