Abstract
Background
In the past two decades, a new epidemiological profile of Chagas' disease (CD) has been registered in the Brazilian Amazon where oral transmission has been indicated as responsible for the increase of acute cases. In the Amazonas state, five outbreaks of acute CD have been registered since 2004. The cardiac manifestations in these cases may be characterized by diffuse myocarditis, with alteration in the electrocardiogram (ECG) and transthoracic echocardiogram (TTE).
Objective
To perform a cardiac evaluation in autochthonous patients in the acute phase and at least one year after submitted to treatment for acute CD and evaluate the demographic variables associated with the presence of cardiac alterations.
Methods
We evaluated patients diagnosed with acute CD through direct parasitological or serological (IgM) methods from 2007 to 2015. These patients were treated with benznidazole and underwent ECG and TTE before and after treatment. We assumed a confidence interval of 95% (CI 95%, p < 0.05) for all variables analyzed.
Results
We observed 63 cases of an acute CD in which oral transmission corresponded to 75%. Cardiac alterations were found in 33% of the cases, with a greater frequency of ventricular repolarization alteration (13%), followed by pericardial effusion (10%) and right bundle branch block and left anterior fascicular block (2%). The follow-up occurred in 48 patients with ECG and 25 with TTE for a mean period of 15.5 ± 4.1 months after treatment. Of these, 8% presented normalization of the cardiac alterations in ECG, 62.5% remained with the normal exams. All of the patients presented normal results in TTE in the post-treatment period. As for the demographic variables, isolated cases presented more cardiac alterations than outbreaks (p = 0.044) as well as cases from Central Amazonas mesoregion (p = 0.020).
Conclusions
Although cardiac alterations have not been frequent in most of the studied population, a continuous evaluation of the clinical-epidemiological dynamics of the disease in the region is necessary in order to establish preventive measures.
Keywords: Chagas Disease/epidemiology, Amazoniany Ecosystem, Trypanosoma cruzi, Chagas Cardiomiopathy/physiopathology
Introduction
Chagas disease (CD) is an emerging infection caused by Trypanosoma cruzi, discovered by the physician Carlos Chagas, in 1909. He described the clinical manifestations, as well as the morphological features of the parasite.1 It is estimated that approximately 75 million people are at risk of acquiring the disease and 8 million are indeed infected by the parasite worldwide.2
CD presents two clinical phases: an acute and a chronic phase. In acute CD, nonspecific clinical symptoms may delay early diagnosis and treatment representing a public health concern. In some cases, the absence of symptoms may lead to a chronic indeterminate form or later evolving to a digestive, cardiac or mixed form.3,4 Oral infection is more likely to cause a symptomatic response and increase the susceptibility to higher mortality rate and may result in unique cardiac characteristics with the most concerning symptom of this phase being diffuse myocarditis with alterations in the ECG and TTE results.5,6
Due to the parasite's genetic characteristics that are thought to be associated with the clinical manifestations of CD, in 1998 Tibayrenc7 proposed a new classification for the parasites' genetic diversity. In a review in 2009, a consensus established the division into six genotypes, named “Discrete Typing Units” (DTUs): TcI-TVI.8
Multiple acute cases have been reported in the Brazilian Amazon with most cases concentrated in Pará and Amazonas,9-14 being the first cases registered in 1968 and 1980, respectively.15,16 Afterwards, micro-epidemics of acute cases have been reported and mostly associated with the ingestion of contaminated food, such as açaí fruits, bacaba fruits and meat of wild mammals.3,17,18 In the last two decades, many new oral transmissions related acute cases have been registered with six outbreaks in the state of Amazonas5,19-21 and T. cruzi DTU described to be related to these cases are TcIV and Z3 (TcIII/TcIV).21,22
Although in the Brazilian Amazon region CD has been widely studied, in the state of Amazonas there still are few data regarding the epidemiological profile of acute CD and more importantly, works related to the cardiac manifestations and post-treatment follow-up are scarce in this group of patients. For that matter, this work aimed to describe cardiac alterations in autochthones patients who had acute CD at least one year after submitted to treatment with benznidazole.
Methods
This was a longitudinal study of patients attended at the Francisca Mendes University Hospital for cardiac follow-up. All of these patients have a confirmed diagnosis of acute CD at the Tropical Medicine Foundation Dr Heitor Vieira Dourado, from January of 2007 to July of 2015.
Study population
Patients were included considering the following criteria: a positive laboratory exam, direct parasitological test (thick blood smear or natural xenodiagnosis) or a reactive immunological essay (IgM anti-T. cruzi) (Enzyme-linked immunoassay - ELISA and/or indirect immunofluorescence assay- IFA) with an epidemiological history such as being originally from the Brazilian Amazon region. All patients were excluded if they referred any previous travel to another Brazilian region or foreign country, did not adhere to or had an incomplete treatment.
Procedures for data collection and treatment
Cardiological exams, standard 12-lead electrocardiogram (ECG) and transthoracic echocardiogram (TTE), was analyzed before treatment and at least one year after the end of treatment. In order to obtain data of patients in pre-treatment stage, a retrospective analysis was made of cases registered in the electronic medical record iDoctor® from 2007 to 2015 in order to access the results of the ECG and TTE as well as demographical, epidemiological and clinical data. During the stage of post-treatment, a prospective evaluation was made which included a clinical examination and performing ECG and TTE in all patients.
The standard 12-lead ECG tracing was done using the software Wincardio (Micromed) and the TTE was performed following the recommendations of the American Society of Echocardiography, using the GE, Vivid 3 equipment.
All patients underwent treatment with benznidazole (Rochagan®) 5-7 mg/kg, for 60 days according to the II Brazilian Guidelines in Chagas Disease of 2015.23 And any cardiac alteration in the ECG or TTE was considered for the description as cardiac alterations in the acute phase of CD.
Statistical analysis
Clinical and epidemiological data were organized using Excel 2016 and the analysis was done using Stata/MP 13.0. For categorical variables, Fisher's exact test was used and the results are presented in tables of absolute and relative frequencies followed by the corresponding p-value. For continuous variables, normal distribution was tested using Shapiro-Wilk normality test, if the normal distribution was observed, an unpaired t-test (Student t-test) was executed and results presented by mean ± SD, otherwise, the Wilcoxon rank-sum (Mann-Whitney) test was used and the results are presented by median and interquartile intervals. We assumed a confidence interval of 95% (CI 95%, p < 0.05) for all statistical tests.
Ethical consideration
This study was approved by the Research Ethics Committee of the Universidade do Estado do Amazonas and is in agreement with the Resolution 466/12 of the Brazilian National Health Council (approval number 923.701/2014).
Results
Case distribution, route of transmission and T. cruzi strain
During the study period, 63 patients with confirmed acute CD were evaluated, all originally from the state of Amazonas. The diagnosis was 98% by a direct parasitological method, thick blood smear. The median age was 29 [16-44] years old, predominantly male (60%). Of these, 44 (70%) were part of an outbreak that was registered from 2007 to 2015, the other 19 (30%) cases are distributed between isolated acute cases associated with oral transmission or classical vector transmission. There were more registered cases of cardiac alterations in the isolated cases reported then in the outbreaks (48% vs. 21%, p = 0.044).
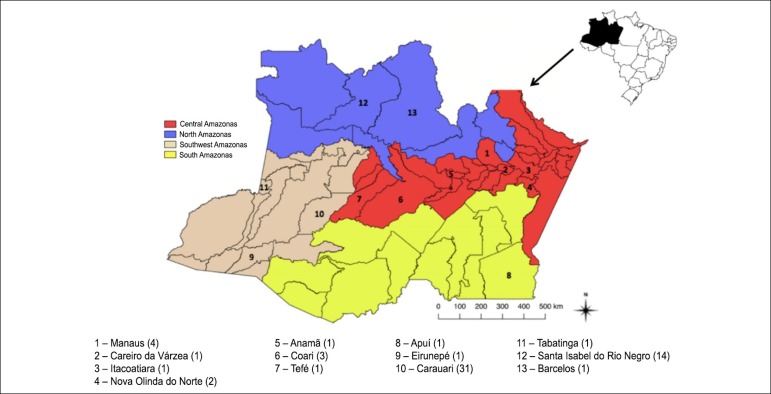
A wide distribution of acute cases is best shown in Figure 1, there can be noticed that most municipalities of the Central Amazonas mesoregion are affected. On the other hand, the Southwest mesoregion concentrated the higher frequency of acute cases corresponding to 33 (53%) cases, and 31 of them being from the outbreaks that happened in Carauari in 2011 and 2015. Cardiac alterations were present in 69% in the Central Amazonas mesoregion which represented a statistical significance (p = 0.020).
Figure 1.
Geographical distribution of the acute cases evaluated in the state of Amazonas. In parenthesis, the number of patients for each municipality.
With regards to the strains of T. cruzi, it was possible to isolate in 35 cases (56%) of which 22 (63%) were Z3 (TcIII/TcIV) and 11 (31%) were TcIV and 2 (6%) TcI, both Z3 (TcIII/TcIV) and TcIV associated with acute oral transmission from outbreaks (Table 1).
Table 1.
Baseline characteristics of acute Chagas' disease patients treated with benznidazol
| Group | ||||
|---|---|---|---|---|
| Variable | Total (n = 63) | Cardiac alterations (n = 21) | No Cardiac alterations (n = 42) | p-value |
| Age (y) | 29 [16-44] | 38 [15-44] | 26.5 [17-44] | 0.694* |
| Gender | 0.588† | |||
| Male | 38 (60%) | 14 (67%) | 24 (57%) | |
| Female | 25 (40%) | 7 (33%) | 18 (43%) | |
| Transmission | 0.364† | |||
| Oral | 47 (75%) | 14 (67%) | 33 (79%) | |
| Vector | 16 (25%) | 7 (33%) | 9 (21%) | |
| Case | 0.044† | |||
| Outbreak | 44 (70%) | 11 (52%) | 33 (79%) | |
| Isolated | 19 (30%) | 10 (48%) | 9 (21%) | |
| Origin (Mesoregion) | 0.020† | |||
| Central Amazonas | 13 (21%) | 9 (43%) | 4 (10%) | |
| North Amazonas | 15 (24%) | 3 (14%) | 12 (29%) | |
| Southwest Amazonas | 33 (53%) | 9 (43%) | 24 (59%) | |
| South Amazonas | 1 (2%) | - | 1 (2%) | |
| T. cruzi DTU | 0.355† | |||
| TcI | 2 (3%) | 2 (9%) | - | |
| TcIV | 11 (17%) | 2 (9%) | 9 (21%) | |
| Z3 (TcIII/TcIV) | 22 (35%) | 9 (43%) | 13 (31%) | |
| ND | 28 (44%) | 8 (38%) | 20 (48%) | |
| Follow-up period (y) | 15.5 ± 4.1 | 14 ± 4 | 16.4 ± 4.1 | 0.050** |
Data are expressed as median [IQ25%-IQ75%] and mean ± SD; In parenthesis are the percentage of the total group; ND: not described; Obs.: It was not possible to obtain the provenance of one case.
Wilcoxon rank-sum (Mann-Whitney) test.
Unpaired t-test (Student t test).
Fisher's exact test.
Cardiac evaluation in Group 1 (pre-treatment)
We observed 33% of any cardiac alterations in our study population. All 63 patients had an ECG prior to initiate the standard treatment with benznidazole. Of these, 44 (70%) presented normal results. Yet, abnormalities such as ventricular repolarization alterations were common. Regarding the TTE results, 87% presented normal parameters. (Table 2). Although the majority of our population presented normal exams, it is noteworthy the death of a three-month-old infant due to severe cardiac condition.
Table 2.
Electrocardiogram, transthoracic echocardiogram alterations of acute Chagas' disease patients before and after treatment
| Variable | Group (n = 63) | ||
|---|---|---|---|
| Pre-treatment | Post-treatment | ||
| Electrocardiogram | (n = 63) | (n = 48) | |
| Ventricular reporalization alteration | 8 (13%) | 4 (8%) | |
| Left anterior fascicular block | 1 (2%) | 1 (2%) | |
| Right bundle branch block | 1 (2%) | 1 (2%) | |
| Right bundle branch block + left anterior fascicular block | 2 (3%) | 2 (4%) | |
| Low QRS voltage | 2 (3%) | - | |
| Bradycardia | - | 3 (6%) | |
| Incomplete right bundle branch block | 1 (2%) | 2 (4%) | |
| Ventricular extrasystols | 1 (2%) | 1 (2%) | |
| Atrial fibrillation | 1 (2%) | - | |
| Tachycardia | 2 (3%) | - | |
| Normal | 44 (70%) | 34 (71%) | |
| Echocardiogram | (n = 31) | (n = 25) | |
| Pericardial effusion | 3 (10%) | - | |
| Left ventricular dysfunction | 1 (3%) | - | |
| Normal | 27 (87%) | 25 (100%) | |
Data are expressed as frequency and in parenthesis are the corresponding percentage for each group.
Cardiac evaluation in Group 2 (post-treatment)
The follow up cardiac evaluation was done at least one year after the end of the treatment regimen established. It occurred in a mean period of 15.5 months. It was possible to reevaluate 48 patients with ECG and 25 with TTE. Among the 48 patients that were evaluated with an ECG, 35 were normal in the pre-treatment period, of the 30 (86%) continued with normal results and 5 (14%) presented alterations in the post-treatment period. Thirteen patients had alterations in ECG before treatment, 9 (69%) of them remained altered and 4 (31%) evolved to a normal ECG. Also, during the pre-treatment period, 4 (16%) out of the 25 patients reevaluated had abnormalities examined in TTE and all of them evolved completely after treatment (Table 3 and 4).
Table 3.
Frequency of ECG results before and after treatment
| Pre-treatment ECG | Post-treatment ECG | |||||
|---|---|---|---|---|---|---|
| Normal | % | Altered | % | Total | ||
| Normal | 30 | 62.5 | 5 | 10.4 | 35 | |
| Altered | 4 | 8.3 | 9 | 18.7 | 13 | |
| Total | 34 | - | 14 | - | 48 | |
ECG: electrocardiogram.
Table 4.
Frequency of TTE results before and after treatment
| Pre-treatment TTE | Post-treatment TTE | |||||
|---|---|---|---|---|---|---|
| Normal | % | Altered | % | Total | ||
| Normal | 21 | 86.9 | 0 | - | 21 | |
| Altered | 4 | 13.1 | 0 | - | 4 | |
| Total | 25 | - | 0 | - | 23 | |
TTE: transthoracic echocardiogram
Discussion
Case distribution, route of transmission and T. cruzi strain
CD in the Brazilian Amazon Region has changed its epidemiological profile in the past several years and most of the cases as being acute and due to oral transmission. A peculiarity of our region is the distance between the municipality of the outbreaks occurrence and the state's capital, Manaus. Therefore, most patients are unable to travel and get the complete cardiac follow-up.
During the period that comprised the study, 2007 to 2015, four outbreaks of six already registered in the Amazonas state with a total of 85 cases reported. All of them somehow associated with oral transmission due to açaí consumption. Most times, individuals don't present cardiac alterations during the acute phase, thus, it's thought that our region presents milder symptoms that might be associated with the T. cruzi DTU present in the Brazilian Amazon.
We observed that only one patient was diagnosed by an immunological assay (IgM anti-T. cruzi) while all the others had their diagnosis confirmed by thick blood smear. This can be related to the intense qualification of microscopists and all health professionals working in the Malaria Laboratory at the Tropical Medicine Foundation. Considering that most patients arrive with febrile syndrome mostly suspected to malaria infection, they are constantly being trained for the identification of the protozoan Trypanosoma cruzi which allows improving the surveillance of acute cases of CD in the state.24
In our study population, we were able to find that among acute cases that had Trypanosoma cruzi strain identified, TcIV was present in patients from outbreaks. This is best described by Monteiro et al.21 Although TcI and Z3 (TcIII/TcIV) have also been identified in humans,22 the pathogenicity of these strains is still not well known, but it's believed to be the cause of low morbidity when compared to endemic areas that present other strain of T. cruzi, TcII.25
Evaluation of cardiac alterations during the pre-treatment and post-treatment stages
Cardiac alterations during acute phase though in small proportion (33%) has highlighted the importance of continuous investigation for chronic chagasic cardiopathy, as it is not certain that treatment with benznidazole can indeed eliminate the chance of the patient not evolving to a chronic condition of the disease.6,26
Analyzing the demographical variables with the presence of any cardiac alterations due to acute infection by T. cruzi, it is possible to observe a significant statistical result for the Central Amazonas mesoregion (p = 0.020) and the isolated cases (p = 0.044). Although it's possible to think that the higher frequency of cardiopathy in the Central mesoregion might be due to the location of state's capital, Manaus, the number of cardiopathy cases in Manaus was very low (n = 4).
Also, higher frequency of cardiopathy reported in isolated acute cases (48%) might suggest a possible association either by oral or classical vector transmission with the strain of the protozoan, for which TcI was already found in all isolated cases of CD, associated to chronic CD and Chagas cardiomyopathy.27,28 And the strain TcIV has been reported in outbreaks.21 But this association is not possible to affirm considering the low number of patients with identified strain of the parasite.
During cardiac evaluation of the acute phase, most of the patients presented normality in both ECG or TTE examination. In the post-treatment period, we observed that most of the patients evolved to a normal result in the cardiological examinations. Pericardial effusion resolved very well, but ventricular repolarization alteration remained in four patients even after treatment. A factor that has been reported in other follow-up examination of acute cases to be undefined due to an unfamiliarity of a predictor parameter of cure.6,13,14
Cardiac alterations in the state of Amazonas are not frequent, but the knowledge is still scarce regarding the whole transmission dynamic and possible influences in a long-term period. Acute cases reported in the neighboring state of Pará presented serious cardiac involvement, with three died due to severe myocarditis, renal failure and cardiac tamponade.19 In a study carried out by Ferreira et al.29 in the Amazon region, five cases were reported of which two were from Pará and three from Amazonas, all of them presented reversed cardiac alterations and no deaths. In this study, one death was registered in a three-month-old infant, who presented a cardiogenic shock and meningoencephalitis due vector transmission with the presence of chagoma, a localized swelling at the site of inoculation. This remarkable difference suggests that the clinical manifestations and mortality is lower in the state of Amazonas, though is unknown the reason.
Study limitations
This was a unicentric longitudinal study, with a small study population and most of the participants living in the countryside of the state. These factors didn't allow a complete follow-up, contributing to a loss of patients. Also, it was possible to obtain the strains of the parasite only from patients that were recruited more recently, which limited the genetic characterization.
Conclusion
In our study, we demonstrated the presence of 33% of patient with cardiac alterations in the acute phase of CD. Although most of the cases were located in the Southwest mesoregion, the higher frequency of cardiac alterations belonged to the Central Amazonas mesoregion and isolated acute cases.
Although cardiac alterations were present in low frequency during the pre-treatment phase, this clinical condition suggests that there is a new epidemiological profile in the state of Amazonas which differs with the profile present in neighbouring states. This changing scenario might be associated with the T. cruzi strain, but no more can be specified. Most patients followed up in this study had a successful outcome, however, in some of them, the cardiac alterations persisted or even, developed afterwards.
Therefore, it is evident the need to reinforce surveillance actions for immediate diagnosis and treatment, as well as long-term and continuous cardiac, follow up of patients with acute CD in order establish preventive measures and improve the prognosis of this group of patients in our region.
Footnotes
Sources of Funding
This study was funded by FAPEAM - Fundação de Amparo à Pesquisa do Estado do Amazonas.
Study Association
This study is not associated with any thesis or dissertation work.
Author contributions
Conception and design of the research and acquisition of data: Pereira BVM; analysis and interpretation of the data: Ortiz JV, Ferreira JMBB; statistical analysis: Ortiz JV, Lira EF; obtaining funding: Ferreira JMBB; writing of the manuscript: Ortiz JV, Couceiro KN, Doria SS, Silva PRL; critical revision of the manuscript for intellectual content: Ortiz JV, Couceiro KN, Silva e Silva MRH, Doria SS, Silva PRL, Guerra MGVB, Guerra JAO, Ferreira JMBB.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Chagas C. Nova tripanozomiaze humana: estudos sobre a morfolojia e o ciclo evolutivo do Schizotrypanum cruzi n. gen., n. sp., ajente etiolojico de nova entidade morbida do homem. Mem Inst Oswaldo Cruz. 1909;1(2):159–218. [Google Scholar]
- 2.World Health Organization (WHO) Integrating neglected tropical diseases into global health and development: fourth WHO report on neglected tropical diseases. Geneva: World Health Organization; 2017. [Google Scholar]
- 3.Andrade DV, Gollob KJ, Dutra WO. Acute Chagas disease: new global challenges for an old neglected disease. PLoS Negl Trop Dis. 2014;8(7):e3010. doi: 10.1371/journal.pntd.0003010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rassi Jr A, Rassi A, Marin-Neto JA. Chagas disease. Lancet. 2010;375(9723):1388–1402. doi: 10.1016/S0140-6736(10)60061-X. [DOI] [PubMed] [Google Scholar]
- 5.Souza-Lima RC, Barbosa MD, Coura JR, Arcanjo AR, Nascimento AS, Ferreira JM, et al. Outbreak of acute Chagas disease associated with oral transmission in the Rio Negro region, Brazilian Amazon. Rev Soc Bras Med Trop. 2013;46(4):510–514. doi: 10.1590/0037-8682-1367-2013. [DOI] [PubMed] [Google Scholar]
- 6.Pinto AY, Valente VC, Coura JR, Valente SA, Junqueira AC, Santos LC, et al. Clinical follow-up of responses to treatment with benznidazol in Amazon: a cohort study of acute Chagas disease. PLoS One. 2013;8(5):e64450. doi: 10.1371/journal.pone.0064450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tibayrenc M. Genetic epiddemiology of parasitic protozoa and other infectious agents: the need for an integrated approach. Int J Parasitol. 1998;28(1):85–104. doi: 10.1016/s0020-7519(97)00180-x. [DOI] [PubMed] [Google Scholar]
- 8.Zingales B, Andrade SG, Briones MRS, Campbell DA, Chiari E, Fernandes O, et al. A new consensus for Trypanosoma cruzi intraspecific nomenclature: second revision meeting recommends TcI to TcIV. Mem Inst Oswaldo Cruz. 2009;104(7):1051–1054. doi: 10.1590/s0074-02762009000700021. [DOI] [PubMed] [Google Scholar]
- 9.Pinto AY, Valente SA, Valente VC, Ferreira Jr AG, Coura JR. Acute phase of Chagas disease in the Brazilian Amazon region: study of 233 cases from Pará, Amapá and Maranhão observed between 1988 and 2005. Rev Soc Bras Med Trop. 2008;41(6):602–614. doi: 10.1590/s0037-86822008000600011. [DOI] [PubMed] [Google Scholar]
- 10.Pinto AYN, Farias JR, Marçal AS, Galúcio AL, Costi RR, Valente VC, et al. Serious acute chagas disease authoctonous from Brazilian Amazon. Rev Para Med. 2007;21(2):1–10. [Google Scholar]
- 11.Pinto AYN, Harada GS, Valente VC, Abud JEA, Gomes FS, Souza GCR, et al. Cardiac attacks in patients with acute Chagas' disease in microepidemic familiar episode, in Abaetetuba City, Brazilian Amazon. Rev Soc Bras Med Trop. 2001;34(5):413–419. doi: 10.1590/s0037-86822001000500003. [DOI] [PubMed] [Google Scholar]
- 12.Pinto AY, Valente SA, Valente VC. Emerging acute Chagas disese in Amazonian Brazil: case reports with serious cardiac involvement. Braz J Infect Dis. 2004;8(6):454–460. doi: 10.1590/s1413-86702004000600010. [DOI] [PubMed] [Google Scholar]
- 13.Pinto AY, Ferreira Jr AG, Valente VC, Harada GS, Valente SAS. Urban outbreak of acute Chagas disease in Amazon region of Brazil?: four-year follow-up after treatment with benznidazole. Rev Panam Salud Publica. 2009;25(1):77–83. doi: 10.1590/s1020-49892009000100012. [DOI] [PubMed] [Google Scholar]
- 14.Pinto AYN, Ferreira SMAG, Valente SAS, Valente VC, Ferreira Jr AG. Electrocardiographic changes during and after benznidazole treatment against acute-stage Chagas disease indigenous to the Brazilian Amazon. Rev Pan-Amaz Saude. 2010;1(2):67–76. [Google Scholar]
- 15.Shaw J, Laison R, Fraiha H. Observations on the epidemiology of the first autochthonous cases of Chagas' disease in Belém, State of Pará, Brazil. Rev Saúde Publica. 1969;3(2):153–157. [PubMed] [Google Scholar]
- 16.França MS, Frade JM, Konasugawa K, Almeida FB. Doença de Chagas: primeiro caso autóctone na Amazônia Ocidental, Amazonas, Brasil. Acta Amaz. 1980;10(4):759–762. [Google Scholar]
- 17.Nobrega AA, Garcia MH, Tatto E, Obara MT, Costa E, Sobel J, et al. Oral transmission of Chagas disease by consumption of açaí palm fruit, Brazil. Emerg Infect Dis. 2009;15(4):653–655. doi: 10.3201/eid1504.081450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pereira KS, Schmidt FL, Guaraldo AM, Franco RM, Dias VL, Passos LA. Chagas' disease as a foodborne illness. J Food Prot. 2009;72(2):441–446. doi: 10.4315/0362-028x-72.2.441. [DOI] [PubMed] [Google Scholar]
- 19.Silva GM Sperandio da, Mediano MFF, Hasslocher-Moreno AM, Holanda MT, Sousa A Silvestre de, Sangenis LHC, et al. Benznidazole treatment safety: the Médecins Sans Frontieres experience in a large cohort of Bolivian patients with Chagas' disease. J Antimicrob Chemother. 2017;72(9):2596–2601. doi: 10.1093/jac/dkx180. [DOI] [PubMed] [Google Scholar]
- 20.Monteiro WM, Barbosa MGV, Toledo MJO, Fé FA, Fé NF. Series of acute Chagas' disease cases attended at a tertiary-level clinic in Manaus, State of Amazonas, from 1980 to 2006. Rev Soc Bras Med Trop. 2010;43(2):207–210. doi: 10.1590/s0037-86822010000200021. [DOI] [PubMed] [Google Scholar]
- 21.Monteiro WM, Magalhães LK, Sá AR, Gomes ML, Toledo MJ, Borges L, et al. Trypanosoma cruzi IV causing outbreaks of acute chagas disease and infections by different haplotypes in the Western Brazilian Amazonia. PLoS One. 2012;7(7):e41284. doi: 10.1371/journal.pone.0041284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monteiro WM, Magalhães LK, Santana Filho FS, Borborema M, Silveira H, Barbosa MD. Trypanosoma cruzi TcIII/Z3 genotype as agent of an outbreak of Chagas disease in the Brazilian Western Amazonia. Trop Med Int Health. 2010;15(9):1049–1051. doi: 10.1111/j.1365-3156.2010.02577.x. [DOI] [PubMed] [Google Scholar]
- 23.Dias JCP, Ramos Jr. AN, Gontijo ED, Luquetti A, Shikanai-Yasuda MA, Coura JR, et al. Brazilian Consensus on Chagas Disease, 2015. Epidemiol Serv Saúde. 2016;25(esp):7–86. doi: 10.5123/S1679-49742016000500002. [DOI] [PubMed] [Google Scholar]
- 24.Barbosa MGV, Ferreira JMBB, Arcanjo ARL, Santana RAG, Magalhães LKC, Magalhães LKC, et al. Chagas disease in the state of Amazonas: history, epidemiological evolution, risks of endemicity and future perspectives. Rev Soc Bras Med Trop. 2015;48(Suppl. 1):27–33. doi: 10.1590/0037-8682-0258-2013. [DOI] [PubMed] [Google Scholar]
- 25.Aguilar HM, Abad-Franch F, Dias JCP, Junqueira ACV, Coura JR. Chagas disease in the Amazon Region. Mem Inst Oswaldo Cruz. 2007;102(Suppl. I):47–56. doi: 10.1590/s0074-02762007005000098. [DOI] [PubMed] [Google Scholar]
- 26.Antunes AF, Maduro SG, Pereira BV, Barbosa MD, Guerra JA, Ferreira JM. Chronic heart disease after treatment of oral acute Chagas disease. Arq Bras Cardiol. 2016;107(2):184–186. doi: 10.5935/abc.20160115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Santana RA, Magalhães LK, Magalhães LKC, Prestes SR, Maciel MG, Silva GA, et al. Trypanosoma cruzi strain TcI is associated with chronic Chagas disease in the Brazilian Amazon. Parasit Vectors. 2014 Jun 11;7:267–267. doi: 10.1186/1756-3305-7-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramirez JD, Guhl F, Rendón LM, Rosas F, Marin-Neto JA, Morillo CA. Chagas cardiomyopathy manifestations and Trypanosoma cruzi genotypes circulating in chronic chagasic patients. PLoS Negl Trop Dis. 2010;4(11):e899. doi: 10.1371/journal.pntd.0000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barbosa-Ferreira JM, Guerra JA, Santana Filho FS, Magalhães BM, Coelho LI, Barbosa MD. Cardiac involvement in acute Chagas' disease cases in the Amazon Region. Arq Bras Cardiol. 2010;94(6):147–149. doi: 10.1590/s0066-782x2010000600023. [DOI] [PubMed] [Google Scholar]