Abstract
Immune checkpoint inhibitors (ICIs) are now commonly used to treat patients with metastatic malignant melanoma. Although concerns have been raised that the inflammatory response induced by ICIs may limit the ability of 18F-FDG PET/CT to assess tumor response, systematic analyses on the use of 18F-FDG PET/CT in this setting are mostly lacking. Thus, we set out to evaluate the association between tumor response on 18F-FDG PET/CT and prognosis in patients with metastatic malignant melanoma treated with ipilimumab. Methods: We analyzed 60 consecutive patients with metastatic melanoma who underwent 18F-FDG PET/CT scans both before and after treatment to evaluate treatment response after completion of ipilimumab therapy. Tumor response was assessed by the change in the sum of SULpeak (voxels with the highest average SUL [SUV normalized to lean body mass]) of up to 5 lesions according to PERCIST5. New lesions on PET that appeared suggestive of metastases were considered progressive metabolic disease (PMD). Because immunotherapy may cause new inflammatory lesions that are detectable on 18F-FDG PET/CT, we also evaluated an immunotherapy-modified response classification (imPERCIST5). In this classification, new lesions do not define PMD per se; rather, PMD requires an increase in the sum of SULpeak by 30%. The correlation between tumor response according to these 3 definitions and overall survival (OS) was evaluated and compared with known prognostic factors. Results: In responders and nonresponders, the 2-y OS was 66% versus 29% for imPERCIST5 (P = 0.003). After multivariate analysis, imPERCIST5 remained prognostic (hazard ratio, 3.853; 95% confidence interval, 1.498–9.911; P = 0.005). New sites of focal 18F-FDG uptake occurred more often in patients with PMD (n = 24) by imPERCIST5 than in those with stable metabolic disease (n = 7) or partial metabolic response (n = 4). In patients with partial metabolic response, 2 of 4 isolated new lesions regressed spontaneously during follow-up. Conclusion: In patients with metastatic melanoma treated with ipilimumab, tumor response according to PERCIST was associated with OS. Our data suggest that PMD should not be defined by the appearance of new lesions, but rather by an increase in the sum of SULpeak.
Keywords: immune checkpoint inhibitor, ipilimumab, melanoma, PERCIST, 18F-FDG
Ipilimumab is a fully human IgG1 monoclonal antibody that blocks cytotoxic T lymphocyte antigen (CTLA-4), a negative regulator of the immune response (1–3). Clinical studies have shown that ipilimumab significantly improves survival of patients with metastatic melanoma when compared with chemotherapy; in fact, patients responding to ipilimumab may survive for 5+ years (4,5). However, only about 15%–20% of patients with metastatic melanoma have an objective radiographic response to ipilimumab, although such responses and stable disease can be durable (6,7). Assessing tumor response to ipilimumab and other checkpoint inhibitors by size criteria has been found to be challenging because tumor infiltration by immune cells may cause delayed tumor shrinkage or even a temporary increase in tumor size (pseudoprogression) (8,9). To overcome these difficulties, new response criteria have been developed for assessing the efficacy of immune checkpoint inhibitors (ICIs) (10–12). These new criteria require confirmation of tumor progression on a follow-up scan, and in contrast to the commonly used RECIST, they do not necessarily consider the appearance of new lesions as progression of disease (13).
The use of 18F-FDG PET/CT to monitor treatment with ICIs has also been questioned because tumor infiltration by immune cells may cause a transient increase in metabolic activity (14). A few studies and case reports have suggested that the presence and appearance of 18F-FDG–avid lesions in patients treated with checkpoint inhibitors may be due to immune cell infiltrates (15,16). However, the frequency of pseudoprogression as seen on 18F-FDG PET/CT is not well documented, and it remains unclear whether pseudoprogression has a significant impact on tumor response assessment by PERCIST (16–18).
The purpose of this retrospective study was to investigate the relationship between changes in 18F-FDG tumor uptake—using standard PERCIST and immunotherapy-modified PERCIST (imPERCIST)—and survival in patients with advanced melanoma undergoing treatment with ipilimumab.
MATERIALS AND METHODS
Patients
The institutional review board approved this retrospective single-center study and waived the informed consent requirement. The study was compliant with the Health Insurance Portability and Accountability Act.
Our hospital information system was screened for patients with metastatic melanoma who had received ipilimumab monotherapy from 2010 to 2015 and had undergone 18F-FDG PET/CT both before and after treatment. All patients underwent brain MRI or CT as well as 18F-FDG PET/CT before initiation of therapy. Patients with metastatic disease limited to the brain or without hypermetabolic lesions outside the brain were excluded from analysis. Other exclusion criteria were as follows: advanced primary cancer other than melanoma, treatment with other checkpoint inhibitors before or during ipilimumab therapy, no lesion on 18F-FDG PET/CT exceeding the limits for minimum SUV normalized to lean body mass (SUL) as defined by PERCIST (1.5 × liver SUL + 2 SDs of liver SUL), and 18F-FDG uptake time differing by more than 30 min between baseline and follow-up scans.
18F-FDG PET/CT Protocol
Before injection of 18F-FDG, patients fasted for at least 6 h. If plasma glucose levels were less than 200 mg/dL, patients were injected intravenously with 444–555 MBq of radiotracer. After injection, patients rested for 60–90 min before image acquisition. At baseline and follow-up, 25 and 21 cases, respectively, were scanned outside of the PERCIST-recommended time window of 50–70 min after injection. In 16 paired scans, the difference in uptake time at baseline versus follow-up was more than 15 min (in 8 cases, the baseline scan was done >15 min earlier, and in another 8 cases, it was done >15 min later than the respective follow-up scan). 18F-FDG PET/CT scans were obtained with GE Healthcare PET/CT systems (GE Discovery Series: VCT, ST, STE, 600, and 690). Of the 60 paired examinations, 35 (58%) were performed with the same scanner type. The medical physics group at our institution has harmonized the acquisition and reconstruction parameters to minimize SUV differences between scanners and keep them within 10% as tested by regular phantom studies. Cross-calibration between the dose calibrator and PET scanners is performed monthly. Eleven cases showed the difference of more than 0.3 SUL unit of liver uptake between baseline and follow-up scans.
Scans were generally acquired with an axial field of view from the vertex to the toes (n = 47). In 13 patients, only images from the base of the skull to the midthighs were obtained because no lesions in the extremities were expected clinically. Low-dose CT images during PET/CT were used for attenuation correction of the PET emission scan and for anatomic orientation. PET/CT images were reconstructed using an ordered-subset expectation maximization algorithm and a gaussian filter using the standard manufacture-supplied reconstruction software.
Image Analysis
One experienced physician board-certified in both diagnostic radiology and nuclear medicine reviewed all 18F-FDG PET/CT images. An 18F-FDG–avid lesion was defined as focal, abnormally increased 18F-FDG uptake versus background, with or without a corresponding anatomic lesion on the CT scan and suggestive of metastasis. At the time of image analysis, the reviewer was unaware of the results of any other imaging tests and the clinical outcome of the patient. Images were analyzed using PET VCAR software by visually examining all the images on a computer display and the workstation (Advantage Workstation; GE Healthcare).
To determine SUL, the reviewer placed a sphere or cube as the volume of interest (VOI) around the target lesion. Within this VOI, the software searched for the 1.0 cm3 sphere that encompassed the voxels with the highest average SUL. This SUL was reported as SULpeak. Response of SULpeak (%) was defined as (sum of baseline SULpeak − sum of follow-up SULpeak)/(sum of baseline SULpeak) × 100.
Response to ipilimumab therapy was classified as complete metabolic response (CMR), partial metabolic response (PMR), stable metabolic disease (SMD), or progressive metabolic disease (PMD). Three different approaches were used to assess response: in the first approach (PERCIST5), we followed the recommendations of PERCIST (18). Briefly, CMR was defined as the resolution of all malignant lesions and was nominally assigned an SULpeak of zero for quantitative analysis. 18F-FDG uptake of a lesion was considered resolved if it was less than mean liver activity and indistinguishable from the surrounding background. In patients with metabolically active lesions on the follow-up scan, the SULpeak of up to 5 lesions on the baseline and follow-up scan was summed (maximum of 2 per organ). Since the hottest lesions were selected in each scan, target lesions on follow-up scans were not necessarily the same as target lesions at baseline. If the sum of SULpeak decreased by at least 30%, tumor response was classified as PMR. Conversely, PMD was defined as an increase of the sum of SULpeak by at least 30% or the appearance of new hypermetabolic lesions on follow-up 18F-FDG PET/CT scan. Cases not meeting the definitions for CMR, PMR, or PMD were classified as SMD.
For the second analysis (PERCIST1), the lesions with the highest SULpeak between the baseline and follow-up scans were selected (not necessarily the same lesion except a new lesion on the follow-up scan). An increase of SULpeak by 30% or more was considered PMD, and a decrease by 30% or more PMR. As for PERCIST5, the appearance of new lesions alone resulted in a PMD classification.
The third analysis (imPERCIST5, or immunotherapy-modified PERCIST, 5-lesion analysis) was performed in the same way as described for PERCIST5, but the appearance of new lesions alone did not result in PMD. Thus, PMD was defined only by an increase of the sum of SULpeaks by 30%. New lesions were included in the sum of SULpeak if they showed higher uptake than existing target lesions or if fewer than 5 target lesions were detected on the baseline scan. A case illustrating the 3 different response classifications is shown in Figure 1. A comparison of PERCIST and imPERCIST is shown in Supplemental Table 3 (supplemental materials are available at http://jnm.snmjournals.org).
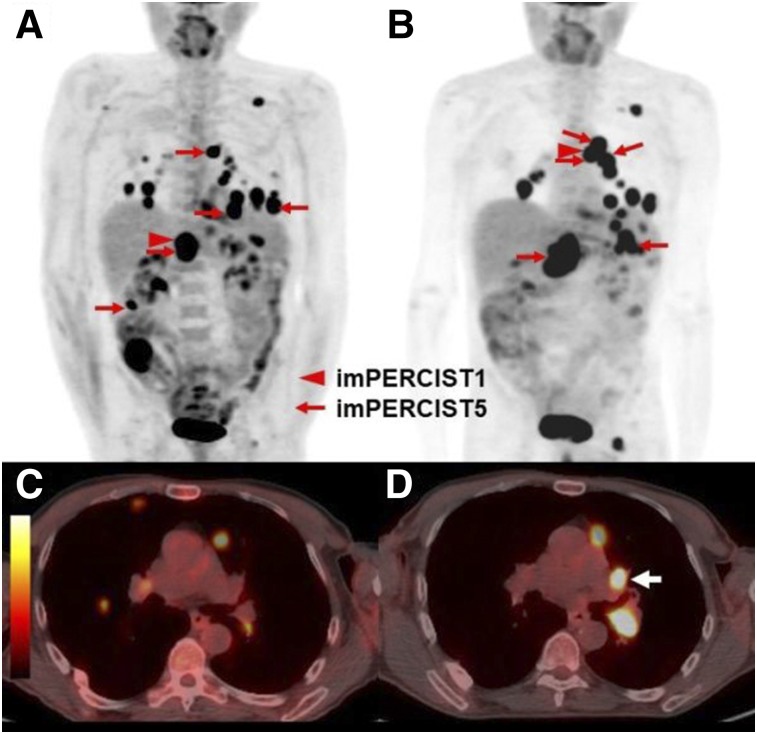
FIGURE 1.
Representative case for the differences between response classifications. A 66-y-old man classified as progressive disease by PERCIST5 and PERCIST1 (due to the appearance of a new lesion), but SMD by imPERCIST5. Maximum-intensity-projection (MIP) images at baseline (A) and follow-up (B). Target lesions for PERCIST5 and imPERCIST5 are indicated by red arrows (sum of SULpeak 47.61 at baseline). The target lesion for PERCIST1 at baseline is an abdominal lymph node (SULpeak, 15.07, red arrowhead). On the follow-up scan (B), the target lesion for PERCIST1 is a thoracic lymph node (SULpeak, 10.05) because the SULpeak of the abdominal lymph node had decreased to 8.86. Comparison of axial images of the chest at baseline (C) and follow-up (D) show the development of a new hypermetabolic left hilar lymph node (white arrow). This lesion (SULpeak, 9.29) was included in the target lesions for imPERCIST5.
Statistical Analysis
Statistical analysis was performed using SPSS software (version 24; IBM) and R 3.4.3 for Windows (R Foundation for Statistical Computing). Data were presented as mean ± SD, and a P value of 0.05 or less was considered significant. Concordance between response assessments of 2 analyses was evaluated using κ-statistics. Overall survival (OS) was defined as time from start of ipilimumab therapy until death from any cause or last follow-up visit. Patients who remained alive were censored at last follow-up. For OS analysis, the data were dichotomized into responders (CMR and PMR) and nonresponders (SMD and PMD). The log-rank (Mantel–Cox) test was used to evaluate the difference between Kaplan–Meier curves. We realize the potential bias in the comparison of OS by treatment response (19). However, treatment response is usually observed in 2–4 mo, which is a rather short time compared with the follow up length in this study. Therefore, we expect the potential bias to be minimal. To calculate the risk ratios and 95% confidence intervals (CIs), univariate analysis was used to identify factors associated with OS. Then, factors found to be significant by univariate analysis (P < 0.05) were entered into a Cox multivariate regression analysis model. For the univariate analysis, we used dummy variables of 1 for the following factors: age ≥ 75 y, male, 1 or more lines of previous systemic chemotherapies, no cutaneous primary, prior radiotherapy, prior surgery, presence of distant metastasis, presence of active brain metastasis, presence of BRAF V600 mutation, receiving 2 or 3 cycles of ipilimumab, elevated lactate dehydrogenase level above upper limit of the normal, and response on 18F-FDG PET/CT. Then, forward stepwise multivariate regression analysis was performed to identify factors correlated with OS based on calculating hazard ratios (HRs) and 95% CIs. The strength of the concordance between significant prognostic factors in the multivariate model and patient survival was described by Gönen–Heller concordance coefficients (R package clinfun, VE Seshan, MSKCC) (20).
RESULTS
Patient Characteristics and PET Scanning
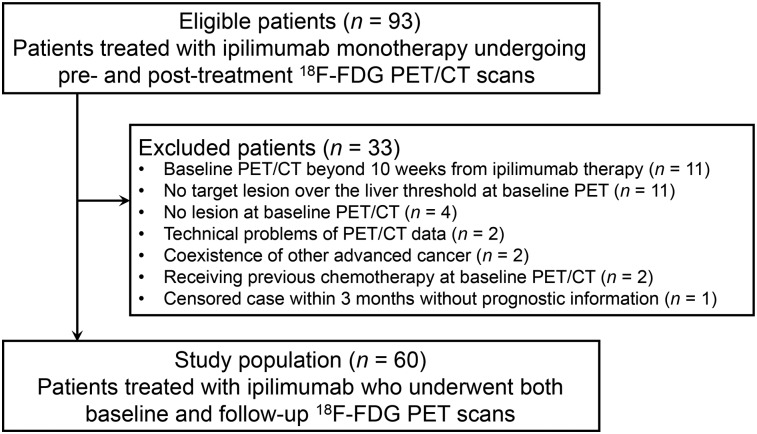
A flow diagram summarizing the selection of patients is shown in Figure 2. Overall, 60 evaluable patients were identified. The last follow-up date for OS calculation was December 31, 2017. Baseline 18F-FDG PET/CT scans were obtained at a median of 2.36 wk (range, 0–10 wk) before initiation of ipilimumab therapy. Follow-up scans were performed 2.9 wk (median; range, 1.0–11.1) after the last dose of ipilimumab. The interval from initiation of ipilimumab to follow-up PET scan was 12.2 wk (median; range, 7.8–20.3). Twenty-five baseline scans and 21 follow-up scans were acquired outside the PERCIST-recommended window for uptake time (50–70 min after injection). Moreover, for 16 paired scans, the difference in uptake time (baseline-follow-up) was greater than 15 min. Eleven patients showed a difference of more than 0.3 SUL in liver uptake between baseline and follow-up, including 5 with liver involvement. Patient characteristics are summarized in Supplemental Table 1. Ipilimumab was dosed at 3 mg/kg in all patients. Fifty patients received the full course of 4 cycles of ipilimumab. Ten patients received only 2 (n = 5) or 3 (n = 5) cycles of therapy due to immune-related colitis (n = 9) or immune-related aseptic meningitis (n = 1), respectively.
FIGURE 2.
Flow diagram of study patients.
18F-FDG PET/CT Results
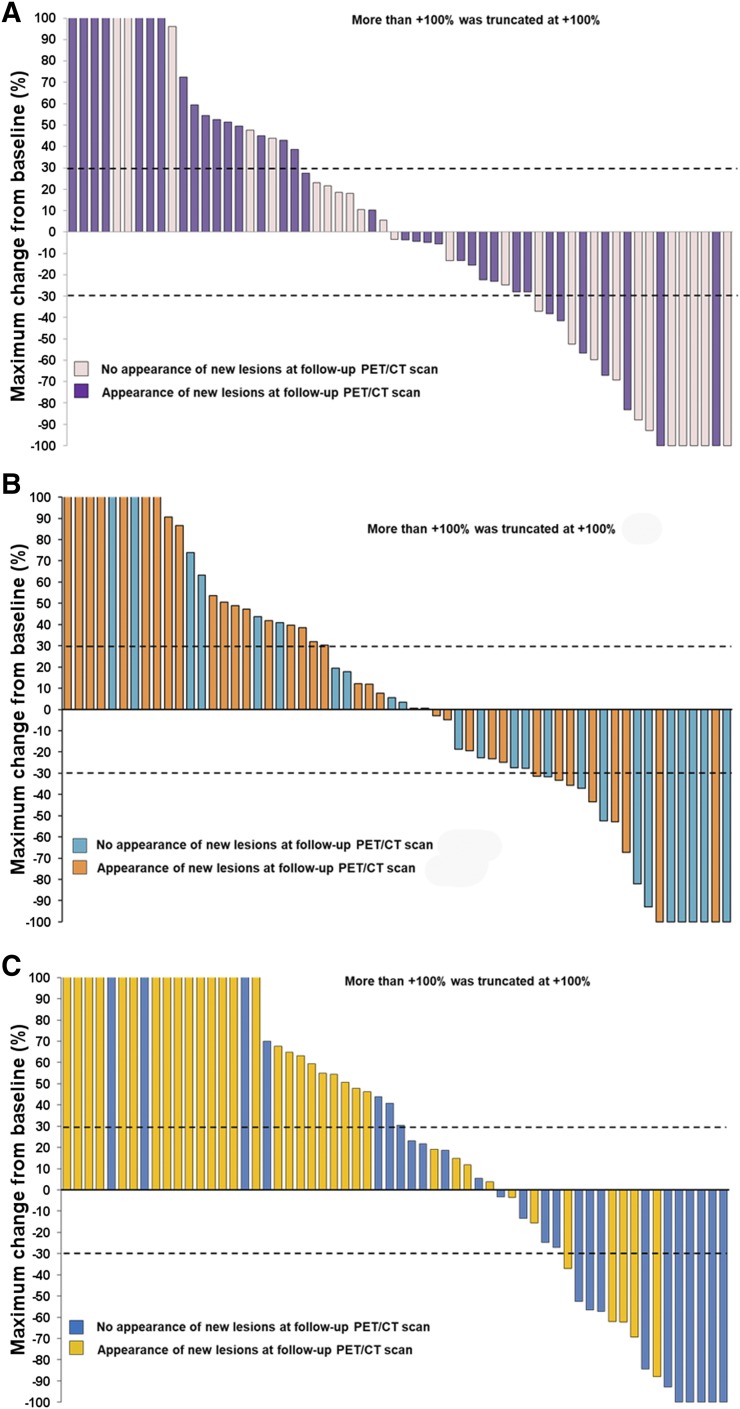
Median changes of SULpeak (%) for PERCIST5, PERCIST1, and imPERCIST5 were −3.60% (range, −100% to +227.02%), +4.46% (range, −100% to +287.57%), and +30.32% (range, −100% to +779.90%), respectively (Fig. 3). Response rates (CMR and PMR) by PERCIST5, PERCIST1, and imPERCIST5 were 18%, 16.7%, and 25%, respectively. Disease control rates (CMR, PMR, and SMD) for the 3 approaches to response assessment were 33%, 32%, and 48%, respectively. In 35 patients, new lesions became apparent on the follow-up scan. Most of these new lesions occurred in patients classified as PMD (n = 24) by imPERCIST5 (with an increase in the sum of SULpeak, and therefore not causing any difference in response classifications by imPERCIST5 vs. PERCIST5). However, in 4 patients, response was classified as PMR by imPERCIST5, but as PMD by PERCIST5 due to the appearance of new lesions. Because of these cases, the response rate by PERCIST5 (18%) was lower than the response rate by imPERCIST5 (25%). In 2 of the 4 patients, the lesions resolved spontaneously, without significantly increasing 18F-FDG uptake or tumor diameter during the follow-up period, indicating a benign etiology. In the other 2 patients, new metastatic disease was confirmed during follow-up (Table 1).
FIGURE 3.
Waterfall plot of maximum changes in SULpeak for PERCIST5 (A), PERCIST1 (B), and imPERCIST5 (C). Upper short dashed line indicates separation of PMD from SMD. Lower short dashed line indicates separation of SMD from PMR.
TABLE 1.
Cases with Appearance of New Lesions in PMR and SMD in imPERCIST5
| Patient no. | Response in imPERCIST5 | Completed ipilimumab cycles | Follow-up PET/CT duration from initial ipilimumab (wk) | %Change of imPERCIST5 | New lesion site | SULpeak | Clinical course and diagnosis |
| 1 | PMR | 4 | 12 | −57.2 | Pancreas body | 2.24 | Metastasis |
| 2 | PMR | 4 | 11 | −84.4 | Skin at right thigh | 0.95 | SR 4 mo later |
| 3 | PMR | 4 | 12 | −61.9 | Left serratus anterior muscle | 1.49 | SR 2 mo later |
| 4 | PMR | 4 | 11 | −62.2 | Paraaortic lymph node | 4.73 | Metastasis |
| 5 | SMD | 4 | 17 | 3.9 | Abdomen lymph node | 2.89 | Metastasis |
| 6 | SMD | 4 | 11 | −3.4 | Left hilar lymph node | 9.29 | Metastasis |
| 7 | SMD | 4 | 11 | −27 | Left hilar lymph node | 3.54 | SR 2 mo later |
| Right hilar lymph node | 3.36 | SR 2 mo later | |||||
| 8 | SMD | 4 | 10 | −15.7 | Left gluteus maximus muscle | 5.69 | Metastasis |
| Right intrailiac lymph mode | 2.98 | Metastasis | |||||
| 9 | SMD | 4 | 15 | 19.1 | Left hilar lymph node | 2.7 | SR 2 mo later |
| Right hilar lymph node | 2.34 | SR 2 mo later | |||||
| 10 | SMD | 4 | 11 | 11.8 | Left cervical lymph node | 2.3 | Unknown |
| Right cervical lymph node | 1.68 | Unknown | |||||
| 11 | SMD | 4 | 11 | 14.8 | Right neck lymph node | 3.79 | Metastasis |
| Transverse colon | 3.67 | SR 2 mo later | |||||
| Soft tissue at right elbow | 1.94 | SR 2 mo later |
SR = spontaneous remission.
A total of 7 patients with a decrease in the sum of SULpeak of target lesions by at least 30% by PERCIST5 showed new suggestive lesions on follow-up imaging. However, 4 of these patients were considered as PMR by imPERCIST5 because the percentage change of the sum of SULpeak including new suggestive lesions was more than −30%; in the other 3 patients, the new lesions included in the sum of SULpeak led to response classification as SMD (n = 2) or PMD (n = 1).
In addition, new lesions were seen in 6 of the 14 patients with SMD by imPERCIST5. Thus, the disease control rate of PERCIST5 was only 33% as compared with 48% for imPERCIST5. In 3 of these patients, metastatic disease was confirmed during follow-up, in 2 patients the lesions resolved without specific treatment, and in 1 patient no definitive decision could be made. The correlations between the response patterns according to imPERCIST5 and other response criteria are shown in Table 2. Discordance in response assessment among PERCIST5, PERCIST1, and imPERCIST5 was observed in 13 and 17 patients (Cohen’s κ; κ = 0.637 and 0.521), respectively.
TABLE 2.
Correlation Between Response Assessments
| PERCIST5 |
PERCIST1 |
|||||||||
| imPERCIST5 | CMR | PMR | SMD | PMD | Total | CMR | PMR | SMD | PMD | Total |
| CMR | 5 | 0 | 0 | 0 | 5 | 5 | 0 | 0 | 0 | 5 |
| PMR | 0 | 6 | 0 | 4 | 10 | 0 | 4 | 2 | 4 | 10 |
| SMD | 0 | 0 | 7 | 7 | 14 | 0 | 1 | 5 | 8 | 14 |
| PMD | 0 | 0 | 2 | 29 | 31 | 0 | 0 | 2 | 29 | 31 |
| Total | 5 | 6 | 9 | 40 | 60 | 5 | 5 | 9 | 41 | 60 |
Treatment Outcome
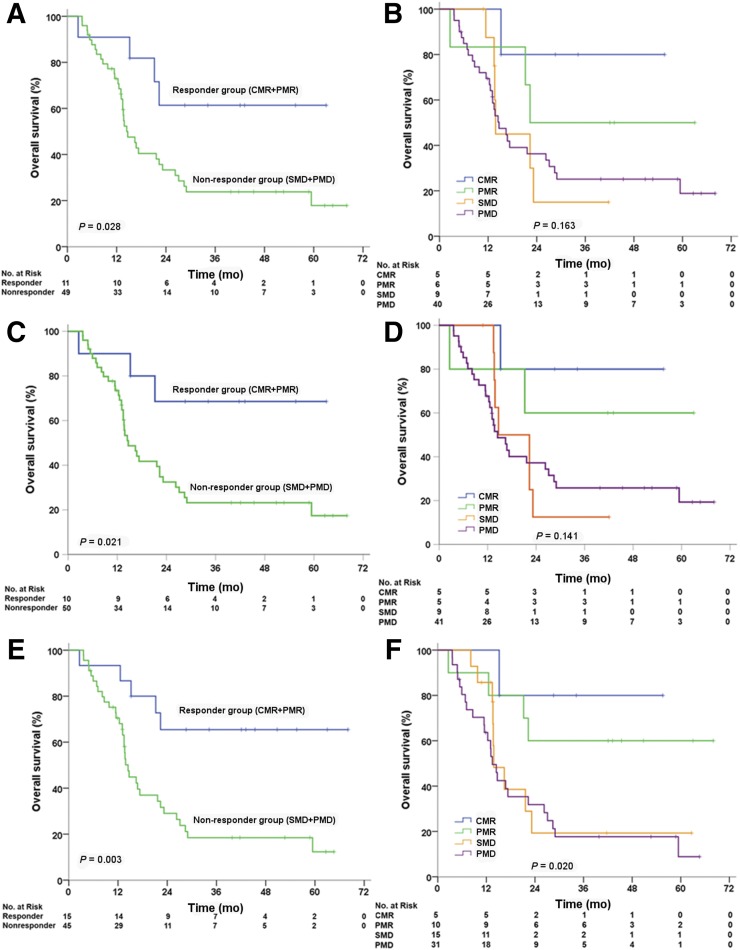
The median duration of follow-up was 14.9 mo (range, 2.6–68.0 mo). At the time of data cutoff for the analysis, 39 patients had died. Median OS for all patients was 17.31 mo (95% CI, 9.45–25.18 mo). The 2-y OS for responders versus nonresponders according to PERCIST5, PERCIST1, and imPERCIST5 was 61% versus 33% (P = 0.028), 69% versus 33% (P = 0.021), and 66% versus 29% (P = 0.003), respectively. In the nonresponder groups of PERCIST5, PERCIST1, and imPERCIST5, median OS was 14.5, 14.7, and 14.5 mo, respectively. In the responder groups, median survival was not reached (Fig. 4). Survival was better in patients with CMR than in those with PMR by imPERCIST5. On the other hand, survival was similar for patients with SMD and PMD (Fig. 4). The Gönen–Heller concordance index was highest for the correlation of response by imPERCIST5 and OS (0.61; 95% CI, 0.541–0.679), followed by PERCIST1 (0.57; 95% CI, 0.507–0.645) and PERCIST5 (0.57; 95% CI, 0.501–0.639).
FIGURE 4.
Kaplan–Meier estimates of OS for responders and nonresponders (left) and survival rates by response category (right). (A and B) PERCIST5. (C and D) PERCIST1. (E and F) imPERCIST5.
In a univariate Cox proportional hazards model, lines of prior chemotherapy, prior radiotherapy, active brain metastases, and response on 18F-FDG PET/CT were significantly associated with OS (Supplemental Table 2). In the multivariate analysis, imPERCIST5 (hazard ratio, 3.853; 95% CI, 1.498–9.911; P = 0.005) was the only independent factor associated with OS.
DISCUSSION
The results of this study indicate that tumor response on 18F-FDG PET/CT as classified by PERCIST is significantly correlated with OS in patients with advanced melanoma treated with ipilimumab. As in previous case reports, we observed a few cases with pseudoprogression, that is, the appearance of new lesions that resolved spontaneously and were probably inflammatory in nature. However, in most patients, the appearance of new lesions was associated with progression of known metastases and poor prognosis.
The correlation between response on 18F-FDG PET/CT and patient survival was improved using modified response criteria (imPERCIST). The key difference between imPERCIST and PERCIST lies in the interpretation of new lesions on the posttreatment scan. In PERCIST, new lesions always indicate PMD. In contrast, imPERCIST includes new lesions in the quantification of tumor 18F-FDG uptake, and a patient is only classified as PMD if the intensity of 18F-FDG uptake for measured lesions increases by at least 30%. In imPERCIST5, the sum of SULpeak for up to 5 lesions is measured to assess response. These modified response criteria use an approach similar to that of the immune-related response criteria for morphologic imaging (12), which include new lesions in the sum of tumor diameters used to quantify overall tumor burden. New lesions do not necessarily result in a scan to be classified as PMD. Of note, whereas imPERCIST5 reduces overdiagnosis of progressive disease, new lesions in patients with PMR or SMD by imPERICST5 were eventually found to have metastases in 55% of the cases (6/11, Table 1). Thus, the prognosis of patients with decreasing or stable target lesions but appearance of new lesions appears indeterminate, and biopsy should be considered before any change in treatment.
To date, only a few reports have been published on the use of 18F-FDG PET/CT to monitor tumor response to ipilimumab and other checkpoint inhibitors. The first results were presented by Sachpekidis et al. (16), who studied a group of 22 patients receiving ipilimumab. Tumor response on 18F-FDG PET/CT was classified by European Organization for Research and Treatment of Cancer (EORTC) criteria (21). Only 2 of the patients achieved a PMR at the end of therapy. Therefore, the authors compared the prognosis of patients with PMD and SMD (and not responders with nonresponders). Progression-free survival was significantly longer for patients with disease stabilization (9.8 vs. 3.6 mo, P < 0.001). Median OS was slightly longer in the group of patients with SMD than in that of patients with PMD (9.8 vs. 9.1 mo). Here we confirm the prognostic value of 18F-FDG PET/CT in an almost 3-fold-larger patient population. The longer OS for the whole patient group in our study is probably related to different baseline patient characteristics and the availability of second-generation immunotherapies in patients progressing after ipilimumab.
In a follow-up publication (22), the same group showed in 41 patients that the number of new 18F-FDG–avid lesions on a posttreatment 18F-FDG PET/CT scan was closely correlated with the clinical benefit of the therapy. Clinical benefit was defined by clinical follow-up, 18F-FDG PET/CT, brain MRI, and laboratory tests. All patients without clinical benefit from ipilimumab therapy demonstrated 4 or more new lesions at the end of therapy, whereas 84% of the patients with clinical benefit demonstrated fewer than 4 new lesions. Unexpectedly, changes in SUVs showed no correlation with clinical benefit, although the previous analysis of 21 patients had demonstrated a correlation with tumor response by EORTC criteria (which define response and progression by changes of SUV) and progression-free survival (22).
In contrast, we observed a significant association between changes in tumor SUV and OS for all 3 approaches for response assessment (PERCIST5, imPERCIST5, and PERCIST1). We used OS, rather than best overall response, as the outcome parameter because best overall response is largely defined by imaging studies, that is, is not an independent reference standard.
As shown in Figure 4, patients with CMR showed longer survival than those with PMR. However, patients with SMD showed almost the same poor survival as patients with PMD. A similar observation has been made in patients with breast cancer treated with chemotherapy (23). This contrasts with response assessment by CT and RECIST, because stable disease on CT is generally associated with better prognosis than progressive disease. The difference may be explained by the fact that at the end of therapy a residual mass on CT may be fibrotic tissue, whereas persistent 18F-FDG uptake usually indicates the presence of viable tumor cells.
Our study has some limitations: although we report on the largest patient population treated with ipilimumab, the results may be affected by selection bias because PET/CT imaging was used at the discretion of the referring physicians. Further, the time between completion of ipilimumab therapy and follow-up imaging was not standardized, which may have affected changes in tumor 18F-FDG uptake and the number of lesions detected. Moreover, timing of scans (uptake time, differences between baseline and follow-up) did not always adhere to PERCIST specifications. Another consequence of the retrospective study design is the use of different PET/CT scanners, which, despite our efforts at standardization, may have caused variability in SUV measurements and insensitivity to detection of new metastases. Despite this variability, which reflects the typical use of 18F-FDG PET/CT in clinical practice, we observed a clear correlation between PET responses and OS, suggesting that response assessment by PERCIST or imPERCIST is robust for clinical use.
CONCLUSION
In this retrospective study, assessment of tumor response to ipilimumab by PERCIST after completion of treatment was significantly correlated with survival of patients with advanced melanoma. Slight modifications of PERCIST (imPERCIST5), changing the definition of PMD, further improved the prognostic value of 18F-FDG PET/CT. These findings are encouraging for the use of FDG PET/CT to assess tumor response to ipilimumab in research and clinical practice.
DISCLOSURE
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748. Dr. Jedd Wolchok is a consultant for Adaptive Biotech; Advaxis; Amgen; Apricity; Array BioPharma; Ascentage Pharma; Astellas; Beigene; Bristol Myers Squibb; Celgene; Chugai; Elucida; Eli Lilly; F Star; Genentech; Imvaq; Kleo Pharma; MedImmune; Merck; Neon Therapeutics; Ono; Polaris Pharma; Polynoma; Psioxus; Puretech; Recepta; Trienza; Sellas Life Sciences; Serametrix; Surface Oncology; and Syndax. He received research support from Bristol Myers Squibb; Medimmune; Merck Pharmaceuticals; and Genentech and holds equity in Potenza Therapeutics; Tizona Pharmaceuticals; Adaptive Biotechnologies; Elucida; Imvaq; Beigene; and Trieza. Dr. Wolfgang Weber received research support from Ipsen, Piramal, Blue Earth Diagnostics, and Bristol-Myers Squibb. He has served as a consultant for Progenics Pharmaceuticals Inc., Endocyte, Merck, Bayer, and Blue Earth Diagnostics. No other potential conflict of interest relevant to this article was reported.
Supplementary Material
REFERENCES
- 1.Postow MA, Callahan MK, Wolchok JD. Immune checkpoint blockade in cancer therapy. J Clin Oncol. 2015;33:1974–1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolchok JD, Hodi FS, Weber JS, et al. Development of ipilimumab: a novel immunotherapeutic approach for the treatment of advanced melanoma. Ann N Y Acad Sci. 2013;1291:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pennock GK, Waterfield W, Wolchok JD. Patient responses to ipilimumab, a novel immunopotentiator for metastatic melanoma: how different are these from conventional treatment responses? Am J Clin Oncol. 2012;35:606–611. [DOI] [PubMed] [Google Scholar]
- 4.Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517–2526. [DOI] [PubMed] [Google Scholar]
- 6.Schadendorf D, Hodi FS, Robert C, et al. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J Clin Oncol. 2015;33:1889–1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Postow MA, Chesney J, Pavlick AC, et al. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N Engl J Med. 2015;372:2006–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chiou VL, Burotto M. Pseudoprogression and immune-related response in solid tumors. J Clin Oncol. 2015;33:3541–3543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hodi FS, Hwu WJ, Kefford R, et al. Evaluation of immune-related response criteria and RECIST v1.1 in patients with advanced melanoma treated with pembrolizumab. J Clin Oncol. 2016;34:1510–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seymour L, Bogaerts J, Perrone A, et al. iRECIST: guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 2017;18:e143–e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishino M, Giobbie-Hurder A, Gargano M, Suda M, Ramaiya NH, Hodi FS. Developing a common language for tumor response to immunotherapy: immune-related response criteria using unidimensional measurements. Clin Cancer Res. 2013;19:3936–3943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolchok JD, Hoos A, O’Day S, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res. 2009;15:7412–7420. [DOI] [PubMed] [Google Scholar]
- 13.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–247. [DOI] [PubMed] [Google Scholar]
- 14.Kubota R, Kubota K, Yamada S, Tada M, Ido T, Tamahashi N. Microautoradiographic study for the differentiation of intratumoral macrophages, granulation tissues and cancer cells by the dynamics of fluorine-18-fluorodeoxyglucose uptake. J Nucl Med. 1994;35:104–112. [PubMed] [Google Scholar]
- 15.Wachsmann JW, Ganti R, Peng F. Immune-mediated disease in ipilimumab immunotherapy of melanoma with FDG PET-CT. Acad Radiol. 2017;24:111–115. [DOI] [PubMed] [Google Scholar]
- 16.Sachpekidis C, Larribere L, Pan L, Haberkorn U, Dimitrakopoulou-Strauss A, Hassel JC. Predictive value of early 18F-FDG PET/CT studies for treatment response evaluation to ipilimumab in metastatic melanoma: preliminary results of an ongoing study. Eur J Nucl Med Mol Imaging. 2015;42:386–396. [DOI] [PubMed] [Google Scholar]
- 17.Cho SY, Lipson EJ, Im HJ, et al. Prediction of response to immune checkpoint inhibitor therapy using early-time-point 18F-FDG PET/CT imaging in patients with advanced melanoma. J Nucl Med. 2017;58:1421–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(suppl 1):122S–150S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson JR, Cain KC, Gelber RD. Analysis of survival by tumor response. J Clin Oncol. 1983;1:710–719. [DOI] [PubMed] [Google Scholar]
- 20.Gönen M, Heller G. Concordance probability and discriminatory power in proportional hazards regression. Biometrika. 2005;92:965–970. [Google Scholar]
- 21.Young H, Baum R, Cremerius U, et al. Measurement of clinical and subclinical tumour response using [18F]-fluorodeoxyglucose and positron emission tomography: review and 1999 EORTC recommendations. European Organization for Research and Treatment of Cancer (EORTC) PET Study Group. Eur J Cancer. 1999;35:1773–1782. [DOI] [PubMed] [Google Scholar]
- 22.Anwar H, Sachpekidis C, Winkler J, et al. Absolute number of new lesions on 18F-FDG PET/CT is more predictive of clinical response than SUV changes in metastatic melanoma patients receiving ipilimumab. Eur J Nucl Med Mol Imaging. 2018;45:376–383. [DOI] [PubMed] [Google Scholar]
- 23.Riedl CC, Pinker K, Ulaner GA, et al. Comparison of FDG-PET/CT and contrast-enhanced CT for monitoring therapy response in patients with metastatic breast cancer. Eur J Nucl Med Mol Imaging. 2017;44:1428–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.