Abstract
BACKGROUND
Inflammatory bowel disease (IBD) presents an inflammatory picture that in the long run can lead to complications and consequently more hospitalizations compared to other diseases.
AIM
To evaluate the influence of nutritional status on the occurrence of IBD-related hospitalization.
METHODS
This integrative review was conducted in the online databases PubMed and MEDLINE, using the terms “obesity” and “malnutrition” accompanied by “hospitalization”, each combined with “Crohn’s disease” or “ulcerative colitis”. Only studies conducted with humans, adults, and published in English or Spanish were selected, and those that were not directly associated with nutritional status and hospitalization were excluded from this review. The Preferred Reporting Items for Systematic Reviews and Meta-Analyzes guide was used as the basis for selection of studies.
RESULTS
Of the 80 studies identified, only five met the proposal of this review. None evaluated the association of good nutritional status with the risk of hospitalization. Malnutrition had a strong correlation with the risk of hospitalization related to IBD, and there was disagreement among three studies regarding the association of obesity and hospitalization rates.
CONCLUSION
Few studies have evaluated nutritional status as a predictor of IBD-related hospitalization. The presence of malnutrition appears to be associated with hospitalization in these patients, but further studies are needed to elucidate the issue.
Keywords: Nutritional status, Inflammatory bowel disease, Hospitalization, Obesity, Malnutrition
Core tip: Hospitalization in patients with inflammatory bowel disease (IBD) is common. Identifying involved factors, especially controllable ones, may help the development of strategies that can decrease the number of hospitalizations. Among these potential factors is nutritional status, as it is associated with the clinical evolution of patients with IBD. However, few studies have evaluated the association between nutritional status and hospitalization, the consequent complications of the disease, and surgical procedures. Few studies have described the association of malnutrition with hospitalization in IBD, and we cannot say whether adequate nutritional status alters this risk, and the results with obesity are conflicting. Thus, further studies are needed to answer this question.
INTRODUCTION
Inflammatory bowel disease (IBD) affects different portions of the gastrointestinal tract and can be classified as Crohn’s disease (CD) and ulcerative colitis (UC). IBD is an inflammatory condition, and long term it can lead to complications and consequently a greater number of hospitalizations compared to patients with other diseases. In addition to the greater number of hospitalizations, these patients require longer hospital stays, resulting in significant expenditures for the health system[1,2].
The hospitalizations of patients with IBD are associated with complications of the disease, which involve the absence of specialized outpatient follow-up, surgical procedures, and non-use of medication for treatment. Thus, keeping the disease in the remission phase, in this case, is an important protective factor to prevent the occurrence of complications and consequent hospitalizations[1,3].
It is known that enteral nutritional support for patients with IBD helps to increase body mass index (BMI) as well as improve disease activity, clinical signs, and symptoms, and it also allows adequate food consumption of energy, proteins, fats, carbohydrates, and fibers[2]. However, few studies have evaluated the association between nutritional status and hospitalization of patients with IBD and the consequent complications in the disease and surgical procedures[4-8]. Thus, the objective of this study was to evaluate the influence of nutritional status on the occurrence of hospitalization related to IBD.
MATERIALS AND METHODS
The research was conducted in the PubMed and MEDLINE online databases in May 2018, using the terms “obesity” and “malnutrition” accompanied by “hospitalization”, each combined with “Crohn’s disease” or “ulcerative colitis”. Only articles published in English or Spanish until May 2018, with patients diagnosed with IBD, were included.
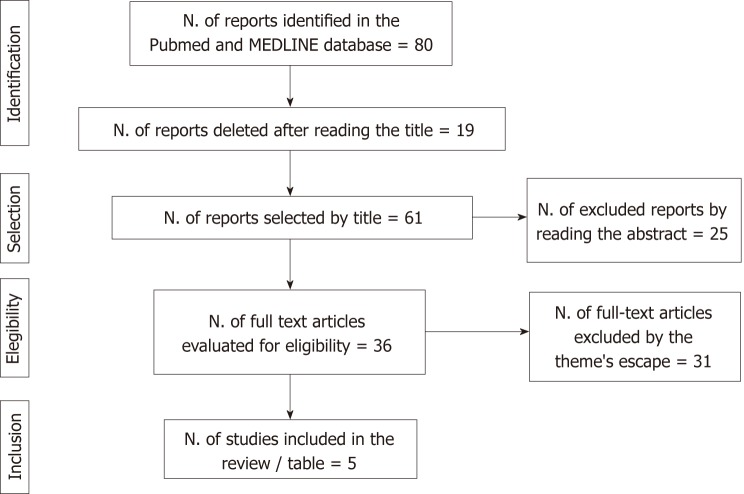
The studies were selected by three independent authors and include information on a large number of individuals and adults, with a diagnosis of CD or UC. Initially, 80 studies were found, and 61 were selected after reading the title. After reading the abstract, 25 were excluded because they were articles of revision, case reports, or abstracts of symposium. For the analysis of the full text, 36 articles were elected, and 29 were excluded because they did not directly associate nutritional status and hospitalization for IBD. The flow chart for the selection of the studies of this review was constructed from the structure of the Preferred Reporting Items for Systematic Reviews and Meta - Analyses (PRISMA)[9] (Figure 1).
Figure 1.
Flowchart adapted from PRISMA.
RESULTS
Of the 36 articles selected, only five evaluated the association between nutritional status and hospitalization for IBD[4-8]. One study included a small number of children, and the information on the sample size was confusing[4]. Four studies had a cohort study design[4-7], three of which were retrospective[4,5,7] and one was a cross-sectional study (Table 1).
Table 1.
Five studies on nutritional status as a predictor of hospitalization in patients with inflammatory bowel disease
| Author | Study design/study population | Main results |
| Blain et al[4], 2002 | Retrospective study, follow-up | 3% (62) were obese |
| 2065 patients of any age with CD: 62 obese vs 124 non-obese, matched by age, sex, disease location and date of diagnosis of CD | Patients with obese CD had a higher chance of hospitalization than non-obese patients (OR = 2.35, 95%CI: 1.56-3.52) | |
| Flores et al[5], 2015 | Retrospective study, follow-up | Obese and overweight patients are less likely to experience hospitalization than the group with low / adequate BMI (42% vs 44% vs 66%, P < 0.001) |
| 518 patients with IBD divided into obese (BMI ≥ 30 kg/m²), overweight (25-29.9 kg/m²), eutrophic (18.5-24.9 kg/m²) and low weight (< 18.5 kg/m²) | ||
| Seminerio et al[6], 2015 | Prospective study | There was no association between increased BMI and hospitalization in patients with IBD, in both those with CD and UC (P = 0.396) |
| 1494 patients with IBD | ||
| Ananthakrishnan et al[7], 2010 | Retrospective study cohort | Severe hospitalizations were more associated with anemia (20.8% vs 15.1%, P < 0.001) and malnutrition (8.7% vs 2.3%, P < 0.001) |
| 6169 patients with CD | ||
| Gajendran et al[8], 2016 | Cross-sectional study (2 yr) | There is an association between malnutrition and hospitalization of patients diagnosed with IBD (OR = 6.29, 95%CI: 5.84–6.78) |
| Patients diagnosed with IBD | ||
| Estimated number of 109392 annual visits with a primary diagnosis of IBD |
CD: Crohn’s disease; UC: Ulcerative colitis; IBD: Inflammatory bowel disease; BMI: Body mass index.
Adequate nutritional status and hospitalization
The articles evaluated did not describe an association between good nutritional status and the risk of hospitalization for IBD.
Malnutrition versus hospitalization
We accept the definition of malnutrition that each author used in the studies. Of the five studies, two evaluated nutritional deficits using different databases in the United States[7,8]. In both cases, Ananthakrishnan et al[7] and Gajendran et al[8], malnutrition was diagnosed by the ICD-9-CM (International Classification of Diseases), which used serum levels of albumin (< 3.4) as indicators; involuntary weight loss of 5% in 3-6 mo and 10% in 6-12 mo; BMI < 18.5 kg/m² associated with comorbidity, poor diet, and loss of muscle mass[7,8]. In the cross-sectional study, the presence of malnutrition was associated with hospitalization in patients with IBD[8]. Similarly, in the retrospective study, severe hospitalization (classified as the need for any intestinal surgery or hospitalization time for more than 7 d) was also associated with malnutrition in patients with CD[7].
Obesity and hospitalization
Three studies evaluated obesity as a risk factor for IBD-related hospitalization, and the results were contradictory[4-6]. In Blain et al[4], it was observed that obese patients with CD had a greater chance of hospitalization related to the disease than those who were non-obese. However, in Flores et al[5], obese and overweight patients with CD and UC were less likely to experience a hospital stay related to IBD than those with eutrophic/thinness, thus suggesting that excess weight is an indicator of lower severity of disease. In a prospective study, Seminerio et al[6] observed that high a BMI (obesity classes I, II and III) is not associated with rates of hospitalization for IBD.
DISCUSSION
The main difficulty in nutritional assessment studies is exactly how to define nutritional status or to choose the indicator to be used. This is due to some limitations of the indicators and the consequent need to use several anthropometric parameters, biochemical tests, physical examinations, and food surveys and the interpretation of the data collected to arrive at an individualized diagnosis[10]. BMI is the most used nutritional indicator in clinical practice and in studies because it is simple, low cost, noninvasive, and practical[11]. Of the five studies evaluated, the majority used only BMI as an indicator of nutritional status, and only two studies defined nutritional status using other indicators[7,8].
Malnutrition is the most commonly found nutritional status in patients with hospitalized IBD, and in about 50% of those with severe malnutrition, the loss of body mass occurs 6 mo before hospital admission[2,12]. Quality of life in these patients is generally lower[13], and malnutrition has been associated with increased in-hospital mortality and length of stay and increased risk of hospitalization for IBD[8,14]. However, only two of the five studies selected evaluated malnutrition as a risk variable for hospitalization for IBD[7,8].
The use of nutritional therapy in patients with undernourished IBD has efficacy in improving nutritional status in some studies, especially in cases of disease-related surgery[15,16]. In one study, improvement in the malnutrition status after use of exclusive preoperative enteral nutrition in patients with CD was characterized by increased serum albumin levels and body weight gain in a 45 d period[15]. On the other hand, in patients with hospitalized undernourished CD, the need for nutritional therapy was identified as a predictor of disease severity[7]. Nutritional therapy and the risk of hospitalization IBD was not an objective of this study, but it is a relevant topic for future revisions.
Serum albumin, although commonly used to identify the nutritional status of patients with IBD, is not a good indicator, especially in the active phase of the disease due to the negative effect of inflammatory cytokines on this plasma protein[15,17,18]. However, it may influence the prognosis and consequent hospitalization related to IBD. In patients with UC, higher albumin values at admission were a protective factor for early hospital readmission[19]. In a sample evaluating mortality predictors in IBD patients admitted to the intensive care unit, hypoalbuminemia was associated with increased mortality in this population[20].
Poor or insufficient serum vitamin D levels increased the need for surgeries and hospitalizations in IBD patients when compared to patients who had normal serum vitamin D[21,22]. Considering that vitamin D is also referred to by some authors as a hormone and that diet is one of the factors that has little influence on the serum concentrations of 25(OH)D[23], some studies[21,24] were not chosen in our sample since the authors did not evaluate dietary intake or use of vitamin D supplements.
The prevalence of obesity has increased in patients with IBD, and in some places it is highly prevalent. This higher prevalence is accompanied by an increase in obese individuals in the general population[4,5,25], which may contribute to the early initiation of drug therapy, a greater number of surgeries, and more complications due to the disease[26]. Visceral obesity and IBD have in common the increased production of proinflammatory cytokines in the body; however, few studies have evaluated the relationship between obesity and the evolution and severity of IBD[11,27].
Different studies indicate that obesity in patients with IBD is not related to complications of the disease or need for surgeries, and it represents a less severe course of the disease in obese individuals[28,29]. The meta-analysis that assessed the impact of obesity on the clinical course of patients with IBD found that obese patients had less hospitalization experiences than non-obese patients (RR = 0.84 (95%CI: 0.74-0.94); Heterogeneity I2 = 0%, P = 0.32)[29]. These authors based their conclusions with a moderate degree of evidence from two studies, both included in this review: Flores et al[5], a retrospective, follow-up study of 518 patients with IBD in which obese and overweight patients were less likely to have hospitalization experience than the group with low/adequate BMI (42% vs 44% vs 66%, P < 0.001) and Seminerio et al[6], a prospective study of 1494 patients with IBD. There was no association between increased BMI and hospitalization in patients with IBD, in both those with CD and UC (P = 0.396)
The controversial results can be explained by the inclusion of retrospective studies in two of them and the nutritional indicator used to define obesity, BMI. BMI as the only measure of obesity has limitations because it does not differentiate between subcutaneous and visceral adipose tissue, resulting in an inadequate association with IBD[11,30,31]. Visceral obesity is more related to an increase in inflammatory cytokines, and assessing abdominal obesity requires other indicators, such as waist circumference[11,32].
Some studies have identified bariatric surgery as important in the treatment of obese patients with IBD, showing benefits such as the interruption or significant reduction in drug use and/or improvement of IBD-related symptoms[33,34]. New studies with more detailed investigation are needed to elucidate the role of obesity in IBD.
Nutritional status may influence hospitalizations for IBD. Among the few studies analyzed, the relationship with adequate nutritional status was not described, but malnutrition was related to hospitalization for the disease. Due to the contradictory results among studies on obesity, it was not possible to conclude the correlation with protective or risk factors for hospitalization for IBD. Since there were few studies identified for this review, further investigations are needed to evaluate the association between nutritional status and hospitalizations for IBD.
ARTICLE HIGHLIGHTS
Research background
Inflammatory bowel disease (IBD) presents an inflammatory picture that in the long run can lead to complications and consequently more hospitalizations when compared to other diseases.
Research motivation
Few studies have evaluated the association between nutritional status and hospitalization of patients with IBD and the consequent complications in the disease and surgical procedures.
Research objectives
The objective of our study was to evaluate the influence of nutritional status on the occurrence of IBD-related hospitalization.
Research methods
The research was conducted in the PUBMED and MEDLINE online databases in May 2018.
Research results
Of the 80 studies initially identified, five met the inclusion criteria of this review. None evaluated the association between good nutritional status and the risk of hospitalization. Malnutrition had a strong correlation with the risk of hospitalization related to IBD, and there was disagreement among the three studies regarding the association of obesity and hospitalization rates.
Research conclusions
Few studies have evaluated nutritional status as a predictor of IBD-related hospitalization, and the presence of malnutrition appears to be associated with hospitalization in these patients. Additional studies are needed to elucidate the issue.
Research perspectives
The few studies found in this review reveal the need for further investigations to evaluate the association between nutritional status and hospitalizations for IBD.
Footnotes
Conflict-of-interest statement: No potential conflicts of interest.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Manuscript source: Invited manuscript
Peer-review started: October 2, 2018
First decision: November 22, 2018
Article in press: January 10, 2019
Specialty type: Gastroenterology and hepatology
Country of origin: Brazil
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P- Reviewer: Day AS, Lee JEE, Tandon RK S- Editor: Ji FF L- Editor: Filipodia E- Editor: Song H
Contributor Information
Raquel Rocha, Escola de Nutrição, Universidade Federal da Bahia, Salvador 40110-150, Bahia, Brazil. raquelrocha2@yahoo.com.br.
Uli H Sousa, Escola de Nutrição, Universidade Federal da Bahia, Salvador 40110-150, Bahia, Brazil.
Thamiris L M Reis, Escola de Nutrição, Universidade Federal da Bahia, Salvador 40110-150, Bahia, Brazil.
Genoile O Santana, Pós graduação em Medicina e Saúde, Universidade Federal da Bahia, Salvador 40110-060, Bahia, Brazil; Department of Life Sciences, Universidade do Estado da Bahia, Salvador 41150-000, Bahia, Brazil.
References
- 1.Allegretti JR, Borges L, Lucci M, Chang M, Cao B, Collins E, Vogel B, Arthur E, Emmons D, Korzenik JR. Risk Factors for Rehospitalization Within 90 Days in Patients with Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:2583–2589. doi: 10.1097/MIB.0000000000000537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sökülmez P, Demirbağ AE, Arslan P, Dişibeyaz S. Effects of enteral nutritional support on malnourished patients with inflammatory bowel disease by subjective global assessment. Turk J Gastroenterol. 2014;25:493–507. doi: 10.5152/tjg.2014.4955. [DOI] [PubMed] [Google Scholar]
- 3.Matsumoto S, Yoshida Y. What are the factors that affect hospitalization and surgery for aggravation of ulcerative colitis? Eur J Gastroenterol Hepatol. 2014;26:282–287. doi: 10.1097/MEG.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 4.Blain A, Cattan S, Beaugerie L, Carbonnel F, Gendre JP, Cosnes J. Crohn's disease clinical course and severity in obese patients. Clin Nutr. 2002;21:51–57. doi: 10.1054/clnu.2001.0503. [DOI] [PubMed] [Google Scholar]
- 5.Flores A, Burstein E, Cipher DJ, Feagins LA. Obesity in Inflammatory Bowel Disease: A Marker of Less Severe Disease. Dig Dis Sci. 2015;60:2436–2445. doi: 10.1007/s10620-015-3629-5. [DOI] [PubMed] [Google Scholar]
- 6.Seminerio JL, Koutroubakis IE, Ramos-Rivers C, Hashash JG, Dudekula A, Regueiro M, Baidoo L, Barrie A, Swoger J, Schwartz M, Weyant K, Dunn MA, Binion DG. Impact of Obesity on the Management and Clinical Course of Patients with Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:2857–2863. doi: 10.1097/MIB.0000000000000560. [DOI] [PubMed] [Google Scholar]
- 7.Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. A novel risk score to stratify severity of Crohn's disease hospitalizations. Am J Gastroenterol. 2010;105:1799–1807. doi: 10.1038/ajg.2010.105. [DOI] [PubMed] [Google Scholar]
- 8.Gajendran M, Umapathy C, Loganathan P, Hashash JG, Koutroubakis IE, Binion DG. Analysis of Hospital-Based Emergency Department Visits for Inflammatory Bowel Disease in the USA. Dig Dis Sci. 2016;61:389–399. doi: 10.1007/s10620-015-3895-2. [DOI] [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Lacey KM, Pritchett ER. Nutrition Diagnosis: A Critical Step in the Nutrition Care Process. J Am Diet Assoc. 2006 [Google Scholar]
- 11.Carneiro Roriz AK, Santana Passos LC, Cunha De Oliveira C, Eickemberg M, De Almeida Moreira P, Barbosa Ramos L. Anthropometric clinical indicators in the assessment of visceral obesity: an update. Nutr Clínica Y Dietética Hosp. 2016;36:168–179. [Google Scholar]
- 12.Skowrońska-Piekarska U, Matysiak K, Sowińska A. The impact of the nutritional state of patients on the results of the surgical treatment of ulcerative colitis. Pol Przegl Chir. 2013;85:424–432. doi: 10.2478/pjs-2013-0065. [DOI] [PubMed] [Google Scholar]
- 13.Norman K, Kirchner H, Lochs H, Pirlich M. Malnutrition affects quality of life in gastroenterology patients. World J Gastroenterol. 2006;12:3380–3385. doi: 10.3748/wjg.v12.i21.3385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen GC, Munsell M, Harris ML. Nationwide prevalence and prognostic significance of clinically diagnosable protein-calorie malnutrition in hospitalized inflammatory bowel disease patients. Inflamm Bowel Dis. 2008;14:1105–1111. doi: 10.1002/ibd.20429. [DOI] [PubMed] [Google Scholar]
- 15.Zhu W, Guo Z, Zuo L, Gong J, Li Y, Gu L, Cao L, Li N, Li J. CONSORT: Different End-Points of Preoperative Nutrition and Outcome of Bowel Resection of Crohn Disease: A Randomized Clinical Trial. Medicine (Baltimore) 2015;94:e1175. doi: 10.1097/MD.0000000000001175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yao GX, Wang XR, Jiang ZM, Zhang SY, Ni AP. Role of perioperative parenteral nutrition in severely malnourished patients with Crohn's disease. World J Gastroenterol. 2005;11:5732–5734. doi: 10.3748/wjg.v11.i36.5732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henriksen M, Jahnsen J, Lygren I, Stray N, Sauar J, Vatn MH, Moum B IBSEN Study Group. C-reactive protein: a predictive factor and marker of inflammation in inflammatory bowel disease. Results from a prospective population-based study. Gut. 2008;57:1518–1523. doi: 10.1136/gut.2007.146357. [DOI] [PubMed] [Google Scholar]
- 18.Vagianos K, Bector S, McConnell J, Bernstein CN. Nutrition assessment of patients with inflammatory bowel disease. JPEN J Parenter Enteral Nutr. 2007;31:311–319. doi: 10.1177/0148607107031004311. [DOI] [PubMed] [Google Scholar]
- 19.Tinsley A, Naymagon S, Mathers B, Kingsley M, Sands BE, Ullman TA. Early readmission in patients hospitalized for ulcerative colitis: incidence and risk factors. Scand J Gastroenterol. 2015;50:1103–1109. doi: 10.3109/00365521.2015.1020862. [DOI] [PubMed] [Google Scholar]
- 20.Ha C, Maser EA, Kornbluth A. Clinical presentation and outcomes of inflammatory bowel disease patients admitted to the intensive care unit. J Clin Gastroenterol. 2013;47:485–490. doi: 10.1097/MCG.0b013e318275d981. [DOI] [PubMed] [Google Scholar]
- 21.Ananthakrishnan AN, Cagan A, Gainer VS, Cai T, Cheng SC, Savova G, Chen P, Szolovits P, Xia Z, De Jager PL, Shaw SY, Churchill S, Karlson EW, Kohane I, Plenge RM, Murphy SN, Liao KP. Normalization of plasma 25-hydroxy vitamin D is associated with reduced risk of surgery in Crohn's disease. Inflamm Bowel Dis. 2013;19:1921–1927. doi: 10.1097/MIB.0b013e3182902ad9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kabbani TA, Koutroubakis IE, Schoen RE, Ramos-Rivers C, Shah N, Swoger J, Regueiro M, Barrie A, Schwartz M, Hashash JG, Baidoo L, Dunn MA, Binion DG. Association of Vitamin D Level With Clinical Status in Inflammatory Bowel Disease: A 5-Year Longitudinal Study. Am J Gastroenterol. 2016;111:712–719. doi: 10.1038/ajg.2016.53. [DOI] [PubMed] [Google Scholar]
- 23.Gozdzik A, Barta JL, Wu H, Wagner D, Cole DE, Vieth R, Whiting S, Parra EJ. Low wintertime vitamin D levels in a sample of healthy young adults of diverse ancestry living in the Toronto area: associations with vitamin D intake and skin pigmentation. BMC Public Health. 2008;8:336. doi: 10.1186/1471-2458-8-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Venkata KVR, Arora SS, Xie FL, Malik TA. Impact of vitamin D on the hospitalization rate of Crohn's disease patients seen at a tertiary care center. World J Gastroenterol. 2017;23:2539–2544. doi: 10.3748/wjg.v23.i14.2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nic Suibhne T, Raftery TC, McMahon O, Walsh C, O'Morain C, O'Sullivan M. High prevalence of overweight and obesity in adults with Crohn's disease: associations with disease and lifestyle factors. J Crohns Colitis. 2013;7:e241–e248. doi: 10.1016/j.crohns.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Steed H, Walsh S, Reynolds N. A brief report of the epidemiology of obesity in the inflammatory bowel disease population of Tayside, Scotland. Obes Facts. 2009;2:370–372. doi: 10.1159/000262276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karmiris K, Koutroubakis IE, Xidakis C, Polychronaki M, Voudouri T, Kouroumalis EA. Circulating levels of leptin, adiponectin, resistin, and ghrelin in inflammatory bowel disease. Inflamm Bowel Dis. 2006;12:100–105. doi: 10.1097/01.MIB.0000200345.38837.46. [DOI] [PubMed] [Google Scholar]
- 28.Mendall MA, Gunasekera AV, John BJ, Kumar D. Is obesity a risk factor for Crohn's disease? Dig Dis Sci. 2011;56:837–844. doi: 10.1007/s10620-010-1541-6. [DOI] [PubMed] [Google Scholar]
- 29.Hu Q, Ren J, Li G, Wu X, Li J. The Impact of Obesity on the Clinical Course of Inflammatory Bowel Disease: A Meta-Analysis. Med Sci Monit. 2017;23:2599–2606. doi: 10.12659/MSM.901969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii, 1-253. [PubMed] [Google Scholar]
- 31.Singh S, Dulai PS, Zarrinpar A, Ramamoorthy S, Sandborn WJ. Obesity in IBD: epidemiology, pathogenesis, disease course and treatment outcomes. Nat Rev Gastroenterol Hepatol. 2017;14:110–121. doi: 10.1038/nrgastro.2016.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fain JN, Madan AK, Hiler ML, Cheema P, Bahouth SW. Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissues of obese humans. Endocrinology. 2004;145:2273–2282. doi: 10.1210/en.2003-1336. [DOI] [PubMed] [Google Scholar]
- 33.Aminian A, Andalib A, Ver MR, Corcelles R, Schauer PR, Brethauer SA. Outcomes of Bariatric Surgery in Patients with Inflammatory Bowel Disease. Obes Surg. 2016;26:1186–1190. doi: 10.1007/s11695-015-1909-y. [DOI] [PubMed] [Google Scholar]
- 34.Keidar A, Hazan D, Sadot E, Kashtan H, Wasserberg N. The role of bariatric surgery in morbidly obese patients with inflammatory bowel disease. Surg Obes Relat Dis. 2015;11:132–136. doi: 10.1016/j.soard.2014.06.022. [DOI] [PubMed] [Google Scholar]