Abstract
Purpose
To report a case of acute syphilitic posterior placoid chorioretinopathy (ASPPC) that demonstrated partial resolution with immunosuppressive therapy secondary to a misdiagnosis as Behçet's disease followed by a relapse which was successfully treated with the appropriate treatment.
Observations
A 34-year-old female patient presented to our service with complaints of decreased vision in the left eye (OS). She initially developed similar symptoms seven months prior to presentation and was diagnosed as Behçet's disease based on the clinical picture of papillitis, vasculitis and placoid chorioretinitis in the posterior pole of OS. She was started on daily oral prednisone 60 mg and weekly methotrexate 10mg by her rheumatologist. The patient's ocular symptoms improved one month prior to presentation with resolution of the placoid lesion but persistence of vasculitis and papillitis. At that time, the dose of the prednisone was decreased to 30 mg which resulted in a relapse of the placoid chorioretinal lesions and worsened visual acuity at the time of presentation to us. Extensive laboratory workup demonstrated positive serology for syphilis. A diagnosis of syphilitic placoid chorioretinitis was made and the patient was treated with intravenous penicillin G for 2 weeks. The vitritis, papillitis, and placoid chorioretinitis resolved along with improvement in vision following the treatment.
Conclusions and importance
Ocular findings in syphilis are heterogeneous and may mimic variety of ocular diseases. ASPPC is a rare ocular manifestation of syphilis and its natural course and underlying pathophysiology is not well understood. However, irrespective of the underlying mechanism of the disease, all patients with ASPPC should receive treatment to prevent recurrence and long-term functional damage.
Keywords: Uveitis, Syphilis, Acute syphilitic posterior placoid chorioretinopathy, Immunosuppression
1. Introduction
Syphilis is a sexually transmitted, systemic infection caused by the Gram-negative spirochete Treponema pallidum. It can affect any organ in the body, including the eyes. Known as the ¨great imitator¨, syphilis has a wide variety of ocular presentations such as anterior uveitis, intermediate uveitis, interstitial keratitis, chorioretinitis, retinal vasculitis, retinitis, perineuritis, papillitis, retrobulbar neuritis, optic atrophy, and optic nerve gumma.1,2 Therefore, it is recommended to test every patient with ocular inflammation for syphilis.1,2
Since non-specific treponemal test such as venereal disease research laboratory (VDRL) test and rapid plasma reagin (RPR) test normalize during the latent and tertiary stages, testing for syphilis should include both non-specific and specific treponemal tests such as fluorescent treponemal antibody absorption (FTA-ABS) and the micro-hemagglutination assay for T. pallidum (MHA-TP).3
Acute syphilitic posterior placoid chorioretinopathy (ASPPC) is a rare ocular manifestation of syphilis that was first described by Gass et al.4,5 It is characterized by the presence of one or more yellowish placoid retinal lesions that are typically present in the macula. However, the natural course of ASPPC is not well understood.6
In the index report, we describe a case of ASPPC that demonstrated partial resolution with immunosuppressive therapy secondary to a misdiagnosis as Behçet's disease followed by a relapse which was successfully treated with the appropriate anti-infectious treatment.
2. Case report
A 34-year-old female patient was admitted to our service with complaints of pain and blurriness of vision in the left eye (OS) for 10 days.
On further exploration of her past ocular history, she had first developed similar symptoms in OS seven months ago. She was presumably diagnosed with Behçet's disease because of the presence of concomitant oral and genital ulcers and cutaneous lesions in palms and soles. She was started on oral prednisone 60 mg daily along with oral methotrexate 10 mg weekly by her rheumatologist. Her ocular signs and symptoms improved one month prior to presentation to our service and therefore, the dose of oral prednisone was decreased to 30 mg per day by the rheumatologist. However, her symptoms returned and the patient was referred to us for further evaluation.
On ocular examination, the best corrected visual acuity (BCVA) was 20/20 in right eye (OD) and 20/80 in OS. The Amsler test showed micropsia in OS and was normal in OD. Slit-lamp examination demonstrated 1 + anterior chamber cells and 3 + vitreous cells in OS. Dilated fundus examination revealed exudative retinal detachment and extensive area of chorioretinitis with vitritis and superficial retinal precipitates in OS (Fig. 1). These findings appeared more active compared to those documented in medical records and photographs taken seven months ago when she presented with large yellowish placoid macular lesions with papillitis and vasculitis as seen on fluorescein angiography (FA) (Fig. 2). The retinal lesions resolved a month before the presentation with residual retinal pigment epithelial changes; however, there was persistence of papillitis and vasculitis (Fig. 3). The biomicroscopy and fundus examination of the OD were unremarkable.
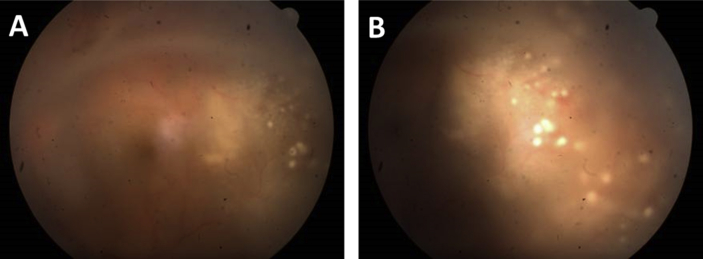
Fig. 1.
Color fundus photograph of the left eye (A and B) at the time of presentation to our service demonstrating severe vitritis. Additionally, a yellowish white placoid lesion can be seen temporal to the fovea (A) with surrounding serous retinal detachment and superficial retinal precipitates (B). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
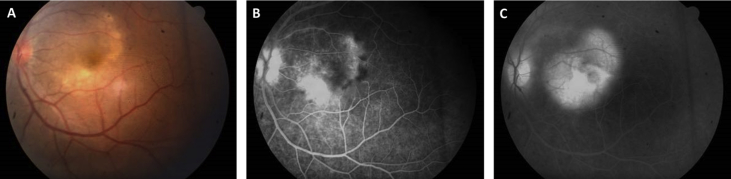
Fig. 2.
A) Color fundus photograph of the left eye 7 months prior to presentation to our clinic demonstrates 1 + vitreous haze and a large yellowish white placoid lesion in the posterior pole. Fluorescein angiogram of the left eye in: B) mid-late phase shows hyperfluorescent optic disc suggestive of papillitis. Additionally, the lesion appears hyperfluorescent secondary to leakage with surrounding vascular leakage suggestive of vasculitis. C) late phase shows progressive increase in leakage in the area of the lesion along with papillitis and vasculitis. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
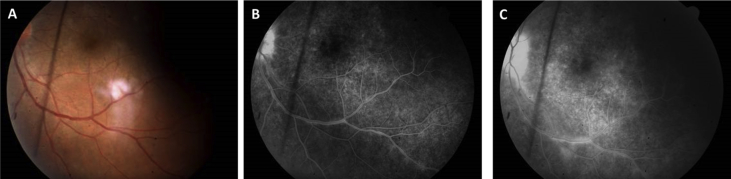
Fig. 3.
A) Color fundus photograph of the left eye 1 month prior to presentation to our clinic and after 6 months of treatment with oral prednisolone and methotraxate. There is resolution of the placoid lesion. Fluorescein angiogram of the left eye in B) in mid-late phase demonstrates absence of the placoid lesion with residual retinal pigment epithelial alterations. However, there is presence to persistent papillitis and vasculitis which is also evident in the late phase (C). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Various laboratory tests including complete blood count, fasting blood glucose level, blood urea nitrogen, creatinine, HIV antibody, Hepatitis B and C serology, Bartonella IgM/IgG, Toxoplasma IgM/IgG, anti-nuclear antibodies had been performed in the past and were within normal limits. In our clinics, we repeated the laboratory tests with the addition of VDRL and FTA-ABS tests for syphilis as a possible etiology. Both tests for syphilis yielded positive results. The patient also underwent a lumbar puncture and cerebrospinal fluid was negative for VDRL.
Upon the diagnosis of syphilis, she was treated with 4 million units of intravenous penicillin G every 4 hours for 2 weeks. Her steroid therapy was discontinued. After the completion of intravenous penicillin G treatment, her symptoms improved. On ocular examination, BCVA demonstrated improvement to 20/25 in OS. Slit lamp examination demonstrated a decrease in the anterior chamber cells to +0.5 in OS. Dilated fundus examination showed complete resolution of chorioretinitis and improvement of vitreous haze in OS (Fig. 4).
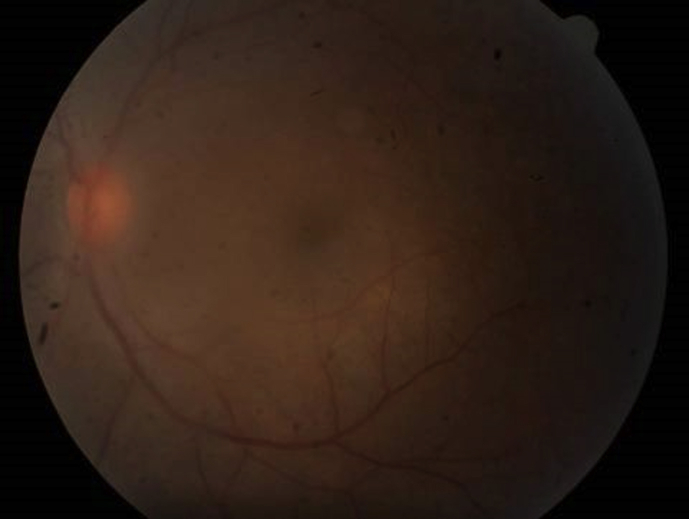
Fig. 4.
A) Color fundus photograph of the left eye after receiving treatment with Penicillin G for two weeks demonstrates resolution of the placoid lesion with 1 + vitreous haze and focal retinal pigment epithelial atrophy. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
3. Discussion
Syphilis is a sexually transmitted disease caused by the spirochete Treponema pallidum. It is colloquially known as ‘the great imitator’ for its ability to mimic many diseases due to its extensive range of clinical manifestations.7 Therefore, a high index of clinical suspicion and a low threshold for serological testing can help with early detection and treatment of the disease, allowing us to reverse retinal changes and prevent permanent damage.8 Posterior segment manifestations of ocular syphilis can include, among others, superficial retinal precipitates, exudative retinal detachment, acute syphilitic placoid posterior chorioretinopathy, papillitis, vasculitis, neuroretinitis, chorioretinitis, and retinitis.9,10
ASPPC is a rare ocular manifestation of syphilis and its natural course is not well known.4, 5, 6,11 It is characterized by the development of a placoid macular deposit in the outer retina.12 Furthermore, the ocular disease can be accompanied by central nervous system and/or mucocutaneous abnormalities, which can mimic other systemic diseases and complicate the diagnosis.
The underlying pathophysiology of ASPPC is not very well understood. Similar to our report, it has been documented in immunocompetent patients. Franco et al. and Ji et al. reported findings of ASPPC in immunocompetent patients with spontaneous resolution without receiving any therapy.4,5 On the other hand, our patient was initially treated with immunosuppressive therapy which is often not a suggested therapy for syphilis. Surprisingly, in contrast to the general infectious behavior of worsening with immunosuppression, our case demonstrated improvement in the visual and anatomical outcome as the placoid chorioretinal lesion resolved after steroid therapy. The vasculitis and papillitis, however, persisted. Such treatment outcomes underscore the thought that maybe the underlying mechanism leading to the chorioretinal lesions seen in ASPPC is different than the vasculitis and papillitis seen in syphilitic uveitis which has been thought previously.13,14 Additionally, unlike other reports of ASPPC, there was a recurrence of the lesion with a decrease in the dose of the immunosuppressive agents. This clinical course in our case suggests an autoimmune component in the pathophysiology of ASPPC. De Souza et al. suggested a possible role of immune-complex mediated hypersensitivity as the underlying mechanism of ASPPC.13 Similarly, Brito et al. demonstrated an increase in the level of anti-beta 2 glycoprotein antibodies in a subject with ASPPC.14 They suggested that these antibodies can potentially lead to choroidal thrombosis and impairment of retinal pigment epithelium and photoreceptor function due to their propensity for cardiolipin which is normally involved in anticoagulation and mitochondrial metabolism. In addition, Sahin et al. demonstrated the use and benefits of methotrexate in the management of ocular syphilis, which further highlights the inflammatory component of the disease.15
On the other hand, some of the studies have suggested immunosuppression as a major stimulator of ASPPC. Aranda et al. documented a case with ASPPC in an HIV patient which resolved spontaneously as the immune system recovered following anti-retroviral therapy.12 Zamani et al. reported another case of ASPPC which presented secondary to immunosuppression following corticosteroid therapy.16 Furthermore, Erol et al. and Song et al. published cases of ASPPC following local intravitreal triamcinolone injections suggesting the role of local immunomodulation in the pathogenesis of the disease.17,18 In contrast to the findings of these reports, our patient received corticosteroid and methotrexate for 7 months and demonstrated no worsening of the disease.
Based on these contrasting evidences published in the literature and what we noted in our patient, we suggest that the ASPPC lesions may be a single clinical manifestation of two different underlying pathophysiological pathways. These lesions can either result from direct attack by the spirochete secondary to reactivation from immunosuppression or as a consequence of indirect immune-mediated hypersensitivity.
Despite the complex underlying mechanisms leading to ASPPC, there should be a low threshold to test for syphilis in patients presenting with chorioretinitis. It is important to recognize that the chorioretinal lesions of ASPPC may appear similar to other ocular autoimmune diseases as was seen in our case which was initially misinterpreted and treated as Behçet's disease. Furthermore, all the patients with positive serology for syphilis, even with spontaneous resolution of the chorioretinal lesions, should receive the appropriate anti-infectious treatment for the underlying infection. Otherwise, the ocular syphilis can lead to recurrence of ASPPC as we noted or can lead to a more permanent functional damage via other syphilitic manifestations in the eye as was seen in eyes in which the diagnosis was delayed.19,20
4. Conclusion
ASPPC is a rare ocular manifestation of syphilis and its natural course is not well understood. However, it may have both autoimmune as well as infectious basis in its pathophysiology. Irrespective of the pathogenesis, all patients with ASPPC should receive anti-infectious treatment to treat the underlying disease to avoid recurrence of the disease and permanent functional damage.
Patient consent
Consent to publish this case report has been obtained from the patient in writing.
Conflicts of interest
QDN is a recipient of a Physician Scientist Award from Research to Prevent Blindness, New York, NY, and serves on the Scientific Advisory Board for AbbVie, Bayer, Genentech, Regeneron, and Santen, among others. QDN also chaired the Steering Committee for the RISE and RIDE studies and was on the Steering Committee for the VISTA Study, and other studies sponsored by Genentech and Regeneron.
MSO, MH, AS have no financial disclosures.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgement
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2019.03.002.
Abbreviations
- ASPPC
Acute Syphilitic Posterior Placoid Chorioretinopathy
- BCVA
Best Corrected Visual Acuity
- FA
Fluorescein Angiography
- FTA-ABS
Fluorescent Treponemal Antibody Absorption
- MHA-TP
Micro-Hemagglutination Assay for T. pallidum
- OD
Right Eye
- OS
Left Eye
- RPR
Rapid Plasma Reagin
- VDRL
Venereal Disease Research Laboratory
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Pichi F., Ciardella A.P., Cunningham E.T., Jr. Spectral domain optical coherence tomography findings in patients with acute syphilitic posterior placoid chorioretinopathy. Retina (Philadelphia, Pa) 2014;34(2):373–384. doi: 10.1097/IAE.0b013e3182993f11. [DOI] [PubMed] [Google Scholar]
- 2.Loureiro M.M., Sepulveda P.A. Bilateral chorioretinitis as syphilis presentation: multimodal characterization and therapy response. J Clin Diagn Res: JCDR. 2016;10(9):Nd01–nd02. doi: 10.7860/JCDR/2016/19359.8406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sahin O., Ziaei A. Clinical and laboratory characteristics of ocular syphilis, co-infection, and therapy response. Clin Ophthalmol. 2016;10:13–28. doi: 10.2147/OPTH.S94376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ji Y.S., Yang J.M., Park S.W. Early resolved acute syphilitic posterior placoid chorioretinitis. Optom Vis Sci: Offic Publ Am Acad Optom. 2015;92(4 Suppl 1):S55–S58. doi: 10.1097/OPX.0000000000000531. [DOI] [PubMed] [Google Scholar]
- 5.Gass J.D., Braunstein R.A., Chenoweth R.G. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990;97(10):1288–1297. doi: 10.1016/s0161-6420(90)32418-1. [DOI] [PubMed] [Google Scholar]
- 6.Eandi C.M., Neri P., Adelman R.A., Yannuzzi L.A., Cunningham E.T., Jr. Acute syphilitic posterior placoid chorioretinitis: report of a case series and comprehensive review of the literature. Retina (Philadelphia, Pa) 2012;32(9):1915–1941. doi: 10.1097/IAE.0b013e31825f3851. [DOI] [PubMed] [Google Scholar]
- 7.Dutta Majumder P., Chen E.J., Shah J. Ocular syphilis: an update. Ocul Immunol Inflamm. 2017:1–9. doi: 10.1080/09273948.2017.1371765. [DOI] [PubMed] [Google Scholar]
- 8.Wells J., Wood C., Sukthankar A., Jones N.P. Ocular syphilis: the re-establishment of an old disease. Eye. 2018;32(1):99–103. doi: 10.1038/eye.2017.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu E.X., Geraets R.L., Dodds E.M. Superficial retinal precipitates in patients with syphilitic retinitis. Retina (Philadelphia, Pa) 2010;30(7):1135–1143. doi: 10.1097/IAE.0b013e3181cdf3ae. [DOI] [PubMed] [Google Scholar]
- 10.Curi A.L., Sarraf D., Cunningham E.T., Jr. Multimodal imaging of syphilitic multifocal retinitis. Retin Cases Brief Rep. 2015;9(4):277–280. doi: 10.1097/ICB.0000000000000186. [DOI] [PubMed] [Google Scholar]
- 11.Franco M., Nogueira V. Severe acute syphilitic posterior placoid chorioretinitis with complete spontaneous resolution: the natural course. GMS Ophthalmol Cases. 2016;6 doi: 10.3205/oc000039. Doc02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aranda S., Amer R. Sequential spontaneous resolution of acute syphilitic posterior placoid chorioretinitis. Eur J Ophthalmol. 2015;25(3):263–265. doi: 10.5301/ejo.5000530. [DOI] [PubMed] [Google Scholar]
- 13.de Souza E.C., Jalkh A.E., Trempe C.L., Cunha S., Schepens C.L. Unusual central chorioretinitis as the first manifestation of early secondary syphilis. Am J Ophthalmol. 1988;105(3):271–276. doi: 10.1016/0002-9394(88)90009-8. [DOI] [PubMed] [Google Scholar]
- 14.Brito P., Penas S., Carneiro A., Palmares J., Reis F.F. Spectral-domain optical coherence tomography features of acute syphilitic posterior placoid chorioretinitis: the role of autoimmune response in pathogenesis. Case Rep Ophthalmol. 2011;2(1):39–44. doi: 10.1159/000324086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sahin O., Ziaei A. The role of methotrexate in resolving ocular inflammation after specific therapy for presumed latent syphilitic uveitis and presumed tuberculosis-related uveitis. Retina (Philadelphia, Pa) 2014;34(7):1451–1459. doi: 10.1097/IAE.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 16.Zamani M., Garfinkel R.A. Corticosteroid-induced modulation of acute syphilitic posterior placoid chorioretinitis. Am J Ophthalmol. 2003;135(6):891–894. doi: 10.1016/s0002-9394(02)02160-8. [DOI] [PubMed] [Google Scholar]
- 17.Erol N., Topbas S. Acute syphilitic posterior placoid chorioretinitis after an intravitreal triamcinolone acetonide injection. Acta Ophthalmol Scand. 2006;84(3):435. doi: 10.1111/j.1600-0420.2005.00641.x. [DOI] [PubMed] [Google Scholar]
- 18.Song J.H., Hong Y.T., Kwon O.W. Acute syphilitic posterior placoid chorioretinitis following intravitreal triamcinolone acetonide injection. Graefes Arch Clin Exp Ophthalmol. 2008;246(12):1775–1778. doi: 10.1007/s00417-008-0928-y. [DOI] [PubMed] [Google Scholar]
- 19.Park J.H., Joe S.G., Yoon Y.H. Delayed diagnosis of ocular syphilis that manifested as retinal vasculitis and acute posterior multifocal placoid epitheliopathy. Indian J Ophthalmol. 2013;61(11):676–678. doi: 10.4103/0301-4738.119415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Y., Yang L., Zhang Z.L. [Panuveitis with oral and genital ulcer misdiagnosed as Behcet's disease: two cases report and literature review] Beijing Da Xue Xue Bao Yi Xue Ban. 2016;48(5):910–914. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.