Abstract
Background:
Degenerative medial meniscus posterior root tears (MMPRTs) are reportedly associated with medial compartment osteoarthritis and meniscal extrusion with a displaced gap from the root insertion. However, degenerative MMPRTs have not yet been clearly classified according to arthroscopic findings.
Purpose:
To classify degenerative MMPRTs according to the tear gap and to investigate how the classification could reflect the joint condition properly.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Patients who underwent arthroscopic surgery, performed by a single orthopaedic surgeon, for degenerative MMPRTs between August 2006 and February 2017 were included. MMPRTs were classified according to tear patterns observed during arthroscopic surgery (type 1, incomplete root tear; types 2-5, complete root tears), with each type further divided by the size of the tear gap, defined as the degree of tear displacement from the root (type 2, no gap or overlapped; type 3, gap of 1-3 mm; type 4, gap of 4-6 mm; type 5, gap of ≥7 mm). We compared preoperative factors, including the Kellgren-Lawrence (K-L) grade, absolute extrusion, relative percentage of extrusion (RPE), tear gap on magnetic resonance imaging (MRI), and mechanical alignment, as well as intraoperative factors, including chondral wear at surgery, between each MMPRT type.
Results:
A total of 116 root tears were categorized according to this classification: type 1, 16.4% (19 knees); type 2, 9.5% (11 knees); type 3, 40.5% (47 knees); type 4, 25.0% (29 knees); and type 5, 8.6% (10 knees). Chondral wear of the medial femoral condyle (MFC) (P = .001), K-L grade (P = .001), meniscal extrusion (P = .001), and tear gap on MRI (P = .001) showed a tendency to increase with a higher tear type. Chondral wear (ρ for MFC = 0.388; ρ for MTP = 0.311), K-L grade (ρ = 0.390), and meniscal extrusion (ρ for absolute extrusion = 0.500; ρ for RPE = 0.451) showed a moderate correlation with tear type, whereas tear gap on MRI (ρ = 0.907) showed a strong correlation with tear type.
Conclusion:
Our study introduces a new classification based on the tear gap that can concisely describe a degenerative MMPRT. The classification system demonstrated that a higher tear type (increasing displacement of the tear gap in arthroscopic surgery) is associated with higher meniscal extrusion, severe chondral wear, and greater severity of arthritis.
Keywords: medial meniscus, root tear, classification, displacement
The menisci have important biomechanical functions, including load transmission, shock absorption, joint stabilization, lubrication, and proprioception.26,32 The medial meniscus is rigidly attached to the tibia and is therefore less mobile, making it more vulnerable to traumatic injuries and degenerative changes than the lateral meniscus.14,31 Recently, medial meniscus posterior root tears (MMPRTs), defined as radial tears occurring within 9 mm from the root attachment, have become an active topic of research.3,21 The loss of hoop strain by MMPRTs leads to a physiological state equivalent to total meniscectomy and can accelerate the process of degenerative arthritis with meniscal extrusion.11,15 Many studies have shown that MMPRTs are associated with osteoarthritis, but the most precipitating factor is unclear,5,28 and debate about the associative factors and treatment strategy of MMPRTs is ongoing.1,4,6,8,18–20,26
Recently, 1 study21 attempted to identify meniscal root tears according to tear morphology through an arthroscopic examination. However, their classification system had some limitations. First, the classification was a general description of meniscal root tears in both traumatic and degenerative conditions and included the relatively rare lateral meniscal anterior and posterior horn tears and medial meniscal anterior horn tears. Second, most meniscal tears were classified as radial tears, and the remaining types were rare. This raised the question of whether the system could classify root tears properly. Most MMPRTs are degenerative tears observed in middle-aged or older women10,12,17,24; therefore, this classification might be a limited clinical indicator of degenerative MMPRTs for further treatment plans and later prognoses. Another study demonstrated that if physiological loading is applied for an extended period, the gap becomes widely displaced, with meniscal extrusion.2 The extruded meniscus can increase peak contact pressure in the medial compartment of the knee, similar to total meniscectomy, and can lead to arthritic changes.11,15 In the current study, we hypothesized that a displaced tear gap in degenerative MMPRTs would reflect the joint condition and thus could be used to classify MMPRTs. In addition, we analyzed how well this classification reflects the degree of meniscal extrusion and severity of arthritis.
Methods
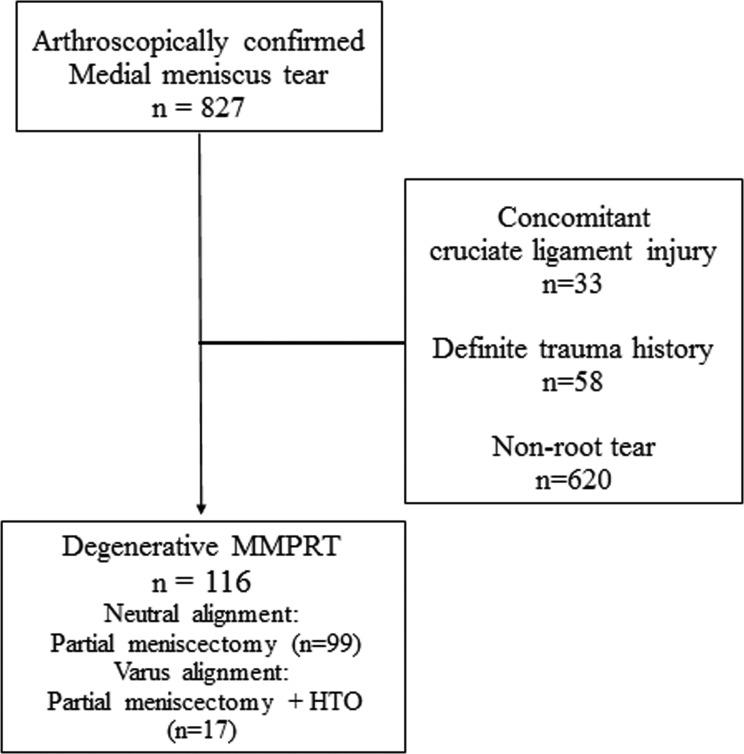
This study was undertaken with institutional review board approval. We retrospectively reviewed patients who underwent arthroscopic surgery for medial meniscal tears between August 2006 and February 2017, as performed by a single surgeon (S.-I.B.). Of the 827 knees with medial meniscal tears, 33 knees with accompanying anterior cruciate ligament injuries, 58 knees with a definite trauma history, and 620 knees that revealed nonroot tears (such as horizontal, flap, longitudinal, or complex tears) on arthroscopic examination were excluded. Consequently, 116 knees that were arthroscopically confirmed as having degenerative MMPRTs were enrolled in the present study. Indications for surgery were root tears diagnosed by magnetic resonance imaging (MRI) and the persistence of mechanical symptoms despite at least 3 months of medication (including nonsteroidal anti-inflammatory drugs) and muscle strengthening exercises. Arthroscopic partial meniscectomy was performed alone in 99 knees with neutral knee alignment (within 4° of varus or valgus on the hip-knee-ankle [HKA] angle).3,26 In patients with ≥5° varus mechanical alignment, high tibial osteotomy was performed in addition to partial meniscectomy (17 knees) (Figure 1).
Figure 1.
Flowchart of inclusion and exclusion criteria for the classification of degenerative medial meniscus posterior root tears (MMPRTs). Neutral alignment, within 4° of varus or valgus on the hip-knee-ankle angle; varus alignment, over 5° of varus on the hip-knee-ankle angle. HTO, high tibial osteotomy.
Measurement of Tear Gap and Classification of MMPRTs
The tear gap, which is the distance between the torn meniscus and the midportion of the corresponding edge of the root attachment, was measured using a probe scale at 10° of knee flexion and valgus stress. Root tears were classified into 5 types according to the presence of a complete tear and the measured value of the tear gap: type 1, incomplete root tear; type 2, complete root tear with no gap or overlapped; type 3, complete root tear with gap measuring 1-3 mm; type 4, complete root tear with gap measuring 4-6 mm; and type 5, complete root tear with gap measuring ≥7 mm (Figure 2). A single experienced knee surgeon (S.-I.B.) measured and recorded the tear gap during surgery, while 2 other surgeons (J.-Y.K., S.-M.O.) retrospectively reviewed the captured images and medical records, and there were no differences of opinion on the classification.
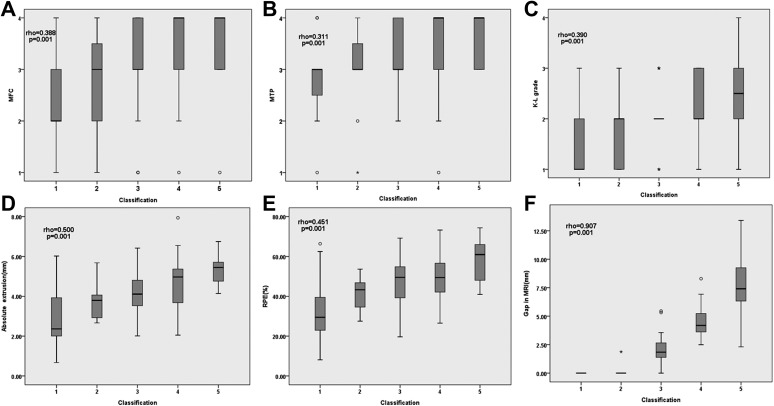
Figure 2.
Arthroscopic image from a 69-year-old female patient showing a tear gap measuring 0 mm with a complete tear, corresponding to a type 2 root tear (arrow). The tear gap was measured using a probe scale at 10° of knee flexion and valgus stress.
Chondral Wear and Osteoarthritis Radiographic Assessment
The cartilage status of both the medial femoral condyle (MFC) and medial tibial plateau (MTP) were assessed during arthroscopic surgery by a single surgeon. The worst area of cartilage at each compartment was assessed using the Outerbridge classification and used as a representation for analysis.25 It was documented in the electronic medical record system just after surgery by the surgeon. Mechanical alignment was assessed by measuring the HKA angle on preoperative radiographs with a true long-standing anteroposterior view.30 The radiographic assessment of medial compartment osteoarthritis was conducted using the Kellgren-Lawrence (K-L) grading system.13
Meniscal Extrusion and Tear Gap on MRI
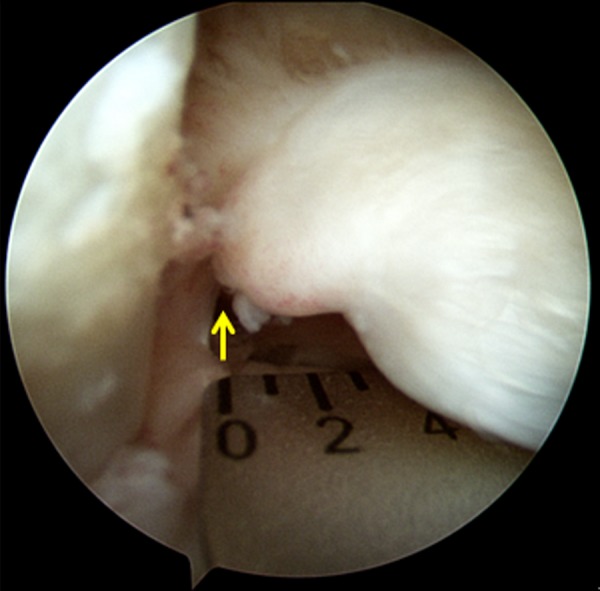
Extrusion was evaluated on the midcoronal plane of preoperative MRI by measuring the absolute extrusion and relative percentage of extrusion (RPE). Absolute extrusion was defined as the distance between 2 lines drawn perpendicular to the articular surface: one on the outer margin of the MTP and one on the outer edge of the meniscus. RPE was defined as the percentage of the meniscus that extruded from the width of the entire meniscus (Figure 3).22 Absolute extrusion exceeding 3 mm was categorized as major extrusion, and all lesser values were categorized as minor extrusion.7
Figure 3.
Example of extrusion measurement. The relative percentage of extrusion was defined as the width of the extruded meniscus divided by the width of the entire meniscus (%): a/b × 100, where a is the absolute extrusion (mm) and b is the width of the entire meniscus (mm).
To measure the tear gap on MRI, the coronal plane image with the most prominently visible medial meniscal posterior root insertion was selected. The medial joint line was drawn while considering the obliquity of the MTP. A line perpendicular to the medial joint line was drawn on the intercondylar fossa (or in applicable cases, the location of the remaining insertional ligament). A second line perpendicular to the medial joint line was drawn on the medial edge of the displaced meniscus. The distance between these 2 lines was defined as the tear gap (Figure 4).
Figure 4.
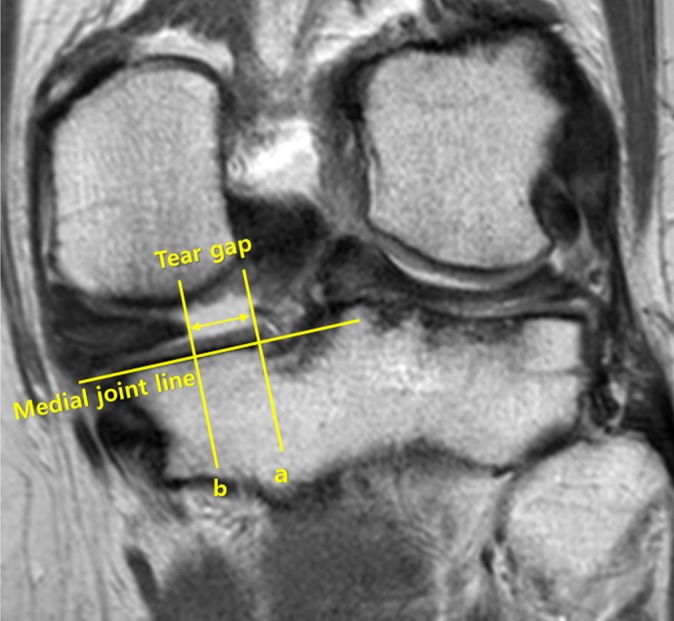
Tear gap measurements were made on coronal magnetic resonance imaging with the most prominently visible medial meniscal posterior horn root insertion (cleft sign). The tear gap was defined as the distance between the vertical line from the intercondylar fossa or remnant insertional ligament to the medial joint line, a, and to the medially displaced meniscal edge, b.
Statistical Analysis
Statistical analysis was performed using SPSS version 18.0 for Windows (IBM). Overall significance and differences in covariates among the 5 tear types were analyzed using the Kruskal-Wallis test. The Mann-Whitney U test was used to compare the pairing of 2 types. Significance among the different types was affirmed through the Mann-Whitney U test (as there were 5 types, the statistical significance obtained through the Bonferroni correction [.05/5C2] was P < .005). Additionally, Spearman correlation analysis was performed to determine the intensity of association between each tear type and chondral wear, meniscal extrusion, and severity of arthritis. Two orthopaedic surgeons (J.-Y.K., S.-M.O.) measured the absolute extrusion, RPE, and tear gap on MRI. The reliability for absolute extrusion, RPE, and tear gap on MRI was evaluated using intraclass correlation coefficients (ICCs); the ICCs for intraobserver/interobserver reliability were 0.92/0.86 for absolute extrusion, 0.90/0.82 for RPE, and 0.89/0.80 for tear gap (P = .001 for all).
Results
The demographics of patients with degenerative MMPRTs are reported in Table 1, and the incidence of each tear type, according to our proposed classification, is presented in Table 2.
TABLE 1.
Demographics of Patientsa
| Parameter | Value |
|---|---|
| Age, y | 58.60 ± 8.90 (43-77) |
| Male/female sex, n | 26/90 |
| Symptom duration, mo | 7.47 ± 2.35 |
| Weight, kg | 65.15 ± 10.22 |
| Body mass index, kg/m2 | 25.98 ± 2.89 |
| Preoperative HKA angle, deg | 2.79 ± 2.95 |
aData are shown as mean ± SD or mean ± SD (range) unless otherwise indicated. HKA, hip-knee-ankle.
TABLE 2.
Incidence of Each Tear Type According to Novel Arthroscopic Classification
| Type | Description | n (%) |
|---|---|---|
| 1 | Incomplete root tear | 19 (16.4) |
| Complete root tear | ||
| 2 | No gap or overlapped | 11 (9.5) |
| 3 | Gap of 1-3 mm | 47 (40.5) |
| 4 | Gap of 4-6 mm | 29 (25.0) |
| 5 | Gap of ≥7 mm | 10 (8.6) |
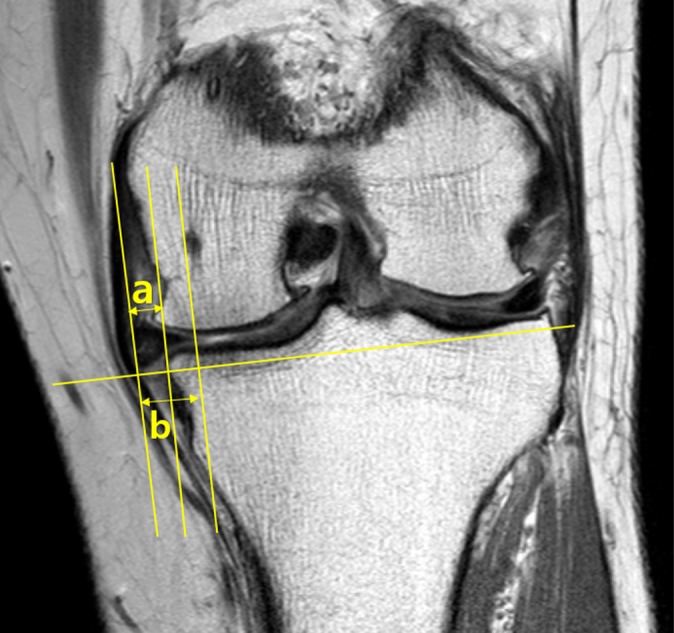
The differences in covariates according to tear type classification are presented in Table 3, and the associations between the covariates and the classifications are plotted in Figure 5. There were no significant differences in mechanical alignment, body mass index, sex, age, and MTP grade among the 5 types. However, there were significant differences in the Outerbridge grade of the MFC, K-L grade, absolute extrusion, RPE, and tear gap on MRI among the 5 types (Table 3). When the tear type was higher, the Outerbridge grade of the MFC (P = .001), K-L grade (P = .001), absolute extrusion (P = .001), RPE (P = .001), and tear gap on MRI (P = .001) increased. In addition, there was a trend of covariates showing that the intra-articular status of the knee gradually worsened as the tear gap increased. This correlation was confirmed through Spearman correlation analysis (Figure 5). As shown in Figure 5C, most patients with type 3 root tears were assessed as having K-L grade 2; thus, a box plot was omitted and the graph was marked with a median value of grade 2.
TABLE 3.
Covariates According to Novel Arthroscopic Classificationa
| Covariate | Tear Type | P | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| MFC Outerbridge grade | 2.32 ± 1.03e | 2.82 ± 0.98 | 3.04 ± 0.86 | 3.38 ± 0.76b | 3.50 ± 0.97 | .001 |
| MTP Outerbridge grade | 2.84 ± 0.76 | 3.00 ± 0.89 | 3.40 ± 0.58 | 3.38 ± 0.77 | 3.70 ± 0.48 | .009 |
| K-L grade | 1.53 ± 0.61d,e | 1.64 ± 0.67 | 2.04 ± 0.51b | 2.21 ± 0.62b | 2.40 ± 0.97 | .001 |
| Absolute extrusion, mm | 2.89 ± 1.45d,e,f | 3.68 ± 0.90f | 4.15 ± 0.96b,f | 4.66 ± 1.25b | 5.41 ± 0.75b,c,d | .001 |
| RPE, % | 32.44 ± 15.24d,e,f | 41.03 ± 9.06f | 47.04 ± 11.27b | 49.95 ± 12.06b | 57.39 ± 11.29b,c | .001 |
| Tear gap on MRI, mm | 0d,e,f | 0.17 ± 0.56d,e,f | 2.07 ± 1.02b,c,e,f | 4.57 ± 1.38b,c,d,f | 8.10 ± 3.21b,c,d,e | .001 |
| Age, y | 54.05 ± 13.16 | 54.73 ± 7.81 | 60.83 ± 7.53 | 59.21 ± 7.37 | 59.79 ± 7.24 | .190 |
| HKA angle, deg | 3.11 ± 3.14 | 1.64 ± 3.33 | 2.94 ± 2.78 | 2.83 ± 3.08 | 2.70 ± 2.87 | .561 |
| Body mass index, kg/m2 | 25.40 ± 2.87 | 25.20 ± 3.14 | 26.46 ± 2.86 | 26.08 ± 3.08 | 25.38 ± 2.25 | .424 |
| Sex, male/female, n | 7/12 | 2/9 | 8/39 | 7/22 | 2/8 | .483 |
aData with the exception of sex are shown as mean ± SD. Pairs with P < .005 (according to the Bonferroni correction) on the Mann-Whitney U test indicate a significant difference from the following tear types: b1, c2, d3, e4, and f5. HKA, hip-knee-ankle (with positive and negative values representing varus and valgus mechanical alignment, respectively); K-L, Kellgren-Lawrence; MFC, medial femoral condyle; MRI, magnetic resonance imaging; MTP, medial tibial plateau; RPE, relative percentage of extrusion.
Figure 5.
Covariates according to the novel arthroscopic tear type classification: (A) medial femoral condyle (MFC) Outerbridge grade, (B) medial tibial plateau (MTP) Outerbridge grade, (C) Kellgren-Lawrence (K-L) grade, (D) absolute extrusion, (E) relative percentage of extrusion (RPE), and (F) tear gap on magnetic resonance imaging (MRI). Correlations between each covariate and the classifications were calculated using Spearman correlation analysis and were defined as weak (0.1 ≤ ρ < 0.3), moderate (0.3 ≤ ρ < 0.7), or strong (ρ ≥ 0.7). *Most patients with type 3 tears were assessed as having K-L grade 2; thus, a box plot was omitted and the graph was instead marked with a median value.
Discussion
This study presents an arthroscopic classification system for degenerative MMPRTs based on the tear gap. The most important finding is that a higher tear type was correlated with a higher severity of arthritis. Arthritic changes visible on radiographs and arthroscopic surgery as well as meniscal extrusion visible on MRI were correlated with an advanced tear type. Spearman correlation analysis showed that chondral wear of the MFC and MTP, K-L grade, absolute extrusion, and RPE had a moderate correlation with tear type, and tear gap on MRI had a strong correlation with tear type. These findings suggest that in degenerative MMPRTs, as the transected meniscus becomes displaced under long-standing physiological loading, meniscal extrusion increases and chondral wear accelerates; that is, an MMPRT could be a precursor to osteoarthritis, or alternatively, the loss of cartilage and joint space causes increased loading, which in turn produces the MMPRT or widening and extrusion of an existing MMPRT.
LaPrade et al21 presented a classification system of meniscal root tears and divided the tears into 5 types according to morphological features. Although this system details the chronology and treatment of various tears according to morphological type and is a comprehensive classification system for meniscal root tears, the LaPrade classification is based on the distance of the tear from the root, whereas our classification is based on the gap of the tear. One of the major shortcomings of their classification is that it contained both traumatic and degenerative MMPRTs and did not reveal the association between the cartilage status of the joint and the type, thus limiting its use in the clinical setting.
Furumatsu et al9 reported that meniscal extrusion in MMPRTs increased with time after a painful popping event. In our study, as the tear gap and meniscal extrusion showed a positive correlation, it could be deduced that as the duration of the tear increases, the tear gap and meniscal extrusion increase.
A similar study by Bin et al2 classified degenerative MMPRTs into nondisplaced, overlapped, and widely displaced groups through an arthroscopic examination and compared the results with radiographic and MRI findings. The widely displaced group had a greater amount of meniscal extrusion, greater joint space narrowing, and greater varus alignment than the nondisplaced and overlapped groups. These findings are similar to our findings of a worsening joint status with greater meniscal displacement. However, the criterion for a “widely displaced” root tear is somewhat vague; hence, we based our classification on objective measurements, which makes it more accurate than the classification of Bin et al.2 MMPRTs have the highest incidence among root tears, and our classification is comparatively more concise and specific and has correlation with the articular status. In patients who underwent surgical repair for MMPRTs, factors such as Outerbridge grade 3 or 4 chondral lesions, pre-existing osteoarthritis with K-L grade >3, definite meniscal degeneration, and higher body mass index (>30 kg/m2) were associated with poor clinical outcomes.16,17,23,27,29 When considering treatment options for MMPRTs in reference to our classification, patients with tear type ≥3 typically had chondral wear exceeding Outerbridge grade 3 and arthritic changes exceeding K-L grade 2 and are thus more likely to have poor clinical outcomes after surgical repair. These worse outcomes may be related to higher forces on the repair site for increased gapping or may be a result of pre-existing degenerative changes.
This study has several limitations. First, it had a small sample size, and as with any retrospective study, there is a possibility of recall bias. However, all the data (such as tear gap and cartilage status) had been collected prospectively and were recorded by a single experienced knee surgeon immediately after surgery into the electronic medical record system, thus minimizing possible errors due to recall bias. Second, as the sample consisted only of patients with symptomatic degenerative MMPRTs who had undergone partial meniscectomy, selection bias was unavoidable. Therefore, the results should not be compared with or applied to asymptomatic patients or patients with traumatic avulsion MMPRTs. Third, this was a cross-sectional study of the knee status before and during surgery and thus does not provide postoperative clinical and radiological outcomes for each tear type. Finally, the surgeon measuring the gap arthroscopically was not blinded to the articular cartilage findings, although there was generally good consistency when the other 2 orthopaedic surgeons reviewed the arthroscopic results. In future studies, clinical and radiological outcomes after meniscectomy or root repair for each tear type should be investigated.
Conclusion
Our study introduces a new classification based on the tear gap that can concisely describe a degenerative MMPRT. The classification system demonstrated that a higher tear type (increasing displacement of the tear gap in arthroscopic surgery) is associated with higher meniscal extrusion, severe chondral wear, and greater severity of arthritis.
Footnotes
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the institutional review board of Asan Medical Center, Seoul, Republic of Korea.
References
- 1. Ahn JH, Jeong HJ, Lee YS, et al. Comparison between conservative treatment and arthroscopic pull-out repair of the medial meniscus root tear and analysis of prognostic factors for the determination of repair indication. Arch Orthop Trauma Surg. 2015;135(9):1265–1276. [DOI] [PubMed] [Google Scholar]
- 2. Bin SI, Jeong TW, Kim SJ, Lee DH. A new arthroscopic classification of degenerative medial meniscus root tear that correlates with meniscus extrusion on magnetic resonance imaging. Knee. 2016;23(2):246–250. [DOI] [PubMed] [Google Scholar]
- 3. Bin SI, Kim JM, Shin SJ. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20(4):373–378. [DOI] [PubMed] [Google Scholar]
- 4. Bin S-I, Lee S-H, Kim C-W, Kim T-H, Lee D-H. Results of arthroscopic medial meniscectomy in patients with grade IV osteoarthritis of the medial compartment. Arthroscopy. 2008;24(3):264–268. [DOI] [PubMed] [Google Scholar]
- 5. Chan WP, Huang GS, Hsu SM, Chang YC, Ho WP. Radiographic joint space narrowing in osteoarthritis of the knee: relationship to meniscal tears and duration of pain. Skeletal Radiol. 2008;37(10):917–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chung KS, Ha JK, Ra HJ, Nam GW, Kim JG. Pullout fixation of posterior medial meniscus root tears: correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45(1):42–49. [DOI] [PubMed] [Google Scholar]
- 7. Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23. [DOI] [PubMed] [Google Scholar]
- 8. Feucht MJ, Kuhle J, Bode G, et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31(9):1808–1816. [DOI] [PubMed] [Google Scholar]
- 9. Furumatsu T, Kamatsuki Y, Fujii M, et al. Medial meniscus extrusion correlates with disease duration of the sudden symptomatic medial meniscus posterior root tear. Orthop Traumatol Surg Res. 2017;103(8):1179–1182. [DOI] [PubMed] [Google Scholar]
- 10. Habata T, Uematsu K, Hattori K, Takakura Y, Fujisawa Y. Clinical features of the posterior horn tear in the medial meniscus. Arch Orthop Trauma Surg. 2004;124(9):642–645. [DOI] [PubMed] [Google Scholar]
- 11. Hein CN, Deperio JG, Ehrensberger MT, Marzo JM. Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee. 2011;18(3):189–192. [DOI] [PubMed] [Google Scholar]
- 12. Hwang BY, Kim SJ, Lee SW, et al. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40(7):1606–1610. [DOI] [PubMed] [Google Scholar]
- 13. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kim JG, Lee SY, Chay S, Lim HC, Bae JH. Arthroscopic meniscectomy for medial meniscus horizontal cleavage tears in patients under age 45. Knee Surg Relat Res. 2016;28(3):225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kim JG, Lee YS, Bae TS, et al. Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2121–2125. [DOI] [PubMed] [Google Scholar]
- 16. Kim J-H, Chung J-H, Lee D-H, Lee Y-S, Kim J-R, Ryu K-J. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644–1653. [DOI] [PubMed] [Google Scholar]
- 17. Kim SB, Ha JK, Lee SW, et al. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27(3):346–354. [DOI] [PubMed] [Google Scholar]
- 18. Kim YM, Joo YB, Noh CK, Park IY. The optimal suture site for the repair of posterior horn root tears: biomechanical evaluation of pullout strength in porcine menisci. Knee Surg Relat Res. 2016;28(2):147–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Krych AJ, Johnson NR, Mohan R, Dahm DL, Levy BA, Stuart MJ. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1117–1122. [DOI] [PubMed] [Google Scholar]
- 20. Krych AJ, Reardon PJ, Johnson NR, et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):383–389. [DOI] [PubMed] [Google Scholar]
- 21. LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–369. [DOI] [PubMed] [Google Scholar]
- 22. Lee DH, Lee BS, Kim JM, et al. Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):222–229. [DOI] [PubMed] [Google Scholar]
- 23. Lee DW, Ha JK, Kim JG. Medial meniscus posterior root tear: a comprehensive review. Knee Surg Relat Res. 2014;26(3):125–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951–958. [DOI] [PubMed] [Google Scholar]
- 25. Outerbridge RE. Further studies on the etiology of chondromalacia patellae. J Bone Joint Surg Br. 1964;46:179–190. [PubMed] [Google Scholar]
- 26. Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):849–854. [DOI] [PubMed] [Google Scholar]
- 27. Papalia R, Vasta S, Franceschi F, D’Adamio S, Maffulli N, Denaro V. Meniscal root tears: from basic science to ultimate surgery. Br Med Bull. 2013;106(1):91–115. [DOI] [PubMed] [Google Scholar]
- 28. Raynauld JP, Martel-Pelletier J, Berthiaume MJ, et al. Long term evaluation of disease progression through the quantitative magnetic resonance imaging of symptomatic knee osteoarthritis patients: correlation with clinical symptoms and radiographic changes. Arthritis Res Ther. 2006;8(1):R21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Seo H-S, Lee S-C, Jung K-A. Second-look arthroscopic findings after repairs of posterior root tears of the medial meniscus. Am J Sports Med. 2010;39(1):99–107. [DOI] [PubMed] [Google Scholar]
- 30. Sheehy L, Felson D, Zhang Y, et al. Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study. Osteoarthritis Cartilage. 2011;19(1):58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM. Meniscal movement: an in-vivo study using dynamic MRI. J Bone Joint Surg Br. 1999;81(1):37–41. [DOI] [PubMed] [Google Scholar]
- 32. Villegas DF, Hansen TA, Liu DF, Donahue TL. A quantitative study of the microstructure and biochemistry of the medial meniscal horn attachments. Ann Biomed Eng. 2008;36(1):123–131. [DOI] [PubMed] [Google Scholar]