Abstract
A 74-year-old man presented to our hospital with recurrent lower gastrointestinal bleeding. His past medical history was remarkable for a duodenal papilla carcinoma and he underwent a pylorus-preserving pancreaticoduodenectomy 4 years before. During diagnostic work-up a severe portal vein stenosis after surgery and multiple dilated intramural jejunal varices, which formed as collateral pathways could be detected. Based on these findings, the recurrent haemorrhages were considered to be due to repeated rupturing and bleeding of jejunal varices. Therapeutically, the portal vein stenosis was treated with endovascular stent placement leading to a reduction in prestenotic portal pressure. During follow-up no further episodes of gastrointestinal bleeding were observed. Bleeding from jejunal varices is a very rare cause of gastrointestinal haemorrhages and represents a diagnostic and therapeutic challenge. However, it should be considered in differential diagnosis of obscure recurrent gastrointestinal haemorrhages in patients with a history of hepato-pancreato-biliary surgery.
Keywords: gi bleeding, endoscopy, varices, portal hypertension, small intestine
Background
Intramural jejunal varices are an uncommon manifestation of portal hypertension and bleeding from such jejunal varices is very rare cause of gastrointestinal haemorrhages and represents a diagnostic and therapeutic challenge as well.
With our case report we want to raise awareness of this rare pathology and want to achieve that small-bowel variceal bleeding should be considered in differential diagnosis of obscure recurrent gastrointestinal haemorrhages in patients with a history of hepato-pancreato-biliary surgery.
Case presentation
A 74-year-old man presented to our hospital with recurrent signs and symptoms of lower gastrointestinal bleeding. He had intermittent melena and fatigue, but denied haematemesis, dyspnoea, nausea, weight loss, night sweats or fever. His blood pressure was 90/70 mm Hg and his heart rate was 110 beats/min. Laboratory tests revealed a microcytic hypochromic anaemia with a haemoglobin level of 67 g/L (normal range: 130–180 g/L), a thrombocytopenia with platelet count of 74×109/L (normal range: 150–400×109/L), a slightly increased C reactive protein level 15.7 mg/dL (normal range:<5.0 mg/dL) and normal liver function test.
His medical history was remarkable for a duodenal papilla carcinoma and he underwent a pylorus-preserving pancreaticoduodenectomy 4 years before. Postsurgery, an extrahepatic portal vein stenosis due to postsurgical adhesions as well as a portal vein thrombosis was observed and oral anticoagulation therapy was initiated.
Investigations
To clarify the aetiology of the recurrent gastrointestinal haemorrhages an oesophagogastroduodenoscopy (OGD) was performed and revealed grade II oesophageal varices, mild portal hypertensive gastropathy and gastric antral vascular ectasia, none of which displayed stigmata of recent bleeding.
Although, detected varices were successfully ligated, gastric antral vascular ectasia was treated with argon plasma coagulation and oral anticoagulation therapy was stopped, further episodes of melena occurred.
Additional endoscopic investigations were performed, including colonoscopy and upper intestinoscopy, however no particular source of bleeding could be identified.
Since the patient continued to have melena and anaemia due to substantial gastrointestinal blood loss another OGD was performed.
On repeated OGD signs of bleeding were recognised within the afferent jejunal loop and a small bleeding lesion was detected close to the hepaticojejunostomy (figure 1). Two endoclips were placed on the lesion and haemostasis was obtained.
Figure 1.
Upper endoscopy of the afferent jejunal loop, showing a small bleeding lesion close to the hepaticojejunostomy.
Concomitantly, abdominal ultrasound, CT angiography of the abdomen and a percutaneous transhepatic portography were performed for further diagnostic work up.
Abdominal imaging revealed the persistent severe portal vein stenosis and multiple dilated intramural collaterals of the afferent jejunal loop surrounding the hepaticojejunostomy (figures 2-4).
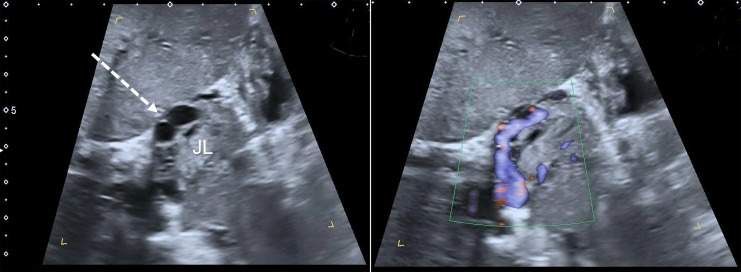
Figure 2.
Focused abdominal ultrasound. Right flank scan with colour Doppler of the liver and portal vein, showing segmental hypoechoic discontinuation (solid white arrow) of the portal vein and multiple intramural prestenotic collaterals of the afferent jejunal loop (dashed white arrow).
Figure 3.
Focused abdominal ultrasound. Intercostal scan with colour Doppler of a proximal jejunal loop (JL), showing multiple perfused and dilated intramural jejunal varices (dashed white arrow).
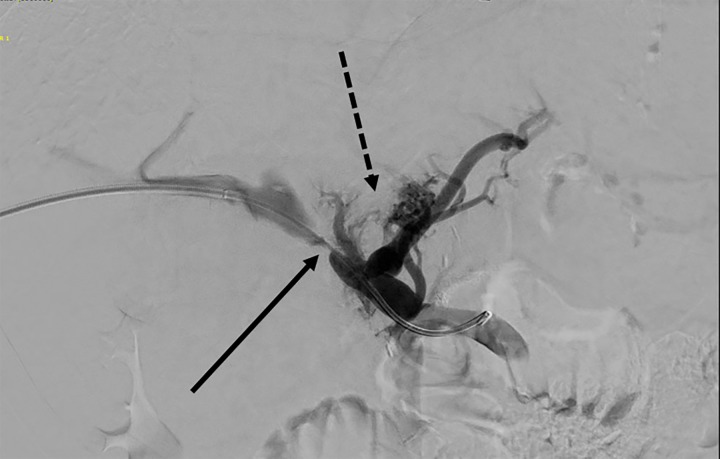
Figure 4.
Direct portogram via transhepatic approach, showing severe stenosis of the extrahepatic portal vein (solid black arrow) and markedly dilated hepatopetal collaterals surrounding the afferent Roux-en-Y jejunal loop and the hepaticojejunostomy (dashed black arrow).
Based on these findings, the recurrent haemorrhages were considered to be due to repeated rupturing and bleeding of intramural jejunal varices, which had developed due to extrahepatic portal venous obstruction.
Treatment
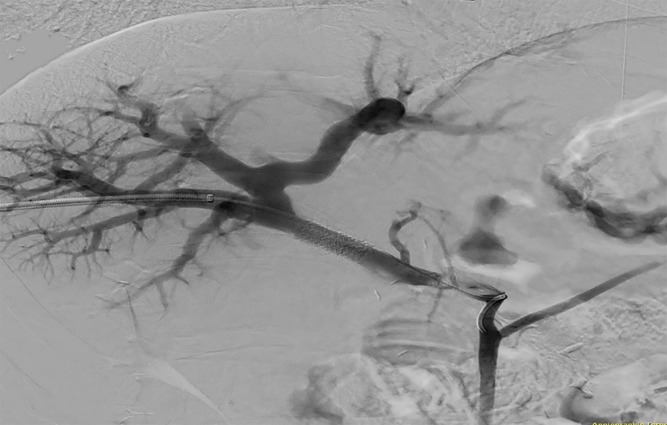
Therapeutically, the portal vein stenosis was treated with endovascular stent placement via a percutaneous transhepatic balloon dilatation leading to a significant reduction in prestenotic portal pressure and relief of the jejunal varices (figure 5). Subsequent portography demonstrated the disappearance of the jejunal collaterals and sufficient reduction of portal pressure was measured.
Figure 5.
Percutaneous transhepatic portography after stent placement showed that the portal stenosis was relieved and disappearance of the collaterals.
Outcome and follow-up
During follow-up no further episodes of gastrointestinal bleeding were observed.
Discussion
Jejunal varices are an uncommon manifestation of portal hypertension, which may be due to liver cirrhosis, portal vein thrombosis or postsurgery extrahepatic portal vein stenosis and are challenging in terms of diagnosis and treatment.1–5 Whereas bleeding due to portal hypertension mostly arises from gastro-oesophageal varices, jejunal varices as bleeding source in patients with portal hypertension are rare.
Bleeding from jejunal varices occurs if the portal vein pressure increases and (micro-) ruptures develop.2 Clinical signs resemble those of upper or middle gastrointestinal bleeding like melena with absence of haematemesis. A history of previous hepato-pancreato-biliary surgery should also raise suspicion of jejunal varices. In those patients who have undergone hepato-pancreato-biliary tract surgery, postsurgery induced inflammation may induce periportal fibrosis leading to a portal vein obstruction with consecutive development of prehepatic portal hypertension.6
Based on these aspects, the most common clinical features of jejunal varices are portal hypertension, a history of abdominal surgery and melena without haematemesis.
Problematically, jejunal variceal bleeding is difficult to diagnose due to the small bowel’s length and tortuous configuration. Haemorrhages from jejunal varices might be best detected during CT angiography of the abdomen, OGD, capsule endoscopy or intestinoscopy.1 4 However, reaching the afferent jejunal loop endoscopically might be difficult in postsurgical state.2
Therapeutic approaches for bleeding from jejunal varices either focus on varices itself or on resolving the underlying portal hypertension.2Treatment options include surgical resection of the bowel segment containing varices, transjugular intrahepatic portosystemic shunt insertion, surgical portosystemic shunt formation, endoscopic sclerotherapy, variceal embolisation or angiographic portal vein dilatation with or without stent implantation.2 6–8
In conclusion, bleeding from jejunal varices is very rare cause of gastrointestinal haemorrhages and represents a diagnostic and therapeutic challenge. However, it should be considered in differential diagnosis of obscure recurrent gastrointestinal haemorrhages in patients with portal hypertension or a history of hepato-pancreato-biliary surgery and negative findings in upper and lower endoscopy.
Learning points.
Jejunal variceal bleeding represents an extremely rare cause of gastrointestinal bleeding.
Jejunal varices are associated with intrahepatic and extrahepatic portal hypertension, which may be due to liver cirrhosis, extrahepatic portal venous obstruction after surgical procedures or abdominal vascular thrombosis.
Typical clinical features of jejunal varices are portal hypertension, a history of abdominal surgery and melena without haematemesis.
Treatment options of small-bowel varices includes surgery, transjugular intrahepatic portosystemic shunt insertion, endoscopic sclerotherapy, variceal embolisation or angiographic portal vein dilatation with or without stent implantation.
Footnotes
Contributors: PK: internist, wrote the manuscript, reviewed the literature and involved in the management of the patient. CS, NJ and TG: internist, involved in the management of the patient, involved in conception and design of the article, revised and critically reviewed the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Koo SM, Jeong SW, Jang JY, et al. Jejunal variceal bleeding successfully treated with percutaneous coil embolization. J Korean Med Sci 2012;27:321–4. 10.3346/jkms.2012.27.3.321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hyun D, Park KB, Cho SK, et al. Portal Vein Stenting for Delayed Jejunal Varix Bleeding Associated with Portal Venous Occlusion after Hepatobiliary and Pancreatic Surgery. Korean J Radiol 2017;18:828–34. 10.3348/kjr.2017.18.5.828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yuki N, Kubo M, Noro Y, et al. Jejunal varices as a cause of massive gastrointestinal bleeding. Am J Gastroenterol 1992;87:514–7. [PubMed] [Google Scholar]
- 4. Joo YE, Kim HS, Choi SK, et al. Massive gastrointestinal bleeding from jejunal varices. J Gastroenterol 2000;35:775–8. 10.1007/s005350070037 [DOI] [PubMed] [Google Scholar]
- 5. Mansoor E, Singh A, Nizialek G, et al. Massive Gastrointestinal Bleeding Due to Isolated Jejunal Varices in a Patient With Extrahepatic Portal Hypertension: A Case Report. Am J Gastroenterol 2016;111:1209–11. 10.1038/ajg.2016.191 [DOI] [PubMed] [Google Scholar]
- 6. Ota S, Suzuki S, Mitsuoka H, et al. Effect of a portal venous stent for gastrointestinal hemorrhage from jejunal varices caused by portal hypertension after pancreatoduodenectomy. J Hepatobiliary Pancreat Surg 2005;12:88–92. 10.1007/s00534-004-0941-4 [DOI] [PubMed] [Google Scholar]
- 7. Hiraoka K, Kondo S, Ambo Y, et al. Portal venous dilatation and stenting for bleeding jejunal varices: report of two cases. Surg Today 2001;31:1008–11. 10.1007/s005950170013 [DOI] [PubMed] [Google Scholar]
- 8. Gubler C, Glenck M, Pfammatter T, et al. Successful treatment of anastomotic jejunal varices with N-butyl-2-cyanoacrylate (Histoacryl): single-center experience. Endoscopy 2012;44:776–9. 10.1055/s-0032-1309834 [DOI] [PubMed] [Google Scholar]