Abstract
Body packing is one of the common ways to traffic illicit drugs. Drug mules usually swallow or insert drugs within the gastrointestinal tract or other orifices. Detection of such drug packets has become difficult because of the constantly improving packaging techniques and the sophistication used by traffickers. Suspected obstruction or perforated hollow viscus requires employment of appropriate radiological procedures and techniques for accurate detection and precise diagnosis. A delay diagnosis and inappropriate action may carry disastrous physical consequences for the body packers. It is crucial for radiologists to acquire enough experience to deduce different types of drug packets from their imaging characteristics and to accurately guide emergency physicians and security officials. The packets are not always radiodense, therefore they can be difficult to detect on conventional abdominal radiographs. In this report, the authors illustrate 5 cases with different packaging methods and materials that give rise to radiological challenges.
Keywords: Body packer, Illicit drug smuggling, Imaging modalities
Introduction
Thousands of body packers every year risk their lives, their health, and their freedom for illegal drugs transportation to cross high-security port of entries worldwide such as airports. Body packing is the concealment of illicit drugs within the gastrointestinal tract or other orifices [1]. The material of the drug packets is mostly made with latex sheath given to its waterproof nature, more sophisticated packets may use hollow pellets. Predominantly, latex material includes the usage of latex gloves fingers, balloons, or multilayered condoms [2]. These packets are usually tightly packed, tiny and tapered at both ends, they are varied in size from handmade diverse to machine-made forms [1], [2], [3], [4]. Compare to genital inserted packets, oral ingested packets are usually smaller in size and relatively round in shape. However, the size, weight, and amount of the ingested packets are mostly dependent on the type of illicit drugs, the size of the body packer, and sophistication of the packaging skills [5].
Packets with fewer layers or loosely packed (eg, condoms) are highly prone to leakage, tearing, bursting, and rupture. Such kinds of packets are life-threatening and can lead to disastrous physical consequences including death. On the other hand, when drug is wrapped by thicker packaging medium or special materials, it can be difficult to detect by conventional imaging techniques. Also, their prompt and accurate detection depend on the experience of the radiologist, the material used and even the clinical information provided prior to radiological examinations. The purpose of this report is to present different packaging techniques that give rise to radiological challenges.
Case reports
Five body packing cases are presented in this study. All of the body packers were male, age between 25 to 40. They were suspected of drug smuggling and were brought to our emergency department (ED) by Dubai airport police. On presentation, three of the suspects were conscious, vitally stable and oriented. One of them presented to ED with bowel obstruction and one was unconscious. All expelled, surgically or endoscopically removed packets were collected, sealed and handed over to the anti-narcotics department at police authority for further lab analysis. Upon recovery, all suspects were also handed over to the anti-narcotics department at police authority.
Case 1
A 26-year-old male was escorted by airport police to hospital due to suspicious behavior at the airport after landing. He was suspected of body packing but without abdominal pain nor vomiting. Plain abdominal X-ray was performed. The examination shows multiple, well-defined, oval shaped, and radiopaque packets within large colon (Fig. 1). He was admitted under the care of general surgery as a case of drug carrier. After given lactulose 30 mL BD, suspect passed drug packets and a follow-up plain X-ray revealed no further packets. At the time of discharge, suspect was doing well, mobilizing with no active complaints. He was subsequently handed over to police authorities.
Fig. 1.
X-ray abdomen supine shows typical tic-tac sign packets within large colon.
Case 2
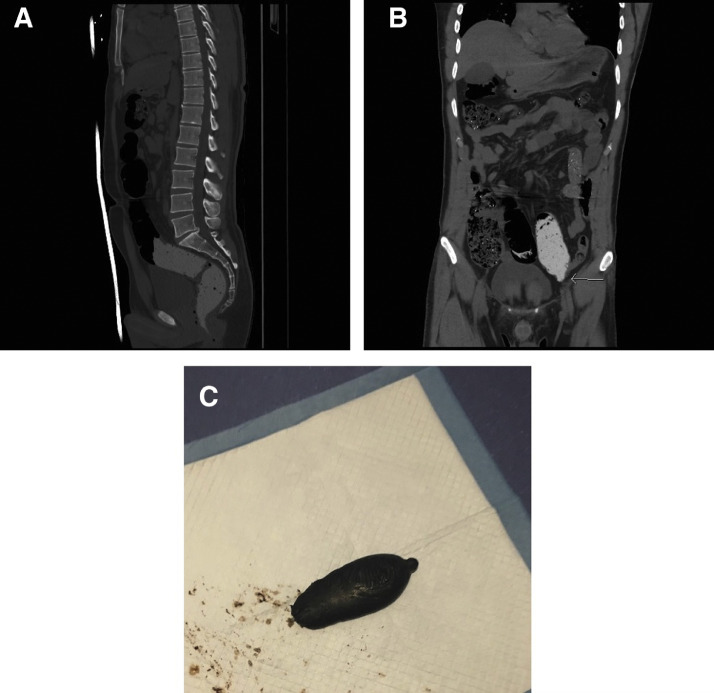
A 36-year-old male vomited once during the flight and later found uncommunicative and unresponsive to voice in his seat on a flight landing at Dubai. He was immediately taken to our hospital after landing. Upon arrival in ED, he was unconscious with Glasgow Coma Scale 9/15. Hypertonia, clonus, and sweaty were noticed. On examination, the pupils were symmetrically moderately dilated and nonreactive. He was intubated and mechanically ventilated with stable vital signs (heart rate: 100 bmp, blood pressure: 116/79 mm Hg, oxygen saturation: 100%, body temperature: 36.4°C). His abdomen was rigid with absent bowel sounds. Some stool mixed with blood and some plastic materials was passed. At this point, he was suspected of being a body packer with rupture of packets. Noncontrasted computed tomography (CT) brain was performed and the result was unremarkable. Noncontrast abdominal CT shows high-density foreign body filling the anal canal, rectum, and sigmoid colon with resultant dilatation of the sigmoid colon (Fig. 2A). There is also similar high-density foreign body seen in colon descent which has nipple on the one end that appears to be a condom (Fig. 2B). An emergency colonoscopy was performed. One large (15 cm × 6 cm) plastic bag filled with dark material (Fig. 2C) removed from the rectum and another large plastic bag filled with dark material was at 60 cm of anal verge between descending and transverse colon. Colonoscopy showed inflamed rectal mucosa with ulcer and sticky dark material on the wall. He was kept in the intensive care unit after colonoscopy for around a week, during which he was kept on regular bowel wash. Suspect physical condition gradually improved, extubated and was shifted later on to general ward. He was well at the time of discharge. Without the need of follow-up plan, he was handed over to police authorities. The foreign bodies that retrieved by colonoscopy were later proved to be paste of heroin.
Fig. 2.
Noncontrast CT abdomen sagittal in (A) and coronal in (B) showing high-density foreign body filling the anal canal, rectum, and sigmoid colon. A 15 cm × 6 cm retrieved foreign body specimen in (C).
Case 3
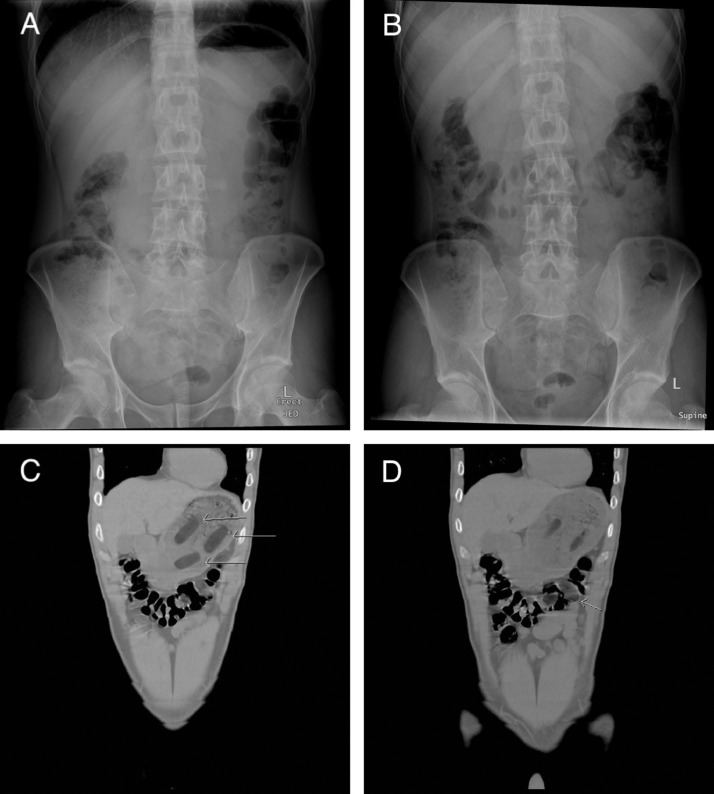
A 29-year-old male was brought from airport police to ED with suspicion of foreign body ingestion. On examination, the suspect was afebrile, his chest was clear and abdomen was soft and lax. Abdominal radiographs (Fig. 3A, B) could not reveal any radiopaque foreign bodies in gastrointestinal tract and shows no signs of bowel obstruction or perforation. Noncontrast abdominal CT (Fig. 3C, D) reveals multiple spherical and cylindrical shaped hypodense, almost same sized foreign bodies with −200 to −220 HU density in stomach, small and large bowel. In view of highly suspicious history of the patient and CT density of the foreign bodies, radiological impression of ingested drug capsule possibly pure cocaine with radiolucent packing material was given. Suspect was given lactulose and passed a large number of packets. CT follow-up revealed no remaining packets in abdomen or pelvis. Suspect was generally well, vitally stable, afebrile, on full diet, and passing stools at the time of discharge.
Fig. 3.
X-ray abdomen erect in (A) and supine in (B) that shows no radiodense foreign bodies in gastrointestinal tract. Noncontrast CT abdomen coronal in (C) and (D) showing multiple spherical and cylindrical shaped foreign bodies in stomach, small and large bowel.
Case 4
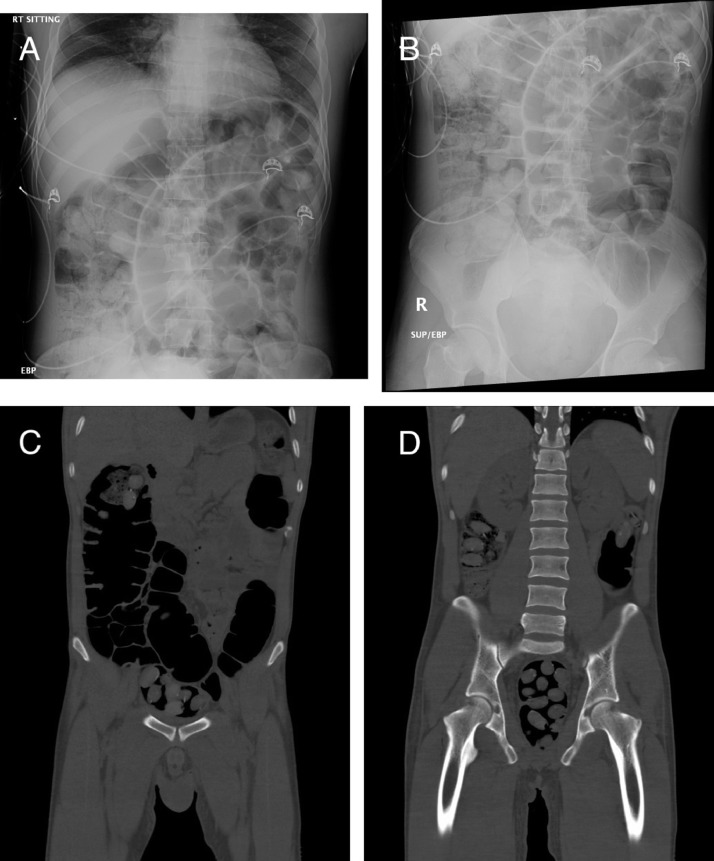
A 32-year-old male was taken to airport terminal clinic by ground staff due to nausea, abdominal pain, and distension as soon as he was landed at the airport. Suspect revealed that he had swollen drug packets. He was immediately brought to hospital as his condition worsened. Plain abdominal X-ray was done and it shows multiple ovoid and uniformly shaped packets in large bowel presented with intestinal obstruction (Fig. 4A, B). Noncontrast abdominal CT (Fig. 4C, D) shows multiple well-circumscribed, low-density oval foreign bodies, uniform in size scattered in loops of large bowel. General surgeon decided on laparotomy for removal of the drug packets. Fifty drug packets were extracted in the rectum, sigmoid, ascending transverse, and descending colon. Hugely dilated large bowel and moderately dilated small bowel were noticed. After operation, he was kept in intensive care unit 24 hours for observation. Further clinical course was unremarkable. He was discharged 7 days after operation and subsequently handed over to police authorities.
Fig. 4.
X-ray abdomen supine in (A) and erect in (B) showing multiple ovoid and uniformly shaped packets in large bowel with intestinal obstruction. Noncontrast CT abdomen coronal in (C) and (D) showing numerous, well-defined and low-density oval-shaped foreign bodies in large bowel.
Case 5
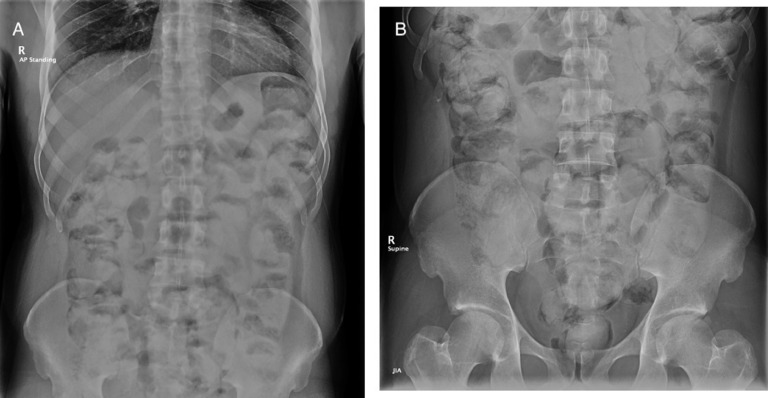
A 34-year-old male brought to hospital by airport security personnel for screening as there was intelligence input regarding body packing on certain flight routes. Suspect admitted ingestion of 45 cocaine packets and was brought to our hospital. On presentation, suspect was vitally stable, well-oriented, and exhibited no abdominal distension but with mild abdominal pain. Plain abdominal X-ray shows multiple radiopaque foreign bodies with unusual appearances (round and oblong) in large and small bowel (Fig. 5A, B). He was referred to general surgery department and given lactulose. He passed 45 drug packets in the hospital stay and a follow-up X-ray was done. No remaining packets were found and suspect was doing well at the time of discharge.
Fig. 5.
X-ray abdomen erect in (A) and supine in (B) showing multiple radiopaque foreign bodies in large and small bowel.
Discussion
One of the noninvasive, rapid, and widely available radiological examination to rule out body packer is plain abdominal X-ray. It is a relative accessible and low cost method for screening and diagnosing body packers with accuracy of 40%-90% [6]. The accuracy, however, can be strongly influenced by factors like drug packaging methods and the masking skill of the smugglers. Usually, the signs of drug packets on plain abdominal X-ray appear as numerous, radiopaque, regular in shape with similar dimensions (Fig. 1). Such ingested drug packets may also be noticeable by the presence of following signs: air trapped at tapered end of a package (“rosette sign”) [7], [8]; thin air trapped between multiple layers of latex that forms a crescent of air fringing an ovoid opacity (“double condom sign”) [9], [10]; multiple spherical or cylindrical shaped packages all through the abdomen (“tic-tac sign”) (Fig. 1) [11]; packages that are arranged in parallel within the bowel lumen (“parallelism”) [11]; and the sign of dense surrounding wrapping material [2], [12]. If one or more of these signs are present, the finding can be confirmed as positive. In the past, drugs were usually loosely packed and amateurishly wrapped in multiple layers of condoms or tightly packed and wrapped in multiple layers of latex gloves [2]. In both methods, the packages were tied at the end. Such drug packets are easily visible under plain X-ray film as rim of air trapped between the wrapping layers (the “double condom sign”) [9], [10] and in knots (the “rosette sign”) [7], [8]. Newer packaging techniques sophisticatedly combine different material, such as plastic film, aluminum foil, and other medium [2], [13] to lower the detectability by reducing the radiodensity of ingested drug packets. Using machines in drug filling process to extract the air between layers of latex further the detection difficulties for radiologists as the typical visible signs are eliminated [4], [10]. Body packers may mask the packets by ingesting oil, water, or other liquid as all have similar radio densities on plain abdominal X-ray [13]. In such cases, it is difficult to delineate the drug packets and to differentiate the packet from the usual bowel contents [10], [13]. By using drug induced constipation, drug packets can be also masked within ample surrounded stool [2].
All these newer packaging and masking methods inevitably decrease the detection rate in plain abdominal X-ray. Abdominal X-ray is still commonly performed for a person with suspicion of body packing even it may be inconclusive due to overlap of air, feces, and other dense structures [14]. With a sensitivity of 95.6%-100% [2], [6], CT abdominal examination is a more accurate imaging modality in detecting the retention of drug packets due to its high contrast resolution and ability to differentiate densities of drug packets from their adjacent tissues by measuring their Hounsfield unit (HU) [1], [10], [15]. According to a study, CT can be used to distinguish different types of drugs by their HUs: cocaine is less dense than fat (−219 HU), cannabis shows a density similar to bone (700 HU), and heroin is between the density of fat and air (−520 HU) [6], [15], [16].
CT scan without contrast is sufficient for the detection of drug packets. To acquire a better view of body packing, an adjustment of usual abdominal CT setting with window width 350 HU and window level 50 HU together with lung setting with window width 1000 HU and window level 2700 HU is important [17]. CT scan should be conducted without oral or rectal contrast medium as it obscures ingested drug packets due to the similarities in density [6]. In our case studies, CT scans were performed without any contrast medium.
Sonography is another useful modality in detecting the presence of drug packets in body packers as it is low cost and radiation free [6]. Without exposure to radiation, abdominal ultrasound is especially valuable to examine female suspects who claim to be pregnant. As ultrasound is sensitive in detecting free fluid, the presence of free fluid not only can indicate bowel perforation, it also acts as window to reveal more clearly the presence of drug packets [6], [20], [21]. One study shows that the accuracy of using ultrasound in detecting ingested drug packets as high as 94% [22], [23]. Despite all these advantages, using abdominal ultrasound in detecting sparsely scattered drug packets can be time consuming and requires experience of the radiologists [10]. Compact feces and gas surrounding drug packages in the intestinal lumen may reduce diagnostic accuracy [24]. Abdominal ultrasound also fails to identify the number of ingested packets [10]. Therefore, plain abdominal X-ray film is comparatively a better method in detecting drug packets. Till now, there are only few studies that provide data to support its use [25].
Magnetic resonance imaging (MRI) is not a suitable modality in detecting body packets as it has few limitations. MRI is usually available only within service hour and it poses harm to body packers if the packaging material contains ferromagnetic materials. Patient cooperation is required during examination, as by moving, MR images can become nondiagnostic.
Body packing is a one of the common way to smuggle drugs across the border via air traffic. As the smugglers continue to improve their packaging techniques to disguise the ingested drug packets, it is very important for radiologist to familiarize themselves with the signs of ingested drug packets and to acquire enough experience to interpret the plain abdominal X-ray film for correct diagnoses [18]. In our institution, when suspected body packer is brought to the hospital without symptoms of drug toxicity, intestinal obstruction or perforated hollow viscus, a plain abdominal X-ray is first performed. In highly suspicious case with negative finding in X-ray film, nonenhanced CT abdominal scan is conducted with appropriate window settings [10], [17]. In comparison, CT scan is superior to plain abdominal X-ray as it yields higher contrast resolution images and provides accurate information of the location, size, and amount of drug packages. Use of CT scan for detecting drug packets not only allows us to assess associated complications like bowel obstruction or perforation quickly, it also allows us to handle the intoxicated patient promptly due to ruptured packages [10], [19]. In spite of all the advantages provided by CT scan, we are currently using plain abdominal X-ray for initial screening. Using CT scan to search for body packets is extremely accurate, but it is also associated with comparatively high radiation doses [10], [11]. Therefore, it should be taken into consideration, which imaging techniques should be used to produce a high level of accuracy with the lowest possible burden on the patients.
Conclusion
Illicit drug smuggling represents a hazardous activity with potentially high physical risks. The radiologist must be aware of the eventual consequences, as the use of adequate imaging methods is essential for prompt detection of these ingested smuggled materials.
Footnotes
Declarations of interest: None.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2019.03.002.
Appendix. Supplementary materials
References
- 1.Traub S.J., Hoffman R.S., Nelson L.S. Body packing—the internal concealment of illicit drugs. N Engl J Med. 2003;349(26):2519–2526. doi: 10.1056/NEJMra022719. [DOI] [PubMed] [Google Scholar]
- 2.McCarron M.M., Wood J.D. The cocaine ‘bodypacker’ syndrome. Diagnosis and treatment. JAMA. 1983;250(11):1417–1420. [PubMed] [Google Scholar]
- 3.Pidoto R.R., Agliata A.M., Bertolini R., Mainini A., Rossi G., Giani G. A new method of packaging cocaine for international traffic and implications for the management of cocaine body packers. J Emerg Med. 2002;23(2):149–153. doi: 10.1016/s0736-4679(02)00505-x. [DOI] [PubMed] [Google Scholar]
- 4.Prabhu R., Ne'eman A., Bier K., Patel N. Radiology of body packers: the detection of internally concealed illegal materials. Appl Radiol. 2008;37(5):26–28. [Google Scholar]
- 5.Hergan K., Kofler K., Oser W. Drug smuggling by body packing: what radiologists should know about it. Eur Radiol. 2004;14(4):736–742. doi: 10.1007/s00330-003-2091-5. [DOI] [PubMed] [Google Scholar]
- 6.Pinto A., Reginelli A., Pinto F., Sica G., Scaglione M., Berger F.H. Radio-logical and practical aspects of body packing. Br J Radiol. 2014;87(1036) doi: 10.1259/bjr.20130500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sinner W.N. The gastrointestinal tract as a vehicle for drug smuggling. Gastrointest Radiol. 1981;6(4):319–323. doi: 10.1007/BF01890277. [DOI] [PubMed] [Google Scholar]
- 8.Traub S.J., Kohn G.L., Hoffman R., Nelson L.S. Pediatric “body packing”. Arch Pediatr Adolesc Med. 2003;157(2):174–177. doi: 10.1001/archpedi.157.2.174. [DOI] [PubMed] [Google Scholar]
- 9.Chaljub G., Shah R.K., Limon D., Ozkan O.S., Marroquin S. CT of small bowel obstruction secondary to a cocaine-filled condom. Emerg Radiol. 2002;9(6):333–335. doi: 10.1007/s10140-002-0257-0. [DOI] [PubMed] [Google Scholar]
- 10.Sica G., Guida F., Bocchini G., Iaselli F., Iadevito I., Scaglione M. Imaging of drug smuggling by body packing. Semin Ultras CT MR. 2015;36(1):39–47. doi: 10.1053/j.sult.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Niewiarowski S., Gogbashian A., Afaq A., Kantor R., Win Z. Abdominal X-ray signs of intra-intestinal drug smuggling. J Forensic Leg Med. 2010;17(4):198–202. doi: 10.1016/j.jflm.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 12.Poletti P.-A., Canel L., Becker C.D. Screening of illegal intracorporeal containers (“body packing”): is abdominal radiography sufficiently accurate? A comparative study with low-dose CT. Radiology. 2012;265(3):772–779. doi: 10.1148/radiol.12112767. [DOI] [PubMed] [Google Scholar]
- 13.Shahnazi M., Taheri M.S., Pourghorban R. Body packing and its radiologic manifestations: a review article. Iran J Radiol. 2011;8(4):205–210. doi: 10.5812/iranjradiol.4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ross S., Hatch G., Preiss U., Ruder T., Thali M., Patak M., M.D . RSNA; 2010. CT best at uncovering drug mule payload.https://press.rsna.org/timssnet/media/pressreleases/pr_target.cfm?ID=517 [online] Available at: [Accessed 27 Jan. 2019] [Google Scholar]
- 15.Wong G.C.K., Lai K.K., Chung C.H. Management of body packers in the emergency department. Hong Kong J Emerg Med. 2005;12(2):112–118. [Google Scholar]
- 16.Wackerle B., Rupp N., von Clarmann M., Kahn T., Heller H., Feurbach S. Demonstration of narcotic packages in “body packers” by various imaging methods. In vitro and in vivo investigations. Fortschr Roengenstr. 1986;145:274–277. doi: 10.1055/s-2008-1048932. In German. [DOI] [PubMed] [Google Scholar]
- 17.Booker R.J.S.J., Smith J.E., Rodger M.P. Packers, pushers and stuffers—managing patients with concealed drugs in UK emergency departments: a clinical and medicolegal review. Emerg Med J. 2009;26(4):316–320. doi: 10.1136/emj.2008.057695. [DOI] [PubMed] [Google Scholar]
- 18.Cappelletti S., Piacentino D., Ciallella C. Systematic review of drug packaging methods in body packing and pushing: a need for a new classification. Am J Forensic Med Pathol. 2018 doi: 10.1097/PAF.0000000000000436. [DOI] [PubMed] [Google Scholar]
- 19.Bulakci M., Kalelioglu T., Bulakci B.B., Kiris A. Comparison of diagnostic value of multidetector computed tomography and X-ray in the detection of body packing. Eur J Radiol. 2013;82(8):1248–1254. doi: 10.1016/j.ejrad.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 20.Grassi R., Di Mizio R., Pinto A., Cioffi A., Romano L., Rotondo A. Sixty-one consecutive patients with gastrointestinal perforation: comparison of conventional radiology, ultrasonography, and computerized tomography, in terms of the timing of the study. Radiol Med. 1996;91(6):747–755. [PubMed] [Google Scholar]
- 21.Catalano O., Grassi R., Rotondo A. Diagnosis of free air in the abdomen. Role of echography. Radiol Med. 1994;87(5):632–635. [PubMed] [Google Scholar]
- 22.Meijer R., Bots M. Detection of intestinal drug containers by ultrasound scanning: an airport screening tool? Eur Radiol. 2003;13(6):1312–1315. doi: 10.1007/s00330-002-1689-3. [DOI] [PubMed] [Google Scholar]
- 23.Pärtan G., Lomoschitz K., Pamberger P., Bauer W., Hruby W. ECR 2004, March 5-9. 2004. Body packing: radiology in the social problem of drug smuggling. Vienna, Austria URL: https://posterng.netkey.at/esr/viewing/index.php?module=viewing\_poster&task=viewsection&pi=3355&ti=16177&searchkey= [Google Scholar]
- 24.Hierholzer J., Cordes M., Tantow H., Keske U., Mäurer J., Felix R. Drug smuggling by ingested cocaine-filled packages: conventional x-ray and ultrasound. Abdom Imaging. 1995;20(4):333–338. doi: 10.1007/BF00203366. [DOI] [PubMed] [Google Scholar]
- 25.Soriano-Perez M.J., Serrano-Carrillo J.L., Marin-Montin I., Cruz-Caballero A. Hashish body packing: a case report. Case Rep Med. 2009 doi: 10.1155/2009/712573. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.