Abstract
This study aims to compare the effect of topical anesthesia against the use of no topical agent on pain of needle penetration and local anesthesia deposition during buccal infiltration in anterior maxilla. In a randomized controlled trial, 100 adult participants were randomly allocated to the benzocaine group (received 20% benzocaine gel) and no benzocaine group (received no topical agent) prior to buccal infiltration in maxillary anterior teeth. A 27-gauge needle was used to deposit 2% lidocaine with 1:100,000 epinephrine. Pain of needle penetration and local anesthesia deposition was recorded separately using an 11-point Numeric Pain Rating Scale. Results showed that although 20% benzocaine significantly reduced pain on needle penetration during buccal infiltration in maxillary anterior teeth, the difference was small and the clinical significance is not clear. Topical anesthetic did not affect pain of local anesthetic deposition.
Key Words: Topical, Anesthesia, Local, Pain, Benzocaine, Infiltration, Randomized controlled trial
Administration of local anesthesia (LA) for dental procedures is a frequent cause of discomfort, apprehension1,2 and anxiety1 in patients. Various modalities are practiced to reduce this discomfort, which include warming the cartridge, providing vibration, pressure, or cold at the site of injection, distraction techniques, and lastly application of topical anesthesia, which is commonly practiced in modern dentistry.3
Topical anesthetics target free nerve endings in the mucosa and block nerve impulse conduction thereby producing temporary loss of sensation at the site of administration.4 The pharmacological and psychological effects of topical anesthesia application prior to administration of LA have variable outcomes. While some studies report reduction in pain of needle penetration,5–7 others conclude that the difference in pain using a topical anesthetic and placebo is insignificant.8–10 Conflicting results may be explained by variations in the site11 duration of application of topical anesthesia, low sensitivity of pain scales, and psychological factors.12
The clinical implication of topical anesthesia being no more effective in pain reduction than placebo is not to use topical prior to LA administration. This clinical approach has not been thoroughly studied in randomized controlled trials and this study aims to compare the effects of the use of topical anesthesia against the use of no topical agent prior to buccal infiltration of LA in maxillary anterior teeth.
MATERIALS AND METHODS
This experimental nonblinded parallel group randomized clinical trial was conducted on patients presenting for extraction of maxillary anterior teeth to the Oral and Maxillofacial Surgery Department at the Institute of Dentistry, CMH Lahore Medical College.
All patients included in the research were above the age of 17 years and had an ASA physical status of 1 or 2. Patients with known allergy to agents used in the study, those who used medications that altered pain perception in the previous 2 weeks (eg, opioids, antidepressants, antianxiety medications) or used analgesics on the day of data collection, and those showing signs of inflammation of the oral mucosa were excluded from the study.
The study protocol was approved by the Institutional Review Board of the Institute of Dentistry, CMH Lahore Medical College. Each participant signed a consent form after the nature of procedure and possible risks and discomforts were fully explained. The sample consisted of 50 subjects in each group (Figure 1) to provide a power of 0.9, significance level of 0.05 with a standard deviation of 1, and a difference in means of 0.7. This value of difference in means is lesser than the clinically relevant difference reported on the visual analogue scale in previous studies13 but was used in this study to compensate for the reduced sensitivity of the numeric rating scale.14 A larger sample size also allowed us to study gender differences in pain perception.
Figure 1.
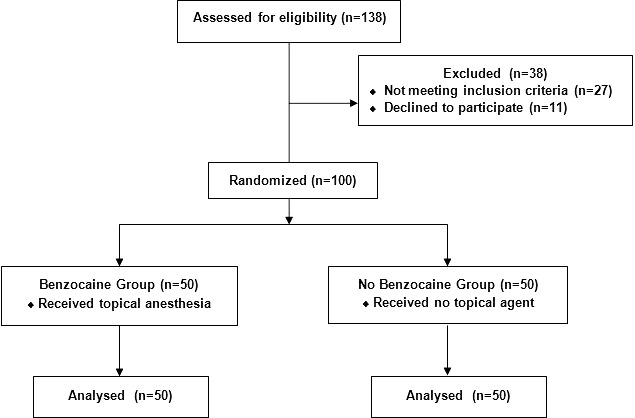
Flowchart illustrating participant enrolment, groups, and interventions.
Integers from 1 to 100 were randomly sorted into the benzocaine group (to receive topical anesthesia) and no benzocaine group (to receive no topical agent) using the sequence generator at www.random.org. These integers represented study numbers that were later allocated to the study participants in a sequential manner as they presented to the department. All LA injections and topical agent applications were performed by the first author.
Before submitting to the experimental procedures, patients were questioned about their history of intraoral LA injections and related past experiences, phobia of needles, and fear of dental settings or dentists. For both groups, 0.6 mL of 2% lidocaine with epinephrine 1:100,000 via a 1.8-mL cartridge (Medicaine, Huons Co Ltd, Korea) and a 27-gauge needle was used for every participant. The standard procedure of administering infiltration was as follows15:
The area of needle insertion was first dried using sterile gauze. In the benzocaine group, 1 mL of topical anesthetic gel containing 20% of benzocaine was dispensed into a dosing spoon. Sterilized cotton square pieces measuring (1 × 1 cm) were used to make cotton balls with which the gel was applied to the dry labial alveolar mucosa associated with the tooth to be anesthetized. The topical gel was rubbed in the area for 30 seconds and left in place for another 30 seconds, the total application time being 1 minute. Before infiltration was given, 1.2 mL of the LA solution was discarded from the syringe to ensure that every participant received an equal 0.6 mL of the solution. The injection needle was inserted into the height of the mucobuccal fold 3 to 5 mm deep into the labial mucosa. Care was taken to prevent the needle from coming in contact with the bone and the LA solution was deposited over a period of 20 seconds.
To evaluate pain, the numeric pain rating scale was employed with markings from 0 to 10 (Figure 2). Prior to commencement of the procedure, the participant was made familiar with the numeric pain rating scale and was informed that during the procedure the operator would signal at the participant twice, first when the injection needle was inserted and second when the LA solution was deposited. The numeric pain scale was held by an assistant and constantly kept in patient's view during the procedure. The patient was instructed to point at a number on the pain scale after the first signal of needle penetration and the second signal at the end of LA deposition before the needle was withdrawn. In the no benzocaine group, the area was dried with sterile gauze followed by the same steps of infiltration and pain evaluation. After the reporting of pain was concluded, the planned dental procedure was performed.
Figure 2.
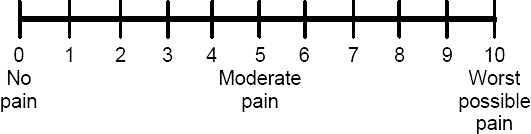
Eleven-Point Numeric Pain Rating Scale.
Statistical analysis of the data was done using SPSS version 23 (IBM Corp; 2015). Descriptive analysis was done by calculating frequencies, means, medians, and standard deviation. Data did not fulfil parametric assumptions (Shapiro Wilk test, p < 0.001) and groups were compared using Mann-Whitney U test with a significance level established at 5%.
RESULTS
There were a total of 100 participants in the study, 50 in each group. There were 49 males and 51 females. The mean age of participants was 54.55 ± 12.3 years. The benzocaine group had 25 females and 25 males, whereas the no benzocaine group included 26 females and 24 males (Table 1). There was no significant difference in gender distribution (p = 0.85) and mean age (p = 0.23) between the 2 groups. Moreover, analysis rendered no significant difference among the distribution of teeth (eg, central incisor vs cuspid) between the 2 groups.
Table 1.
Demographics of Study Participants and Frequency of Dental Phobias and Previous LA Administration
|
Groups |
n |
Gender |
Smokers |
History of LA Administration |
Fear of Dentists/Dental Setting |
Phobia of Needles |
|||||
| Male |
Female |
Yes |
No |
Yes |
No |
Yes |
No |
Yes |
No |
||
| Benzocaine | 50 | 50% | 50% | 18% | 82% | 52% | 48% | 18% | 82% | 4% | 96% |
| No Benzocaine | 50 | 48% | 52% | 18% | 82% | 50% | 50% | 20% | 80% | 2% | 98% |
| Total Number | 100 | 49 | 51 | 18 | 82 | 51 | 49 | 19 | 81 | 4% | 96 |
On needle penetration, median pain was significantly lower in the benzocaine group, as compared to the no benzocaine group (2 vs 3 respectively, p < 0.001; Table 2). On LA deposition, there was no significant difference in pain scores between the benzocaine group and no benzocaine groups (p = 0.64; Table 2).
Table 2.
Median Scores of Pain Evaluated Using Numeric Pain Rating Scale
|
Participants |
n |
Pain Scores |
|||
|
Needle Penetration |
Local Anesthesia Deposition |
||||
|
Median |
P* |
Median |
P* |
||
| Group | |||||
| Benzocaine | 50 | 2 | 0.001 | 2 | 0.64 |
| No Benzocaine | 50 | 3 | 2 | ||
| Gender | |||||
| Male | 49 | 2 | <0.001 | 1 | <0.001 |
| Female | 51 | 3.50 | 2 | ||
| Fear of dental setting | |||||
| Yes | 19 | 5 | <0.001 | 4 | <0.001 |
| No | 81 | 3 | 2 | ||
| Phobia of needles | |||||
| Yes | 4 | 4 | 0.14 | 4 | 0.2 |
| No | 96 | 3 | 2 | ||
| Smoker | |||||
| Yes | 18 | 2.5 | 0.47 | 1 | 0.27 |
| No | 82 | 3 | 2 | ||
Mann-Whitney U test.
Females compared to males displayed significantly higher pain scores on both needle penetration of 3.5 vs 2 and LA deposition of 2 vs 1 (both p < 0.001; Table 2).
Patients with a fear of dentists or dental settings showed higher pain scores for both needle penetration of 5 vs 3 and LA deposition of 4 vs 2 (both p < 0.001; Table 2). No significant difference was reported in pain scores between smokers and nonsmokers and patients with and without phobia of needles (Table 2).
DISCUSSION
The results of this study demonstrate that the application of 20% benzocaine gel significantly reduced pain of needle penetration but had no effect on the pain of local anesthetic deposition. In addition to the pharmacological effect, this reduction in pain of needle penetration may also have been associated with psychological factors16 as placebo effect alters expected pain, reduces anxiety, and consequently reduces pain perception of LA injection.17 Some studies demonstrate similar results to this study, favoring the use of topical anesthetics,6,7 while others found no significant reduction in pain with use of topical agents.8,9 Since most of these studies have compared the use of topical anesthetics to placebo, an appropriate comparison to this study cannot be drawn. One nonrandomized experimental study that compared the use of 20% benzocaine to the use of no topical agent rendered similar results to our study.5
In this study, females reported significantly higher pain scores than males for both needle penetration and LA deposition. These results contradict previous studies testing the efficacy of topical anesthesia, which report higher pain scores by males on the visual analogue scale.8,16 Differences in pain perception may be a result of biological (genetics, gonadal hormones, endogenous pain inhibition), psychological (anxiety, depression, cognitive and behavioral factors), and socio-cultural factors (age, ethnicity, family history, gender roles).18 However, recent epidemiological studies found women to be more sensitive to pain19 and less capable of enduring pain than men,20 supporting the findings of this study. Greater pain sensitivity in women has been associated with 3 psychosocial factors: hypervigilance (women focus more on threatening situations than men do), greater bodily monitoring, and greater prevalence of anxiety and depression.21 One study found men less willing to report pain as compared to women20 possibly due to the influence of gender-related expectations of pain response.
Patients in this study with a fear of dentists and/or dental settings showed pain scores that were significantly higher on both needle penetration and LA deposition. This is in accordance with expectations and with studies that find a significant correlation between dental fear or anxiety and pain perception.22,23 Higher pain scores were also observed for patients with a phobia of needles in this study, but these were statistically insignificant likely due to a low percentage (4%) of patients presenting with this phobia.
We chose 20% benzocaine gel for our study as it has been reported to be the most popular topical anesthetic in United States.24 Most previous studies have also used 20% benzocaine as the topical anesthetic.5,8,25 In previous studies, intraoral application time of topical anesthesia usually ranges from 30 seconds to 10 minutes,5,8,26,27 although a 20-minute application period on the alveolar mucosa of maxillary incisors has also been employed in 1 study.28 While some believe this variation in application time to be associated with conflicting results of these studies,12 others report this factor to have no significant effect on pain perception.26 Some report reduction in pain on needle penetration after 1-minute application time,5,25 others demonstrate no significant pain reduction even after a period of 20 minutes.28 In this study, like most other studies that used benzocaine,5,9,25,29 the topical agent was applied for 1 minute, which is in accordance with recommendations of the ADA and FDA and has reported to be sufficient time for the agent to become effective30 and efficacious in the maxillary mucobuccal fold.25
The labial mucosa of maxillary anterior teeth was selected as the site of injection for ease of access and isolation in order to measure the time of topical agent application accurately and for comparison with previous studies. Needles used for administration of LA were of 27 gauge. No difference in pain perception has been observed between the use of 25-gauge or 27-gauge needles.31
Most previous such studies obtained pain scores from the participants for needle penetration after the injection was given and the needle was removed from the patient's oral cavity.8,9,29 However, in this study the pain score was obtained from the participants immediately after needle penetration, prior to advancement of the needle or LA deposition. This was done to decrease the bias that the overall experience of injection or pain of needle advancement may have caused on pain perception of needle penetration. The operator did observe, however, that if what appeared to be high discomfort was caused by needle advancement, this may have had an impact on the pain scores reported for LA deposition with some patients reporting unusually higher pain scores for LA deposition. This was not studied and therefore cannot be verified.
A numeric pain rating scale was employed in this study to evaluate pain as it is reported to have good sensitivity3 and the local patient population found it most easily comprehensible. Although, a statistically significant difference of 1 in medians and 0.9 in means was observed between the 2 groups for pain on needle penetration, and in the operator's subjective perspective pain was reduced with the use of benzocaine in this study, these findings may not be clinically significant as other studies have suggested a difference in means of up to 25% or greater to be clinically relevant.8,13 Regardless of the clinical relevance of the use of topical anesthesia, increased pain scores reported by females and patients with fear of dental settings showed a higher difference in means approaching the 25% threshold and therefore would appear to warrant the use of topical anesthesia in such patients.
In this study, participants were not asked to rate the overall experience of the injection and blinding was not carried out to simulate the conditions in clinical practice. Further studies on topical anesthesia need not evaluate pain of LA deposition since it is not influenced by the use of topical anesthesia as demonstrated by the results of this and other studies.
Topical anesthesia not only has pharmacological but also psychological effects on pain of needle penetration.14,32 Although its routine use seems to be prevalent in developed countries, the same cannot be said for low resource developing countries (eg, Kenya33 and Pakistan). An Internet survey by the authors revealed that 39% of responding dentists in Pakistan use topical anesthesia routinely and none of them use it routinely in institution-based practice.
In conclusion, the findings of this study indicate that female gender and fear of dentists/dental settings increase pain perception of local anesthetic injections during buccal infiltration in maxillary anterior teeth. Although 20% benzocaine significantly reduced pain on needle penetration during buccal infiltration in maxillary anterior teeth, the difference was small and the clinical significance is not clear. Topical anesthetic did not affect pain of local anesthetic deposition.
ACKNOWLEDGMENTS
The authors would like to acknowledge the contributions of the staff of Oral and Maxillofacial Surgery Department at Institute of Dentistry, CMH Lahore Medical College.
No conflicts of interest by the authors. This trial has been registered at Clinicaltrial.gov (number NCT03261115).
REFERENCES
- 1.Milgrom P, Coldwell SE, Getz T, Weinstein P, Ramsay DS. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997;128:756–766. doi: 10.14219/jada.archive.1997.0301. [DOI] [PubMed] [Google Scholar]
- 2.Kleinknecht RA, Klepac RK, Alexander LD. Origins and characteristics of fear of dentistry. J Am Dent Assoc. 1973;86:842–848. doi: 10.14219/jada.archive.1973.0165. [DOI] [PubMed] [Google Scholar]
- 3.Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nursing. 2005;14:798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]
- 4.Kumar M, Chawla R, Goyal M. Topical anesthesia. J Anaesthesiol Clin Pharmacol. 2015;31:450–456. doi: 10.4103/0970-9185.169049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nusstein JM, Beck M. Effectiveness of 20% benzocaine as a topical anesthetic for intraoral injections. Anesth Prog. 2003;50:159–163. [PMC free article] [PubMed] [Google Scholar]
- 6.Rosa AL, Sverzut CE, Xavier SP, Lavrador MA. Clinical effectiveness of lidocaine and benzocaine for topical anesthesia. Anesth Prog. 1999;46:97–99. [PMC free article] [PubMed] [Google Scholar]
- 7.Rosivack RG, Koenigsberg SR, Maxwell KC. An analysis of the effectiveness of two topical anesthetics. Anesth Prog. 1990;37:290–292. [PMC free article] [PubMed] [Google Scholar]
- 8.De Freiras GC, Pozzobon RT, Blaya DS, Moreira CH. Efficacy of benzocaine 20% topical anesthetic compared to placebo prior to administration of local anesthesia in the oral cavity: a randomized controlled trial. Anesthesia Prog. 2015;62:46–50. doi: 10.2344/0003-3006-62.2.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parirokh M, Sadeghi AS, Nakhaee N, Pardakhty A, Abbott PV, Yosefi MH. Effect of topical anesthesia on pain during infiltration injection and success of anesthesia for maxillary central incisors. J Endod. 2012;38:1553–1556. doi: 10.1016/j.joen.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 10.Gill CJ, Orr DL., 2nd A double-blind crossover comparison of topical anesthetics. J Am Dent Assoc. 1979;98:213–214. doi: 10.14219/jada.archive.1979.0476. [DOI] [PubMed] [Google Scholar]
- 11.Nakanishi O, Haas D, Ishikawa T, Kameyama S, Nishi M. Efficacy of mandibular topical anesthesia varies with the site of administration. Anesth Prog. 1996;43:14–19. [PMC free article] [PubMed] [Google Scholar]
- 12.Meechan JG. Effective topical anesthetic agents and techniques. Dent Clin North Am. 2002;46:759–766. doi: 10.1016/s0011-8532(02)00035-6. [DOI] [PubMed] [Google Scholar]
- 13.Bhalla J, Meechan JG, Lawrence HP, Grad HA, Haas DA. Effect of time on clinical efficacy of topical anesthesia. Anesth Prog. 2009;56:36–41. doi: 10.2344/0003-3006-56.2.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bolton JE, Wilkinson RC. Responsiveness of Pain Scales: a comparison of three pain intensity measures in chiropractic patients. J Manip Physiol Ther. 1998;21:1–7. [PubMed] [Google Scholar]
- 15.Malamed SF. Handbook of Local Anaesthesia 5th ed. St. Louis, MO: Mosby;; 2004. [Google Scholar]
- 16.Martin MD, Ramsay DS, Whitney C, Fiset L, Weinstein P. Topical anesthesia: differentiating the pharmacological and psychological contributions to efficacy. Anesth Prog. 1994;41:40–47. [PMC free article] [PubMed] [Google Scholar]
- 17.Koshi EB, Short CA. Placebo theory and its implications for research and clinical practice: a review of the recent literature. Pain Pract. 2007;7:4–20. doi: 10.1111/j.1533-2500.2007.00104.x. [DOI] [PubMed] [Google Scholar]
- 18.Wiesenfeld HZ. Sex differences in pain perception. Gend Med. 2005;2:137–145. doi: 10.1016/s1550-8579(05)80042-7. [DOI] [PubMed] [Google Scholar]
- 19.Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009;10:447–485. doi: 10.1016/j.jpain.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robinson ME, Riley JL, 3rd, Myers CD, et al. Gender role expectations of pain: relationship to sex differences in pain. J Pain. 2001;2:251–257. doi: 10.1054/jpai.2001.24551. [DOI] [PubMed] [Google Scholar]
- 21.Rollman GB, Abdel-Shaheed J, Gillespie JM, Jones KS. Does past pain influence current pain: Biological and psychosocial models of sex differences. Eur J Pain. 2004;8:427–433. doi: 10.1016/j.ejpain.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 22.Kunzelmann KH, Dünninger P. Dental fear and pain: effect on patient's perception of the dentist. Community Dent Oral Epidemiol. 1990;18:264–266. doi: 10.1111/j.1600-0528.1990.tb00073.x. [DOI] [PubMed] [Google Scholar]
- 23.Ivana P, Martina KR, Marina P, Silvana JK. The level of anxiety and pain perception of endodontic patients. Acta Stomatol Croat. 2014;48:258–267. doi: 10.15644/asc47/4/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kohli K, Ngan P, Crout R, Linscott CC. A survey of local and topical anesthesia use by pediatric dentists in the United States. Pediatr Dent. 2001;23:265–269. [PubMed] [Google Scholar]
- 25.Hutchins HS, Young FA, Lackland DT, Fishburne CP. The effectiveness of topical anesthesia and vibration in alleviating the pain of oral injections. Anesth Prog. 1997;44:87–89. [PMC free article] [PubMed] [Google Scholar]
- 26.Dhawan P, Dhawan G. Topical anaesthetic: how effective are they. Int J Dent Clin. 2011;3:11–13. [Google Scholar]
- 27.Saurabh S, Basavapatanna SJ, Khushboo G. Diminution of pain from needle insertion in palatal mucosa by two topical anaesthetics: a comparative study between lidocaine/prilocaine (EMLA) and benzocaine. JAMDSR. 2015;3:9–15. [Google Scholar]
- 28.Fukayama H, Suzuki N, Umino M. Comparison of topical anesthesia of 20% benzocaine and 60% lidocaine gel. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:157–161. doi: 10.1067/moe.2002.124858. [DOI] [PubMed] [Google Scholar]
- 29.Milani AS, Zand V, Abdollahi AA, Froughreyhani M, Zakeri-Milani P, Jafarabadi MA. Effect of topical anesthesia with lidocaine-prilocaine (EMLA) cream and local pressure on pain during infiltration injection for maxillary canines: a randomized double-blind clinical trial. J Contemp Dent Pract. 2016;17:592–596. [PubMed] [Google Scholar]
- 30.Nayak R, Sudha P. Evaluation of three topical anaesthetic agents against pain: a clinical study. Indian J Dent Res. 2006;17:155–160. doi: 10.4103/0970-9290.29871. [DOI] [PubMed] [Google Scholar]
- 31.Carr MP, Horton JE. Evaluation of a transoral delivery system for topical anesthesia. J Am Dent Assoc. 2001;132:1714–1719. doi: 10.14219/jada.archive.2001.0127. [DOI] [PubMed] [Google Scholar]
- 32.Kincheloe JE, Mealiea WL, Jr, Mattison GD, Seib K. Psychophysical measurement on pain perception after administration of a topical anesthetic. Quintessence Int. 1991;22:311–315. [PubMed] [Google Scholar]
- 33.Ngugi JG. Usage and perception of intra-oral topical anaesthesia among dentists in Nairobi. Available at http://periodontology.uonbi.ac.ke/node/946 Accessed May 14, 2018.


