Abstract
Aims
To present a surgically relevant update of trunnionosis.
Materials and Methods
Systematic review performed April 2017.
Results
Trunnionosis accounts for approximately 2% of the revision total hip arthroplasty (THA) burden. Thinner (reduced flexural rigidity) and shorter trunnions (reduced contact area at the taper junction) may contribute to mechanically assisted corrosion, exacerbated by high offset implants. The contribution of large heads and mixed metallurgy is discussed.
Conclusion
Identifying causative risk factors is challenging due to the multifactorial nature of this problem.
Cite this article: Bone Joint J 2018;100-B(1 Supple A):44–9.
Keywords: Hip, Arthroplasty, Revision, Corrosion, Trunnionosis
Trunnionosis is a potential cause for revision in total hip arthroplasty (THA),1 however, this is not a new phenomenon. Corrosion at the head-neck junction was described in 19912 and a soft-tissue reaction around a metal-on-polyethylene (MoP) THA in 1988.3 Differential patterns of material loss at the head-neck junction may indicate several failure modes,4 and the co-existence of multiple modes of corrosion and wear has been demonstrated.5 These are now encompassed under the umbrella term of mechanically assisted crevice corrosion. This article serves as a critical review of the various contributing factors that have been proposed.6
Materials and Methods
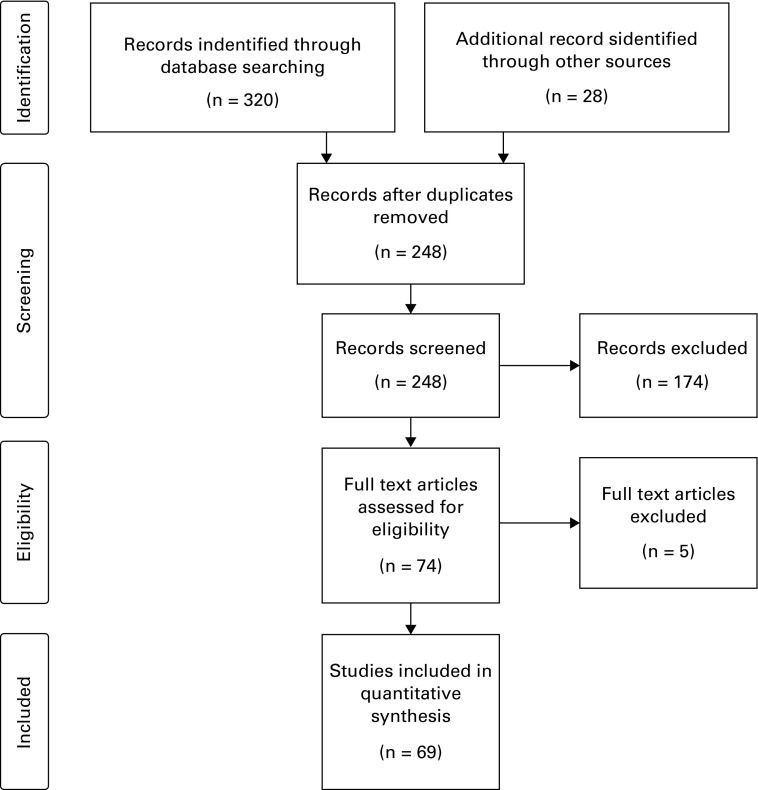
The search strategy for this systematic review is presented in Table I, and study flow described in Figure 1.
Fig. 1.
Study flow diagram: A total of 320 records were identified from searching the literature; two reviewers (JB and MW) independently screened the abstracts of these records to identify potentially relevant articles for inclusion in this review. After screening, 41 studies were included in this review and an additional 28 studies were identified via reference lists and other sources. There was no disagreement between reviewers.
Table I.
Keywords for the literature search
| Keywords | |
|---|---|
| 1 | Tru*nionosis |
| 2 | Tru*nion corrosion |
| 3 | Taperosis |
| 4 | Crevice corrosion |
| 5 | Fretting corrosion |
| 6 | Mechanically assisted crevice corrosion |
| 7 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 |
Search strategy: MEDLINE 1946 to 2017 Week 15, AMED (Allied and Complementary Medicine) 1985 to April 2017, CAB Abstracts 1973 to 2017 Week 14, Embase 1974 to 2017 Week 16. Searches were performed on 18 April 2017, using the keywords above appearing in any field. Searches were limited to studies published in the English language. We also searched the reference lists of articles identified by this search strategy and included additional studies deemed relevant
Results
Prevalence
A total of 12 revisions for adverse tissue reaction due to trunnion corrosion were reported in a consecutive series of 4813 non-metal-on-metal (MoM) THAs, a 0.25% prevalence for revision.7 National Joint Registry (NJR) data for England, Wales, Northern Ireland and the Isle of Man, shows a revision risk for adverse reactions to metal debris of 0.032% (249 of 789 397; 95% confidence interval (CI) 0.028 to 0.036%) in non-MoM THAs, compared with 3.7% in MoM THAs (p < 0.001).8 A consecutive series study of same-implant MoP THAs estimated a 1.1% prevalence of adverse local tissue reactions due to mechanically assisted crevice corrosion (based on symptoms, raised serum cobalt levels, cross sectional imaging and the absence of infection). These criteria correlated well with intra-operative findings.9
Revision for trunnionosis accounts for 1.8% to 3.3% of the total revision THA burden.7,10 Clinically relevant trunnionosis is reported in approximately 1%, not all of which results in revision. The proportion revised may rise in the future due to detection bias, and there is likely to be wide variation in unit prevalence due to differential use of implants and surgical technique.
Risk factors
Body mass index (BMI) > 30kg/m2 was identified in a five-patient series of head-stem dissociations secondary to trunnion corrosion.11 Laboratory studies have demonstrated increased micromotion (fretting wear) at the head-neck junction with increasing weight.12 Increased BMI may contribute to the problem but robust evidence is lacking.
Head/stem material couples
Due to galvanic corrosion with mixed metal combinations at the head-neck junction, cobalt-chrome/cobalt-chrome couples are less susceptible to corrosion than cobalt-chrome/titanium or stainless steel couples.13,14 Corrosion was observed in 28% of similar metal couples, compared with 42% in mixed couples.13
No difference in the rate of material loss at the head-neck junction was identified when head-stem combinations from the same manufacturer were compared with those from different manufacturers.15 No difference was observed in material loss when cobalt-chrome heads were used on cobalt-chrome or stainless steel stems.16
Laboratory studies of different implant designs with 12/14 tapers have shown a higher grade of corrosion and greater variation in debris particle size with a stainless steel/stainless steel couple compared with a stainless steel/titanium couple.17 Taper length, taper angle, neck-shaft angle and offset were not investigated. Of note, ‘12’ and ‘14’ refer only to the proximal and distal diameter of the trunnion. Trunnion length and cone angle are independent of these diameters, hence compatibility between manufacturers is not guaranteed by the designation ‘12/14’.
An association between titanium stems and increased fretting corrosion at the head-neck junction has been reported in a comparison of cobalt-chrome/cobalt-chrome, cobalt-chrome/titanium and ceramic/cobalt-chrome couples. The use of ceramic heads reduced but did not eliminate corrosion.18
Retrieval analysis has demonstrated lower mean corrosion scores with Oxidised Zirconium (Oxinium, Smith & Nephew, Memphis, Tennessee) heads compared with cobalt-chrome (1.9, sd 0.7 versus 2.5, sd 1.0; p < 0.001);19 corroborating the findings of other studies.20 Comparison of non-oxidised zirconia/cobalt-chrome and cobalt-chrome/cobalt-chrome couples also identified lower fretting corrosion;21 similar to a comparative retrieval study of alumina compared with cobalt-chromium heads,22 and a matched study comparing corrosion of retrieved stems associated with either a ceramic or cobalt-chromium head.23 Oxinium heads conferred no advantage over cobalt-chromium in a retrieval analysis of 16 matched stems (eight Oxinium heads, eight cobalt chrome heads).23
Increased corrosion is associated with lower flexural rigidity of the neck, typical of titanium stems with narrow diameter necks.13
Amalgamating heterogeneous data is difficult but it appears combining titanium stems and cobalt-chrome heads may predispose to trunnionosis.
Head diameter
Wear analysis of a series of 5/17 retrieved large diameter (> 40 mm) MoM THAs revealed increased wear at the head-neck junction, but normal wear at the articulating surface suggesting an association between large heads and trunnionosis.24 Finite element analysis of head-neck junctions demonstrated increased maximum stress on the trunnion as head diameter increased from 28 mm to 40 mm.25 Significantly higher corrosion scores were observed on the trunnion of revised stems with 36 mm when compared with 28 mm heads.26 Corrosion at the head taper is observed in almost all (99/110) large head (> 36 mm) MoM THRs, with similar wear at the head taper to the bearing surfaces.27 Matched (taper design, manufacturer, time in vivo and head length) analysis of 23 femoral heads of 32 mm diameter and 28 mm heads revealed greater corrosion scores for the 32 mm femoral heads.28 Analysis of NJR data showed a relative risk of adverse reaction to metal debris (ARMD) revision 2.8 times (95% CI 1.74 to 4.36) higher in 36 mm MoP bearings compared with 28 mm and 32 mm (p < 0.001).8
Other studies have refuted an association between trunnionosis and head size. Corrosion in the head taper was observed in 93% of 154 revised MoP THAs; however, no correlation between Goldberg score13 and head size was identified,29 corroborating the findings of similar retrieval studies.19,20
Currently evidence is conflicting for the association of head size with trunnion corrosion. Head size may play a role.
Head length and offset
In small case series, high offset and low neck-shaft angles were identified as a contributing factor.30 Higher total fretting scores are seen in high-offset stems when there is control for other variables.31 Trunnion corrosion scores seem to show a parabolic relationship with head offset, with lower scores for neutral offsets.19 This may be related to deviation away from the neutral point where femoral head centre and stem taper gage point coincide20 and decreased taper engagement area.31 Laboratory assessment of loading reveals rocking of the head on the trunnion for higher offset heads.14 Asymptomatic MoP THA patients have shown an association between increased femoral offset and elevated serum cobalt levels.32
A large retrieval comparison of two different stems with 12/14 tapers of different lengths found no discernible differences in corrosion scores in multivariate analyses controlled for head offset, implantation time, taper flexibility and patient weight.33
Reducing the contact area between the head and trunnion or increasing the lever arm is likely to lead to reduced stability and hence increased risk of mechanically assisted corrosion.
Taper geometry
The move towards shorter, thinner trunnions to allow compatibility with ceramic heads and to increase impingement free range of movement is a potential risk factor for trunnion corrosion.34,35 The 11/13 S-ROM taper (DePuy, Leeds, United Kingdom) in comparison with the 12/14 appears protective in MoP THA.36-38 It is suggested that shorter trunnions reduce contact areas, and sit completely within the head taper increasing edge loading and contact stress at the base. Thinner trunnions are associated with a reduced cross-sectional area contributing to micromotion and exacerbating fluid ingress. However, the thin 11/13 taper has been shown to have low flexural rigidity39 and to be associated with the greatest corrosion in comparison to other designs, seen maximally at the base of the trunnion, potentially due to a combination of fluid ingress and greater torque.40
In contrast, analysis of three taper types from 40 large MoM THA retrievals showed no correlation between taper design, corrosion score and volumetric wear.41 Greater fretting scores were associated with thicker tapers with longer contact lengths but implantation time, head offset and taper surface roughness were not accounted for. No correlation has been observed between taper angle clearance and visual fretting-corrosion scores in either ceramic or metal heads.42
The association between taper geometry and trunnion corrosion is inconclusive.
Assembly impact forces
A linear relationship between impaction force and disassembly force has been demonstrated.43,44 Improved contact between trunnion ridges and head taper (9% to 100%) has been shown as assembly force is increased from 500 N to 8000 N.45 Impaction forces of at least 4 kN are required to improve pull off strength and reduce micromotion, hence corrosion.46,47 Impaction onto a dry trunnion results in higher resistance to fretting.14,48
Other studies have shown no association between impaction force and fretting corrosion, although an angular mismatch between the head and neck assembly did increase fretting corrosion.12
Although a definitive association between assembly force and trunnionosis has not been established, it seems prudent to aim for higher head-neck stability using impaction forces between 4 kN and 8 kN with a dry taper junction and a well-centred head.
Investigations
Metal ion levels
A serum cobalt threshold of 1.6 ng/mL, in association with unexplained hip pain, stiffness or limping in non-septic MoP THA has been shown to be predictive of trunnion corrosion at revision.9 Intra-articular cobalt and chromium levels are significantly higher for trunnionosis cases when compared with patients undergoing revision for other causes, potentially contributing to observed soft tissue reactions.49 Differential elevation of serum cobalt over chromium levels and cobalt levels of > 1 ppb are associated with adverse local tissue reactions secondary to corrosion.50 The risk of pseudotumour formation increases with cobalt levels above 7 ppb, cut off levels for discussion with patients about the risk of revision of 5 ppb for cobalt and 2.5 ppb for chromium have been suggested in the context of hip resurfacing.51
There is not a precise level at which ion levels should precipitate revision surgery. The measurement of intra-articular cobalt and chromium levels may be a useful adjunct, as discussed by McGrory et al.49
Imaging
Adverse local tissue reactions associated with the presence of corrosion debris at the head-neck junction following MoP THA have been observed by multiple authors.3,10,52-57 Intra-operative findings form a spectrum ranging from mild macroscopic trunnion corrosion to aggressive pseuotumour formation. Histological analysis reveals features consistent with aseptic lymphocyte-dominated vasculitis-associated lesions (ALVAL). Metal artefact reduction sequence (MARS) MRI findings include muscle oedema, atrophy, tissue necrosis, marrow oedema, osteolysis, extracapsular fluid collections and synovitis.58 Capsular thickness > 3 mm, periprosthetic fluid and complex synovitis strongly correlated with soft tissue damage and trunnion damage. Hip arthroscopy has also been advanced as a possible adjunct for examining the head-neck junction prior to revision surgery if there is diagnostic uncertainty.59
Soft-tissue changes can be assessed using cross-sectional imaging which is an important part of investigation.
Treatment
The decision to avoid the morbidity associated with stem revision in a well-fixed stem with no macroscopic trunnion damage is appealing. Some authors suggest it is safe to revise a metal head to a new metal head in trunnion corrosion,60 however most recommend cleaning the trunnion and using a new ceramic head with a titanium taper sleeve10,61 particularly if the old trunnion is not compatible with the use of a modern ceramic.62 Although the mechanical properties at the head-neck junction are not impaired by placing a new cobalt-chrome head on a corroded cobalt-chrome trunnion, placing a new cobalt-chrome head on a corroded titanium trunnion is associated with a 73% increase in interface motion compared with a new cobalt-chrome/titanium interface.63
The majority of reported cases in which titanium sleeve adaptors have been used are for well-fixed uncemented titanium stems. There is less evidence regarding stainless steel or cobalt chrome stems. In vitro studies of non-corroded interfaces have shown only very minor differences in fretting corrosion when a ceramic head is used in conjunction with a titanium sleeve on stainless steel, cobalt chrome and titanium stems.64
For macroscopically intact trunnions, we recommend the use of a ceramic head in combination with a sleeve of complimentary metallurgy to the stem, if available. It should be noted that whilst ceramic heads decrease metal release caused by head-taper fretting and corrosion,18,22,23,65,66 a ceramic head does not eliminate the possibility of trunnion corrosion.67
In conclusion, the use of ceramic compared with metal heads in the primary setting significantly reduces the incidence of trunnionosis but there is an increase in implant costs. Ceramic heads may be economical on a societal scale.68 For patients < 85 years, ceramic-on-polyethylene is cost effective if the cost differential to MoP was $325 or less. At $600, ceramic is only cost effective for patients < 65 years.69 There is not enough evidence to suggest that Oxinium heads further reduce the risk of trunnionosis over ceramic.
Among non-MoM bearing hip replacements in the NJR, the risk of ARMD revision surgery by primary bearing surface was greatest for ceramic-on-ceramic 0.055% (75 of 135 267; 95% CI 0.044 to 0.070), and similar for both MoP 0.024% (125 of 526 951; 95% CI 0.020 to 0.02) and ceramic-on-polyethylene 0.023% (29 of 124 656; 95% CI 0.016 to 0.033).8
We currently recommend the use of ≤ 36 mm head sizes, the judicious use of ceramic heads, neutral offset wherever possible and an assembly force of 4 kN to 8 kN in dry conditions for the reduction of risk factors associated with trunnionosis.
Take home message:
- Trunnionosis currently accounts for approximately 2% of the revision THA burden
- Thinner, shorter trunnions may contribute to mechanically assisted corrosion and the observation of trunnionosis.
- Correct assembly with adequate force, ceramic heads of ≤ 36 mm diameter and the use of neutral head length and stem offset where possible may reduce the occurrence of trunnionosis.
References
- 1.Gee C, Poole W, Wilson D, Gibbs J, Stott P. Adverse reaction to metal debris in uncemented metal on polyethylene accolade-trident total hip replacement. Hip Int 2015;25:S13. [Google Scholar]
- 2.Collier JP, Surprenant VA, Jensen RE, Mayor MB. Corrosion at the interface of cobalt-alloy heads on titanium-alloy stems. Clin Orthop Relat Res 1991;271:305–312. [PubMed] [Google Scholar]
- 3.Svensson O, Mathiesen EB, Reinholt FP, Blomgren G. Formation of a fulminant soft-tissue pseudotumor after uncemented hip arthroplasty. A case report. J Bone Joint Surg [Am] 1988;70-A:1238–1242. [PubMed] [Google Scholar]
- 4.Hothi HS, Panagiotopoulos AC, Whittaker RK, et al. Damage patterns at the head-stem taper junction helps understand the mechanisms of material loss. J Arthroplasty 2017;32:291–295. [DOI] [PubMed] [Google Scholar]
- 5.Bryant MG, Buente D, Oladokun A, et al. Surface and subsurface changes as a result of tribocorrosion at the stem-neck interface of bi-modular prosthesis. Biotribology 2017;10:1–16. [Google Scholar]
- 6.Mistry JB, Chughtai M, Elmallah RK, et al. Trunnionosis in total hip arthroplasty: a review. J Orthop Traumatol 2016;17:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whitehouse MR, Endo M, Zachara S, et al. Adverse local tissue reactions in metal-on-polyethylene total hip arthroplasty due to trunnion corrosion: the risk of misdiagnosis. Bone Joint J 2015;97-B:1024–1030. [DOI] [PubMed] [Google Scholar]
- 8.Matharu GS, Pandit HG, Murray DW, Judge A. Adverse reactions to metal debris occur with all types of hip replacement not just metal-on-metal hips: a retreospective observational study of 3340 revisions for adverse reactions to metal debris from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. BMC Musculoskelet Disord 2016;17:495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGrory BJ, MacKenzie J, Babikian G. A high prevalence of corrosion at the head-neck taper with contemporary Zimmer non-cemented femoral hip components. J Arthroplasty 2015;30:1265–1268. [DOI] [PubMed] [Google Scholar]
- 10.Cooper HJ, Della Valle CJ, Berger RA, et al. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg [Am] 2012;94-A:1655–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsen Ko L, Chen AF, Deirmengian GK, Hozack WJ, Sharkey PF. Catastrophic Femoral Head-Stem Trunnion Dissociation Secondary to Corrosion. J Bone Joint Surg [Am] 2016;98-A:1400–1404. [DOI] [PubMed] [Google Scholar]
- 12.Donaldson FE, Coburn JC, Siegel KL. Total hip arthroplasty head-neck contact mechanics: a stochastic investigation of key parameters. J Biomech 2014;47:1634–1641. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg JR, Gilbert JL, Jacobs JJ, et al. A multicenter retrieval study of the taper interfaces of modular hip prostheses. Clin Orthop Relat Res 2002;401:149–161. [DOI] [PubMed] [Google Scholar]
- 14.Gilbert JL, Mehta M, Pinder B. Fretting crevice corrosion of stainless steel stem-CoCr femoral head connections: comparisons of materials, initial moisture, and offset length. J Biomed Mater Res B Appl Biomater 2009;88:162–173. [DOI] [PubMed] [Google Scholar]
- 15.Whittaker RK, Hothi HS, Meswania JM, et al. The effect of using components from different manufacturers on the rate of wear and corrosion of the head-stem taper junction of metal-on-metal hip arthroplasties. Bone Joint J 2016;98-B:917–924. [DOI] [PubMed] [Google Scholar]
- 16.Hothi HS, Berber R, Panagiotopoulos AC, et al. Clinical significance of corrosion of cemented femoral stems in metal-on-metal hips: a retrieval study. Int Orthop 2016;40:2247–2254. [DOI] [PubMed] [Google Scholar]
- 17.Dos Santos CT, Barbosa C, Monteiro MJ, et al. Characterization of the fretting corrosion behavior, surface and debris from head-taper interface of two different modular hip prostheses. J Mech Behav Biomed Mater 2016;62:71–82. [DOI] [PubMed] [Google Scholar]
- 18.Panagiotidou A, Meswania J, Osman K, et al. The effect of frictional torque and bending moment on corrosion at the taper interface: an in vitro study. Bone Joint J 2015;97-B:463–472. [DOI] [PubMed] [Google Scholar]
- 19.Aldinger P, Cartner J, Li C, Collins D. Femoral head taper corrosion assessment of a 19-year retrieval database. Hip Int 2015;25:S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cartner J, Aldinger P, Li C, Collins D. Characterization of Femoral Head Taper Corrosion Features Using a 22-Year Retrieval Database. HSS J 2017;13:35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hallab NJ, Messina C, Skipor A, Jacobs JJ. Differences in the fretting corrosion of metal-metal and ceramic-metal modular junctions of total hip replacements. J Orthop Res 2004;22:250–259. [DOI] [PubMed] [Google Scholar]
- 22.Kurtz SM, Kocagöz SB, Hanzlik JA, et al. Do ceramic femoral heads reduce taper fretting corrosion in hip arthroplasty? A retrieval study. Clin Orthop Relat Res 2013;471:3270–3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tan SC, Lau AC, Del Balso C, et al. Tribocorrosion: ceramic and oxidized zirconium vs cobalt-chromium heads in total hip arthroplasty. J Arthroplasty 2016;31:2064–2071. [DOI] [PubMed] [Google Scholar]
- 24.Bolland BJ, Culliford DJ, Langton DJ, et al. High failure rates with a large-diameter hybrid metal-on-metal total hip replacement: clinical, radiological and retrieval analysis. J Bone Joint Surg [Br] 2011;93-B:608–615. [DOI] [PubMed] [Google Scholar]
- 25.Lavernia CJ, Iacobelli DA, Villa JM, et al. Trunnion-head stresses in THA: are big heads trouble? J Arthroplasty 2015;30:1085–1088. [DOI] [PubMed] [Google Scholar]
- 26.Dyrkacz RM, Brandt JM, Ojo OA, Turgeon TR, Wyss UP. The influence of head size on corrosion and fretting behaviour at the head-neck interface of artificial hip joints. J Arthroplasty 2013;28:1036–1040. [DOI] [PubMed] [Google Scholar]
- 27.Matthies AK, Racasan R, Bills P, et al. Material loss at the taper junction of retrieved large head metal-on-metal total hip replacements. J Orthop Res 2013;31:1677–1685. [DOI] [PubMed] [Google Scholar]
- 28.Del Balso C, Teeter MG, Tan SC, Howard JL, Lanting BA. Trunnionosis: does head size affect fretting and corrosion in total hip arthroplasty? J Arthroplasty 2016;31:2332–2336. [DOI] [PubMed] [Google Scholar]
- 29.Triantafyllopoulos GK, Elpers ME, Burket JC, et al. Otto Aufranc Award: large heads do not increase damage at the head-neck taper of metal-on-polyethylene total hip arthroplasties. Clin Orthop Relat Res 2016;474:330–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Raju S, Chinnakkannu K, Puttaswamy MK, Phillips MJ. Trunnion Corrosion in Metal-on-Polyethylene Total Hip Arthroplasty: A Case Series. J Am Acad Orthop Surg 2017;25:133–139. [DOI] [PubMed] [Google Scholar]
- 31.Del Balso C, Teeter MG, Tan SC, Lanting BA, Howard JL. Taperosis: does head length affect fretting and corrosion in total hip arthroplasty? Bone Joint J 2015;97-B:911–916. [DOI] [PubMed] [Google Scholar]
- 32.Martin JR, Camp CL, Wyles CC, et al. Increased femoral head offset is associated with elevated metal Ions in asymptomatic patients with metal-on-polyethylene total hip arthroplasty. J Arthroplasty 2016;31:2814–2818. [DOI] [PubMed] [Google Scholar]
- 33.Higgs GB, MacDonald DW, Gilbert JL, Rimnac CM, Kurtz SM. ; Implant Research Center Writing Committee. Does taper size have an effect on taper damage in retrieved metal-on-polyethylene total hip devices? J Arthroplasty 2016;31(suppl):277–281. [DOI] [PubMed] [Google Scholar]
- 34.Langton DJ, Sidaginamale R, Lord JK, Nargol AV, Joyce TJ. Taper junction failure in large-diameter metal-on-metal bearings. Bone Joint Res 2012;1:56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hussenbocus S, Kosuge D, Solomon LB, Howie DW, Oskouei RH. Head-neck taper corrosion in hip arthroplasty. Biomed Res Int 2015;2015:758123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hothi HS, Kendoff D, Lausmann C, et al. Clinically insignificant trunnionosis in large-diameter metal-on-polyethylene total hip arthroplasty. Bone Joint Res 2017;6:52–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hothi HS, Eskelinen AP, Berber R, et al. Factors associated with trunnionosis in the metal-on-metal pinnacle hip. J Arthroplasty 2017;32:286–290. [DOI] [PubMed] [Google Scholar]
- 38.Brock TM, Sidaginamale R, Rushton S, et al. Shorter, rough trunnion surfaces are associated with higher taper wear rates than longer, smooth trunnion surfaces in a contemporary large head metal-on-metal total hip arthroplasty system. J Orthop Res 2015;33:1868–1874. [DOI] [PubMed] [Google Scholar]
- 39.Porter DA, Urban RM, Jacobs JJ, et al. Modern trunnions are more flexible: a mechanical analysis of THA taper designs. Clin Orthop Relat Res 2014;472:3963–3970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tan SC, Teeter MG, Del Balso C, Howard JL, Lanting BA. effect of taper design on trunnionosis in metal on polyethylene total hip arthroplasty. J Arthroplasty 2015;30:1269–1272. [DOI] [PubMed] [Google Scholar]
- 41.Nassif NA, Nawabi DH, Stoner K, et al. Taper design affects failure of large-head metal-on-metal total hip replacements. Clin Orthop Relat Res 2014;472:564–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kocagöz SB, Underwood RJ, Sivan S, et al. Does taper angle clearance influence fretting and corrosion damage at the head-stem interface? A matched cohort retrieval study. Semin Arthroplasty 2013;24:246–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pennock AT, Schmidt AH, Bourgeault CA. Morse-type tapers: factors that may influence taper strength during total hip arthroplasty. J Arthroplasty 2002;17:773–778. [DOI] [PubMed] [Google Scholar]
- 44.Nevelos J, Scholl L, Pierre D, et al. Influence of impaction force and support compliance on initial taper stability. Hip Int 2016;26:S28–SS9. [Google Scholar]
- 45.Witt F, Gührs J, Morlock MM, Bishop NE. Quantification of the contact area at the head-stem taper interface of modular hip prostheses. PLoS One 2015;10:0135517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rehmer A, Bishop NE, Morlock MM. Influence of assembly procedure and material combination on the strength of the taper connection at the head-neck junction of modular hip endoprostheses. Clin Biomech (Bristol, Avon) 2012;27:77–83. [DOI] [PubMed] [Google Scholar]
- 47.Panagiotidou A, Cobb T, Meswania J, et al. The effect of impact assembly on the interface deformation and fretting corrosion of modular hip tapers: an in vitro study. Hip Int 2015;25:S61. [DOI] [PubMed] [Google Scholar]
- 48.Mroczkowski ML, Hertzler JS, Humphrey SM, Johnson T, Blanchard CR. Effect of impact assembly on the fretting corrosion of modular hip tapers. J Orthop Res 2006;24:271–279. [DOI] [PubMed] [Google Scholar]
- 49.McGrory BJ, Payson AM, MacKenzie JA. Elevated intra-articular cobalt and chromium levels in Mechanically Assisted Crevice Corrosion in Metal-on-Polyethylene Total Hip Arthroplasty. J Arthroplasty 2017;32:1654–1658. [DOI] [PubMed] [Google Scholar]
- 50.Plummer DR, Berger RA, Paprosky WG, et al. Diagnosis and management of adverse local tissue reactions secondary to corrosion at the head-neck junction in patients with metal on polyethylene bearings. J Arthroplasty 2016;31:264–268. [DOI] [PubMed] [Google Scholar]
- 51.Carlson BC, Bryan AJ, Carrillo-Villamizar NT, Sierra RJ. The utility of metal Ion trends in predicting revision in metal-on-metal total hip arthroplasty. J Arthroplasty 2017;16. [DOI] [PubMed] [Google Scholar]
- 52.Lindgren JU, Brismar BH, Wikstrom AC. Adverse reaction to metal release from a modular metal-on-polyethylene hip prosthesis. J Bone Joint Surg [Br] 2011;93-B:1427–1430. [DOI] [PubMed] [Google Scholar]
- 53.Walsh AJ, Nikolaou VS, Antoniou J. Inflammatory pseudotumor complicating metal-on-highly cross-linked polyethylene total hip arthroplasty. J Arthroplasty 2012;27:324–325. [DOI] [PubMed] [Google Scholar]
- 54.54. Lash NJ, Whitehouse MR, Greidanus NV, et al. Delayed dislocation following metal-on-polyethylene arthroplasty of the hip due to 'silent' trunnion corrosion. Bone Joint J 2016;98-B:187–193. [DOI] [PubMed] [Google Scholar]
- 55.Gill IP, Webb J, Sloan K, Beaver RJ. Corrosion at the neck-stem junction as a cause of metal ion release and pseudotumour formation. Bone Joint J 2012;94:895–900. [DOI] [PubMed] [Google Scholar]
- 56.Hsu AR, Gross CE, Levine BR. Pseudotumor from modular neck corrosion after ceramic-on-polyethylene total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2012;41:422–426. [PubMed] [Google Scholar]
- 57.Stahnke JT, Sharpe KP. Pseudotumor formation in a metal-on-polyethylene total hip arthroplasty due to trunnionosis at the head-neck taper. Surg Technol Int 2015;27:245–250. [PubMed] [Google Scholar]
- 58.Sana M, Morozov P, Abrahams T, McGrory B, Farraher S. MRI findings of adverse local tissue reaction due to mechanically assisted crevice corrosion in total hip arthroplasty. Skeletal Radiol 2017;45:422. [Google Scholar]
- 59.Whitehouse MR, Duncan CP. Arthroscopy as a diagnostic tool for painful trunnion corrosion after hip arthroplasty. Knee Surg Sports Traumatol Arthrosc 2015;23:2601–2604. [DOI] [PubMed] [Google Scholar]
- 60.Goyal N, Ho H, Fricka KB, Engh CA Jr. Do you have to remove a corroded femoral stem? J Arthroplasty 2014;29(suppl):139–142. [DOI] [PubMed] [Google Scholar]
- 61.Cooper HJ. Diagnosis and treatment of adverse local tissue reactions at the head-neck junction. J Arthroplasty 2016;31:1381–1384. [DOI] [PubMed] [Google Scholar]
- 62.Leibiger T, McGrory BJ. Custom titanium sleeve for surgical treatment of mechanically assisted crevice corrosion in the well-fixed, noncontemporary stem in total hip arthroplasty. Arthroplast Today 2015;1:107–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Derasari A, Gold JE, Ismaily S, Noble PC, Incavo SJ. Will new metal heads restore mechanical integrity of corroded trunnions? J Arthroplasty 2017;32:1356–1359. [DOI] [PubMed] [Google Scholar]
- 64.Preuss R, Lars Haeussler K, Flohr M, Streicher RM. Fretting corrosion and trunnion wear-is it also a problem for sleeved ceramic heads? Semin Arthroplasty 2012;23:251–257. [Google Scholar]
- 65.Kocagoz SB, Underwood RJ, MacDonald DW, Gilbert JL, Kurtz SM. Ceramic heads decrease metal release caused by head-taper fretting and corrosion. Clin Orthop Relat Res 2016;474:985–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pandorf T, Kurtz S, Streicher R. Fretting and corrosion-what are the influencing factors? Hip Int 2016;26:S27–SS8. [Google Scholar]
- 67.Di Laura A, Whittaker R, Hothi H, et al. Does the use of a ceramic head eliminate the risk of trunnionosis? Hip Int 2015;25:S26. [Google Scholar]
- 68.Wyles CC, McArthur BA, Wagner ER, et al. Ceramic femoral heads for all patients? Am J Orthop 2016;45:E362–E3E6. [PubMed] [Google Scholar]
- 69.Carnes KJ, Odum SM, Troyer JL, Fehring TK. Cost analysis of ceramic heads in primary total hip arthroplasty. J Bone Joint Surg [Am] 2016;98-A:1794–1800. [DOI] [PubMed] [Google Scholar]