Abstract
Aerobic exercise has received increasing attention in the scientific literature as a component of management for individuals who sustain a concussion. Since exercise training has been reported to reduce symptoms and improve function for those experiencing persistent postconcussion symptoms, it represents a potentially useful and clinically pragmatic rehabilitation technique. However, the specific exercise parameters that best facilitate recovery from concussion remain poorly defined and unclear. This review will provide a brief summary of the current understanding of the role of sub-symptom exercise to improve outcomes after a concussion and will describe the exercise parameters that appear to be important. This latter will take into account the three pillars of exercise dose – frequency, duration, and intensity – to examine what is currently known. In addition, we identify important gaps in our knowledge of exercise as a treatment for those who develop persistent symptoms of concussion.
Keywords: aerobic exercise, concussion, symptom, postconcussion syndrome, rehabilitation
Introduction
The incidence of sport-related concussion, defined as a mild traumatic brain injury induced by biomechanical forces (1), has steadily increased over the past decade (2, 3). Although concussion symptoms most often resolve within the first month of injury, a substantial proportion of patients continue to experience persistent symptoms that last more than a month after the injury (4), leading to loss of school or work, loss of function, and/or loss of sports participation. Currently, treatment protocols to improve outcomes and to reduce symptom burden are not well established and are based on expert opinion rather than empirical data (1). Until recently, a major recommendation for concussion recovery was physical rest. In 2013, consensus-based recommendations were that patients should rest until symptom resolution before beginning physical activity (5). However, consensus-based recommendations published in 2017 recommend that limited physical activity is safe prior to complete symptom resolution, and that participation in symptom-limited exercise can be beneficial for concussion recovery (1). This recommendation was based primarily on studies showing sub-symptom exercise improves self-reported symptoms in individuals who are slow to recover from concussion (6–9). Lending further support to this notion, results from animal models suggest a beneficial effect of voluntary exercise after traumatic brain injury leading to enhanced recovery potential (10). The majority of clinical studies, although not all, have focused on the role of exercise to improve outcomes among individuals with persistent concussion symptoms (7–9, 11–14), typically defined as the presence of symptoms lasting for more than 28 days after injury (4, 15, 16), rather than those with acute symptoms. Although a recent meta-analysis reported that exercise was associated with decreased symptom severity (17), the specific exercise parameters that best facilitate recovery from the persistent symptoms of concussion remain poorly defined and unclear in the existing literature.
Though the physiological benefits of aerobic exercise are well known, it is important to note that there is a dose-response relationship between the amount of aerobic exercise performed and its benefits; exercise below a minimum ‘dose’ may not yield any physiological benefits (18). In all individuals, whether or not they have experienced a concussion, exercise must meet certain threshold criteria. Therefore, regular aerobic exercise must take into account the three pillars of an exercise prescription: frequency, duration, and intensity. In addition, there are other important considerations such as the length of the exercise treatment, the modality of exercise used, and the timing and progression of the exercise intervention. The aim of this review is to survey the parameters of aerobic exercise that should be considered when implementing concussion treatment programs as a method to improve outcomes following concussion. We will first define the exercise prescription, then examine the existing studies that have used exercise to affect concussion outcomes grouped by study design, and finally describe the components of an exercise prescription relative to concussion interventions.
Defining the Exercise Prescription
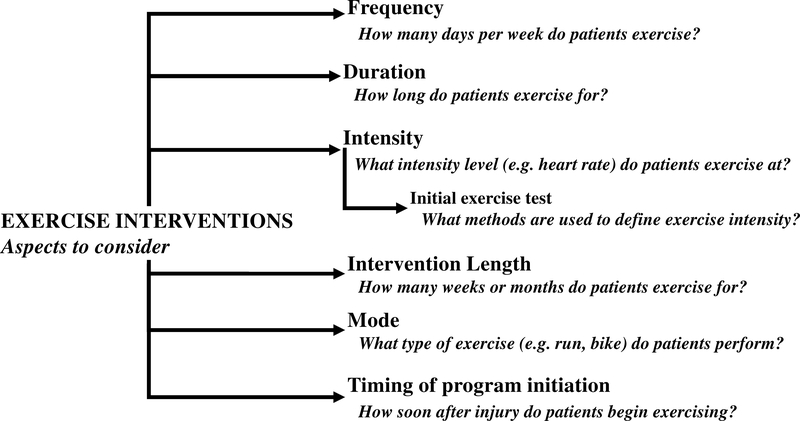
Defining and reporting the exercise parameters used by study participants in any intervention study will help researchers and clinicians to clearly interpret the findings. Most studies that have investigated the role of aerobic exercise to facilitate concussion recovery in patients who are slow to recover did not measure adherence to suggested exercise prescriptions or have a non-exercise control group with which to compare outcomes. As a result, in many cases the results cannot be clearly interpreted in relation to the prescription or in relation to spontaneous abatement of symptoms. Nonetheless, the data are suggestive of a beneficial effect, though mild. The optimal frequency, duration, and intensity of prescribed exercise remain equivocal. Recently, concussion care has evolved from physical and cognitive rest to individualized and progressive management of activity following a 24–48 hour period of post-injury rest (19). As a result of this development, there is heightened interest in using exercise as a form of treatment for concussion rehabilitation. While encouraging individuals to remain physically active after injury represents a step forward, there are still many gaps in the literature to date on how specifically exercise affects concussion outcomes. Few studies report outcomes necessary to convey the precise effects of exercise on concussion recovery. As such, exercise prescription elements, such as intensity, frequency, duration, intervention length, mode, and timing of initiation of an exercise regimen should be considered in future study designs (Figure 1). Causal effects due to exercise, rather than correlational, can be determined only if information about each of these parameters are provided (11, 20, 21). However, most studies report on only some of these elements (Table 1), and consequently, it is currently difficult to determine the effect of exercise on concussion recovery. Of primary importance for future studies, defining the exercise prescription used as well as including time-matched controls can help to determine the efficacy of exercise.
Figure 1.
The six parameters of exercise dosage to consider when implementing and reporting on the use of aerobic exercise as a treatment for concussion.
Table 1.
The parameters of exercise dosage used in existing studies evaluating the effect of aerobic exercise on concussion outcomes.
| Lead Author | Exercise frequency | Exercise duration | Intensity | Intervention length | Mode of exercise | Timing of program initiation |
|---|---|---|---|---|---|---|
| Dobney (20) | Daily | 20 – 30 minutes/day | Perceived level of effort corresponding to target HR zone | N/A | Stationary bike or treadmill | 3–4 weeks post-concussion (mean=28 days post-injury) |
| Chan (26) | N/A | 15 minutes/day | 60% of age-predicted maximum HR | 6 weeks | Stationary bike or treadmill | ≥ 4 weeks post-concussion |
| Chrisman (11) | N/A | Maximum 20 minutes/day | 80% of symptom exacerbation HR | > 1 week | N/A | ≥ 1 month and < 300 days post-concussion |
| Grool (21) | N/A | N/A | Self-reported as none, light, moderate, or full physical activity | 7 days | N/A | Within 7 days of concussion |
| Moore (24) | 3–5 days/week | 20–30 minutes/day | 60–80% of symptom exacerbation HR | 6 months | Stationary bike | Median= 107 days postconcussion Range= 14–992 days |
| Grabowski (12) | 5–6 days/week | Duration achieved during initial exercise test | 80% of symptom exacerbation HR | Median = 84 days Range = 7–266 days | Patient preference | ≥ 3 weeks and <36 weeks post-concussion Median = 41 days post-concussion |
| Cordingley (9) | 5 days/week | 20 minutes/day | 80% of symptom exacerbation HR | Until return-to-play or specialist referral | N/A | ≥ 1 month post-concussion Median = 35 days |
| Kurowski (13) | 5–6 days/week | 80% of the exercise test duration that exacerbated symptoms | Gradual increase to Borg RPE that exacerbates symptoms | 6 weeks | Stationary bike | 4–16 weeks post-concussion |
| Clausen (8) | 5–6 days/week | 20 minutes/day | 80% of symptom exacerbation HR | 12 weeks | Treadmill | 6–12 weeks post-concussion |
| Gagnon (6) | Daily | 20 – 30 minutes/day | 60% of age-predicted HR maximum | Median=5.5 weeks Range=2–15.2 weeks | Stationary bike or treadmill | ≥ 4 weeks post-concussion |
| Leddy (7) | 6 days/week | 20 minutes/day | 80% of symptom exacerbation HR | 12 weeks | N/A | ≥ 6 weeks and < 12 months post-concussion |
Note: N/A (Not available), HR (heart rate), RPE (rating of perceived exertion).
Existing Aerobic Exercise Intervention Studies
Studies with no defined exercise prescription and no control
In a prior systematic review of studies that assessed any type of treatment for concussion, one conclusion was that the common methodological limitations for rehabilitation research in this area include a lack of control group, randomization procedures, and controlling for potential confounding variables (22). With such limitations, studies of aerobic exercise after concussion that show changes in symptom burden from pre- to post-program are difficult to interpret (11, 20). As pointed out by Chrisman and colleagues, it is impossible to know if study participants would have reported improvement over time regardless of intervention (11). Studies that use observational or chart review designs and simply follow patients across time who were engaged in an exercise regimen without specified intensity, frequency, or duration of exercise testing (11, 20, 23), yield only limited useful information (Table 1). Nonetheless, following initiation of a home-based exercise program, decreased symptom severity has been reported (11, 20). While the rate of symptom improvement did not vary by how long after injury the intervention began (11), female patients reported higher symptom severity at follow-up compared to male patients (20). Therefore, while these studies demonstrate that exercise can be performed by those with persistent postconcussion symptoms, the lack of a control group or precise exercise intervention specifics limits the ability to interpret the precise role that initiating an exercise program plays on symptom improvement.
Studies with a defined exercise prescription and no control
While numerous studies describe the prescribed exercise for patients with persistent postconcussion symptoms who begin an exercise program (6, 9, 12, 24) (Table 1), they do not include a comparison group to assess the efficacy of the specified intervention. Three studies have reported statistically significant improvements in overall symptom severity or in the severity of specific symptoms after the aerobic exercise intervention relative to the initial test (6, 12, 24). Others reported the majority of persistent postconcussion symptom patients who completed the exercise intervention were able to return to full daily functioning (25) or sport participation (9). Results from this body of work do provide support for the hypothesis that exercise may improve outcomes for those who continue to experience symptoms after a concussion. However, as improved outcomes may be a result of the natural course of recovery, study designs without a control group do not provide information about the efficacy of exercise as a treatment for persistent concussion symptoms. Nonetheless, these findings are useful, as they indicate that patients experiencing persistent concussion symptoms can complete a sub-symptom aerobic exercise program without significant worsening. This implies that initiating aerobic exercise programs among patients who are experiencing persistent postconcussion symptoms may at least be safe and not detrimental.
Studies with a defined exercise prescription and control
There are four studies that report both a defined exercise prescription and a control group to assess the efficacy of an exercise-based intervention protocol on participants who are slow to recover from concussion. These studies each enrolled participants who continued to have symptoms for more than 4 weeks after injury with intervention durations ranging from 6 weeks (13, 26) to 12 weeks (7, 8). Each of the intervention groups completed an initial exercise test to determine appropriate intensity, and began sub-symptom aerobic exercise at levels from 60% of age-predicted maximal heart rate (26) or 80% of peak heart rate at exercise test cessation (7, 8), with a duration of 15–30 minutes per day for 5–6 days per week (Table 1). The non-exercise control groups varied between studies. Two studies enrolled individuals with a concussion into a non-exercise based full-body stretching program (7, 13) and another followed individuals who received treatment as usual (26). In an attempt to determine the converse of exercise for concussion treatment, one study used a group of healthy athletes who regularly exercise as a comparison for the effects of concussion on the responses to aerobic exercise intervention (8). In the first three studies, exercise training was associated with a lower symptom burden (7, 13, 26). However, it is important to note that patients in these studies were in the chronic stage of their injury (i.e., they were experiencing persistent concussion symptoms at the beginning of the exercise). Thus, while these studies collectively point toward a beneficial effect of sub-symptom aerobic exercise training, they may not apply to patients in the acute stage of concussion recovery.
Studies of acute postconcussion exercise effects
As noted, the majority of concussion-related aerobic exercise studies focus on patients who begin exercise at least four weeks after the injury. Relative to the overall body of literature in this area, there are far fewer studies that have evaluated the effect of sub-symptom aerobic exercise on concussion symptoms when an exercise program is initiated within the first four weeks of injury. One study by Leddy and colleagues observed that within the first ten days of a concussion, graded treadmill exercise testing was not associated with a longer symptom recovery time or worsened symptom severity, suggesting that acute post-concussion exercise testing does not produce detrimental effects (27). Similarly, Micay and colleagues reported that among adolescents, implementation of a standardized aerobic exercise intervention beginning 6 days after concussion was both feasible and safe for patients to engage in, and was associated with a faster symptom severity reduction across time (28). Furthermore, earlier initiation of an aerobic exercise program after a concussion was associated with faster return to sport and return to school/work times, suggesting that aerobic exercise interventions initiated may result with a more rapid recovery than standard care (29). Other studies have assessed physical activity levels, rather than an aerobic exercise intervention, but noted physical activity initiation within 7 days of a concussion was associated with a lower risk of developing persistent postconcussion symptoms (21). Taken together, these results suggest that in addition to being a viable treatment option for those with persistent postconcussion symptoms, initiating some form of physical activity soon after a concussion may represent a method to reduce the risk of developing persistent postconcussion symptoms.
Exercise Frequency, Intensity, and Duration
The dose of an exercise training program is comprised of intensity, frequency, duration, mode, pattern, and volume (Figure 1). Exercise training undertaken with regularity should lead to the development of cardiorespiratory fitness. However, the American College of Sports Medicine (ACSM) has published a Position Stand on the Quality and Quantity of Exercise (18) and recommended moderate- or vigorous-intensity exercise in order to achieve improved fitness among apparently healthy adults. Accordingly, exercise intensity is considered the most important parameter of an exercise program (18).
Exercise intensity is commonly expressed as heart rate (HR), percentage of maximum heart rate, heart rate reserve, percent of maximal aerobic capacity (VO2max), and/or VO2 reserve. To observe adaptations to regular aerobic exercise, it is recommended that healthy adults complete moderate and/or vigorous intensity exercise, defined as exercise at 60–80% (moderate) or >80% (vigorous) of maximum intensity (30). Obviously, this recommendation in athletes who have recently sustained a concussion should be balanced against the symptom status of the patient at the individual level. While expert consensus guidelines advise “light activity” after a brief rest period following a concussion (1), the prescribed intensity for athletes following a concussion should be one that does not exacerbate symptoms (7–9, 11, 12, 24). Other general exercise recommendations put forth by ACSM include:
Frequency: 5 days/week of moderate intensity or >3 days/week of vigorous intensity exercise
Duration: 30–60 min/day (150 min/week) at moderate intensity or 20–60 min/day (75 min/week) at vigorous intensity
Mode: exercise using major muscle groups. Examples include walking, jogging, cycling, or swimming.
Volume: ≥ 500–1000 Metabolic Equivalent Task (MET) min/week. One MET is defined as the amount of oxygen consumed during quiet sitting: 3.5 ml O2/kg/min. Activities are expressed in multiples of MET, and MET min measures the activity in METs and the duration (min) spent in that activity (31).
Pattern: Exercise is ideally performed as a single continuous session, however, multiple sessions of ≥ 10 min can be performed to accumulate the desired duration or volume of exercise.
Progression: Gradual progression of the exercise volume by adjusting exercise duration, intensity and/or frequency is recommended to gain continued aerobic fitness improvements.
Thus, concussion studies should assess the exercise dose of their training program using the above components to allow comparisons of programs and assessment of the results and reported benefits. In the concussion literature, it appears that many programs adhered to similar standards as those set forth by ACSM for exercise quantity and quality. For example, Clausen and colleagues implemented an exercise program among patients who were still symptomatic at least six weeks after injury that consisted of running on a treadmill at 80% of the HR that exacerbated symptoms, 5–6 days per week, 20 minutes per day, for a 12 week period (8). Participants in the exercise group achieved a higher HR relative to a control group during follow-up exercise testing, indicating that this level of training may evoke a physiological effect on exercise capacity and cardiovascular fitness among those who are slow to recover from concussion. In addition, Gagnon and colleagues reported that exercising on a stationary bike or treadmill at 60% of age-predicted HR maximum for 15 minutes per day, 7 days per week, for 6 weeks led to decreased fatigue and improved mood among patients who began this program at least 4 weeks after concussion (6). This suggests that the ACSM recommendations for healthy individuals may be a useful guide to apply among a group of individuals who have sustained a concussion and continue to experience symptoms for longer than the typical recovery duration.
Exercise Testing Protocols and Intervention Duration
A plethora of test protocols to assess cardiorespiratory fitness with reported validity and reliability are available. They primarily include the laboratory tests using treadmill, cycle, and step ergometers as well as field tests such as 20m shuttle run and Coopers 12-minute run. Laboratory tests increase workloads at incremental/graded intensity and completed at exhaustion (maximal HR) or at a percentage of maximal (submaximal HR). The appropriate selection of a test protocol should reflect the population, specificity of exercise being assessed, and purpose of the test. Within the realm of exercise testing protocols for patients with concussion, the most commonly reported method is a graded treadmill exercise test, or the Buffalo Concussion Treadmill Test (BCTT) (7–9, 11, 12, 25, 32). The BCTT was developed as an adaptation specifically for concussion patients based upon the Balke protocol, intended to increase exercise intensity gradually until symptoms are evoked (14). Typically, patients walk on a treadmill until symptom onset or maximal exhaustion is achieved by beginning at a speed of 3.2 mph and 0% grade, with a 1% increased grade during each of the first 15 minutes of the trial and an increase of 0.2 mph for the subsequent duration of the test (9, 32). Once symptoms are evoked or exacerbated, typically defined as a 3 point or greater increase in visually-rated symptoms (27), the test administrator stops the test. Exercise intensity recommendations for subsequent training are based upon a percentage (i.e. 80%) of the heart rate at which symptoms are evoked, thereby creating a “sub-symptom” intensity level for use in subsequent exercise. Others, such as Kurowski et al., have used a recumbent stationary bike to determine exercise intensity (13). The concepts of this protocol are similar to the BCTT. Participants biked at a speed consistent with a Borg-scale Rating of Perceived Exertion level of 11 and gradually increased Borg-scale intensity by 1 level until they experienced symptom exacerbation. Similar designs have been used by others, where exercise is completed on a stationary bike and resistance is increased gradually until symptom worsening (6, 20). Thus, the majority of exercise intensity recommendations for patients with persistent postconcussion symptoms have been based on a target HR set below the HR that exacerbates symptoms during initial intensity testing.
Adaptations and improvements from aerobic exercise training are seen after approximately six to eight weeks of training, dependent on the dose of exercise and the initial level of fitness. An additional consideration is compliance or adherence to the program. Once the exercise training ceases, the accrued benefits can be lost in as little as one to two weeks (18). The duration of exercise programs used to improve symptoms and function after a concussion range widely, as published studies report a pre-/post-testing interval ranging from at least 1–2 weeks (11) to a duration of 6 months (24). More commonly, an intervention duration of 4–8 weeks (20), 6 weeks (6, 13, 26, 33), or 12 weeks (7, 8, 12) have been used to assess pre and post-test symptoms or aerobic levels. The duration of exercise programs does not appear to affect symptoms, as each of these studies report symptom reduction regardless of the length of exercise program prescribed. However, given that as few as 4–8 weeks can lead to symptom abatement, the effects on postconcussion symptoms may occur independent of other systemic adaptations to exercise training. Thus, the cause and effect relationship between exercise program length and concussion recovery cannot be fully deduced from these studies.
Conclusion
Current evidence supports the notion that sub-symptom aerobic exercise is a beneficial treatment strategy for athletes after a concussion. However, the effect of training intensity, duration, frequency, or program duration within aerobic exercise programs on concussion recovery remains unknown. In addition, the efficacy of initiating an exercise training protocol within the first month of a concussion has not yet been evaluated to the same degree as protocols that begin after persistent symptoms have developed. Therefore, while promising, there are many additional areas that require investigation to fully determine the physiologic effect of aerobic exercise among those who are recovering from a concussion.
Among the areas that require further exploration is determining whether the improvements that patients report following an exercise program are due to a physiologic mechanism. If the effect of an exercise program on symptom resolution, for example, is simply not physiologically detrimental, then the observed positive benefits may relate to the psychological or social benefits that come with exercise. If there is truly a physiological benefit to exercise, however, this likely would require a program duration of greater than 6 weeks (34), a duration of time that outlasts the expected recovery for most patients recovering from a sport-related concussion. Future prospective studies are required to assess the causal effects pertaining to concussion recovery, namely the specific parameters of an exercise program and the association between symptom resolution with psychosocial function, physiologic function, or a combination of these factors.
Acknowledgements
This work was funded by The Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (R03HD094560) and The National Institute of Neurological Disorders and Stroke of the National Institutes of Health (R03NS106444).
Footnotes
Conflict of Interest
The results of the present study do not constitute endorsement by ACSM. Our work is presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
References
- 1.McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838–47. [DOI] [PubMed] [Google Scholar]
- 2.Lincoln AE, Caswell SV, Almquist JL, Dunn RE, Norris JB, Hinton RY. Trends in concussion incidence in high school sports: a prospective 11-year study. Am J Sports Med. 2011;39(5):958–63. [DOI] [PubMed] [Google Scholar]
- 3.Rosenthal JA, Foraker RE, Collins CL, Comstock RD. National high school athlete concussion rates from 2005–2006 to 2011–2012. Am J Sports Med. 2014;42(7):1710–5. [DOI] [PubMed] [Google Scholar]
- 4.Steindel SJ. International classification of diseases, 10th edition, clinical modification and procedure coding system: descriptive overview of the next generation HIPAA code sets. J Am Med Inform Assoc JAMIA. 2010;17(3):274–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47(5):250–8. [DOI] [PubMed] [Google Scholar]
- 6.Gagnon I, Grilli L, Friedman D, Iverson GL. A pilot study of active rehabilitation for adolescents who are slow to recover from sport-related concussion. Scand J Med Sci Sports. 2016;26(3):299–306. [DOI] [PubMed] [Google Scholar]
- 7.Leddy JJ, Cox JL, Baker JG, et al. Exercise treatment for postconcussion syndrome: a pilot study of changes in functional magnetic resonance imaging activation, physiology, and symptoms. J Head Trauma Rehabil. 2013;28(4):241–9. [DOI] [PubMed] [Google Scholar]
- 8.Clausen M, Pendergast DR, Willer B, Leddy J. Cerebral Blood Flow During Treadmill Exercise Is a Marker of Physiological Postconcussion Syndrome in Female Athletes. J Head Trauma Rehabil. 2016;31(3):215–24. [DOI] [PubMed] [Google Scholar]
- 9.Cordingley D, Girardin R, Reimer K, et al. Graded aerobic treadmill testing in pediatric sports-related concussion: safety, clinical use, and patient outcomes. J Neurosurg Pediatr. 2016;25(6):693–702. [DOI] [PubMed] [Google Scholar]
- 10.Griesbach GS, Hovda DA, Molteni R, Wu A, Gomez-Pinilla F. Voluntary exercise following traumatic brain injury: brain-derived neurotrophic factor upregulation and recovery of function. Neuroscience. 2004;125(1):129–39. [DOI] [PubMed] [Google Scholar]
- 11.Chrisman SPD, Whitlock KB, Somers E, et al. Pilot study of the Sub-Symptom Threshold Exercise Program (SSTEP) for persistent concussion symptoms in youth. NeuroRehabilitation. 2017;40(4):493–9. [DOI] [PubMed] [Google Scholar]
- 12.Grabowski P, Wilson J, Walker A, Enz D, Wang S. Multimodal impairment-based physical therapy for the treatment of patients with post-concussion syndrome: A retrospective analysis on safety and feasibility. Phys Ther Sport Off J Assoc Chart Physiother Sports Med. 2017;23:22–30. [DOI] [PubMed] [Google Scholar]
- 13.Kurowski BG, Hugentobler J, Quatman-Yates C, et al. Aerobic Exercise for Adolescents With Prolonged Symptoms After Mild Traumatic Brain Injury: An Exploratory Randomized Clinical Trial. J Head Trauma Rehabil. 2017;32(2):79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leddy JJ, Baker JG, Kozlowski K, Bisson L, Willer B. Reliability of a graded exercise test for assessing recovery from concussion. Clin J Sport Med Off J Can Acad Sport Med. 2011;21(2):89–94. [DOI] [PubMed] [Google Scholar]
- 15.Zemek R, Barrowman N, Freedman SB, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. 2016;315(10):1014–25. [DOI] [PubMed] [Google Scholar]
- 16.Howell DR, Zemek R, Brilliant AN, Mannix RC, Master CL, Meehan WP. Identifying Persistent Postconcussion Symptom Risk in a Pediatric Sports Medicine Clinic. Am J Sports Med. 2018;363546518796830. [DOI] [PubMed] [Google Scholar]
- 17.Lal A, Kolakowsky-Hayner SA, Ghajar J, Balamane M. The Effect of Physical Exercise After a Concussion: A Systematic Review and Meta-analysis. Am J Sports Med. 2017;363546517706137. [DOI] [PubMed] [Google Scholar]
- 18.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59. [DOI] [PubMed] [Google Scholar]
- 19.Giza CC, Choe MC, Barlow KM. Determining If Rest Is Best After Concussion. JAMA Neurol. 2018;75(4):399–400. [DOI] [PubMed] [Google Scholar]
- 20.Dobney DM, Grilli L, Kocilowicz H, et al. Evaluation of an active rehabilitation program for concussion management in children and adolescents. Brain Inj. 2017;1–7. [DOI] [PubMed] [Google Scholar]
- 21.Grool AM, Aglipay M, Momoli F, et al. Association Between Early Participation in Physical Activity Following Acute Concussion and Persistent Postconcussive Symptoms in Children and Adolescents. JAMA. 2016;316(23):2504–14. [DOI] [PubMed] [Google Scholar]
- 22.Schneider KJ, Leddy JJ, Guskiewicz KM, et al. Rest and treatment/rehabilitation following sport-related concussion: a systematic review. Br J Sports Med. 2017;51(12):930–94. [DOI] [PubMed] [Google Scholar]
- 23.Howell DR, Mannix RC, Quinn B, Taylor JA, Tan CO, Meehan WP. Physical activity level and symptom duration are not associated after concussion. Am J Sports Med. 2016;44(4):1040–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moore BM, Adams JT, Barakatt E. Outcomes Following a Vestibular Rehabilitation and Aerobic Training Program to Address Persistent Post-Concussion Symptoms. J Allied Health. 2016;45(4):e59–68. [PubMed] [Google Scholar]
- 25.Baker JG, Freitas MS, Leddy JJ, Kozlowski KF, Willer BS. Return to full functioning after graded exercise assessment and progressive exercise treatment of postconcussion syndrome. Rehabil Res Pract. 2012;2012:705309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chan C, Iverson GL, Purtzki J, et al. Safety of Active Rehabilitation for Persistent Symptoms After Pediatric Sport-Related Concussion: A Randomized Controlled Trial. Arch Phys Med Rehabil. 2018;99(2):242–9. [DOI] [PubMed] [Google Scholar]
- 27.Leddy JJ, Hinds AL, Miecznikowski J, et al. Safety and Prognostic Utility of Provocative Exercise Testing in Acutely Concussed Adolescents: A Randomized Trial. Clin J Sport Med. 2018;28(1):13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Micay R, Richards D, Hutchison MG. Feasibility of a postacute structured aerobic exercise intervention following sport concussion in symptomatic adolescents: a randomised controlled study [Internet]. BMJ Open Sport — Exerc Med. 2018. [cited 2018 Jul 20]; 4(1) available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6045733/. doi: 10.1136/bmjsem-2018-000404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lawrence DW, Richards D, Comper P, Hutchison MG. Earlier time to aerobic exercise is associated with faster recovery following acute sport concussion. PloS One. 2018;13(4):e0196062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO | What is Moderate-intensity and Vigorous-intensity Physical Activity? WHO. [date unknown]; [cited 2018 Sep 14] Available from: http://www.who.int/dietphysicalactivity/physical_activity_intensity/en/. [Google Scholar]
- 31.Jetté M, Sidney K, Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol. 1990;13(8):555–65. [DOI] [PubMed] [Google Scholar]
- 32.Leddy JJ, Kozlowski K, Donnelly JP, Pendergast DR, Epstein LH, Willer B. A preliminary study of subsymptom threshold exercise training for refractory post-concussion syndrome. Clin J Sport Med. 2010;20(1):21–7. [DOI] [PubMed] [Google Scholar]
- 33.Yuan W, Wade SL, Quatman-Yates C, Hugentobler JA, Gubanich PJ, Kurowski BG. Structural Connectivity Related to Persistent Symptoms After Mild TBI in Adolescents and Response to Aerobic Training: Preliminary Investigation. J Head Trauma Rehabil. 2017;32(6):378–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McArdle WD, Katch FI, Katch VL. Exercise Physiology: Nutrition, Energy, and Human Performance. 8th edition. Philadelphia: LWW; 2014. 1088 p. [Google Scholar]