Abstract
Aims
The purpose of this study was to evaluate trends in opioid use after unicompartmental knee arthroplasty (UKA), to identify predictors of prolonged use and to compare the rates of opioid use after UKA, total knee arthroplasty (TKA) and total hip arthroplasty (THA).
Materials and Methods
We identified 4205 patients who had undergone UKA between 2007 and 2015 from the Humana Inc. administrative claims database. Post-operative opioid use for one year post-operatively was assessed using the rates of monthly repeat prescription. These were then compared between patients with and without a specific variable of interest and with those of patients who had undergone TKA and THA.
Results
A total of 4205 UKA patients were analysed. Of these, 1362 patients (32.4%) were users of opioids. Pre-operative opioid use was the strongest predictor of prolonged opioid use after UKA. Opioid users were 1.4 (81.6% versus 57.7%), 3.7 (49.5% versus 13.3%) and 5.5 (35.8% versus 6.5%) times more likely to be taking opioids at one, two and three months post-operatively, respectively (p < 0.05 for all). Younger age and specific comorbidities such as anxiety/depression, smoking, back pain and substance abuse were found to significantly increase the rate of repeat prescription for opioids after UKA. Overall, UKA patients required significantly less opioid prescriptions than patients who had undergone THA and TKA.
Conclusion
One-third of patients who undergo UKA are given opioids in the three months pre-operatively. Pre-operative opioid use is the best predictor of increased repeat prescriptions after UKA. However, other intrinsic patient characteristics are also predictive.
Cite this article: Bone Joint J 2018;100-B(1 Supple A):62–7.
Keywords: Opioid, Arthroplasty
Appropriate management of pain is an important consideration in the care of patients with orthopaedic conditions. Opioids have long been used for analgesia in the acute post-operative setting and in short courses for severe pain. Unfortunately usage has expanded exponentially beyond this and the United States is now in the midst of an epidemic of opioids.1,2 While judicious use of these medications can be beneficial, prolonged or inappropriate use has tremendous implications for both patients and society, in terms of healthcare expenditure, the criminal justice system and lost workplace productivity.3 In the United States, there was an exponential increase in the number of unintentional opioid-related deaths between 1999 and 2007. It now exceeds the number of deaths from heroin and cocaine combined.4
Orthopaedic surgeons are the third highest prescribers of opioids. A better understanding of trends in their use and the risk factors for prolonged use after surgery may guide prescribers to use them more appropriately.1 The American Academy of Orthopaedic Surgeons (AAOS), recognising the extent of the problem, released a statement about opioid use, abuse, and misuse in orthopaedics in 2015, which included practice recommendations for managing excessive or inappropriate use.5
As well as acknowledging the clear risks of these drugs, a growing body of evidence questions the benefits of opioids. Several studies have shown that their use is associated with higher morbidity and mortality and a worse clinical outcome in patients undergoing orthopaedic trauma surgery, spinal surgery, shoulder arthroplasty, total hip arthroplasty (THA), and total knee arthroplasty (TKA).6-12 Despite the known risks and questionable benefits of these drugs, little is known about the frequency of their use or which patients are at an increased risk of prolonged usage following surgery. This information is essential to monitor the effectiveness of interventions, to reduce opioid use and to identify patients who are at risk and who may benefit from additional interventions, such as pre-operative weaning from opioids, multimodal analgesic regimens, or the involvement of a pain specialist.
A recent study showed that the pre-operative use of opioids and the presence of underlying conditions, such as low back pain, anxiety or depression, myalgia and chemical dependence, resulted in significantly prolonged opioid use after TKA.13 However, opioid use after unicompartmental knee arthroplasty (UKA) has not been studied and it is not known whether these risk factors also apply to patients undergoing UKA.
The purpose of this study was firstly, to evaluate post-operative trends in the use of opioids after UKA; secondly, to determine if the previously established risk factors for increased opioid use after TKA were also predictive of prolonged opioid use after UKA, and thirdly, to compare the rates of post-operative opioid use after UKA, TKA, and THA.
Materials and Methods
The PearlDiver Research Program (PearlDiver Inc, Fort Wayne, Indiana) was used to question the Humana Inc. administrative claims database. The Humana Inc. database is a database of approximately 16 million patients’ insurance records and includes patients with private insurance or Medicare/Medicaid Advantage plans through Humana. We used the Current Procedural Terminology (CPT) code 27446 to identify patients who had undergone primary UKA between 2007 and the second quarter of 2015. All data within this database is compliant with the Health Insurance Portability and Accountability Act of 1996 (including the 2002 modifications to the Privacy Rule) and were thus exempt for institutional review board approval by our institution’s Human Subjects Office.
To evaluate post-operative trends in the use of opioids after UKA, we tracked the number of repeat monthly prescriptions for the whole of the first post-operative year. To ensure that results were not biased by patients joining and leaving the dataset, only patients who had been active with the insurance provider for three months before their UKA and for one year after were included in the analysis. All common oral and transdermal opioids were included. Prescriptions for tramadol were not included as the AAOS currently recommends this for the treatment of symptomatic osteoarthritis of the knee.13
A second aim of this study was to evaluate the impact of various pre-operative comorbidities on opioid use after UKA. Patient risk factors were analysed for their impact on post-operative rates of repeat opioid prescription, including a pre-operative diagnosis of low back pain (Internal Classification of Diseases (ICD), Ninth Revision (ICD-9), codes14 724.2 or 724.5), myalgia (ICD-9 729.1), anxiety or depression (ICD-9 296.2x, 296.3x and 300.02), drug dependence (ICD-9 304.xx), smoking (ICD-9 305.1), patient age at time of surgery (< 50 years versus ≥ 50 years), gender and pre-operative opioid use.
A pre-operative opioid user (OU) was defined as a patient who had been prescribed opioids in the three months prior to UKA. A non-opioid user (NOU) was defined as a patient with no history of opioid prescription prior to UKA. These definitions resulted in a group of patients who did not meet the definition of either OU or NOU (e.g. a patient who had been given a single opioid prescription one year prior to UKA). These patients were not included in the analysis when opioid user status was a variable of interest.
To compare post-operative opioid use after UKA with after TKA and THA, patients who underwent TKA and THA were identified in the same manner as UKA patients but using the CPT codes 27447 and 27130, respectively. This identified 37 393 THA patients and 73 959 TKA patients. This group of TKA patients have previously been involved in a study of trends and risk factors for prolonged opioid use after TKA.13 The percentage of repeat prescriptions for opioids were then compared at each monthly interval in the first post-operative year after UKA, TKA and THA for both OU and NOU.
Statistical analysis
Differences in the rate of repeat prescription for each type of arthroplasty and differences between UKA patients with and without comorbidities of interest were compared using risk ratios with 95% confidence intervals. Microsoft Excel (Microsoft Corporation, Redmond, Washington) was used for statistical analysis.
Results
A total of 4205 UKA patients were analysed: 2283 (54%) were women and 1922 (46%) were men. Of these, 1362 (32.4%) had been given a prescription for opioids at least three months before their UKA and were therefore classified as an OU. The 1733 patients (41.2%) with no history of opioid prescription prior to UKA were classified as a NOU.
There were 127 patients (3%) < 50 years of age at the time of UKA. The number of patients with a pre-operative diagnosis of interest were: 265 with anxiety or depression (6.3%), 1419 with low back pain (33.7%), 534 with myalgia (12.7%), 78 with drug abuse (1.8%) and 299 were smokers (7.1%).
The percentage of repeat opioid prescriptions after UKA fell from 50.2% in the first post-operative month to 21.5% and 14.2% in the second and third post-operative months. The percentage of patients being prescribed opioids continued to fall for the next three months and then plateaued at around 10% over the six to 12 month time interval (9.8% to 10.5%) (Table I).
Table I.
Trends in opioid use following joint arthroplasty amongst all patients regardless of opioid user status
| Total patients | TKA | THA | UKA | Risk ratio (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|
| mths | Patients (n) | % | Patients (n) | % | Patients (n) | % | TKA vs THA | TKA vs UKA | THA vs UKA |
| 73 959 | 100 | 37 393 | 100 | 4205 | 100 | ||||
| 1 | 51 279 | 69.3 | 22 580 | 60.4 | 2110 | 50.2 | 1.14 (1.13 to 1.16) | 1.38 (1.34 to 1.42) | 1.20 (1.17 to 1.24) |
| 2 | 28 230 | 38.2 | 9524 | 25.5 | 905 | 21.5 | 1.50 (1.47 to 1.53) | 1.77 (1.67 to 1.88) | 1.18 (1.11 to 1.26) |
| 3 | 18 451 | 24.9 | 6976 | 18.7 | 599 | 14.2 | 1.34 (130 to 1.37) | 1.75 (1.62 to 1.88) | 1.31 (1.21 to 1.41) |
| 4 | 14 780 | 20.0 | 6280 | 16.8 | 512 | 12.2 | 1.19 (1.16 to 1.22) | 1.64 (1.51 to 1.78) | 1.40 (1.27 to 1.50) |
| 5 | 13 106 | 17.7 | 5927 | 15.9 | 461 | 11.0 | 1.12 (1.09 to 1.15) | 1.62 (1.48 to 1.76) | 1.45 (1.32 to 1.58) |
| 6 | 12 070 | 16.3 | 5643 | 15.1 | 437 | 10.4 | 1.08 (1.05 to 1.11) | 1.57 (1.43 to 1.72) | 1.45 (1.32 to 1.59) |
| 7 | 11 614 | 15.7 | 5516 | 14.8 | 419 | 10.0 | 1.06 (1.03 to 1.10) | 1.57 (1.44 to 1.73) | 1.48 (1.35 to 1.53) |
| 8 | 11 380 | 15.4 | 5347 | 14.3 | 431 | 10.2 | 1.08 (1.04 to 1.11) | 1.50 (1.37 to 1.64) | 1.40 (1.27 to 1.53) |
| 9 | 10 995 | 14.9 | 5256 | 14.1 | 439 | 10.4 | 1.06 (1.03 to 1.09) | 1.42 (1.30 to 1.56) | 1.35 (1.23 to 1.48) |
| 10 | 10 780 | 14.6 | 5110 | 13.7 | 419 | 10.0 | 1.07 (1.03 to 1.10) | 1.46 (1.33 to 1.60) | 1.37 (1.25 to 1.51) |
| 11 | 10 750 | 14.5 | 5204 | 13.9 | 441 | 10.5 | 1.04 (1.01 to 1.08) | 1.39 (1.27 to 1.52) | 1.33 (1.21 to 1.45) |
| 12 | 10 825 | 14.6 | 5139 | 13.7 | 414 | 9.8 | 1.06 (1.03 to 1.10) | 1.48 (1.35 to 1.63) | 1.40 (1.27 to 1.53) |
TKA, total knee arthroplasty; THA, total hip arthroplasty; UKA, unicompartmental knee arthroplasty; CI, confidence interval
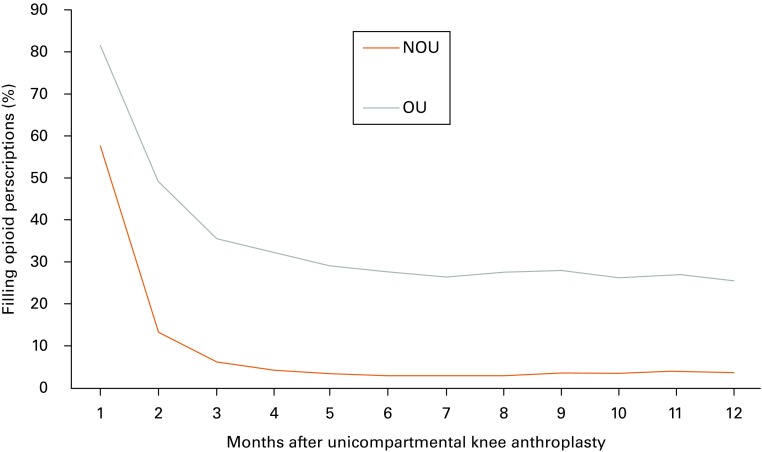
For both OU and NOU, the number of patients who had repeat prescriptions after UKA followed a downward trend with time (Fig. 1). However, the percentage of OU who had repeat prescriptions was significantly higher than that of NOU at every monthly interval for the whole post-operative year (Table II). Additionally, the percentage of patients with a repeat prescription for opioids who had a pre-operative diagnosis of low back pain, drug dependence, anxiety or depression, or myalgia was significantly higher at every time point compared with patients without those diagnoses (Table III). After the first post-operative month, smokers were also significantly more likely to have a repeat opioid prescription at every other interval analysed (Table III) as were patients < 50 years old at all time points except the 12th post-operative month (Table III).
Fig. 1.
Opioid use after uni-compartmental knee arthroplasty (NOU, non-opioid user; OU, opioid user).
Table II.
Opioid user (OU) versus non-opioid user (NOU) filling opioid prescriptions following UKA
| UKA | OU | NOU | OU vs NOU | |||
|---|---|---|---|---|---|---|
| mths | Patients filling opioid Rx | % | Patients filling opioid Rx | % | Risk ratio | 95% Confidence interval |
| 1 | 1111 | 81.57 | 999 | 57.65 | 1.42 | 1.35 to 1.48 |
| 2 | 674 | 49.49 | 231 | 13.33 | 3.71 | 3.26 to 4.23 |
| 3 | 487 | 35.76 | 112 | 6.46 | 5.53 | 4.56 to 6.71 |
| 4 | 434 | 31.86 | 78 | 4.50 | 7.08 | 5.62 to 8.91 |
| 5 | 397 | 29.15 | 64 | 3.69 | 7.89 | 6.12 to 10.18 |
| 6 | 382 | 28.05 | 55 | 3.17 | 8.84 | 6.72 to 11.62 |
| 7 | 363 | 26.65 | 56 | 3.23 | 8.25 | 6.28 to 10.83 |
| 8 | 375 | 27.53 | 56 | 3.23 | 8.52 | 6.49 to 11.18 |
| 9 | 380 | 27.90 | 59 | 3.40 | 8.20 | 6.29 to 10.68 |
| 10 | 359 | 26.36 | 60 | 3.46 | 7.61 | 5.85 to 9.91 |
| 11 | 369 | 27.09 | 72 | 4.15 | 6.52 | 5.12 to 8.31 |
| 12 | 349 | 25.62 | 65 | 3.75 | 6.83 | 5.29 to 8.82 |
CI, confidence interval; Rx, prescription; UKA, unicompartmental knee arthroplasty
Table III.
Risk factors for increased use of opioids following UKA
| UKA (mths) | Female vs male | Age < 50 yrs vs ≥ 50 yrs | Anxiety/depression vs none | Low back pain vs none | Myalgia vs none | Drug dependence vs none | Smoker vs none |
|---|---|---|---|---|---|---|---|
| 1 | 1.02 (0.9 to 1.1)* | 1.2 (1.2 to 1.3) | 1.1 (1.1 to 1.2) | 1.1 (1.01 to 1.1) | 1.01 (1.01 to 1.11) | 1.2 (1.1 to 1.3) | 1.02 (0.9 to 1.1)* |
| 2 | 1.3 (1.1 to 1.4) | 1.8 (1.5 to 2.2) | 1.6 (1.4 to 1.9) | 1.4 (1.3 to 1.6) | 1.4 (1.2 to 1.6) | 2.2 (1.9 to 2.7) | 1.6 (1.4 to 1.9) |
| 3 | 1.2 (1.01 to 1.3) | 2.2 (1.7 to 2.8) | 1.9 (1.5 to 2.3) | 1.8 (1.6 to 2.1) | 1.5 (1.2 to 1.7) | 3.0 (2.4 to 3.8) | 1.9 (1.6 to 2.3) |
| 4 | 1.1 (0.9 to 1.3)* | 2.0 (1.5 to 2.7) | 2.2 (1.8 to 2.7) | 1.9 (1.6 to 2.2) | 1.7 (1.5 to 2.1) | 3.5 (2.8 to 4.5) | 2.0 (1.7 to 2.5) |
| 5 | 1.1 (0.9 to 1.3)* | 2.0 (1.5 to 2.7) | 2.3 (1.9 to 2.9) | 2.0 (1.7 to 2.4) | 1.9 (1.6 to 2.3) | 3.7 (2.9 to 4.9) | 2.1 (1.7 to 2.6) |
| 6 | 1.3 (1.1 to 1.5) | 2.0 (1.4 to 2.7) | 2.4 (1.9 to 3.0) | 2.2 (1.9 to 2.6) | 2.2 (1.8 to 2.6) | 3.6 (2.7 to 4.7) | 2.3 (1.8 to 2.8) |
| 7 | 1.2 (1.02 to 1.4) | 2.1 (1.5 to 2.9) | 2.3 (1.8 to 2.9) | 2.4 (2.0 to 2.8) | 2.1 (1.8 to 2.6) | 4.8 (3.8 to 6.1) | 2.4 (2.0 to 3.0) |
| 8 | 1.2 (1.03 to 1.4) | 1.7 (1.2 to 2.4) | 2.3 (1.8 to 2.9) | 2.4 (2.0 to 2.8) | 1.9 (1.6 to 2.3) | 4.4 (3.4 to 5.6) | 2.5 (2.0 to 3.0) |
| 9 | 1.2 (1.03 to 1.5) | 1.6 (1.1 to 2.3) | 2.3 (1.8 to 2.9) | 2.4 (2.1 to 2.9) | 2.0 (1.7 to 2.4) | 3.8 (2.9 to 5.0) | 2.0 (1.6 to 2.5) |
| 10 | 1.2 (1.04 to 1.5) | 1.7 (1.2 to 2.4) | 2.6 (2.1 to 3.3) | 2.4 (2.0 to 2.8) | 1.9 (1.6 to 2.3) | 4.5 (3.5 to 5.8) | 2.5 (2.0 to 3.1) |
| 11 | 1.1 (0.9 to 1.3)* | 2.0 (1.4 to 2.8) | 2.5 (2.1 to 3.2) | 2.3 (1.9 to 2.7) | 2.1 (1.8 to 2.5) | 3.7 (2.9 to 4.9) | 2.3 (1.9 to 2.9) |
| 12 | 1.2 (0.9 to 1.4)* | 1.4 (0.9 to 2.2)* | 2.3 (1.8 to 2.9) | 2.5 (2.1 to 2.9) | 2.3 (2.0 to 2.8) | 4.0 (3.0 to 5.2) | 2.3 (1.8 to 2.8) |
Data presented as risk ratios (95% confidence interval) *95% confidence interval crosses one, thus risk ratio is not significant UKA, unicompartmental knee arthroplasty
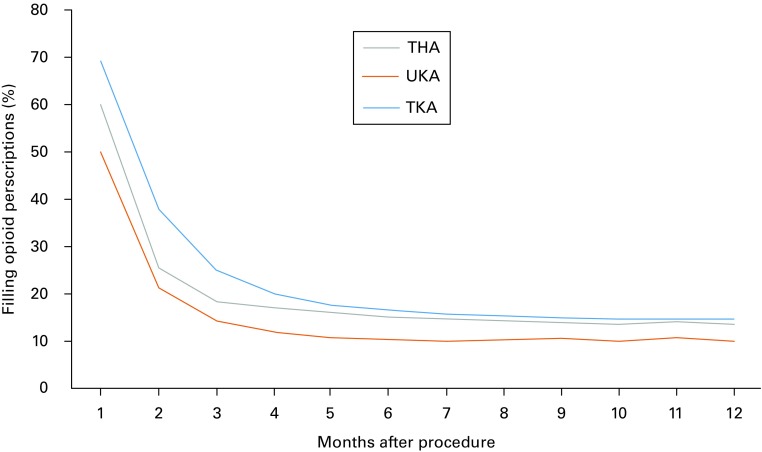
A smaller percentage of UKA patients had a repeat prescription at every monthly interval for the entire year post-operatively compared with patients who had undergone either primary TKA or THA (Table I). The decrease in repeat prescriptions over the first post-operative year was similar in each group (Fig. 2). Among NOU, a higher percentage of TKA patients had a repeat opioid prescription each month for the first ten months post-operatively than UKA patients (Table IV). Similarly, NOU THA patients also had a significantly higher percentage of repeat prescriptions during the first three months post-operatively compared with NOU UKA patients (Table IV). However, there were no significant differences in the rate of prescribing over the four to 12-month period.
Fig. 2.
Graph showing use of opioids after total joint arthroplasty (THA, total hip arthroplasty; UKA, unicompartmental knee arthroplasty; TKA, total knee arthroplasty).
Table IV.
Trends in opioid use following joint arthroplasty amongst non-opioid users
| Total patients | TKA | THA | UKA | Risk Ratio (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|
| (mths) | Patients | % | Patients | % | Patients | % | TKA vs THA | UKA vs TKA | UKA vs THA |
| 29 901 | 100 | 15 093 | 100 | 1733 | 100 | ||||
| 1 | 15 544 | 52.2 | 6646 | 44.0 | 999 | 57.6 | 1.18 (1.16 to 1.21) | 1.11 (1.06 to 1.15) | 1.31 (1.25 to 1.37) |
| 2 | 6321 | 21.2 | 1426 | 9.4 | 231 | 13.3 | 2.24 (2.13 to 2.37) | 0.63 (0.56 to 0.71) | 1.41 (1.24 to 1.61) |
| 3 | 3046 | 10.2 | 730 | 4.8 | 112 | 6.5 | 2.11 (1.95 to 2.29) | 0.63 (0.53 to 0.76) | 1.34 (1.10 to 1.62) |
| 4 | 1882 | 6.3 | 561 | 3.7 | 78 | 4.5 | 1.69 (1.55 to 1.86) | 0.71 (0.57 to 0.89) | 1.21* (0.96 to 1.53) |
| 5 | 1410 | 4.7 | 477 | 3.2 | 64 | 3.7 | 1.50 (1.35 to 1.66) | 0.78 (0.61 to 0.99) | 1.17* (0.96 to 1.51) |
| 6 | 1191 | 4.0 | 460 | 3.0 | 55 | 3.2 | 1.31 (1.18 to 1.46) | 0.79* (0.61 to 1.03) | 1.04* (0.80 to 1.37) |
| 7 | 1101 | 3.7 | 460 | 3.0 | 56 | 3.2 | 1.21 (1.09 to 1.35) | 0.87* (0.67 to 1.14) | 1.06* (0.81 to 1.39) |
| 8 | 1012 | 3.4 | 420 | 2.8 | 56 | 3.2 | 1.22 (1.09 to 1.37) | 0.95* (0.73 to 1.24) | 1.16* (0.89 to 1.56) |
| 9 | 951 | 3.2 | 430 | 2.8 | 59 | 3.4 | 1.12 (1.01 to 1.25) | 1.07* (0.82 to 1.38) | 1.19* (0.91 to 1.56) |
| 10 | 942 | 3.2 | 419 | 2.8 | 60 | 3.5 | 1.14 (1.02 to 1.28) | 1.09* (0.84 to 1.42) | 1.25* (0.96 to 1.63) |
| 11 | 935 | 3.1 | 432 | 2.9 | 72 | 4.2 | 1.10* (0.98 to 1.23) | 1.32 (1.05 to 1.67) | 1.45 (1.14 to 1.85) |
| 12 | 969 | 3.3 | 440 | 2.9 | 65 | 3.8 | 1.11* (0.99 to 1.25) | 1.15* (0.90 to 1.48) | 1.29* (0.99 to 1.66) |
Data presented as risk ratios (95% confidence interval) *95% confidence interval crosses 1, thus risk ratio is not significant UKA, unicompartmental knee arthroplasty; THA, total hip arthroplasty; TKA, total knee arthroplasty
Discussion
In this study, we could evaluate post-operative opioid use after UKA. A significant number of patients initially received a prescription for opioids post-operatively but this decreased over the following three months (Fig. 1). Pre-operative opioid use was the best predictor of repeat prescription of opioids after UKA. However, other patient demographics and comorbidities also predicted a higher risk of opioid refills post-operatively.
Opioid users were significantly more likely to continue with opioid pain medication in the year after UKA compared with NOU. Table II shows that the risk appears to increase rapidly in the first few post-operative months, peaks at six months, then decreases slightly. Approximately 25% of pre-operative OU were still having opioids prescribed 12 months after UKA. This is in stark contrast to NOU, where < 4% of patients were doing so. Given that over one-third of UKA patients were prescribed opioids pre-operatively, a significant number of patients are at risk of prolonged opioid use based on pre-operative opioid status alone. This is also of concern given the increasing number of reports which show that patients who use opioids for a long period pre-operatively are at substantially greater risk of complications and a more painful recovery after TKA.8 Although the impact of pre-operative opioid use on outcome after UKA has not been well studied, we suspect that the association also applies to UKA.
A study using the French Health Insurance System Database and similar methodology analysed the use of analgesic drugs before and after both UKA and TKA.15 Unlike the present study, only 9.3% of all patients were prescribed an opioid at some point during the years pre- and post-operatively. Additionally, only 4.4% of patients were prescribed opioids pre-operatively and 6.6% during the post-operative year.15 This difference is likely to reflect the current epidemic over prescription of opioids in the United States. Physicians in the United States may be able to learn more effective pain management strategies from our colleagues around the world and thereby reduce unnecessary opioid prescribing.
We found associations between prolonged opioid use and concurrent diagnoses of depression or anxiety, low back pain, drug dependence, smoking and age < 50 years old for all or most of the study period. Female gender was also associated with prolonged use, but only at post-operative months two, three and six to ten. These findings are consistent with those of a similar study which evaluated opioid use after TKA.13 The magnitudes of the risk ratios associated with each of these comorbidities, except age, were similar between the two studies.8,13 Having reproduced these findings in UKA patients strengthens the validity of the association. Age was less strongly associated with prolonged opioid use after UKA (risk ratio range: 1.2 to 2.2) than after TKA (risk ratio range: 1.3 to 2.7). This may be a result of differences between patients who are offered UKA rather than TKA. These findings are also consistent with a recent study which showed greater difficulty with post-operative pain control and increased opioid usage in patients with fibromyalgia who had undergone TKA and THA.16
The highest incidence of opioid use and highest risk ratio throughout the study period was found in TKA patients, followed by THA patients (Table I). Patients who underwent TKA and THA had a significantly higher percentage of patients receiving repeat prescriptions at every time point than those undergoing UKA. All groups showed a rapid decrease in opioid prescription in the three months post-operatively, followed by a plateau over the next nine months (Fig. 2).
Limitations to this study include the reliance on accurate coding and documentation, the inability to measure the size of opioid prescriptions and to determine whether patients were taking the medication as prescribed. These limitations are inherent to research using administrative claims databases. Additionally, patients who have not had a history of opioid prescription may have received a prescription for opioids pre-operatively, in anticipation of post-operative pain and could have been considered OU, rather than NOU. However, there was a clear difference in the usage patterns of opioids post-operatively between the two groups: incorrectly classifying NOUs as OUs would decrease the magnitude of the observed effect. Limitations also include the inability to carry out a multivariate analysis or to follow individual patients throughout the study period to evaluate the impact of opioid use on post-operative outcome.
In conclusion, this study identifies several risk factors for prolonged opioid use after UKA, including the diagnoses of anxiety or depression, low back pain, myalgia, drug dependence, smoking, and pre-operative opioid use. Several of these factors have been previously reported for THA and TKA.8,12,16 It is essential that providers exercise caution when considering prescribing opioids for osteoarthritis of the hip or knee. Not only do clinical practice guidelines and systematic reviews fail to show a clear benefit, it is also becoming clear that patients are at risk of a worse clinical outcome and long-term opioid use post-operatively.5,17 Inappropriately prescribing opioids in this setting contributes to the United States opioid epidemic and exposes our patients to unnecessary risk.
Take home message:
- In patients undergoing UKA, pre-operative opioid use is the strongest predictor of prolonged post-operative opioid use.
- Smoking, drug use, and younger age were also associated with high rates of post-operative opioid use.
- Despite these findings, patients undergoing UKA had lower overall opioid usage as compared with those undergoing TKA/THA.
References
- 1.Manchikanti L, Singh A. Therapeutic opioids: A ten-year perspective on the complexities and complications of the escaliating use, abuse, and nonmedical use of opioids. Pain Physician 2008;11:S63–S69. [PubMed] [Google Scholar]
- 2.Helmerhorst GTT, Teunis T, Janssen SJ, Ring D. An epidemic of the use, misuse and overdose of opioids and deaths due to overdose, in the United States and Canada: is Europe next? Bone Joint J 2017;99-B:856–864. [DOI] [PubMed] [Google Scholar]
- 3.Birnbaum HG, White AG, Schiller M, et al. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med 2011;12:657–667. [DOI] [PubMed] [Google Scholar]
- 4.Okie S. A flood of opioids, a rising tide of deaths. N Engl J Med 2010;363:1981–1985. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Orthopaedic Surgeons. Opioid use, misuse, and abuse in orthopaedic practice, AAOS Information Statement. https://www.aaos.org/uploadedFiles/PreProduction/About/Opinion_Statements/advistmt/1045%20Opioid%20Use,%20Misuse,%20and%20Abuse%20in%20Practice.pdf (date last accessed 17 August 2017).
- 6.Morris BJ, Laughlin MS, Elkousy HA, Gartsman GM, Edwards TB. Preoperative opioid use and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg 2015;24:11–16. [DOI] [PubMed] [Google Scholar]
- 7.Lee D, Armaghani S, Archer KR, et al. Preoperative opioid use as a predictor of adverse postoperative self-reported outcomes in patients undergoing spine surgery. J Bone Joint Surg [Am] 2014;96-A:89. [DOI] [PubMed] [Google Scholar]
- 8.Zywiel MG, Stroh A, Yong Lee S, Bonutti PM, Mont MA. Chronic opioid use prior to total knee arthroplasty. J Bone Joint Surg [Am] 2011;93-A:1988–1993. [DOI] [PubMed] [Google Scholar]
- 9.Holman JE, Stoddard GJ, Higgins TF. Rates of prescription opiate use before and after injury in patients with orthopaedic trauma and the risk factors for prolonged opiate use. J Bone Joint Surg [Am] 2013;95:1075–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lawrence JT, London N, Bohlman HH, Chin KR. Preoperative narcotic use as a predictor of clinical outcome: results following anterior cervical arthrodesis. Spine (Phila Pa 1976) 2008;33:2074–2078. [DOI] [PubMed] [Google Scholar]
- 11.Menendez ME, Ring D, Bateman BT. Preoperative opioid misuse is associated with increased morbidity and mortality after elective crthopaedic surgery. Clin Orthop Relat Res 2015;473:2402–2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pivec R, Issa K, Naziri Q, et al. Opioid use prior to total hip arthroplasty leads to worse clinical outcomes. Int Orthop 2014;38:1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bedard NA, Pugely AJ, Westermann RW, et al. Opioid use after total knee arthroplasty: trends and risk factors for prolonged use. J Arthroplasty 2017;32:2390–2394. [DOI] [PubMed] [Google Scholar]
- 14.No authors listed. ICD-9-CM Diagnosis and Procedure Codes: Abbreviated and Full Code Titles. https://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html (date last accessed 21 August 2017).
- 15.Fuzier R, Serres I, Bourrel R, et al. Analgesic drug consumption increases after knee arthroplasty: a pharmoepidemiological study investigating postoperative pain. Pain 2014;155:1339–1345. [DOI] [PubMed] [Google Scholar]
- 16.Brummett CM, Urquhart AG, Hassett AL, et al. Characteristics of fibromyalgia independently predict poorer long-term analgesic outcomes following total knee or hip arthroplasty. Arthritis Rheumatol 2015;67:1386–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.da Costa BR, Nüesch E, Kasteler R, et al. Oral or transdermal opioids for osteoarthritis of the knee or hip. Cochrane Database Syst Rev 2014;9:CD003115. [DOI] [PMC free article] [PubMed] [Google Scholar]