Abstract
Fibroblast growth factor 15 (FGF15) was previously identified to be highly expressed in the ileum and functions as an endocrine factor to regulate bile acid synthesis in the liver. FGF15 targets its receptor fibroblast growth factor receptor 4 in the liver and serves important roles in energy metabolism, including bile acid homeostasis, glucose metabolism and protein synthesis. The expression of FGF15 is known to be regulated by the transcription factor farnesoid X receptor (FXR). In the present study, reverse transcription-quantitative polymerase chain reaction was used for measuring Fgf15 expression from the animal and tissue culture experiments, and it was identified that dexamethasone, a drug widely used in anti-inflammation therapy, and a classical inducer of glucocorticoid receptor (GR)- and pregnane X receptor (PXR)-target genes, may downregulate Fgf15 expression in the ileum. GR was identified to be highly expressed in the ileum by western blot analysis. Furthermore, it was demonstrated that the downregulation of Fgf15 by dexamethasone is due to the repression of ileal FXR activity via GR; however, not PXR, in the ileum. The present results provide insight for a better understanding of the adverse effects associated with dexamethasone therapy.
Keywords: Dex, Fgf15 expression, ileum
Introduction
Fibroblast growth factor 15 (FGF15) was initially identified in the developing nervous system of a mouse (1). Subsequently, the human ortholog, fibroblast growth factor 19 (FGF19), was identified to be expressed in the fetal brain (2). Previous studies suggested that FGF15 functioned in cell division and patterning within specific regions of the embryonic brain, spinal cord and sensory organs (1,2). Other previous studies demonstrated that FGF15/19 exhibited high expression in the small intestine of adult mice and humans, where they function as an enterohepatic signal to regulate hepatic homeostasis (3,4). Further studies demonstrated that circulating FGF15/19 as metabolic hormones functioned through fibroblast growth factor receptor 4 (FGFR4) in the liver and regulated numerous metabolism pathways, including hepatic bile acid (BA), carbohydrate and protein metabolism (3–7).
FGF15 expression is regulated by farnesoid X receptor (FXR), a BA receptor (3). Retinoid X receptors (RXRs) are hypothesized to form a heterodimer with FXR and serve a role in the transcriptional regulation of Fgf15 (3). Vitamin D may additionally activate the transcription of Fgf15 through vitamin D receptor (8), whereas, vitamin A upregulates Fgf15 expression through the RXR/FXR heterodimer (8). Notably, Diet1 was demonstrated to promote FGF15 production at the post-transcriptional level, and an absence of Diet1 was accompanied by significantly reduced FGF15 secretion (9). These results demonstrate the present understanding of Fgf15 regulation. Whether other transcription factors are involved in the regulation of Fgf15 expression is unclear.
Dexamethasone (Dex), a synthetic analog of glucocorticoids (GCs), is a potent agonist for the glucocorticoid receptor (GR). Due to its function of anti-inflammation, Dex has been widely used in the treatment of acute inflammatory and autoimmune diseases (10). Unfortunately, accumulating evidence demonstrated that the clinical use of GCs or Dex causes a lot of undesirable side effects (11,12). For example, GC intake may result in glucose intolerance and insulin resistance (11). Increased GCs may cause liver steatosis and hyperlipidemia (12). Treatment with GCs additionally leads to BA overproduction and gallstone disease (13). As FGF15 serves an important role in glucose metabolism, insulin resistance and BA synthesis (3,14), the effects of Dex on Fgf15 expression were hypothesized to affect the homeostasis of BA and glucose, and may lead to the adverse effects associated with treatments with GCs in the clinical setting. The present study aimed to investigate the effect of Dex on the expression of Fgf15 in the mouse ileum. It was identified that treatment with Dex significantly downregulated ileal Fgf15 expression, and this downregulation of Fgf15 expression by Dex is due to GR-mediated suppression of FXR transcriptional activity.
Materials and methods
Materials
Cholic acid (CA), pregnenolone-16-α-carbonitrile (PCN) and Dex were purchased from Sigma-Aldrich (Merck KGaA, Darmstadt, Germany). An anti-GR antibody was purchased from Epitomics (Abcam, Cambridge, UK) and an anti-GAPDH antibody was purchased from GenScript (Piscataway, NJ, USA).
Animals and treatments
All animal studies were approved by the Institutional Animal Care and Use Committee of the Wadsworth Center (State University of New York, Albany, NY, USA) or the Animal Ethics Committee of the Fujian Agriculture and Forestry University (Fuzhou, China). In total, 120 adult male C56BL/6J mice (~25 g; 2–3 months old, 3 mice per group; breeding and feeding in the laboratory) were used for all experiments. Animals were maintained at 22°C, 50% relative humidity and a 12-h light/dark cycle in a specific pathogen-free clean room with food and water ad libitum. Dex dissolved in corn oil was administered to the mice at various doses via intraperitoneal (i.p.) injection. For dose-response experiments, mice were treated with Dex at three different doses (0.8, 8 and 80 mg/kg) for 24 h. Animals were sacrificed at the indicated timepoints following treatment with Dex for tissue collection. Additionally, the weights of the mice and tissue, and tissue morphology were examined to evaluate the toxicity of treatment with Dex. PCN (25 mg/kg, dissolved in corn oil) was administered via oral gavage, and mice were sacrificed at 24 h after treatment with PCN for tissue Collection.
For the co-treatment of CA and Dex, Dex at 80 mg/kg or vehicle (corn oil) was administered by i.p. injection. Mice fasted for 2 h prior to administration of CA (200 mg/kg in PBS by oral gavage). After another 4 h, ileal epithelial cells were collected for RNA preparation.
Sample collection and western blot analysis
The small intestine was removed and flushed with ice cold PBS. The small intestine was divided into three segments designated the duodenum (proximal 5 cm), jejunum (middle 5 cm) and ileum (distal 5 cm). The three segments were cut open longitudinally and the epithelial cells were removed by gentle scraping. The collected cells were washed once in cold PBS and subsequently lysed in radioimmunoprecipitation assay buffer (Thermo Fisher Scientific, Inc., Waltham, MA, USA) containing Protease & Phosphatase Inhibitor (Thermo Fisher Scientific, Inc.) and 5 mM EDTA, and homogenized using a polytron homogenizer. The homogenates were mixed for 10 min at 4°C, and subsequently centrifuged at 14,000 g and 4°C for 15 min. The supernatant was collected and the protein concentration was determined by the bicinchoninic acid method (Pierce; Thermo Fisher Scientific, Inc.).
Proteins (50 µg) were resolved on 10% NuPAGE Bis-Tris-gels (Invitrogen; Thermo Fisher Scientific, Inc.) and subsequently transferred to nitrocellulose membranes. For immunodetection, subsequent to blocking with 5% fat-free milk at room temperature for 1 h, pre-cut membranes were incubated with monoclonal rabbit anti-GR (Epitomics; Abcam; cat. no. EPR4595; 1:4,000) and goat anti-GAPDH (GenScript; cat. no. A00191-40; 1:40,000) antibodies at 4°C overnight. Subsequent to washing, the membranes were incubated with goat anti-rabbit immunoglobulin G (IgG) heavy and light chain (H&L) horseradish peroxidase (HRP)-conjugated antibod (GenScript; cat. no. A00098; 1:8,000) or donkey anti-goat IgG H&L HRP-conjugated antibody (GenScript; cat. no. A00178; 1:8,000) according to the host species of the primary antibody at room temperature for 1 h. Pierce™ Enhanced Chemiluminescent Western Blotting Substrate (Thermo Fisher Scientific, Inc.) was used for the detection of HRP on the immunoblots. Immunoblot quantification was performed using a Bio-Rad ChemiDoc XRS+ System (Bio-Rad Laboratories, Inc., Hercules, CA, USA) with Image Lab 3.0 (Bio-Rad Laboratories, Inc.).
Ex vivo culture of ileum tissues
Immediately after harvesting the intestine, 5 cm of the terminal ileum was flushed with PBS to remove the contents and was subsequently cut into small segments (1×3 mm). The segments were cultured at 37°C for 4 h in Dulbecco's modified Eagle's medium (Thermo Fisher Scientific, Inc.) supplemented with 10% heat-inactivated fetal bovine serum (Thermo Fisher Scientific, Inc.), 100 units/ml penicillin and 100 µg/ml streptomycin. Dex (1 µM final concentration) or vehicle (ethanol), and CA (100 µg/ml) or PBS were added to the culture medium. The epithelial cells were collected at the end of 4-h culture for RNA preparation.
RNA isolation and reverse transcription-quantitative polymerase chain reaction (RT-qPCR) analysis
Total RNA was prepared from the enterocytes of individual mice, with the use of TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Inc.), as previously described (15). RNA concentration and purity were determined spectrally, and the integrity of the RNA samples was assessed by ethidium bromide staining following agarose gel electrophoresis. RT-PCR was performed using 3 µg total RNA and SYBR Green PCR Master PCR Mix (Applied Biosystems; Thermo Fisher Scientific, Inc.), as previously described (16). The comparative 2−∆∆Cq method was used for quantifying the relative mRNA expression levels (17,18). PCR primers for FXR (19), PXR (20), Fgf15 (3), small heterodimer partner (SHP) (3), glucocorticoid-induced leucine zipper (GILZ) (21), apical sodium dependent bile acid transporter (ASBT) (22), ileum bile acid binding protein (IBABP) (22) and cytochrome P450, family 3, subfamily a, polypeptide 11 Cyp3a11 (23) were as follows: FXR, 5′-CCAACCTGGGTTTCTACCC-3′ (forward) and 5′-CACACAGCTCATCCCCTTT-3′ (reverse); PXR, 5′-CAAGGCCAATGGCTACCA-3′ (forward) and 5′-CGGGTGATCTCGCAGGTT-3′ (reverse); Fgf15, 5′-GAGGACCAAAACGAACGAAATT-3′ (forward) and 5′-ACGTCCTTGATGGCAATCG-3′ (reverse); SHP, 5′-CGATCCTCTTCAACCCAGATG-3′ (forward) and 5′-AGGGCTCCAAGACTTCACACA-3′ (reverse); GILZ, 5′-CAGCAGCCACTCAAACCAGC-3′ (forward) and; 5′-ACCACATCCCCTCCAAGCAG-3′ (reverse); ASBT, 5′-TGGGTTTCTTCCTGGCTAGACT-3′ (forward) and 5′-TGTTCTGCATTCCAGTTTCCAA-3′ (reverse); IBABP, 5′-AGATCATCACAGAGGTCCAGC-3′ (forward) and 5′-GGTAGCCTTGAACTTCTTGCC-3′ (reverse); Cyp3a11, 5′-GACAAACAAGCAGGGATGG-3′ (forward) and 5′-AATGTGGGGGACAGCAAAG-3′ (reverse); and U36B4, 5′-CGTCCTCGTTGGAGTGACA-3′ (forward) and 5′-CGGTGCGTCAGGGATTG-3′ (reverse). The levels of the target mRNAs in various total RNA preparations were normalized by the level of U36B4 mRNA (8).
Statistical analysis
All experiments were repeated at least three times. Data are presented as the mean ± standard deviation. Statistical analysis was performed using Student's t-test with SPSS 11.5 software (SPSS, Inc., Chicago, IL, USA). For multiple comparisons, one-way analysis of variance followed by Fisher's Least Significant Difference test was used. P<0.05 was considered to indicate a statistically significant difference.
Results
Treatment with Dex significantly downregulates Fgf15 expression in the mouse ileum
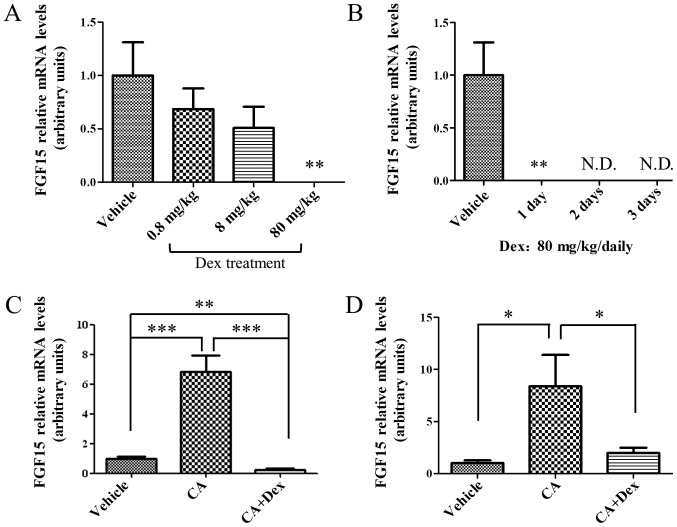
To examine the effect of treatment with Dex on ileal Fgf15 expression, the mRNA expression levels of Fgf15 were compared prior to and following treatment with Dex. Mice were treated with Dex at three different doses (0.8, 8 and 80 mg/kg) for 24 h. The ileal Fgf15 expression decreased in a dose-dependent manner following treatment with Dex (Fig. 1A). At 80 mg/kg Dex, the expression level of FGF15 mRNA was decreased to an undetectable level two days later (Fig. 1B). The downregulation of ileal Fgf15 expression by treatment with Dex was maintained when the mice were treated with Dex for 3 consecutive days (Fig. 1B). These results suggested that treatment with Dex was able to suppress ileal Fgf15 expression at the RNA level. At the same time, although the highest dosage of Dex used, 80 mg/kg, in the present study was effective, the potential cytotoxicity of Dex with this dosage for 3 days requires consideration (data not shown). The phenomenon of tissue hypertrophy was observed (data not shown), which may be due to the compensation for the cytotoxicity of treatment with Dex with high dosage for 3 days.
Figure 1.
Effect on FGF15 expression in mouse ileum. (A) Expression levels of ileal FGF15 mRNA were decreased in a dose-dependent manner by treatment with Dex for 24 h. (B) Expression of FGF15 mRNA was completely suppressed following consecutive treatment with 80 mg/kg Dex for 1–3 days. **P<0.01 vs. vehicle. (C) Dex diminished the induction of FGF15 by CA (200 mg/kg) in vivo. (D) Dex diminished the induction of FGF15 by treatment with CA (100 µg/ml) in the ileum culture ex vivo. The data were normalized to the expression levels of mouse U36B4. The data are presented as the mean ± standard deviation. n=3. *P<0.05, ***P<0.001. FGF15, fibroblast growth factor 15; Dex, dexamethasone; CA, cholic acid; N.D., not detectable.
To investigate whether this downregulation of Fgf15 expression is mediated by FXR, the critical transcriptional factor for regulating Fgf15 expression (3), the effect of treatment with Dex on the FXR transcriptional activity was examined in vivo. Mice were pre-treated with Dex or corn oil, and subsequently FXR was activated with CA. After a 4 h treatment with CA, as presented in Fig. 1C, the mRNA expression level of Fgf15 was upregulated. However, the upregulation of Fgf15 expression by treatment with CA was significantly inhibited in mice pre-treated with Dex (Fig. 1C; P<0.001), suggesting that Dex may interfere with FXR activation. Whether this suppression of Fgf15 expression by Dex directly occurred in ileal enterocytes, using an ex vivo culture system, was further investigated. As presented in Fig. 1D, CA induced Fgf15 expression in the ex vivo culture system, whereas, Dex interfered with the CA-induced FGF15 upregulation in ileal cells.
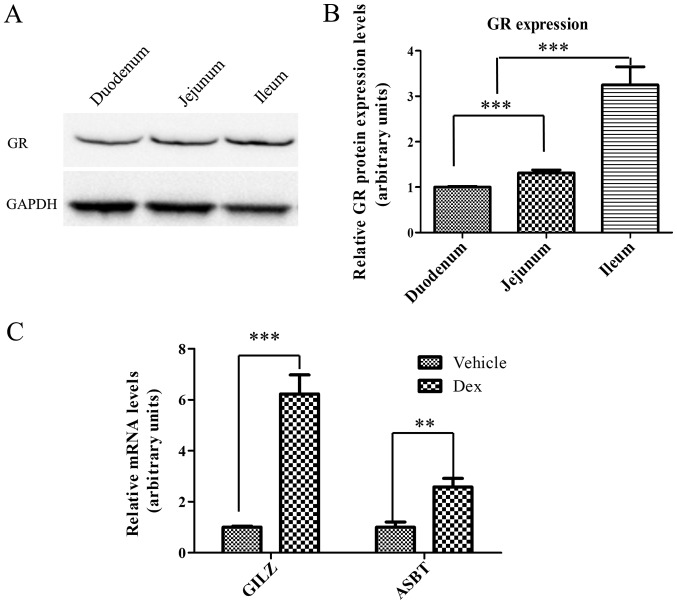
GR is expressed in the intestine and is able to respond to activation by Dex
GR may be activated by Dex, to trigger the transactivation or transrepression of GC-responsive genes (24–26). Therefore, GR protein expression levels in the small intestine were examined by western blot analysis. As presented in Fig. 2A, GR (~86 kDa) was expressed throughout the entire small intestine, between the duodenum and the ileum. Notably, GR expression in the small intestine exhibited a gradual increase between the duodenum and the ileum. The expression level of GR in ileum was ~3-times higher compared with the duodenum and ~2-times higher compared with the jejunum (Fig. 2B), suggesting that GR may have an important function in the ileum. Subsequently, it was determined whether ileal GR may be activated by treatment with Dex at a concentration of 80 mg/kg. It was identified that the mRNA expression levels of two selected GR target genes, GILZ and ASBT (27–29), were upregulated by ~6 and ~2.5-times, respectively, in the ileum following treatment with Dex for 24 h (Fig. 2C). These results demonstrated that GR was highly expressed in the ileum and may be activated by Dex, and thus may potentially mediate the repression of Fgf15 expression by Dex.
Figure 2.
Expression of GR and GR target genes in the ileum. (A) Western blot analysis of GR protein expression in the small intestine. The entire small intestine was equally divided into three segments, representing the duodenum, jejunum and ileum. Proteins (50 µg each) were analyzed on western blots with antibodies against GR and GAPDH. (B) Quantification of GR protein expression from three independent experiments. The data were normalized to the expression levels of mouse GAPDH. (C) Upregulation of GR target genes (GILZ and ASBT) expression following treatment with Dex for 24 h. The data were normalized to the expression levels of mouse U36b4. The data are presented as the mean ± standard deviation. n=3. **P<0.01, ***P<0.001. GR, glucocorticoid receptor; GILZ, glucocorticoid-induced leucine zipper; ASBT, apical sodium dependent bile acid transporter; Dex, dexamethasone.
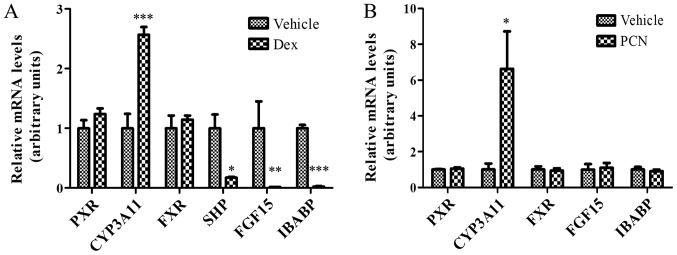
Suppression of Fgf15 expression by Dex is not associated with PXR
As Dex is able to activate GR and PXR, it was further examined if the effect of Dex on FGF15 expression is mediated by PXR. As presented in Fig. 3A, the suppression of Fgf15 expression was observed following treatment with Dex. Since Fgf15 is the downstream gene for FXR activation, the expression of SHP and IBABP, another two classical FXR target genes (3,30,31), was further examined in the ileum following treatment with Dex. As expected, SHP and IBABP expression were additionally significantly downregulated following treatment with Dex (Fig. 3A; P<0.01). This downregulation of Fgf15, SHP and IBABP gene expression reflects the inhibition of FXR activity; however, not FXR expression, as there was no significant difference in FXR expression.
Figure 3.
Suppression of FGF15 expression by Dex is potentially mediated by GR activation in the ileum. (A) GR activation by Dex (80 mg/kg) for 24 h induced CYP3A11 expression and suppressed the expression of FXR target genes (SHP, FGF15 and IBABP); however, did not affect FXR expression in the ileum. (B) PXR activation by PCN (25 mg/kg) for 24 h additionally induced CYP3A11 expression; however, did not affect the expression of FXR target genes (FGF15 and IBABP). The data were normalized to the expression levels of mouse U36B4. The data are presented as the mean ± standard deviation. n=3. *P<0.05, **P<0.01, ***P<0.001 vs. respective vehicle. FGF15, fibroblast growth factor 15; Dex, dexamethasone; GR, glucocorticoid receptor; CYP3A11, cytochrome P450, family 3, subfamily a, polypeptide 11; FXR, farnesoid X receptor; SHP, small heterodimer partner; IBABP, ileum bile acid binding protein; PXR, pregnane X receptor; PCN, pregnenolone-16-α-carbonitrile.
In addition to activating GR, Dex may additionally activate PXR to induce CYP3A expression (32,33). As presented in Fig. 3A, the expression of Cyp3a11, the target gene of PXR, was significantly increased in the ileum following treatment with Dex; however, there was no alteration in PXR expression, a result suggesting that the increased CYP3A expression was due to increased PXR activation. To confirm whether the suppression of Fgf15 expression by Dex is mediated by PXR activation, PCN, a typical PXR agonist, was used to treat mice in the same way as Dex. As presented in Fig. 3B, PCN induced the expression of Cyp3a11, a PXR target gene; however, it had no effect on the expression of either FXR or PXR, or FXR target genes, Fgf15 and IBABP, in the ileum. This result suggested that PXR activation did not contribute to the suppression of FGF15 expression by treatment with Dex.
Discussion
The present study demonstrated that treatment with Dex significantly suppressed the expression of Fgf15 in the mouse ileum. Although the concentration of serum FGF15 protein was not determined, the mRNA expression levels of Fgf15 are routinely used to represent the Fgf15 expression levels (3,4). Furthermore, as the Fgf15 mRNA expression levels were below the detectable level for at least 3 days during treatment with Dex, this suggested that the protein expression level of FGF15 was additionally reduced by treatment with Dex. As previously demonstrated, FGF15/FGF19 serves an important role in BA homeostasis, glucose metabolism and hepatic protein synthesis (3,4,6). For example, Inagaki et al (3) identified that FGF15 inhibited BA synthesis by repressing associated gene expression in the liver (3). Potthoff et al (4) demonstrated that FGF15 inhibited hepatic gluconeogenesis by blocking the expression of genes involved in gluconeogenesis (4). Therefore, Dex intake has the potential to increase the risks of metabolic disorder by repressing Fgf15 expression. Of note, GCs or their synthetic analogs (including Dex) have been demonstrated to cause metabolic diseases, including hyperglycemia and liver steatosis in specific patients (11–13). Notably, the effects of Dex on Fgf15 expression were dose dependent. Therefore, an initial high dosage is occasionally recommended in the clinical setting; however, the consecutive use of Dex at high dosage is not recommended. Although the most effective dose of Dex (80 mg/kg) was studied, is higher compared with therapeutic doses, which may be as high as ~6 mg/kg in emergency treatment, according to the US Food and Drug Administration approved drug dosage information for Dex (34), used in patients, a trend of inhibition was additionally observed at the lower, therapeutic, doses. Therefore, the underlying risks require consideration.
The present study further demonstrated that the downregulation of Fgf15 by Dex is associated with decreased transcriptional activity of FXR. As previously demonstrated, FXR, which may be activated by BAs, is considered the principal transcriptional factor regulating Fgf15 expression (3). Therefore, the decrease in Fgf15 expression reflected the repression of FXR activity. The inhibition of FXR activity was further demonstrated by the result that treatment with Dex additionally suppressed the expression of SHP and IBABP, another two classical target genes of FXR in the ileum (3,30,31). Notably, the suppression of Fgf15 and IBABP by Dex was restricted to the ileum, as Fgf15 and IBABP are primarily expressed in the ileum (3,30). However, the inhibition of FXR activity by Dex may be not restricted to the ileum based on the preliminary observations of the present study. Considering that FXR and GR additionally coexist in other segments of small intestine (3), this hypothesis is reasonable. This suppression of FXR target gene expression by Dex was not accompanied by an alteration in the FXR expression level, which suggested that Dex did not regulate Fgf15 expression via suppression of FXR expression. However, how Dex interferes with FXR activation remains unclear.
As Dex is able to activate PXR and GR, it was additionally determined whether the downregulation of Fgf15 by Dex may be attributed to GR activation alone (33,35). It was demonstrated that PXR may be activated by higher dosages of Dex compared with those typically required by classical GR activation (33,36,37). In the present study, although PXR additionally responded to Dex in the ileum, the activation of PXR by PCN had no effect on the Fgf15 expression, demonstrating that the suppression of Fgf15 expression was not associated with PXR activation. Notably, GR, as a classical, accepted receptor of Dex, has the highest expression in the ileum among the three anatomical parts of the small intestine. Furthermore, ileal GR responded to treatment with Dex; the mRNA expression levels of two selected GR target genes, GILZ and ASBT were significantly upregulated. These results suggested that GR activation by Dex may be responsible for the suppression of FXR activation, leading to the downregulation of Fgf15 expression in ileum. However, the hypothesis that anti-GC drugs, including RU486, may induce Fgf15 expression based on the preliminary data of the present study requires further investigation. This investigation may help to better clarify the role of GR in regulating Fgf15 expression in the intestine.
How GR activation by Dex inhibits the transcriptional activity of FXR remains to be determined. GR is a classical receptor for GCs, and the activation of GR may repress a number of pro-inflammatory genes by interacting with nuclear factor-κB (NF-κB) (10). For example, GR activation represses TNFα and IL-6 expression by inhibiting NF-κB transcriptional activity (10). It has additionally been identified that GR may interact with FXR, by recruiting the C-terminal binding domain protein and repressing its activity in the liver (38). As GR and FXR are transcriptional factors that exhibit high expression levels in ileal cells, it is hypothesized that their crosstalk may serve an important role. However, further studies are required to provide molecular evidence and determine the underlying mechanisms.
In summary, the present results suggested that treatment with Dex may downregulate ileal Fgf15 expression, and this downregulation is associated with GR-mediated repression of FXR activity. The present results provide insight for a better understanding of the mechanism of regulation of Fgf15 expression and suggest the possible occurrence of adverse events resulting from Fgf15/19 suppression associated with treatment with Dex in patients.
Acknowledgements
Not applicable.
Glossary
Abbreviations
- FGF15
fibroblast growth factor 15
- Dex
dexamethasone
- FXR
farnesoid X receptor
- GR
glucocorticoid receptor
- CA
cholic acid
- PCN
pregnenolone-16-α-carbonitrile
- PXR
pregnane X receptor
- RXR
retinoid X receptors
- GC
glucocorticoid
Funding
The present study was supported by The National Institute of General Medical Sciences (grant no. GM082978), The Chinese National Nature Sciences Foundation (grant no. 31501232), The Scientific Research Foundation for the Returned Overseas Chinese Scholars, State Education Ministry, The Fujian Provincial Nature Science Foundation (grant no. 2015J05052), and The Fujian Agriculture and Forestry University Science Fund for Distinguished Young Scholars (grant no. xjq201629; Fuzhou, China).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
KZ performed the experiments and wrote the manuscript. QJ, QZ and DZ contributed to the design of the study and the writing of the manuscript.
Ethics approval and consent to participate
All animal studies were approved by the Institutional Animal Care and Use Committee of the Wadsworth Center (State University of New York, Albany, NY, USA) or the Animal Ethics Committee of the Fujian Agriculture and Forestry University (Fuzhou, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.McWhirter JR, Goulding M, Weiner JA, Chun J, Murre C. A novel fibroblast growth factor gene expressed in the developing nervous system is a downstream target of the chimeric homeodomain oncoprotein E2A-Pbx1. Development. 1997;124:3221–3232. doi: 10.1242/dev.124.17.3221. [DOI] [PubMed] [Google Scholar]
- 2.Nishimura T, Utsunomiya Y, Hoshikawa M, Ohuchi H, Itoh N. Structure and expression of a novel human FGF, FGF-19, expressed in the fetal brain. Biochim Biophys Acta. 1999;1444:148–151. doi: 10.1016/S0167-4781(98)00255-3. [DOI] [PubMed] [Google Scholar]
- 3.Inagaki T, Choi M, Moschetta A, Peng L, Cummins CL, McDonald JG, Luo G, Jones SA, Goodwin B, Richardson JA, et al. Fibroblast growth factor 15 functions as an enterohepatic signal to regulate bile acid homeostasis. Cell Metab. 2005;2:217–225. doi: 10.1016/j.cmet.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Potthoff MJ, Boney-Montoya J, Choi M, He T, Sunny NE, Satapati S, Suino-Powell K, Xu HE, Gerard RD, Finck BN, et al. FGF15/19 regulates hepatic glucose metabolism by inhibiting the CREB-PGC-1α pathway. Cell Metab. 2011;13:729–738. doi: 10.1016/j.cmet.2011.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fu L, John LM, Adams SH, Yu XX, Tomlinson E, Renz M, Williams PM, Soriano R, Corpuz R, Moffat B, et al. Fibroblast growth factor 19 increases metabolic rate and reverses dietary and leptin-deficient diabetes. Endocrinology. 2004;145:2594–2603. doi: 10.1210/en.2003-1671. [DOI] [PubMed] [Google Scholar]
- 6.Kir S, Beddow SA, Samuel VT, Miller P, Previs SF, Suino-Powell K, Xu HE, Shulman GI, Kliewer SA, Mangelsdorf DJ. FGF19 as a postprandial, insulin-independent activator of hepatic protein and glycogen synthesis. Science. 2011;331:1621–1624. doi: 10.1126/science.1198363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tomlinson E, Fu L, John L, Hultgren B, Huang X, Renz M, Stephan JP, Tsai SP, Powell-Braxton L, French D, Stewart TA. Transgenic mice expressing human fibroblast growth factor-19 display increased metabolic rate and decreased adiposity. Endocrinology. 2002;143:1741–1747. doi: 10.1210/endo.143.5.8850. [DOI] [PubMed] [Google Scholar]
- 8.Schmidt DR, Holmstrom SR, Fon Tacer K, Bookout AL, Kliewer SA, Mangelsdorf DJ. Regulation of bile acid synthesis by fat-soluble vitamins A and D. J Biol Chem. 2010;285:14486–14494. doi: 10.1074/jbc.M110.116004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reue K, Lee JM, Vergnes L. Diet1 is a regulator of fibroblast growth factor 15/19-dependent bile acid synthesis. Dig Dis. 2015;33:307–313. doi: 10.1159/000371649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baschant U, Lane NE, Tuckermann J. The multiple facets of glucocorticoid action in rheumatoid arthritis. Nat Rev Rheumatol. 2012;8:645–655. doi: 10.1038/nrrheum.2012.166. [DOI] [PubMed] [Google Scholar]
- 11.Andrews RC, Walker BR. Glucocorticoids and insulin resistance: Old hormones, new targets. Clin Sci (Lond) 1999;96:513–523. doi: 10.1042/CS19980388. [DOI] [PubMed] [Google Scholar]
- 12.Lemke U, Krones-Herzig A, Berriel Diaz M, Narvekar P, Ziegler A, Vegiopoulos A, Cato AC, Bohl S, Klingmüller U, Screaton RA, et al. The glucocorticoid receptor controls hepatic dyslipidemia through Hes1. Cell Metab. 2008;8:212–223. doi: 10.1016/j.cmet.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Yamanishi Y, Nosaka Y, Kawasaki H, Hirayama C, Ikawa S. Sterol and bile acid metabolism after short-term prednisolone treatment in patients with chronic active hepatitis. Gastroenterol Jpn. 1985;20:246–251. doi: 10.1007/BF02774711. [DOI] [PubMed] [Google Scholar]
- 14.Ge H, Zhang J, Gong Y, Gupte J, Ye J, Weiszmann J, Samayoa K, Coberly S, Gardner J, Wang H, et al. Fibroblast growth factor receptor 4 (FGFR4) deficiency improves insulin resistance and glucose metabolism under diet-induced obesity conditions. J Biol Chem. 2014;289:30470–30480. doi: 10.1074/jbc.M114.592022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jia K, Li L, Liu Z, Hartog M, Kluetzman K, Zhang QY, Ding X. Generation and characterization of a novel CYP2A13-transgenic mouse model. Drug Metab Dispos. 2014;42:1341–1348. doi: 10.1124/dmd.114.059188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.D'Agostino J, Ding X, Zhang P, Jia K, Fang C, Zhu Y, Spink DC, Zhang QY. Potential biological functions of cytochrome P450 reductase-dependent enzymes in small intestine: Novel link to expression of major histocompatibility complex class II genes. J Biol Chem. 2012;287:17777–17788. doi: 10.1074/jbc.M112.354274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 18.Schmittgen TD, Livak KJ. Analyszing real-time PCR data by the comparative C(T) method. Nat Protoc. 2008;3:1101–1108. doi: 10.1038/nprot.2008.73. [DOI] [PubMed] [Google Scholar]
- 19.Cariou B, van Harmelen K, Duran-Sandoval D, van Dijk TH, Grefhorst A, Abdelkarim M, Caron S, Torpier G, Fruchart JC, Gonzalez FJ, et al. The farnesoid X receptor modulates adiposity and peripheral insulin sensitivity in mice. J Biol Chem. 2006;281:11039–11049. doi: 10.1074/jbc.M510258200. [DOI] [PubMed] [Google Scholar]
- 20.Trousson A, Makoukji J, Petit PX, Bernard S, Slomianny C, Schumacher M, Massaad C. Cross-talk between oxysterols and glucocorticoids: Differential regulation of secreted phopholipase A2 and impact on oligodendrocyte death. PLoS One. 2009;4:e8080. doi: 10.1371/journal.pone.0008080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berrebi D, Bruscoli S, Cohen N, Foussat A, Migliorati G, Bouchet-Delbos L, Maillot MC, Portier A, Couderc J, Galanaud P, et al. Synthesis of glucocorticoid-induced leucine zipper (GILZ) by macrophages: An anti-inflammatory and immunosuppressive mechanism shared by glucocorticoids and IL-10. Blood. 2003;101:729–738. doi: 10.1182/blood-2002-02-0538. [DOI] [PubMed] [Google Scholar]
- 22.Miyata M, Yamakawa H, Hamatsu M, Kuribayashi H, Takamatsu Y, Yamazoe Y. Enterobacteria modulate intestinal bile acid transport and homeostasis through apical sodium-dependent bile acid transporter (SLC10A2) expression. J Pharmacol Exp Ther. 2011;336:188–196. doi: 10.1124/jpet.110.171736. [DOI] [PubMed] [Google Scholar]
- 23.Zhang QY, Dunbar D, Kaminsky LS. Characterization of mouse small intestinal cytochrome P450 expression. Drug Metab Dispos. 2003;31:1346–1351. doi: 10.1124/dmd.31.11.1346. [DOI] [PubMed] [Google Scholar]
- 24.Yamamoto KR. Steroid receptor regulated transcription of specific genes and gene networks. Annu Rev Genet. 1985;19:209–252. doi: 10.1146/annurev.ge.19.120185.001233. [DOI] [PubMed] [Google Scholar]
- 25.Yamamoto KR, Darimont BD, Wagner RL, Iñiguez-Lluhí JA. Building transcriptional regulatory complexes: Signals and surfaces. Cold Spring Harb Symp Quant Biol. 1998;63:587–598. doi: 10.1101/sqb.1998.63.587. [DOI] [PubMed] [Google Scholar]
- 26.Weikum ER, Knuesel MT, Ortlund EA, Yamamoto KR. Glucocorticoid receptor control of transcription: Precision and plasticity via allostery. Nat Rev Mol Cell Biol. 2017;18:159–174. doi: 10.1038/nrm.2016.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ayroldi E, Riccardi C. Glucocorticoid-induced leucine zipper (GILZ): A new important mediator of glucocorticoid action. FASEB J. 2009;23:3649–3658. doi: 10.1096/fj.09-134684. [DOI] [PubMed] [Google Scholar]
- 28.Wang JC, Derynck MK, Nonaka DF, Khodabakhsh DB, Haqq C, Yamamoto KR. Chromatin immunoprecipitation (ChIP) scanning identifies primary glucocorticoid receptor target genes. Proc Natl Acad Sci USA. 2004;101:15603–15608. doi: 10.1073/pnas.0407008101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jung D, Fantin AC, Scheurer U, Fried M, Kullak-Ublick GA. Human ileal bile acid transporter gene ASBT (SLC10A2) is transactivated by the glucocorticoid receptor. Gut. 2004;53:78–84. doi: 10.1136/gut.53.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grober J, Zaghini I, Fujii H, Jones SA, Kliewer SA, Willson TM, Ono T, Besnard P. Identification of a bile acid-responsive element in the human ileal bile acid-binding protein gene. Involvement of the farnesoid X receptor/9-cis-retinoic acid receptor heterodimer. J Biol Chem. 1999;274:29749–29754. doi: 10.1074/jbc.274.42.29749. [DOI] [PubMed] [Google Scholar]
- 31.Hwang ST, Urizar NL, Moore DD, Henning SJ. Bile acids regulate the ontogenic expression of ileal bile acid binding protein in the rat via the farnesoid X receptor. Gastroenterology. 2002;122:1483–1492. doi: 10.1053/gast.2002.32982. [DOI] [PubMed] [Google Scholar]
- 32.Huss JM, Kasper CB. Two-stage glucocorticoid induction of CYP3A23 through both the glucocorticoid and pregnane X receptors. Mol Pharmacol. 2000;58:48–57. doi: 10.1124/mol.58.1.48. [DOI] [PubMed] [Google Scholar]
- 33.Kliewer SA, Moore JT, Wade L, Staudinger JL, Watson MA, Jones SA, McKee DD, Oliver BB, Willson TM, Zetterström RH, et al. An orphan nuclear receptor activated by pregnanes defines a novel steroid signaling pathway. Cell. 1998;92:73–82. doi: 10.1016/S0092-8674(00)80900-9. [DOI] [PubMed] [Google Scholar]
- 34.Dietzman RH, Ersek RA, Bloch JM, Lilleheir RC. High-output, low-resistance gram-negative septic shock in man. Angiology. 1969;20:691–700. doi: 10.1177/000331976902001108. [DOI] [PubMed] [Google Scholar]
- 35.Lehmann JM, McKee DD, Watson MA, Willson TM, Moore JT, Kliewer SA. The human orphan nuclear receptor PXR is activated by compounds that regulate CYP3A4 gene expression and cause drug interactions. J Clin Invest. 1998;102:1016–1023. doi: 10.1172/JCI3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schuetz EG, Guzelian PS. Induction of cytochrome P-450 by glucocorticoids in rat liver. II. Evidence that glucocorticoids regulate induction of cytochrome P-450 by a nonclassical receptor mechanism. J Biol Chem. 1984;259:2007–2012. [PubMed] [Google Scholar]
- 37.Schuetz EG, Wrighton SA, Barwick JL, Guzelian PS. Induction of cytochrome P-450 by glucocorticoids in rat liver. I. Evidence that glucocorticoids and pregnenolone 16 alpha-carbonitrile regulate de novo synthesis of a common form of cytochrome P-450 in cultures of adult rat hepatocytes and in the liver in vivo. J Biol Chem. 1984;259:1999–2006. [PubMed] [Google Scholar]
- 38.Lu Y, Zhang Z, Xiong X, Wang X, Li J, Shi G, Yang J, Zhang X, Zhang H, Hong J, et al. Glucocorticoids promote hepatic cholestasis in mice by inhibiting the transcriptional activity of the farnesoid X receptor. Gastroenterology. 2012;143:1630–1640. doi: 10.1053/j.gastro.2012.08.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.