Abstract
An 89-year-old man presented to the emergency department with a 1-month history of upper right quadrant pain, worsened in the last 3 days and accompanied by fever and chills. On physical examination, he had scleral icterus and right upper quadrant tenderness. Laboratory findings showed hyperbilirubinemia, elevated liver enzymes and C reactive protein. The patient was admitted, suspecting of an acute cholangitis and started on antibiotics. An upper gastrointestinal endoscopy revealed the presence of a juxtapapillary diverticulum in the second portion of the duodenum, which was confirmed by a magnetic resonance cholangiopancreatography, along with upstream biliary tract ectasia. The imaging findings allowed us to diagnose a Lemmel’s syndrome. Due to potential surgical risk, we decided for a conservative approach. The patient had a favourable course and was discharged home.
Keywords: pancreas and biliary tract, infection (gastroenterology)
Background
This case alerts us to rare benign situations that can lead to disease and can mimic malignant neoplasms. Is important to make a full investigation to perform the correct diagnostic. According to the diagnosis and the patient characteristics we should decide the best treatment and follow-up.
Case presentation
An 89-year-old man presented to the emergency department with a 1-day history of fever and chills. Additionally, he referred intermittent abdominal pain located to the upper right quadrant during the last month, worsened in the last 3 days. He had no significant medical history except for dementia and osteoarthritis, and his medications included analgesics, donepezil and a benzodiazepine.
Investigations
On physical examination, he had scleral icterus and tenderness on his right upper quadrant of the abdomen. Murphy’s sign was equivocal. The blood pressure was of 124/67 mmHg with a normal heart rate and a tympanic temperature of 38.9°C.
Laboratory findings revealed a total bilirubin of 5.1 mg/dL with a direct fraction of 2.9 mg/dL, serum aspartate aminotransferase of 171 U/L, alanine aminotransferase of 243 U/L, alkaline phosphatase of 236 U/L, γ-glutamyl transferase of 374 U/L and C reactive protein of 13.2 mg/dL (table 1). The leucocyte count was normal. The remaining laboratory values were unremarkable.
Table 1.
Evolution of analytical parameters
| Parameters | Reference values | Day 1 emergency department |
Day 12 at discharge |
4 months after discharge |
| Total bilirubin (mg/dL) | 0.2–1.2 | 5.1 | 1.6 | 1.4 |
| Direct bilirubin (mg/dL) | 0.1–0.4 | 2.9 | 0.3 | 0.3 |
| Serum aspartate aminotransferase (U/L) | 6–34 | 171 | 40 | 23 |
| Serum alanine aminotransferase (U/L) | 20–60 | 243 | 29 | 13 |
| γ-Glutamyl transferase (U/L) | 0–30 | 374 | 255 | 64 |
| Alkaline phosphatase (U/L) | 50–100 | 236 | 193 | 78 |
| C reactive protein (mg/dL) | <0.5 | 13.2 | 1.30 | 0.14 |
Abdominal ultrasonography was performed, with no evidence of choledocholithiasis or dilatation of biliary and main pancreatic ducts.
The patient was admitted to the internal medicine ward with suspected acute cholangitis and started on antibiotic piperacillin/tazobactam.
As the patient remained symptomatic, an upper gastrointestinal endoscopy was performed, revealing the presence of a juxtapappilary diverticulum in the second portion of the duodenum.
Abdominal CT was carried out. The liver had normal dimensions and no nodular formations were identified. There was prominence of the intrahepatic bile ducts in the lateral segments of the left lobe as well as of the extrahepatic ones, with a main bile duct maximum calibre of 7 mm. There were no abrupt size calibre reductions of the biliary tract or anomalous enhancements of its wall. On the gallbladder, there were no stones. A diverticulum was observed in the medial wall of the second portion of the duodenum with about 22×17 mm, insinuating itself in the pancreatic head, causing the dilatation of the bile ducts (figures 1 and 2).
Figure 1.
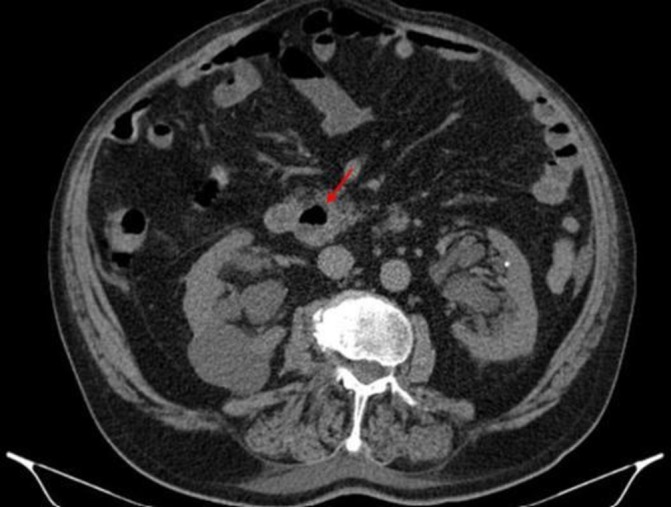
Abdominal CT showing a periampullary duodenal diverticulum filled with fluid on transverse plane.
Figure 2.
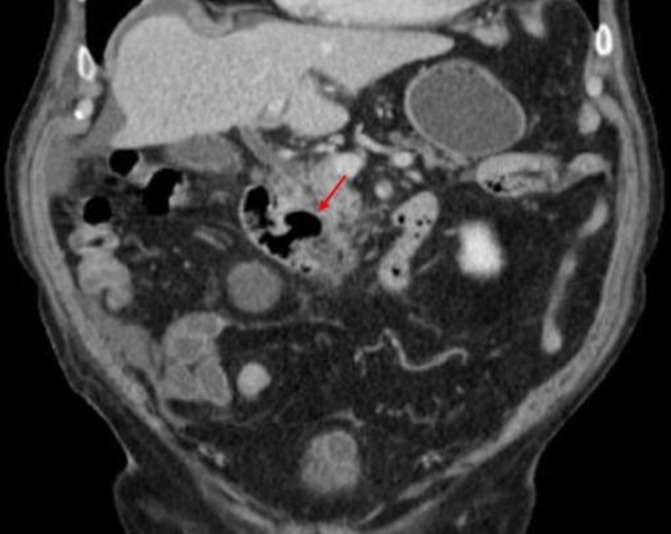
Abdominal CT showing a periampullary duodenal diverticulum filled with fluid on coronal plane.
All microbiologic studies, including blood cultures and serologic tests for cytomegalovirus, Epstein-Barr virus, herpes simplex virus, leptospirosis, toxoplasmosis, hepatitis A, B and C virus and syphilis screening were negative.
Differential diagnosis
Potential causes for the signs and symptoms presented by the patient, like viral hepatitis or bacterial infections that can affect the liver were considered, but serological tests were negative. Choledocholithiasis, acute cholecystitis and malignant causes, such as cholangiocarcinoma or ampullary cancer, were excluded by imaging methods that showed no evidence of stones or malignancy.
Treatment
The patient was on nothing by mouth for 4 days with intravenous fluids and oral feeding was resumed on day 4, when pain subsided. He completed a total of 7 days of antibiotic therapy, with clinical and laboratorial improvement (table 1). No complications were registered during the hospital stay.
Outcome and follow-up
One month after discharge, a magnetic resonance cholangiopancreatography (MRCP) confirmed the abdominal CT findings: discrete dilation of the intrahepatic bile ducts, a 25 mm juxtapappilary diverticulum on the second portion of the duodenum, suggestive of being the cause of the dilatation of the upstream billiary tract (figure 3), and no signs of chronic pancreatitis or choledocholithiasis.
Figure 3.
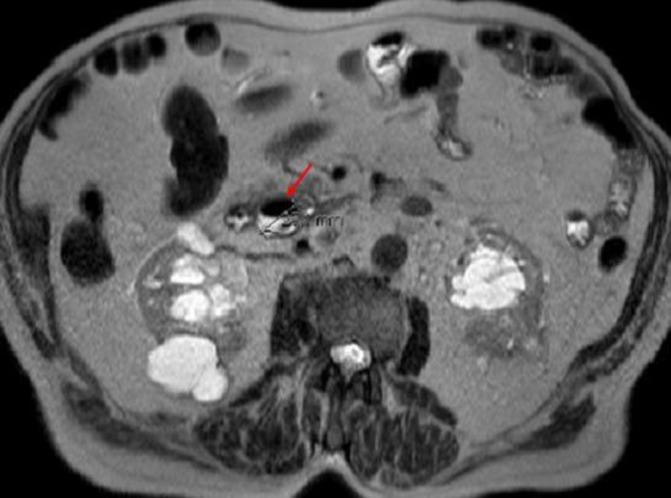
Magnetic resonance cholangiopancreatography showing a periampullary duodenal diverticulum filled with fluid, with 25 mm.
The imaging findings along with the exclusion of other causes, such as bile duct calculi or tumours, confirmed the diagnosis of Lemmel’s syndrome.
The patient was observed at our outpatient clinic 4 months after discharge, asymptomatic and with normalised laboratory results (table 1).
Discussion
In our case, the clinic and laboratory results presented by the patient were highly suggestive of acute cholangitis. In the absence of cholelithiasis, recent surgical history or another detectable obstacle besides the juxtapapillary diverticulum, Lemmel’s syndrome complicated by acute cholangitis was diagnosed.
Most juxtapapillary diverticula are asymptomatic, but complications can occur in about 5% of cases.1 Complications can be divided in non-pancreaticobiliary or pancreaticobiliary. Non-pancreaticobiliary complications are rare and may include diverticulitis, haemorrhage, perforation or fistula formation.2 Pancreaticobiliary complications can present as obstructive jaundice, acute pancreatitis or cholangitis,2 gallbladder or bile duct stones.3 These complications can be recurrent, due to mechanical compression of the terminal bile duct by duodenal diverticulum.4
There are three possible causes leading to the development of Lemmel’s syndrome: first, fibrosis of the papilla can be caused by direct mechanical irritation of periampullary diverticula that may lead to chronic inflammation of the ampulla; second, periampullary diverticula may cause dysfunction of the sphincter of Oddi; and third, periampullary diverticula cause mechanical compression of the distal common bile duct or ampulla.5
Imaging is essential to correctly identify and diagnose this syndrome. The diverticula may appear as thin-walled cavitary lesions, sometimes filled with fluid in the abdominal CT scan or MRCP3 (as in this case). These findings imply differential diagnosis with pancreatic abscess, cystic neoplasm in the pancreatic head or metastatic lymph node.6
Therapeutic options for this syndrome include surgery, endoscopic intervention or conservative treatment. Surgical option may be necessary in case of complicated billiary obstruction or pancreatitis, but the procedure is difficult and has high mortality.4 Symptomatic patients can also be successfully managed endoscopically through sphincterotomy or endoscopic papillary balloon dilatation.1 7 Despite being a minimal-invasive procedure, complications, such as delayed perforation of the diverticulum or stent obstruction, can occur.4 In relatively asymptomatic patients, a conservative treatment is recommended.8 However, it can recur and even progress to stenosis of the bile duct, leading to subsequent episodes of obstructive jaundice or even cholangiocarcinoma, therefore the patient should be kept on regular observation.7
Attending to the patient’s age and the quick recovery of the acute complication, we decided on a conservative approach and regular follow-up at our outpatient clinic.
Learning points.
Lemmel’s syndrome is a rare and benign cause of obstructive jaundice that should be considered in the differential diagnosis of biliary obstruction.
A high index of suspicion is important since it can mimic malignant neoplasm.
The correct diagnosis is crucial to administer the proper treatment and adequate follow-up to prevent further complications.
Depending on the patient’s characteristics, symptoms and complications, it can be treated surgically, endoscopically or a conservative approach can be preferred.
Footnotes
Contributors: DMO wrote the manuscript with support from CC, FC and PD. PD helped supervise the work and conceived the original idea.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
References
- 1. Kang HS, Hyun JJ, Kim SY, et al. Lemmel’s syndrome, an unusual cause of abdominal pain and jaundice by impacted intradiverticular enterolith: case report. J Korean Med Sci 2014;29:874–8. 10.3346/jkms.2014.29.6.874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Castilho Netto JM, Speranzini MB. Ampullary duodenal diverticulum and cholangitis. Sao Paulo Med J 2003;121:173–5. 10.1590/S1516-31802003000400007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Desai K, Wermers JD, Beteselassie N. Lemmel syndrome secondary to duodenal diverticulitis: a case report. Cureus 2017;9:e1066 10.7759/cureus.1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yoneyama F, Miyata K, Ohta H, et al. Excision of a juxtapapillary duodenal diverticulum causing biliary obstruction: report of three cases. J Hepatobiliary Pancreat Surg 2004;11:69–72. 10.1007/s00534-003-0854-7 [DOI] [PubMed] [Google Scholar]
- 5. Rouet J, Gaujoux S, Ronot M, et al. Lemmel’s syndrome as a rare cause of obstructive jaundice. Clin Res Hepatol Gastroenterol 2012;36:628–31. 10.1016/j.clinre.2012.05.002 [DOI] [PubMed] [Google Scholar]
- 6. Macari M, Lazarus D, Israel G, et al. Duodenal diverticula mimicking cystic neoplasms of the pancreas: CT and MR imaging findings in seven patients. AJR Am J Roentgenol 2003;180:195–9. 10.2214/ajr.180.1.1800195 [DOI] [PubMed] [Google Scholar]
- 7. Carmona Agúndez M, López Guerra D, Fernández Pérez J, et al. Lemmel’s syndrome: obstructive jaundice secondary to a duodenal diverticulum. Cir Esp 2017;95:487–554. 10.1016/j.ciresp.2017.02.003 [DOI] [PubMed] [Google Scholar]
- 8. Ferreira-Aparicio FE, Gutiérrez-Vega R, Gálvez-Molina Y, et al. Diverticular disease of the small bowel. Case Rep Gastroenterol 2012;6:668–76. 10.1159/000343598 [DOI] [PMC free article] [PubMed] [Google Scholar]


