Abstract
Objectives
Localized cutaneous leishmaniasis and its evolving forms diffuse cutaneous leishmaniasis, mucosal leishmaniasis and cutaneous leishmaniasis recidivans, together with the visceral leishmaniasis sequelae post-kala azar dermal leishmaniasis account for about one million dermal leishmaniases cases per year worldwide. Although not lethal, the dermal leishmaniases cause chronic and disfiguring skin lesions, which are an important cause of morbidity and stigma.
Microscopy remains the reference test for diagnosis of dermal leishmaniasis; however, it has low and variable sensitivity and requires well trained personnel. The technical complexity and cost of the more sensitive molecular techniques (e.g. PCR) limits their application in routine diagnosis in endemic areas. Point-of-care (POC) tests for early diagnosis are much needed in order to benefit both patients and communities, by reducing the risk of both sequelae and Leishmania transmission. To this end we developed a Target Product Profile (TPP) for a POC test for dermal leishmaniases.
Methods
The TPP was defined through several rounds of discussions and by consensus with stakeholders and experts in dermal leishmaniases from different type of organizations and endemic regions.
Results and conclusions
A rapid, simple and robust test that can be implemented in resource-limited settings, enabling decentralized diagnosis and treatment of dermal leishmaniasis should be developed. Ideally it should enable the diagnosis of all forms of dermal leishmaniasis, but the minimally accepted target would be localized cutaneous leishmaniasis. A minimum sensitivity of 95% and specificity of 90% would be required. The consensus was that the POC test should target Leishmania antigens.
Keywords: Leishmaniasis, Cutaneous leishmaniasis, Dermal leishmaniasis, Point-of-care diagnostics, Target Product Profile
1. Introduction
The leishmaniases are a group of infections caused by parasites of the genus Leishmania, which are transmitted through the bite of female phlebotomine sand flies, through either a zoonotic or anthroponotic cycle (WHO Expert Committee on the Control of the Leishmaniases and World Health Organization, 2010). Most dermal leishmaniasis cases are localized cutaneous leishmaniasis (CL) but other more aggressive forms include, diffuse cutaneous leishmaniasis (DCL), mucosal leishmaniasis (ML) and cutaneous leishmaniasis recidivans (CLR), which in total account for an estimated 0.7–1.2 million cases/year worldwide (Alvar et al., 2012). Another form of dermal leishmaniasis is post-kala azar dermal leishmaniasis (PKDL), a complication of visceral leishmaniasis (VL) caused by Leishmania donovani that affects up to 5% of VL cases in the Indian subcontinent and up to 50% in eastern Africa. PKDL patients may also play an important role in transmission of L. donovani (World Health Organization, 2013; Zijlstra et al., 2017). Although not lethal, dermal leishmaniases cause chronic and disfiguring skin lesions, which are an important cause of morbidity and social stigma (Toledo Jr et al., 2013; Kassi et al., 2008; Nilforoushzadeh et al., 2010; Vares et al., 2013; Pal et al., 2017).
Microscopy of Giemsa stained samples from lesions, including skin scrapings, fine needle aspirates, or slit-skin smears, remains the reference test for diagnosis of the different forms of dermal leishmaniasis. However, microscopy has a low and variable sensitivity and requires trained and experienced personnel (de Vries et al., 2015; Adams et al., 2013). As a result a high number of patients are put on treatment without laboratory confirmation, exposing a variable number of them to unnecessary toxic treatment (Zijlstra et al., 2017; World Health Organization, 2016). The technical complexity and cost of the more sensitive molecular techniques (e.g. PCR) limits their application as routine diagnostic tools in endemic areas. Other simpler tests for detection of leishmanial DNA, such as loop-mediated isothermal amplification (LAMP), are yet to be implemented (de Vries et al., 2015; Adams et al., 2018; Verma et al., 2017). Other approaches include serology, which may be useful for screening of PKDL and mucosal leishmaniasis, but cannot be used for confirmation as presence of antibodies may be due to previous episodes or exposure to the parasite by living in endemic areas. The leishmanin skin test (LST) can also aid in the diagnosis of CL, but again the tests is not a marker of active infection, and therefore has limited value (WHO Expert Committee on the Control of the Leishmaniases and World Health Organization, 2010; Zijlstra et al., 2017; de Vries et al., 2015).
Thus there is a great need for point-of-care (POC) tests for early diagnosis of dermal leishmaniases, in order to benefit both patients and communities by early identification of those that need treatment, reducing the risk of both sequelae and ongoing Leishmania transmission. It is then important that new POC tests to be developed meet the needs of the target population and the requirements for implementation in resource-limited settings, where most cases of dermal leishmaniasis occur. To this end we present here a Target Product Profile (TPP) for a POC test for dermal leishmaniases that was defined through consensus with stakeholders and experts in these forms of leishmaniases.
2. Methods
Target Product Profiles (TPPs) for diagnostics provide details on the desired minimal and optimal features of priority diagnostic tests, including performance and operational characteristics. Adherence to TPPs ensures that research and development activities are focused on products designed for the contexts and needs of end users. To develop a TPP for a POC for dermal leishmaniases we followed a three steps process: i) a draft TPP was developed by the leishmaniasis groups at the Foundation for Innovative New Diagnostics (FIND) and Drug for Neglected Diseases initiative (DNDi), ii) the draft TPP was discussed at a meeting of experts in leishmaniasis, and a revised version was prepared, then iii) the revised version was reviewed through an online survey with a larger audience of stakeholders and experts, and a consensus TPP developed.
The draft TPP had 29 test features for which optimal (desired) and minimally accepted targets were defined. This first draft was presented at the 2nd redeLEISH Meeting (Medellín, Colombia, July 2015) for discussion with a panel of 70 experts on leishmaniasis (DNDi.www.dndi.org, 2015). The draft was refined based on the inputs received from experts in that meeting, and a new document prepared to be shared with a second panel of experts. Eighty-two experts in leishmaniasis and stakeholders were invited to participate in an online review of the TPP. Participants were requested to indicate their level of agreement with the optimal and minimal targets proposed for each feature, using a scale from 1 to 5, where 1 = Disagree, 2 = Somewhat disagree, 3 = Neither agree or disagree, 4 = Mostly agree and 5 = Fully agree. Where the level of agreement was 3 or less, the experts were requested to provide an explanation. The consensus among experts was scored as the percentage that indicated a level of agreement of >4 (mostly agree or 5, fully agree).
3. Results
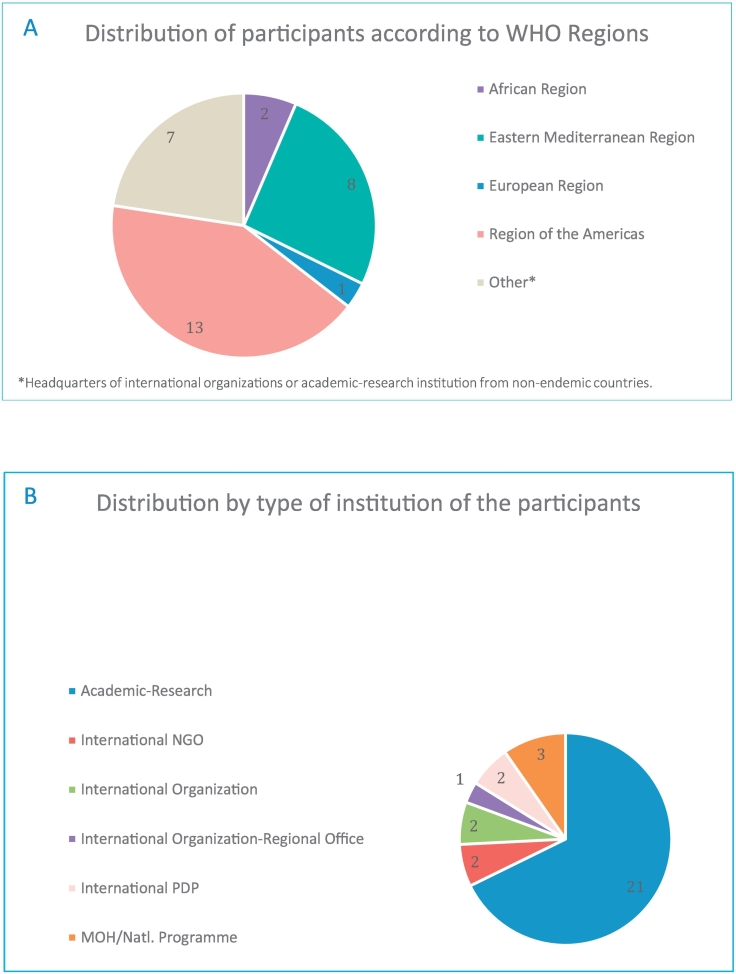
Out of 82 experts invited to participate in the online review, 31 completed the full questionnaire indicating their level of agreement with each of the features in the TPP. The experts were drawn from different endemic regions and types of organizations (Fig. 1).
Fig. 1.
Distribution of people who participated in an online review of the TPP for dermal leishmaniases according to WHO region (A) and type of organization (B).
There was consensus on all features (i.e. >50% of replies were either “mostly agree” or “fully agree”). The consensus scores were high for both the optimal (mean % of replies scoring 4 or 5 = 92.5 ± 9.3) and minimal targets (88.5 ± 11.1). Details on the features of TPP defined and the consensus scores for each of them is given in Table 1.
Table 1.
Target Product Profile for a point-of-care diagnostic test for dermal leishmaniases.
| Feature | Optimal | Minimal | Rationale and evidence | Consensus score |
|---|---|---|---|---|
| Priority features: SCOPE | ||||
| 1. Goal of test. Intended use | Detection of active CL (any form) or PKDL with the purpose of initiating treatment during the same clinical encounter (or same day) | Detection of active LCL. | LCL is the most prevalent form of dermal leishmaniasis (>80% of the cases). This clinical form is present in all CL endemic regions. All Leishmania species cause LCL. Other forms of CL usually evolve from LCL | Optimal 100% Minimal 97% |
| 2. Target population | Individuals with clinical signs suggestive of any form of CL, or PKDL | Individuals with clinical signs suggestive of LCL | Optimal 100% Minimal 97% |
|
| 3. Target operator of test | Health worker at PHC level without laboratory training | Trained laboratory staff | Most patients go to health facilities with limited human resources | Optimal 90% Minimal 93% |
| 4. Lowest setting for implementation. Target use setting |
Decentralized health care facilities with no laboratory infrastructure, or mobile team | Decentralized health care facilities with minimum laboratory infrastructure | This test could replace microscopy, as has happened with other diseases (e.g. malaria) | Optimal 93% Minimal 90% |
| 5. Target analyte to be detected | Leishmania antigen | Optimal 84% Minimal 87% |
||
| Priority features: PERFORMANCE CHARACTERISTICS | ||||
| 6. Clinical sensitivity | 100% in parasitologically confirmed cases | 95% in parasitologically confirmed cases | Measured in frozen or fresh samples from parasitologically confirmed patients (microscopy and/or culture and/or PCR from skin scrapings, swabs, biopsies, aspirates, etc.). A combined reference standard according to each region should be considered | Optimal 90% Minimal 90% |
| 7. Clinical specificity | >95% | >90% | Tested against reference standard (according to each endemic setting), including subjects with other diseases affecting the skin | Optimal 90% Minimal 81% |
| 8. Leishmania species-specificity | Leishmania species-specific | Leishmania genus-specific | Different treatment options might be needed for different species | Optimal 90% Minimal 90% |
| 9. Type of analysis. Quantitation | Qualitative | There is no need for quantification as parasite burden will not guide therapy | Optimal 97% Minimal 97% |
|
| Priority features: TEST PROCEDURE | ||||
| 10. Training needs. Time dedicated to training session for end users | Less than half a day for any level health care worker. Job aid provided | One day for any level health care worker. Job aid provided | Optimal 100% Minimal 100% |
|
| 11. Sample type | Lesion swab | Lesion fine needle aspirate, skin scrapping, biopsy, etc. | Minimally invasive sampling procedures will be preferred | Optimal 87% Minimal 80% |
| 12. Sample preparation. Total steps | Direct testing from lesion swab | 3–5 simple steps procedure | Optimal 90% Minimal 90% |
|
| 13. Number of steps to be performed by operator | <3; 1 timed steps | <10; 1 timed steps | Optimal 100% Minimal 64% |
|
| 14. Need for operator to transfer a precise volume of sample | No | Acceptable with a disposable transfer device provided | Sample may need to be eluted in specific buffer (included in the kit) | Optimal 90% Minimal 93% |
| 15. Time to result | <20 min | <1 h | Optimal 93% Minimal 90% |
|
| 16. Internal control | Included | Positive control to confirm validity of the test | Optimal 97% Minimal 97% |
|
| 17. Reading system How the test result will be seen |
Visual (naked eye). | Visual (naked eye) or simple reading device | Optimal 97% Minimal 93% |
|
| 18. Auxiliary equipment | None, instrument free (required materials are included in the kit) | Test reader (for lateral flow assay, dual path platform, or similar) | Connectivity: the reader could enable sending results to a reference lab, coordinator | Optimal 100% Minimal 84% |
| 19. Power Requirements | None required | Small, portable or hand-held instrument (<1 kg) that can operate on rechargeable battery or solar power lasting at least 4 h (8 h preferred) | Optimal 93% Minimal 87% |
|
| 20. Need for maintenance/spare parts | None | Optimal 97% Minimal 97% |
||
| Priority features: OPERATIONAL CHARACTERISTICS | ||||
| 21. Operating conditions | 5–50 °C, up to 90% relative humidity (RH), 0–4000 m above sea level | 5–40 °C, up to 80% RH, 0–2000 m above sea level | High environmental temperatures and high humidity are often a problem in countries where CL is endemic. Some laboratories for CL diagnosis are located at high altitude (e.g. La Paz, Bolivia) | Optimal 97% Minimal 93% |
| 22. Reagent kit transport | No cold chain required; tolerance of transport stress for a minimum of 72 h at −15 °C to 50 °C | No cold chain required; tolerance of transport stress for a minimum of 48 h at −15 °C to 50 °C | Refrigerated transport is costly and often cannot be guaranteed during the entire transportation process. Frequent delays in transport are common | Optimal 93% Minimal 97% |
| 23. Reagent kit storage/stability | No cold chain required. Up to 24 months at 50 °C, up to 90% humidity | No cold chain required. Up to 12 months at 40 °C, up to 70% humidity | Should be able to tolerate transport stress (48 h at 50 °C). To include test quality detector (for surpassed T or RH) | Optimal 93% Minimal 93% |
| 24. Reagents reconstitution. Need to prepare the reagents prior to utilization | All reagents ready to use | Optimal 97% Minimal 97% |
||
| 25. In use stability | >1 h for single use test after opening the pouch | High environmental temperatures and high humidity are often a problem in countries where CL is endemic | Optimal 100% Minimal 97% |
|
| 26. Biosafety requirement. Level of protection to be made. Available for the staff and the samples |
No need for biosafety cabinet. Standard biosafety precautions when handling potentially infectious materials. No contraindications to routine use | Optimal 100% Minimal 100% |
||
| Priority features: PRICING | ||||
| 27. Maximum price for individual test. | <1 USD per test | <5 USD per test | Assumption that the test is produced at a large scale, transport costs from producing company not included. | Optimal 97% Minimal 68% |
| 28. Maximum price for instrumentation. If needed | <2000 USD | <2000 USD | In case a test reading device is needed. | Optimal 55% Minimal 58% |
| 29. Expected scale of manufacture | 2.5 million test per year | 1.0 million test per year | Based on 0.7–1.2 million estimated CL cases; and provided the test has better performance than microscopy | Optimal 74% Minimal 68% |
CL: cutaneous leishmaniasis; LCL: localized cutaneous leishmaniasis; PHC: public health centre; PKDL: post kala-azar dermal leishmaniasis.
4. Discussion
Due to the low sensitivity and/or specificity, as well as the complexity of some of the techniques currently available for CL diagnosis, most patients do not have access to early and reliable diagnosis, which increases morbidity and decreases the possibility of control. To advance CL control, new diagnostic options that are affordable, simple, specific, sensitive, and robust are still needed, preferably in the format of a rapid diagnostic test.
Stakeholders and experts in leishmaniasis participated in the development of the TPP described here, which can be used to guide product development. The aim should be for a rapid (<1 h), simple (<10 steps) and robust (stable at defined temperature and humidity) test that can be implemented in resource-limited settings enabling decentralized management of dermal leishmaniases. Ideally the test can be used to diagnose all forms of dermal leishmaniases, including CL and its complicated forms as well as PKDL. The minimally accepted target would be localized CL, the most prevalent, and the one that if diagnosed early, would reduce the risk of developing other forms such as mucosal leishmaniasis and cutaneous leishmaniasis recidivans. The targeted sensitivity should be at least 95% in parasitologically confirmed patients. Specificity should reach a minimum of 90%, to avoid treating non-leishmaniasis patients with other dermal conditions.
The experts who participated in the process of developing the TPP described here agreed that the POC test should target Leishmania antigens. Optimally, the test should be able to identify Leishmania species, as this enable the adaptation of treatment according to the infecting species. However, a test with broad specificity for the whole Leishmania genus would be a minimally accepted target, a test able to detect an antigen that is common across species and that can be used with different sample types may present additional advantages: (i) it can be used to diagnose CL caused by species of both the Leishmania and Viannia subgenera, (ii) it can be used as well to diagnose other clinical forms evolving from CL such as ML, CLR and DCL; and (iii) by detecting species of the L. donovani complex, the diagnosis of PKDL and VL (if the test can also be used in urine or blood) would be possible.
An important aspect to take into consideration during test development would be its affordability. Features related to the test price were the most discussed by experts, and for these lower consensus scores were obtained (see Table 1, features 27–29). Dermal leishmaniases mainly affect poor populations in low and middle income countries that have limited resources to address public health issues. As a consequence, the resources devoted to improving their management and control are scarce. However interventions that allow early detection and treatment would contribute to reducing a huge burden of disease, which is often overlooked, and indirectly, poverty (Bailey et al., 2017). The TPP of a POC diagnostic test for dermal leishmaniases described here could be an important guide in the development of such a test.
Conflict of interest
The authors declare they have no conflict of interest.
Acknowledgements
We would like to thank all experts and colleagues involved in the consultations, the animated discussions during the meetings of experts and online reviews, the useful comments and contributions to the different features of the TPP.
UK aid from the UK Government, and the Government of Switzerland contributed to FIND's participation in this work. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- Adams E.R., Versteeg I., Leeflang M.M. Systematic review into diagnostics for post-kala-azar dermal leishmaniasis (PKDL) J. Trop. Med. 2013;2013 doi: 10.1155/2013/150746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams E.R., Schoone G., Versteeg I., Gomez M.A., Diro E., Mori Y. Development and evaluation of a novel loop-mediated isothermal amplification assay for diagnosis of cutaneous and visceral leishmaniasis. J. Clin. Microbiol. 2018 Jun 25;56(7) doi: 10.1128/JCM.00386-18. pii: e00386-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvar J., Vélez I.D., Bern C., Herrero M., Desjeux P., Cano J. Leishmaniasis worldwide and global estimates of its incidence. PLoS One. 2012;7(5) doi: 10.1371/journal.pone.0035671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey F., Mondragon-Shem K., Hotez P., Ruiz-Postigo J.A., Al-Salem W., Acosta-Serrano Á. A new perspective on cutaneous leishmaniasis-implications for global prevalence and burden of disease estimates. PLoS Negl. Trop. Dis. 2017 Aug 10;11(8) doi: 10.1371/journal.pntd.0005739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries H.J., Reedijk S.H., Schallig H.D. Cutaneous leishmaniasis: recent developments in diagnosis and management. Am. J. Clin. Dermatol. 2015 Apr;16(2):99–109. doi: 10.1007/s40257-015-0114-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DNDi.www.dndi.org . Available from. 2015. Highlights.https://www.dndi.org/strengthening-capacity/redeleish-network/ [Google Scholar]
- Kassi M., Kassi M., Afghan A.K., Rehman R., Kasi P.M. Marring leishmaniasis: the stigmatization and the impact of cutaneous leishmaniasis in Pakistan and Afghanistan. PLoS Negl. Trop. Dis. 2008;2(10):e259. doi: 10.1371/journal.pntd.0000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilforoushzadeh M., Roohafza H., Jaffary F., Khatuni M. Comparison of quality of life in women suffering from cutaneous leishmaniasis treated with topical and systemic glucantime along with psychiatric consultation compared with the group without psychiatric consultation. J. Skin Leishmaniasis. nov. 2010;1 http://jsl.mui.ac.ir/index.php/jsl/article/view/6 North America. Available at: [Google Scholar]
- Pal B., Murti K., Siddiqui N.A., Das P., Lal C.S., Babu R. Assessment of quality of life in patients with post kalaazar dermal leishmaniasis. Health Qual. Life Outcomes. 2017 Jul 24;15(1):148. doi: 10.1186/s12955-017-0720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toledo A.C., Jr., da Silva R.E., Carmo R.F., Amaral T.A., Luz Z.M., Rabello A. Assessment of the quality of life of patients with cutaneous leishmaniasis in Belo Horizonte, Brazil, 2009–2010. A pilot study. Trans. R. Soc. Trop. Med. Hyg. 2013 May;107(5):335–336. doi: 10.1093/trstmh/trt021. [DOI] [PubMed] [Google Scholar]
- Vares B., Mohseni M., Heshmatkhah A., Farjzadeh S., Safizadeh H., Shamsi-Meymandi S. Quality of life in patients with cutaneous leishmaniasis. Arch. Iran. Med. 2013 Aug;16(8):474–477. (doi: 013168/AIm.008) [PubMed] [Google Scholar]
- Verma S., Singh R., Sharma V., Bumb R.A., Negi N.S., Ramesh V. Development of a rapid loop-mediated isothermal amplification assay for diagnosis and assessment of cure of Leishmania infection. BMC Infect. Dis. 2017 Mar 23;17(1):223. doi: 10.1186/s12879-017-2318-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Expert Committee on the Control of the Leishmaniases & World Health Organization . World Health Organization; Geneva: 2010. Control of the Leishmaniases: Report of a Meeting of the WHO Expert Committee on the Control of Leishmaniases, Geneva, 22–26 March 2010.http://www.who.int/iris/handle/10665/44412 [Google Scholar]
- World Health Organization . World Health Organization; 2013. Post-kala-azar Dermal Leishmaniasis: A Manual for Case Management and Control: Report of a WHO Consultative Meeting, Kolkata, India, 2–3 July 2012.http://www.who.int/iris/handle/10665/78608 [Google Scholar]
- World Health Organization Leishmaniasis in high-burden countries: an epidemiological update based on data reported in 2014. Wkly Epidemiol. Rec. 2016;91(22):286–296. http://www.who.int/iris/handle/10665/254453 World Health Organization. [PubMed] [Google Scholar]
- Zijlstra E.E., Alves F., Rijal S., Arana B., Alvar J. Post-kala-azar dermal leishmaniasis in the Indian subcontinent: a threat to the South-East Asia region kala-azar elimination programme. PLoS Negl. Trop. Dis. 2017 Nov 16;11(11) doi: 10.1371/journal.pntd.0005877. [DOI] [PMC free article] [PubMed] [Google Scholar]