Abstract
Introduction
Sepsis results from a dysregulated host response to an infection that is associated with an imbalance between pro- and anti-inflammatory cytokines. This imbalance is hypothesized to be a driver of patient mortality. Certain autoimmune diseases modulate the expression of cytokines involved in the pathophysiology of sepsis. However, the outcomes of patients with autoimmune disease who develop sepsis have not been studied in detail. The objective of this study is to determine whether patients with autoimmune diseases have different sepsis outcomes than patients without these comorbidities.
Methods
Using the Multiparameter Intelligent Monitoring in Intensive Care III database (v. 1.4) which contains retrospective clinical data for over 50,000 adult ICU stays, we compared 30-day mortality risk for sepsis patients with and without autoimmune disease. We used logistic regression models to control for known confounders, including demographics, disease severity, and immunomodulation medications. We used mediation analysis to evaluate how the chronic use of immunomodulation medications affects the relationship between autoimmune disease and 30-day mortality.
Results
Our study found a statistically significant 27.00% reduction in the 30-day mortality risk associated with autoimmune disease presence. This association was found to be the strongest (OR 0.71, 95% CI 0.54–0.93, P = 0.014) among patients with septic shock. The autoimmune disease-30-day mortality association was not mediated through the chronic use of immunomodulation medications (indirect effect OR 1.07, 95% CI 1.01–1.13, P = 0.020).
Conclusions
We demonstrated that autoimmune diseases are associated with a lower 30-day mortality risk in sepsis. Our findings suggest that autoimmune diseases affect 30-day mortality through a mechanism unrelated to the chronic use of immunomodulation medications. Since this study was conducted within a single study center, research using data from other medical centers will provide further validation.
Electronic supplementary material
The online version of this article (10.1186/s13054-019-2357-1) contains supplementary material, which is available to authorized users.
Keywords: (3–10)-sepsis, Mortality, Autoimmune disease, Large observational database, MIMIC III, Mediation, Disease-modifying antirheumatic drugs
Introduction
Sepsis is a systemic inflammatory response to an infection that can lead to organ failure and death. Severe sepsis accounts for around 10.00% of all intensive care unit (ICU) admissions in the USA, and mortality rates are commonly reported between 28.00 and 50.00% [1, 2]. Sepsis outcomes and mortality have been a major focus of research over the last few years as it pertains to quality improvement and health outcomes.
Sepsis results from a dysregulated host response to an infection that is associated with an imbalance between pro- and anti-inflammatory cytokines [3]. The overactive pro-inflammatory response has been considered a primary driver of sepsis mortality; however, therapies targeting this response have not been successful in human trials [4]. Given these failures, new hypotheses have been proposed which highlight the dysregulation of both pro- and anti-inflammatory pathways [5].
Autoimmune diseases are a group of diseases that arise from an abnormal immune response of the host against substances and tissues normally present in the body. Certain autoimmune diseases have been associated with the over- or underexpression of pro- or anti-inflammatory cytokines involved in the pathophysiology of sepsis [3, 6–12]. Variations in cytokine levels may affect sepsis survival among autoimmune patients. However, there is little information regarding the physiology and outcomes of sepsis in patients with autoimmune diseases.
Examining sepsis outcomes among patients with autoimmune diseases may yield new insights into how the immune system responds to infections given different baseline cytokine levels [13]. The effect of autoimmune disease has been speculated to lead to worse clinical outcomes among patients diagnosed with sepsis as a result of the modulated immune response associated with autoimmune diseases and their treatment [14–17]. However, recent research indicates the contrary, where in certain cases patients with autoimmune diseases may have better sepsis-related clinical outcomes [13]. Yet the underlying cause of these improved clinical outcomes remains unknown.
The objective of this study is to determine the effect of autoimmune disease on sepsis outcomes. We compare 30-day mortality rates for sepsis patients with autoimmune disease and without autoimmune disease, controlling for known confounders.
Methods
Data source
This study used the publicly available Multiparameter Intelligent Monitoring in Intensive Care (MIMIC) III database version 1.4 [18]. MIMIC III contains de-identified clinical data for over 50,000 adult ICU stays at Beth Israel Deaconess Medical Center in Boston, MA, from 2001 to 2012 [18], and was jointly developed by the Massachusetts Institute of Technology, Phillips Healthcare, and Beth Israel Deaconess Medical Center. Any researcher who adheres to the data use requirements is permitted to use the database.
Patient population
The primary study population consists of adult ICU patients with sepsis. We identified a sepsis population according to the Martin criteria, a widely used approach for identifying sepsis in administrative health data [19]. We identified a septic shock subpopulation—a cohort of patients meeting both sepsis and hypotension criteria indicative of substantial medical distress. We defined hypotension as three consecutive mean arterial blood pressure readings below 65 mmHg in a 30-min period or at least one dose of vasopressors during the ICU stay [20].
All patients were required to have at least 24 h of ICU data, and we selected the last ICU stay meeting these criteria for each patient. We identified 6200 patients in the database meeting the sepsis inclusion criterion and 4190 meeting the septic shock criteria.
Predictor and outcome variables
Throughout this study, autoimmune disease refers to a set of related conditions, defined using ICD-9-CM diagnosis codes and free text analysis of the patient discharge summaries (Table 1). These conditions were selected based upon their association with the over- or underexpression of pro- or anti-inflammatory cytokines involved in the pathophysiology of sepsis [3, 6–12] (Additional file 1: Table S1). In total, we identified 496 septic patients with autoimmune disease, with rheumatoid arthritis and Crohn’s disease being the most prevalent conditions.
Table 1.
Conditions included in autoimmune definition
| Autoimmune condition | ICD-9-CM | Sepsis | Septic shock |
|---|---|---|---|
| All autoimmune conditions | – | N = 496 | N = 328 |
| Rheumatoid arthritis | 714 | 130 (26.21%) | 92 (28.05%) |
| Crohn’s disease | 555 | 114 (22.98%) | 85 (25.91%) |
| Ulcerative colitis | 556.5, 556.6, 556.8, 556.9 | 86 (17.34%) | 57 (17.38%) |
| Multiple sclerosis | 340 | 64 (12.90%) | 40 (12.20%) |
| Systemic lupus erythematosus | 710.0 | 52 (10.48%) | 40 (12.20%) |
| Ankylosing spondylitis | 720 | 23 (4.64%) | 16 (4.88%) |
| Psoriatic arthritis | 696.0 | 20 (4.03%) | 11 (3.35%) |
| Myasthenia gravis | 358.0 | 16 (3.23%) | 9 (2.74%) |
| Inflammatory myopathies | 710.4, 710.3, 359.71 | 12 (2.41%) | 6 (1.83%) |
| Polymyositis | 710.4 | 9 (1.80%) | 5 (1.52%) |
| Dermatomyositis | 710.3 | 1 (0.20%) | 1 (0.30%) |
| Inclusion body myositis | 359.71 | 2 (0.40%) | 0 (0.00%) |
| Giant cell arteritis | 446.5 | 11 (2.22%) | 4 (1.22%) |
| Systemic sclerosis | 710.1 | 10 (2.01%) | 7 (2.13%) |
| Scleroderma | 701.1 | 9 (1.81%) | 7 (2.13%) |
For each patient in the study, we extracted several confounding factors from data stored in the MIMIC III database. They included age, race, sex, infection site (pulmonary or non-pulmonary), documented bacteremia, Sequential Organ Failure Assessment (SOFA) score at ICU admission, Elixhauser comorbidity index at hospital admission, ICU care unit, and pre-admission chronic conventional-synthetic and biologic disease-modifying antirheumatic drug (DMARD; Additional file 2: Table S2) and prednisone usage. SOFA includes information about the condition of a patient’s respiratory, renal, and cardiovascular systems, among others, and has been found to be a strong predictor of prognosis for ICU patients with sepsis [21]. The Elixhauser comorbidity index is a measure of disease burden that was specifically developed for use with administrative health data [22].
The primary outcome of interest in this study is patients’ 30-day mortality. Thirty-day mortality is based on data from the Social Security Death Index and reflects deaths within a 30-day window after the patient’s hospital discharge date as well as in-hospital deaths.
Statistical analysis and modeling
In the primary analysis, we estimated relative risks with odds ratios (OR) and 95% confidence intervals (CI) for patients with autoimmune disease, compared with patients without autoimmune disease using a multivariable logistic regression model [23]. ORs were adjusted for potential confounders using two approaches: (1) all potential confounders were included in the final model and (2) only potential confounders that meaningfully affected model estimates were included in the final model. In the second approach, individual factors were added into the model one at a time, and if a variable changed the model estimate by more than 10.00%, it was retained in the final model [24, 25]. Factors that were considered as potential confounders included the following: age, race (non-Hispanic white, non-Hispanic black, Hispanic, Asian/Pacific Islander, other, missing), infection site, documented bacteremia, SOFA score, Elixhauser comorbidity index (and the individual comorbidities included in the index), ICU care unit, and chronic pre-admission DMARD or prednisone use. We also performed a survival analysis for the five most frequently reported autoimmune diseases (rheumatoid arthritis, Crohn’s disease, ulcerative colitis, multiple sclerosis, and systemic lupus erythematosus). In this analysis, we used Cox Proportional-Hazards models [24, 25] with both confounder adjustment approaches (discussed above) and report the ratio of the hazard functions, or hazards ratio (HR). To further evaluate study results, we performed additional analyses where we stratified results by the over- and underexpression of sepsis-related cytokines, assessed the joint effect of autoimmune disease and chronic DMARD or prednisone use on 30-day mortality, and performed all aforementioned analyses using the septic shock cohort.
Furthermore, for both cohorts, we performed a mediation analysis treating chronic pre-admission DMARD or prednisone usage as a potential mediator [26]. Both medications are used to treat autoimmune diseases and are strongly associated with autoimmune disease presence (DMARD OR 11.45, 95% CI 8.16–16.07; prednisone OR 4.66, 95% CI 3.67–5.90). Both medications have also been associated with an increased risk for mortality [27, 28]. The mediation analysis assumes a causal relationship between the exposure (autoimmune diseases) and mediator (chronic DMARD or prednisone usage) variables which in turn may affect the outcome (30-day mortality). Mediation analysis clarifies the nature of the relationship between the exposure and mediator to better understand the pathways by which the exposure potentially affects the outcome [26, 29]. We used the mediation analysis to estimate the direct effect of autoimmune disease on 30-day mortality and the effect of autoimmune disease on 30-day mortality that is mediated by chronic DMARD and prednisone use (indirect effect) [26].
We performed all statistical analyses using the R programming language version 3.3.3 [30] and SAS 9.4 software (SAS Institute, Inc., Cary, North Carolina) [31].
Results
Study population
The study cohort consisted of 6200 patients with sepsis. Of these, 496 (8.00%) had at least one autoimmune disease. To understand how the autoimmune and non-autoimmune patient populations differed from each other, we evaluated each group’s baseline characteristics (Table 2). Generally, those with an autoimmune disease were more likely to be white, younger, female; had a lower SOFA score; chronically use DMARDs or prednisone; and did not have a reported pulmonary infection.
Table 2.
Baseline characteristics for sepsis patients, stratified by the presence of autoimmune disease
| Autoimmune disease | No autoimmune disease | P value | |
|---|---|---|---|
| Number of patients | 496 | 5704 | |
| Patient outcomes | |||
| 30-day mortality | 26.61% | 34.55% | < 0.001 |
| Patient characteristics | |||
| Age (mean ± SD) | 64.46 ± 14.64 | 66.21 ± 16.48 | 0.012 |
| Sex (% male) | 44.56% | 57.50% | < 0.001 |
| Race | 0.027 | ||
| White, non-Hispanic | 80.04% | 71.49% | |
| Black, non-Hispanic | 7.26% | 9.34% | |
| Hispanic | 2.02% | 3.30% | |
| Asian/Pacific Islander | 1.61% | 3.00% | |
| Other | 2.42% | 2.58% | |
| Unknown | 6.65% | 10.29% | |
| SOFA at admission (mean ± SD) | 5.63 ± 3.67 | 6.50 ± 3.80 | < 0.001 |
| Elixhauser comorbidity index (mean ± SD) | 9.46 ± 7.74 | 9.75 ± 7.83 | 0.411 |
| Infection site (% pulmonary) | 32.06% | 39.00% | 0.003 |
| Documented bacteremia (% yes) | 16.13% | 18.92% | 0.142 |
| Chronic pre-admission DMARD or prednisone use | 56.05% | 19.78% | < 0.001 |
| Chronic prednisone use | 41.73% | 17.36% | |
| Chronic DMARD use | 34.48% | 5.80% | |
| ICU care unit | 0.694 | ||
| MICU | 63.91% | 62.34% | |
| SICU | 21.57% | 21.27% | |
| CCU | 9.88% | 10.64% | |
| CSRU | 4.64% | 5.75% | |
SOFA Sequential Organ Failure Assessment, DMARD disease-modifying antirheumatic drug, ICU intensive care unit, CCU coronary care unit, CSRU cardiac surgery recovery unit, MICU medical intensive care unit, SICU surgical intensive care unit
Association between autoimmune disease presence and mortality
A total of 132 (26.61%) patients with autoimmune disease and 1971 (34.55%) patients without autoimmune disease died either within the hospital or in the 30 days after hospital discharge.
We analyzed the potential confounders (see the subsection “Statistical analysis and modeling” in the “Methods” section) by adding each variable into the model one at a time and evaluating how much the newly added variable affected the model estimate. We performed this analysis to reduce the number of variables within the model and to account only for those that had a meaningful affect (more than 10.00%) on model estimates. In our analysis, the SOFA score was the only variable that met the inclusion criterion for approach 2 (Table 3). Statistically adjusting for individual comorbidities included within the Elixhauser comorbidity index did not meaningfully affect model estimates (Additional file 3: Table S3). After including SOFA score in the final model, we reevaluated each potential confounder, accounting for SOFA score, and found that no other variable met the inclusion criterion (Additional file 4: Table S4). For approach 2, we only statistically adjusted for the SOFA score.
Table 3.
Analysis of the impact of potential confounders of the autoimmune disease-30-day mortality association
| Adjusting for confounders of the association between autoimmune disease and 30-day mortality | OR (95% CI) | P value | Magnitude of confounding |
|---|---|---|---|
| No confounders adjusted (“crude”) | 0.71 (0.58–0.86) | < 0.001 | – |
| Age adjusted | 0.74 (0.60–0.90) | 0.003 | − 4.46% |
| Sex adjusted | 0.71 (0.60–0.86) | < 0.001 | − 0.31% |
| Race adjusted | 0.71 (0.58–0.87) | < 0.001 | − 0.93% |
| Documented bacteremia adjusted | 0.68 (0.56–0.83) | < 0.001 | 4.41% |
| Infection site adjusted | 0.72 (0.56–0.83) | 0.001 | − 1.39% |
| SOFA score adjusted | 0.81 (0.65–1.00) | 0.051 | − 12.34% |
| Elixhauser comorbidity index adjusted | 0.71 (0.57–0.86) | < 0.001 | 0.26% |
| DMARD or prednisone usage adjusted | 0.66 (0.54–0.81) | < 0.001 | 7.58% |
| ICU care unit adjusted | 0.71 (0.58–0.86) | < 0.001 | 0.10% |
Magnitude of confounding = (ORcrude − ORadjusted)/ORadjusted
OR odds ratio, CI confidence interval, SOFA Sequential Organ Failure Assessment, DMARD disease-modifying antirheumatic drug, ICU intensive care unit
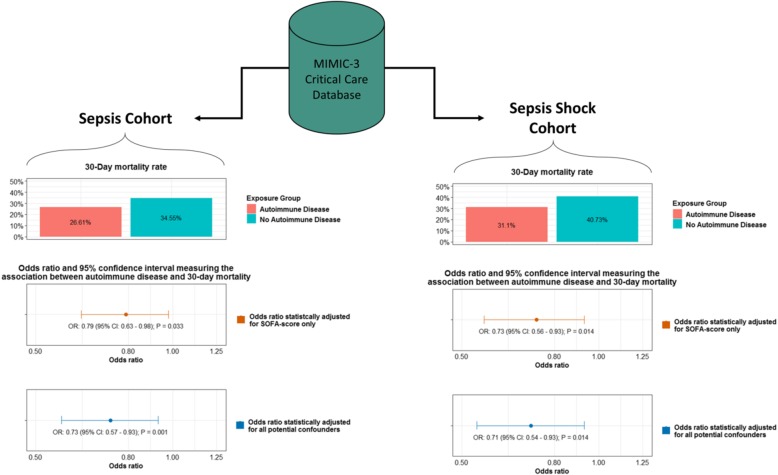
To understand how autoimmune disease presence may influence 30-day mortality, we measured the association between autoimmune disease and 30-day mortality within the sepsis and septic shock cohorts using multivariable logistic regression models (Fig. 1 and Table 4). For the sepsis cohort, controlling for all potential confounders, autoimmune disease was associated with a statistically significant 27.00% decrease in the 30-day mortality risk (OR 0.73, 95% CI 0.57–0.93, P = 0.001). When only SOFA score was adjusted for, we observed a similar statistically significant reduction in the 30-day mortality risk (OR 0.79, 95% CI 0.63–0.98, P = 0.033).
Fig. 1.
Association between autoimmune disease presence and 30-day mortality among sepsis and septic shock patients
Table 4.
Association between autoimmune disease and 30-day mortality according to confounder adjustment strategy
| Association between autoimmune disease and 30-day mortality | Sepsis cohort | Septic shock cohort | ||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| All potential confounders adjusteda | 0.73 (0.57–0.93) | 0.001 | 0.71 (0.54–0.93) | 0.014 |
| SOFA score adjusted | 0.79 (0.63–0.98) | 0.033 | 0.73 (0.56–0.93) | 0.014 |
Sepsis cohort—ICU patients with sepsis as defined by Martin criteria. Septic shock cohort—ICU patients with sepsis as defined by Martin criteria and three consecutive mean arterial blood pressure readings below 65 mmHg in a 30-min period or at least one dose of vasopressors during the ICU stay
OR odds ratio, CI confidence interval, SOFA Sequential Organ Failure Assessment
aOR adjusted for age, sex, race, SOFA score at ICU admission, Elixhauser comorbidity index, pre-admission chronic DMARD or prednisone use, ICU care unit, documented bacteremia, and infection site
For the septic shock cohort, we observed a statistically significant 29.00% (OR 0.71, 95% CI 0.54–0.93, P = 0.014) and 27.00% (OR 0.73, 95% CI 0.56–0.93, P = 0.014) reduction in the 30-day mortality risk for subsequent confounder adjustment strategies.
We performed a survival analysis, using multivariable Cox Proportional-Hazards models, to assess the rate of mortality for the five most frequently reported autoimmune diseases relative to the reference group (those without autoimmune disease). For the sepsis cohort, after statistically adjusting for all potential confounders, we observed a 10.00–55.00% reduction in the 30-day mortality rate (Additional file 5: Table S5). Multiple sclerosis was the only disease where the measured association was statistically significant (HR: 0.45, 95% CI: 0.22–0.89, p = 0.023). For the septic shock cohort, adjusting for all potential confounders, we observed that the five most frequently reported autoimmune diseases were associated with a 10.00–66.00% reduction in the 30-day mortality rate. Once again, only multiple sclerosis was associated with a statistically significant reduction (HR 0.34, 95% CI 0.14–0.82, p = 0.016).
Joint effect of autoimmune disease and chronic DMARD or prednisone use
We evaluated how immunosuppressant medications (DMARDs and prednisone) may modify the association between autoimmune disease and mortality. To do so, we measured the joint effect of autoimmune disease and chronic immunosuppressant use on 30-day mortality. In the sepsis cohort, we observed a non-statistically significant 11.00% reduction in 30-day mortality (OR 0.89, 95% CI 0.65–1.20, P = 0.452) (Table 4) associated with autoimmune disease patients undergoing chronic immunosuppressant therapy. A slightly stronger, yet non-statistically significant, reduction in mortality risk was observed for patients with autoimmune disease who were not on chronic immunosuppressant therapy (OR 0.82, 95% CI 0.58–1.16, P = 0.272). Within the septic shock cohort, we observed a similar non-statistically significant reduction in mortality risk for autoimmune disease patients undergoing chronic immunosuppressant therapy. The protective association was strongest for autoimmune disease patients not on chronic immunosuppressant therapy; however, this association was not statistically significant (OR 0.76, 95% CI 0.52–0.96, P = 0.029). Adjusting for SOFA score alone led to similar conclusions about the joint effect of autoimmune disease and chronic immunosuppressant use.
Effect of autoimmune disease on 30-day mortality mediated through chronic DMARD or prednisone usage
We performed a mediation analysis where we estimated the direct and indirect effects of autoimmune disease on the 30-day mortality risk. In doing so, the mediation analysis allows us to clarify the nature of the relationship between autoimmune disease and chronic use of immunosuppressant medications to understand how autoimmune diseases are associated with mortality risk. Among sepsis patients, we observed statistically significant direct (OR 0.78, 95% CI 0.61–0.98, P = 0.004) and indirect (OR 1.07, 95% CI 1.01–1.13, P = 0.020) effects after adjusting for all confounders (Table 6). Similar direct (OR 0.75, 95% CI 0.57–0.98, P = 0.037) and indirect (OR 1.06, 95% CI 0.99–1.13, P = 0.112) effects were measured among patients in the septic shock cohort. Adjusting for SOFA score alone led to similar conclusions regarding the direct and indirect effects.
Table 6.
Direct and Indirect effects of autoimmune disease on 30-day mortality, mediated through immunomodulation medication use
| Mediation analysis of the effect of autoimmune disease on 30-day mortality | Sepsis cohort | Septic shock cohort | ||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P value | |
| All potential confounders adjusteda | ||||
| Indirect effect | 1.07 (1.01–1.13) | 0.020 | 1.06 (0.99–1.13) | 0.112 |
| Direct effect | 0.78 (0.61–0.98) | 0.004 | 0.75 (0.57–0.98) | 0.037 |
| SOFA adjusted | ||||
| Indirect effect | 1.06 (1.00–1.11) | 0.033 | 1.04 (0.99–1.12) | 0.130 |
| Direct effect | 0.75 (0.60–0.93) | 0.011 | 0.69 (0.53–0.90) | 0.006 |
Sepsis cohort—ICU patients with sepsis defined with Martin criteria. Septic shock cohort—ICU patients with sepsis defined by Martin criteria and three consecutive mean arterial blood pressure readings below 65 mmHg in a 30-min period or at least one dose of vasopressors during the ICU stay
OR odds ratio, CI confidence interval, DMARD disease-modifying antirheumatic drug
aOR adjusted for age, sex, race, SOFA score at ICU admission, Elixhauser comorbidity index, pre-admission chronic DMARD or prednisone use, ICU care unit, documented bacteremia, and infection site
Effect of the cytokine dysregulation on 30-day mortality
We explored additional explanations for the protective effect associated with autoimmune disease by evaluating the autoimmune disease-mortality relationship within the context of over- and underexpression of sepsis-related cytokines (Table 7). Among sepsis cohort patients and adjusting for all potential confounders, the overexpression of pro-inflammatory cytokines interleukin-12 (IL-12) and interferon-γ (INF-γ) was associated with a statistically significant 24.00% and 37.00% reduction in the 30-day mortality risk (IL-12 OR 0.76, 95% CI 0.59–0.99, P = 0.040; INF-γ OR 0.63, 95% CI 0.45–0.89, P = 0.008). We did not observe any statistically significant reduction in the 30-day mortality risk associated with the over- or underexpression of the evaluated anti-inflammatory cytokines.
Table 7.
Association between the dysregulation of cytokines and specific autoimmune diseases
| Pathway | Cytokine dysregulation (based upon literature) | Diseases involved | Sepsis cohort | Septic shock cohort | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | ||||||||
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | ||||
| Pro-inflammatory | Overexpression | IL-1 [8, 9, 12] | Crohn’s disease, ulcerative colitis, inflammatory myopathies*, giant cell arteritis | 0.81 (0.62–1.06) | 0.126 | 0.75 (0.57–0.97) | 0.032 | 0.80 (0.59–1.07) | 0.135 | 0.75 (0.56–1.01) | 0.062 |
| IL-6 [3, 8, 9, 12] | Rheumatoid arthritis, Crohn’s disease, ulcerative colitis, multiple sclerosis, systemic sclerosis, giant cell arteritis | 0.83 (0.68–1.01) | 0.066 | 0.85 (0.70–1.04) | 0.116 | 0.75 (0.60–0.95) | 0.015 | 0.77 (0.62–0.97) | 0.025 | ||
| IL-12 [8, 12] | Crohn’s disease, ulcerative colitis, multiple sclerosis | 0.76 (0.59–0.99) | 0.040 | 0.71 (0.55–0.92) | 0.009 | 0.73 (0.55–0.98) | 0.035 | 0.69 (0.52–0.92) | 0.012 | ||
| INF-y [8, 9, 12] | Crohn’s disease, ulcerative colitis, multiple sclerosis, giant cell arteritis | 0.63 (0.45–0.89) | 0.008 | 0.59 (0.42–0.83) | 0.002 | 0.59 (0.41–0.86) | 0.007 | 0.56 (0.39–0.82) | 0.003 | ||
| TNF-a [3, 8, 9, 12] | Crohn’s disease, ulcerative colitis, rheumatoid arthritis, psoriatic arthritis, multiple sclerosis, systemic sclerosis, scleroderma, inflammatory myopathies*, giant cell arteritis | 0.84 (0.69–1.02) | 0.077 | 0.86 (0.71–1.04) | 0.120 | 0.77 (0.61–0.96) | 0.020 | 0.79 (0.63–0.98) | 0.032 | ||
| Underexpression | IL-12 [8, 11] | Myasthenia gravis | 0.31 (0.08–1.22) | 0.094 | 0.37 (0.09–1.48) | 0.159 | 0.24 (0.03–1.67) | 0.148 | 0.27 (0.04–1.91) | 0.189 | |
| INF-y [8, 12] | Systemic lupus erythematosus | 0.88 (0.52–1.51) | 0.645 | 0.75 (0.45–1.28) | 0.294 | 0.90 (0.53–1.55) | 0.708 | 0.79 (0.47–1.34) | 0.389 | ||
| TNF-a [8, 9] | Systemic lupus erythematosus and ankylosing spondylitis | 0.83 (0.52–1.33) | 0.443 | 0.71 (0.44–1.13) | 0.145 | 0.86 (0.54–1.39) | 0.549 | 0.75 (0.47–1.20) | 0.236 | ||
| Anti-inflammatory | Overexpression | IL-4 [3, 8, 12] | Systemic lupus erythematosus, systemic sclerosis, scleroderma | 1.02 (0.64–1.62) | 0.941 | 0.88 (0.56–1.38) | 0.571 | 1.03 (0.64–1.66) | 0.908 | 0.92 (0.58–1.46) | 0.712 |
| IL-10 [9, 12] | Crohn’s disease, ulcerative colitis, systemic lupus e | 0.85 (0.66–1.10) | 0.220 | 0.77 (0.60–0.99) | 0.039 | 0.85 (0.65–1.11) | 0.239 | 0.79 (0.61–1.03) | 0.083 | ||
| TGF-B [12] | Inflammatory myopathies* | 0.62 (0.15–2.49) | 0.500 | 0.53 (0.13–2.13) | 0.371 | 0.83 (0.21–3.37) | 0.799 | 0.80 (0.20–3.21) | 0.754 | ||
| IL-13 [3, 8] | Multiple sclerosis, systemic sclerosis, scleroderma | 0.63 (0.37–1.06) | 0.084 | 0.62 (0.36–1.04) | 0.072 | 0.55 (0.29–1.02) | 0.058 | 0.53 (0.28–0.98) | 0.043 | ||
| Underexpression | IL-1 receptor antagonist [9] | Rheumatoid arthritis and psoriatic arthritis | 0.90 (0.67–1.21) | 0.492 | 1.11 (0.83–1.47) | 0.481 | 0.76 (0.53–1.07) | 0.118 | 0.90 (0.64–1.27) | 0.555 | |
| IL-4 [12] | Rheumatoid arthritis and multiple sclerosis | 0.76 (0.57–1.00) | 0.054 | 0.89 (0.67–1.18) | 0.411 | 0.62 (0.44–0.87) | 0.006 | 0.70 (0.50–0.98) | 0.040 | ||
| IL-10 [8, 12] | Rheumatoid arthritis and multiple sclerosis | 0.76 (0.57–1.00) | 0.054 | 0.89 (0.67–1.18) | 0.411 | 0.62 (0.44–0.87) | 0.006 | 0.70 (0.50–0.98) | 0.040 | ||
| TGF-B [8, 12] | Systemic lupus erythematosus | 0.88 (0.52–1.51) | 0.645 | 0.75 (0.45–1.28) | 0.294 | 0.90 (0.53–1.55) | 0.708 | 0.79 (0.47–1.34) | 0.389 | ||
Model 1 adjusted for age, sex, race, ICU unit, Elixhauser score, pre-admission chronic DMARD or prednisone use, and SOFA. Model 2 adjusted for SOFA
*Inflammatory myopathies include polymyositis, dermatomyositis, and inclusion body myositis
Among septic shock patients, the overexpression of IL-6, IL-12, INF-γ, and TNF-α was associated with a statistically significant 23.00–41.00% reduction in 30-day mortality, adjusting for all confounders (IL-6 OR 0.75, 95% CI 0.60–0.95, P = 0.015; IL-12 OR 0.73, 95% CI 0.55–0.98, P = 0.0351; INF-γ OR 0.59, 95% CI 0.41–0.86, P = 0.007; TNF-α OR 0.77, 95% CI 0.61–0.96, P = 0.020). Additionally, the underexpression of anti-inflammatory cytokines IL-4 and IL-10 was both associated with a statistically significant reduction in the 30-day mortality risk (OR 0.62, 95% CI 0.44–0.87, P = 0.006).
Discussion
This study examined the sepsis survival among ICU patients with and without autoimmune diseases using multiple analytic approaches. We used Martin criteria to identify a sepsis population in the MIMIC III database and ICD-9-CM diagnosis codes and text analysis of the patient discharge summaries to identify a subset of patients with autoimmune diseases (Table 1). Among all sepsis patients, autoimmune disease presence was associated with a statistically significant 27.00% reduction in the 30-day mortality risk (OR 0.73, 95% CI 0.57–0.93, P = 0.001) (Fig. 1 and Table 4). The autoimmune disease-mortality association was similar when we restricted the study population to those with septic shock (OR 0.71, 95% CI 0.54–0.93, P = 0.014).
In a similar study using National Inpatient Sample data, a statistically significant decrease in mortality risk was associated with Crohn’s disease (OR 0.78, 95% CI 0.63–0.97) and a small non-statistically significant decrease in risk was associated with rheumatoid arthritis (OR 0.91, 95% CI 0.82–1.01) [13]. The same study also identified a statistically significant increase in mortality risk associated with ulcerative colitis (OR 1.61, 95% CI 1.35–1.93) [13]. Our study observed a similar, but non-statistically significant reduction in the 30-day mortality risk associated with Crohn’s disease (OR 0.65, 95% CI 0.40–1.05, P = 0.087) and rheumatoid arthritis (OR 0.79, 95% CI 0.52–1.17, P = 0.247) (Additional file 6: Table S6). In contrast, our study identified a non-statistically significant reduction in the 30-day mortality risk associated with ulcerative colitis (OR 0.87, 95% CI 0.52–1.43, P = 0.594). The lack of statistical significance could be due to the smaller number of patients for each individual condition.
A secondary but important result of this study addresses how medications associated with autoimmune disease treatment may impact the observed association. We observed that patients with autoimmune disease and on immunosuppressant therapy had similar reductions in the 30-day mortality risk (OR 0.89, 95% CI 0.65–1.20, P = 0.452) as autoimmune patients not on immunosuppressant therapy (OR 0.82, 95% CI 0.58–1.16, P = 0.272) (Table 5). This finding indicates that these medications did not modify the association between autoimmune disease and 30-day mortality. The results of the mediation analysis (Table 6) provided further evidence of the limited impact of these medications on the autoimmune disease-mortality relationship (indirect effect OR 1.07, 95% CI 1.01–1.13, P = 0.020). Altogether, these findings suggest that autoimmune diseases affect 30-day mortality through a mechanism unrelated to chronic DMARD or prednisone use.
Table 5.
Joint effect of autoimmune disease and DMARD or prednisone use on 30-day mortality
| Association between autoimmune disease and 30-day mortality, accounting for chronic DMARD and prednisone use | Sepsis cohort | Septic shock cohort | ||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| All potential confounders adjusteda | ||||
| No autoimmune disease presence | ||||
| No chronic DMARD/prednisone usage | 1.00 | Reference | 1.00 | Reference |
| Autoimmune disease presence | ||||
| No chronic DMARD or prednisone usage | 0.82 (0.58–1.16) | 0.272 | 0.76 (0.50–1.14) | 0.186 |
| Chronic DMARD or prednisone usage | 0.89 (0.65–1.20) | 0.452 | 0.87 (0.62–1.22) | 0.428 |
| SOFA score adjusted | ||||
| No autoimmune disease presence | ||||
| No chronic DMARD/prednisone usage | 1.00 | Reference | 1.00 | Reference |
| Autoimmune disease presence | ||||
| No chronic DMARD or prednisone usage | 0.80 (0.57–1.11) | 0.190 | 0.73 (0.49–1.07) | 0.114 |
| Chronic DMARD or prednisone usage | 0.84 (0.62–1.12) | 0.231 | 0.77 (0.55–1.07) | 0.121 |
Sepsis cohort—ICU patients with sepsis as defined by Martin criteria. Septic shock cohort—ICU patients with sepsis as defined by Martin criteria and three consecutive mean arterial blood pressure readings below 65 mmHg in a 30-min period or at least one dose of vasopressors during the ICU stay
OR odds ratio, CI confidence interval, DMARD disease-modifying antirheumatic drug, SOFA Sequential Organ Failure Assessment
aOR adjusted for age, sex, race, SOFA score at ICU admission, Elixhauser comorbidity index, pre-admission chronic DMARD or prednisone use, ICU care unit, documented bacteremia, and infection site
We evaluated the possible effect of cytokine dysregulation on 30-day mortality to understand other potential mechanisms that may explain the observed associations (Table 7). Autoimmune diseases associated with the overexpression of pro-inflammatory cytokines IL-12 and INF-γ were associated with a statistically significant reduction in the 30-day mortality risk (IL-12 OR 0.76, 95% CI 0.59–0.99, P = 0.040; INF-γ OR 0.63, 95% CI 0.45–0.89, P = 0.008). These results highlight how the immunosuppressive state induced by sepsis may play a critical role in mortality among sepsis patients [3] and that therapies that augment IL-12 and INF-γ expression may improve sepsis survival [32].
The observed relationships between cytokine dysregulation and mortality are further supported by previous studies identifying that the sepsis response impairs INF-y production [33], monocyte expression of HLA-DR and production of leukocyte cytokines (e.g., IL-1, IL-6, and TNF-a) [34, 35], and macrophage phagocytic and microbicidal activity and their ability to produce pro-inflammatory cytokines IL-12 and TNF-a [36]. This sepsis-induced immunosuppressive state may be further mediated by the release of anti-inflammatory cytokines (e.g., IL-4 and IL-10) [33]. IL-4 has been shown to reduce pro-inflammatory cytokine expression and increase the expression of other anti-inflammatory cytokines [37, 38] while IL-10 has been shown to downregulate the expression of several pro-inflammatory cytokines and impair HLA-DR expression [33, 39]. Patients who experience pre-sepsis over- or underexpression of specific cytokines may be better suited to survive the immune function impairment [33, 40–44]. The high rates of nosocomial infections (especially of the lung) and mortality among sepsis patients [33, 45] further highlight the clinical importance of the immune function impairment.
There are several limitations to our study. First, our results may be affected by diagnostic bias, where patients with autoimmune disease are admitted to the ICU earlier than the rest of the population due to the severity of the autoimmune diagnosis and the immunocompromised status, thus potentially resulting in better survival. This selection process would result in higher prevalence of patients with autoimmune disease among ICU population. However, the autoimmune disease prevalence among patients in our study was 8.00% which is at the higher end of the estimated prevalence of autoimmune diseases in the general population, estimated between 3.00 and 10.00% [46–49]. The observed prevalence can be explained by the significantly higher than average age of the ICU population (mean age is 66.07 years) since autoimmune disease prevalence increases with increasing age [50]. In our analysis, we observed that patients with autoimmune disease had a significantly lower SOFA score than patients without autoimmune disease implying that autoimmune disease patients enter the ICU in better condition (5.63 ± 3.67 vs. 6.50 ± 3.80, P < 0.001). To account for this difference, we statistically adjusted for SOFA score in all analyses, thus eliminating this bias. To further explore the potential role of diagnostic bias, we estimated the relationship between the presence of other comorbidities involving immunosuppression factors (AIDS, lymphoma, metastatic cancer, and solid-state tumors) and 30-day mortality (Additional file 7: Table S7). We found that for these patients, the 30-day mortality risk was higher (OR 1.98, 95% CI 1.65–2.36, P ≤ 0.001). We believe that further studies with more diverse pre-ICU admission data will help to fully rule out diagnostic bias.
Another limitation of the study stems from the fact that MIMIC database is based on a single-center study institution, and the findings may not be generalizable. The confidence in these results comes from the initial analysis of MIMIC II data, covering half of the time of MIMIC III data. Analysis on half of the population currently available led to similar conclusions. Lastly, we may not have accounted for some important confounding factors, though every attempt was made to include them in the study. Specifically, it is hard to account for past medical history with high certainty. To overcome this limitation, we performed an automated and manual analysis of discharge summaries. Manual evaluation of a subset of discharge summaries revealed some levels of ambiguity or missed information about patient’s condition as compared to automated analysis that requires further exploration. We could not measure the level of uncertainty due to the large number of cases in the study, referring such analysis to further studies measuring the uncertainly related to information extraction from free text.
Conclusion
We demonstrated that select autoimmune diseases are associated with a lower 30-day mortality risk among sepsis patients in the ICU. This association was nearly identical among patients with a more severe form of sepsis. The primary driver of mortality among sepsis patients is still an open question [51]. Our study found that autoimmune disease-induced dysregulation of sepsis-related cytokines (specifically IL-12 and INF-γ) prior to sepsis onset was associated with a lower 30-day mortality risk. These results provide further support regarding the potential benefit of therapies designed to augment the production of IL-12, INF-γ, and other pro-inflammatory cytokines in the treatment of sepsis [32]. Further research utilizing data from other medical centers will provide further validation and insight into these findings and potential causal mechanisms.
Additional files
Table S1. Dysregulated cytokines and specific autoimmune diseases included in the study’s autoimmune definition. (DOCX 16 kb)
Table S2. Biologic and conventional DMARD medications included in the present study. (DOCX 13 kb)
Table S3. Analysis of the impact of individual comorbidities on the autoimmune disease-30-day mortality association. (DOCX 15 kb)
Table S4. Impact of adjusting for potential confounders and SOFA score on the autoimmune disease-30-day mortality association. (DOCX 15 kb)
Table S5. Survival analysis of the five most frequently reported autoimmune diseases. (DOCX 13 kb)
Table S6. Association between each autoimmune disease and 30-day mortality. (DOCX 14 kb)
Table S7. Sensitivity analysis exploring the potential effect of diagnostic bias among other immunocompromised patients. (DOCX 12 kb)
Acknowledgements
The authors would like to thank Dr. Abdulla Chahin for his insightful guidance on the study topic.
Funding
This study was partially funded by internal funding from the Charles Stark Draper Laboratory Inc.
Availability of data and materials
The MIMIC III database (version 1.4) is publically available from https://mimic.physionet.org/. Any researcher who adheres to the data use requirements is permitted access to the database.
Abbreviations
- CI
Confidence interval
- DMARD
Disease-modifying antirheumatic drug
- HR
Hazards ratio
- ICU
Intensive care unit
- IL
Interleukin
- INF-γ
Interferon gamma
- MIMIC
Multiparameter Intelligent Monitoring in Intensive Care
- OR
Odds ratio
- SOFA
Sequential Organ Failure Assessment
- TNF-α
Tumor necrosis factor alpha
Authors’ contributions
MS, CMB, LAC, RGM, and NM all take responsibility for the integrity of the data, interpretation, and analysis. All authors contributed substantially to the study design, data interpretation, and writing of the manuscript. CMB and MS performed the statistical analysis and data synthesis. All authors approved the final version of the manuscript.
Ethics approval and consent to participate
The establishment of the database was approved by the Massachusetts Institute of Technology (Cambridge, MA) and the Institutional Review Boards of Beth Israel Deaconess Medical Center (Boston, MA).
Consent for publication
Requirement for individual patient consent was waived because the project did not impact clinical care and all protected health information was de-identified.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mallory Sheth, Email: mmbounds@mit.edu.
Corey M. Benedum, Email: cbenedum@bu.edu
Leo Anthony Celi, Email: leoanthonyceli@yahoo.com.
Roger G. Mark, Email: rgmark@mit.edu
Natasha Markuzon, Email: nmarkuzon@draper.com.
References
- 1.Angus DC, Van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840–851. doi: 10.1056/NEJMra1208623. [DOI] [PubMed] [Google Scholar]
- 2.National Institute of General Medical Sciences. Sepsis fact sheet [Internet]. Sepsis fact sheet. [cited 2017 Dec 4]. Available from: https://www.nigms.nih.gov/Education/Pages/factsheet_sepsis.aspx
- 3.Schulte W, Bernhagen J, Bucala R. Cytokines in sepsis: potent immunoregulators and potential therapeutic targets—an updated view. Mediat Inflamm. 2013;3(3):155–8. doi: 10.1155/2013/165974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Angus DC. The search for effective therapy for sepsis: back to the drawing board? JAMA. 2011;306:2614–2615. doi: 10.1001/jama.2011.1853. [DOI] [PubMed] [Google Scholar]
- 5.Hotchkiss RS, Monneret G, Payen D. Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol. 2013;13:862–874. doi: 10.1038/nri3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaudhry H, Zhou J, Zhong YIN, Ali MM, McGuire F, Nagarkatti PS, et al. Role of cytokines as a double-edged sword in sepsis. In Vivo. 2013;27:669–684. [PMC free article] [PubMed] [Google Scholar]
- 7.Jaffer U, Wade RG, Gourlay T. Cytokines in the systemic inflammatory response syndrome: a review. HSR Proc Intensive Care Cardiovasc Anesth. 2010;2:161. [PMC free article] [PubMed] [Google Scholar]
- 8.Rose NR, Mackay IR. The autoimmune diseases. 5. San Diego: Academic Press; 2014. [Google Scholar]
- 9.Davidson A, Diamond B. Autoimmune diseases. N Engl J Med. 2001;345:340–350. doi: 10.1056/NEJM200108023450506. [DOI] [PubMed] [Google Scholar]
- 10.Rincon M. Interleukin-6: from an inflammatory marker to a target for inflammatory diseases. Trends Immunol. 2012;33:571–577. doi: 10.1016/j.it.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Li X, Xiao B-G, Xi J-Y, Lu C-Z, Lu J-H. Decrease of CD4+ CD25highFoxp3+ regulatory T cells and elevation of CD19+ BAFF-R+ B cells and soluble ICAM-1 in myasthenia gravis. Clin Immunol. 2008;126:180–188. doi: 10.1016/j.clim.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Santamaria P. Cytokines and chemokines in autoimmune disease: an overview. Adv Exp Med Biol. 2003;520:1–7. doi: 10.1007/978-1-4615-0171-8_1. [DOI] [PubMed] [Google Scholar]
- 13.Colbert JF, Schmidt EP, Faubel S, Ginde AA. Severe sepsis outcomes among hospitalizations with inflammatory bowel disease. Shock. 2017;47:128. doi: 10.1097/SHK.0000000000000742. [DOI] [PubMed] [Google Scholar]
- 14.Delano MJ, Ward PA. Sepsis-induced immune dysfunction: can immune therapies reduce mortality? J Clin Invest. 2016;126:23–31. doi: 10.1172/JCI82224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cuenca AG, Delano MJ, Kelly-Scumpia KM, Moreno C, Scumpia PO, LaFace DM, et al. A paradoxical role for myeloid-derived suppressor cells in sepsis and trauma. Mol Med. 2011;17:281–292. doi: 10.2119/molmed.2010.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Poll T. Myeloid-derived suppressor cells in sepsis. Am J Respir Crit Care Med. 2017;196:256–258. doi: 10.1164/rccm.201701-0046ED. [DOI] [PubMed] [Google Scholar]
- 17.Uhel F, Azzaoui I, Grégoire M, Pangault C, Dulong J, Tadié J-M, et al. Early expansion of circulating granulocytic myeloid-derived suppressor cells predicts development of nosocomial infections in septic patients. Am J Respir Crit Care Med. 2017;196(3):315–27. doi: 10.1164/rccm.201606-1143OC. [DOI] [PubMed] [Google Scholar]
- 18.Johnson AE, Pollard TJ, Shen L, Lehman LH, Feng M, Ghassemi M, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3 [cited 2017 Apr 15]. Available from: https://www-ncbi-nlm-nih-gov.ezproxy.bu.edu/pmc/articles/PMC4878278/. [DOI] [PMC free article] [PubMed]
- 19.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 20.Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:775–787. doi: 10.1001/jama.2016.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bale C, Kakrani AL, Dabadghao VS, Sharma ZD. Sequential organ failure assessment score as prognostic marker in critically ill patients in a tertiary care intensive care unit. Int J Med Public Health. 2013;3:165974. [Google Scholar]
- 22.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Bishop CM. Pattern recognition and machine learning. New York: Springer; 2006.
- 24.Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138:923–936. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- 25.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129:125–137. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]
- 26.Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure–mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18:137. doi: 10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richter A, Listing J, Schneider M, Klopsch T, Kapelle A, Kaufmann J, et al. Impact of treatment with biologic DMARDs on the risk of sepsis or mortality after serious infection in patients with rheumatoid arthritis. Ann Rheum Dis. 2016;75:1667–1673. doi: 10.1136/annrheumdis-2015-207838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hotchkiss RS, Monneret G, Payen D. Immunosuppression in sepsis: a novel understanding of the disorder and a new therapeutic approach. Lancet Infect Dis. 2013;13:260–268. doi: 10.1016/S1473-3099(13)70001-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacKinnon DP. Introduction to statistical mediation analysis. New York: Routledge; 2008.
- 30.R Core Team . R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 31.SAS Institute Inc. SAS 9.4 [Computer software]. SAS Institute Inc Cary, NC; 2013.
- 32.Ono S, Ueno C, Aosasa S, Tsujimoto H, Seki S, Mochizuki H. Severe sepsis induces deficient interferon-gamma and interleukin-12 production, but interleukin-12 therapy improves survival in peritonitis. Am J Surg. 2001;182:491–497. doi: 10.1016/S0002-9610(01)00754-1. [DOI] [PubMed] [Google Scholar]
- 33.Reddy RC, Chen GH, Tekchandani PK, Standiford TJ. Sepsis-induced immunosuppression: from bad to worse. Immunol Res. 2001;24:273. doi: 10.1385/IR:24:3:273. [DOI] [PubMed] [Google Scholar]
- 34.Munoz C, Carlet J, Fitting C, Misset B, Bleriot JP, Cavaillon JM. Dysregulation of in vitro cytokine production by monocytes during sepsis. J Clin Invest. 1991;88:1747–1754. doi: 10.1172/JCI115493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Appel SH, Wellhausen SR, Montgomery R, DeWeese RC, Polk HC., Jr Experimental and clinical significance of endotoxin-dependent HLA-DR expression on monocytes. J Surg Res. 1989;47:39–44. doi: 10.1016/0022-4804(89)90045-0. [DOI] [PubMed] [Google Scholar]
- 36.Reddy RC, Chen GH, Newstead MW, Moore T, Zeng X, Tateda K, et al. Alveolar macrophage deactivation in murine septic peritonitis: role of interleukin 10. Infect Immun. 2001;69:1394–1401. doi: 10.1128/IAI.69.3.1394-1401.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Te Velde AA, Huijbens RJ, Heije K, de Vries JE, Figdor CG. Interleukin-4 (IL-4) inhibits secretion of IL-1 beta, tumor necrosis factor alpha, and IL-6 by human monocytes. Blood. 1990;76:1392. [PubMed] [Google Scholar]
- 38.Jenkins JK, Arend WP. Interleukin 1 receptor antagonist production in human monocytes is induced by IL-1α, IL-3, IL-4 and GM-CSF. Cytokine. 1993;5:407–415. doi: 10.1016/1043-4666(93)90030-9. [DOI] [PubMed] [Google Scholar]
- 39.Monneret G, Finck M-E, Venet F, Debard A-L, Bohé J, Bienvenu J, et al. The anti-inflammatory response dominates after septic shock: association of low monocyte HLA-DR expression and high interleukin-10 concentration. Immunol Lett. 2004;95:193–198. doi: 10.1016/j.imlet.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 40.Netea MG, van der Meer JW, van Deuren M, Kullberg BJ. Proinflammatory cytokines and sepsis syndrome: not enough, or too much of a good thing? Trends Immunol. 2003;24:254–258. doi: 10.1016/S1471-4906(03)00079-6. [DOI] [PubMed] [Google Scholar]
- 41.Takeyama N, Tanaka T, Yabuki T, Nakatani K, Nakatani T. Effect of interferon gamma on sepsis-related death in patients with immunoparalysis. Crit Care. 2004;8:P207. doi: 10.1186/cc2674. [DOI] [Google Scholar]
- 42.Hershman MJ, Appel SH, Wellhausen SR, Sonnenfeld G, Polk HC., Jr Interferon-gamma treatment increases HLA-DR expression on monocytes in severely injured patients. Clin Exp Immunol. 1989;77:67. [PMC free article] [PubMed] [Google Scholar]
- 43.Stanilova SA, Karakolev ZT, Dimov GS, Dobreva ZG, Miteva LD, Slavov ES, et al. High interleukin 12 and low interleukin 10 production after in vitro stimulation detected in sepsis survivors. Intensive Care Med. 2005;31:401–407. doi: 10.1007/s00134-005-2575-7. [DOI] [PubMed] [Google Scholar]
- 44.DiPiro JT, Howdieshell TR, Goddard JK, Callaway DB, Hamilton RG, Mansberger AR. Association of interleukin-4 plasma levels with traumatic injury and clinical course. Arch Surg. 1995;130:1159–1163. doi: 10.1001/archsurg.1995.01430110017004. [DOI] [PubMed] [Google Scholar]
- 45.Ashare A, Powers LS, Butler NS, Doerschug KC, Monick MM, Hunninghake GW. Anti-inflammatory response is associated with mortality and severity of infection in sepsis. Am J Physiol-Lung Cell Mol Physiol. 2005;288:L633–L640. doi: 10.1152/ajplung.00231.2004. [DOI] [PubMed] [Google Scholar]
- 46.Cooper GS, Stroehla BC. The epidemiology of autoimmune diseases. Autoimmun Rev. 2003;2:119–125. doi: 10.1016/S1568-9972(03)00006-5. [DOI] [PubMed] [Google Scholar]
- 47.Cooper GS, Bynum ML, Somers EC. Recent insights in the epidemiology of autoimmune diseases: improved prevalence estimates and understanding of clustering of diseases. J Autoimmun. 2009;33:197–207. doi: 10.1016/j.jaut.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hayter SM, Cook MC. Updated assessment of the prevalence, spectrum and case definition of autoimmune disease. Autoimmun Rev. 2012;11:754–765. doi: 10.1016/j.autrev.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 49.Rose NR, Bona C. Defining criteria for autoimmune diseases (Witebsky’s postulates revisited) Immunol Today. 1993;14:426–430. doi: 10.1016/0167-5699(93)90244-F. [DOI] [PubMed] [Google Scholar]
- 50.Grolleau-Julius A, Ray D, Yung RL. The role of epigenetics in aging and autoimmunity. Clin Rev Allergy Immunol. 2010;39:42–50. doi: 10.1007/s12016-009-8169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Goldenberg NM, Leligdowicz A, Slutsky AS, Friedrich JO, Lee WL. Is nosocomial infection really the major cause of death in sepsis? Crit Care. 2014;18 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4331295/. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Dysregulated cytokines and specific autoimmune diseases included in the study’s autoimmune definition. (DOCX 16 kb)
Table S2. Biologic and conventional DMARD medications included in the present study. (DOCX 13 kb)
Table S3. Analysis of the impact of individual comorbidities on the autoimmune disease-30-day mortality association. (DOCX 15 kb)
Table S4. Impact of adjusting for potential confounders and SOFA score on the autoimmune disease-30-day mortality association. (DOCX 15 kb)
Table S5. Survival analysis of the five most frequently reported autoimmune diseases. (DOCX 13 kb)
Table S6. Association between each autoimmune disease and 30-day mortality. (DOCX 14 kb)
Table S7. Sensitivity analysis exploring the potential effect of diagnostic bias among other immunocompromised patients. (DOCX 12 kb)
Data Availability Statement
The MIMIC III database (version 1.4) is publically available from https://mimic.physionet.org/. Any researcher who adheres to the data use requirements is permitted access to the database.