Abstract
Premenstrual syndrome (PMS) is a common disorder that affects millions of women of reproductive age worldwide. In recent years, there has been a focus on finding accessible, acceptable, and cost-effective therapeutic approaches with minimal side effects to treat the symptoms of PMS. This systematic review aimed to investigate the role of calcium and vitamin D in Premenstrual syndrome. The PubMed, EMBASE, Web of Science, Scopus, Science Direct, and Google Scholar databases were systematically searched for relevant articles from clinical trial, case-control, and cross-sectional studies. The Strengthening the Reporting of Observational Studies in Epidemiology checklist was used to assess the quality of the selected papers. A total of 28 eligible high-quality papers were reviewed. Low serum levels of calcium and vitamin D during the luteal phase of the menstrual cycle were found to cause or exacerbate the symptoms of PMS. Therefore, the administration of calcium and vitamin D supplements or the use of a diet rich in these two substances can restore serum levels and eliminate or reduce the symptoms of PMS. Calcium and vitamin D supplementation are recommended as an inexpensive, low-risk, acceptable, and accessible approach to eliminate or reduce the symptoms of PMS.
Keywords: Premenstrual syndrome, Vitamin D, Calcium
Introduction
Premenstrual syndrome (PMS) is a common disorder that affects millions of women of reproductive age worldwide [1]. PMS is a series of physical symptoms (e.g., edema, weight gain, mastalgia, headache, nasal obstruction, and paresthesia) and psychological complaints (e.g., irritability, anxiety, and depression) experienced by most women during the luteal phase of the menstrual cycle (7–14 days before the menstrual period) [2,3]. The symptoms of PMS can vary from person to person and, since physical, emotional, and behavioral symptoms may have different causes, the biological factors and symptoms of PMS should be separately evaluated [4]. The incidence of PMS depends on the sociocultural conditions and characteristics of the studied women and the diagnostic methods applied. However, the prevalence of PMS has been estimated to be 30–40% among women of reproductive age and 20–32% among premenopausal women [5].
The main cause of PMS is still unknown, and the syndrome is most likely multifactorial. Some researchers argue that hormonal agents and a lack of micronutrients might be involved in the development of PMS [6]. In consideration of the role that various factors can play in PMS, several therapeutic approaches have been proposed for symptom control that include the use of medications, particularly supplements and anti-depressants, dietary modifications, psychological approaches, exercise, and relaxation methods (e.g., yoga). However, researchers are always searching for more efficient, cost-effective, and safer therapies [7]. The World Health Organization and legislative institutions are also interested in the identification of accessible and inexpensive treatments with minimal side effects to control PMS symptoms [8]. According to previous research, 80% of women suffering from PMS seek complementary and alternative therapies [9], and vitamin D and calcium have recently received special attention for the treatment/relief of PMS symptoms.
Vitamin D is a hormone involved in not only calcium and phosphorous metabolism, but also several other important metabolic functions [10,11]. In humans, 80% of the body's daily requirement of vitamin D is usually fulfilled by 7-Dehydrocholesterol on ultraviolet B exposure, and the remaining 20% is received through dietary intake. The role of vitamin D in reducing the risk of PMS is still being studied and seems primarily correlated with the modulation of calcium concentrations, certain neurotransmitters, and sexual steroids [12].
Vitamin D plays a role in the differentiation and proliferation of various cells [13]. Some previous studies reported changes in serum 25-hydroxyvitamin D3 ([25(OH)D3] or [25(OH)D]) during the luteal phase [12]. Ovarian sex hormones induce enzymes that degrade [25(OH)D3]. Estradiol induces incremental catalytic activity of 1-α-hydroxylase and 24-hydroxylase in the liver, which decrease serum [25(OH)D3] [14,15]. Ovarian hormones peak during the luteal phase, and this leads to the degradation of [25(OH)D3] and reduction of its serum levels. As a result, the cyclic disestablishment of serum [25(OH)D3] metabolism by the ovarian hormones could worsen the symptoms of PMS [16]. Vitamin D deficiency is also associated with an increased renin angiotensin aldosterone system function that contributes to increased fluid balance, blood pressure changes, and hypertension [17,18].
Some studies have shown that serum calcium levels increase during different stages of menstrual cycle and are lower during the luteal phase than during the follicular phase [19]. Decreased serum calcium levels have also been reported during the premenstrual period in some women [16]. Different studies suggest that calcium deficiency during the luteal phase of the menstrual cycle can exacerbate PMS symptoms by causing depression, hallucination, and restlessness [20,21]. Moreover, women who have diets rich in vitamin D and calcium are at a lower risk of developing PMS compared to other women [22].
Systematic reviews explicitly summarize the results of previous studies and provide the best form of evidence for an unbiased judgment. To the best of our knowledge, no systematic review has focused on the effects of vitamin D and calcium in the improvement of PMS symptoms, and therefore this study reviewed the role of vitamin D and calcium in PMS. The results of this study can be helpful in decision-making for the administration of alternative therapies to women who want to take advantage of low-risk treatments.
Criteria for considering studies for this review
1. Search strategy
This study was reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. A number of key terms were searched including: ‘premenstrual syndrome’ OR ‘premenstrual dysphoric disorder’ OR ‘premenstrual tension’ OR ‘PMS’ AND ‘vitamin D’ OR ‘cholecalciferol’ OR ‘hydroxycholecalciferol’ OR ‘vitamin D3’ OR ‘25-hydroxyvitamin D3’ AND ‘Calcium’ OR ‘Ca’. In order to collect the data, valid databases (i.e., MEDLINE, ISI Web of Science, PubMed, EMBASE, Scopus, Google Scholar, and Science Direct) were systematically searched (Table 1).
Table 1. Search strategy for PubMed and EMBASE.
| Search number | Search term |
|---|---|
| #1 | 'premenstrual syndrome' [tiab] OR 'premenstrual dysphoric disorder' [tiab] OR 'premenstrual tension' [tiab] OR 'PMS' [tiab] |
| #2 | 'vitamin D' [tiab] OR 'cholecalciferol' [tiab] OR 'hydroxycholecalciferol' [tiab] OR 'vitamin D3' [tiab] OR '25-hydroxyvitamin D3' [tiab] |
| #3 | 'Calcium' [tiab] OR 'Ca' [tiab] |
| #1 AND #2 | |
| #1 AND #3 | |
| #1 AND #2 AND #3 |
2. Inclusion and exclusion criteria
Studies were included if they were published in either English or Persian during 1999–2018 and if they had a case-control, clinical trial, quasi-experimental, or cross-sectional design. Other inclusion criteria were menarche at least one year before the intervention, regular menstrual cycles, moderate to severe PMS symptoms in the second half of the menstrual cycle, no use of hormone therapy or other therapeutic approaches for the treatment of PMS, and no pregnancy.
The exclusion criteria were: chronic diseases; use of calcium and vitamin D supplements; use of other drugs such as anti-diabetes and anti-inflammatory drugs during the six-month period before the intervention; mental disorders such as anxiety, depression, and panic attacks; and migraine headaches.
3. Study selection
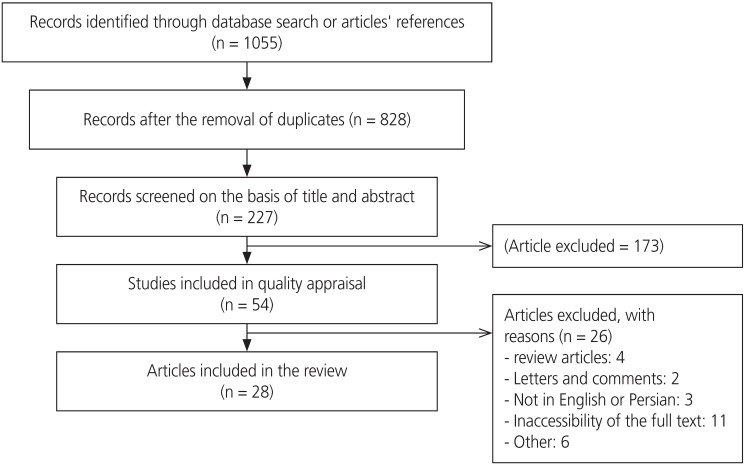
The initial search yielded 1,055 results. The eligibility of these articles was independently evaluated by 2 authors, and any disagreements were resolved through a consensus. During this evaluation, 828 articles were found to be irrelevant or duplicates and were excluded. After reviewing the titles and abstracts of the remaining articles, 173 additional articles were excluded. During the evaluation of the full texts, 26 out of the remaining 54 articles were found ineligible and were excluded. As a result, a total of 28 eligible articles were finally reviewed (Fig. 1).
Fig. 1.
Search flow diagram.
4. Quality assessment
Quality of the quantitative studies was determined by evaluating their adherence to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist [23,24]. The studies that adhered to all 7 items, 6 items, and 2 or more items of the STROBE checklist were classified as having high, medium, and low-quality, respectively.
5. Data extraction
Two authors independently performed the study selection and validity assessment and resolved any disagreements by consulting a third researcher. The first author's name, publication year, country, study design, sample size, chief complaint or problem, intervention group, control group, measures, and outcomes were extracted and entered into the analysis.
Results
After the initial search, the titles and abstracts of the studies extracted from all the databases were examined. The full texts of the studies that were found eligible during the last review stage were then evaluated, and 28 articles were finally analyzed. All of these studies were eligible based on the inclusion criteria and had high-quality according to their adherence to the STROBE checklist. The characteristics of the selected studies are presented in Table 2. The selected studies had different sample sizes (between 39 and 3,025 women) and examined a total of 8,576 women. The participants of the selected studies were of different ages and from different geographical areas including Iran (n=15), India (n=4), the USA (n=4), Indonesia (n=1), Palestine (n=1), Jordan (n=1), Italy (n=1), and Egypt (n=1). The selected studies used clinical trial (n=16), case-control (n=7), cross-sectional (n=4), and quasi-experimental (n=1) designs. The results of the quality assessment of the quantitative studies based on their adherence to the STROBE checklist are detailed in Table 3.
Table 2. Characteristics of the studies included in the systematic review.
| Author | Country | Study type | Chief complaint | Sample size | Intervention group | Control group | Measure | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Bahrami et al. [25] | Iran | RCT | - PMS | 897 | - Nine capsules containing 50,000 IU of vit D for 9 weeks | Without control group | - Serum [25(OH)D3] | - Reduced incidence of PMS: 10.1% |
| - Dysmenorrhea | - Individuals rated scale | - Reduced incidence of PMS and dysmenorrhea: 7% | ||||||
| - Reduced incidence of vit D deficiency: 6.1% | ||||||||
| Dadkhah et al. [26] | Iran | RCT | PMS | 86 | - A tablet containing 200 mg vit D daily for 2 months | Placebo | - Daily rating test | - Decreased incidence of PMS symptoms in vit D group from 37.4 to 25.5 and in vit E group from 38.4 to 22.8 |
| - 100 mg vit E daily for 2 months | ||||||||
| Ghanbari et al. [27] | Iran | RCT | PMS | 179 | - 500 mg of Ca carbonate twice daily for 3 months | Placebo | - Breast tenderness, fatigue, lack of energy, appetite changes, sleep problems, headache, depression, agitation, and irritability | - Dropped mean symptom scores from 7.2±3.8 to 6±3.6 in intervention group and from 6.5±3.6 to 5.8±3.8 in placebo group |
| - Beck test | ||||||||
| Karimi et al. [28] | Iran | RCT | PMS | 40 | - The CBT group (trained in weekly 45-minute sessions for 8 weeks; each week included 1 training session) | Control group | - PSST questionnaire | - Dropped mean PSST scores from 19±1.7 to 14.3±4.1 in CBT group, from 29±5 to 18.8±9.1 in Ca+vit D group, from 41.2±2.1 to 9.1±2.6 in group, Ca+vit D and CBT, and from 27.5±9.5 to 27.2±9.4 in control group |
| - The Ca+vit D group (with 500 mg of Ca and 200 IU of vit D, prescribed twice a day) | ||||||||
| - CBT+Ca+vit D group | ||||||||
| Kermani et al. [29] | Iran | RCT | PMS | 89 | - Combined Ca and vit E (1,000 mg of Ca and 400 units of vit E) | Placebo | - A questionnaire similar to premenstrual profile 2005 | - Decreased mean PMS symptoms from 20 to 9 in intervention group and from 20 to 14.3 in placebo group |
| Khajehei et al. [30] | Iran | RCT | PMS | 180 | - Tablet containing 5 mg of dydrogesterone | Placebo | - American Psychiatric Association standard diagnostic criteria for PMS | - Decreased mean PMS symptoms from 50.6 to 46 in vit D+Ca group, from 52.1 to 47.9 in dydrogesterone group, and from 53.7 to 50.3 in placebo group |
| - 500 mg of Ca+200 mg of vit D | ||||||||
| Mandana and Azar [31] | Iran | RCT | PMS | 155 | - 1 g of Ca during 7 final days of the cycle for 3 cycles | Placebo | - Rosignol Bonlender questionnaire | - Declined mean of social and physical symptoms in Ca group from 19.4±3.4 to 17.3±2.3, in vit E group from 19.4±19 to 16.2±3.4, in Omega-3 group from 19.1±2.3 to 17.1±3.4, in vit B6 group from 19.4±2.6 to 16.7±2.1, and in placebo group from 19.8±2.5 to 18.5±2.4 |
| - 100 mg of vit E daily for 3 cycles | ||||||||
| - 1 g of capsule of fish oil for 3 months | ||||||||
| - 40 mg of vit B6 daily for 3 months | ||||||||
| Samieipour et al. [32] | Iran | RCT | PMS | 210 | - Vit B1 (100 mg) | Placebo | - DMS-IV questionnaire | - Mean pain level in intervention group was 2.6±1.5 during the trial and 7.9±1 in the control. |
| - Ca carbonate (500 mg) | - Ca was more effective on general PMS symptoms than other treatments (P>0.05) | |||||||
| Samieipour et al. [33] | Iran | RCT | PMS | 264 | - Vit B1 (100 mg) daily, 4 days after menstruation for the 2 cycles | Placebo | - DSM-IV questionnaire | - Diminished mean of symptoms in B1 group from 61.2±30.5 to 45.9±13.3, in Ca group from 61.2±31.4 to 29.9±11.1, in Ca + B1 group from 62±30.5 to 25.3±16.8, and in placebo group from 61.5±30.5 to 53.9±18.3 |
| - Ca (500 mg) daily, 4 days after menstruation for the 2 cycles | ||||||||
| - Vit B1 plus Ca, daily, 4 days after menstruation for the 2 cycles | ||||||||
| Shehata [34] | Egypt | RCT | PMS | 210 | - COC pills (drospirenone 3 mg+ethinyl estradiol 0.03 mg) daily for 21 days starting from the third day of menstruation+oral placebo similar to Ca and vit D (daily) | Placebo similar to Ca and vit D+oral placebo similar to COC | - DRSP scores | - Dropped mean scores in Ca+vit D group from 56.9±14.7 to 25.1±9.1, in COC group from 60.6±15.6 to 18.7±6.4, and in placebo group from 61.5±15.7 to 35.2±13.2 |
| - Ca 400 mg+vit D 400 IU once daily+oral placebo similar to COC | ||||||||
| Shobeiri et al. [35] | Iran | RCT | PMS | 66 | - 500 mg of Ca daily for 2 cycles | Placebo | - DMS-IV | - Dropped mean scores in Ca group from 10.5±2.7 to 5.5±2.9, and in placebo group from 8.4±1.7 to 8.2±1.8 (after 2 cycles of intervention) |
| Shobeiri et al. [36] | Iran | RCT | PMS | 64 | - 500 mg of Ca daily for 2 cycles | Placebo | - DSM-IV questionnaire (headache, low back pain, depression, excitability, general pain, and abdominal pain) | - Reductions in the overall severity of physical PMS symptoms in intervention group from 155.9±22.9 to 136.4±19.3 during the first cycle and to 128.9±17.4 in the second cycle |
| Sutariya et al. [37] | India | RCT | PMS | 355 | - Ca carbonate or gluconate 500 mg 1 b.d. for 3 cycles | Health, nutrition, hygiene education | - 17 daily individual symptoms ratings (PMS diary) | - Lowered mean pain scores from 0.8±0.7 to 0.3±0.4 in intervention group, and from 0.6±0.6 to 0.4±0.5 in the control group at the end of the third cycle |
| Tartagni et al. [38] | Italy | RCT | PMS low serum [25(OH)D3] levels (≤10 ng/mL) | 158 | - Vit D supplementation (100,000 IU vit D3 vials) | Placebo | - Serum [25(OH)D3] | - Reduced anxiety score from 50 to 21 |
| - Parathyroid hormone | - Reduced excitability score from 130 to 70 | |||||||
| - Ca | - Reduced crying and anxiety points from 41 and 51 to 30 and 31, respectively | |||||||
| - Standard diagnostic criteria for PMS from ACOG | - Reduced disturbed relationships from 150 to 70 | |||||||
| Yonkers et al. [39] | New Haven, USA | RCT | PMS | 39 | - Fluoxetine (10 mg twice daily) | Placebo | - DSM-IV questionnaire | - 80% improvement in fluoxetine group |
| - Ca carbonate (600 mg twice daily) | - 42% improvement in Ca group | |||||||
| - 42% improvement in placebo group | ||||||||
| Akhlaghi et al. [40] | Iran | Clinical trial | PMS | 100 | - 1,000 mg of effervescent Ca per day in 5 days | Without control group | Utah PMS Calendar II questionnaire | - Decreased PMS psychological symptoms (62%) |
| - Reduced PMS physical symptoms (61%) | ||||||||
| Bharati [41] | India | Quasi-experimental | PMS | 58 | - Yoga group 45 minutes daily, 5 days a week, for 3 months (n=20) | Control group (n=18) | - ACOG diagnostic criteria | - Reductions in mean numbers of PMS symptoms from 5.8 to 3.9 in yoga group, from 5.3 to 4.3 in Ca group, and from 6 to 5.8 in the control group |
| - Ca group, oral tablets of Ca carbonate daily (500 mg, for 3 months) (n=20) | ||||||||
| Bertone-Johnson et al. [42] | Massachusetts, USA | Cross-sectional | PMS | 90 | - | PMS symptom severity of “none” or “mild” | - Serum [25(OH)D3] | - An inverse relationship between severity of PMS symptoms and intake of vit D (OR: 0.3) |
| - Questionnaire similar to those used by Mortola et al. [43] | ||||||||
| Obeidat et al. [44] | Jordan | Cross-sectional | - PMS | 177 | - | Without any intervention | - Plasma [25(OH)D3] level | - In cases of PMS, 91.8% presented hyperparathyroidism with 91.9% showing low levels, and 91% had insufficient amounts of vit D |
| - Primary dysmenorrhea | - Intact parathyroid hormone level | - In cases of PMS, 92.1% of patients consumed dairy products less than 2 meals | ||||||
| - Dairy products intake | ||||||||
| - Primary dysmenorrhea | ||||||||
| - 12 symptoms during the premenstrual phase | ||||||||
| Bahrami et al. [21] | Iran | Cross-sectional | - PMS | 897 | - | Without any intervention | - Serum [25(OH)D3] | - In cases of PMS, 359±46.9 of cases had vit D deficiency and 115±47.3 of subjects had Ca deficiency |
| - Dysmenorrhea | - Serum Ca | |||||||
| - Serum albumin | ||||||||
| - 16 items during the premenstrual phase | ||||||||
| - Self-administered questionnaire | ||||||||
| Pambudi [19] | Indonesia | Cross-sectional | PMS | 45 (case=33, control=12) | - | Women without PMS | - Ca serum levels | - The case group (90.9%) and the control group (25%) contained Ca levels ≤9.4 mg/dL |
| - Daily symptom checklist | - Cut-off point level of Ca for PMS incidence was 9.40 mg/dL | |||||||
| - The case group (9.1%) and the control group (75%) displayed Ca levels >9.4 mg/dL | ||||||||
| Abbasi et al. [45] | India | Case-control | PMS | 85 (case=43, control=42) | - | Healthy women | - Serum Mg | - Mean serum level of vit D was 14.2±2.3 ng/dL in the case group, and 26.2±4 ng/dL in the control group |
| - Serum [25(OH)D3] | - Serum magnesium levels averaged 1.7±0.3 and 1.8±0.1 mg/dL in the case and control groups, respectively | |||||||
| Bertone-Johnson et al. [22] | USA | Case-control | PMS | 3,025 (case=1,057, control=1,968) | - | No diagnosis of PMS and no or minimal menstrual symptoms | - Intake of Ca and vit D | - Total Ca intake values were 12.9±1,027 and 1,057±9.4 mg/dL in the case and control groups, respectively |
| - NHS2 questionnaire | - The overall vit D intake values were 390±7.6 and 401±5.6 IU/dL in the case and control groups, respectively (no significant difference, P>0.5) | |||||||
| Ghalwa et al. [46] | Palestine | Case-control | PMS | 120 (case=60, control=60) | - | Without any suspicion of PMS | - Serum Mg | - Moderate and severe PMS recorded in 26.2% and 2.4%, respectively, in cases of low serum Ca levels |
| - Serum Ca | - Moderate and severe PMS observed in 9.6% and 1.9%, respectively, in cases of low serum Mg levels | |||||||
| - Semi-quantitative food frequency questionnaire | ||||||||
| Rajaei et al. [20] | Iran | Case-control | PMS | 73 (case=41, control=32) | - | Women without PMS | - Serum levels of [25(OH)D3] | - Serum levels of [25(OH)D3] averaged 13.7±2.2 and 12.6±2.2 in the case and control groups, respectively, (no significant difference, P>0.5) |
| - PSST | ||||||||
| Saeedian Kia et al. [47] | Iran | Case-control | PMS | 62 (case=31, control=31) | - | Women without PMS | - Serum Ca level | - Serum levels of [25(OH)D3] averaged 6.8±4 and 6.6±3.7 in the case and control groups, respectively |
| - Serum Mg level | - Mean Ca levels were 9.4±0.4 and 9.5±0.3 in the case and control groups, respectively | |||||||
| - Serum [25(OH)D3] level | - Mean Mg levels were 1.8±0.2 and 1.9±0.2 in the case and control groups, respectively | |||||||
| - Utah PMS Calendar II | ||||||||
| Sharma and Tandon [16] | India | Case-control | PMS | 50 (case=25, control=25) | - | Women without PMS | - Serum Ca level | - Luteal phase reductions of serum Ca levels in PMS patients compared to control group (Chi-square: 4.9) |
| - Serum Mg level | ||||||||
| - Self designed questionnaire | ||||||||
| Bertone-Johnson et al. [48] | USA | Case-control | PMS | 802 (case=401, control=401) | - | No PMS | - Serum [25(OH)D3] | - Mean serum levels of [25(OH)D3] were 66.5±20.5 and 64.8±19.9 nmol/L in the case and control groups, respectively |
| - Total Ca | - Mean Ca levels (mg/dL) were 9.7±0.3 and 9.7±0.3 in the case and control groups, respectively | |||||||
| - Intact parathyroid hormone | - Parathyroid hormone levels (pg/mL) averaged 31.2±11.2 and 31.6±11.6 in the case and control groups, respectively (no significant difference, P>0.05) | |||||||
| - NHS2 questionnaire |
PMS, premenstrual syndrome; COC, combined oral contraceptive; ACOG, The American College of Obstetricians and Gynecologists; Ca, calcium; Mg, magnesium; vit, vitamin; [25(OH)D3], 25-hydroxyvitamin D3; RCT, randomized controlled trial; PSST, premenstrual syndrome screening test; CBT, cognitive behavioral therapy; DMS-IV, Diagnostic and Statistical Manual of Mental Disorders, 4th edition; b.d., twice a day; DRSP, daily record of severity of problems; OR, odds ratio; NHS2, Nurses' Health Study II.
Table 3. Adherence of the selected studies to the Strengthening the Reporting of Observational Studies in Epidemiology checklist.
| Characteristic | Study reference | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bahrami et al. [21] | Dadkhah et al. [26] | Ghanbari et al. [27] | Karimi et al. [28] | Kermani et al. [29] | Khajehei et al. [30] | Mandana and Azar [31] | Samieipour et al. [32] | Samieipour et al. [33] | Shehata [34] | Shobeiri et al. [36] | Shobeiri et al. [35] | Sutariya et al. [37] | Tartagni et al. [38] | Yonkers et al. [39] | Akhlaghi et al. [40] | Bharati [41] | Bertone-Johnson et al. [48] | Obeidat et al. [44] | Bahrami et al. [25] | Pambudi [19] | Abbasi et al. [45] | Bertone-Johnson et al. [22] | Ghalwa et al. [46] | Rajaei et al. [20] | Saeedian Kia et al. [47] | Sharma and Tandon [16] | Bertone-Johnson et al. [42] | ||
| Title & abstract | A | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| B | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Introduction | Background | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Objectives | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | + | + | + | + | + | + | + | + | + | + | − | + | |
| Methods | Study design | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Setting | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | + | + | + | + | |
| Participants | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Variables | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Measurements | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Bias | - | + | + | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | − | − | − | + | − | + | − | + | + | |
| Study size | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | + | + | + | + | |
| Quantitative variables | + | + | + | + | + | − | − | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Statistical methods | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | + | + | + | + | − | + | + | − | + | + | + | + | |
| Results | Participants | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Descriptive data | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Outcome data | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Main results | + | + | − | + | − | + | − | + | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | + | − | − | + | |
| Key results | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | − | + | + | + | + | |
| Discussion | Limitations | + | + | − | + | − | − | − | + | + | + | + | + | − | + | + | + | + | − | + | + | − | − | + | − | + | + | − | + |
| Interpretation | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Generalizability | + | + | + | + | + | + | + | + | + | − | + | + | − | + | + | + | + | + | + | + | − | + | + | + | + | − | − | + | |
The results indicated that low serum levels of vitamin D and calcium during the luteal phase of the menstrual cycle could contribute to the incidence and exacerbation of PMS symptoms. Moreover, the mean severity and number of PMS symptoms decreased after calcium and vitamin D supplementation.
Discussion
This systematic review analyzed the results of high-quality studies regarding the role of calcium and vitamin D in PMS while considering the effects of PMS on the physical and psychological aspects of women's health. The results indicate that low levels of vitamin D and calcium during the luteal phase of menstrual cycle can cause and/or intensify the symptoms of PMS. Calcium and vitamin D supplementation can increase serum levels of these 2 micronutrients and may eliminate or reduce the severity of PMS symptoms. Less severe PMS symptoms were also observed in women using diets rich in vitamin D and calcium.
The positive relationship reported between [25(OH)D3] and PMS symptoms is in contrast to Bertone's hypothesis [49]. Their study showed that [25(OH)D3] levels increased in cases of PMS, due to differences in supplementation methods, and that such results arise from errors in the findings [48]. Although the exact cause of this finding is unclear, the possible use of supplements or multivitamins containing calcium and vitamin D by women with PMS can be one explanation [49].
This finding is consistent with those of Thys-Jacobs et al. [50] who reported insignificantly higher use of calcium supplements (46% vs. 32%) and vitamin D supplements (41% vs. 30%) among women with premenstrual dysphoric disorder (PMDD) than among symptom-free controls. The different doses of calcium supplementation during the intervention support the hypothesis that women experiencing PMS may be self-medicating with dietary supplements. Similarly, the associations of vitamin D with specific symptoms may vary. Bertone-Johnson et al. [48] studied women not yet diagnosed with PMS at the time of blood collection and found [25(OH)D3] levels to be associated with a significantly lower risk of developing breast tenderness, diarrhea/constipation, fatigue, and depression (P<0.05) and a possible lower risk of swelling of the extremities and bloating (P≤0.11).
In addition, the inverse relationship between [25(OH)D3] levels and PMS confirms previous findings that indicated the possible role of vitamin D in decreasing the risk of unipolar depression [51]. Low serum levels of Mg++ and [25(OH)D3] during the luteal phase have also been observed in women suffering from PMS [45]. The findings of the mentioned study are inconsistent with previous research [52,53,54], and this inconsistency can be justified by differences in the study populations, geographic regions, sample sizes, and sample size estimation methods [45].
Another case-control study analyzed serum Mg++ and [25(OH)D3] levels after supplementation in a cohort of 1,057 females and reported less severe PMS symptoms in the case group than in the controls [46]. Serum Mg++ and [25(OH)D3] levels are low during the luteal phase of menstrual cycle due to cyclical changes in the release of hormones from the hypothalamic-pituitary-ovarian axis [45]. Calcium supplementation reduced the severity of the mentioned symptoms and changed the frequencies of severe, moderate, and mild symptoms to 7%, 33%, and 47%, respectively [40].
A high dose of vitamin D3 (50,000 IU/weekly) is recommended for the prevention and treatment of vitamin D deficiency [55]. Bahrami et al. [25] administered high-dose vitamin D pearls (50,000 IU cholecalciferol/weekly) during a period of 9 weeks and observed a significant relationship between vitamin D therapy and improvement of PMS symptoms and dysmenorrhea among adolescents.
In a placebo-controlled study of the effects of calcium (500 mg) plus vitamin D (200 mg) supplementation on PMS, Khajehei et al. [30] showed that supplementation decreased the severity of PMS symptoms. They compared the mean severity of symptoms between groups before and after the intervention and found that dydrogesterone and calcium plus vitamin D had the same effects on decreasing symptom severity (P<0.05). The improvement in symptom ratings was less in this study than in others, but the differences between the scores before and after the intervention were statistically significant.
Bertone-Johnson [56] claimed that low dietary vitamin D was related to the development of PMS. Additionally, high dietary vitamin D intake was suggested to reduce the risk of PMS by affecting calcium levels and oscillation of the cyclic sex steroid hormone, and/or neurotransmitter function [57,58].
Bahrami et al. [21] reported that calcium levels had a significant relationship with the incidence of irritability. Saeedian Kia et al. [47] compared dietary intake and serum levels of calcium, Mg, and vitamin D in students with PMS to those of healthy controls. No significant differences were found between the 2 groups in terms of serum vitamin D levels. The serum concentrations of Ca and Mg were lower in some cases, but the levels were within the normal range in all cases.
Bendich [59] showed lower levels of calcium in participants without PMS and concluded that an increase in dietary calcium intake could help maintain normal calcium levels and prevent the manifestation of PMS symptoms. There was a high prevalence of vitamin D deficiency in their population sample of healthy girls. However, the prevalence of PMS symptoms did not differ significantly in relationship to the vitamin D status. Another study in Iran indicated no significant difference in the vitamin D serum status between the PMS and control groups [21,47]. In a study on dysmenorrheic college students, Obeidat et al. [44] reported that PMS had no relationship with the levels of parathyroid hormone and vitamin D, or intake of dairy products.
Bertone-Johnson et al. [22] performed a nested case-control study and suggested that a high dietary intake of vitamin D and calcium could lower the risk of PMS symptoms. They also observed a significantly lower risk of developing PMS in women with a high intake of vitamin D and calcium from food sources, equivalent to about 4 servings per day of skim or low-fat milk, fortified orange juice, or low-fat dairy foods such as yogurt.
In a clinical trial, Bharati [41] compared yoga exercises and calcium supplements, and observed a considerable reduction in the number of PMS symptoms in the yoga group. Calcium and vitamin D might affect the occurrence of PMS through their associations with endogenous estrogens.
Dadkhah et al. [26] investigated the impacts of vitamins D and E on PMS. Two months after the intervention, they detected a significant improvement in the PMS symptom scores and reported vitamin E to be slightly more effective in reducing PMS symptoms than both vitamin D and the placebo. However, there were no significant differences between the 3 groups. Kermani et al. [29] assessed the effects of calcium, vitamin E, and a placebo and reported that, after 3 months of intervention with 1,000 mg of calcium plus 400 IU of vitamin E, the severity of symptoms was significantly lower in the intervention group than in the placebo group. In a study by Ghalwa et al. [46], PMS was strongly related with calcium and magnesium. Dietary changes and natural treatments were also linked with the pain and discomfort of women with PMS. PMS also had significant relationships with lifestyle, smoking status, physical activity, and sleep. The effects of dietary behaviors with different types of foods on PMS were also considerable.
Ghanbari et al. [27] performed pre- and post-tests and concluded that depression and anxiety significantly decreased in women treated with calcium compared to the placebo group (27% vs. 7%; P<0.002). Similar results were reported by Bertone-Johnson et al. [22]. Bohrer and Krannich [60] found that calcium supplements effectively improved depressive symptoms.
Karimi et al. [28] investigated the effects of cognitive behavioral therapy (CBT) and calcium plus vitamin D supplementation on the reduction of PMS symptoms. In a trial, Mandana and Azar [31] showed that vitamin E, vitamin B6, calcium, and omega-3 had significant effects on enhancing the physical and mental symptoms of women with PMS. Rajaei et al. [20] observed no relationship between the level of 25OHD during the luteal phase and the presence of PMS. The high prevalence of vitamin D deficiency among the case and control groups might justify this finding. In fact, their study was conducted among young women in Tehran [20], and several studies have indicated a high prevalence of vitamin D deficiency in different parts of Iran [61,62,63]. Samieipour et al. [32] highlighted significant reductions in the mean total severity of PMS symptoms following both calcium and vitamin B1 supplementation compared to the placebo group (P<0.001). This reduction was more profound in the calcium group. In a randomized and quadruple-blind study, the same authors found calcium plus vitamin B1 supplementation to be more effective on the severity of PMS symptoms than other supplements [33].
In a double-blind randomized placebo-controlled trial, Shehata [34] indicated that combined oral contraceptive (COC) pills were superior to calcium in reducing the scores of PMS symptoms. However, the difference was only significant in women who had moderate PMS in the 2 months before treatment, and this can be explained by the mechanisms of action of COC and calcium. If calcium affects PMS through its relationship with endogenous estrogen, it will never be as effective as COCs, which prevent endogenous estrogen more effectively. Another mechanism of COC action is related to neurotransmission.
In a double-blind randomized clinical trial, Shobeiri et al. [35] documented the significant effects of low-dose calcium (500 mg) on the reduction of PMS symptoms. A review study in 2015 evaluated numerous non-pharmacological treatments but only found calcium supplements effective [7]. In a double-blind clinical trial, the same authors observed that calcium intake had significant effects on all physical symptoms (cramps, headache, depression, irritability, general pain, and abdominal pain) of PMS in the first and second months after the intervention [36].
In a prospective, randomized controlled interventional study, Sutariya et al. [37] showed that calcium supplementation effectively mitigated the symptoms of PMS during the luteal phase. The calcium treatment resulted in an approximate 50% reduction in total mean symptom scores with significant beneficial effects on symptoms including depression, mood swings, headache, irritability, and breast tenderness. Calcium was not effective during the menstrual or intermenstrual phase of the cycle. Tartagni et al. [38] reported that calcium intake, both alone and in combination with vitamin D, was able to reduce the intensity of PMS. In a pilot parallel clinical trial study, Yonkers et al. [39] compared fluoxetine, calcium, and a placebo as a treatment for moderate to severe PMS and PMDD over the course of 4 menstrual cycles. Their findings suggested small benefits of calcium. However, the estimated effect for fluoxetine was much higher than that of calcium. The placebo response in this study (17–33% depending on the measure) was in line with the range of placebo response rates (11.8–50%) reported in similar studies [64]. In a cross-sectional study, Bertone-Johnson et al. [42] showed that vitamin D consumption was inversely associated with the prevalence of PMS, and perhaps with menstrual symptom severity in general. In contrast, late luteal phase serum [25(OH)D3] levels were not associated with either outcome.
The review of the selected studies indicates that vitamin D and calcium supplementation, or the use of a diet rich in these two micronutrients, could improve serum levels during the luteal phase, and thus eliminate or improve PMS symptoms.
There has been no unanimously accepted therapeutic method to improve PMS symptoms to date. Vitamin D and calcium, when compared to the treatments mentioned in the studies, such as yoga, CBT, medications like Fluoxetine, COC, etc., can be a safe, effective, acceptable, low cost, and convenient method for reducing the intensity and frequency of PMS symptoms, and thus improving women's quality of life.
One of the limitations of this study was the role of confounding factors, such as age, educational and economic status, geographical area, and mental and physical status of the participants, which were considered in most of the reviewed studies. Since PMS symptoms are recalled by the participants, recall bias was another limitation. Other limitations that were found in some of the studies were lack of control groups, short-term treatments, and low sample size. Moreover, differences in the participants' diets might have affected serum levels of vitamin D and calcium in the studies that did not evaluate and control the women's diet.
Acknowledgements
This study is related to the project NO 1396/66168 From Student Research Committee, Shahid Beheshti University of Medical Sciences, Tehran, Iran. We also appreciate the “Student Research Committee” and “Research & Technology Chancellor” in Shahid Beheshti University of Medical Sciences for their financial support of this study.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Abdnezhad R, Simbar M, Sheikhan Z, Mojab F, Nasiri M. The effect of Salvia (Sage) extract on the emotional symptoms of premenstrual syndrome. Iran J Obstet Gynecol Infertil. 2017;20:84–94. [Google Scholar]
- 2.Brahmbhatt S, Sattigeri BM, Shah H, Kumar A, Parikh D. A prospective survey study on premenstrual syndrome in young and middle aged women with an emphasis on its management. Int J Res Med Sci. 2013;1:69–72. [Google Scholar]
- 3.Raval CM, Panchal BN, Tiwari DS, Vala AU, Bhatt RB. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among college students of Bhavnagar, Gujarat. Indian J Psychiatry. 2016;58:164–170. doi: 10.4103/0019-5545.183796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halbreich U, O'Brien PM, Eriksson E, Bäckström T, Yonkers KA, Freeman EW. Are there differential symptom profiles that improve in response to different pharmacological treatments of premenstrual syndrome/premenstrual dysphoric disorder? CNS Drugs. 2006;20:523–547. doi: 10.2165/00023210-200620070-00001. [DOI] [PubMed] [Google Scholar]
- 5.Kahyaoglu Sut H, Mestogullari E. Effect of premenstrual syndrome on work-related quality of life in Turkish nurses. Saf Health Work. 2016;7:78–82. doi: 10.1016/j.shaw.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sepehrirad M, Bahrami H, Noras M. The role of complementary medicine in control of premenstrual syndrome evidence based (Regular Review Study) Iran J Obstet Gynecol Infertil. 2016;19:11–22. [Google Scholar]
- 7.Freeman EW. Therapeutic management of premenstrual syndrome. Expert Opin Pharmacother. 2010;11:2879–2889. doi: 10.1517/14656566.2010.509344. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. National policy on traditional medicine and regulation of herbal medicines: report of a WHO global survey. Geneva: World Health Organization; 2005. [Google Scholar]
- 9.Babazadeh R, Keramat A. Premenstrual syndrome and complementary medicine in Iran: a systematic review. Feyz J Kashan Univ Med Sci. 2011;15:174–187. [Google Scholar]
- 10.Mun MJ, Kim TH, Hwang JY, Jang WC. Vitamin D receptor gene polymorphisms and the risk for female reproductive cancers: a meta-analysis. Maturitas. 2015;81:256–265. doi: 10.1016/j.maturitas.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Kim TH, Lee HH, Kim JM, Lee A, Park J, Kim Y. A comparison in vitamin D receptor expression during oral menopausal hormone therapy and vaginal estrogen therapy. Clin Exp Obstet Gynecol. 2018;45:39–43. [Google Scholar]
- 12.Cioni F, Ferraroni F. Vitamin D and other nutrients in the treatment of premenstrual syndrome. In: Hollins-Martin C, van den Akker O, Martin C, Preedy VR, editors. Handbook of diet and nutrition in the menstrual cycle, periconception and fertility. Wageningen: Wageningen Academic Publishers; 2014. pp. 121–136. [Google Scholar]
- 13.Lee A, Lee MR, Lee HH, Kim YS, Kim JM, Enkhbold T, et al. Vitamin D proliferates vaginal epithelium through RhoA expression in postmenopausal atrophic vagina tissue. Mol Cells. 2017;40:677–684. doi: 10.14348/molcells.2017.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taghizadeh Z, Shirmohammadi M, Feizi A, Arbabi M. The effect of cognitive behavioural psycho-education on premenstrual syndrome and related symptoms. J Psychiatr Ment Health Nurs. 2013;20:705–713. doi: 10.1111/j.1365-2850.2012.01965.x. [DOI] [PubMed] [Google Scholar]
- 15.Sen AP, Gulati A. Use of magnesium in traumatic brain injury. Neurotherapeutics. 2010;7:91–99. doi: 10.1016/j.nurt.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma G, Tandon P. Luteal phase serum calcium and serum magnesium levels in causation of premenstrual syndrome. Int J Basic Appl Physiol. 2015;4:126–130. [Google Scholar]
- 17.Vaidya A, Forman JP. Vitamin D and vascular disease: the current and future status of vitamin D therapy in hypertension and kidney disease. Curr Hypertens Rep. 2012;14:111–119. doi: 10.1007/s11906-012-0248-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forman JP, Williams JS, Fisher ND. Plasma 25-hydroxyvitamin D and regulation of the renin-angiotensin system in humans. Hypertension. 2010;55:1283–1288. doi: 10.1161/HYPERTENSIONAHA.109.148619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pambudi MF. Calcium level is lower in women with premenstrual syndrome. Majalah Obstet Ginekol Indones. 2013;37:99–102. [Google Scholar]
- 20.Rajaei S, Akbari Sene A, Norouzi S, Berangi Y, Arabian S, Lak P, et al. The relationship between serum vitamin D level and premenstrual syndrome in Iranian women. Int J Reprod Biomed (Yazd) 2016;14:665–668. [PMC free article] [PubMed] [Google Scholar]
- 21.Bahrami A, Bahrami-Taghanaki H, Afkhamizadeh M, Avan A, Mazloum Khorasani Z, Esmaeili H, et al. Menstrual disorders and premenstrual symptoms in adolescents: prevalence and relationship to serum calcium and vitamin D concentrations. J Obstet Gynaecol. 2018;38:989–995. doi: 10.1080/01443615.2018.1434764. [DOI] [PubMed] [Google Scholar]
- 22.Bertone-Johnson ER, Hankinson SE, Bendich A, Johnson SR, Willett WC, Manson JE. Calcium and vitamin D intake and risk of incident premenstrual syndrome. Arch Intern Med. 2005;165:1246–1252. doi: 10.1001/archinte.165.11.1246. [DOI] [PubMed] [Google Scholar]
- 23.Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. 2014;14:45. doi: 10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roozbeh N, Banihashemi F, Mehraban M, Abdi F. Potential role of Factor V Leiden mutation in adverse pregnancy outcomes: an updated systematic review. Biomed Res Ther. 2017;4:1832–1846. [Google Scholar]
- 25.Bahrami A, Avan A, Sadeghnia HR, Esmaeili H, Tayefi M, Ghasemi F, et al. High dose vitamin D supplementation can improve menstrual problems, dysmenorrhea, and premenstrual syndrome in adolescents. Gynecol Endocrinol. 2018;34:659–663. doi: 10.1080/09513590.2017.1423466. [DOI] [PubMed] [Google Scholar]
- 26.Dadkhah H, Ebrahimi E, Fathizadeh N. Evaluating the effects of vitamin D and vitamin E supplement on premenstrual syndrome: a randomized, double-blind, controlled trial. Iran J Nurs Midwifery Res. 2016;21:159–164. doi: 10.4103/1735-9066.178237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghanbari Z, Haghollahi F, Shariat M, Foroshani AR, Ashrafi M. Effects of calcium supplement therapy in women with premenstrual syndrome. Taiwan J Obstet Gynecol. 2009;48:124–129. doi: 10.1016/S1028-4559(09)60271-0. [DOI] [PubMed] [Google Scholar]
- 28.Karimi Z, Dehkordi MA, Alipour A, Mohtashami T. Treatment of premenstrual syndrome: appraising the effectiveness of cognitive behavioral therapy in addition to calcium supplement plus vitamin D. PsyCh J. 2018;7:41–50. doi: 10.1002/pchj.206. [DOI] [PubMed] [Google Scholar]
- 29.Kermani AZ, Taavoni S, Hosseini AF. Effect of combined calcium and vitamin E consumption on premenstrual syndrome. Iran J Nurs. 2010;23:8–14. [Google Scholar]
- 30.Khajehei M, Abdali K, Parsanezhad ME, Tabatabaee HR. Effect of treatment with dydrogesterone or calcium plus vitamin D on the severity of premenstrual syndrome. Int J Gynaecol Obstet. 2009;105:158–161. doi: 10.1016/j.ijgo.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 31.Mandana Z, Azar A. Comparison of the effect of vit E, vitB6, calcium and omega-3 on the treatment of premenstrual syndrome: a clinical randomized trial. Annu Res Rev Biol. 2014;4:1141–1149. [Google Scholar]
- 32.Samieipour S, Kiani F, Samiei Pour Y, Babaei Heydarabadi A, Tavassoli E, Rahim Zade R. Comparing the effects of vitamin B1 and calcium on premenstrual syndrome (PMS) among female students, Ilam-Iran. Int J Pediatr. 2016;4:3519–3528. [Google Scholar]
- 33.Samieipour S, Tavassoli E, Heydarabadi B, Daniali SS, Alidosti M, Kiani F, et al. Effect of calcium and vitamin B1 on the severity of premenstrual syndrome: a randomized control trial. Int J Pharm Technol. 2016;8:18706–18717. [Google Scholar]
- 34.Shehata NA. Calcium versus oral contraceptive pills containing drospirenone for the treatment of mild to moderate premenstrual syndrome: a double blind randomized placebo controlled trial. Eur J Obstet Gynecol Reprod Biol. 2016;198:100–104. doi: 10.1016/j.ejogrb.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 35.Shobeiri F, Araste FE, Ebrahimi R, Jenabi E, Nazari M. Effect of calcium on premenstrual syndrome: a double-blind randomized clinical trial. Obstet Gynecol Sci. 2017;60:100–105. doi: 10.5468/ogs.2017.60.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shobeiri F, Ezzati Arasteh F, Ebrahimi R, Nazari M. Effect of calcium on physical symptoms of premenstrual syndrome. Iran J Obstet Gynecol Infertil. 2016;19:1–8. [Google Scholar]
- 37.Sutariya S, Talsania N, Shah C, Patel M. An interventional study (calcium supplementation & health education) on premenstrual syndrome - effect on premenstrual and menstrual symptoms. Natl J Community Med. 2011;2:100–104. [Google Scholar]
- 38.Tartagni M, Cicinelli MV, Tartagni MV, Alrasheed H, Matteo M, Baldini D, et al. Vitamin D supplementation for premenstrual syndrome-related mood disorders in adolescents with severe hypovitaminosis D. J Pediatr Adolesc Gynecol. 2016;29:357–361. doi: 10.1016/j.jpag.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 39.Yonkers KA, Pearlstein TB, Gotman N. A pilot study to compare fluoxetine, calcium, and placebo in the treatment of premenstrual syndrome. J Clin Psychopharmacol. 2013;33:614–620. doi: 10.1097/JCP.0b013e31829c7697. [DOI] [PubMed] [Google Scholar]
- 40.Akhlaghi F, Hamedi A, Javadi Z, Hosseinipoor F. Effects of calcium supplementation on premenstrual syndrome. Razi J Med Sci. 2004;10:669–675. [Google Scholar]
- 41.Bharati M. Comparing the effects of yoga & oral calcium administration in alleviating symptoms of premenstrual syndrome in medical undergraduates. J Caring Sci. 2016;5:179–185. doi: 10.15171/jcs.2016.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bertone-Johnson ER, Chocano-Bedoya PO, Zagarins SE, Micka AE, Ronnenberg AG. Dietary vitamin D intake, 25-hydroxyvitamin D3 levels and premenstrual syndrome in a college-aged population. J Steroid Biochem Mol Biol. 2010;121:434–437. doi: 10.1016/j.jsbmb.2010.03.076. [DOI] [PubMed] [Google Scholar]
- 43.Mortola JF, Girton L, Beck L, Yen SS. Diagnosis of premenstrual syndrome by a simple, prospective, and reliable instrument: the calendar of premenstrual experiences. Obstet Gynecol. 1990;76:302–307. [PubMed] [Google Scholar]
- 44.Obeidat BA, Alchalabi HA, Abdul-Razzak KK, Al-Farras MI. Premenstrual symptoms in dysmenorrheic college students: prevalence and relation to vitamin D and parathyroid hormone levels. Int J Environ Res Public Health. 2012;9:4210–4222. doi: 10.3390/ijerph9114210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abbasi ST, Abbasi P, Suhag AH, Qureshi MA. Serum magnesium and 25-hydroxy cholecalciferol in premenstrual syndrome during luteal phase. J Liaquat Uni Med Health Sci. 2017;16:209–212. [Google Scholar]
- 46.Ghalwa NA, Qedra R, Wahedy K. Impact of calcium and magnesium dietary changes on women pain and discomfort from premenstrual syndrome at the Faculty of Pharmacy-Gaza strip. World J Pharm Pharm Sci. 2014;3:981–1005. [Google Scholar]
- 47.Saeedian Kia A, Amani R, Cheraghian B. The association between the risk of premenstrual syndrome and vitamin D, calcium, and magnesium status among university students: a case control study. Health Promot Perspect. 2015;5:225–230. doi: 10.15171/hpp.2015.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bertone-Johnson ER, Hankinson SE, Forger NG, Powers SI, Willett WC, Johnson SR, et al. Plasma 25-hydroxyvitamin D and risk of premenstrual syndrome in a prospective cohort study. BMC Womens Health. 2014;14:56. doi: 10.1186/1472-6874-14-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.American College of Obstetricians and Gynecologists. Frequently asked questions FAQ057: gynecologic problems: premenstrual syndrome. Washington, D.C.: American College of Obstetricians and Gynecologists; 2011. [Google Scholar]
- 50.Thys-Jacobs S, McMahon D, Bilezikian JP. Cyclical changes in calcium metabolism across the menstrual cycle in women with premenstrual dysphoric disorder. J Clin Endocrinol Metab. 2007;92:2952–2959. doi: 10.1210/jc.2006-2726. [DOI] [PubMed] [Google Scholar]
- 51.Eyles DW, Burne TH, McGrath JJ. Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrinol. 2013;34:47–64. doi: 10.1016/j.yfrne.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 52.Skowrońska P, Pastuszek E, Kuczyński W, Jaszczoł M, Kuć P, Jakiel G, et al. The role of vitamin D in reproductive dysfunction in women - a systematic review. Ann Agric Environ Med. 2016;23:671–676. doi: 10.5604/12321966.1226865. [DOI] [PubMed] [Google Scholar]
- 53.Miyashita M, Koga K, Izumi G, Sue F, Makabe T, Taguchi A, et al. Effects of 1, 25-dihydroxy vitamin D3 on endometriosis. J Clin Endocrinol Metab. 2016;101:2371–2379. doi: 10.1210/jc.2016-1515. [DOI] [PubMed] [Google Scholar]
- 54.Harris HR, Chavarro JE, Malspeis S, Willett WC, Missmer SA. Dairy-food, calcium, magnesium, and vitamin D intake and endometriosis: a prospective cohort study. Am J Epidemiol. 2013;177:420–430. doi: 10.1093/aje/kws247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Guidelines for preventing and treating vitamin D deficiency and insufficiency revisited. J Clin Endocrinol Metab. 2012;97:1153–1158. doi: 10.1210/jc.2011-2601. [DOI] [PubMed] [Google Scholar]
- 56.Bertone-Johnson ER. Vitamin D and the occurrence of depression: causal association or circumstantial evidence? Nutr Rev. 2009;67:481–492. doi: 10.1111/j.1753-4887.2009.00220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Holick MF. Vitamin D: a D-Lightful health perspective. Nutr Rev. 2008;66:S182–94. doi: 10.1111/j.1753-4887.2008.00104.x. [DOI] [PubMed] [Google Scholar]
- 58.Thys-Jacobs S. Micronutrients and the premenstrual syndrome: the case for calcium. J Am Coll Nutr. 2000;19:220–227. doi: 10.1080/07315724.2000.10718920. [DOI] [PubMed] [Google Scholar]
- 59.Bendich A. The potential for dietary supplements to reduce premenstrual syndrome (PMS) symptoms. J Am Coll Nutr. 2000;19:3–12. doi: 10.1080/07315724.2000.10718907. [DOI] [PubMed] [Google Scholar]
- 60.Bohrer T, Krannich JH. Depression as a manifestation of latent chronic hypoparathyroidism. World J Biol Psychiatry. 2007;8:56–59. doi: 10.1080/15622970600995146. [DOI] [PubMed] [Google Scholar]
- 61.Faghih S, Abdolahzadeh M, Mohammadi M, Hasanzadeh J. Prevalence of vitamin d deficiency and its related factors among university students in Shiraz, Iran. Int J Prev Med. 2014;5:796–799. [PMC free article] [PubMed] [Google Scholar]
- 62.Kaykhaei MA, Hashemi M, Narouie B, Shikhzadeh A, Rashidi H, Moulaei N, et al. High prevalence of vitamin D deficiency in Zahedan, southeast Iran. Ann Nutr Metab. 2011;58:37–41. doi: 10.1159/000323749. [DOI] [PubMed] [Google Scholar]
- 63.Hovsepian S, Amini M, Aminorroaya A, Amini P, Iraj B. Prevalence of vitamin D deficiency among adult population of Isfahan City, Iran. J Health Popul Nutr. 2011;29:149–155. doi: 10.3329/jhpn.v29i2.7857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Halbreich U. Selective serotonin reuptake inhibitors and initial oral contraceptives for the treatment of PMDD: effective but not enough. CNS Spectr. 2008;13:566–572. doi: 10.1017/s1092852900016849. [DOI] [PubMed] [Google Scholar]