Abstract
Depressive symptoms vary in severity and chronicity. We used group-based trajectory models to describe trajectories of depressive symptoms (measured using the Patient Health Questionnaire-9) and predictors of trajectory group membership among 1493 HIV-infected men (84%) and 292 HIV-infected women (16%). At baseline, 29% of women and 26% of men had depressive symptoms. Over a median of 30 months of follow-up, we identified four depressive symptom trajectories for women (labeled “low” [experienced by 56% of women], “mild/moderate” [24%], “improving” [14%], and “severe” [6%]) and five for men (“low” [61%], “mild/moderate” [14%], “rebounding” [5%], “improving” [13%], and “severe” [7%]). Baseline antidepressant prescription, panic symptoms, and prior mental health diagnoses were associated with more severe or dynamic depressive symptom trajectories. Nearly a quarter of participants experienced some depressive symptoms, highlighting the need for improved depression management. Addressing more severe or dynamic depressive symptom trajectories may require interventions that additionally address mental health comorbidities.
Keywords: Depression, Depressive symptoms, Trajectory analysis, Group-based trajectory models, HIV
Introduction
Depression is the most commonly reported mental health condition among people living with HIV (PLWH), affecting 20–30% of HIV-infected adults in the United States [1, 2]. For PLWH, depression negatively impacts quality of life [3, 4], antiretroviral therapy (ART) adherence [5, 6], viral suppression [7–9], and long-term survival, and it has been linked to sexual transmission risk behavior [7, 10–15]. Despite numerous calls to improve depression treatment [16, 17] and the availability of effective depression treatment interventions [18–22], depression remains a critical issue affecting quality of life and HIV outcomes for PLWH.
Understanding patterns of depressive symptom presence and severity over time may help to improve the management of depressive symptoms for HIV-infected adults. Many studies implicitly treat different levels and trajectories of depression as the same, measuring the prevalence of depressive symptoms at one time point and categorizing participants dichotomously as either depressed or not depressed [23–27]. However, the clinical manifestation of depression is often more complex. Depressive symptoms may change over time and be reoccurring, particularly among PLWH [28–30]. Similarly, heterogeneity in severity of depressive symptoms exists, with more severe depressive symptoms correlating with increased risk behaviors and lower CD4 counts in HIV-infected adults [31]. Given the complex nature of depression, a more nuanced picture of how individuals who follow similar patterns of depressive symptoms cluster over time may help to guide clinical management.
In this analysis, we use data from a large cohort of HIV-infected adults in routine HIV care to describe distinct trajectories of depressive symptoms over time and to explore characteristics associated with membership in each trajectory. Our analysis provides a longitudinal view of depressive symptoms in which the time origin varies across individuals with respect to time since HIV diagnosis, HIV care entry, and depression emergence. Although more meaningful trajectory origins may be identified from a developmental standpoint, our analyses represent the reality in which assessment of depressive symptoms may begin at varying time points within the lifespan. Our goal is to provide a more realistic conceptualization of the range and patterns of depressive symptoms that patients experience over time, which may help to guide clinical care for depression management among HIV-infected adults and ultimately lead to more targeted depression treatment interventions.
Methods
Data come from the Centers for AIDS Research (CFAR) Network of Integrated Clinical Systems (CNICS) cohort. The CNICS cohort includes over 31,000 HIV-infected adults in routine HIV clinical care across eight sites in the United States. Details about the CNICS cohort have previously been published [32]. Briefly, CNICS captures comprehensive clinical data through electronic medical records and other institutional data systems, including standardized diagnosis, medication prescription, laboratory, and demographic information. Participants in CNICS also complete self-administered questionnaires, or patient-reported outcomes (PROs), on touch-screen tablets as part of routine clinical visits [33, 34]. PROs are completed approximately every 4–6 months, with variation based on individual patients’ clinical follow-up. All participants provide written informed consent to participate in CNICS. Ethical approval for the use of routinely collected clinical data was provided by the institutional review board at each CNICS site.
Study Population
We included HIV-infected adults enrolled in routine HIV care on or after PRO data collection began at their CNICS site (2005–2011, depending on site). Participants were followed from their first PRO measure (baseline) for up to 4 years or until administrative censoring (2014–2015, depending on site), whichever date came first. Follow-up time was divided into six-month intervals and the latest PRO measure in each interval was used in the analysis. In order to have sufficient information on depressive symptoms to describe trajectories over time, we only included participants who had a minimum of four, and a maximum of eight, consecutive six-month windows with a completed PRO. Additionally, we included only participants who had no more than one six-month interval without a PRO measure during their follow-up period. Group-based trajectory models allow for interim missing outcome data, while retaining all observed outcome measures, under the assumption that the data are missing completely at random [35]. Participants who died or were lost to follow-up prior completing four consecutive PRO measures within the allotted time interval were excluded.
Measures
Depressive symptoms were measured as part of routine PRO assessments as a continuous score using the Patient Health Questionnaire-9 (PHQ-9) [36]. The PHQ-9 asks about depressive symptoms over the last 2 weeks and ranges from a score of 0–27, with < 5 representing no depressive symptoms, 5–9 mild depressive symptoms, 10–14 moderate symptoms, 15–19 moderately severe symptoms, and ≥ 20–27 severe depressive symptoms [36]. A PHQ-9 score ≥ 10 has 88% sensitivity and specificity to detect a major depressive episode [36].
We considered a number of baseline clinical, HIV, substance use, mental health, and sociodemographic factors that may be associated with depressive symptom trajectory group membership. All measures were taken during a participant’s first PRO measure or at CNICS enrollment. CNICS PROs include validated measures of ART adherence (Adult AIDS Clinical Trials Unit Adherence Instrument, defined as no missed doses in the past week [37]), panic disorder (PHQ-5, defined as none, some panic disorder symptoms, or panic disorder over the last 4 weeks [38]), high risk alcohol use over the last year (Alcohol Use Disorders Identification Test (AUDIT), defined as AUDIT-C score > 4 for males and > 3 for females [39]), and illicit drug use, excluding marijuana (Alcohol, Smoking and Substance Involvement Screening Test (ASSIST), defined as none, past, or current [40, 41]).
In addition to PRO measures, CNICS also collects sociodemographic and clinical information which may influence depressive symptom trajectory group membership. Self-reported race/ethnicity (white, black, Hispanic, or other) and risk factors for HIV acquisition (male-to-male sexual contact (MSM), heterosexual contact, intravenous drug use (IDU) or other) were collected from participants’ medical records. Information on whether a participant had an active antidepressant prescription was also taken from participants’ medical records. CNICS also captures previous clinician-documented mental health, hypertension, and diabetes-related diagnoses in the medical record. A prior mental health disorder was defined as any previous mental health-related diagnosis, including anxiety, depression, bipolar disorder, post-traumatic stress disorder (PTSD), psychosis, or other personality or mood disorders at the time of a patient’s first PRO measure. We defined a prior hypertension or diabetes comorbidity as any previous medical diagnosis related to hypertension or diabetes at the time of a patient’s first PRO measure. Information on clinician-documental mental health, diabetes or hypertension related diagnoses prior to entry into CNICS care was not available. We used single mean imputation to fill in all missing baseline covariate values (< 5% for all variables, except for illicit drug use which was 9%).
Participants entering CNICS care with a prior HIV diagnosis and treatment history may differ in their depressive symptom trajectories from patients receiving a new HIV diagnosis and starting treatment for the first time. Unfortunately, information on HIV care prior to entering CNICS is not available in our data. To try to approximate which participants may have been new to HIV care, we indexed participants according to whether they had recently entered CNICS care (yes/no) and whether they had recently entered CNICS care and additionally had evidence of prior recent care (yes/no). We categorized participants as recently entering CNICS care if their baseline PRO assessment was completed ≤ 6 months after their initial CNICS visit. Participants with a baseline PRO > 6 months after their initial CNICS visit were categorized as not recently entering CNICS care. Participants who had recently entered CNICS care and had a detectable viral load within 28 days of CNICS entry were categorized as having no evidence of prior recent care. Participants with an undetectable or no recorded viral load within 28 days of CNICS entry or who had not recently entered CNICS care were considered to have evidence of prior recent care.
Statistical Analysis
The goals of this study were to (1) describe trajectories of depressive symptoms separately among HIV-infected men and women currently in HIV care, and (2) explore baseline characteristics associated with membership in a particular trajectory group for HIV-infected men and women. Since depressive symptoms are more common among HIV-infected women [42] and their depressive symptom trajectories may differ from those of men, we stratified all analyses by gender. We used group-based latent trajectory models, which identify clusters of individuals who have similar longitudinal patterns of an outcome [35, 43], to describe trajectories of depressive symptoms over time [35, 44]. We used the censored normal specification of the group-based trajectory model to predict the mean depressive symptoms score in each trajectory group over time, accounting for clustering at the minimum (0) and maximum [27] PHQ-9 values [35, 43, 44]. We specified a random intercept to account for within-participant correlation in depressive symptom scores over time. All statistical analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC).
The selection of a best-fitting trajectory model within each gender involved two steps. First, we selected the number of trajectory groups. A priori, we decided to explore a maximum of five trajectory groups to ensure clinical utility and interpretability. All trajectory groups were modeled using cubic polynomial terms during this step, and the Bayesian Information Criterion (BIC) was used to select the model with the best fit [35]. Second, after we had selected the number of trajectory groups, the optimal functional form (constant vs. linear vs. quadratic vs. cubic) for each trajectory group was selected based on model fit using BIC and graphical inspection of the data. In this second step, we included parameter estimates from step 1 as start values for all model parameters to improve maximum likelihood estimation [35, 43]. While the goal of our analysis was primarily descriptive and exploratory, we assessed the adequacy of each group-based trajectory model by (1) examining whether the estimated probability of group membership corresponded to the proportion of participants assigned to each group based on the model-estimated posterior probability of group membership and (2) assessing if the median of the posterior probabilities of group membership was ≥ 0.70 for each group [35].
We used a second two-stage model building process to identify baseline predictors of trajectory group membership [35]. First, we identified important predictors of trajectory group membership using backwards elimination, from a multivariable multinomial logistic regression model in which the outcome was trajectory group (defined for each participant as the group with the maximum posterior probability of group membership in the best-fitting trajectory model described above), and all candidate predictors included as explanatory variables. Predictor variables with the largest Type 3 Analysis of Effects p-values were removed first until all covariates had at least one category with a p value ≤ 0.10 [35]. Next, indicators for covariates identified in step 1 were included in a multivariable group-based trajectory model to account for probabilities of group membership and covariance between parameter estimates, in order to ensure correct standard errors and 95% confidence interval coverage. Due to limited sample size, we collapsed some three-level variables (drug use and panic disorder) into binary variables (any panic symptoms versus no symptoms and current or past drug use versus no use). For all models including baseline predictors, the group with “low” depressive symptoms (the largest trajectory group) was the referent.
We additionally conducted two descriptive analyses and one secondary analysis. First, in order to describe characteristics of each trajectory group, we assigned each participant to the trajectory group for which he or she had the highest predicted posterior probability of group membership (e.g. most likely trajectory group) from the best fitting group-based trajectory model and examined the distribution of baseline characteristics across groups [35]. Second, in order to understand how depressive symptom scores may have changed over time due to antidepressant treatment, we descriptively examined the distribution of depressive symptom scores and the proportion of participants with an antidepressant prescription over time, stratified by most likely trajectory group and gender. In a secondary analysis, we compared depressive symptom trajectories among the entire study population and those recently entering CNICS care, stratified by gender. This secondary analysis was designed to determine whether different trajectory groups emerge when trajectory measurement starts near the time of entry into CNICS care, as compared to the more variable time origins with respect to care entry in the main analysis.
Results
Baseline Characteristics
Overall, 292 women (16%) and 1493 men (84%) were included in our analysis (Table 1). The majority of women were Black, non-Hispanic (64%) and reported contracting HIV through heterosexual contact (86%). Men were predominately white, non-Hispanic (54%) and reported contracting HIV though male-to-male sexual contact (75%). Over a third of participants (35% of women and 36% of men) were new to CNICS care and approximately one fifth of both women (19%) and men (23%) overall had recently entered CNICS care with no evidence of prior recent care. Approximately 40% of all participants had a detectable viral load within 60 days of their first PRO measure.
Table 1.
Sociodemographic, mental health and HIV clinical characteristics at first patient reported outcome (PRO) measure for 1785 HIV-infected men and women in CNICS, 2005–2014
| Characteristic | Men | Women |
|---|---|---|
| N = 1493(83.6) | N = 292 (16.4) | |
| N (%) or Median (IQR) | N (%) or Median (IQR) | |
| Site | ||
| Fenway | 70 (4.7) | 3 (1.0) |
| UAB | 756 (50.6) | 203 (69.5) |
| UNC | 5 (0.3) | 3 (1.0) |
| UCSD | 381 (25.5) | 50 (17.1) |
| UCSF | 130 (8.7) | 14 (4.8) |
| UW | 151 (10.1) | 19 (6.5) |
| Year of first PRO | 2011 (2009, 2012) | 2010 (2009, 2012) |
| Recently entered CNICS Carea | ||
| No | 949 (63.6) | 191 (65.4) |
| Yes | 544 (36.4) | 101 (34.6) |
| Recently entered CNICS care with no evidence of prior recent careb | ||
| No | 1155 (77.4) | 236 (80.8) |
| Yes | 338 (22.6) | 56 (19.2) |
| Time from entry into CNICS to first PRO, days | 463 (82, 2,214) | 659 (100, 2,770) |
| Age | 44 (36, 51) | 46 (39, 52) |
| Race/ethnicity | ||
| White, non-Hispanic | 809 (54.2) | 74 (25.3) |
| Black, non-Hispanic | 440 (29.5) | 185 (63.6) |
| Hispanic | 203 (13.6) | 26 (8.9) |
| Other | 41 (2.8) | 7 (2.4) |
| HIV risk group | ||
| IDU | 192 (12.9) | 30 (10.3) |
| MSM | 1112 (74.5) | 7 (2.4)e |
| Heterosexual | 172 (11.5) | 251 (86.0) |
| Other | 17 (1.1) | 4 (1.4) |
| Depression status | ||
| Not depression (PHQ-9 < 10) | 1106 (74.1) | 207 (70.9) |
| Depressed (PHQ-9 ≥ 10) | 387 (25.9) | 85 (29.1) |
| Panic disorder | ||
| No symptoms | 1086 (72.7) | 216 (74.0) |
| Some symptoms | 241 (16.1) | 36 (12.3) |
| Panic disorder | 166 (11.1) | 40 (13.7) |
| Antidepressant use | ||
| No antidepressant prescription | 1093 (73.2) | 190 (65.1) |
| Antidepressant prescription | 400 (26.8) | 102 (34.9) |
| Drug use | ||
| No use | 726 (48.6) | 181 (62.0) |
| Current use | 217 (15.4) | 29 (9.9) |
| Past use | 550 (36.8) | 82 (28.1) |
| Alcohol usec | ||
| No high risk alcohol use | 1298 (86.9) | 259 (88.7) |
| High risk alcohol use | 195 (13.1) | 33 (11.3) |
| Previous mental health diagnosis | ||
| No | 750 (50.2) | 122 (41.8) |
| Yes | 743 (49.8) | 170 (58.2) |
| Previous medical diagnosis | ||
| No | 1077 (72.1) | 192 (65.8) |
| Yes | 416 (27.9) | 100 (34.2) |
| ART use and adherenced | ||
| Adherent, on ART | 1021 (68.4) | 187 (64.0) |
| Not adherent, on ART | 140 (9.4) | 37 (12.7) |
| Off ART | 332 (22.2) | 68 (23.3) |
| CD4 count, cells/mmc | 462 (291, 632) | 487 (314, 683) |
| Viral load suppression (< 50 copies/mL) | ||
| Undetectable viral load | 851 (57.0) | 175 (59.9) |
| Detectable viral load | 642 (43.0) | 117 (40.1) |
PRO patient-reported outcomes, MSM: men who have sex with men, IDU intravenous drug use
Defined as participants who had their baseline PRO measure within 6 months of their initial CNICS visit
Defined as participants who had their baseline PRO measure within 6 months of their initial CNICS visit and had a detectable viral load within 28 days of entering CNICS care
Defined as Alcohol Use Disorders Identification Test (AUDIT) score > 4 for males and > 3 for females
Adherence defined as no missed medication doses in the last week
A small proportion of persons identifying as ’female’ at entry into CNICS care endorsed MSM as their primary risk factor for HIV infection. Due to the small number, this group was combined with the “Other” category in statistical analyses
Mental health issues and substance use at baseline were common in our cohort. Overall, 35% of women and 27% of men had an antidepressant prescription, 29% of women and 26% of men had moderate to more severe depressive symptoms (PHQ-9 ≥ 10), and 58% of women and 50% of men had a previous mental health diagnosis at their first PRO measure. Drug use was more common among men: 37% of men reported past drug use and 15% reported current drug use, compared to 28% and 10% of women, respectively. High-risk alcohol use was reported by 11% of women and 13% of men (Table 1).
Participants included in our analysis were largely similar to all participants in CNICS who had their first PRO measure during the study period but did not meet full inclusion criteria, and to all participants entering CNICS during the study period (who may not necessarily have had a PRO measure). However, antidepressant use and previous mental health diagnoses were less common among all participants entering CNICS care during the study period, than among participants included study population and participants with a PRO measure who did not meet inclusion criteria (Table S1).
Description of Trajectory Groups
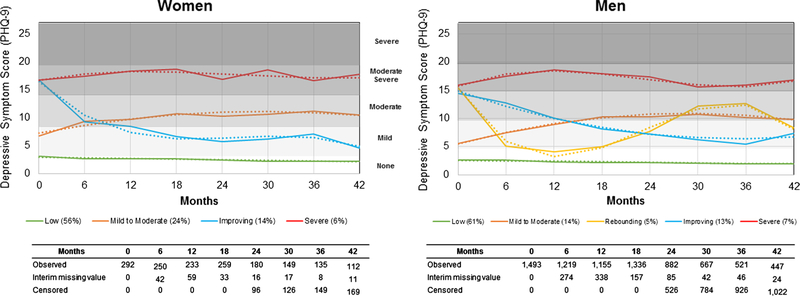
We identified four trajectory groups that were common to both men and women, with a fifth group emerging among men only (Fig. 1). We labeled the four groups identified in both men and women as: “low” depressive symptoms (exhibited by 56% of women and 61% of men), “mild to moderate” (24% of women and 14% of men), “improving” (14% of women and 13% of men) and “severe” (6% of women and 7% of men). In men, 5% followed a fifth pattern, which we termed “rebounding”.” The distribution of depressive symptoms scores within comparable trajectory groups was similar across men and women over time (Fig. 2). The proportion of participants with an interim missing depressive symptom measure was similar across trajectory groups for both men and women. For both men and women, the estimated probability of group membership and the proportion of participants assigned to each trajectory group based on the model’s estimated posterior probability were reasonably close and the median posterior probability of group membership were ≥ 0.70 for all groups, suggesting both models adequately captured trajectories of depressive symptoms (Tables S2, S3).
Fig. 1.
Depressive symptom trajectories for 292 HIV-infected women and 1493 HIV-infected men in care in CNICS between 2005 and 2014. Depressive symptoms were measured using the Patient Health Questionnaire-9 (PHQ-9). Solid lines indicate observed mean depressive symptom scores and dotted lines indicated predicted mean depressive symptom score in each trajectory group, as estimated from a group-based trajectory model using a censored normal specification and random intercept. For women, the “low” trajectory was modeled using a linear term, the “mild to moderate” trajectory using a quadratic term, and the “improving” and “severe” trajectories were modeled using a cubic term. For men, the “low” trajectory group was modeled using a linear term, the “mild to moderate” trajectory using a quadratic term, the “rebounding” trajectory using a cubic term, the “improving” trajectory using a quadratic term, and the “severe” trajectory using a cubic term
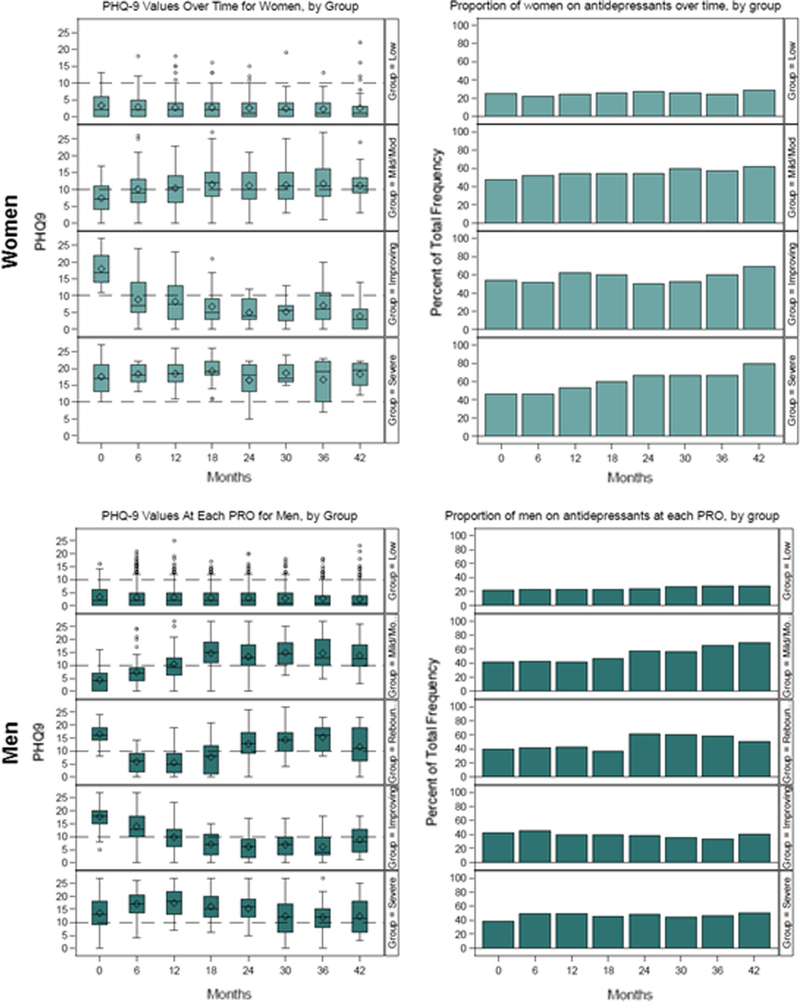
Fig. 2.
Distribution of Patient Health Questionne-9 (PHQ-9) depressive symptoms scores and proportion receiving antidepressant treatment prescription over time, stratified by gender and assigned trajectory group (based on each participant’s highest predicted posterior group-membership probability). Box and whisker plots of depressive symptoms scores indicate median and interquartile range values in the box, minimum and maximum values in the whiskers, and outliers in the circles
For both women and men, median PHQ-9 values in the low trajectory group were consistent with very mild to no depressive symptoms over time (Fig. 1). Median PHQ-9 values in the mild to moderate trajectory started in the mild range and increased to moderate depressive symptoms over time, with slightly higher scores among women across time. Men and women in the improving trajectory group had median PHQ-9 values consistent with moderate or moderate severe depressive symptoms at the start of follow-up, which improved to mild symptoms over time. Men in the rebounding trajectory group also had moderate severe depressive symptoms at baseline, which improved but later returned to moderate levels over follow-up. Finally, median PHQ-9 values for men and women in the severe trajectory group were consistent with moderate severe depressive symptoms throughout the follow-up period. Approximately 20–25% of participants experienced at least moderate depressive symptoms throughout most of the follow-up period. A secondary analysis restricted to participants recently entering CNICS care, trajectory groups were similar in shape and distribution to the primary analysis.
Antidepressant Use Over Time
Antidepressant prescription patterns varied across trajectory groups, and not always in accordance with depressive symptom severity (Fig. 2). In the mild to moderate trajectory groups, antidepressant prescription increased slightly as depressive symptoms increased for men and women. Compared to men, antidepressant prescription was more common among women in several trajectory groups (mild to moderate, improving, and severe groups). Further, antidepressant prescription increased in the severe trajectory group over time only among women. Overall, antidepressant prescription did not change dramatically or consistently over time across trajectory groups with more severe depressive symptoms, including among participants in the improving trajectory group. For both men and women, antidepressant prescription remained well below 60% for much of the follow-up period.
Baseline Predictors of Trajectory Group Membership
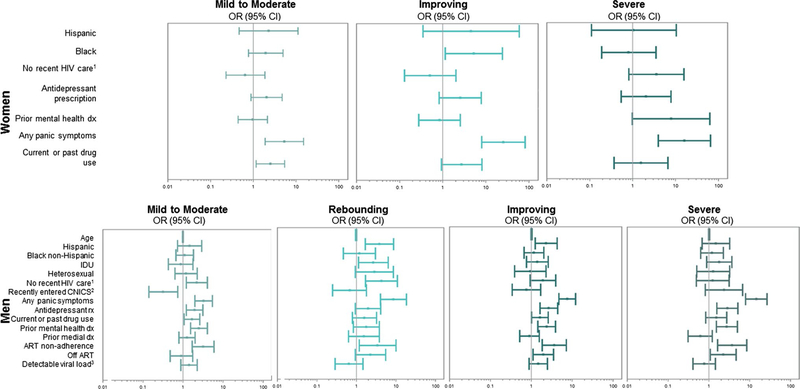
Multivariable associations between baseline covariates and trajectory group membership for men and women are reported in Fig. 3. Additional descriptive profiles of trajectory group membership for both men and women are available in Tables S2 and S3. Among women, compared to being in the low trajectory group, those in the mild to moderate trajectory group were more likely to have any panic disorder symptoms (OR 5.36, 95% CI 1.91, 15.00), or report current or past drug use (OR 2.53, 95% CI 1.17, 5.44). Those in the improving trajectory group were more likely to be black, non-Hispanic (OR 5.26, 95% CI 1.14, 24.24) or have any panic disorder symptoms (OR 25.49, 95% CI 8.01, 81.12). Compared to those in the low group, those in the severe trajectory group were more likely to have a previous mental health diagnosis (OR 7.91, 95% CI 0.99, 62.82) or have any panic disorder symptoms (OR 16.07, 95% CI 3.96, 65.27).
Fig. 3.
Multivariable odds ratios and 95% confidence intervals for the relationship between baseline covariates and membership in each depressive symptoms trajectory group, compared to the low depressive symptom trajectory group, for HIV-infected women (4 groups) and men (5 groups). Each covariate represents a comparison of that factor to all other categories of that variable based on a trajectory model that accounts for group membership probabilities and covariance across parameter values, to ensure correct standard errors and 95% confidence interval coverage. 1Defined as participants who had their baseline PRO measure ≤ 6 months after their initial CNICS visit and had a detectable viral load within 28 days of entering CNICS care. 2Defined as participants who had their baseline PRO measure ≤ 6 months after their initial CNICS visit. 3Defined as < 50 copies/mL; rx = prescription, dx = diagnosis
Among men, compared to those in the low trajectory group, those in the mild to moderate group were less likely to have recently entered CNICS care with no evidence of prior recent care (OR 0.32, 95% CI 0.14, 0.74), and were more likely to have recently entered CNICS care (OR 2.22, 95% CI 1.22, 4.05), have any panic disorder symptoms (OR 3.27, 95% CI 1.97, 5.43), have an antidepressant prescription (OR 1.95, 95% CI 1.21, 3.14), report current or past drug use (OR 1.68, 95% CI 1.07, 2.64), have a previous mental health diagnosis (OR 2.50, 95% CI 1.55, 4.05) and be nonadherent to ART (OR 3.18, 95% CI 1.70, 5.98) at baseline. Those in the rebounding trajectory group were more likely to be Hispanic (OR 3.82, 1.67, 8.74), report contracting HIV through IDU (OR 2.68, 1.13, 6.35), have recently entered CNICS care (OR 4.32, 95% CI 1.70, 10.92), have any panic disorder symptoms (OR 8.65, 95% CI 4.07, 18.38), and to be non-adherent to ART (OR 3.43, 95% CI 1.18, 9.97). Those in the improving trajectory group were more likely to be Hispanic (OR 2.31, 95% CI 1.24, 4.32), have any panic disorder symptoms (OR 7.57, 95% CI 4.73, 12.13), have an antidepressant prescription (OR 2.67, 95% CI 1.63, 4.39), report current or past drug use (OR 1.63, 95% CI 1.02, 2.59), have a previous mental health diagnosis (OR 2.39, 95% CI 1.45, 3.93), be non-adherent to ART (OR 3.66, 95% CI 1.86, 7.20), and to be off ART (OR 1.97, 95% CI 1.10, 3.52). Compared to those in the low trajectory group, those in the severe trajectory group were more likely to have any panic disorder symptoms (OR 14.62, 95% CI 7.98, 26.76), have an antidepressant prescription (OR 2.86, 95% CI 1.58, 5.15), have a previous mental health diagnosis (OR 2.75, 95% CI 1.52, 4.98), be non-adherent to ART (OR 3.72, 95% CI 1.63, 8.47), and to be off ART (OR 2.26, 95% CI 1.09, 4.69).
Discussion
In our population of HIV-infected adults in routine HIV care, we identified four depressive symptom trajectory groups for HIV-infected women and five depressive symptom trajectories for HIV-infected men over a median 30 months of follow-up. For both men and women, depressive symptom trajectories ranged from almost no depressive symptoms to severe depressive symptoms. With the exception of the low and severe depressive symptom trajectory groups, depressive symptom severity changed considerably over the follow-up period. Over 2–4 years of follow-up, nearly a quarter of both HIV-infected men and women experienced moderate to more severe depressive symptoms. Changes in depressive symptom severity did not appear to be driven primarily by changes in antidepressant prescription, with only slight increases in antidepressant prescription being noted in the mild to moderate and severe (women only) trajectory groups. Overall, antidepressant prescription remained below 60% for much of the follow-up period, despite the high level of depressive symptoms in several trajectory groups.
Patterns of depressive symptom trajectories were relatively similar between HIV-infected men and women, with four similar trajectories emerging (low, mild to moderate, improving, and severe) and comparable proportions of the population in each trajectory. A fifth, rebounding, trajectory group was identified among HIV-infected men, but included just 5% of men. The distinct trajectories we identified suggest that HIV-infected adults’ experiences of depressive symptoms over time vary considerably, but may be comparable across genders. While some participants had mild to moderate or improving depressive symptoms, which may respond to antidepressant or counseling treatment [45], others experienced severe, chronic symptoms that may be part of a more complex mental health picture requiring additional resources and treatment [46–48]. For over half of the participants in our study, depressive symptoms were consistently low to absent throughout the follow-up period, suggesting that less frequent depressive symptom screening may be an option for participants with sustained low depressive symptoms scores.
In our study, comorbid mental health conditions were associated with membership in trajectory groups with more severe depressive symptoms. In multivariable analyses for both men and women, panic disorder symptoms and having a previous mental health diagnosis were associated with membership in more severe or dynamic depressive symptom trajectory groups. Being on an antidepressant at baseline was also associated with membership in more severe depressive symptom trajectory groups for men; effect estimates were elevated but imprecise among women. Having a previous mental health diagnosis was most strongly associated with membership in the severe trajectory group for both men and women. However, no clear pattern of factors emerged to distinguish participants in the improving, rebounding (men only), and severe trajectory groups from one another. Depression has been reported as comorbid with other mental health condition in both HIV-infected and uninfected adults [49, 50]. Our study further suggests that participants with comorbid mental health conditions may be likely to experience more severe and persistent depressive symptoms.
We also observed associations for several clinical and socio-demographic factors with trajectory group membership. Across both men and women, there was some limited evidence that substance use was associated with membership in more severe depressive symptom trajectory groups and that racial minorities were more likely to be in improving or rebounding trajectory groups. Among men, baseline reports of poor ART adherence or being off ART were also associated with membership in more severe depressive symptom trajectory groups. Since our population includes HIV-infected adults currently in care, these findings may reflect adherence problems or delayed ART use resulting from depressive symptoms. Among men, participants who were new to CNICS were also more likely to be in the mild to moderate or rebounding trajectory groups, which may indicate increased detection of depressive symptoms among participants recently entering care in CNICS, where depression screening is routine.
Our analysis also confirmed the gap in antidepressant treatment that has been described among HIV-infected adults with depression [51] Just over half of participants in the mild to moderate trajectory groups were on antidepressant medications throughout follow-up. In addition, women were more likely to be treated than men in several trajectory groups [52]. Compared to men, antidepressant prescription was considerably higher among women in the improving and severe trajectory groups. These findings raise the question of whether more participants, and in particular more men, would have experienced improving or remitting depressive symptoms if they had been treated with antidepressants. Interestingly, antidepressant prescription increased slightly over time for both men and women in the mild to moderate trajectory group, suggesting a possible clinical response in antidepressant prescription to increasing depressive symptoms.
There are several limitations to our analysis. First, small sample size, particularly for women, may limit the generalizability of our findings. However, participants in our analysis were fairly similar to participants in the larger CNICs cohort (Table S1). Limited sample size also led to imprecise estimates for many predictors of trajectory group membership and reported estimates should be interpreted with caution. In addition, the limited number of women in our analysis (and more generally, in CNICS) precluded identifying a greater range of predictors of trajectory group membership in women, and may have limited our ability to detect the existence of a fifth trajectory group. Second, while we identified several predictors of trajectory group membership, it was difficult to distinguish between participants who were likely to improve, rebound, or experience chronic, severe depression. More detailed data on mental health comorbidities or access to counseling services may help to further distinguish these groups. We note the use of mean imputation of missing baseline data as a limitation. Finally, information on how counseling or other behavioral therapy may influence depressive symptom trajectories over time was not available in our data.
Our study focused on identifying depressive symptom trajectories in a real-world population currently in HIV care. In order to obtain internally valid estimates of depressive symptom trajectories over time, we restricted our study population to individuals with a minimum of four consecutive depressive symptom measures. However, since persons with depression may be less likely to attend HIV care visits [53], this may limit the generalizability of our findings. Further, our analysis included all HIV-infected individuals in care. Depressive symptom trajectories were similar between those recently entering CNICS care and the entire study population. However, it is possible that depressive symptom trajectories may be more severe or variable in a population of persons newly diagnosed with HIV. Additional work is needed to understand how depressive symptom trajectories may differ among populations newly diagnosed with HIV or newly entering HIV care. Similarly, dual-trajectory analyses could provide important future insights on concomitant patterns of depressive symptoms with antidepressant use, viral load suppression, and HIV risk behaviors.
Our results have several important clinical implications. We found that not all depressive symptoms follow the same trajectory. When patients present with depressive symptoms, understanding the trajectory their depressive symptoms are likely to follow can help to guide clinical care. In particular, we found that comorbid mental health conditions are consistently associated with more severe or dynamic depressive symptom trajectories. For patients with comorbid mental health conditions, addressing depression alone is unlikely to be effective and a more comprehensive strategy addressing the full range of mental health needs may be required. In addition, in order to decrease depressive symptom severity over time, greater access to antidepressant treatment or behavioral therapy among patients with moderate or more severe depressive symptoms is urgently needed.
Conclusions
Not all depressive symptoms are the same. Over a median 30 months of follow-up, HIV-infected adults who were in HIV care followed markedly different—and in many cases, dynamic—depressive symptom trajectories ranging from few or almost no depressive symptoms to chronic, severe depressive symptoms. For both HIV-infected men and women, a sizeable proportion of the population experienced some degree of depressive symptoms throughout the follow-up period, highlighting the pressing need for evidence-based antidepressant treatment or behavioral therapy in this population. Our study focused on identifying depressive symptom trajectories in a real-world population currently in HIV care. Further research is needed to understand how depressive symptom trajectories may differ among populations newly diagnosed with HIV or newly entering HIV care; to distinguish those whose depressive symptoms are likely to improve, rebound, or be chronic and severe; and to understand what additional factors contribute to chronic severe depressive symptoms. Such information will pave the way for more targeted health interventions to address patients’ unique mental needs, and ultimately reduce depressive symptoms among HIV-infected adults.
Supplementary Material
Acknowledgements
The authors wish to thank the University of North Carolina at Chapel Hill Center for AIDS Research and National Institutes of Health [Grant Numbers R01MH100970, R24AI067039, P30 AI50410, L30MH110572, K99MH112413, and UL1TR001111], which supported this work. Dr. Bengtson was supported by a career development award from the National Institute of Mental Health [Grant Number K99MH112413].
Footnotes
Conflict of interest The authors declare no conflicts of interest.
Compliance with Ethical Standards
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board at each CNICS site and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent to participate in the CNICS cohort was obtained from all individual participants included in the study.
Informed Consent Informed consent to participate in the CNICS cohort was obtained from all individual participants included in the study.
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s10461-018-2109-2) contains supplementary material, which is available to authorized users.
References
- 1.Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58(8):721–8. [DOI] [PubMed] [Google Scholar]
- 2.Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. Am J Psychiatry. 2001;158(5):725–30. [DOI] [PubMed] [Google Scholar]
- 3.Bengtson AM, Pence BW, O’Donnell J, Thielman N, Heine A, Zinski A, et al. Improvements in depression and changes in quality of life among HIV-infected adults. AIDS Care. 2015;27(1):47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zimpel RR, Fleck MP. Depression as a major impact on the quality of life of HIV-positive Brazilians. Psychol Health Med. 2014;19(1):47–58. [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: a review and meta-analysis. J Acquir Immune Defic Syndr. 2011;58(2):181–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horberg MA, Silverberg MJ, Hurley LB, Towner WJ, Klein DB, Bersoff-Matcha S, et al. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected patients. J Acquir Immune Defic Syndr. 2008;47(3):384–90. [DOI] [PubMed] [Google Scholar]
- 7.Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285(11):1466–74. [DOI] [PubMed] [Google Scholar]
- 8.Ironson G, O’Cleirigh C, Fletcher MA, Laurenceau JP, Balbin E, Klimas N, et al. Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosom Med. 2005;67(6):1013–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leserman J, Jackson ED, Petitto JM, Golden RN, Silva SG, Perkins DO, et al. Progression to AIDS: the effects of stress, depressive symptoms, and social support. Psychosom Med. 1999;61(3):397–406. [DOI] [PubMed] [Google Scholar]
- 10.Murphy K, Hoover DR, Shi Q, Cohen M, Gandhi M, Golub ET, et al. Association of self-reported race with AIDS death in continuous HAART users in a cohort of HIV-infected women in the United States. Aids. 2013;27(15):2413–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.French AL, Gawel SH, Hershow R, Benning L, Hessol NA, Levine AM, et al. Trends in mortality and causes of death among women with HIV in the United States: a 10-year study. J Acquir Immune Defic Syndr. 2009;51(4):399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Villes V, Spire B, Lewden C, Perronne C, Besnier JM, Garre M, et al. The effect of depressive symptoms at ART initiation on HIV clinical progression and mortality: implications in clinical practice. Antivir Ther. 2007;12(7):1067–74. [PubMed] [Google Scholar]
- 13.Antelman G, Kaaya S, Wei R, Mbwambo J, Msamanga GI, Fawzi WW, et al. Depressive symptoms increase risk of HIV disease progression and mortality among women in Tanzania. J Acquir Immune Defic Syndr. 2007;44(4):470–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Todd JV, Cole SR, Pence BW, Lesko CR, Bacchetti P, Cohen MH, et al. Effects of antiretroviral therapy and depressive symptoms on all-cause mortality among HIV-infected women. Am J Epidemiol. 2017;185(10):869–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Cleirigh C, Newcomb ME, Mayer KH, Skeer M, Traeger L, Safren SA. Moderate levels of depression predict sexual transmission risk in HIV-infected MSM: a longitudinal analysis of data from six sites involved in a “prevention for positives” study. AIDS Behav. 2013;17(5):1764–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asch SM, Kilbourne AM, Gifford AL, Burnam MA, Turner B, Shapiro MF, et al. Underdiagnosis of depression in HIV: who are we missing? J Gen Intern Med. 2003;18(6):450–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Cleirigh C, Magidson JF, Skeer MR, Mayer KH, Safren SA. Prevalence of psychiatric and substance abuse symptomatology among HIV-infected gay and bisexual men in HIV primary Care. Psychosomatics. 2015;56(5):470–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pence BW, Gaynes BN, Adams JL, Thielman NM, Heine AD, Mugavero MJ, et al. The effect of antidepressant treatment on HIV and depression outcomes: the SLAM DUNC randomized trial. AIDS. 2015;29(15):1975–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Safren SA, O’Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: a randomized controlled trial. J Consult Clin Psychol. 2012;80(3):404–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spies G, Asmal L, Seedat S. Cognitive-behavioural interventions for mood and anxiety disorders in HIV: a systematic review. J Affect Disord. 2013;150(2):171–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsai AC, Karasic DH, Hammer GP, Charlebois ED, Ragland K, Moss AR, et al. Directly observed antidepressant medication treatment and HIV outcomes among homeless and marginally housed HIV-positive adults: a randomized controlled trial. Am J Public Health. 2013;103(2):308–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watson LC, Amick HR, Gaynes BN, Brownley KA, Thaker S, Viswanathan M, et al. Practice-based interventions addressing concomitant depression and chronic medical conditions in the primary care setting: a systematic review and meta-analysis. J Prim Care Community Health. 2013;4(4):294–306. [DOI] [PubMed] [Google Scholar]
- 23.Kim MH, Mazenga AC, Devandra A, Ahmed S, Kazembe PN, Yu X, et al. Prevalence of depression and validation of the Beck Depression Inventory-II and the Children’s Depression InventoryShort amongst HIV-positive adolescents in Malawi. J Int AIDS Soc. 2014;17:18965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nyirenda M, Chatterji S, Rochat T, Mutevedzi P, Newell ML. Prevalence and correlates of depression among HIV-infected and -affected older people in rural South Africa. J Affect Disord. 2013;151(1):31–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rochat TJ, Tomlinson M, Barnighausen T, Newell ML, Stein A. The prevalence and clinical presentation of antenatal depression in rural South Africa. J Affect Disord. 2011;135(1–3):362–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Su X, Lau JT, Mak WW, Choi KC, Chen L, Song J, et al. Prevalence and associated factors of depression among people living with HIV in two cities in China. J Affect Disord. 2013;149(1–3):108–15. [DOI] [PubMed] [Google Scholar]
- 27.Tesfaw G, Ayano G, Awoke T, Assefa D, Birhanu Z, Miheretie G, et al. Prevalence and correlates of depression and anxiety among patients with HIV on-follow up at Alert Hospital, Addis Ababa, Ethiopia. BMC Psychiatry. 2016;16(1):368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carta MG, Angst J, Moro MF, Mura G, Hardoy MC, Balestrieri C, et al. Association of chronic hepatitis C with recurrent brief depression. J Affect Disord. 2012;141(2–3):361–6. [DOI] [PubMed] [Google Scholar]
- 29.Choi SK, Boyle E, Cairney J, Collins EJ, Gardner S, Bacon J, et al. Prevalence, recurrence, and incidence of current depressive symptoms among people living with HIV in Ontario, Canada: results from the Ontario HIV Treatment Network Cohort Study. PLoS ONE. 2016;11(11):e0165816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johnson JG, Rabkin JG, Lipsitz JD, Williams JB, Remien RH. Recurrent major depressive disorder among human immunodeficiency virus (HIV)-positive and HIV-negative intravenous drug users: findings of a 3-year longitudinal study. Compr Psychiatry. 1999;40(1):31–4. [DOI] [PubMed] [Google Scholar]
- 31.Taniguchi T, Shacham E, Onen NF, Grubb JR, Overton ET. Depression severity is associated with increased risk behaviors and decreased CD4 cell counts. AIDS Care. 2014;26(8):1004–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kitahata MM, Rodriguez B, Haubrich R, Boswell S, Mathews WC, Lederman MM, et al. Cohort profile: the Centers for AIDS Research Network of Integrated Clinical Systems. Int J Epidemiol. 2008;37(5):948–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crane HM, Lober W, Webster E, Harrington RD, Crane PK, Davis TE, et al. Routine collection of patient-reported outcomes in an HIV clinic setting: the first 100 patients. Curr HIV Res. 2007;5(1):109–18. [DOI] [PubMed] [Google Scholar]
- 34.Fredericksen R, Crane PK, Tufano J, Ralston J, Schmidt S, Brown T, et al. Integrating a web-based, patient-administered assessment into primary care for HIV-infected adults. J AIDS HIV Res. 2012;4(2):47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nagin DS. Group-based modeling of development. Cambridge: Harvard University Press; 2005. [Google Scholar]
- 36.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG). AIDS Care. 2000;12(3):255–66. [DOI] [PubMed] [Google Scholar]
- 38.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–44. [DOI] [PubMed] [Google Scholar]
- 39.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT, The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Care. Geneva, Switzerland: World Health Organization, Dependence DoMHaS; 2001. [Google Scholar]
- 40.WHO Assist Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–94. [DOI] [PubMed] [Google Scholar]
- 41.Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, et al. Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction. 2008;103(6):1039–47. [DOI] [PubMed] [Google Scholar]
- 42.Bengtson AM, Pence BW, Crane HM, Christopoulos K, Fredericksen RJ, Gaynes BN, et al. Disparities in Depressive symptoms and antidepressant treatment by gender and race/ethnicity among people living with HIV in the United States. PLoS ONE. 2016;11(8):e0160738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29(3):374–93 [Google Scholar]
- 44.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38. [DOI] [PubMed] [Google Scholar]
- 45.Madhoo M, Levine SZ. Initial severity effects on residual symptoms in response and remission: a STAR*D Study during and after failed citalopram treatment. J Clin Psychopharmacol. 2015;35(4):450–3. [DOI] [PubMed] [Google Scholar]
- 46.Barroso J, Bengtson AM, Gaynes BN, McGuinness T, Quinlivan EB, Ogle M, et al. Improvements in depression and changes in fatigue: results from the SLAM DUNC depression treatment trial. AIDS Behav. 2016;20(2):235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Illangasekare SL, Burke JG, McDonnell KA, Gielen AC. The impact of intimate partner violence, substance use, and HIV on depressive symptoms among abused low-income urban women. J Interpers Violence. 2013;28(14):2831–48. [DOI] [PubMed] [Google Scholar]
- 48.Uebelacker LA, Weisberg RB, Herman DS, Bailey GL, PinkstonCamp MM, Stein MD. Chronic pain in HIV-infected patients: relationship to depression, substance use, and mental health and pain treatment. Pain Med. 2015;16(10):1870–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gaynes BN, O’Donnell J, Nelson E, Heine A, Zinski A, Edwards M, et al. Psychiatric comorbidity in depressed HIV-infected individuals: common and clinically consequential. Gen Hosp Psychiatry. 2015;37(4):277–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Simon NM. Generalized anxiety disorder and psychiatric comorbidities such as depression, bipolar disorder, and substance abuse. J Clin Psychiatry. 2009;70(Suppl 2):10–4. [DOI] [PubMed] [Google Scholar]
- 51.Pence BW, O’Donnell JK, Gaynes BN. The depression treatment cascade in primary care: a public health perspective. Curr Psychiatry Rep. 2012;14(4):328–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bengtson AM, Pence PW, Crane HM, Christopoulos K, Fredericksen R, Gaynes BN, et al. Disparities in depression diagnosis and treatment by gender and race/ethnicity among HIV-infected adults in the United States. PLoS One. 2016;11(8):e160738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Traeger L, O’Cleirigh C, Skeer MR, Mayer KH, Safren SA. Risk factors for missed HIV primary care visits among men who have sex with men. J Behav Med. 2012;35(5):548–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.