Abstract
Objective
To develop a new patient-reported outcome measure that captures feelings of being trapped that are commonly experienced by caregivers of individuals with traumatic brain injury (TBI).
Design
Cross-sectional
Setting
Three TBI Model Systems rehabilitation hospitals, an academic medical center, and a military medical treatment facility.
Participants
Caregivers of civilians with TBI (n=344) and caregivers of service members/veterans with TBI (n=216).
Interventions
Not applicable.
Outcome Measures
TBI-CareQOL Feeling Trapped Item Bank
Results
From an initial item pool of 28 items, exploratory and confirmatory factor analyses supported the retention of 16 items. After graded response model (GRM) and differential item functioning (DIF) analyses were conducted, 15 items were retained in the final measure. GRM calibration data, along with clinical expert input, was used to choose a 6-item, static short form, and the calibration data was utilized for programming of the TBI-CareQOL Feeling Trapped computer adaptive test (CAT). CAT simulation analyses produced an r = 0.99 correlation between CAT scores and the full item-bank. Three-week short form test-retest reliability was very good (r = 0.84).
Conclusions
The new TBI-CareQOL Feeling Trapped item bank was developed to provide a sensitive and efficient examination of the impact that feelings of being trapped, due to the caregiver role, have on health-related quality of life (HRQOL) for caregivers of individuals with TBI. Both the CAT and corresponding 6-item short form demonstrate excellent psychometric properties. Future work is needed to establish the responsiveness of this measure to clinical interventions for these caregivers.
Keywords: Health-related quality of life, PROMIS, TBI-CareQOL, traumatic brain injury, caregiver, feeling trapped, patient reported outcome
Moderate to severe traumatic brain injury (TBI) can result in a variety of impairments that render the person with injury dependent on caregivers. About one-third to one-half of persons with moderate to severe TBI (per TBI model system criteria)1 are not independent in everyday activities.2,3 Physical impairments (e.g., motor spasticity and balance problems) can lead to the need for physical assistance with mobility and transportation.4,5 Cognitive impairments can result in dependence in everyday tasks, including scheduling appointments, taking medication, and performing basic self-care.6 Behavioral impairments such as impulsivity can pose a safety risk.7,8 Emotional distress leads to suicidal ideation for many people with TBI,9,10 increasing the need for supervision. Given these difficulties, it is not surprising that about one-third of persons with moderate to severe TBI require supervision one year following injury,11,12 and over one-fourth receive some form of supervision 2–9 years post-injury.13 Cognitive and behavioral impairments can also result in social isolation, rendering caregivers the primary source of social support for persons with an injury.14 Furthermore, unemployment is a major problem, resulting in financial dependence on family caregivers.2,15,16
The need for partial or full-time supervision for persons with moderate to severe TBI can negatively impact caregivers. The presence of emotional distress17–19 and perceived burden (i.e., caregiver’s perceptions that caring for the person with TBI negatively affects them) have been shown to have long-term effects.20,21 The extent to which caregivers feel trapped or not in control can impact the level of distress and perceived burden they experience. The concept of entrapment or role captivity refers to the extent to which caregivers feel they are not free to live their own life or they are trapped by the illness or condition of the person for whom they provide care.22 The feeling of entrapment has been shown to be associated with depression in caregivers of persons with dementia23 and a warning sign of caregiver burnout (i.e., physical, emotional, and/or mental exhaustion) for caregivers of persons with Amyotrophic Lateral Sclerosis.24 The concept of entrapment has not been applied to caregivers of persons with TBI to date; however, qualitative research indicates that this feeling is present in this population. In early work on the impact of TBI on family members, Lezak (p. 593) noted that “Feeling trapped is an almost universal phenomenon,”25 and that family members can feel trapped even if they are working and maintaining activity outside of the home. This feeling is related to fear of what will happen to the person with the injury while they are gone. Subsequent literature emphasized emotional distress and perceived burden in caregivers, but not the specific feeling of entrapment. The theme of feeling trapped emerged in recent focus groups conducted with caregivers of civilians with TBI, and with caregivers of service members/veterans (SMVs) with TBI.26,27
As rehabilitation for individuals with TBI continues to evolve, many programs have recognized the need to treat not only the person with TBI, but also their care system. Although there is literature to support the reciprocal relationship of the well-being of the caregiver and of the person with TBI28,29 there has been little done to develop ways of measuring symptoms or experiences unique to caregivers of persons with brain injury.
Given its potential contribution to emotional distress and to overall health for caregivers of civilians and SMVs with TBI, the concept of feeling trapped is important to quantify. Although measures of caregiver burden currently exist, we are unaware of measures that include the concept of feeling trapped. As such, an item bank was developed to assess this concept (i.e., TBI-CareQOL Feeling Trapped) in caregivers of civilians and SMVs with TBI in the hopes of being able to measure this common experience.
Methods
Study Participants
Five hundred sixty caregivers of civilians (n=344) or SMVs with TBI (n=216) participated in this study; a subset also completed a retest survey (n=56 civilian and n=89 military). A description of this sample is detailed elsewhere.30 Briefly, participants were recruited through existing TBI-specific caregiver databases, medical record data capture systems,31 hospital-based recruitment and community outreach efforts at two TBI model system sites, an academic medical treatment center, and Walter Reed National Military Medical Center (WRNMMC). A caregiver was defined as an individual who provides physical assistance, financial assistance, or emotional support to an individual with a TBI. Caregivers of civilians and SMVs were ≥18 years old, able to read and understand English, and were caring for someone who was ≥1 year post-injury (given that the majority of recovery occurs within the first 12-months post-TBI, we excluded individuals who were caring for more acute injuries to maximize sample homogeneity32–43). Caregivers of civilians with TBI were caring for an individual that was ≥16 years old at the time of the initial injury and who met TBI Model Systems criteria for a medically-documented complicated mild, moderate, or severe TBI.1 Caregivers of SMVs with TBI were included if they were caring for an individual who was ≥16 years old at the time of the injury and that had a TBI that was medically documented by a Department of Defense or Department of Veteran Affairs treatment facility. All data were collected in accordance with each site’s local institutional review board. Participants (i.e. caregivers) provided consent prior to participation. Study participants completed study measures online (https://www.assessmentcenter.net) between 12/2014 and 04/2016. Surveys were completed using a designated research visit computer or on a personal or publically-available computer with internet access. All measures were completed within a 2-week time period. The retest only occurred at a single data collection site (72.5% of participants at this site completed the retest).
Feeling Trapped Item Pool
A detailed summary of the origination of the Feeling Trapped Item Pool can be found in Carlozzi et al.30 Briefly, in accordance with established measurement development standards, 44 an initial item pool of 75 items was generated from focus group discussion among caregivers of individuals with TBI (nine groups with caregivers of civilian-related TBI and nine groups with caregivers of SVMs with TBI)26,27 and systematic literature reviews. Items were refined via an iterative process that included expert review, evaluation of item literacy level, and caregiver cognitive debriefing to ensure adequate content coverage and appropriate reading and comprehension levels. The final pool included 28 items designed to evaluate feelings of being trapped; all items used the same response options (never, rarely, sometimes, usually, always). These items served as the basis of this new patient-reported outcome measure (PRO), which assesses caregiver feelings of being unable to leave the person for whom they provide care.
Statistical Analyses
Sample size considerations are reported in Carlozzi et al., this issue.30
Overview
In order to develop an item bank from the initial item pool, we followed established guidelines44 incorporating classical test theory and item response theory (IRT) for measurement development. IRT is a mathematical modeling technique used to find a latent scale score from its component items, rather than using simple linear addition (as in classical test theory); it offers several advantages, including providing data about both the discriminability and difficulty of each item, and it can be used to program computer adaptive test (CAT) administration of a PRO measure.45,46
First, we identified a unidimensional set of items. Second, we used IRT47 analyses to estimate the bank’s item parameters (slopes and thresholds), thereby establishing the calibrations required for CAT and short form (SF) administrations of this final item bank. Initial analyses commenced by utilizing all 28 items in the item pool.
Exploratory Factor Analysis (EFA)/Confirmatory Factor Analysis (CFA), Initial Item Performance Assessments.
Full-sample EFA then CFA were used to iteratively examine the dimensionality of the item pool.48–50 Analyses were conducted using MPlus (version 7.4).51 For EFA, unidimensionality was considered supported if the ratio of eigenvalue 1 to eigenvalue 2 was >4 and the proportion of variance accounted for by eigenvalue 1 was >.40. Items were deleted from the item pool if they had sparse cells (one or more response categories with n<10 respondents), low item-adjusted total score correlations (r <0.40), or were non-monotonicity (item response scores did not increase as measure response scores increased; this assumption was tested using Testgraf52 by examining item-rest plots and expected scores by latent trait plots obtained from a non-parametric IRT model). Next, CFA was used to identify (and delete) items with low factor loadings (lx<0.50), as well as items demonstrating local dependence (residual correlation>0.20; correlated error modification index≥100).48–50
IRT Modeling, Final Item Performance Assessments, Differential Item Function (DIF) Studies, Final CFA Modeling.
Once a unidimensional item set was identified and refined, Samejima’s graded response model (GRM)53 was used to model the data using IRTPRO (version 3.1).54 Items were retained if they demonstrated good individual item fit (items displaying significant misfit, S-X2, p<0.01, were deleted from the item pool). Next, a hybrid IRT ability score-ordinal logistic regression framework55 was used to flag items for DIF that were potentially biased for age, education, and caregiver civilian vs. SMV status; items that exhibited impactful DIF (Nagelkerke pseudo-R2 change ≥0.20, plus >2% of DIF-corrected vs. uncorrected score differences exceeding uncorrected score standard errors) were deleted from the item pool (analyses were conducted using the R package LORDIF Version 0.3–256,57). A final CFA model was run to confirm unidimensionality and assess overall model fit. Standard fit criteria were employed: comparative fit index (CFI) ≥0.95, Tucker-Lewis index (TLI) ≥0.95, and root mean square error of approximation (RMSEA) <0.15.58–61
CAT Simulation, Short Form Development
CAT scores on the new Feeling Trapped Item Bank were simulated using Firestar simulation software.62 In addition, a six-item short form was also constructed that balanced psychometric and clinical considerations to attain item bank representativeness.
Scoring of the Feeling Trapped Item bank
IRT-based theta scores for the Feeling Trapped CAT and SF administrations were estimated using the GRM; scores were then placed on a T-score metric (mean=50, SD=10); higher scores indicate more feelings of entrapment.
Results
Study Participants
Detailed descriptive data about the study sample can be found in Carlozzi et al.30 Briefly, on average caregivers were 46.1 years old (SD=14.1) and in the caregiver role for 5.8 years (SD=5.4). The majority of caregivers were female (85.5%), Caucasian (77.2%), married (74.2%), caring for a spouse (58.2%) or parent (22.9%), and well educated (81.5% have some college or a college degree). The vast majority of TBIs for the SMV group were a result of military involvement (98%).
Unidimensional Modeling and Analyses
Table 1 provides a summary of the iterative process described below.
Table 1.
Unidimensional Modeling and Analyses
| Domain | Unidimensional Modeling | Initial Item Performance | IRT Modeling | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| item pool | EFA E1/E2ratio (craticriterion >4) | Proportion of variance for E1 (criterion >0.40) | 1-factor CFA loading (criterion <.50 | 1-factor CFA residual correlation (criterion >.20) | 1-factor CFA modification index (criterion >100) | Item-adjusted total score correlations (Criterion <.40) | Sparse cells (criterion<10) | Problems with monotonicity | IRT item misfit |
DIF | Final item bank | |
| Feeling Trapped | 28 items | 6.11 | 0 items | 1 item | 10 items | 0 items | 1 item | 0 items | 0 items | 1 item | 0 items | 15 items |
Note. CFA = Confirmatory Factor Analysis; EFA = Exploratory Factor Analysis, IRT = Item Response Theory
EFA/CFA, Initial Item Performance Assessments.
Field testing was conducted for the 28 items from the Feeling Trapped item pool. Initial EFA evidence suggested unidimensionality of this item pool. None of the items demonstrated problems with non-monotonicity, nor were there problems with sparse cells; one item was removed for low factor loadings and 11 items were excluded due to evidence of local dependence (ten items were deleted due to large residual correlations; one item was deleted due to large correlated error modification indices). The resultant item pool was 16 items.
IRT Modeling, Final Item Performance Assessments, DIF Studies, Final CFA Modeling
IRT modeling (GRM) identified an additional item with significant misfit (S-X2, p<0.01) which was excluded from the pool. Analyses did not identify any items with significant DIF for age, education, or civilian/SMV status.
Final Item Bank Criteria
A final CFA model indicated good overall model fit for the final 15 Feeling Trapped items; findings also supported response pattern (marginal) reliability (r = .93) and Cronbach’s alpha (internal consistency; r = .97); see Table 2.
Table 2.
Caregiver Strain Final Item Parameters
| Domain | Item Bank | CFI (criterion ≥.95) | TLI (criterion ≥.95) | CFA-based RMSEA (criterion < .15) | Cronbach’s Alpha Reliability (criterion > .80) | IRT-based RMSEA (criterion < .15) | Response Pattern Reliability (criterion > .80) |
|---|---|---|---|---|---|---|---|
| Feeling Trapped | 15 items | .98 | .97 | .14 | .97 | .05 | .93 |
Note. CFI = Comparative Fit Index, TLI = Tucker-Lewis Index, RMSEA: Root Mean Square Error of Approximation
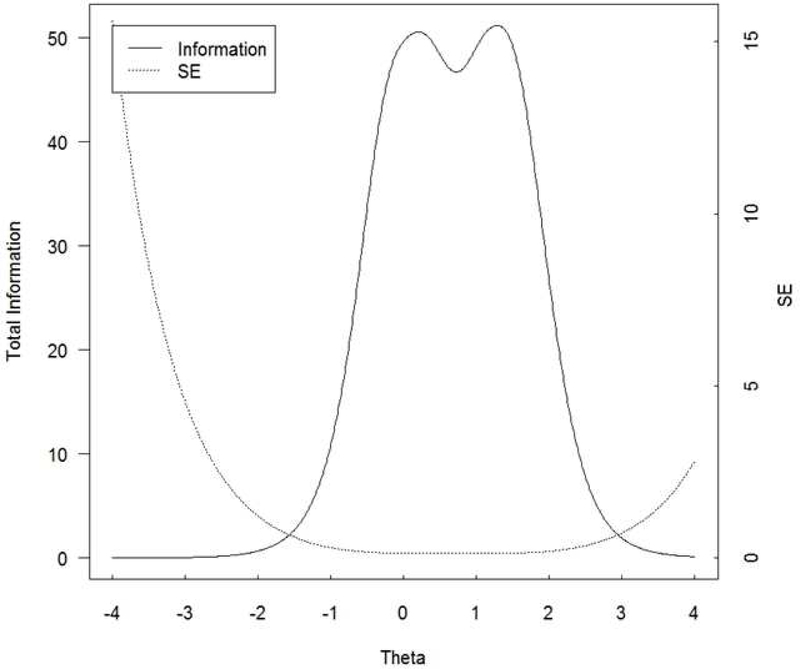
Estimates of final item bank item parameters are shown in Table 3. Score-level reliability was excellent from theta=−0.8 to +2.4, with expected score-level reliability ≥.90; score-level from theta =−1.2 to +2.4 was at least very good (≥.80), while score-level reliability from theta =−1.2 to +2.8 was at least good (≥.70). Feeling Trapped Test information is found in Figure 1.
Table 3.
TBI-CareQOL Item Parameters for Feeling Trapped
| Item | Slope | Threshold 1 | Threshold 2 | Threshold 3 | Threshold 4 |
|---|---|---|---|---|---|
| I feel like I cannot leave home because of the responsibilities I have as a caregiver. | 4.83 | −0.21 | 0.35 | 1.09 | 1.5 |
| I cannot run errands because I need to be with the person I care for. | 4.20 | 0.01 | 0.57 | 1.39 | 1.81 |
| I find it difficult to do things alone because of the care I give to the person with the injury. | 4.12 | −0.26 | 0.31 | 1.1 | 1.62 |
| My freedom feels limited when it comes to providing care for the person with the injury. | 3.91 | −0.37 | 0.2 | 1.11 | 1.52 |
| I feel like I need to rush home to be with the person I care for. | 3.64 | −0.4 | 0.07 | 0.78 | 1.25 |
| I feel limited about the places I can go because of the care I give to the person with the injury. | 3.58 | −0.31 | 0.2 | 0.97 | 1.41 |
| I feel as if I am unable to go to public places because I need to take care of the person with the injury. | 3.55 | 0.08 | 0.7 | 1.5 | 1.91 |
| I feel like I cannot leave the person with the injury, even if other people are providing care. | 3.49 | 0.12 | 0.61 | 1.25 | 1.64 |
| I come home early from social gatherings because I need to be with the person I care for. | 3.40 | −0.37 | 0.22 | 0.89 | 1.39 |
| I feel like I cannot have a minute away from the person I care for without worrying about him/her. | 3.30 | −0.2 | 0.37 | 1 | 1.49 |
| I feel sad because I lost the freedom I once had before the person I care for was injured. | 2.84 | −0.2 | 0.47 | 1.29 | 1.7 |
| I feel I have to be physically near the person I care for. | 2.63 | −0.47 | 0.07 | 1.02 | 1.79 |
| I am unable to leave the person I care for alone. | 2.50 | 0 | 0.54 | 1.19 | 1.55 |
| It is difficult for me to trust that someone else can care for the person with the injury as well as I do. | 2.37 | −0.39 | 0.18 | 0.81 | 1.31 |
| I feel restricted by the disability of the person I care for. | 2.24 | −0.45 | 0.27 | 1.33 | 1.94 |
Note. Items that are indicated in bold were selected for inclusion on the 6-item short form
Figure 1.
Feeling Trapped Test Information Plot
In general, we want total information to be . 10.0 and the standard error to be . 0.32 (this provides a reliability of 0.9). This figure shows excellent total information and standard error for Feeling Trapped scale scores between −0.8 and +2.4.
CAT Simulation, Short Form Development
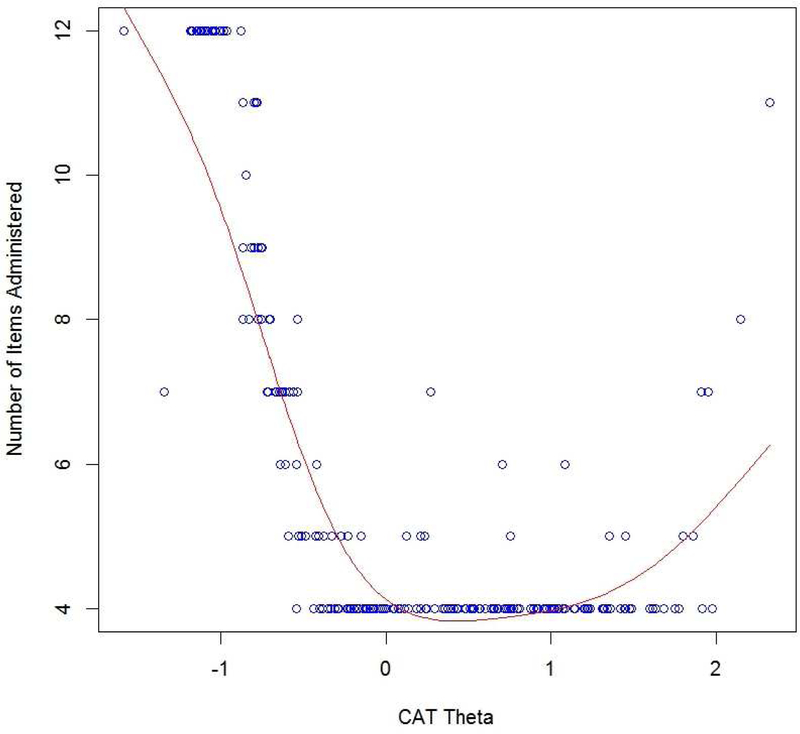
For Feeling Trapped estimated scores (full item bank vs. CAT administration), the correlation between the item bank and the CAT scores was excellent (r = .99). The most frequent occurring CAT lengths were (in descending order) 4 items (n=357, 64.2%), 12 items (n= 114, 20.5%), 5 items (n= 33, 5.9%), and 7 items (n= 19, 3.4%). CATs 6 or 8 to 11 items long occurred infrequently (n= 33, 5.9%). For 4-item CATs, observed thetas ranged from −0.54 to +1.98; theta ranges for 5 and 7-item CATs were similar to those observed for 4-item CATs, though slightly wider (five items: −0.59 to +1.86; seven items: - 1.34 to +1.95). Observed thetas for 12-item CATs were negative and ranged from −1.58 to - 0.87. Thus, 12-item CATs occurred when extreme low levels of Feeling Trapped were measured.
Figure 2 shows the number of CAT items used for different scale scores at standard deviation units: at −1 SD units, the CAT always used the maximum 12 items administered from the item bank; from +0 to +2 SD units, the CAT tended to use the minimum number of four items administered from the item bank; and at >+2 SD units the CAT used more than four items from the item bank. The average CAT administration time was 32 seconds.
Figure 2.
Feeling Trapped Number of CAT Items by CAT Theta
This figure shows the number of CAT items used for different scale scores in standard deviation units: at approximately . −1.0 SD units, the maximum of 12 items from the item bank were used by the CAT; from approximately −0.5 to +2.0 SD units, the CAT tended to use the minimum of four items from the item bank.
Clinical expert knowledge and psychometric considerations (i.e., item performance statistics) were used to select the best set of items for the Feeling Trapped six-item SF. The reliability for this SF was examined on a measurement continuum from theta −2.8 (T-score=22) to +2.8 (T-score=78). Score-level reliability was excellent (i.e. ≥.90) from theta −0.4 to +2.0. Score-level reliability from theta −0.8 to +2.0 was very good (≥.80), while score-level reliability from theta −0.8 to +2.4 was at least good (≥.70). Three-week test-retest reliability was very good (r = 0.84). Summed score to T-score conversions for the Feeling Trapped 6-item SF are shown in Table 4. The average 6-item SF administration time was 34 seconds.
Table 4.
Short-Form Summed Score to t Score Conversion Table for TBI-CareQOL Feeling Trapped Item Bank
| Raw Score | T-score | SE * |
|---|---|---|
| 6 | 37.00 | 5.39 |
| 7 | 42.90 | 3.07 |
| 8 | 44.97 | 2.73 |
| 9 | 46.70 | 2.38 |
| 10 | 48.06 | 2.11 |
| 11 | 49.29 | 2.11 |
| 12 | 50.41 | 2.06 |
| 13 | 51.49 | 2.04 |
| 14 | 52.55 | 2.04 |
| 15 | 53.60 | 2.06 |
| 16 | 54.65 | 2.07 |
| 17 | 55.69 | 2.08 |
| 18 | 56.72 | 2.08 |
| 19 | 57.74 | 2.08 |
| 20 | 58.75 | 2.07 |
| 21 | 59.76 | 2.06 |
| 22 | 60.76 | 2.04 |
| 23 | 61.76 | 2.02 |
| 24 | 62.76 | 2.02 |
| 25 | 63.80 | 2.05 |
| 26 | 64.89 | 2.12 |
| 27 | 66.09 | 2.22 |
| 28 | 67.55 | 2.48 |
| 29 | 69.16 | 2.68 |
| 30 | 73.16 | 4.10 |
SE = Standard error
Discussion
Given that feelings of entrapment or role captivity appear to be associated with emotional distress and burnout in caregivers,22–24 a better understanding of these feelings and how they impact health-related quality of life (HRQOL) is important and may help to drive the development and implementation of clinical interventions. Despite this need, there is an understudied need for caregivers of individuals with TBI. To help foster research in this area, this study provided a comprehensive effort to develop a new assessment tool that assesses feelings of entrapment for caregivers of individuals with TBI. It also marks the first effort to develop CATs that are specific to caregiver needs.
The final Feeling Trapped item bank was comprised of a unidimensional set of 15 items that were free from bias (related to age, or education-level and status—civilian or SMV); we interpret the measure as reflecting the feelings of entrapment experienced by caregivers of individuals with TBI. Resulting scores are on a T-score metric, allowing for clinical interpretation of scores relative to other caregivers of individuals with TBI. Scores that are ≥60 indicate feelings of entrapment that are worse than 84.1% of their peers, whereas scores ≥70 indicate feelings that are worse than 97.7% of their peers. Both the TBI-CareQOL Feeling Trapped Item Bank CAT and SF administrations demonstrated excellent reliability and can be administered in under a minute.
The psychometric developmental strengths of incorporating the patient perspective, as well as the advantages afforded by the combination of classical test theory and IRT-based approaches to development, 45,46 and the strong psychometric properties of this measure (internal consistency, test-retest reliability, convergent and discriminant validity, and known groups validity findings, reported elsewhere in this special issue63) support the clinical utility of this measure. The brief administration time makes this measure an ideal candidate for inclusion within an outpatient visit that is focused on the support network of the person with the TBI. Ideally, this type of integration could help foster appropriate referrals for caregivers that are in need of additional services/support. Such services should also have downstream positive effects for the person with the TBI, given the established relationship between caregiver and care-recipient outcomes.29,64–70
Study Limitations
Several study limitations must be acknowledged. While diverse, this sample was comprised largely of spousal caregivers; there were not enough parent caregivers to determine if items perform differently among parent caregivers. In addition, we were not able to control for caregiver health status, intensity of care provided, or TBI severity; medical record documentation for TBI severity was not available for a large portion of the military sample (i.e., those recruited outside of the WRNMMC). Also, caregivers of persons with acute injuries (<1 year post-injury) were excluded, limiting the generalizability of findings to these individuals. However, given the likely universal applicability of feelings of entrapment related to the caregiver role, these items may be appropriate for other caregiver subgroups. Future work could examine caregiver-specific factors like overall health status and occupation, as they might have an impact on the level of perceived stress.
Conclusion
This is the first time that a measure of feelings of entrapment has been developed, and the TBI-CareQOL measurement system is the first to be developed specifically for caregivers of individuals with TBI that includes CAT measures. Additionally, both CAT and SF administrations from the item bank generate standardized scores (T-scores), which has the advantage of aiding clinicians and researchers in score interpretations; scores systematically indicate how a caregiver is functioning relative to other caregivers of individuals with TBI. Ultimately, this measure can be used to help identify caregivers who are in need of respite care services and will foster assistance for caregivers who are seeking instrumental support in their daily lives.
Highlights:
Caregivers of persons with traumatic brain injury often feel trapped
TBI-CareQOL Feeling Trapped was developed to assess quality of life in caregivers
This new measure addresses an important caregiver emotional concern
Acknowledgements
Work on this manuscript was supported by the National Institutes of Health (NIH)- National Institute of Nursing Research (R01NR013658), the National Center for Advancing Translational Sciences (UL1TR000433), and the Defense and Veterans Brain Injury Center (DVBIC). We thank the investigators, coordinators, and research associates/assistants who worked on this study, the study participants, and organizations who supported recruitment efforts. The University of Michigan Research Team would also like to thank the Hearts of Valor and the Brain Injury Association of Michigan for assistance with community outreach for recruitment efforts at this site.
TBI-CareQOL Site Investigators and Coordinators: Noelle Carlozzi, Anna Kratz, Amy Austin, Mitchell Belanger, Micah Warschausky, Siera Goodnight, Jennifer Miner (University of Michigan, Ann, Arbor, MI); Angelle Sander (Baylor College of Medicine and TIRR Memorial Hermann, Houston, TX), Curtisa Light (TIRR Memorial Hermann, Houston, TX); Robin Hanks, Daniela Ristova-Trendov (Wayne State University/Rehabilitation Institute of Michigan, Detroit, MI); Nancy Chiaravalloti, Dennis Tirri, Belinda Washington (Kessler Foundation, West Orange, NJ); Tracey Brickell, Rael Lange, Louis French, Rachel Gartner, Megan Wright, Angela Driscoll, Diana Nora, Jamie Sullivan, Nicole Varbedian, Johanna Smith, Lauren Johnson, Heidi Mahatan, Mikelle Mooney, Mallory Frazier, Zoe Li, and Deanna Pruitt (Walter Reed National Military Medical Center/Defense and Veterans Brain Injury Center, Bethesda, MD)
List of Abbreviations:
- CAT
Computer Adaptive Test
- CFA
Confirmatory Factor Analysis
- CFI
Confirmatory Fit Index
- DIF
Differential Item Functioning
- EFA
Exploratory Factor Analysis
- GRM
Graded Response Model
- HRQOL
Health-Related Quality of Life
- PRO
Patient-Reported Outcome
- PROMIS
Patient-Reported Outcomes Measurement Information System
- RMSD
Root Mean Square Deviation
- RMSEA
Root Mean Squared Error of Approximation
- SF
Short Form
- SMV
Service Member/Veteran
- TBI
Traumatic Brain Injury
- TBI
CareQOL Traumatic Brain Injury Caregiver Quality of Life
- TLI
Tucker Lewis Index
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Publisher's Disclaimer: Disclaimer:
The identification of specific products or scientific instrumentation does not constitute endorsement or implied endorsement on the part of the author, DoD, or any component agency. While we generally exercise reference to products companies, manufacturers, organizations etc. in government produced works, the abstracts produced and other similarly situated research presents a special circumstance when such a product inclusions become an integral part of the scientific endeavor.
References
- 1.Corrigan JD, Cuthbert JP, Whiteneck GG, et al. Representativeness of the Traumatic Brain Injury Model Systems National Database. Journal of Head Trauma Rehabilitation 2012;27(6):391–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corrigan JD, Cuthbert JP, Harrison-Felix C, et al. US population estimates of health and social outcomes 5 years after rehabilitation for traumatic brain injury. J Head Trauma Rehabil 2014;29(6):E1–9. [DOI] [PubMed] [Google Scholar]
- 3.Jourdan C, Bayen E, Vallat-Azouvi C, et al. Late Functional Changes Post-Severe Traumatic Brain Injury Are Related to Community Reentry Support: Results From the PariS-TBI Cohort. J Head Trauma Rehabil 2017. [DOI] [PubMed]
- 4.Kapoor N, Ciuffreda KJ. Vision disturbances following traumatic brain injury. Current Treatment Options in Neurology 2002;4(4):271–280. [DOI] [PubMed] [Google Scholar]
- 5.Krauss JK. Movement disorders secondary to craniocerebral trauma. Handbook of Clinical Neurology 2015;128:475–496. [DOI] [PubMed] [Google Scholar]
- 6.Rabinowitz AR, Levin HS. Cognitive sequelae of traumatic brain injury. Psychiatric Clinics of North America 2014;37(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seel RT, Macciocchi S, Velozo CA, et al. The Safety Assessment Measure for persons with traumatic brain injury: Item pool development and content validity. NeuroRehabilitation 2016;39(3):371–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sabaz M, Simpson GK, Walker AJ, Rogers JM, Gillis I, Strettles B. Prevalence, comorbidities, and correlates of challenging behavior among community-dwelling adults with severe traumatic brain injury: A multicenter study. Journal of Head Trauma Rehabilitation 2014;29(2):E19–30. [DOI] [PubMed] [Google Scholar]
- 9.Fisher LB, Pedrelli P, Iverson GL, et al. Prevalence of suicidal behaviour following traumatic brain injury: Longitudinal follow-up data from the NIDRR Traumatic Brain Injury Model Systems. Brain Inj 2016;30(11):1311–1318. [DOI] [PubMed] [Google Scholar]
- 10.Brenner LA, Ignacio RV, Blow FC. Suicide and traumatic brain injury among individuals seeking Veterans Health Administration services. J Head Trauma Rehabil 2011;26(4):257–264. [DOI] [PubMed] [Google Scholar]
- 11.Hart T, Millis S, Novack T, Englander J, Fidler-Sheppard R, Bell KR. The relationship between neuropsychologic function and level of caregiver supervision at 1 year after traumatic brain injury. Arch Phys Med Rehabil 2003;84(2):221–230. [DOI] [PubMed] [Google Scholar]
- 12.Bailey EK, Nakase-Richardson R, Patel N, et al. Supervision Needs Following Veteran and Service Member Moderate to Severe Traumatic Brain Injury: A VA TBI Model Systems Study. J Head Trauma Rehabil 2017. [DOI] [PubMed]
- 13.Hall KM, Bushnik T, Lakisic-Kazazic B, Wright J, Cantagallo A. Assessing traumatic brain injury outcome measures for long-term follow-up of community-based individuals. Arch Phys Med Rehabil 2001;82(3):367–374. [DOI] [PubMed] [Google Scholar]
- 14.Jacobs HE. The Los-Angeles Head-Injury Survey - Procedures and initial findings. Archives of Physical Medicine and Rehabilitation 1988;69(6):425–431. [PubMed] [Google Scholar]
- 15.Doctor JN, Castro J, Temkin NR, Fraser RT, Machamer JE, Dikmen SS. Workers’ risk of unemployment after traumatic brain injury: a normed comparison. J Int Neuropsychol Soc 2005;11(6):747–752. [DOI] [PubMed] [Google Scholar]
- 16.Dillahunt-Aspillaga C, Nakase-Richardson R, Hart T, et al. Predictors of Employment Outcomes in Veterans With Traumatic Brain Injury: A VA Traumatic Brain Injury Model Systems Study. J Head Trauma Rehabil 2017. [DOI] [PubMed]
- 17.Winstanley J, Simpson G, Tate R, Myles B. Early indicators and contributors to psychological distress in relatives during rehabilitation following severe traumatic brain injury: findings from the Brain Injury Outcomes Study. J Head Trauma Rehabil 2006;21(6):453–466. [DOI] [PubMed] [Google Scholar]
- 18.Kreutzer JS, Rapport LJ, Marwitz JH, et al. Caregivers’ well-being after traumatic brain injury: a multicenter prospective investigation. Arch Phys Med Rehabil 2009;90(6):939–946. [DOI] [PubMed] [Google Scholar]
- 19.Ponsford J, Schonberger M. Family functioning and emotional state two and five years after traumatic brain injury. Journal of the International Neuropsychological Society 2010;16(2):306–317. [DOI] [PubMed] [Google Scholar]
- 20.Bayen E, Jourdan C, Ghout I, et al. Objective and Subjective Burden of Informal Caregivers 4 Years After a Severe Traumatic Brain Injury: Results From the PariS-TBI Study. J Head Trauma Rehabil 2016;31(5):E59–67. [DOI] [PubMed] [Google Scholar]
- 21.Manskow US, Friborg O, Roe C, Braine M, Damsgard E, Anke A. Patterns of change and stability in caregiver burden and life satisfaction from 1 to 2 years after severe traumatic brain injury: A Norwegian longitudinal study. NeuroRehabilitation 2017;40(2):211–222. [DOI] [PubMed] [Google Scholar]
- 22.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist 1990;30(5):583–594. [DOI] [PubMed] [Google Scholar]
- 23.Martin Y, Gilbert P, Mcewan K, Irons C. The relation of entrapment, shame and guilt to depression, in carers of people with dementia. Aging & Mental Health 2006;10(2):101–106. [DOI] [PubMed] [Google Scholar]
- 24.ALS Association. http://www.alsa.org/. Accessed 09/11, 2017.
- 25.Lezak MD. Living with the characterologically altered brain injured patient. J Clin Psychiatry 1978;39(7):592–598. [PubMed] [Google Scholar]
- 26.Carlozzi NE, Brickell TA, French LM, et al. Caring for our wounded warriors: A qualitative examination of health-related quality of life in caregivers of individuals with military-related traumatic brain injury. Journal of Rehabilitation Research & Development 2016;53(6):669–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carlozzi NE, Kratz AL, Sander AM, et al. Health-related quality of life in caregivers of individuals with traumatic brain injury: development of a conceptual model. Archives of Physical Medicine & Rehabilitation 2015;96(1):105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ergh TC, Rapport LJ, Coleman RD, Hanks RA. Predictors of caregiver and family functioning following traumatic brain injury: social support moderates caregiver distress. J Head Trauma Rehabil 2002;17(2):155–174. [DOI] [PubMed] [Google Scholar]
- 29.Vangel SJ Jr., Rapport LJ, Hanks RA. Effects of family and caregiver psychosocial functioning on outcomes in persons with traumatic brain injury. J Head Trauma Rehabil 2011;26(1):20–29. [DOI] [PubMed] [Google Scholar]
- 30.Carlozzi NE, Kallen MA, Hanks R, et al. The TBI-CareQOL Measurement System: Development and validation of health-related quality of life measures for caregivers of civilians and service members/veterans with traumatic brain injury. Archives of Physical Medicine & Rehabilitation Under Review, This Issue. [DOI] [PMC free article] [PubMed]
- 31.Hanauer DA, Mei Q, Law J, Khanna R, Zheng K. Supporting information retrieval from electronic health records: A report of University of Michigan’s nine-year experience in developing and using the Electronic Medical Record Search Engine (EMERSE). Journal of Biomedical Informatics 2015;55:290–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dikmen S, Corrigan JD, Levin HS, Machamer J, Stiers W, Weisskopf MG. Cognitive outcome following traumatic brain injury. Journal of Head Trauma Rehabilitation 2009;24(6):430–438. [DOI] [PubMed] [Google Scholar]
- 33.Dikmen S, Machamer JE, Winn HR, Temkin NR. Neuropsychological Outcome at 1-Year Post Head-Injury. Neuropsychology 1995;9(1):80–90. [Google Scholar]
- 34.Dikmen S, Mclean A, Temkin N. Neuropsychological and Psychosocial Consequences of Minor Head-Injury. Journal of Neurology Neurosurgery and Psychiatry 1986;49(11):1227–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dikmen S, Reitan RM, Temkin NR. Neuropsychological recovery in head injury. Archives of Neurology 1983;40(6):333–338. [DOI] [PubMed] [Google Scholar]
- 36.Burns AS, Marino RJ, Flanders AE, Flett H. Clinical diagnosis and prognosis following spinal cord injury. Handb Clin Neurol 2012;109:47–62. [DOI] [PubMed] [Google Scholar]
- 37.Ditunno JF Jr., Stover SL, Freed MM, Ahn JH. Motor recovery of the upper extremities in traumatic quadriplegia: a multicenter study. Arch Phys Med Rehabil 1992;73(5):431–436. [PubMed] [Google Scholar]
- 38.Waters RL, Yakura JS, Adkins RH, Sie I. Recovery following complete paraplegia. Arch Phys Med Rehabil 1992;73(9):784–789. [PubMed] [Google Scholar]
- 39.Waters RL, Adkins RH, Yakura JS, Sie I. Motor and sensory recovery following complete tetraplegia. Arch Phys Med Rehabil 1993;74(3):242–247. [PubMed] [Google Scholar]
- 40.Waters RL, Adkins RH, Yakura JS, Sie I. Motor and sensory recovery following incomplete paraplegia. Arch Phys Med Rehabil 1994;75(1):67–72. [PubMed] [Google Scholar]
- 41.Waters RL, Adkins R, Yakura J, Sie I. Donal Munro Lecture: Functional and neurologic recovery following acute SCI. J Spinal Cord Med 1998;21(3):195–199. [DOI] [PubMed] [Google Scholar]
- 42.Jorgensen HS, Nakayama H, Raaschou HO, Vive-Larsen J, Stoier M, Olsen TS. Outcome and time course of recovery in stroke. Part II: Time course of recovery. The Copenhagen Stroke Study. Arch Phys Med Rehabil 1995;76(5):406–412. [DOI] [PubMed] [Google Scholar]
- 43.Jorgensen HS, Nakayama H, Raaschou HO, Vive-Larsen J, Stoier M, Olsen TS. Outcome and time course of recovery in stroke. Part I: Outcome. The Copenhagen Stroke Study. Arch Phys Med Rehabil 1995;76(5):399–405. [DOI] [PubMed] [Google Scholar]
- 44.Zaider TI, Heimberg RG, Fresco DM, Schneier FR, Liebowitz MR. Evaluation of the clinical global impression scale among individuals with social anxiety disorder. Psychological Medicine 2003;33(4):611–622. [DOI] [PubMed] [Google Scholar]
- 45.Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Medical Care 2007;45(5 Suppl 1):S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol 2010;63(11):1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.PARSCALE [computer program] Lincolnwood, IL: Scientific Software International Inc; 2003. [Google Scholar]
- 48.McDonald RP. Test theory: A unified treatment Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 1999. [Google Scholar]
- 49.Cook KF, Kallen MA, Amtmann D. Having a fit: Impact of number of items and distribution of data on traditional criteria for assessing IRT’s unidimensionality assumption. Quality of Life Research 2009;18(4):447–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reise SP, Morizot J, Hays RD. The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Quality of Life Research 2007;16 Suppl 1:19–31. [DOI] [PubMed] [Google Scholar]
- 51.Muthén LK, Muthén BO. Mplus User’s Guide Los Angeles, CA: Muthén & Muthén; 2011. [Google Scholar]
- 52.TestGraf [computer program] Canada: McGill University; August 1, 2000. [Google Scholar]
- 53.Samejima F, van der Liden WJ, Hambleton R. The graded response model. In: van der Liden WJ, ed. Handbook of modern item response theory NY, NY: Springer; 1996:85–100. [Google Scholar]
- 54.IRTPRO for Windows [Computer software] [computer program] Lincolnwood, IL: Scientific Software International; 2011. [Google Scholar]
- 55.Crane PK, Gibbons LE, Jolley L, van Belle G. Differential item functioning analysis with ordinal logistic regression techniques. DIFdetect and difwithpar. Medical Care 2006;44(11 Suppl 3):S115–123. [DOI] [PubMed] [Google Scholar]
- 56.R: A language and environment for statistical computing. [computer program] Vienna, Austria: R Foundation for Statistical Computing; 2014. [Google Scholar]
- 57.Choi SW, Gibbons LE, Crane PK. Lordif: An R package for detecting differential item functioning using iterative hybrid ordinal logistic regression/item response theory and monte carlo simulations. Journal of Statistical Software 2011;39(8):1–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kline RB. Principles and Practice of Structural Equation Modeling, Second Edition. New York: Guilford Press; 2005. [Google Scholar]
- 59.Bentler PM. Comparative Fit Indexes in Structural Models. Psychological Bulletin 1990;107(2):238–246. [DOI] [PubMed] [Google Scholar]
- 60.Hu LT, Bentler PM. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria Versus New Alternatives. Structural Equation Modeling-a Multidisciplinary Journal 1999;6(1):1–55. [Google Scholar]
- 61.Hatcher L A step-by-step approach to using SAS for factor analysis and structural equation modeling Cary, NC: SAS Institute, Inc; 1994. [Google Scholar]
- 62.Choi SW. Firestar: Computerized Adaptive Testing Simulation Program for Polytomous Item Response Theory Models. Applied Psychological Measurement 2009;33(8):644–645. [Google Scholar]
- 63.Carlozzi NE, Lange R, French L, et al. Reliability and validity data for the TBI-CareQOL measurement system: Data from caregivers of civilian- and military-related traumatic brain injury. Under Review [DOI] [PMC free article] [PubMed]
- 64.Smith AM, Schwirian PM. The relationship between caregiver burden and TBI survivors’ cognition and functional ability after discharge. Rehabilitation Nursing 1998;23(5):252–257. [DOI] [PubMed] [Google Scholar]
- 65.Florian V, Katz S, Lahav V. Impact of traumatic brain damage on family dynamics and functioning: A review. Brain Injury 1989;3(3):219–233. [DOI] [PubMed] [Google Scholar]
- 66.McLaughlin AM, Carey JL. The adversarial alliance: developing therapeutic relationships between families and the team in brain injury rehabilitation. Brain Injury 1993;7(1):45–51. [DOI] [PubMed] [Google Scholar]
- 67.Pelletier PM, Alfano DP. Depression, social support, and family coping following traumatic brain injury. Brain and Cognition 2000;44(1):45–49. [Google Scholar]
- 68.Sander AM, Caroselli JS, High WM, Becker C, Neese L, Scheibel R. Relationship of family functioning to progress in a post-acute rehabilitation programme following traumatic brain injury. Brain Injury 2002;16(8):649–657. [DOI] [PubMed] [Google Scholar]
- 69.Sander AM, Maestas KL, Sherer M, Malec JF, Nakase-Richardson R. Relationship of caregiver and family functioning to participation outcomes after postacute rehabilitation for traumatic brain injury: a multicenter investigation. Arch Phys Med Rehabil 2012;93(5):842–848. [DOI] [PubMed] [Google Scholar]
- 70.Sady MD, Sander AM, Clark AN, Sherer M, Nakase-Richardson R, Malec JF. Relationship of preinjury caregiver and family functioning to community integration in adults with traumatic brain injury. Arch Phys Med Rehabil 2010;91(10):1542–1550. [DOI] [PubMed] [Google Scholar]