Abstract
Aims
The aims of this study were to compare the efficacy of two agents, aspirin and warfarin, for the prevention of venous thromboembolism (VTE) after simultaneous bilateral total knee arthroplasty (SBTKA), and to elucidate the risk of VTE conferred by this procedure compared with unilateral TKA (UTKA).
Patients and Methods
A retrospective, multi-institutional study was conducted on 18 951 patients, 3685 who underwent SBTKA and 15 266 who underwent UTKA, using aspirin or warfarin as VTE prophylaxis. Each patient was assigned an individualised baseline VTE risk score based on a system using the Nationwide Inpatient Sample. Symptomatic VTE, including pulmonary embolism (PE) and deep vein thrombosis (DVT), were identified in the first 90 days post-operatively. Statistical analyses were performed with logistic regression accounting for baseline VTE risk.
Results
The adjusted incidence of PE following SBTKA was 1.0% (95% confidence interval (CI) 0.86 to 1.2) with aspirin and 2.2% (95% CI 2.0 to 2.4) with warfarin. Similarly, the adjusted incidence of VTE following SBTKA was 1.6% (95% CI 1.1 to 2.3) with aspirin and 2.5% (95% CI 1.9 to 3.3) with warfarin. The risk of PE and VTE were reduced by 66% (odds ratio (OR) 0.44, 95% CI 0.25 to 0.78) and 38% (OR 0.62, 95% CI 0.38 to 1.0), respectively, using aspirin. In addition, the risk of PE was 204% higher for patients undergoing SBTKA relative to those undergoing UTKA. For each ten-point increase in baseline VTE risk, the risk of PE increased by 25.5% for patients undergoing SBTKA compared with 10.5% for those undergoing UTKA. Patients with a history of myocardial infarction or peripheral vascular disease had the greatest increase in risk from undergoing SBTKA instead of UTKA.
Conclusion
Aspirin is more effective than warfarin for the prevention of VTE following SBTKA, and serves as the more appropriate agent for VTE prophylaxis for patients in all risk categories. Furthermore, patients undergoing SBTKA are at a substantially increased risk of VTE, even more so for those with significant underlying risk factors. Patients should be informed about the risks associated with undergoing SBTKA.
Cite this article: Bone Joint J 2018;100-B(1 Supple A):68–75.
Keywords: Knee, Venous thromboembolism, Total Knee Arthroplasty, Bilateral, Aspirin
Up to one third of patients contemplating total knee arthroplasty (TKA) have been reported to have end-stage bilateral osteoarthritis.1 In this common scenario, patients and providers must choose between simultaneous bilateral TKA (SBTKA) or staged unilateral TKA (UTKA). SBTKA offers several clear benefits: a single admission and anaesthetic, lower costs and a quicker return of function.2,3 However, it has also been shown to be associated with greater morbidity than a unilateral procedure.4,5 Specifically, the risk of venous thromboembolism (VTE), including pulmonary embolism (PE) and deep vein thrombosis (DVT), is greater following SBTKA.6,7
While potent anticoagulants, such as warfarin, low molecular weight heparin (LMWH), direct thrombin inhibitors, and factor Xa inhibitors, among others, have been used for thrombophylaxis following TKA, aspirin has been endorsed by the American Academy of Orthopaedic Surgeons (AAOS) since 2009 and the American College of Chest Physicians (ACCP) since 2012.8,9 It was recently reported that aspirin was more effective than other agents for the prevention of VTE and had a favourable risk profile.10-12 However, there are no clear recommendations about the most appropriate method for thromboprophylaxis in high risk patients, such as those undergoing SBTKA.8,9
The purposes of this study were: (1) to compare the efficacy of aspirin (regular or low dose) and warfarin for the prevention of VTE following SBTKA, (2) to better understand the risk of VTE conferred by SBTKA compared with UTKA, and (3) to determine for whom an increased VTE risk with SBTKA may outweigh the benefits of this approach.
Patients and Methods
A retrospective, multi-institutional study was conducted on all patients who underwent primary SBTKA or UTKA performed by fellowship trained arthroplasty or sports surgeons, including CH, JP, and RR, at two large academic institutions between 2000 and 2017.
The patients were divided into four groups based on VTE prophylaxis, as determined by institutional electronic databases, and whether they had undergone SBTKA or UTKA: (1) unilateral aspirin, (2) bilateral aspirin, (3) unilateral warfarin, (4) bilateral warfarin. The following patients were excluded: those receiving VTE prophylaxis with an agent other than aspirin or warfarin such as LMWH, direct thrombin inhibitors, and factor Xa inhibitors among others; those receiving multiple pharmaceutical agents for prophylaxis, those for whom the details of chemoprophylaxis or medical comorbidities were not available and those who underwent revision TKA. We identified 18 951 patients, 3685 who underwent SBTKA and 15 266 who underwent UTKA, from the institutional databases who met the inclusion criteria.
During the 18 years of the study, both institutions changed from using warfarin to aspirin as the predominant method for VTE prophylaxis. Warfarin was routinely used until 2008 and aspirin had become the most frequently used agent by 2011 (Fig. 1). Decisions about VTE prophylaxis were made by individual surgeons and were not based on institutional standards. The dose of warfarin was titrated against an international normalised ratio (INR) target of between 1.5 and 2.0. Patients were not bridged prior to reaching a therapeutic INR. Aspirin was administered twice daily either as a regular dose (325 mg) or a low dose (81 mg). Prophylaxis with either warfarin or aspirin was continued for the first month post-operatively. A fast track rehabilitation program, in which patients were mobilised on the day of surgery with physiotherapy began in 2006, and resulted in a decrease in the mean length of stay. Also, tranexamic acid infusion was introduced in 2011. A tourniquet was used routinely for all procedures unless contraindicated.
Fig. 1.
Graph showing aspirin versus warfarin usage for thromboprophylaxis over time.
All patients with a definitive diagnosis of symptomatic VTE, including PE or DVT, within 90 days of surgery were identified from review of administrative and radiological databases, as well as records of patient-provider phone communications and dictations from clinical encounters.
Each patient was assigned a VTE risk score based on an individualised model of risk for arthroplasty developed from the National Inpatient Sample (NIS) database.13 A score, ranging from 0 to 980 points, assuming a maximum age of 100 years old, can be calculated for each patient based on the presence or absence of 26 key factors, which include demographics, comorbidities and the procedure to be performed (Table I). The value contributed by each factor had been previously established by regression analysis of > 1.7 million patients who underwent arthroplasty, with the most points allotted to factors with the most significant association with VTE. Given that all patients in this study had undergone TKA, the minimum baseline score was 43 points. Also, as a goal of this study was to improve the understanding of the risks associated with performing SBTKA, ‘bilateral joints’ (NIS point value 21 points) was omitted from the calculation of the NIS VTE risk score. Thus, scores in this study was limited to a range between 43 and 959 points. Patient demographics and comorbidities used for the calculation of baseline risk were identified based on data recorded in an electronic database pre-admission. This study had ethical approval from both institutional review boards.
Table I.
Point values for predictors of venous thromboembolism (VTE) from the National Inpatient Sample (NIS) VTE calculator of risk13
| Predictor | Point value* | Incidence in study population (%) |
|---|---|---|
| Anaemia | 16 | 17.9 |
| Congestive heart failure | 22 | 1.6 |
| Coagulation deficiency | 39 | 3.5 |
| Lymphoma | 30 | 0.3 |
| Fluid and electrolyte disorders | 45 | 8.1 |
| Metastatic cancer | 87 | 0.4 |
| Peripheral vascular disease | 10 | 3.7 |
| Nonmetastatic solid tumors | 16 | 3.5 |
| Weight loss | 46 | 1.3 |
| Chronic pulmonary heart disease | 61 | 0.7 |
| Blood transfusion | 32 | 0.6 |
| History of VTE | 30 | 2.6 |
| Myeloproliferative disorders | 38 | 0.5 |
| Hypercoagulable state | 100 | 0.2 |
| Myocardial infarction | 13 | 4.5 |
| Varicose veins | 28 | 4.5 |
| Fracture | 43 | 1.8 |
| Inflammatory bowel disease | 17 | 0.5 |
| Sepsis | 72 | 0.1 |
| Periprosthetic joint infection | 27 | 0.3 |
| Atrial fibrillation | 30 | 5.1 |
| Stroke | 78 | 1.0 |
| Apnea | 9 | 10.0 |
| Bilateral joints† | 21 | 19.4 |
| Not primary THA | 43 | 100.0 |
| Age (yrs)‡ | 0.267 × yrs over 40 | N/A |
*Point values of predictors are added to calculate an NIS VTE score for each patient †Bilateral joints omitted from NIS VTE score calculation in this study dz, disease; VTE, venous thromboembolism; ‡For this portion of the formula used to calculate a patient’s NIS Risk Score, every year of the patient’s age over 40 is multiplied by 0.267. For a 60-year-old patient, for example, this would be 0.267 × (60 - 40) = 5.34 THA, total hip arthroplasty; N/A, not applicable
Statistical analyses
Bivariate analyses were performed with an independent-samples t-test for normally distributed continuous variables or a non-parametric Mann-Whitney U test for continuous variables with skewed distributions. Bivariate analyses of categorical variables were performed with Fisher’s exact test. The primary analysis, a comparison of VTE prophylaxis with aspirin or warfarin for patients undergoing SBTKA, was performed using a logistic regression predicting PE and VTE and accounting for baseline VTE risk score. A secondary analysis was performed using logistic regression to determine the risk of VTE associated with SBTKA compared with UTKA after accounting for differences in baseline risk. Based on the logistic regression, the adjusted incidence of PE and VTE for each of the four patient groups was calculated assuming a median baseline VTE risk score for the entire study population (median NIS VTE score = 52.6 points). All analyses were performed using Statistical Package for the Social Sciences version 23 (IBM Corporation, Armonk, New York). Statistical significance was set at p < 0.05.
Results
Of the 3685 SBTKAs, 1528 patients (41.5%) received aspirin and 2157 (58.5%) received warfarin. While there was no statistically significant difference in age, those receiving warfarin had a slight but statistically significantly higher body mass index (BMI) (31.5 vs 30.4) and baseline VTE risk (50.7 vs 50.0) (Table II). The patients receiving aspirin had a higher proportion of men (46.3% vs 38.5%).
Table II.
Comparison of baseline patient demographics and venous thromboembolism (VTE) risk: simultaneous bilateral total knee arthroplasty patients based on method of VTE prophylaxis
| Variable | Bilateral TKA cohort | p-value | |
|---|---|---|---|
| Aspirin (n = 1528) | Warfarin (n = 2157) | ||
| Mean age, yrs (sd) | 63.1 (7.8) | 63.3 (8.8) | 0.54* |
| Male gender, n (%) | 708 (46.3) | 831 (38.5) | < 0.0001† |
| Mean BMI, kg/m2 (sd) | 30.4 (5.0) | 31.5 (5.9) | < 0.0001* |
| Median NIS VTE score‡ (IQR) | 50.0 (48.2 to 53.5) | 50.7 (48.32 to 61.9) | < 0.0001§ |
*independent-samples t-test †Fisher’s exact test ‡NIS VTE score excluding bilateral joint as a risk factor §Mann–Whitney U test TKA, total knee arthroplasty; BMI, body mass index, NIS, Nationwide Inpatient Sample; VTE, venous thromboembolism; IQR, interquartile range
The unadjusted incidence of PE was 1.05% (16/1528) (95% confidence interval (CI) 0.65 to 1.70) for patients who underwent SBTKA using aspirin and 2.32% (50/2157; 95% CI 1.76 to 3.05) for those using warfarin (Fig. 2a). Assuming a baseline VTE risk at the median for the study population, the adjusted incidence of PE was 1.0% (95% CI 0.86 to 1.2) with aspirin and 2.2% (95% CI 2.0 to 2.4) with warfarin. The risk of PE was significantly lower using aspirin after accounting for baseline VTE risk (relative risk (RR) 0.44; 95% CI 0.25 to 0.78; p = 0.005) (Table III).
Figs. 2a - 2b.
Unadjusted and adjusted incidence of venous thromboembolism by group: a) pulmonary embolism; b) combined venous thromboembolism. Adjusted based on logistic regression model assuming the median National Inpatient Sample venous thromboembolism risk score for the study population.
Table III.
Logistic regression model comparing method of venous thromboembolism prophylaxis in bilateral total knee arthroplasty
| Variable | PE model | p-value* | Combined VTE model | p-value* | ||
|---|---|---|---|---|---|---|
| Exp RR | 95% CI | Exp RR | 95% CI | |||
| Aspirin | 0.44 | 0.25 to 0.78 | 0.005 | 0.62 | 0.38 to 1.01 | 0.052 |
| NIS VTE score (per 10 points)† | 1.26 | 1.14 to 1.38 | < 0.0001 | 1.23 | 1.13 to 1.34 | < 0.0001 |
*p-values calculated using logistic regression †NIS VTE score excluding bilateral joint as a risk factor PE, pulmonary embolism; VTE, venous thromboembolism; Exp RR, exponential relative risk; CI, confidence interval; NIS, National Inpatient Sample
Similarly, the unadjusted incidence of combined VTE, including both PE and DVT, was 1.57% (24/1528; 95% CI 1.06 to 2.33) for those using aspirin and 2.50% (54/2157; 95% CI 1.92 to 3.25) for those using warfarin (Fig. 2). Assuming a baseline VTE risk at the median for the study population, the adjusted incidence of VTE was 1.5% (95% CI 1.3 to 1.7) with aspirin and 2.3% (95% CI 2.1 to 2.6) with warfarin. The relative risk for VTE with aspirin, 0.62 (95% CI 0.38 to 1.0) after accounting for baseline VTE risk, was nearly statistically significant (p = 0.052) (Table III).
Of the patients undergoing SBTKA using aspirin, 981 received a regular dose (325 mg) twice daily and 546 received a low dose (81 mg) twice daily. One patient was excluded from this sub-analysis, as the dose of aspirin was unavailable. The incidence of PE was 0.82% (8/981) using a regular dose compared with 1.47% (8/546) using a low dose. The difference in the risk of PE for those using a regular dose compared with a low dose (RR 0.54; 95% CI 0.20 to 1.5; p = 0.23) was not statistically significant after accounting for baseline VTE risk. The incidence of combined VTE was 1.22% (12/981) for those using a regular dose and 2.20% (12/546) for those using a low dose. Again, the difference in risk of VTE for those receiving a regular dose compared with a low dose (RR 0.55; 95% CI 0.24 to 1.2; p = 0.14) was not statistically significant after accounting for baseline VTE risk.
Of 15 266 unilateral knee arthroplasties, 6583 patients (43.1%) received aspirin and 8683 (56.9%) received warfarin. The cohort of patients who underwent SBTKA was younger, had a higher proportion of men, and a lower mean BMI than those who underwent UTKA (Table IV). Furthermore, those undergoing SBTKA had significantly lower mean baseline VTE risk scores. When considering only patients who received warfarin, the unadjusted incidences of PE and combined VTE were 2.32% and 2.50%, respectively, for those who underwent SBTKA and 1.42% and 1.61%, respectively, for those who underwent UTKA (Fig. 2). After accounting for differences in baseline VTE risk, the relative risk of PE and VTE for SBTKA compared with UTKA was 1.75 and 1.67, respectively (Table V). When considering only patients who received aspirin, the unadjusted incidences of PE and combined VTE were 1.05% and 1.57%, respectively, for those who underwent SBTKA and 0.41% and 0.70%, respectively, for those who underwent UTKA (Fig. 2). After accounting for differences in baseline VTE risk, the relative risk of PE and VTE for SBTKA compared with UTKA was 4.25 and 3.38, respectively (Table VI).
Table IV.
Comparison of baseline patient demographics and venous thromboembolism risk: simultaneous bilateral and unilateral total knee arthroplasty patients
| Variable | Aspirin prophylaxis cohort | p-value | Warfarin prophylaxis cohort | p-value | |||
|---|---|---|---|---|---|---|---|
| Bilateral (n = 1528) | Unilateral (n = 6583) | Bilateral (n = 2157) | Unilateral (n = 8683) | ||||
| Mean age, yrs (sd) | 63.1 (7.8) | 65.0 (10.3) | < 0.0001* | 63.3 (8.8) | 65.9 (10.6) | < 0.0001* | |
| Male gender, n (%) | 708 (46.3) | 2637 (40.1) | < 0.0001† | 831 (38.5) | 2984 (34.4) | < 0.0001† | |
| Mean BMI, kg/m2 (sd) | 32.3 (5.0) | 30.4 (6.8) | < 0.0001* | 31.5 (5.9) | 31.8 (6.7) | 0.02* | |
| Median NIS VTE score‡ (IQR) | 50.0 (48.2 to 53.5) | 66.2 (50.7 to 104.4) | < 0.0001§ | 50.7 (48.32 to 61.9) | 51.8 (48.9 to 62.7) | < 0.0001§ | |
*independent-samples t-test †Fisher’s exact test ‡NIS VTE score excluding bilateral joint as a risk factor §Mann–Whitney U test BMI, body mass index; NIS, Nationwide Inpatient Sample; VTE, venous thromboembolism
Table V.
Logistic regression comparing simultaneous bilateral and unilateral total knee arthroplasty: warfarin prophylaxis cohort
| Variable | PE model | p-value* | Combined VTE model | p-value* | ||
|---|---|---|---|---|---|---|
| Exp RR | 95% CI | Exp RR | 95% CI | |||
| Simultaneous bilateral TKA | 1.75 | 1.25 to 2.44 | 0.001 | 1.67 | 1.21 to 2.29 | 0.002 |
| NIS VTE score (per 10 points)† | 1.12 | 1.07 to 1.17 | < 0.0001 | 1.13 | 1.08 to 1.17 | < 0.0001 |
*p-values calculated using logistic regression †NIS VTE score excluding bilateral joint as a risk factor PE, pulmonary embolism; VTE, venous thromboembolism; Exp RR, exponential relative risk; CI, confidence interval; TKA, total knee arthroplasty; NIS, National Inpatient Sample
Table VI.
Logistic regression comparing simultaneous bilateral and unilateral total knee arthroplasty: aspirin prophylaxis cohort
| Variable | PE model | p-value* | Combined VTE model | p-value* | ||
|---|---|---|---|---|---|---|
| Exp RR | 95% CI | Exp RR | 95% CI | |||
| Simultaneous bilateral TKA | 4.26 | 2.13 to 8.52 | < 0.0001 | 3.38 | 1.96 to 5.84 | < 0.0001 |
| NIS VTE score (per 10 points)† | 1.12 | 1.06 to 1.16 | < 0.0001 | 1.09 | 1.05 to 1.14 | < 0.0001 |
*p-values calculated using logistic regression †NIS VTE score excluding bilateral joint as a risk factor PE, pulmonary embolism; VTE, venous thromboembolism; Exp RR, exponential relative risk; CI, confidence interval; TKA, total knee arthroplasty; NIS, National Inpatient Sample
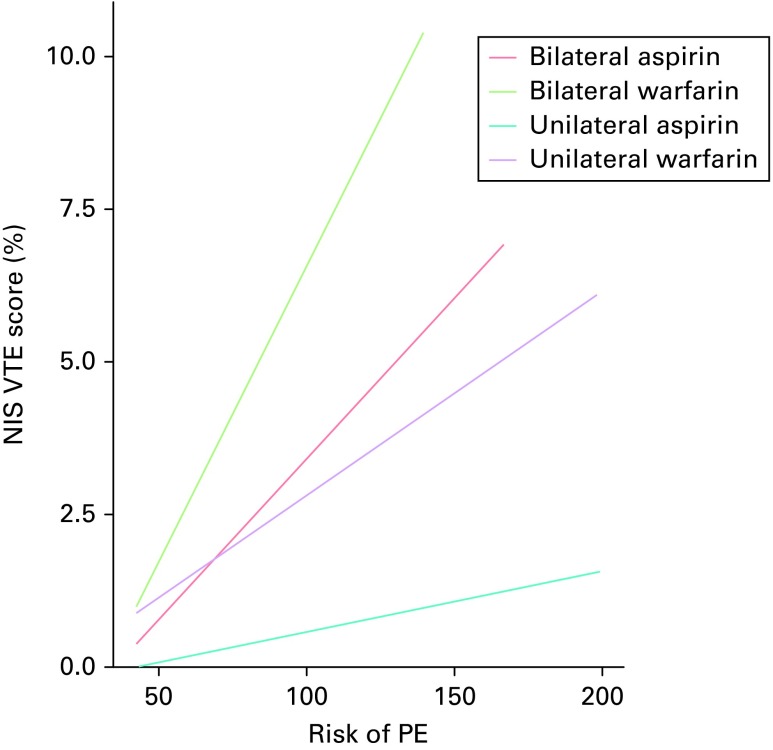
While the rate of PE and VTE was higher for those undergoing SBTKA even for those with the lowest possible baseline risk, the rate of increase in risk with an increasing NIS VTE score was considerably greater for simultaneous bilateral relative to UTKA. This is represented as an increased slope for both SBTKA groups in Figure 3. For every ten-point increase in NIS VTE score, the risk of PE increased by 25.5% for patients undergoing SBTKA compared with only 10.5% for those undergoing UTKA. The highest risk patients, defined as those in the top 20th percentile for NIS VTE score in the study population, had a 5.8% risk of PE after undergoing SBTKA compared with a risk of 1.5% after UTKA (RR 3.9; 95% CI 2.2 to 7.1) (Table VII). However, the lowest risk patients, defined as those in the bottom 20th percentile for NIS VTE score, had a risk of PE of 1.1% following SBTKA compared with 0.50% after UTKA (RR 2.2; 95% CI 1.0 to 4.9). As seen in Table VII, patients with a history of myocardial infarction (MI), peripheral vascular disease (PVD), or varicose veins had the greatest increase in risk when undergoing SBTKA compared with UTKA. While advanced age was clearly a risk factor for VTE, the relative increase in risk from undergoing SBTKA compared with UTKA (1.6 fold for patients aged > 70 years) was similar to the relative increase in the larger patient population (1.7-fold increase).
Figs. 3a - 3b.
Risk of venous thromboembolism (VTE) based on baseline VTE risk score: a) Risk of pulmonary embolism (PE); b) Risk of combined VTE. NIS, National Impatient Sample.
Table VII.
Relative venous thromboembolism risk ratio of bilateral total knee arthroplasty (TKA) relative to unilateral TKA by risk factor. Only comorbidities with a sample size > 10 for bilateral TKA were analysed
| Risk factor | Bilateral PE, n (%) | Unilateral PE, n (%) | PE RR (95% CI) | Bilateral VTE, n (%) | Unilateral VTE, n (%) | VTE RR (95% CI) |
|---|---|---|---|---|---|---|
| Reference* | 66/3685 (1.8) | 150/15 266 (1.0) | 1.8 (1.4 to 2.4) | 78/3685 (2.1) | 186/15 266 (1.2) | 1.7 (1.3 to 2.3) |
| Elderly (> 70 yrs) | 19/835 (2.3) | 75/5477 (1.4) | 1.7 (1.0 to 2.7) | 21/835 (2.5) | 89/5477 (1.6) | 1.6 (1.0 to 2.5) |
| High VTE risk† | 13/223 (5.8) | 53/3567 (1.5) | 3.9 (2.2 to 7.1) | 15/223 (6.7) | 72/3567 (2.0) | 3.3 (1.9 to 5.7) |
| Low VTE risk‡ | 11/994 (1.1) | 14/2820 (0.5) | 2.2 (1.0 to 4.9) | 17/994 (1.7) | 18/2820 (0.6) | 2.7 (1.4 to 5.2) |
| Anaemia | 15/455 (3.3) | 24/2943 (0.8) | 4.0 (2.1 to 7.6) | 17/455 (3.7) | 32/2943 (1.1) | 3.4 (1.9 to 6.1) |
| Varicose veins | 1/14 (7.1) | 8/837 (1.0) | 7.5 (1.0 to 56.0) | 1/14 (7.1) | 16/837 (1.9) | 3.7 (0.5 to 26.0) |
| History of MI | 4/55 (7.3) | 8/796 (1.0) | 7.2 (2.2 to 23.0) | 4/54 (7.4) | 14/796 (1.8) | 4.2 (1.4 to 12.0) |
| Sleep apnoea | 5/287 (1.7) | 19/1604 (1.2) | 1.5 (0.55 to 3.9) | 6/287 (2.1) | 25/1604 (1.6) | 1.3 (0.6 to 3.2) |
| Afib | 6/97 (6.2) | 22/860 (2.6) | 2.4 (1.0 to 5.8) | 6/97 (6.2) | 26/860 (3.0) | 2.1 (0.9 to 4.9) |
| COPD | 1/34 (2.9) | 1/98 (1.0) | 2.9 (0.2 to 45.0) | 1/34 (2.9) | 1/98 (1.0) | 2.9 (0.2 to 45.0) |
| History of VTE | 2/58 (3.5) | 7/437 (1.6) | 2.2 (0.5 to 10.0) | 3/58 (5.2) | 12/437 (2.8) | 1.9 (0.6 to 6.5) |
| PVD | 2/31 (6.5) | 9/669 (1.4) | 4.8 (1.1 to 21.0) | 2/31 (6.5) | 14/669 (2.1) | 3.1 (0.7 to 13.0) |
| Solid tumour | 1/95 (1.1) | 8/574 (1.4) | 0.76 (0.1 to 6.0) | 1/95 (1.1) | 10/574 (1.7) | 0.60 (0.1 to 4.7) |
*All study patients included as a baseline reference for risk of bilateral relative to unilateral TKA †High VTE risk is taken to be the top 20% of National Inpatient Sample VTE scores above 80.63 points ‡Low VTE risk is taken to be the bottom 20% of NIS VTE scores below 48.34 points PE, pulmonary embolism; Bilateral PE, risk of PE for simultaneous bilateral total knee arthroplasty (TKA); Unilateral PE, risk of PE for unilateral TKA; Bilateral VTE, risk of combined VTE for simultaneous bilateral TKA; Unilateral VTE, risk of combined VTE for unilateral TKA; RR, relative risk; CI, confidence interval; VTE, venous thromboembolism, MI, myocardial infarction; COPD, chronic obstructive pulmonary disease; PVD, peripheral vascular disease
Discussion
While there are clear advantages to undergoing SBTKA, there are inherent risks that may stem from the larger physiological insult of two knees being replaced at the same time. One such risk is VTE, which occurs at a higher rate after SBTKA than after UTKA.14 The impetus for this study was an observation at our institution that an increasing proportion of patients with post-operative PE had undergone SBTKA than had been seen previously. As aspirin has replaced warfarin as the preferred agent for thromboprophylaxis after arthroplasty, it seemed to be logical to examine the efficacy of aspirin compared with warfarin for patients undergoing SBTKA. Thus, the goal of this study was to assess the latter and to determine the group of patients for whom the risk of VTE with SBTKA was too high to justify this therapeutic approach.
The results clearly show that aspirin is more effective than warfarin for thromboprophylaxis in all patients undergoing TKA, including those undergoing SBTKA. For a patient undergoing this procedure with a median baseline risk, the risk of PE was 1.0% with aspirin and 2.2% with warfarin, a reduction with aspirin of 66%. Aspirin also reduced the risk for VTE (PE and DVT) by 38%, though this was not statistically significant. Our conclusion, the superiority of aspirin for SBTKA, is based solely on its efficacy for the prevention of VTE. While not specifically evaluated in this study, we also expect, as in previous studies, that aspirin may provide the secondary benefit of limiting wound complications and bleeding events.10,11
We believe that the reason for a higher rate of VTE with warfarin relates to its mechanism of action. Warfarin exerts its anti-thrombotic properties by inhibiting the production of factors in the clotting cascade.15,16 However, it also inhibits protein C and S, both of which have anti-thrombotic properties.15 Thus, warfarin is believed to act as a ‘pro-coagulant’ initially after administration. Such an effect was observed in ROCKET-AF, a crossover trial evaluating the use of rivaroxaban, a direct factor Xa inhibitor, compared with warfarin for patients with atrial fibrillation. Patients were found to have a high rate of VTE immediately after changing from rivaroxaban to warfarin.17
While aspirin is clearly the prophylactic agent of choice for SBTKA, a comparison of regular (325 mg) and low dose (81 mg) aspirin did not give a definitive conclusion. There was an apparent trend in favour of a reduced incidence of both PE and VTE using a regular dose compared with a low dose, although statistical significance was not achieved (p = 0.226). This is in contrast to a preliminary study on the dose of aspirin for thromboprophylaxis in primary arthroplasty from our institution, in which low dose aspirin was not inferior to regular dose aspirin, and also presented a reduced risk profile.18 It is important to remain cautious in drawing conclusions from the relatively small comparative sample aspirin dosing in this study. However, the impact of aspirin dosing on its efficacy for thromboprophylaxis should continue to be examined as further data become available.
The increased risk of PE associated with SBTKA is well known. In one large study using Medicare data, the adjusted risk of PE was 81% higher for patients undergoing SBTKA, suggesting that the risk of PE after SBTKA is less than the sum of risk for two UTKAs.14 In this study, the adjusted risk of PE was 75% higher for SBTKA patients who were using warfarin, mirroring the results of the previous study.14 However, while aspirin reduced the risk of PE for both simultaneous bilateral and UTKA compared with warfarin, the reduction in risk was much greater for patients undergoing a UTKA, as shown by the adjusted incidences of PE in Figure 2. As a result, the adjusted risk of PE was 426% higher for SBTKA patients using aspirin. Although PE would be less likely to occur in a median risk patient following SBTKA using aspirin (adjusted risk 1.0%) compared with UTKA using warfarin (adjusted risk 1.28%), the risk of PE would still be greater than the sum of two UTKAs using aspirin (adjusted risk 0.23%).
Although simple and convenient, the sum of risk approach is probably insufficient to allow conclusions to be drawn about the acceptable level of risk of PE for all patients making the decision to undergo SBTKA. While the risk of PE increased by only 10.5% for each ten point increase in NIS VTE score for those undergoing UTKA patients, a ten-point increase in baseline VTE risk resulted in a 25.5% increase in PE for those undergoing SBTKA. This implies a strong synergy between the characteristics of the patients that may predispose to thrombosis and SBTKA in promoting VTE. As such, the difference in risk between simultaneous bilateral and UTKA increased exponentially for those with risk factors.
The major, clinically relevant, question that remains is what degree of risk of VTE is acceptable in patients undergoing SBTKA? It is our belief that, in most instances, such a decision ultimately lies with the well-informed patient who can weigh the risks and benefits of undergoing this procedure. However, there may be certain patients with baseline VTE risk above a critical level, who should not be candidates for SBTKA. Provided a 0.84% incidence of PE for high-risk patients (top 20% of NIS VTE scores) after undergoing UTKA with aspirin, it would be reasonable to set the limit of acceptable risk at 2.5% (three-fold higher than for high-risk UTKA patients). This means SBTKA should not be considered for patients with a NIS VTE score > 80 points, which represents a single major (high point value) comorbidity or two minor (low point value) comorbidities in a typical patient aged > 60 years (Table I). Based on this recommendation, 43.9% (29/66) of patients undergoing SBTKA who developed a PE would no longer have been candidates for this procedure, which may have prevented the development of a PE. Similarly, patients with a risk for PE > 1.7% (NIS VTE score > 70 points), or twice that of high-risk patients undergoing UTKA, should be cautioned before proceeding with SBTKA. Finally, patients with specific high-risk comorbidities, such as a history of MI or PVD, should probably undergo staged UTKA.
This study has limitations. A major shortcoming was its retrospective nature. Because of this, institutional intra-operative guidelines were used for all patients and individual protocol deviations could not be assessed. Although we exhausted all resources to identify post-operative VTEs, including patient-nurse call logs that document all interactions between patients and nurses pre- and post-operatively, clinic dictations, and a radiographic database, it is possible that some VTEs may not have been properly recorded and could have been missed. Specifically, we believe that DVT may have been more underreported than PE, which is typically a critical event that would appear in the medical records. Furthermore, several changes in practice occurred during the 18 year study period, which may have contributed to the reduction in the risk of VTE with aspirin. Primarily, patients who underwent TKA prior to the beginning of the fast track program for early rehabilitation in 2006 would have received warfarin. However, patients in the latter years of the study received intra-operative intravenous tranexamic acid, which, interestingly, was not associated with an increase in the incidence of VTE. Additionally, agents other than aspirin or warfarin were not evaluated due to the lack of their routine use in the participating institutions. Finally, baseline risk of VTE, as calculated using the NIS VTE risk score, was validated as a predictor of VTE in the first 90 days post-operatively. However, this risk score was initially developed to predict in-hospital VTE and may not have been completely representative of our cohort.
In conclusion, aspirin is more effective than warfarin and serves as the most appropriate agent for thromboprophylaxis in all patients after TKA, including those undergoing SBTKA. While there are clear advantages to undergoing simultaneous bilateral procedures, there is also a substantial increase in the risk of VTE compared with UTKA. This is especially true for patients with predisposing comorbidities and other underlying risk factors for VTE. Patients should be informed about all the risks associated with undergoing SBTKA.
Take home message:
- Aspirin is a more effective chemoprophylactic agent than warfarin for the prevention of VTE and PE following simultaneous bilateral total knee arthroplasty
- A thorough medical risk assessment is necessary for all patients considering undergoing simultaneous bilateral total knee arthroplasty, and the increased risks associated with this procedure must be carefully explained to patients.
Footnotes
Supplementary material. Graphs showing incidence by institution and year are available alongside the online version of this article at www.bjj.boneandjoint.org.uk
References
- 1.Zhao YT, Chu HJ, Heng DF, Lei J. Comparison of the effectiveness and safety of one-stage versus two-stage bilateral total knee arthroplasty. Acta Orthop Belg 2015;81:784–789. [PubMed] [Google Scholar]
- 2.Odum SM, Troyer JL, Kelly MP, Dedini RD, Bozic KJ. A cost-utility analysis comparing the cost-effectiveness of simultaneous and staged bilateral total knee arthroplasty. J Bone Joint Surg [Am] 2013;95-A:1441–1449. [DOI] [PubMed] [Google Scholar]
- 3.Patil N, Wakankar H. Morbidity and mortality of simultaneous bilateral total knee arthroplasty. Orthopedics 2008;31:780–789. [DOI] [PubMed] [Google Scholar]
- 4.Hu J, Liu Y, Lv Z, et al. Mortality and morbidity associated with simultaneous bilateral or staged bilateral total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg 2011;131:1291–1298. [DOI] [PubMed] [Google Scholar]
- 5.Yeager AM, Ruel AV, Westrich GH. Are bilateral total joint arthroplasty patients at a higher risk of developing pulmonary embolism following total hip and knee surgery? J Arthroplasty 2014;29:900–902. [DOI] [PubMed] [Google Scholar]
- 6.Levy YD, Hardwick ME, Copp SN, Rosen AS, Colwell CW Jr. Thrombosis incidence in unilateral vs. simultaneous bilateral total knee arthroplasty with compression device prophylaxis. J Arthroplasty 2013;28:474–478. [DOI] [PubMed] [Google Scholar]
- 7.Stefánsdóttir A, Lidgren L, Robertsson O. Higher early mortality with simultaneous rather than staged bilateral TKAs: results from the Swedish Knee Arthroplasty Register. Clin Orthop Relat Res 2008;466:3066–3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012;141(suppl):278S–325S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johanson NA, Lachiewicz PF, Lieberman JR, et al. American academy of orthopaedic surgeons clinical practice guideline on. Prevention of symptomatic pulmonary embolism in patients undergoing total hip or knee arthroplasty. J Bone Joint Surg [Am] 2009;91-A:1756–1757. [DOI] [PubMed] [Google Scholar]
- 10.Raphael IJ, Tischler EH, Huang R, et al. Aspirin: an alternative for pulmonary embolism prophylaxis after arthroplasty? Clin Orthop Relat Res 2014;472:482–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilson DGG, Poole WEC, Chauhan SK, Rogers BA. Systematic review of aspirin for thromboprophylaxis in modern elective total hip and knee arthroplasty. Bone Joint J 2016;98-B:1056–1061. [DOI] [PubMed] [Google Scholar]
- 12.Haynes J, Barrack RL, Nam D. Mobile pump deep vein thrombosis prophylaxis: just say no to drugs. Bone Joint J 2016;98-B:341–348. [DOI] [PubMed] [Google Scholar]
- 13.Parvizi J, Huang R, Rezapoor M, Bagheri B, Maltenfort MG. Individualized risk model for venous thromboembolism after total joint arthroplasty. J Arthroplasty 2016;31(suppl):180–186. [DOI] [PubMed] [Google Scholar]
- 14.Barrett J, Baron JA, Losina E, et al. Bilateral total knee replacement: staging and pulmonary embolism. J Bone Joint Surg [Am] 2006;88-A:2146–2151. [DOI] [PubMed] [Google Scholar]
- 15.Hirsh J, Dalen J, Anderson DR, et al. Oral anticoagulants: mechanism of action, clinical effectiveness, and optimal therapeutic range. Chest 2001;119(suppl):8S–21S. [DOI] [PubMed] [Google Scholar]
- 16.Fasco MJ, Hildebrandt EF, Suttie JW. Evidence that warfarin anticoagulant action involves two distinct reductase activities. J Biol Chem 1982;257:11210–11212. [PubMed] [Google Scholar]
- 17.Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 2011;365:883–891. [DOI] [PubMed] [Google Scholar]
- 18.Parvizi J, Huang R, Restrepo C, et al. Low-dose aspirin is effective chemoprophylaxis against clinically important venous thromboembolism following total joint arthroplasty: a preliminary analysis. J Bone Joint Surg [Am] 2017;99-A:91–98. [DOI] [PubMed] [Google Scholar]