Abstract
Introduction:
Hypertrophic non-union of the tibia is rare in children. Gradual deformity correction by distraction osteogenesis is the conventional management strategy for this problem. In cases with significant multiplanar deformities, this needs careful pre-operative planning and execution that involves long periods of “dynamic” phase of Ilizarov method.
Case Report:
We devised a simpler strategy of complete intraoperative deformity correction in one or two stages followed by compression osteosynthesis. We report the good outcome in four patients (3 males, and 1 female, age 4-—years) with regard to union, alignment, limb length, and function, with significantly short duration of the “dynamic” phase of Ilizarov osteosynthesis.
Conclusion:
Acute deformity correction and compression osteosynthesis is are an effective strategy in hypertrophic non-union of tibia in children. This is applicable for cases with significant deformity without shortening. This considerably shortens the “dynamic” phase of Ilizaov osteosynthesis, facilitating early return to home of patients who need to travel long distances for treatment.
Keywords: Hypertrophic non-union, tibia, Ilizarov, compression osteosynthesis, pediatric non-union
Learning Point of the Article:
Acute deformity correction and compression osteosynthesis are an easy and effective solution for hypertrophic nonunion of the tibia in children.
Introduction
Distraction osteogenesis with Ilizarov external fixator has been reported an effective treatment modality of the closed treatment of hypertrophic nonunion of the tibia in adults [1]. Similar reports are available in children, though extremely rare [2]. Distraction osteogenesis undoubtedly is the most versatile strategy in this situation as it does not involve opening of fracture site and addresses all associated problems such as angulation, rotation, and limb length. This is the most relevant in cases with associated shortening. However, this requires careful pre-operative planning and meticulous post-operative adjustment of fixator and radiological evaluation of nonunion site to achieve optimum results. In addition, these cases may need multiple realignments to correct translations and rotations which are very challenging to correct otherwise. This can be effort intensive for both the surgeon and the patient [2]. Even in cases of hypertrophic union without any shortening, literature speaks only of gradual correction of deformity by distraction [1, 2]. If this results in lengthening compared to the opposite limb, the fracture site is longitudinally compressed (after deformity correction) to equalize limb length. It is thought that distraction converts the fibrous tissue to immature osseous tissue by metaplasia that promotes healing of fracture. In cases with shortening, it is allowed to heal in distraction, whereas if this produces lengthening, compression is applied until the desired amount of shortening is achieved. Gradual compression in this setting is thought to accelerate healing by inducing microfractures of the regenerate and stimulating callus response [1]. We report our experience of a simpler strategy that we employed due to patient-related reason. These patients (belonging to poor socioeconomic strata of the society) had traveled for long distances to come to our tertiary level referral teaching hospital and had difficulty with staying nearby our center for monitored adjustment of fixator postoperatively. Our strategy was devised primarily to shorten the “dynamic” phase of Ilizarov so that the children could return to their homes during the “static” phase, causing less economic and social stress to the family. All these children had hypertrophic nonunion of the tibia with significant multiplanar deformity and no shortening.
Case Report
Patient profile
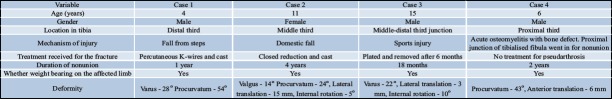
We had four children (3 males and 1 female, age 4—years) with hypertrophic nonunion of the tibia. Three of them were post-traumatic. The fourth patient had tibial bone defect following acute osteomyelitis. He underwent tibialisation of the fibula elsewhere. The distal junction united uneventfully, but the proximal junction went in for hypertrophic nonunion. The demographic and clinical characteristics of our patient cohort are summarized in Table 1 (Fig. 1, 2, 3, 4).
Table 1.
Figure 1.
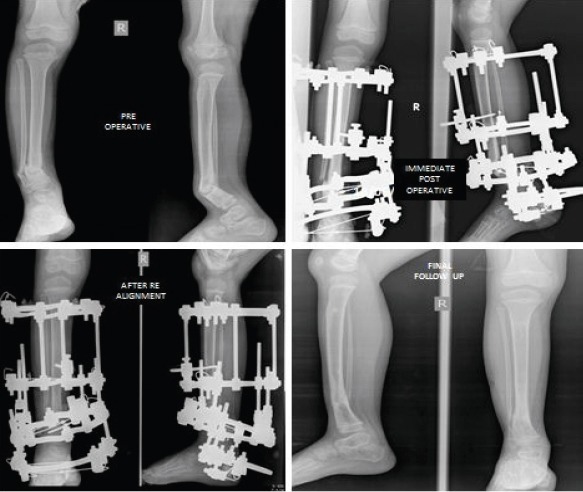
Pre-operative, post-operative, and follow-up radiographs of case 1 (male, 4 years)
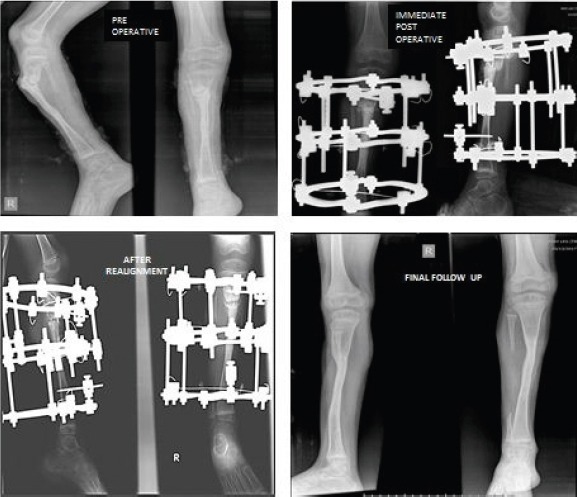
Figure 2.

Pre-operative, post-operative, and follow-up radiographs of case 2 (female, 11 years)
Figure 3.

Pre-operative, post-operative, and follow-up radiographs of case 3 (male, 15 years)
Figure 4.
Pre-operative, post-operative, and follow-up radiographs of case 4 (male, 6 years, nonunion of fibular graft)
Surgical technique
All patients were operated in the supine position in radiolucent table under radiological monitoring. The fibula was osteotomized through a stab incision at the junction its middle and lower third in three of the cases (one patient lacked fibula due to prior tibialisation). Mobility of the pseudarthrosis was reassessed at this stage, and all nonunions were stiff. Ilizarov apparatus was assembled in the standard fashion with its proximal and distal modules parallel to their respective segments. Once the rings were assembled independently in proximal and distal segments, the fracture site was accessed through a stab incision. Vigorous drilling of the pseudarthrosis was done with 4.5mm drill bit, and the pseudarthrosis was made relatively mobile (one case needed passage of osteotome percutaneously to achieve mobility). At this stage, deformity correction was attempted by making the proximal and distal modules parallel to each other and connecting them with straight rods. Near-complete deformity correction was achieved on the table in two of our cases. In the other two, there was residual deformity. A complete correction was not attempted as there would be undue stretch of the soft tissue otherwise. Both these cases were taken for realignment under anesthesia after a week, and complete deformity correction was achieved.
Post-operative care
Compression at the pseudarthrosis was used as the sole post-operative strategy. It was ensured during surgery (as much as possible) that there was no residual translational or rotational deformity. After a latent period of 3 days, minor residual deformity correction in the coronal or sagittal plane was performed by differential compression of the connecting rods. Once this was achieved, compression was applied all around the pseudarthrosis at a rate of 0.5 mm per day until there was good approximation of cortices radiologically in orthogonal views. The patients were made to mobilize the knee and ankle (the ankle was spanned in one patient where the pseudarthrosis was in the distal fourth of the tibia) and bear weight fully with support. The patients were taught pin tract care and asked to go home with proper instructions for rehabilitation and were asked to follow-up once in 6 weeks or whenever necessary.
Results
All patients had a follow-up of 2 years from the removal of external fixator. All four non-unions united uneventfully. In the ntwo patients were deformity correction was completed in two stages, compression commenced after 3 days after second surgery. (No manipulation was done during the week in between two stages as it would inadvertently stretch the soft tissue.) Another patient (where all deformities were acutely corrected) developed minimal swelling of the limb and blebs on the 2nd day. It responded to limb elevation and delay of rehabilitation. Compression was started after a latent period of 7 days. In the fourth patient, the latent phase lasted only for 3 days. After completion of “dynamic” phase, patients were sent home with advice to follow-up every 6 weeks. Three of the nonunions were united at the second follow-up (12 weeks) and the fourth at third follow-up (18 weeks). Thus, the total duration of external fixator was 14 weeks in one patient, 15 weeks in two patients, and 21 weeks in the fourth patient. The fixators were removed after satisfactory stress test after loosening all connecting rods. Patellar tendon bearing cast was given for all cases for 6 weeks with the advice of full weight-bearing. Apart from limb swelling and blebs in one case, another patient had pin tract infection that was detected at first follow-up that needed a week of dressings and oral antibiotics. The infection settled uneventfully without any need of wire exchange. Two patients each had minimal residual deformity and shortening <1 cm, well within acceptable limits with potential to remodel. The intraoperative, post-operative, and follow-up characteristics of our patient cohort are summarized in Table 2 (Fig. 1, 2, 3, 4).
Table 2.
Intra-operative, post-operative, and follow-up characteristics of our patient cohort (also refer Fig. 1, 2, 3, 4)

Discussion
Tibia is the third most common long bone to fracture in children [3]. Nonunion is extremely rare with closed fractures [3]. With open fracture, its incidence increases to 7.5—.3% [4, 5, 6]. In all our patients, the diagnosis of hypertrophic nonunion was essentially radiological with a visible gap at the fracture site, abundant bone formation, and lack of clearly bridging trabeculae. All our patients had significant deformity at the fracture site with no abnormal mobility. All of them had apparent shortening due to deformity. However, radiological measurements revealed that there was no true shortening and it was expected that deformity correction would itself correct the apparent shortening. Distraction osteogenesis has been extensively reported as a successful treatment strategy of hypertrophic tibial nonunion in adults [1, 7, 8, 9], but reports in children are rare [2]. All these cases need meticulous post-operative correction of deformity and monitoring of regeneration that needs reasonable time in “dynamic” phase and frequent radiological examinations. Some reports have even used complex software-assisted deformity correction systems [2, 8, 10]. To the best of our knowledge, a strategy involving acute deformity correction and compression is not reported as a treatment strategy for hypertrophic nonunion, either in children or adults. Our strategy has the following merits. The technique is simple and reproducible and does not rely on meticulous assembly of manual or software-assisted Ilizarov systems. Complete deformity correction in all axes is achieved on the day of surgery or utmost within 1 week. A few millimeters of compression are all that are needed postoperatively. Both factors put together to make the “dynamic” phase of the fixator simple and short. Since below-knee frames are well tolerated by children, all children could be trained to walk full weight-bearing with support during this “dynamic” phase itself and were sent home during the “static” phase. All our patients could be sent home within 3 weeks, including the patients who had a repeat intervention. The total duration of fixator in our patients was 14—weeks. We agree that this could have been reduced by closer clinicoradiological follow-up. Still, we chose to follow up these patients once in 6 weeks since the very purpose of the strategy was to facilitate patients coming from long distances and all children were well adapted to the fixator in terms of activity and quality of life. There was no opportunity for us to evaluate these children in the interim period. A similar series of three children employing distraction osteogenesis reports the duration of external fixation varying from 9 to 29 weeks [2]. We acknowledge the following demerits. Acute deformity correction can potentially cause soft tissue complications, and this must be staged if required. Meticulous monitoring for soft tissue complications and modification of rehabilitation is needed in the first couple of weeks. This technique is not applicable for children who need concurrent correction of shortening. We are also unsure whether this strategy will work in adults.
Conclusion
We conclude that compression osteosynthesis is a simple, effective, and easily reproducible strategy in children with hypertrophic nonunion of the tibia without shortening. This keeps the “dynamic” phase of Ilizaov osteosynthesis short, facilitating early return to the home of patients who need to travel long distances for treatment.
Clinical Message.
Despite being versatile and effective, the major disadvantage of the Ilizarov method is prolonged treatment time and the need to follow-up the patients frequently when they are in the “dynamic” phase of treatment. This can be a problem for patients who travel for long distances to get treated from referral centers. Wherever applicable, strategies must be adopted to shorten the “dynamic” phase in such cases, which considerably reduces the socioeconomic burden on patients. We believe that the strategy of acute deformity correction and compression osteosynthesis satisfies this philosophy of treatment, in addition to making the technique simpler and more replicable.
Biography


Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
References
- 1.Catagni MA, Guerreschi F, Holman JA, Cattaneo R. Distraction osteogenesis in the treatment of stiff hypertrophic nonunions using the ilizarov apparatus. Clin Orthop Relat Res. 1994;301:159–63. [PubMed] [Google Scholar]
- 2.Gordon JE, Jani M, Dobbs M, Luhmann SJ, Szymanski DA, Schoenecker PL, et al. Treatment of rigid hypertrophic posttraumatic pseudarthrosis of the tibia in children using distraction osteogenesis. J Pediatr Orthop. 2002;22:419–23. [PubMed] [Google Scholar]
- 3.Shannak AO. Tibial fractures in children:Follow-up study. J Pediatr Orthop. 1988;8:306–10. doi: 10.1097/01241398-198805000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Grimard G, Naudie D, Laberge LC, Hamdy RC. Open fractures of the tibia in children. Clin Orthop Relat Res. 1996;332:62–70. doi: 10.1097/00003086-199611000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Hope PG, Cole WG. Open fractures of the tibia in children. J Bone Joint Surg Br. 1992;74:546–53. doi: 10.1302/0301-620X.74B4.1624514. [DOI] [PubMed] [Google Scholar]
- 6.Kreder HJ, Armstrong P. A review of open tibia fractures in children. J Pediatr Orthop. 1995;15:482–88. doi: 10.1097/01241398-199507000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Kocaoğlu M, Eralp L, Sen C, Cakmak M, Dincyürek H, Göksan SB, et al. Management of stiff hypertrophic nonunions by distraction osteogenesis:A report of 16 cases. J Orthop Trauma. 2003;17:543–8. doi: 10.1097/00005131-200309000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Ferreira N, Marais LC, Aldous C. Hexapod external fixator closed distraction in the management of stiff hypertrophic tibial nonunions. Bone Joint J. 2015;97:1417–22. doi: 10.1302/0301-620X.97B10.35504. [DOI] [PubMed] [Google Scholar]
- 9.Xu J, Jia YC, Kang QL, Chai YM. Management of hypertrophic nonunion with failure of internal fixation by distraction osteogenesis. Injury. 2015;46:2030–5. doi: 10.1016/j.injury.2015.06.020. [DOI] [PubMed] [Google Scholar]
- 10.Schoenleber SJ, Hutson JJ., Jr Treatment of hypertrophic distal tibia nonunion and early malunion with callus distraction. Foot Ankle Int. 2015;36:400–7. doi: 10.1177/1071100714558509. [DOI] [PubMed] [Google Scholar]