To the Editor:
Associations between new arrhythmias and the risk of death during a critical illness are well described (1, 2). However, whether arrhythmias during a critical illness are markers of more severe disease or lie on pathways that mediate increased mortality risks is unclear. Results from two randomized trials suggested that the use of higher blood pressure targets during shock increased the risks for arrhythmias and, in patients requiring more than 6 hours of vasopressors before trial enrollment, mortality (3–5). We analyzed data from these randomized trials to evaluate the role of new arrhythmias in pathways linking higher blood pressure targets to poor outcomes during shock.
Methods
We performed a secondary analysis of individual patient-level data from two randomized controlled trials: SEPSISPAM (Assessment of Two Levels of Arterial Pressure on Survival in Patients with Septic Shock) (5) and OVATION (Optimal Vasopressor Titration) (6). Details of the source trial methods can be found in the original publications (6, 7). Briefly, adult patients with vasodilatory shock (OVATION) or septic shock (SEPSISPAM) were randomized to vasopressors titrated to achieve either higher (mean arterial pressure 75–85 mm Hg) or lower (mean arterial pressure 60–70 mm Hg) blood pressure targets. Each trial recorded postrandomization ventricular and supraventricular arrhythmias as adverse events.
Pathways that link interventions with outcomes may be explored through mediation and moderation analyses. Mediation quantifies the extent to which hypothesized pathways may explain the effect of an intervention on an outcome. Moderation (i.e., interaction) analyses evaluate the extent to which a variable modifies the effect of an intervention on an outcome without representing an intermediate step on the causal pathway. We used Proc Causalmed in SAS 9.4 T1M5 (7) to quantify mediation and interaction by new tachyarrhythmias within previously described associations between higher (versus lower) blood pressure targets and the outcome of persistent organ dysfunction or death at Day 28 (4). Aspects of mediation and interaction that are most relevant for evaluating the potential benefits of a therapeutic intervention include 1) the controlled direct effect (i.e., the component of the effect of higher blood pressure targets not due to mediation or interaction with arrhythmia) and 2) the “portion eliminated”—a composite of mediation and interaction effects that represents the theoretical proportion of adverse outcomes that could be eliminated if the proposed mediator (new-onset tachyarrhythmias) were prevented (8). Models were adjusted for potential confounders between the mediator and outcome using a propensity score for arrhythmia onset calculated from age, sex, medical or surgical admission, predicted probability of mortality (from Simplified Acute Physiology Score II or Acute Physiology and Chronic Health Evaluation II), Day 1 total vasopressor dose, comorbid hypertension, heart failure, coronary artery disease, arrhythmia history, and trial, using a random effect for study center. The primary analysis was conducted among patients who were enrolled after 6 or more hours of shock, in whom higher blood pressure targets were associated with higher risks of death (4). Sensitivity analyses evaluated patients who were enrolled within 6 hours of shock, and supraventricular and ventricular arrhythmias were considered separately.
Results
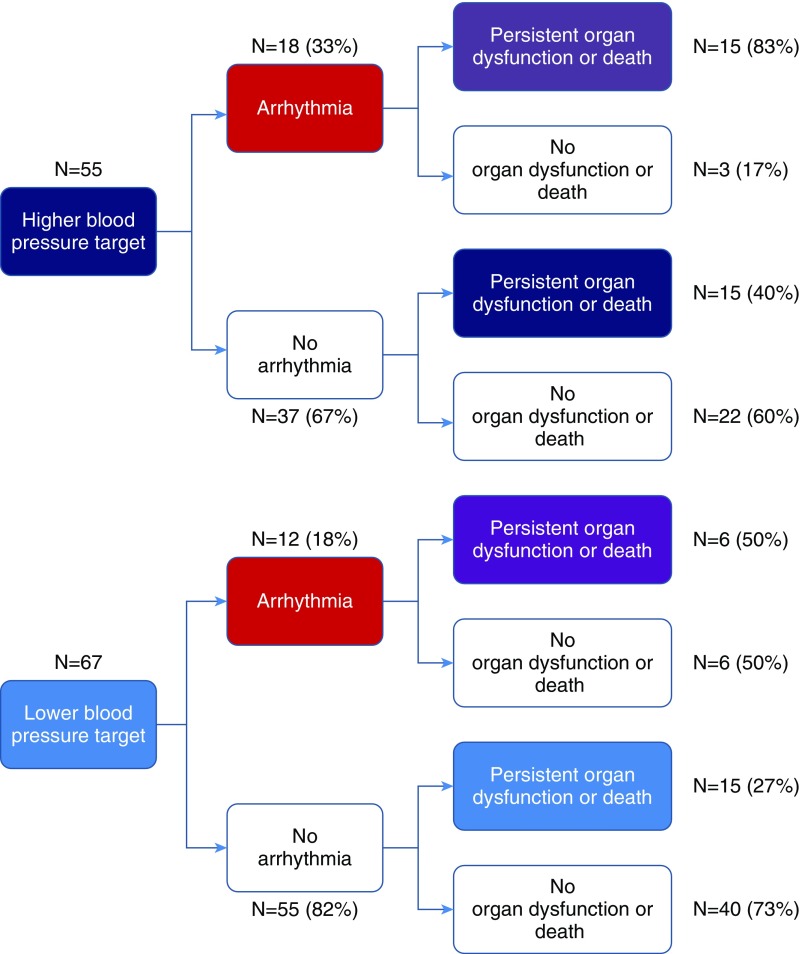
Among 894 patients across two randomized trials of blood pressure targets during septic shock (5), 122 (14%) had more than 6 hours of shock before enrollment and were included in the primary analysis. Figure 1 shows the observed outcomes in the proposed pathways between high blood pressure targets (intervention), new tachyarrhythmias (proposed mediator), and persistent organ dysfunction or death by Day 28 (outcome). Compared with lower blood pressure targets, higher targets were associated with increased risk for persistent organ dysfunction or death (odds ratio [OR], 2.49 [95% confidence interval (CI), 1.17–5.31], P = 0.02), and a numerically higher risk of new arrhythmia (OR, 2.36 [95% CI, 0.97–5.72], P = 0.06). New arrhythmias were also associated with increased risk of the primary outcome of persistent organ dysfunction or death at Day 28 (OR, 4.69 [95% CI, 1.83–12.0], P = 0.001). Analysis stratified by presence of arrhythmia suggested an interaction between arrhythmia onset and higher blood pressure targets for persistent organ dysfunction or death by Day 28 (OR, 1.75 [95% CI, 0.72–4.28] among patients without arrhythmia; OR, 4.5 [95% CI, 0.78–26] among patients with arrhythmia).
Figure 1.
Outcome distributions in the proposed pathways among higher blood pressure targets, arrhythmia, and persistent organ dysfunction or death.
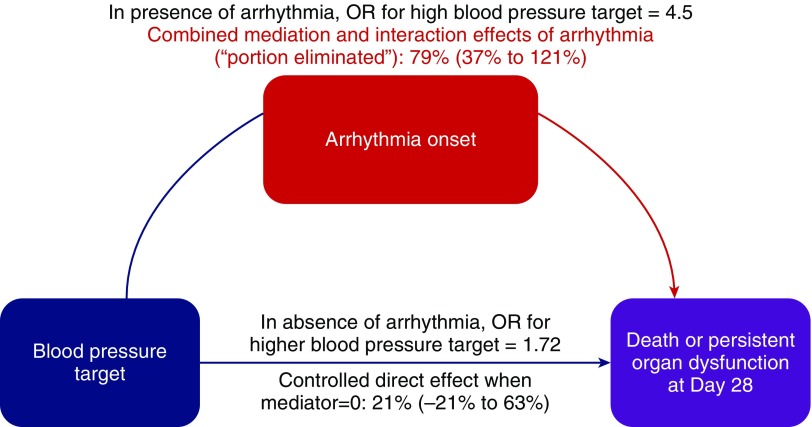
Results of the mediation analysis are shown in Figure 2. Approximately 79% (95% CI, 37–121%) of the observed effects of higher blood pressure targets on persistent organ dysfunction or death were due to either mediation by or interaction with arrhythmias (i.e., the “portion eliminated”), whereas controlled direct effects of higher blood pressure targets accounted for 21% (95% CI, −21% to 63%). Sensitivity analyses showed a “portion eliminated” for supraventricular arrhythmias of 68% (95% CI, 14–121%); however, ventricular arrhythmia models were not estimable because there were only four recorded ventricular events. Among patients who were randomized before 6 hours of shock, in whom higher blood pressure targets were not associated with primary outcome (OR, 0.90 [95% CI, 0.70–1.16]), the portion eliminated for arrhythmias was 5% (95% CI, −140% to 150%).
Figure 2.
Results of analyses assessing proposed pathways between higher blood pressure targets and persistent organ dysfunction or death that account for effects of arrhythmia through mediation and interaction. Arrhythmias were estimated to account for 79% (95% confidence interval, 37–121%) of the observed effects of higher blood pressure targets on persistent organ dysfunction or death. Effects of higher blood pressure targets on persistent organ dysfunction or death could be decomposed into 1) controlled direct effects 21% (−21% to 63%)—the component not due to mediation by or interaction with arrhythmias, i.e., setting arrhythmia to 0; 2) reference interaction 37% (0.92% to 74%)—the component due to interaction, but not mediation, with arrhythmias; 3) mediated interaction 35% (−0.3% to 70%)—the component due to both mediation by and interaction with arrhythmias; and 4) pure indirect effects 7% (−11% to 24%)—the component due to mediation through arrhythmia alone. OR = odds ratio.
Discussion
We explored the potential role of arrhythmias in mediating associations between higher blood pressure targets and persistent organ dysfunction or mortality among patients with shock. Our findings suggest that arrhythmias have a complex role in pathways linking higher blood pressure targets to poor outcomes, acting to both mediate and potentiate the downstream effects of higher blood pressure targets. The mechanisms of mediation of poor outcomes by arrhythmias are mostly speculative. One possible mechanism that is supported by temporal associations between supraventricular arrhythmia onset and hemodynamic worsening is higher vasopressor doses triggering arrhythmias, which then lead to reduced diastolic filling, cardiac output, and perfusion (9). Mechanisms by which arrhythmias may interact with higher blood pressure targets are less clear and require further study, but potentially involve synergistic potentiation of diastolic dysfunction or ventriculoarterial uncoupling (10). Our findings should be considered in light of the limitations of a small sample size, low statistical power, lack of differentiation between arrhythmias (e.g., atrial fibrillation vs. other supraventricular arrhythmias), and evaluation of secondary subgroup analyses of randomized trials. The validity of our results is based on assumptions that associations between higher blood pressure targets, arrhythmias, and persistent organ dysfunction or mortality are not affected by unmeasured confounders. Thus, our results should be considered exploratory and hypothesis generating, but they support the concept that new supraventricular arrhythmias may play both direct and indirect roles in pathways that lead to poor patient outcomes during shock. Future trials are needed to test the hypothesis that prevention or improved treatment of supraventricular arrhythmias during critical illness (e.g., through alternative vasopressor strategies or β blockade) may positively impact patient outcomes.
Supplementary Material
Acknowledgments
Acknowledgment
We acknowledge the immense contributions of the patients, staff, and investigators for the OVATION and SEPSISPAM trials, without whom this analysis could not have been performed.
Footnotes
Supported by NIH/NHLBI grants K01HL116768 and R01 HL136660 (A.J.W.).
Author Contributions: A.J.W.: study conception and design, data analysis and interpretation, and drafting and approval of the manuscript. A.G.D.: data acquisition and approval of the manuscript. N.K.J.A.: study conception and design, data interpretation, and drafting and approval of the manuscript. P.R.: data acquisition and interpretation, and drafting and approval of the manuscript. P.A.: data acquisition and interpretation, and drafting and approval of the manuscript. F.L.: study conception and design, data acquisition and interpretation, and drafting and approval of the manuscript.
Originally Published in Press as DOI: 10.1164/rccm.201808-1435LE on December 19, 2018
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Walkey AJ, Wiener RS, Ghobrial JM, Curtis LH, Benjamin EJ. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. JAMA. 2011;306:2248–2254. doi: 10.1001/jama.2011.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaver CM, Chen W, Janz DR, May AK, Darbar D, Bernard GR, et al. Atrial fibrillation is an independent predictor of mortality in critically ill patients. Crit Care Med. 2015;43:2104–2111. doi: 10.1097/CCM.0000000000001166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McIntyre WF, Um KJ, Alhazzani W, Lengyel AP, Hajjar L, Gordon AC, et al. Association of vasopressin plus catecholamine vasopressors vs catecholamines alone with atrial fibrillation in patients with distributive shock: a systematic review and meta-analysis. JAMA. 2018;319:1889–1900. doi: 10.1001/jama.2018.4528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lamontagne F, Day AG, Meade MO, Cook DJ, Guyatt GH, Hylands M, et al. Pooled analysis of higher versus lower blood pressure targets for vasopressor therapy septic and vasodilatory shock. Intensive Care Med. 2018;44:12–21. doi: 10.1007/s00134-017-5016-5. [DOI] [PubMed] [Google Scholar]
- 5.Asfar P, Meziani F, Hamel J-F, Grelon F, Megarbane B, Anguel N, et al. SEPSISPAM Investigators. High versus low blood-pressure target in patients with septic shock. N Engl J Med. 2014;370:1583–1593. doi: 10.1056/NEJMoa1312173. [DOI] [PubMed] [Google Scholar]
- 6.Lamontagne F, Meade MO, Hébert PC, Asfar P, Lauzier F, Seely AJE, et al. Canadian Critical Care Trials Group. Higher versus lower blood pressure targets for vasopressor therapy in shock: a multicentre pilot randomized controlled trial. Intensive Care Med. 2016;42:542–550. doi: 10.1007/s00134-016-4237-3. [DOI] [PubMed] [Google Scholar]
- 7.VanderWeele TJ. A unification of mediation and interaction: a 4-way decomposition. Epidemiology. 2014;25:749–761. doi: 10.1097/EDE.0000000000000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.VanderWeele TJ. Policy-relevant proportions for direct effects. Epidemiology. 2013;24:175–176. doi: 10.1097/EDE.0b013e3182781410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kanji S, Williamson DR, Yaghchi BM, Albert M, McIntyre L Canadian Critical Care Trials Group. Epidemiology and management of atrial fibrillation in medical and noncardiac surgical adult intensive care unit patients. J Crit Care. 2012;27:326.e1–326.e8. doi: 10.1016/j.jcrc.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 10.Guarracino F, Ferro B, Morelli A, Bertini P, Baldassarri R, Pinsky MR. Ventriculoarterial decoupling in human septic shock. Crit Care. 2014;18:R80. doi: 10.1186/cc13842. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.