Abstract
Purpose:
To investigate the influence of sexual activity and contraceptive use on the decline in adolescent birth rates and pregnancy rates since 2007.
Methods:
We estimated trends in pregnancy risk from 2007 to 2014 using national data on behaviors of women aged 15–19.
Results:
In 2007–2014, increases occurred in use of one or more contraceptive methods at last sex (78%–88%), dual method use (24%–33%), long-acting reversible contraception including intrauterine device and implant (1%–7%), withdrawal (15%–26%), and withdrawal in combination with other methods (7%–17%). Pill use rose and then fell over time. Level of sexual activity did not change over time. The decline in pregnancy risk among women aged 15–19 was entirely attributable to improvements in contraceptive use.
Conclusions:
Improvements in contraceptive use—including increases in use of long-acting reversible contraception and withdrawal in combination with another method—appear to be driving recent declines in adolescent birth and pregnancy rates.
Keywords: Abstinence, Contraception, Sexual behaviors, Adolescent pregnancy, Birthrate
Adolescent birth rates declined dramatically between 2007 and 2016 in the United States (U.S.), following long-term declines in 1957–1986 and 1991–2005; since 1991 adolescent pregnancy rates have also fallen [1,2]. To understand the behavioral drivers of these declines, we developed the pregnancy risk index (PRI), which attributes changes in adolescent pregnancy rates to changes in sexual activity and contraceptive use, the key proximal determinants of fertility [3–5]. The PRI has been validated by demonstrating that changes over time in the PRI track relatively closely with changes over time in adolescent pregnancy and birth rates.
Our published research using the National Survey of Family Growth (NSFG) and the Youth Risk Behavior Survey found that declines in adolescent women’s rates of pregnancy and birth after 1991 were influenced primarily by increases in contraceptive use, and, to a lesser degree, declines in sexual activity; we found considerable increases in condom use and declines in contraceptive nonuse in the 1990s and 2000s [4,5]. In our most recent study of NSFG data, we documented increases in 2007–2012 in hormonal methods among women aged 15–19, as well as declines in contraceptive nonuse, but no change in sexual activity [3].
This brief report updates our last study by using the most recent NSFG data to extend the study period to 2015. Both adolescent sexual activity and contraceptive use continue to be the focus of policy debates. Understanding their relative roles in recent declines in rates of birth and pregnancy among adolescents can inform policies and programs designed to help young people achieve their reproductive goals.
Methods
We used data from women aged 15–19 from the 2006 to 2015 NSFG, a national probability household survey. Sampling weights provided by the National Center for Health Statistics allow division of the data into nationally representative and nonoverlapping 2-year periods, which we refer to by their midpoints (2007, 2009, 2012, and 2014) [6]. Methods of data collection and dissemination of the public-use dataset were approved by the National Center for Health Statistics Institutional Review Board’s protections of human subjects.
We calculated the PRI for each period, estimating adolescent women’s annualized risk of becoming pregnant based on their recent sexual activity (vaginal-penile sex in the last 3 months), contraceptive method(s) used at last sexual intercourse and method-specific contraceptive failure rates [7]; nonuse of contraception was also assigned a specific pregnancy risk. Logistic regression with continuous and quadratic terms for survey year was used to test for linear and quadratic (U-shaped) changes in measures between 2007 and 2014. Statistical decomposition was used to attribute change in the PRI to changes in sexual activity or contraceptive method use. Complete methodological details can be found in our 2016 paper [3].
Results
Sexual activity in the last 3 months did not change between 2007 (31%) and 2014 (31%) (Table 1); alternative measures of sexual activity (ever had sex, sex in the last 12 months, sex in the last 4 weeks) were also stable over time (results not shown). From 2007 to 2014, there were significant linear increases in use of any contraceptive method (78%–88%, p < .05) and 2 or more methods (24%–33% (p < .05), as well as intrauterine device and implant (1%–7%, p < .05), and withdrawal (15%–26%, p < .05) (Table 1). There were significant quadratic changes (i.e., rising and then falling) in pill use (p = .023). Withdrawal use in combination with other methods more than doubled (7%–17%, p < .01).
Table 1.
Sexual activity among all women aged 15–19, and contraceptive method use among sexually-active women aged 15–19, by NSFG survey year, 2007–2014
| Survey year |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2007 |
2009 |
2012 |
2014 |
Test for change over time |
||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | p value (Linear terma) | p value (Quadratic terma) | |
| All women 15–19years | (N = 1,085) | (N = 1,199) | (N = 1,037) | (N = 1,010) | ||||||
| Sexually active in last 3 months | 31 | (27, 35) | 33 | (30, 37) | 30 | (25, 35) | 31 | (27,36) | .737 | .768 |
| Sexually active women 15–19 years | (N = 366) | (N = 403) | (N = 320) | (N = 308) | ||||||
| Number of methods used at last sex | ||||||||||
| No method | 22 | (17,28) | 13 | (9,19) | 14 | (9, 20) | 12 | (8,18) | .012 | .262 |
| One or more methods | 78 | (72,83) | 87 | (81,91) | 86 | (80, 91) | 88 | (82,92) | .012 | .262 |
| Two or more methods | 24 | (18,30) | 30 | (23, 38) | 34 | (26,43) | 33 | (26,41) | .040 | .301 |
| Method type | ||||||||||
| IUD and implant | 1 | (0.5,4) | 4 | (2,9) | 3 | (1,9) | 7 | (4,13) | .023 | .718 |
| Injectable | 6 | (4,10) | 10 | (7,14) | 7 | (4,11) | 8 | (5,13) | .815 | .405 |
| Pill | 26 | (21,32) | 33 | (27, 40) | 35 | (27,43) | 27 | (20,34) | .775 | .023 |
| Patch and ring | 5 | (3,9) | 4 | (2,7) | 1 | (0.2, 2) | 3 | (0.7,15) | .478 | .402 |
| Condom | 49 | (42, 56) | 50 | (43, 58) | 55 | (48, 63) | 55 | (45,64) | .212 | .881 |
| Alone | 29 | (24, 34) | 25 | (19, 32) | 30 | (22, 38) | 30 | (21,39) | .667 | .493 |
| With another methodb | 19 | (14,26) | 26 | (20, 33) | 25 | (18, 34) | 24 | (18,32) | .299 | .288 |
| Withdrawal | 15 | (10,22) | 18 | (13, 25) | 20 | (14,28) | 26 | (20,33) | .020 | .775 |
| Alone | 8 | (5,12) | 9 | (5,15) | 8 | (5,13) | 9 | (5,14) | .912 | .841 |
| With another methodc | 7 | (4,11) | 9 | (5,15) | 12 | (6, 21) | 17 | (12,25) | .004 | .813 |
IUD = intrauterine devices; NSFG = National Survey of Family Growth.
Centered to the mean of survey year.
Includes condom use in combination with any of the following methods: IUD, injectable, implant, pill, patch, ring, and withdrawal.
Includes withdrawal use in combination with any of the following methods: IUD, injectable, implant, pill, patch, ring, and condom.
Data for adolescent men (not shown) showed similar trends in 2007–2014: no change in sexual activity or condom use but a significant linear increase in withdrawal at last sex (14%–32%, p < .01).
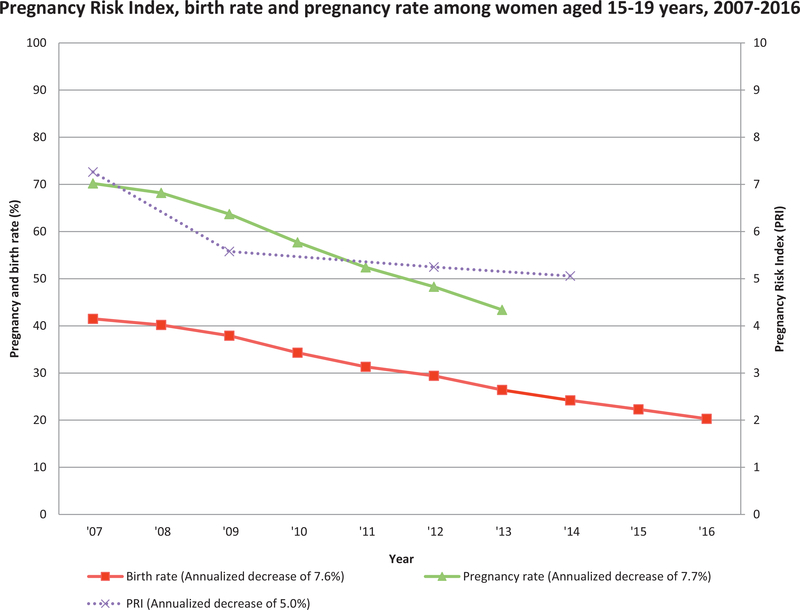
Over the full study period, the PRI underwent a significant annualized decline of 5.0% (p < .05; Figure 1). The birth and pregnancy rates had annualized declines of 7.6% (2007–2016) and 7.7% (2007–2013), respectively [1,2]. Statistical decomposition estimated that the 2007–2014 decline in the PRI was entirely attributable to improvement in contraceptive use.
Figure 1.
Birth Rate, Pregnancy Rate, Pregnancy Risk Index and Percent Change Over Time among women aged 15–19 years, 2007–2014.
Discussion
Improvement in contraceptive use, including increases in use of any method, dual methods, LARC and withdrawal, was the primary proximal determinant of declines in adolescent pregnancy and birth rates in the United States from 2007 to 2014. Compared with our previous study examining change in pregnancy risk in 2007–2012, this study identifies increases in the use of LARC and withdrawal; these patterns have also been documented in other studies [8].
These recent changes in contraceptive use may reflect greater motivation among young people to avoid unintended pregnancy. Even use of withdrawal, with a relatively high failure rate, improves upon no method use. Overall, unintended pregnancy has declined recently among U.S. women [9]. But three in four adolescent pregnancies are still reported as unintended [9], suggesting a need for further improvements in contraceptive use. Recent increases in rates of sexually transmitted infections among young people also highlight the need to support condom use alone or in combination with other contraceptive methods [10]. Supporting adolescents’ health should include ensuring their access to confidential sexual and reproductive health care including contraceptive methods and to medically accurate contraceptive information, using approaches such as classroom sex education and innovative digital efforts.
While our analysis using NSFG data finds no change in sexual experience or activity among 15–19 year olds, the Youth Risk Behavior Survey estimates that sexual experience declined from 2005 to 2015 among high school students [11]. This variation in findings may reflect methodological differences, including different age ranges, samples and survey modes, between the two national surveys. Analyzing upcoming 2015–2017 data from both sources will be important in understanding trends in adolescent sexual activity and pregnancy risk.
Trends in the estimated PRI have correlated well with trends in adolescent birth and pregnancy rates in this and our previous studies [1,2]. In this study, the PRI somewhat underestimated declines in both rates, which may reflect improvements in contraceptive efficacy [7].
Supplementary Material
IMPLICATIONS AND CONTRIBUTION.
This study and previous work support the important contribution of contraceptive use to declines in U.S. adolescent fertility since 1991. Improving adolescent access to contraceptive methods is essential. Likewise, classroom and digital education efforts are needed to equip adolescents with critical resources to achieve their reproductive goals.
Acknowledgment
The analysis was funded by an anonymous donor. Additional support was provided by the Guttmacher Center for Population Research Innovation and Dissemination through grant 5 R24 HD074034 from the National Institutes of Health.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Supplementary Data
Supplementary data related to this article can be found at doi:10.1016/j.jadohealth.2018.05.017.
References
- [1].Kost K, Maddow-Zimet I, Arpaia A. Pregnancies, births and abortions among adolescents and young women in the United States, 2013: National and State Trends by Age, Race and Ethnicity. 2017.
- [2].Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: Final data for 2016. Natl Vital Stat Rep Cent Dis Control Prev Natl Cent Health Stat Natl Vital StatSyst 2018;67:55. [PubMed] [Google Scholar]
- [3].Lindberg L, Santelli J, Desai S. Understanding the decline in adolescent fertility in the United States, 2007–2012. J Adolesc Health 2016;59:577–83. 10.1016/jjadohealth.2016.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Santelli JS, Lindberg LD, Finer LB, Singh S. Explaining recent declines in adolescent pregnancy in the United States: The contribution of abstinence and improved contraceptive use. Am J Public Health 2007;97:150–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Santelli JS, Abma J, Ventura S, et al. Can changes in sexual behaviors among high school students explain the decline in teen pregnancy rates in the 1990s? J Adolesc Health 2004;35:80–90. 10.1016/jjado-health.2004.05.001. [DOI] [PubMed] [Google Scholar]
- [6].2011–2013 National Survey of Family Growth (NSFG): Summary of Design and Data Collection Methods. https://www.cdc.gov/nchs/data/nsfg/nsfg_2011_2013_designanddatacollectionmethods.pdf. Accessed January 23, 2018.
- [7].Sundaram A, Vaughan B, Kost K, et al. Contraceptive failure in the United States: Estimates from the 2006 to 2010 National Survey of Family Growth. Perspect Sex Reprod Health 2017;49:7–16. 10.1363/psrh.12017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kavanaugh ML, Jerman J. Contraceptive method use in the United States: Trends and characteristics between 2008, 2012 and 2014. Contraception 2018;97:14–21. 10.1016/j.contraception.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N EnglJ Med 2016;374:843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Sexually transmitted disease surveillance 2016. Atlanta: U.S. Department of Health and Human Services: Center for Disease Control and Prevention; 2017. https://www.cdc.gov/std/stats. [Google Scholar]
- [11].Ethier KA, Kann L, McManus T. Sexual intercourse among high school students—29 States and United States overall, 2005–2015. MMWR Morb Mortal Wkly Rep 2018;66:1393–7. 10.15585/mmwr.mm665152a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.