Abstract
Background:
Heart failure (HF), a serious and costly condition, is increasingly prevalent. We estimated the US burden including emergency department (ED) visits, inpatient hospitalizations and associated costs, and mortality.
Methods and Results:
We analyzed 2006–2014 data from the Healthcare Cost and Utilization Project’s (HCUP) Nationwide ED Sample, the HCUP National (Nationwide) Inpatient Sample, and the National Vital Statistics System. ICD codes identified HF and comorbidities. Burden was estimated separately for ED visits, hospitalizations, and mortality. In addition, criteria were applied to identify total unique acute events. Rates of “primary HF” (primary diagnosis or underlying cause of death) and “comorbid HF” (comorbid diagnosis or contributing cause of death) were calculated, age-standardized to the 2010 US population. In 2014, there were an estimated 1,068,412 ED visits, 978,135 hospitalizations, and 83,705 deaths with primary HF. There were 4,071,546 ED visits, 3,370,856 hospitalizations, and 230,963 deaths with comorbid HF. Between 2006–2014, the total unique acute event rate for primary HF declined from 536 to 449 per 100,000 [Relative percent change (RPC) of −16%, p for trend <0.001], but increased for comorbid HF from 1,467 to1,689 per 100,000 (RPC 15%, p for trend<0.001). HF-related mortality decreased significantly from 2006–2009 but did not change meaningfully after 2009. For hospitalizations with primary HF, the estimated mean cost was $11,552 in 2014, totaling an estimated $11 billion.
Conclusions:
Given substantial healthcare and mortality burden of HF, rising healthcare costs, and the aging US population, continued improvements in HF prevention, management, and surveillance are important.
Keywords: heart failure, surveillance, hospitalization, mortality
Introduction
In the United States, heart failure (HF) affects approximately 6.5 million adults,1 and lifetime risk of HF is estimated to be one in five at age 40.2 Incidence of HF increases with age, and HF prevalence in the aging US population is projected to increase 46% between 2012 and 2030.3 Older adults diagnosed with HF have a 5-year mortality approaching 50%.4, 5 Total direct medical costs of HF were estimated at $30.7 billion in 2012, and are projected to increase by nearly 127% to $69.7 billion by 2030.3
Evidence-based interventions exist to prevent or manage HF, yet suboptimal care has been cited as a reason for poor HF-related outcomes in the US.6 For example, despite many HF hospitalizations being considered preventable,6 HF is the leading cause of hospitalization among older adults and Medicare beneficiaries with HF have the highest readmission rate of any condition.7 In response, reducing preventable hospitalizations has been made a national priority. This includes creating the Hospital Readmission Reduction Program (HRRP) through the enactment of the Patient Protection and Affordable Care Act in 2010.8, 9 Effective October 1, 2012, the HRRP requires CMS to reduce payments to hospitals with excess readmissions for certain conditions, including HF.10
Although HF has considerable health and economic impact, and reducing the burden of HF hospitalizations has been the focus of legislative, policy, and public health attention, there is no comprehensive national surveillance system to track HF-related healthcare and mortality burden across all ages and all health insurance provider types in the United States. The purpose of this study was to address this surveillance gap using national Healthcare Cost and Utilization Project (HCUP) and National Vital Statistics System data from 2006–2014. Specifically, we aimed to describe the burden of HF in emergency department (ED) visits, inpatient hospitalizations and costs, and mortality, including both primary HF events and events in which HF was listed as a comorbidity.
Methods
Using data from the HCUP Nationwide Emergency Department Sample (NEDS), the National (Nationwide) Inpatient Sample (NIS), and the National Vital Statistics System (NVSS), this cross-sectional study examined ED visits, hospitalizations, and deaths, respectively, during 2006–2014. The largest all-payer ED database in the US, the NEDS includes data from approximately 30 million annual discharges across 950 hospitals in 30 states. These data approximate a 20% stratified sample of US hospital-based EDs, and are weighted to produce national estimates.11 The NIS includes data from over 7 million hospitalizations annually, and is the largest publicly-available all-payer inpatient healthcare database in the US. Data approximate a 20% stratified sample of discharges from US community hospitals (including teaching hospitals, but excluding rehabilitation and long-term acute care hospitals), and are weighted to produce national estimates of hospitalizations.12 The NIS was re-designed in 2012, and the Agency for Healthcare Research and Quality (AHRQ) developed trend weights to make estimates comparable for data prior to 2012. Created by the National Center for Health Statistics, the NVSS collects data from death certificates filed in every US state and the District of Columbia.13 All events for US adults aged ≥18 years were included. The data used are publicly available to other researchers, and analytic methods will be shared upon request for the purpose of reproducing results.
Conditions of interest were identified by applying adapted Clinical Classification Software (CCS) codes, created by AHRQ (Supplemental Table 1). HF was defined using the CCS code 108 [excluding International Classification of Disease (ICD)-9 Clinical Modification code 398.91; Rheumatic HF] and ICD-9 of 402.01, 402.11, 402.91, 404.11, 404.13, 404.91, 404.93 for the NEDS and NIS, and using ICD-10 code I50, I11.0, I13.0, I13.2 for the NVSS. Events for which HF was listed as a primary diagnosis or underlying cause of death (referred to throughout as “primary HF”) were examined separately from events for which HF was listed as a comorbid diagnosis or contributing cause of death (referred to as “comorbid HF”). Due to uncertainty regarding the accuracy of HF coded as an underlying cause of death,14, 15 we examined trends in combined HF-related deaths (listed as either an underlying or contributing cause of death), in addition to reporting primary or comorbid HF deaths separately. Additional conditions that have been associated with HF, including those affecting the lungs [asthma, chronic obstructive pulmonary disease (COPD), pneumonia], cardiometabolic conditions [atrial fibrillation and flutter (AF), chronic kidney disease (CKD), diabetes, hypertension, ischemic heart disease (IHD), stroke (both ischemic and hemorrhagic)] and mental health conditions (depression, dementia or Alzheimer’s), were examined as both primary and comorbid diagnoses.1, 16
Event totals were calculated for each event type (ED visits, hospitalizations, and deaths), to examine overall health system and mortality burden related to HF. For these analyses, hospitalization totals included both elective and acute hospitalizations, as both types of hospitalization contribute to burden and cost.
For a second set of analyses examining trends over time, exclusion criteria were applied to each event type to identify “unique” (mutually exclusive) events, to avoid double-counting, and to identify “acute” events (so that observed temporal changes would not be confounded by shifts in management of elective procedures in the inpatient or outpatient setting). To do this, ED visits that resulted in hospitalization, transfer to another facility, or death were excluded, as were hospitalizations that resulted in transfer to another hospital or death, or hospitalizations that were reported as elective.17, 18 Thus, unique ED visits, unique acute hospitalizations, and deaths were summed to estimate the overall “unique acute event” burden, which reflects the total number of acute events that could be targeted by public health and health system prevention efforts. In addition, estimating unique acute events allowed us to assess trends in “treat and release” ED visits (i.e., ED visits that did not result in hospitalization, transfer, or death), which are of interest given the unique role of the ED, the cost implications of ED use for patients and the healthcare system, the number of patients who need care but may not be ill enough for inpatient admission, and also recent speculation that hospitals may be increasing the use of the ED and observation-service in order to avoid inpatient admissions.19, 20
Hospitalization costs were estimated from total charges using hospital-level cost-to-charge ratios provided by HCUP. Charges represent what the hospital billed for the case and do not include professional (physician) fees. Cost-to-charge ratio data were not available for ED visits, so ED costs could not be estimated.
Event rates were calculated using intercensal population estimates as the denominators,21, 22 and were standardized by age to the 2010 US population. To identify different patterns in HF rates, we conducted trend analyses based on the age-standardized unique event rates using Joinpoint software (version 4.3.1.0 National Cancer Institute). Joinpoint regression fits a series of joined straight lines on a logarithmic scale to the trend data. Analyses were conducted in SAS 9.3-callable SUDAAN (Research Triangle Institute, Research Triangle Park, NC) to account for the multistage, disproportionate stratified sampling design of the HCUP datasets. T-tests or Wilcoxon rank-sum tests (2-sided) were used for statistical comparisons of continuous variables and chi-square tests were used for categorical variables. The data were de-identified and publicly available, and thus this project was determined not to be human subjects research.
Results
In 2014, there were nearly 1.1 million ED visits, 980,000 hospitalizations, and 84,000 deaths with primary HF (Table 1). In addition, there were approximately 4.1 million ED visits, 3.4 million hospitalizations and 231,000 deaths with comorbid HF (Table 2). As expected, patients with either primary or comorbid HF were significantly older than patients without HF, and approximately three quarters of ED visits and hospitalizations for both primary and comorbid HF were among Medicare beneficiaries (Tables 1 and 2). Among hospitalizations for primary HF, the most common comorbid diagnoses were hypertension (72%), IHD (56%), diabetes (48%), chronic kidney disease (47%), and AF (43%) (Table 1). Among deaths with comorbid HF, the most common underlying causes were IHD (44%), hypertension (21%), and COPD (21%) (Table 2).
Table 1.
Characteristics of patients age 18+ with heart failure as the primary diagnoses – Nationwide Emergency Department Sample 2014, National Inpatient Sample 2014, and National Vital Statistics System 2014
| Demographic | Emergency Department Visits | Hospitalizations | Deaths | |||
|---|---|---|---|---|---|---|
| Weighted % (Standard error) | Weighted % (Standard error) | % | ||||
| HF N=1,068,412 |
No HF N=106,386,429 |
HF N=978,135 |
No HF N=25,398,477 |
HF N=83,705 |
No HF N=2,275,039 |
|
| Mean age in years (SE) | 71.6 (0.2) | 46.4 (0.2) £ | 72.1 (0.1) | 54.7 (0.1)£ | 83.3 (0.04) | 73.1(0.01) £ |
| Age in groups | ||||||
| 18–44 | 4.7 (0.2) | 50.7 (0.3)£ | 4.2 (0.1) | 33.7 (0.2)£ | 0.8 | 6.1£ |
| 45–64 | 25.4 (0.5) | 29.2 (0.2)£ | 24.4 (0.2) | 30.1 (0.1)£ | 7.8 | 21.8£ |
| 65–74 | 21.2 (0.2) | 9.2 (0.1)£ | 21.7 (0.1) | 16.3 (0.1)£ | 11.1 | 18.8£ |
| 75–84 | 25.4 (0.3) | 6.8 (0.1)£ | 26.1 (0.2) | 12.5 (0.1)£ | 23.7 | 23.8§ |
| 85+ | 23.3 (0.4) | 4.2 (0.1)£ | 23.6 (0.2) | 7.4 (0.1)£ | 56.6 | 29.4£ |
| Men | 51.5 (0.2) | 42.5 (0.2)£ | 51.5 (0.2) | 39.7 (0.1)£ | 43.2 | 50.9£ |
| Age sex group | ||||||
| Men and age<65 | 18.5 (0.4) | 34.1 (0.2)£ | 17.6 (0.2) | 23.7 (0.1)£ | 5.3 | 17.3£ |
| Men and age≥65 | 33.0 (0.4) | 8.4 (0.1)£ | 33.9 (0.2) | 15.9 (0.1)£ | 37.8 | 33.6£ |
| Women and age<65 | 11.6 (0.3) | 45.8 (0.2)£ | 11.0 (0.1) | 40.1 (0.2)£ | 3.3 | 10.7£ |
| Women and age≥65 | 36.9 (0.3) | 11.7 (0.2)£ | 37.6 (0.2) | 20.2 (0.1)£ | 53.6 | 38.4£ |
| Health insurance | ||||||
| Medicare | 73.3 (0.6) | 25.6 (0.3)£ | 74.3 (0.3) | 41.2 (0.2)£ | NA | NA |
| Medicaid | 11.1 (0.5) | 25.6 (0.5)£ | 9.3 (0.2) | 19.4 (0.2)£ | NA | NA |
| Private | 10.3 (0.4) | 27.8 (0.5)£ | 11.6 (0.2) | 30.9 (0.3)£ | NA | NA |
| Other | 5.2 (0.3) | 20.8 (0.5)£ | 4.7 (0.1) | 8.2 (0.1)£ | NA | NA |
| Elective | NA | NA | 6.0 (0.2) | 27.2 (0.3)£ | NA | NA |
| Comorbidities identified by secondary diagnoses codes | ||||||
| Conditions affecting the lungs | ||||||
| Asthma | 7.6 (0.2) | 4.4 (0.1)£ | 8.0 (0.1) | 7.0 (0.1)£ | 0.28 | 0.38£ |
| COPD | 28.9 (0.3) | 3.6 (0.1)£ | 31.3 (0.2) | 9.4 (0.1)£ | 6.0 | 9.8£ |
| Pneumonia | 11.7 (0.2) | 1.0 (0.02)£ | 13.6 (0.1) | 4.2 (0.03)£ | 4.6 | 6.0£ |
| Cardiometabolic conditions | ||||||
| Chronic kidney disease | 40.4 (0.4) | 3.0 (0.1)£ | 46.5 (0.2) | 10.0 (0.1)£ | 4.1 | 2.8£ |
| Atrial fibrillation or flutter | 37.8 (0.4) | 2.4 (0.1)£ | 42.9 (0.2) | 7.7 (0.1)£ | 4.4 | 4.0£ |
| Diabetes | 45.2 (0.3) | 11.3 (0.1)£ | 47.9 (0.2) | 22.6 (0.1)£ | 6.6 | 8.8£ |
| Hypertension | 70.4 (0.4) | 24.0 (0.3)£ | 72.1 (0.2) | 47.0 (0.2)£ | 19.0 | 15.0£ |
| Ischemic heart disease | 51.1 (0.4) | 5.6 (0.1)£ | 56.4 (0.2) | 15.2 (0.1)£ | 0.03 | 18.9£ |
| Stroke | 0.41 (0.01) | 0.16 (0.01)£ | 0.5 (0.02) | 0.69 (0.01)£ | 2.6 | 8.2£ |
| Mental Health Conditions | ||||||
| Dementia or Alzheimer’s | 8.6 (0.1) | 2.1 (0.04)£ | 9.4 (0.1) | 6.0 (0.05)£ | 7.3 | 15.2£ |
| Depression | 10.2 (0.2) | 6.0 (0.2)£ | 11.8 (0.1) | 14.3 (0.1)£ | 0.3 | 0.6£ |
| None of above conditions | 5.4 (0.2) | 64.0 (0.5)£ | 2.0 (0.04) | 34.0 (0.2)£ | 60.9 | 42.1£ |
P<0.001;
P<0.05; P-values for comparison of hospitalizations with or without HF, using T-test for continuous variables and Chi-square test for categorical variables. HF= Heart Failure. Patients with primary or comorbid HF were excluded from “No HF” group.
Table 2.
Characteristics of patients age 18+ with comorbid heart failure – Nationwide Emergency Department Sample, National Inpatient Sample and National Vital Statistics System, 2014
| Demographic | Emergency Department Visits | Hospitalizations | Deaths | |||
|---|---|---|---|---|---|---|
| Weighted % (Standard error) | Weighted % (Standard error) | % | ||||
| HF N=4,071,546 |
No HF N=106,386,429 |
HF N=3,370,856 |
No HF N= 25,398,477 |
HF N=230,963 |
No HF N=2,275,039 |
|
| Mean age in years (SE) | 70.8 (0.2) | 46.4 (0.2)£ | 72.1 (0.1) | 54.7 (0.1)£ | 81.2 (0.03) | 73.1 (0.01)£ |
| Age in groups | ||||||
| 18–44 | 5.1 (0.1) | 50.7 (0.3)£ | 3.5 (0.05) | 33.7 (0.2)£ | 0.9 | 6.1£ |
| 45–64 | 27.1 (0.4) | 29.2 (0.2)£ | 24.1 (0.2) | 30.2 (0.1)£ | 9.4 | 21.8£ |
| 65–74 | 21.8 (0.1) | 9.2 (0.1)£ | 23.8 (0.1) | 16.3 (0.1)£ | 14.7 | 18.8£ |
| 75–84 | 24.6 (0.2) | 6.8 (0.1)£ | 26.8 (0.1) | 12.5 (0.1)£ | 27.4 | 23.8£ |
| 85+ | 21.5 (0.4) | 4.2 (0.1)£ | 21.8 (0.2) | 7.4 (0.1)£ | 47.6 | 29.4£ |
| Men | 47.0 (0.2) | 42.5 (0.2)£ | 48.9 (0.1) | 39.7 (0.1)£ | 48.7 | 50.9£ |
| Age sex group | ||||||
| Men and age<65 | 16.9 (0.3) | 34.1 (0.2)£ | 15.3 (0.1) | 23.7 (0.1)£ | 6.4 | 17.3£ |
| Men and age≥65 | 30.1 (0.3) | 8.4 (0.1)£ | 33.5 (0.1) | 15.9 (0.1)£ | 42.3 | 33.6£ |
| Women and age<65 | 15.3 (0.3) | 45.8 (0.2)£ | 12.2 (0.1) | 40.1 (0.2)£ | 3.9 | 10.7£ |
| Women and age≥65 | 37.8 (0.3) | 11.7 (0.2)£ | 38.9 (0.1) | 20.2 (0.1)£ | 47.4 | 38.4£ |
| Health insurance | ||||||
| Medicare | 74.7 (0.5) | 25.6 (0.3)£ | 77.1 (0.2) | 41.2 (0.2)£ | NA | NA |
| Medicaid | 10.9 (0.3) | 25.6 (0.5)£ | 8.1 (0.1) | 19.5 (0.2)£ | NA | NA |
| Private | 10.0 (0.4) | 27.8 (0.5)£ | 11.2 (0.2) | 30.9 (0.3)£ | NA | NA |
| Other | 4.3 (0.3) | 20.8 (0.5)£ | 3.5 (0.1) | 8.2 (0.1)£ | NA | NA |
| Elective | NA | NA | 11.7 (0.2) | 27.2 (0.3)£ | NA | NA |
| As the primary diagnoses and HF as comorbidity | ||||||
| Conditions affecting the lungs | ||||||
| Asthma | 1.27 (0.04) | 1.12 (0.03)£ | 1.07 (0.02) | 0.79 (0.01)£ | 0.46 | 0.38£ |
| COPD | 5.3 (0.1) | 1.5 (0.02)£ | 4.7 (0.05) | 1.7 (0.02)£ | 20.5 | 9.8£ |
| Pneumonia | 4.8 (0.1) | 0.96 (0.01)£ | 5.8 (0.1) | 2.4 (0.02)£ | 6.8 | 6.0£ |
| Cardiometabolic conditions | ||||||
| Chronic kidney disease | 0.20 (0.02) | 0.05 (0.01)£ | 0.14 (0.01) | 0.06 (0.01)£ | 8.2 | 2.8£ |
| Atrial fibrillation | 3.6 (0.05) | 0.43 (0.01)£ | 4.6 (0.04) | 1.2 (0.01)£ | 18.3 | 4.0£ |
| Diabetes | 1.97 (0.03) | 1.0 (0.01)£ | 1.96 (0.02) | 1.80 (0.01)£ | 17.9 | 8.8£ |
| Hypertension | 1.91 (0.1) | 0.95 (0.01)£ | 1.6 (0.1) | 0.66 (0.01)£ | 21.3 | 15.0£ |
| Ischemic heart disease | 5.5 (0.1) | 0.69 (0.01)£ | 8.2 (0.1) | 2.9 (0.04)£ | 43.8 | 18.9£ |
| Stroke | 1.86 (0.03) | 0.55 (0.01)£ | 2.4 (0.03) | 2.0 (0.02)£ | 6.0 | 8.2£ |
| Mental Health Conditions | ||||||
| Dementia or Alzheimer’s | 0.32 (0. 01) | 0.20 (0.004)£ | 0.35 (0.01) | 0.38 (0.01)£ | 13.3 | 15.2£ |
| Depression | 0.25 (0.01) | 1.11 (0.04)£ | 0.38 (0.01) | 2.8 (0.1)£ | 0.6 | 0.6 |
| None of above conditions | 73.1 (0.2) | 91.4 (0.1)£ | 68.6 (0.1) | 83.4 (0.1)£ | 14.2 | 42.1£ |
P<0.001;
P<0.05;
P-values for comparison of hospitalizations with or without HF, using T-test for continuous variables and Chi-square test for categorical variables. HF = Heart Failure. Patients with HF as the primary diagnosis were excluded from this table.
The majority (82%) of ED visits for primary HF resulted in hospital admission or transfer to another facility (Table 3). For all hospitalizations with primary HF, the median length of stay was 3 days (interquartile range 2–6), the estimated mean cost was approximately $11,552 (standard error $163), and the total estimated cost was $11.3 billion in 2014 (cost * estimated number of primary HF hospitalizations). Among patients with a primary diagnosis of asthma, COPD, pneumonia, AF, diabetes, IHD, stroke, or depression, the presence of comorbid HF was associated with significantly higher hospitalization cost compared to patients with these primary diagnoses but without HF (p<0.001 for all).
Table 3.
Emergency department and hospitalization outcomes, charges, and costs among patients with or without heart failure, by primary diagnosis or comorbid condition, Nationwide Emergency Department Sample 2014 and National Inpatient Sample 2014
| Weighted Mean or Percent (Standard Error) | ||||
|---|---|---|---|---|
| Emergency Department Visits | Hospitalizations | |||
| Primary HF | No HF++ | Primary HF | No HF++ | |
| Total | ||||
| Admitted to hospital or transferred, % | 82.1 (0.4) | 15.7 (0.2)£ | 3.0 (0.1) | 1.8 (0.02)£ |
| Died, % | 0.11 (0.01) | 0.16 (0.004) | 2.9 (0.05) | 1.7 (0.02)£ |
| Median length of stay, days (IQR) | NA | NA | 3 (2–6) | 3 (1–5)£ |
| Total charge, mean (SE) | 3127 (86) | 3289 (77)£ | 44841 (794) | 42549 (506) |
| Total cost, mean (SE) | NA | NA | 11552 (163) | 11059 (91) |
| Comorbid HF* | No HF | Comorbid HF* | No HF | |
| Conditions affecting the lungs | ||||
| Asthma | ||||
| Admitted to hospital or transferred, % | 67.2 (1.3) | 16.2 (0.4)£ | 1.00 (0.1) | 0.64 (0.04)§ |
| Died, % | + | + | 1.40 (0.1) | 0.32 (0.03)£ |
| Median length of stay, days (IQR) | NA | NA | 3 (2–6) | 2 (1–4)£ |
| Total charge, mean (SE) | 3440 (129) | 2699 (95)£ | 38062 (830) | 26288 (376)£ |
| Total cost, mean (SE) | NA | NA | 9691 (165) | 6739 (57)£ |
| COPD | ||||
| Admitted to hospital or transferred, % | 68.7 (0.7) | 24.8 (0.5)£ | 1.7 (0.09) | 1.1 (0.04)£ |
| Died, % | + | 0.02 (0.002) | 1.7 (0.08) | 0.9 (0.04)£ |
| Median length of stay, days (IQR) | NA | NA | 3 (2–5) | 3 (2–4)£ |
| Total charge, mean (SE) | 3306 (79) | 2934 (67)£ | 34781 (465) | 28094 (330)£ |
| Total cost, mean (SE) | NA | NA | 9111 (78) | 7539 (68)£ |
| Pneumonia | ||||
| Admitted to hospital or transferred, % | 90.7 (0.3) | 53.7 (0.6)£ | 2.7 (0.1) | 2.2 (0.1)£ |
| Died, % | 0.12 (0.02) | 0.07 (0.01)§ | 4.9 (0.1) | 2.5 (0.05)£ |
| Median length of stay, days (IQR) | NA | NA | 4 (3–7) | 3 (2–5)£ |
| Total charge, mean (SE) | 2633 (68) | 3260 (70)£ | 44977 (584) | 34005 (369)£ |
| Total cost, mean (SE) | NA | NA | 12240 (112) | 9284 (76)£ |
| Cardiometabolic conditions | ||||
| Chronic kidney disease (CKD) | ||||
| Admitted to hospital or transferred, % | 45.4 (3.3) | 20.1 (3.3)£ | + | + |
| Died, % | + | + | 4.2 (0.7) | 3.5 (0.5) |
| Median length of stay, days (IQR) | NA | NA | 3 (1–6) | 2 (0–4)£ |
| Total charge, mean (SE) | 4350 (313) | 4337 (327) | 40386 (2855) | 46863 (4714) |
| Total cost, mean (SE) | NA | NA | 10782 (711) | 12875 (1359) |
| Atrial fibrillation or flutter | ||||
| Admitted to hospital or transferred, % | 86.3 (0.4) | 54.8 (0.8)£ | 2.9 (0.1) | 2.0 (0.07)£ |
| Died, % | + | 0.04 (0.01) | 1.5 (0.07) | 0.63 (0.03)£ |
| Median length of stay, days (IQR) | NA | NA | 3 (2–5) | 2 (1–3)£ |
| Total charge, mean (SE) | 3263 (97) | 4279 (102)£ | 42640 (655) | 30565 (470)£ |
| Total cost, mean (SE) | NA | NA | 10942 (115) | 7699 (82)£ |
| Diabetes | ||||
| Admitted to hospital or transferred, % | 66.8 (1.0) | 38.2 (0.5)£ | 1.8 (0.1) | 1.2 (0.04)£ |
| Died, % | + | 0.03 (0.004) | 1.6 (0.1) | 0.4 (0.02)£ |
| Median length of stay, days (IQR) | NA | NA | 4 (2–8) | 3 (1–5)£ |
| Total charge, mean (SE) | 3153 (85) | 3154 (83) | 55272 (986) | 36778 (472)£ |
| Total cost, mean (SE) | NA | NA | 13996 (186) | 9369 (87)£ |
| Hypertension | ||||
| Admitted to hospital or transferred, % | 63.8 (1.1) | 15.5 (0.4)£ | 1.3 (0.1) | 1.1 (0.1) |
| Died, % | + | 0.03 (0.004) | 1.2 (0.1) | 0.5 (0.04)£ |
| Median length of stay, days (IQR) | NA | NA | 3 (2–5) | 2 (1–4)£ |
| Total charge, mean (SE) | 3715 (103) | 3379 (88)£ | 41256 (778) | 39425 (953) |
| Total cost, mean (SE) | NA | NA | 10279 (157) | 9891 (235) |
| Ischemic heart disease | ||||
| Admitted to hospital or transferred, % | 92.4 (0.3) | 80.0 (0.5)£ | 7.2 (0.2) | 7.0 (0.2) |
| Died, % | 0.3 (0.03) | 0.7 (0.03)£ | 6.1 (0.1) | 2.3 (0.04)£ |
| Median length of stay, days (IQR) | NA | NA | 4 (2–7) | 2 (1–4)£ |
| Total charge, mean (SE) | 4024 (133) | 7282 (252)£ | 98091 (1600) | 77239 (891)£ |
| Total cost, mean (SE) | NA | NA | 24091 (289) | 19163 (139)£ |
| Stroke | ||||
| Admitted to hospital or transferred, % | 95.9 (0.2) | 89.7 (0.3)£ | 2.7 (0.1) | 3.2 (0.1)§ |
| Died, % | 0.25 (0.04) | 0.39 (0.02)§ | 10.2 (0.2) | 7.3 (0.1)£ |
| Median length of stay, days (IQR) | NA | NA | 4 (2–7) | 3 (2–6)£ |
| Total charge, mean (SE) | 3002 (119) | 4270 (111)£ | 66653 (1453) | 60682 (1207)£ |
| Total cost, mean (SE) | NA | NA | 16816 (279) | 15037 (227)£ |
| Mental Health Conditions | ||||
| Dementia or Alzheimer’s | ||||
| Admitted to hospital or transferred, % | 66.5 (1.6) | 34.6 (1.0)£ | 6.1 (0.6) | 4.4 (0.2)§ |
| Died, % | + | + | 2.7 (0.4) | 1.7 (0.1)§ |
| Median length of stay, days (IQR) | NA | NA | 6 (3.0–11) | 6 (3.0–12)£ |
| Total charge, mean (SE) | 3478 (145) | 3739 (101)£ | 33030 (980) | 32589 (731) |
| Total cost, mean (SE) | NA | NA | 9901 (358) | 9395 (188) |
| Depression | ||||
| Admitted to hospital or transferred, % | 69.2 (2.0) | 43.6 (1.4)£ | 6.7 (0.5) | 1.9 (0.1)£ |
| Died, % | + | + | + | + |
| Median length of stay, days (IQR) | NA | NA | 6 (3–10) | 4 (3–7)£ |
| Total charge, mean (SE) | 2564 (106) | 2401 (97)£ | 26992 (710) | 19071 (412)£ |
| Total cost, mean (SE) | NA | NA | 7600 (187) | 5400 (104)£ |
Not reportable based on the estimates with a relative standard error greater than 0.30.
P<0.001;
P<0.05. HF = Heart Failure. IQR=Interquartile range.
These columns include all events with primary and comorbid diagnosis other than HF for rows pertaining to “Total” events.
Results for patients with or without HF as a secondary diagnosis, “comorbid HF”, exclude patients with HF as a primary diagnosis.
There were approximately 1.1 million total unique acute events with primary HF, and 4.3 million total unique acute events with comorbid HF, in 2014 (Table 4). Overall, the age-standardized total unique primary HF event rate (including ED visits, hospitalizations, and deaths) declined significantly from 536 to 449 per 100,000 population between 2006–2014 [Relative Percent Change (RPC) of −16%, p for trend<0.001, Figure 1, Supplemental Table 2]. For comorbid HF, the total unique acute event rate increased significantly from 1,467 to 1,689 per 100,000 between 2006 and 2014 (RPC of 15%, p for trend<0.001).
Table 4.
The unique acute event burden of heart failure, Nationwide Emergency Department Sample 2014, National Inpatient Sample 2014 and National Vital Statistics System 2014
| Total HF, Primary Diagnosis | Total HF, Comorbid Diagnosis | |||||
|---|---|---|---|---|---|---|
| N | % | Rate/100,000 people | N | % | Rate/100,000 people | |
| Total*% | 1,140,891 | 449 | 4,289,755 | 1689 | ||
| ED | 190,310 | 16.7 | 75 | 1,350,516 | 31.5 | 535 |
| Hospitalization+ | 866,875 | 76.0 | 341 | 2,708,276 | 63.1 | 1063 |
| Deaths | 83,705 | 7.3 | 33 | 230,963 | 5.4 | 91 |
| Age | ||||||
| 18–44 | 50,046 | 4.4 | 43 | 212,468 | 5.0 | 184 |
| 45–64 | 276,634 | 24.2 | 331 | 1,133,177 | 26.4 | 1357 |
| 65–74 | 235,473 | 20.6 | 892 | 934,271 | 21.8 | 3539 |
| 75–84 | 288,917 | 25.3 | 2112 | 1,057,136 | 24.6 | 7726 |
| 85+ | 289,820 | 25.4 | 4703 | 952,703 | 22.2 | 15460 |
| Sex* | ||||||
| Men | 579,637 | 50.8 | 514 | 2,019,984 | 47.1 | 1785 |
| Women | 561,253 | 49.2 | 393 | 2,269,771 | 52.9 | 1607 |
| Age sex group | ||||||
| Men and age<65 | 200,796 | 17.6 | 203 | 708,391 | 16.5 | 716 |
| Men and age≥65 | 378,842 | 33.2 | 1862 | 1,311,592 | 30.6 | 6445 |
| Women and age<65 | 125,884 | 11.0 | 126 | 637,253 | 14.9 | 637 |
| Women and age≥65 | 435,369 | 38.2 | 1682 | 1,632,518 | 38.1 | 6305 |
Standardized by age to the 2010 U.S. Census Population distribution among adults aged ≥18 years;
Non-elective hospitalizations; The crude age-sex specific rates were reported for sub group estimates.
Figure 1: Trends in total unique acute heart failure event rates, by age group and primary versus comorbid diagnosis – Nationwide Emergency Department Sample, National (Nationwide) Inpatient Sample and National Vital Statistics System, 2006–2014.
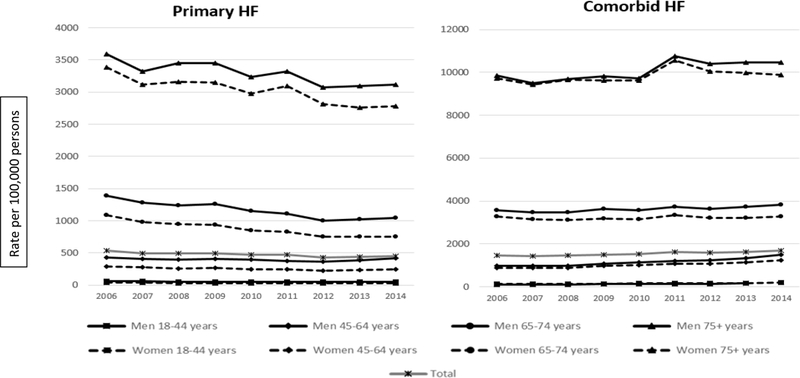
Totals standardized by age to the 2010 U.S. Census Population distribution among adults aged ≥18 years. Crude age-sex specific rates were reported for sub group estimates. Includes combination of emergency department visits, acute hospitalizations, and deaths. HF=heart failure. See Supplemental Table 4 for detailed numeric results.
Trends in unique acute hospitalizations and ED visits (i.e., “treat and release” ED visits) were examined to assess whether burden may have shifted from the inpatient to the ED setting. While the unique acute hospitalization rate for primary HF declined significantly from 427 to 341 per 100,000 (RPC of −20%, p for trend<0.001, Figure 2, Supplemental Table 3), the “treat and release” ED visit rate for primary HF also declined significantly between 2006 to 2011 (78 to 63 per 100,000, p for trend<0.001) and then did not change significantly (75 per 100,000 in 2014, p for trend=0.1). Thus, while possible, it does not appear likely that a decline in primary HF hospitalizations was created by shifting burden to the ED in the form of primary HF “treat and release” ED visits. While comorbid treat and release ED visits did increase during this time (from 308 to 535 per 100,000, RPC of 74%, p for trend<0.001, Figure 2, Supplemental Table 4), there was no evidence of a change in the slope of increase in comorbid HF ED visits at the time of HRRP implementation, as might be expected if policy incentives were driving this increase.
Figure 2: Trends in unique “treat and release” ED visits, unique acute hospitalizations, and mortality, for HF – Nationwide Emergency Department Sample, National (Nationwide) Inpatient Sample and National Vital Statistics System, 2006–2014.
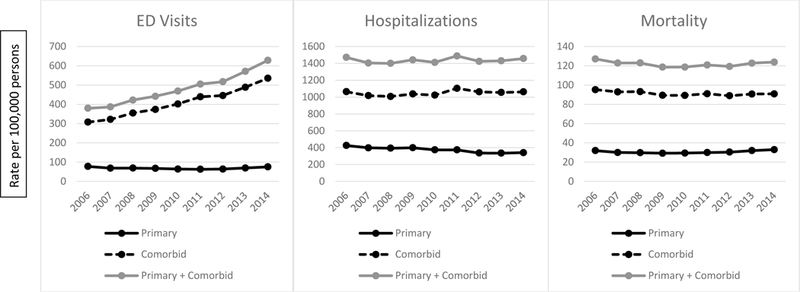
Totals standardized by age to the 2010 U.S. Census Population distribution among adults aged ≥18 years. HF=heart failure. See Supplemental Tables 2, 3, and 4 for detailed numeric results.
The total HF-related mortality rate (including both primary and comorbid HF) decreased significantly during 2006–2009 (127 to 119 per 100,000, p for trend<0.001), and then did not change meaningfully (124 per 100,000 in 2014, p for trend=0.1) (Figure 2). Combined HF-related event rates (including both primary and comorbid HF) for unique ED visits, hospitalizations, deaths, and total events, are presented in Supplemental Table 5 and Supplemental Figure 1.
Discussion
The burden of HF in the US is considerable. In 2014, there were around 1.1 million ED visits, 1.0 million hospitalizations, and 84,000 deaths with HF as the primary cause. In addition, there were an additional 4.1 million ED visits, 3.4 million hospitalizations, and 231,000 deaths with HF as a comorbid or contributing cause. For hospitalizations with primary HF, the estimated mean cost was $11,552 in 2014, with a total estimated cost of over $11 billion. Among hospitalizations for primary HF, the most common comorbid diagnoses were hypertension (almost 3 of every 4), IHD (over 1 of every 2), diabetes (nearly 1 of every 2), chronic kidney disease (nearly 1 of every 2), and AF (over 2 of every 5). Compared to patients without HF, patients who were hospitalized with comorbid HF had significantly higher costs for primary diagnoses of asthma, COPD, pneumonia, AF, diabetes, IHD, stroke, or depression.
Despite significant declines from 2006–2014, the total unique acute HF event burden remained high, with approximately 1.1 million primary HF events and 4.3 million comorbid HF events occurring in 2014. This includes the age-standardized rate of unique acute hospitalizations with primary HF declining significantly from 427 to 341 per 100,000 (RPC of 20% decline). While national initiatives such as the HRRP may have helped continue progress in reducing HF readmissions, including among Medicare beneficiaries as well as with broader spillover effects across the healthcare system,23 the rate of primary HF hospitalization was already decreasing at the time of implementation in 2012. This observation is consistent with other studies that have reported declines in HF hospitalization prior to recently implemented policy changes. For example, a 29.5% decline in age-, sex-, and race-adjusted HF hospitalization was observed between 1998 to 2008 in the Medicare population of adults aged 65 years and older,24 while a study using NIS data for all hospitalizations among adults aged 18 years and older showed an average annual rate of decline of 2.8% between 2001–2009.25
Declines in hospitalization burden are noteworthy, as survival of patients with HF has improved, and would be expected to increase HF prevalence and hospitalizations.4, 26 On the other hand, positive trends in some HF risk factors, such as better control of hypertension and declines in IHD, may be decreasing HF incidence and event burden.1 Changes in these risk factors may have substantial impact, as hypertension and IHD are estimated to each account for the development of about 20% of HF cases,27 and HF incidence has been steady or declining in recent decades.4, 28 Additionally, hospitalizations and outcomes for HF may be improved by better treatment, including newer treatment modalities such as implantable cardioverter defibrillators, cardiac resynchronization therapy, and left ventricular assist devices (LVAD), as well as better adherence to recommended guidelines for care such as use of β-blockers, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, and better care for comorbidities such as anticoagulant therapy for AF.26, 29, 30 Lastly, and potentially related to better management of HF, some HF care may have shifted to the outpatient setting, reducing inpatient hospitalizations.31
Better HF treatment and improved survival may have contributed to the observed increase in comorbid HF ED visits,26, 29 as patients living longer with HF would be expected to have more time to develop a need for emergency care for other conditions. In addition, it has been hypothesized that some hospitals might increase the use of ED treatment or observation-service in order to decrease HF readmissions.19, 32 (Observation-service may occur within or outside of the ED, and thus our unique “treat-and-release” ED estimates may have captured some but not all observation-service use.) In the present study, we did not observe evidence of this potential shift, given that the primary HF ED “treat and release” visit rate did not increase, and while the cormorbid HF ED visit rate did increase, there was no change in slope of the increase at the time of HRRP implementation. Using Medicare data, Zuckerman and colleagues reported increased use of observation-service and decreased readmissions for HRRP-targeted conditions, but no within-hospital association between increases in observation-service use and reductions in readmissions.33
In addition to potential changes in use of the ED and observation-service, it is possible that some hospitals may shift coding of HF from a primary to a comorbid diagnosis, and also that coding of HF as a comorbid diagnosis may be increasing more generally.34 However, the present study observed a stable rate of unique acute comorbid HF hospitalizations and a steady increase in the ED visit rate for comorbid HF. While some HF events may have shifted from being coded as primary to comorbid diagnoses, the increase in comorbid HF ED visits occurred steadily throughout the observation period, so is unlikely to be driven by recent policy changes.
Despite reported population trends of better management and improved survival, we observed a stalled decline in the age-standardized HF-related mortality rate, with a significant decrease from 2006 to 2009, followed by no significant changes from 2010–2014. Given that reporting guidelines indicate heart failure should not be listed as the underlying cause of death if another plausible cause is identified,35, 36 it is valuable to consider combined HF-related mortality, in which HF was listed as either an underlying or a contributing cause of death. Although not statistically significant, the observed recent increase in combined HF mortality after 2009 is consistent with other work.37 This increase is also consistent with the broader context of cardiovascular disease in the United States, which reveals increases in mortality between 2010–2014 for numerous cardiovascular conditions,38, 39 and may reflect health effects of ongoing population trends such as increasing physical inactivity, obesity, and diabetes.1 The stalled decline in HF-related mortality, despite improvements in treatment and decreases in primary HF hospitalization, highlights the need for HF prevention, better treatment of risk factors, and improved surveillance.26, 40
This study used nationally-weighted, all-payer databases to estimate the event burden of HF among US adults. While the data used were a key strength of the study, there were limitations. First, the NEDS and NIS are event-level databases, so patients could not be tracked over time, and patient-level information (such as prior events and diagnoses, or annual per-patient cost) was not available. Second, this study did not examine burden of HF in outpatient clinical settings; HF may be present in 1.6% of all outpatient visits, increasing to 5.9% of outpatient visits among those age 75 years and older.41 The present study also did not capture burden of HF in nursing homes or long-term care facilities, and cost estimates did not include physician fees, which are not captured in HCUP. For these reasons, the true healthcare and cost burden of HF is likely to be considerably higher than estimated in this paper. Third, criteria for identifying unique events excluded elective hospitalizations, because management of these events (within acute care hospitals or outpatient surgical centers) may vary over time, and unique acute events were examined from 2006–2014. Fourth, analyses relied on accurate coding of HF and other conditions of interest, and biases may have resulted from underreporting or changes in diagnosis or coding patterns over time.34, 42 Fifth, this study did not distinguish between stages or subcategories of HF. Sixth, this study did not examine hospital procedures during admissions, and because the data do not track patients over time, we were unable to examine longitudinal questions such as whether certain procedures were associated with subsequent reductions in readmissions.
In addition to the impact of HF on human health, the economic burden that HF places on the health care system has been described as “staggering”,43 and is projected to rise as the population ages and survival of HF patients improves.3 In 2008 dollars, the total lifetime cost of HF was estimated at over $100,000 per person, with the majority of this cost due to hospitalizations.43 Much of the financial burden falls to Medicare, as approximately three quarters of ED visits and hospitalizations with primary or comorbid HF were among Medicare beneficiaries. Many hospitalizations for HF are regarded as preventable,6 and efforts such as the HRRP have aimed to reduce burden and improve outcomes. However, further improvement is needed. Additional avenues are being explored, such as value-based models of care (including Hospital Value-Based Purchasing, Bundled Payments for Care Improvement, the Merit-Based Incentive Payment System, and Accountable Care Organizations),44 development and use of performance measures and performance improvement programs, and care coordination and transition programs, such as those that facilitate the hospital to home transition and provide in-home aftercare.3 Improved treatment modalities may also improve outcomes, and more patients are using LVAD as destination therapy rather than only as a bridge to transplant therapy.45, 46 Another potential avenue for improvement of HF outcomes is use of cardiac rehabilitation. Cardiac rehabilitation has been found to reduce hospitalization, is recommended for stable outpatients with HF, and is covered as a Medicare fee for service benefit, yet only one tenth of eligible HF patients receive a referral.47, 48 In addition, lack of medication adherence is one of the most common causes of cardiac decompensation and subsequent hospital admission,6 while having a pharmacist or nurse responsible for medication reconciliation can reduce medication errors and reduce hospital-level HF readmissions.49, 50 In conclusion, continued improvements in prevention, management, treatment, and surveillance of HF are important, given the considerable health impact of HF, the aging US population, and rising health care costs.
Supplementary Material
What is new?
Heart failure (HF) is burdensome and costly, yet a comprehensive national surveillance system is lacking.
We report primary (nearly 1.1 million emergency department (ED) visits, 1 million hospitalizations, and 80,000 deaths) and co-morbid (4 million ED visits, 3.4 million hospitalizations, and 230,000 deaths) HF burden in 2014.
Of hospitalizations with primary HF, the estimated mean cost was $11,552 in 2014, with a total estimated cost of over $11 billion; Medicare incurs the majority of this burden.
Between 2006–2014, the age-standardized total unique acute event rate for primary HF decreased, while the comorbid HF event rate increased.
What are the clinical implications?
While national initiatives such as the Hospital Readmissions Reduction Program may have supported progress in reducing HF readmissions, the rate of primary HF hospitalization was already decreasing at the time of implementation, and trends in HF-related ED visits, comorbid hospitalizations, and mortality have not improved.
Positive trends in some HF risk factors, such as declines in ischemic heart disease, may be decreasing HF incidence and event burden, while advances in HF management may be increasing survival and improving outcomes.
Given increasing HF prevalence and an aging US population, continued improvements in HF prevention, management, and surveillance are important.
Acknowledgments
Funding Sources
None
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of Interest Disclosures
None
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS and Muntner P. Heart Disease and Stroke Statistics—2017 Update: A Report From the American Heart Association. Circulation. 2017:e16–e458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D’Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ and Levy D. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068–3072. [DOI] [PubMed] [Google Scholar]
- 3.Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Pina IL and Trogdon JG. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circulation Heart failure. 2013;6:606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KKL, Murabito JM and Vasan RS. Long-Term Trends in the Incidence of and Survival with Heart Failure. New England Journal of Medicine. 2002;347:1397–1402. [DOI] [PubMed] [Google Scholar]
- 5.Gerber Y, Weston SA, Redfield MM, Chamberlain AM, Manemann SM, Jiang R, Killian JM and Roger VL. A Contemporary Appraisal of the Heart Failure Epidemic in Olmsted County, Minnesota, 2000–2010. JAMA internal medicine. 2015;175:996–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michalsen A, Konig G and Thimme W. Preventable causative factors leading to hospital admission with decompensated heart failure. Heart. 1998;80:437–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jencks SF, Williams MV and Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. New England Journal of Medicine. 2009;360:1418–1428. [DOI] [PubMed] [Google Scholar]
- 8.McIlvennan CK, Eapen ZJ and Allen LA. Hospital Readmissions Reduction Program. Circulation. 2015;131:1796–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Congress. Patient Protection and Affordable Care Act. Pub L. No. 111–148, 124 Stat. 408, § 3025. 2010. Accessed on December 13, 2017 https://www.congress.gov/111/plaws/publ148/PLAW-111publ148.pdf
- 10.Hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and FY 2012 rates. Federal register. 2011;76:51665–51666. [PubMed] [Google Scholar]
- 11.Healthcare Cost and Utilization Project (HCUP). NEDS Overview. 2016. Agency for Healthcare Research and Quality. Accessed on December 8, 2016 www.hcup-us.ahrq.gov/nedsoverview.jsp [PubMed]
- 12.Healthcare Cost and Utilization Project (HCUP). NIS Overview. 2016. Agency for Healthcare Research and Quality. Accessed on December 8, 2016 www.hcup-us.ahrq.gov/nisoverview.jsp [PubMed]
- 13.Centers for Disease Control and Prevention. National Vital Statistics System. 2016. Accessed on Feb 13, 2017 https://www.cdc.gov/nchs/nvss/about_nvss.htm
- 14.Stevens GA, King G and Shibuya K. Deaths from heart failure: using coarsened exact matching to correct cause-of-death statistics. Population health metrics. 2010;8:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Snyder ML, Love SA, Sorlie PD, Rosamond WD, Antini C, Metcalf PA, Hardy S, Suchindran CM, Shahar E and Heiss G. Redistribution of heart failure as the cause of death: the Atherosclerosis Risk in Communities Study. Population health metrics. 2014;12:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bui AL, Horwich TB and Fonarow GC. Epidemiology and risk profile of heart failure. Nature reviews Cardiology. 2011;8:30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ritchey MD, Loustalot F, Wall HK, Steiner CA, Gillespie C, George MG and Wright JS. Million Hearts - Description of the National Surveillance and Modeling Methodology Used to Monitor the Number of Cardiovascular Events Prevented During 2012–2016. J Am Heart Assoc. 2017:DOI 10.1161/JAHA.1117.006021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jackson SL, Tong X, Yin X, George MG and Ritchey MD. Emergency Department, Hospital Inpatient, and Mortality Burden of Atrial Fibrillation in the United States, 2006–2014. American Journal of Cardiology. 2017;In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Himmelstein D and Woolhandler S. Quality Improvement: ‘Become Good At Cheating And You Never Need To Become Good At Anything Else’. 2015. Accessed on September 5, 2017 http://healthaffairs.org/blog/2015/08/27/quality-improvement-become-good-at-cheating-and-you-never-need-to-become-good-at-anything-else/
- 20.Blecker S, Gavin NP, Park H, Ladapo JA and Katz SD. Observation Units as Substitutes for Hospitalization or Home Discharge. Annals of emergency medicine. 2016;67:706–713.e702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Center for Health Statistics. Intercensal estimates of the resident population of the United States for July 1, 2000-July 1, 2009, by year, county, single-year of age (0, 1, 2, .., 85 years and over), bridged race, Hispanic origin, and sex. Prepared under a collaborative arrangement with the U.S. Census Bureau. Available from: http://www.cdc.gov/nchs/nvss/bridged_race.htm.as of October 26, 2012, following release by the U.S. Census Bureau of the revised unbridged intercensal estimates by 5-year age group on October 9, 2012 Accessed on November 3, 2017.
- 22.National Center for Health Statistics. Vintage 2014 postcensal estimates of the resident population of the United States (April 1, 2010, July 1, 2010-July 1, 2014), by year, county, single-year of age (0, 1, 2, .., 85 years and over), bridged race, Hispanic origin, and sex. Prepared under a collaborative arrangement with the U.S. Census Bureau. Available from: http://www.cdc.gov/nchs/nvss/bridged_race.htm. as of June 30, 2015, following release by the U.S. Census Bureau of the unbridged Vintage 2014 postcensal estimates by 5-year age group on June 25, 2015 Accessed on November 3, 2017.
- 23.Chernew M, Baicker K and Martin C. Spillovers in Health Care Markets: Implications for Current Law Projections. 2010. Accessed on October 20, 2017 https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/downloads/spillovereffects.pdf
- 24.Chen J, Normand SL, Wang Y and Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. Jama. 2011;306:1669–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blecker S, Paul M, Taksler G, Ogedegbe G and Katz S. Heart failure-associated hospitalizations in the United States. Journal of the American College of Cardiology. 2013;61:1259–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dunlay SM and Roger VL. Understanding the epidemic of heart failure: past, present, and future. Current heart failure reports. 2014;11:404–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dunlay SM, Weston SA, Jacobsen SJ and Roger VL. Risk factors for heart failure: a population-based case-control study. The American journal of medicine. 2009;122:1023–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP and Jacobsen SJ. Trends in heart failure incidence and survival in a community-based population. Jama. 2004;292:344–350. [DOI] [PubMed] [Google Scholar]
- 29.Fonarow GC, Albert NM, Curtis AB, Stough WG, Gheorghiade M, Heywood JT, McBride ML, Inge PJ, Mehra MR, O’Connor CM, Reynolds D, Walsh MN and Yancy CW. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF). Circulation. 2010;122:585–596. [DOI] [PubMed] [Google Scholar]
- 30.Fonarow GC and Albert NM. Team-Based Care for Heart Failure. Heart Failure Clinics. 11:i. [DOI] [PubMed] [Google Scholar]
- 31.Ezekowitz JA, Kaul P, Bakal JA, Quan H and McAlister FA. Trends in heart failure care: has the incident diagnosis of heart failure shifted from the hospital to the emergency department and outpatient clinics? European journal of heart failure. 2011;13:142–147. [DOI] [PubMed] [Google Scholar]
- 32.Gupta A, Allen LA, Bhatt DL, Cox M, DeVore AD, Heidenreich PA, Hernandez AF, Peterson ED, Matsouaka RA, Yancy CW and Fonarow GC. Association of the Hospital Readmissions Reduction Program Implementation With Readmission and Mortality Outcomes in Heart Failure. JAMA Cardiol. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J and Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. New England Journal of Medicine. 2016;374:1543–1551. [DOI] [PubMed] [Google Scholar]
- 34.Roger VL. The heart failure epidemic. International journal of environmental research and public health. 2010;7:1807–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ritchey MD, Loustalot F, Bowman BA and Hong Y. Trends in mortality rates by subtypes of heart disease in the United States, 2000–2010. Jama. 2014;312:2037–2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.National Center for Health Statistics CfDCaP. Physicians’ Handbook on Medical Certification of Death. 2003. Accessed on November 3, 2017 https://www.cdc.gov/nchs/data/misc/hb_cod.pdf
- 37.Ni H and Xu J. Recent Trends in Heart Failure-related Mortality: United States, 2000–2014. NCHS Data Brief. 2015:1–8. [PubMed] [Google Scholar]
- 38.Weir HK, Anderson RN, Coleman King SM, Soman A, Thompson TD, Hong Y, Moller B and Leadbetter S. Heart Disease and Cancer Deaths - Trends and Projections in the United States, 1969–2020. Preventing Chronic Disease. 2016;13:E157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sidney S, Quesenberry CP, Jaffe MG, Sorel M, Nguyen-Huynh M, Kushi L, Go A and Rana J. Recent Trends in Cardiovascular Mortality in the United States and Public Health Goals. JAMA Cardiology. 2016;1:594–599. [DOI] [PubMed] [Google Scholar]
- 40.Avery CL, Loehr LR, Baggett C, Chang PP, Kucharska-Newton AM, Matsushita K, Rosamond WD and Heiss G. The population burden of heart failure attributable to modifiable risk factors: The Atherosclerosis Risk in Communities (ARIC) study. Journal of the American College of Cardiology. 2012;60: 10.1016/j.jacc.2012.1007.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.National Center for Health Statistics. National Ambulatory Medical Care Survey: 2014 State and National Summary Tables. Accessed on September 28, 2017 https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2014_namcs_web_tables.pdf
- 42.Cox ZL, Lai P, Lewis CM and Lenihan DJ. Centers for Medicare and Medicaid Services’ readmission reports inaccurately describe an institution’s decompensated heart failure admissions. Clinical cardiology. 2017;40:620–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dunlay SM, Shah ND, Shi Q, Morlan B, VanHouten H, Hall Long K and Roger VL. Lifetime Costs of Medical Care After Heart Failure Diagnosis. Circulation: Cardiovascular Quality and Outcomes. 2011;4:68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Srinivasan D and Desai NR. The Impact of the Transition From Volume to Value on Heart Failure Care: Implications of Novel Payment Models and Quality Improvement Initiatives. Journal of cardiac failure. 2017;23:615–620. [DOI] [PubMed] [Google Scholar]
- 45.Gustafsson F and Rogers JG. Left ventricular assist device therapy in advanced heart failure: patient selection and outcomes. European journal of heart failure. 2017;19:595–602. [DOI] [PubMed] [Google Scholar]
- 46.Bonacchi M, Harmelin G, Bugetti M and Sani G. Mechanical Ventricular Assistance as Destination Therapy for End-Stage Heart Failure: Has it Become a First Line Therapy? Frontiers in surgery. 2015;2:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJV, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WHW, Tsai EJ and Wilkoff BL. 2013 ACCF/AHA Guideline for the Management of Heart Failure. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013. [Google Scholar]
- 48.Golwala H, Pandey A, Ju C, Butler J, Yancy C, Bhatt DL, Hernandez AF and Fonarow GC. Temporal Trends and Factors Associated With Cardiac Rehabilitation Referral Among Patients Hospitalized With Heart Failure: Findings From Get With The Guidelines-Heart Failure Registry. Journal of the American College of Cardiology. 2015;66:917–926. [DOI] [PubMed] [Google Scholar]
- 49.Bradley EH, Curry L, Horwitz LI, Sipsma H, Wang Y, Walsh MN, Goldmann D, White N, Piña IL and Krumholz HM. Hospital Strategies Associated with 30-Day Readmission Rates for Patients with Heart Failure. Circulation Cardiovascular quality and outcomes. 2013;6:444–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cheng JW and Cooke-Ariel H Pharmacists’ role in the care of patients with heart failure: review and future evolution. Journal of managed care pharmacy : JMCP. 2014;20:206–213.` [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


