Abstract
The six-component maintenance of lipid asymmetry (Mla) system is responsible for retrograde transport of phospholipids, ensuring the barrier function of the Gram-negative cell envelope. Located within the outer membrane, MlaA (VacJ) acts as a channel to shuttle phospholipids from the outer leaflet. We identified Neisseria gonorrhoeae MlaA (ngo2121) during high-throughput proteomic mining for potential therapeutic targets against this medically important human pathogen. Our follow-up phenotypic microarrays revealed that lack of MlaA results in a complex sensitivity phenome. Herein we focused on MlaA function in cell envelope biogenesis and pathogenesis. We demonstrate the existence of two MlaA classes among 21 bacterial species, characterized by the presence or lack of a lipoprotein signal peptide. Purified truncated N. gonorrhoeae MlaA elicited antibodies that cross-reacted with a panel of different Neisseria. Little is known about MlaA expression; we provide the first evidence that MlaA levels increase in stationary phase and under anaerobiosis but decrease during iron starvation. Lack of MlaA resulted in higher cell counts during conditions mimicking different host niches; however, it also significantly decreased colony size. Antimicrobial peptides such as polymyxin B exacerbated the size difference while human defensin was detrimental to mutant viability. Consistent with the proposed role of MlaA in vesicle biogenesis, the ΔmlaA mutant released 1.7-fold more membrane vesicles. Comparative proteomics of cell envelopes and native membrane vesicles derived from ΔmlaA and wild type bacteria revealed enrichment of TadA–which recodes proteins through mRNA editing–as well as increased levels of adhesins and virulence factors. MlaA-deficient gonococci significantly outcompeted (up to 16-fold) wild-type bacteria in the murine lower genital tract, suggesting the growth advantage or increased expression of virulence factors afforded by inactivation of mlaA is advantageous in vivo. Based on these results, we propose N. gonorrhoeae restricts MlaA levels to modulate cell envelope homeostasis and fine-tune virulence.
Author summary
The Gram-negative outer membrane is a formidable barrier, primarily because of its asymmetric composition. A layer of lipopolysaccharide is exposed to the external environment and phospholipids are on the internal face of the outer membrane. MlaA is part of a bacterial system that prevents phospholipid accumulation within the lipopolysaccharide layer. If MlaA is removed, membrane asymmetry is disrupted and bacteria become more vulnerable to certain antimicrobials. Neisseria gonorrhoeae causes millions of infections worldwide annually. A growing number are resistant to available antibiotics. Improving our understanding of gonococcal pathogenicity and basic biological processes is required to facilitate the discovery of new weapons against gonorrhea. We investigated the role of MlaA in N. gonorrhoeae and found that when MlaA was absent, bacteria were more sensitive to antibiotics and human defensins. However, the mutant bacteria produced more membrane vesicles–packages of proteins wrapped in membrane material. Mutant vesicles and cell envelopes were enriched in proteins that contribute to disease. These alterations significantly increased mutant fitness during experimental infection of the female mouse genital tract. Our results provide new insights into the processes N. gonorrhoeae uses to fine-tune its ability to stay fit in the hostile environment of the genital tract.
Introduction
The Gram-negative cell envelope (CE) plays an important role in bacterial physiology. Not only does it prevent cell lysis through the structure of the peptidoglycan cell wall [1], but it also acts to prevent entry of toxic lipophilic, hydrophilic, and amphipathic molecules. This barrier function is accomplished by the asymmetric outer membrane, which, in contrast to the phospholipid bilayer common to eukaryotic cells, is composed of an outer leaflet of lipopolysaccharide (LPS) or lipooligosaccharide (LOS) and an inner leaflet of phospholipids [2]. Due to the saturated fatty acids found in the hexa-acylated lipid A portion of LPS/LOS, the lipid interior of the LPS/LOS layer is less fluid than that of a phospholipid layer. As a result, the asymmetric bilayer is a more effective barrier than a phospholipid bilayer would be, and is thus less permeable to lipophilic compounds. If the asymmetry of the outer membrane is perturbed, phospholipids diffuse from the inner leaflet to the outer leaflet, which compromises the barrier function of the outer membrane [3].
Three lipid asymmetry-maintaining systems, primarily studied in Escherichia coli, are the phospholipase A PldA [4], the LPS palmitoyltransferase PagP [5], and the maintenance of lipid asymmetry (Mla) [6] systems. PagP and PldA both remove phospholipids from the outer membrane by destroying the phospholipid. PagP transfers a palmitate residue from the sn-1 position of outer leaflet phospholipids to lipid A to form hepta-acylated LPS, which increases hydrophobic interactions between adjacent LPS molecules [7]. PldA forms an active dimer in the outer membrane in the presence of phospholipids or lyso-phospholipids, then removes the sn-1 and sn-2 fatty acid side chains from the misplaced phospholipids [8]. These fatty acids can act as signal molecules to enhance LPS production, which suggests PldA possesses a secondary function as a sensor for altered membrane homeostasis [9]. In contrast to PagP and PldA, the six-component Mla system, composed of MlaA-F, does not destroy phospholipids in the outer leaflet. Instead, the Mla system is proposed to participate in retrograde transport of phospholipids from the outer leaflet, through the periplasm via MlaC, and back to the inner membrane, where phospholipids are thought to be integrated through the action of the MlaFEDB complex (Fig 1A; [6]). The outer membrane component of this system, MlaA, was recently crystallized from Klebsiella pneumoniae and Serratia marcescens in complex with the outer membrane β-barrel protein OmpF. The crystal structure revealed that MlaA forms a pore through which phospholipid head groups are able to travel [10]. Loss of MlaA disrupts outer membrane integrity, as demonstrated by increased bacterial sensitivity to a combination of sodium dodecyl sulfate (SDS) and ethylenediaminetetraacetic acid (EDTA), in addition to several antibiotics [6, 10–12]. Single knockouts in any component of the Mla system in E. coli appear to mirror the defects caused by the lack of MlaA, and double knockouts of mlaA with any other Mla component exhibit similar sensitivity to single knockouts [6]. With the exception that iron limitation restricts MlaA transcription in vitro and in vivo [13], little is known about regulation of the Mla system.
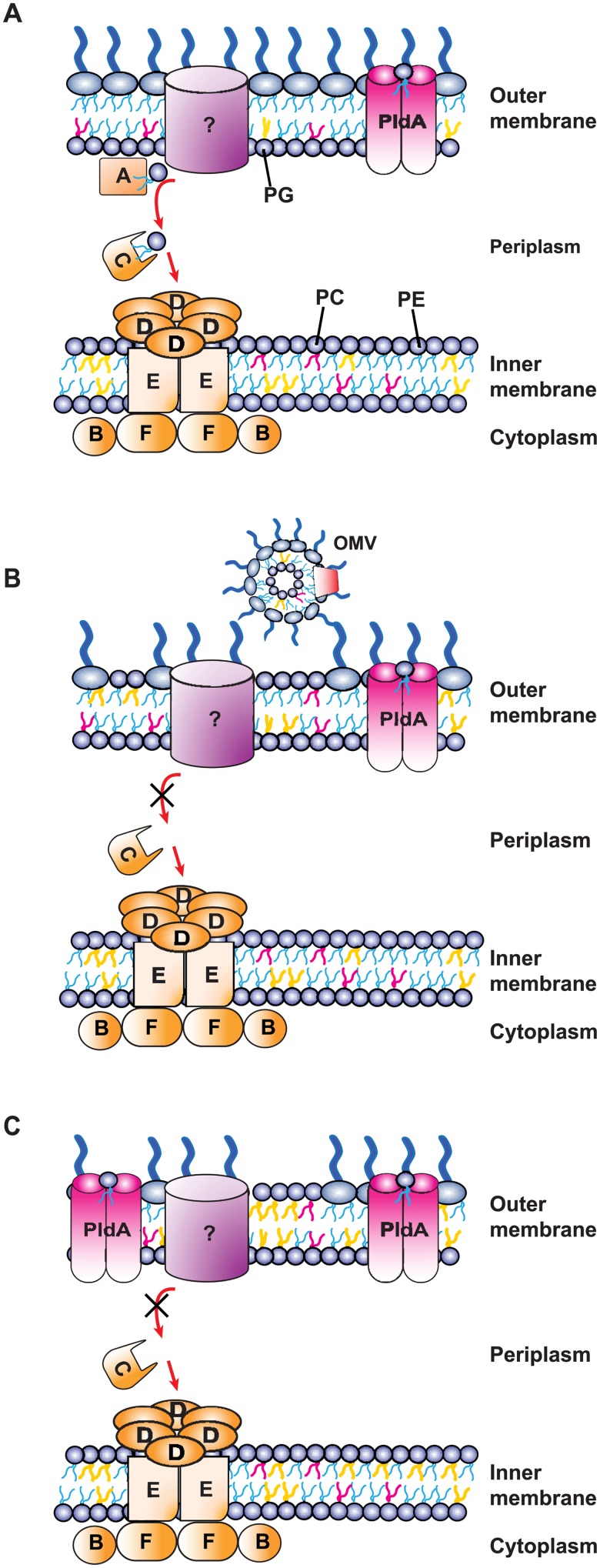
Fig 1. Model of phospholipid homeostasis systems in N. gonorrhoeae.
(A) In WT N. gonorrhoeae, MlaA, potentially interacting with an unknown partner, participates in retrograde trafficking of phospholipids from the outer leaflet of the outer membrane, through the periplasmic component of the system, MlaC, to the inner membrane MlaBDEF complex. The phospholipase PldA dimerizes to its active form upon detection of mis-localized phospholipids and removes the sn-1 and sn-2 fatty acid side chains. Different phospholipids are represented by lipid tails of different colors (phosphatidylglycerol [PG], yellow; phosphatidylcholine [PC], red; phosphatidylethanolamine [PE], blue). Native N. gonorrhoeae membrane phospholipid composition can be found in Table 4. (B) When MlaA is removed, phospholipids cannot be transported through the Mla system and invade the outer leaflet of the outer membrane. Increased amounts of membrane vesicles are also produced. (C) When the phospholipase PldA is overexpressed in the absence of MlaA, the PE substrate preference of PldA leads to a membrane phospholipid profile that is skewed toward PG, including in the outer leaflet of the outer membrane. OMV, outer membrane vesicle.
MlaA is present in pathogenic and non-pathogenic Gram-negative bacteria. Its primary function, therefore, appears to be the maintenance of lipid asymmetry. However, infection studies with different pathogenic bacteria suggest that MlaA possesses divergent moonlighting roles. Originally discovered in Shigella flexneri and named VacJ for virulence associated, chromosome locus J, this protein contributes to the ability of S. flexneri to invade adjacent epithelial cells [14, 15]. In Haemophilus influenzae, VacJ plays a role in serum resistance [16], and in Pseudomonas putida and Campylobacter jejuni, MlaA provides protection against oxidative stress [17, 18]. Downregulation of VacJ has also been associated with the increased formation of membrane vesicles in H. influenzae and Vibrio cholerae [13]. MlaA/VacJ knockouts in S. flexneri, H. parasuis, and Salmonella enterica Typhimurium exhibit virulence defects [11, 14, 15]. In contrast, P. aeruginosa deficient in VacJ was significantly more virulent [12].
Phospholipid regulation other than the action of PldA has not been studied in the genus Neisseria, which includes the human pathogens N. meningitidis and N. gonorrhoeae. The Neisserial Mla system has not been characterized. N. gonorrhoeae, the causative agent of gonorrhea, is a worldwide public health threat. The World Health Organization estimates that 78 million new cases are acquired globally every year [19]. Treatment failures with the last effective class of antibiotics have been encountered in several countries, highlighting the necessity of developing new therapeutic interventions [20, 21]. We identified MlaA as a therapeutic candidate for gonorrhea in a high-throughput proteomic examination of the CE and naturally released membrane vesicles (MVs). Deletion of this protein, encoded by the ngo2121 open reading frame in N. gonorrhoeae FA1090, resulted in phenotypes that suggested disrupted outer membrane integrity [22]. We subsequently performed a comprehensive phenotypic microarray screen to assess the function of seven proteome-derived gonorrhea vaccine candidates and therapeutic targets, including MlaA, in CE homeostasis. The results revealed an extensive sensitivity phenome in a ΔmlaA mutant, including increased susceptibility to compounds that trigger oxidative stress. Importantly, deletion of mlaA in the highly antibiotic resistant WHO X strain resulted in similar phenotypes to those observed for a ΔmlaA mutant constructed in the FA1090 laboratory strain [23].
In this work, we further characterized the role of MlaA in gonococcal physiology and pathogenesis using different in silico, genetic, proteomic, and in vitro and in vivo assays. The results of our investigations revealed a previously unknown gonococcal virulence pathway and suggest that N. gonorrhoeae may employ MlaA to modulate its CE and MV protein profile and fine-tune its ability to colonize the host.
Results
MlaA conservation
Despite the importance of MlaA in the Gram-negative cell envelope and its different outcomes on pathogenesis, its conservation across bacterial species has not been addressed. Accordingly, we analyzed the similarity at the amino acid level in a diverse range of Gram-negative bacteria in comparison to N. gonorrhoeae MlaA. With the exception of other Neisseria species, the percent identity was relatively low and ranged from 26.15% to 34.53% (Table 1, S1 File). We previously noted that although N. gonorrhoeae MlaA is annotated as a predicted lipoprotein, it lacks the universally conserved cysteine residue required for lipidation and membrane anchoring [23, 24]. We were curious whether the lack of a lipoprotein signal peptide is limited to N. gonorrhoeae; therefore, MlaA homologs from Neisseria species and other bacteria in which MlaA/VacJ has been characterized were scrutinized for the presence of a lipoprotein signal peptide. This analysis revealed that homologous proteins in P. aeruginosa, P. putida, C. jejuni, Caulobacter crescentus, and Desulfovibrio vulgaris did not contain the conserved cysteine residue. Additionally, homologs in the closely-related N. meningitidis, N. lactamica, and N. weaveri did not contain a lipoprotein signal peptide (Table 1). We subsequently carried out a secondary search for MlaA without a predicted lipoprotein signal sequence for the presence of a signal peptidase I (SPaseI) motif and constructed a maximum likelihood phylogenetic tree (Fig 2A). Within the tree, SPaseI-cleaved MlaA homologs clustered separately from those containing a lipoprotein signal peptide (SPaseII-cleaved proteins), with the exception of K. pneumoniae and Francisella tularensis, with the latter protein forming an outgroup within the larger cluster.
Table 1. Amino acid identity of MlaA homologs.
| Organism with Accession No. | Amino Acid Identity | Predicted Lipoprotein Signal Peptide? | Molecular Mass (kDa)c |
|---|---|---|---|
| Neisseria gonorrhoeae FA1090 [WP_010951410.1] | 100% | No | 29.6 |
| Escherichia coli [WP_000776765] | 28.26% | Yes | 28.0 |
| Neisseria meningitidis [WP_002214840.1] | 95.64% | No | 29.5 |
| Neisseria lactamica [WP_003711038.1] | 96.36% | No | 29.5 |
| Neisseria weaveri [WP_004284372.1] | 63.50% | No | 31.5 |
| Haemophilus influenzae [WP_005694634.1] | 28.38% | Yes | 28.1 |
| Vibrio cholerae [WP_001881772.1] | 28.14% | Yes | 28.6 |
| Shigella flexneri [WP_000776763.1] | 28.26% | Yes | 28.0 |
| Pseudomonas aeruginosa [WP_044486151.1] | 34.53% | No | 26.2 |
| Pseudomonas putida [WP_010953149.1] | 33.93% | No | 26.1 |
| Campylobacter jejuni [WP_002853724.1] | 30.00% | No | 26.5 |
| Salmonella enterica Typhimurium [NP_461334.1] | 28.26% | Yes | 28.2 |
| Pasteurella multocida [AHW46103.1] | 29.52% | Yes | 27.6 |
| Francisella tularensis [AJI58656.1] | 26.15% | Yes | 37.5 |
| Klebsiella pneumoniae [WP_099452242.1] | 34.39% | Yes/Noa | 28.8 |
| Serratia marcescens [WP_015673230.1] | 29.74% | Yes | 28.1 |
| Haemophilus parasuis [WP_005712539.1] | 27.51% | Yes | 28.0 |
| Yersinia enterocolitica [WP_011815902.1] | 29.18% | Yes | 28.1 |
| Caulobacter crescentus [WP_010921519.1] | 28.86% | No | 30.3 |
| Desulfovibrio vulgaris [WP_010940416.1] | 33.18% | Nob | 32.2 |
| Haemophilus ducreyi [WP_064082213.1] | 27.63% | Yes | 27.7 |
a24 sequences with lipoprotein signal peptide, 3 sequences without any signal peptide
bNo signal peptide detected.
cMolecular mass calculated from unprocessed primary amino acid sequence.
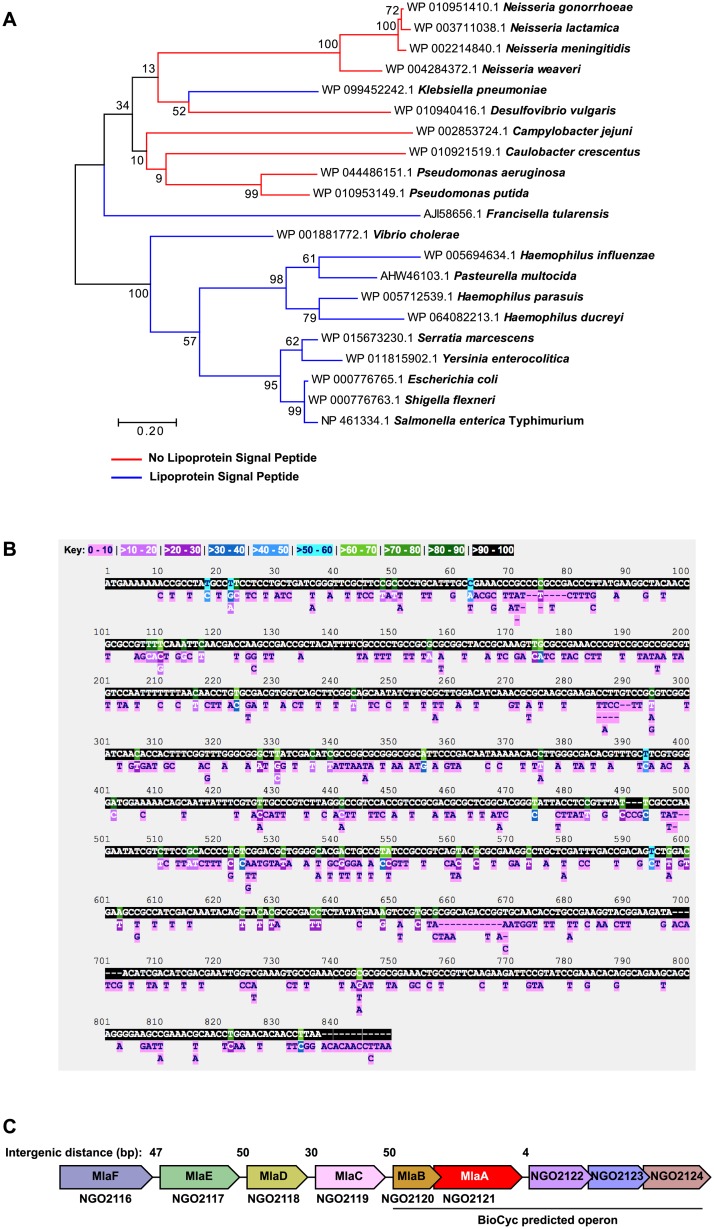
Fig 2. Bioinformatic analysis of MlaA conservation and genome context.
(A) A phylogenetic tree of MlaA was constructed in MEGA using amino acid sequences of MlaA/VacJ homologs downloaded from NCBI. The Jones-Taylor-Thornton model was used to generate a pairwise distance matrix. Neighbor-Join and BioNJ algorithms were subsequently applied to the matrix to obtain the initial tree for a heuristic search. 500 bootstrap iterations were performed to test the phylogenies. The highest log-likelihood tree is presented. Homologs without lipoprotein signal peptides are represented by red branches; blue branches represent homologs with lipoprotein signal peptides. (B) The PubMLST Neisseria database was used to search for nucleotide polymorphic sites in the mlaA (NEIS1933) locus across 44,289 Neisseria isolates. (C) Local genome context of N. gonorrhoeae mlaA. Intergenic distances between open reading frames are noted above the schematic. The operon predicted by biocyc.org is noted below. Schematic and intergenic distances are not to scale.
An examination of the level of nucleotide conservation between MlaA homologs in all Neisseria performed using the Neisseria Multi Locus Sequence Typing database (locus identifier NEIS1933) indicated that the majority of the ngo2121 nucleotide sequence represented 90–100% of the alleles, with 461 alleles exhibiting 410 polymorphic sites (Fig 2B). Phylogenetic analyses of amino acid sequences representing MlaA alleles from all Neisseria and from N. gonorrhoeae isolates exclusively showed that MlaA alleles are closely related among Neisseria sp. and within N. gonorrhoeae (S1A and S1B Fig, respectively).
In summary, our examinations of MlaA conservation, both outside and within the Neisseria genus, revealed differences that warranted further investigation into the function of this protein in N. gonorrhoeae.
Genome context and organization of MlaA
To extend our observations of the differences between MlaA in divergent bacteria, we examined the genomic location of mlaA across 7 bacterial species in which MlaA has been investigated. Predictions by biocyc.org suggested that N. gonorrhoeae mlaA is a member of an operon consisting of ngo2120 to ngo2124 (Fig 2C). However, upon closer inspection of the local genome context, mlaA appeared to be a part of a polycistronic operon composed of ngo2116 to ngo2124, primarily because of the small intergenic distances and the lack of predicted promoters between each open reading frame. Importantly, NGO2120, NGO2119, NGO2118, NGO2117, and NGO2116 exhibited homology to the other components of the E. coli Mla system, MlaB, MlaC, MlaD, MlaE, and MlaF, respectively (Fig 2C, Table 1 in S1 Text). The genetic organization surrounding mlaA is shared by N. meningitidis and N. lactamica. In contrast, E. coli, S. marcescens, S. flexneri, K. pneumoniae, P. aeruginosa, and S. enterica enterica serovar Typhimurium mlaA are spatially isolated from the genes encoding the remaining components of the Mla system (S2 Fig). The genomic organization of the Mla system into one operon within the Neisseria genomes suggests regulation of Mla complex expression differs between various bacterial species.
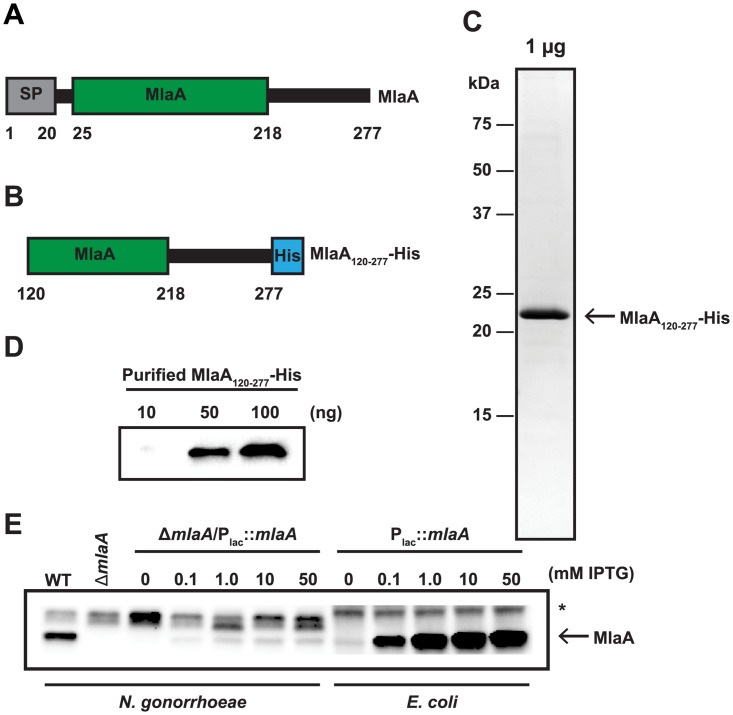
Protein purification and antibody generation
To generate molecular tools for our studies, we set out to purify a soluble, recombinant variant of MlaA. A representative schematic of full-length MlaA is presented in Fig 3A. This protein contains a predicted signal peptide from residues 1 to 20, cleaved by SPaseI, and an ABC transporter Mla domain from residues 25 to 218. Although full-length MlaA was predominantly found in the soluble protein fraction, initial purification attempts with a 6× His-tag or a maltose-binding protein purification handle were unsuccessful due to extensive aggregation of MlaA (S3 Fig). To circumvent this challenge, a truncated version of the protein without the first predicted transmembrane helix, MlaA120-277, with a C-terminal 6× His-tag was generated (Fig 3B) and purified by affinity chromatography, yielding 99% pure MlaA that migrated at ~22 kDa, consistent with the predicted size of the engineered protein (Fig 3C). Rabbit polyclonal antibodies produced against this protein recognized purified MlaA120-277-His (Fig 3D) and a protein band corresponding to the approximate size of native MlaA (29.6 kDa) in whole cell lysates of WT N. gonorrhoeae but not the ΔmlaA mutant (Fig 3E). In all cell lysates, a major cross-reactive protein with highly variable expression that was not associated with MlaA levels was also observed (Fig 3E, marked with an asterisk). BLAST searches of the FA1090 genome with the MlaA120-277 amino acid sequence did not reveal any proteins that could be the cross-reactive band. A titration with isopropyl β-D-1-thiogalactopyranoside (IPTG) to examine induction of MlaA in the complemented strain (ΔmlaA/Plac::mlaA) constructed previously [23] revealed that maximal expression of MlaA was achieved with 50 mM IPTG (Fig 3E). However, even with this high level of inducer, expression was not restored to WT levels, indicating that certain phenotypes observed for the mlaA null strain may not be entirely complemented, as we previously observed with hypersensitivity to bile salts [23]. A similar IPTG titration performed with an E. coli strain harboring the pGCC4-ngo2121 complementation plasmid revealed that MlaA expression was readily induced in a heterologous host (Fig 3E). We independently generated additional complementation strains, one in the FA1090 ΔmlaA mutant and four in WHO X lacking MlaA [23]. The non-specific cross-reactive band was not observed in the WHO X strain. WT levels of protein expression were not restored in any of the strains (S4A Fig). These results suggest that MlaA may be under the influence of secondary regulation or requires the presence of additional Mla components for stability in N. gonorrhoeae.
Fig 3. Purification of a truncated recombinant version of MlaA and polyclonal anti-MlaA serum validation.
(A) Representative schematic of full length MlaA with annotated MlaA domain. A signal peptide (SP) is noted by a grey rectangle. (B) Schematic of truncated MlaA used for purification with first 119 amino acids removed and a 6 × Histidine tag (His; as a blue rectangle) added to the N-terminus. Schematics are not to scale. (C) Truncated MlaA construct was overexpressed in E. coli and purified by nickel affinity chromatography in the presence of 1% Triton-X 100 detergent. Detergent was subsequently removed by incubation with Bio-Rad Bio-Beads SM-2 resin. To assess purity, 1 μg of protein was subjected to 1D SDS-PAGE and visualized by staining with Colloidal Coomassie Blue G-250. Open arrow indicates migration band of MlaA120-277. Migration of a molecular weight marker (in kDa) is indicated to the left of the gel. (D) Immunoblot evaluation of anti-MlaA antiserum. Indicated amounts of purified MlaA120-277 were separated by SDS-PAGE, transferred to a nitrocellulose membrane, and probed with anti-MlaA antiserum. (E) Equivalent OD600 units of WT, isogenic ΔmlaA, and either ΔmlaA/Plac::mlaA or E. coli harboring the pGCC4-ngo2121 complementation plasmid cultured with indicated concentrations of IPTG, were separated by SDS-PAGE, transferred to a nitrocellulose membrane, and probed with anti-MlaA antiserum. Open arrow indicates MlaA. Non-specific cross-reactive band is marked with an asterisk (*). OD600, optical density at 600 nm; IPTG, isopropyl β-D-thiogalactopyranoside; SDS-PAGE, sodium dodecyl sulfate-polyacrylamide gel electrophoresis.
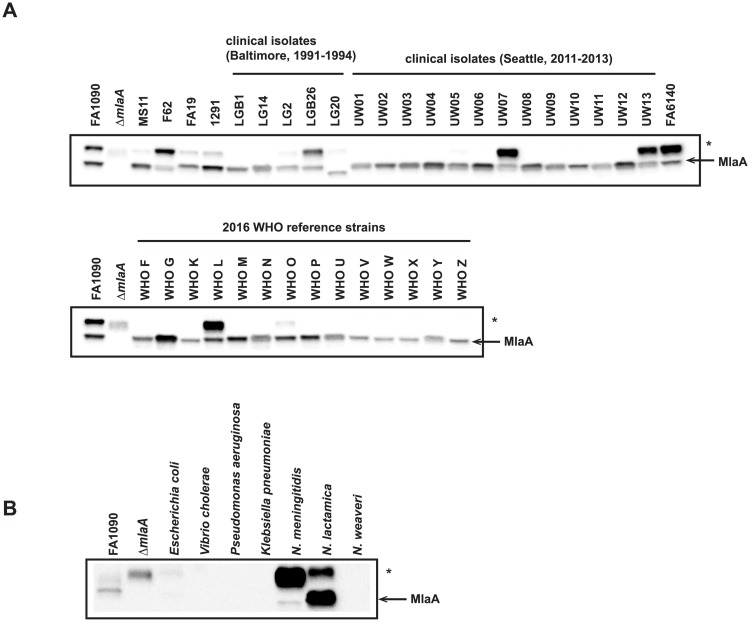
Expression of MlaA among gonococcal clinical isolates and within Neisseria
We examined the expression pattern of MlaA in whole cell lysates collected from geographically and temporally distinct clinical isolates [25, 26]. Immunoblots indicated that MlaA was expressed by all 38 strains at different levels (Fig 4A). Additionally, in the case of isolate LG20, MlaA migrated at a lower molecular weight than FA1090 MlaA. Finally, the non-specific band observed in FA1090 lysates (band marked by asterisk in Fig 4A) was highly abundant only in three of the 18 clinical isolates (LGB26, UW07, and UW13), one WHO reference strain (WHO L), FA6140, and three of the four laboratory strains examined (F62, FA19, and 1291).
Fig 4. Truncated, recombinant MlaA elicits broadly cross-reactive antisera that recognize MlaA in Neisseria species.
(A) 37 N. gonorrhoeae isolates, including common laboratory strains; clinical isolates collected in Baltimore between 1991 and 1994 and Seattle between 2011 and 2013; and the 2016 WHO reference strains were grown on solid media for 20 h at 37 °C in 5% CO2. Whole cell lysates were collected and subjected to immunoblotting analysis. (B) Whole cell lysates of different Gram-negative bacteria, including E. coli BL21(DE3); V. cholerae N19691; P. aeruginosa PA01; K. pneumoniae 6069; N. meningitidis MC58; the commensal bacterium N. lactamica NLI83/-01; and the opportunistic pathogen N. weaveri 1032 were subjected to immunoblot analysis. All lysates were standardized by OD600 values, separated in a 4–15% Tris-glycine gel, and probed with polyclonal rabbit antiserum against MlaA. FA1090 and ΔmlaA were included in blots as positive controls. Open arrow indicates MlaA. Non-specific cross-reactivity is marked with an asterisk (*). OD600, optical density at 600 nm; SDS-PAGE, sodium dodecyl sulfate-polyacrylamide gel electrophoresis.
We further assessed whether antiserum against FA1090 MlaA could recognize homologous proteins from other Neisseria species, as well as more distantly related bacteria. Of the seven species tested, only N. meningitidis and N. lactamica homologs were detected (Fig 4B). In summary, these observations provide additional support for the results of our bioinformatic analyses and indicate that MlaA is likely to play a similar role in the CE of clinical isolates collected from different geographical locations, at different points in time, and exhibiting all known antibiotic resistance profiles [25, 26]. Further, the expression of MlaA across a range of diverse clinical isolates supports our use of FA1090 as a type strain to study the effects of the loss of MlaA on gonococcal fitness and pathogenesis.
Phenotypic characterization of MlaA in vitro
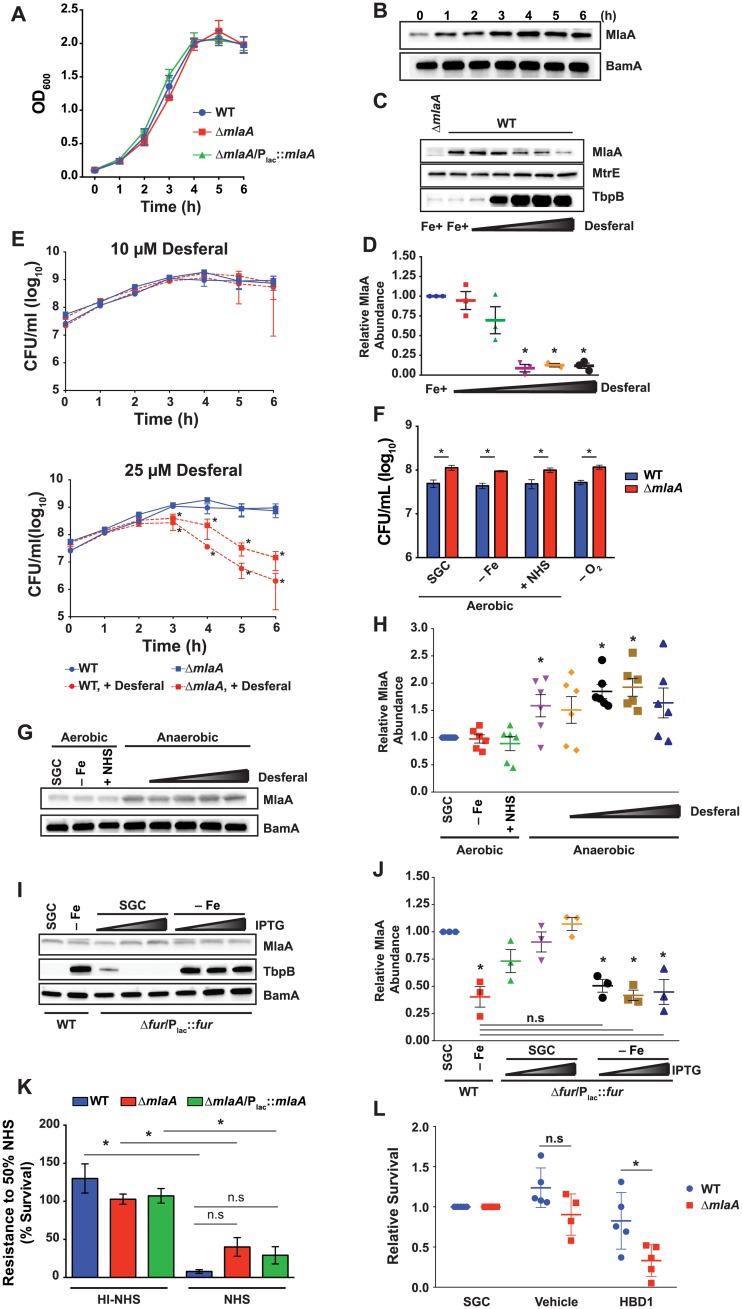
To gain further insights into the impact of MlaA on gonococcal physiology, we first examined the growth kinetics of the WT and ΔmlaA mutant under standard growth conditions in liquid medium. Neither the ΔmlaA mutant nor the complemented strain displayed a difference in growth compared to WT (Fig 5A), consistent with our previous observations using solid medium and chemically defined Graver-Wade liquid medium [22, 23]. An assessment of MlaA abundance in WT whole cell lysates from liquid cultures over time revealed that expression of MlaA was lower during the lag phase, slightly increased during logarithmic growth, reached maximum expression at approximately mid-logarithmic phase, and was maintained at similar levels until stationary phase (Fig 5B), at which point the experiment was terminated to avoid the effects of autolysis [27].
Fig 5. In vitro fitness assessments and MlaA expression profiling.
(A) WT FA1090, isogenic knockout ΔmlaA, and complementation strain ΔmlaA/Plac::mlaA were cultured aerobically in liquid medium. IPTG was added to 0.1 mM in ΔmlaA/Plac::mlaA cultures. Bacterial growth was monitored every hour by OD600 measurement. (B) Samples of WT FA1090 were collected at the times indicated. Whole cell lysates were separated by SDS-PAGE and probed with polyclonal rabbit anti-MlaA or anti-BamA (as a loading control) antisera. (C) Whole cell lysates of WT FA1090 were collected after 6 h culture in liquid medium containing desferal at concentrations ranging from 5–25 μM. Samples were probed with antisera against MlaA, MtrE, and TbpB. ΔmlaA cultured under standard conditions was included as a reference. (D) Densitometry analyses of MlaA using immunoblots from three independent desferal titration experiments shown as a representative blot in panel (C). (E) WT FA1090 and isogenic ΔmlaA were cultured in liquid medium containing either 10 μM (top panel) or 25 μM (bottom panel) desferal for 6 h. At each hour, samples were withdrawn and diluted for CFU/mL enumeration. Both graphs contain growth curves from cultures maintained under standard conditions (blue curves). Statistical significance was assessed by two-way ANOVA using Sidak’s multiple comparisons test. (F) WT FA1090 and isogenic knockout ΔmlaA were cultured in liquid medium under standard conditions until OD600 had at least doubled (~3 h). Cultures were standardized to an OD600 of 0.2 and dilutions were spotted onto GCB. Plates were prepared as normal (SGC); under iron deprivation (-Fe); supplemented with 7.5% normal human serum (+NHS); or supplemented with 1.2 mM NaNO2 and cultured anaerobically (-O2). Strains were maintained at 37 °C in 5% CO2 for approximately 22 h or at 37 °C anaerobically for 48 h and CFU were enumerated. (G) WT bacteria cultured as in (F), with the addition of a desferal titration from 0–25 μM under anaerobiosis, were collected from plates, separated by SDS-PAGE, and probed with polyclonal rabbit anti-MlaA antiserum or anti-BamA antiserum as a loading control. (H) Densitometry analyses of MlaA abundance under each host relevant condition presented in (G). Densitometry was performed twice on each of three independent experiments. (I) WT FA1090 and conditional knockout Δfur/Plac::fur were cultured in liquid medium in the absence (SGC) or presence of 25 μM desferal (-Fe). Fur expression was induced by the addition of 10, 50, or 100 μM IPTG. Samples were collected after 6 h of growth and probed with indicated antisera. (J) Densitometry analyses of MlaA abundance in immunoblots from three independent Fur induction experiments with and without iron starvation. (K) WT FA1090, isogenic knockout ΔmlaA, and ΔmlaA/Plac::mlaA were cultured aerobically in liquid medium until culture density had doubled (~3 h). Cultures were diluted to an OD600 of 0.05 in sterile PBS and diluted 1000-fold in EMEM. Suspensions were combined with an equal volume of EMEM, NHS, or heat-inactivated NHS and incubated for 1 h in 5% CO2 at 37 °C. Bacteria from each well were spotted onto GCB plates. CFUs were scored after 20–22 h incubation in 5% CO2 at 37 °C (p value between WT and ΔmlaA exposed to active NHS, 0.07). (L) Rapidly growing cultures of WT FA1090 and isogenic knockout ΔmlaA were diluted to 105 CFU/mL and cultured for 3 h in the presence of liquid medium (SGC), 0.01% acetic acid (vehicle), or 10 μM human defensin (HBD1). Bacteria were serially diluted and spotted onto GCB plates. CFUs were scored after 20–22 h incubation in 5% CO2 at 37 °C and survival was calculated relative to SGC. n≥3; mean ± SEM presented for all experiments; panels D, H, J, and L present values from each replicate; *p < 0.05; OD600, optical density at 600 nm; SGC, standard growth conditions; IPTG, isopropyl β-D-thiogalactopyranoside; SDS-PAGE, sodium dodecyl sulfate-polyacrylamide gel electrophoresis; CFU, colony forming unit; GCB, gonococcal base medium; GCBL, gonococcal base liquid medium; PBS, phosphate buffered saline; EMEM, Eagle’s minimal essential medium.
N. gonorrhoeae restricts the MlaA cellular pool during iron deprivation
Iron is a well-characterized regulator of gonococcal gene expression. Numerous genes are iron-repressed and are thus expressed in body sites where iron is limited [28, 29]. Therefore, we assessed the expression of N. gonorrhoeae MlaA and its effect on bacterial viability under iron deprivation. Titration with the iron chelator desferal (up to 25 μM) revealed that MlaA production decreased under increasing iron limitation, in contrast to TbpB, a well-characterized protein induced during iron starvation ([30]; Fig 5C). Antiserum against MtrE, a component of the MtrCDE efflux pump that is not influenced by iron [25, 31], was used as a loading control and showed that MtrE expression was unaffected under any of the desferal concentrations tested. Densitometry analysis of MlaA abundance indicated a statistically significant decrease in the MlaA cellular pool under exposure to 15 μM desferal and higher (Fig 5D).
To examine whether the lack of MlaA affects bacterial viability under various iron concentrations, we monitored the growth of WT and ΔmlaA bacteria over time by enumeration of colony forming units (CFU/mL). Both strains were equivalently viable when exposed to moderate iron starvation (10 μM desferal; Fig 5E, top panel). In contrast, exposure to high iron starvation (25 μM of the iron chelator) resulted in a significant decrease in bacterial viability beginning at 3 h and continuing to the experimental endpoint for both strains, with the ΔmlaA mutant exhibiting a slight, non-statistically significant growth advantage over the WT (Fig 5E, bottom panel).
Together, these results show that depletion of iron negatively regulates the MlaA cellular pool and suggest that decreased levels of MlaA are favored by the bacteria under iron starvation encountered in the host.
MlaA affects bacterial viability under other in vitro conditions relevant to infection
N. gonorrhoeae is also exposed to conditions other than iron limitation during infection of different niches within the human host. Gonococci proliferate in microaerobic or anaerobic conditions within the female reproductive tract and may also be exposed to serum within inflammatory exudates and during disseminated infections [32]. The recovery of viable ΔmlaA mutant bacteria was statistically significantly higher (~2-fold) than that of the WT for all tested conditions relevant to infection of the host using solid medium with 5 μM desferal (- Fe), 7.5% normal human serum (NHS), or with nitrite under anaerobic conditions (- O2; Fig 5F). As expected from our investigations into iron starvation in liquid medium, immunoblotting analysis indicated no difference in MlaA expression under aerobic exposure to 5 μM desferal. The presence of serum also had no effect on MlaA levels. In contrast, MlaA was elevated under anaerobiosis in comparison to standard growth (Fig 5G). To examine the interplay between iron starvation and anoxia on MlaA expression, immunoblotting was also performed on bacteria collected from anaerobic conditions with increasing concentrations of desferal. Densitometry analysis indicated a significant difference in the abundance of MlaA during anoxia, as well as during anaerobic exposure to 10 or 20 μM desferal, although MlaA expression was highly variable under each anaerobic condition tested (Fig 5H). The integral membrane component of the β-barrel assembly machinery (BAM) complex, BamA [25, 33], was used as a loading control (Fig 5G), and its expression was not altered under any of the conditions examined [25].
Iron starvation diminishes the MlaA cellular pool independent of Fur levels
In N. gonorrhoeae, the ferric uptake regulator (Fur) protein governs expression of iron homeostasis genes in response to the intracellular pools of this important metal. To dissect the mechanism of MlaA repression during iron deprivation, we employed a conditional Fur knockout, Δfur/Plac::fur, as Fur is essential in N. gonorrhoeae (S5A Fig, [34]). Initial viability assessment indicated that Δfur/Plac::fur proliferated identically to WT bacteria in liquid medium supplemented with IPTG, both in the presence and absence of desferal (S5B Fig). Immunoblotting (Fig 5I) coupled with densitometry revealed a statistically significant decrease in MlaA levels under iron starvation, which was not restored with low (10 μM IPTG) or high (100 μM IPTG) Fur induction (Fig 5J). A non-significant reduction in MlaA expression compared to standard conditions was observed with the lowest Fur level examined during iron repletion, and MlaA abundance trended upward as IPTG was added (Fig 5J). We also examined TbpB expression as a Fur-regulated control [35]. Our analysis indicated that low Fur expression during iron repletion was insufficient to repress TbpB to the levels observed for the WT under standard conditions (Fig 5I and S5C Fig). Upon iron depletion, TbpB was derepressed in the Δfur/Plac::fur strain, regardless of Fur induction (Fig 5I), reflecting the inability of the repressor to dimerize and bind to its DNA target in the absence of iron [36]. BamA was used as a loading control and exhibited no alterations under any condition examined. Our quantitative immunoblotting assessments suggest Fur may exert a slight positive effect on MlaA expression under iron replete conditions, but that iron starvation overrules this influence. It is possible that MlaA is regulated by several factors–similar to TbpB, which is controlled by a long non-coding RNA and the MisR response regulator [28, 36].
N. gonorrhoeae MlaA does not contribute to serum resistance
Next, we sought to examine the sensitivity of WT, ΔmlaA, or ΔmlaA/Plac::mlaA bacteria to NHS in an assay using liquid medium [37], as VacJ has been described to contribute to serum resistance in H. influenzae [16]. Enumeration of CFUs after exposing gonococci to 50% NHS for 1 h revealed a significant decrease in viability for all strains compared to the same concentration of heat-inactivated NHS. No significant difference in survival, however, was observed between the WT, ΔmlaA, or ΔmlaA/Plac::mlaA strains during exposure to active serum (Fig 5K).
Bacteria lacking MlaA are more sensitive to human defensins
To extend our examination into the possible physiological contribution of MlaA during infection of the host, we exposed WT and ΔmlaA bacteria to human β-defensin 1 (HBD1). Defensins are cationic antimicrobial peptide components of the innate immune system which interfere with membrane integrity to exert their antibacterial effect [38]. Lack of MlaA was associated with a significant 2.5-fold reduction in viability compared to WT after HBD1 treatment (Fig 5L). N. gonorrhoeae is naturally resistant to HBD1 [39], which is constitutively expressed by epithelial cells [38]. The ΔmlaA mutant’s diminished viability upon HBD1 exposure suggests that loss of MlaA results in a cell envelope defect.
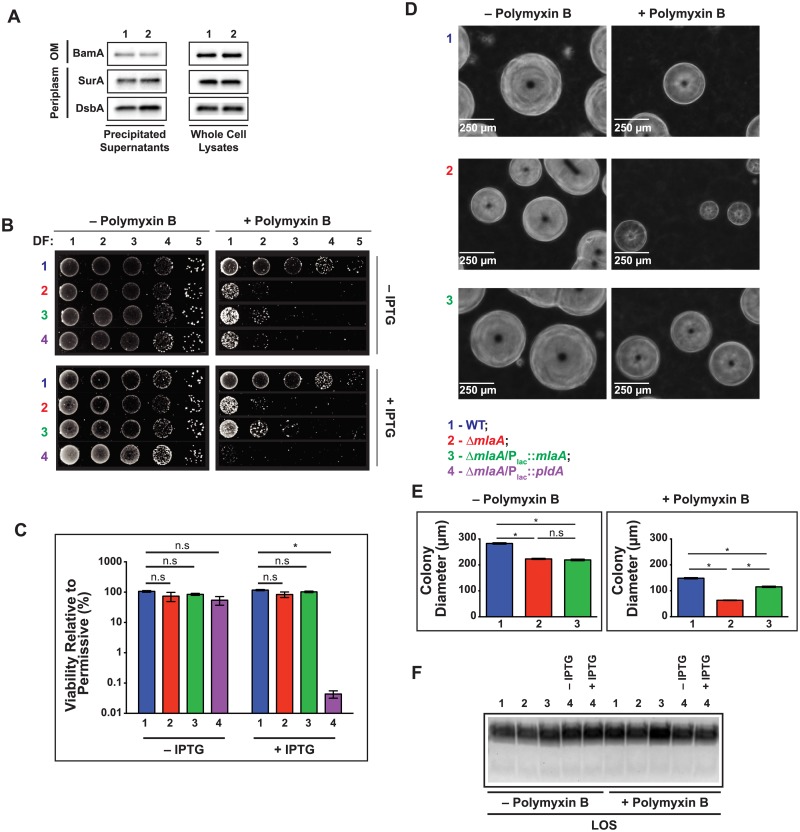
Outer membrane integrity is altered in a mlaA null mutant and can be partly rescued by PldA overproduction
Our observation that the ΔmlaA mutant was more susceptible to the membrane perturbing activity of HBD1 is consistent with our previous studies, in which we reported increased sensitivity of ΔmlaA mutants in the FA1090 and WHO X genetic backgrounds to polymyxin B on solid medium [22, 23]. Gonococci lacking MlaA were also more susceptible to several antibiotics during growth in chemically defined liquid medium, a sensitivity phenome that suggested an outer membrane defect, rather than general loss of membrane integrity [23]. To further determine how the altered outer membrane integrity in the ΔmlaA mutant translates to antibiotic tolerance, we applied an alternative approach and examined bacterial susceptibility to ten antibiotics with different mechanisms of action using Etest strips (Table 2). As expected from our previous studies, loss of MlaA resulted in a 2-fold decrease in the minimal inhibitory concentration (MIC) of polymyxin B (ΔmlaA mutant, MIC 32 μg/mL; WT bacteria, MIC 64 μg/mL), ampicillin (0.064 μg/mL, versus 0.125 μg/mL against the WT), and vancomycin (4 μg/mL, versus 8 μg/mL against the WT). All three antimicrobial compounds act by interfering with the barrier function of the outer membrane and the cell wall [40], and vancomycin was selected specifically to serve as a marker for outer membrane permeability, as an intact Gram-negative outer membrane excludes this antibiotic [41]. No differences in the MICs of other antibiotics with different mechanisms of action were observed. Consistent with results in the FA1090 background, deletion of mlaA from the WHO X genome resulted in 16- and 2-fold lower polymyxin B and vancomycin MICs, respectively (Table 2). Additionally, the clinically relevant antibiotics ceftriaxone and cefixime were not more effective against the WHO X ΔmlaA mutant, which provided further evidence that the permeability defect solely affects the outer membrane, as observed for the FA1090 mlaA null strain. On the other hand, the loss of MlaA does not interfere with cell envelope integrity to the extent that periplasmic proteins are released to the extracellular milieu, as no increase in the abundance of DsbA or SurA was observed in ΔmlaA–derived supernatants (Fig 6A). Additionally, neither DsbA nor SurA was upregulated in whole cell lysates of the ΔmlaA mutant, suggesting that absence of MlaA does not interfere with proper outer membrane protein folding [42–44].
Table 2. Etest assessments of cell envelope integrity.
| FA1090 background | WHO X background | ||||
|---|---|---|---|---|---|
| WTa | ΔmlaAa | ΔmlaA/Plac::pldAa | WTa | ΔmlaAa | |
| Polymyxin B | 64 | 32 | 16 | 128 | 8 |
| Vancomycin | 8 | 4 | 4 | 16 | 8 |
| Ceftriaxoneb | N/D | N/D | N/D | 1.0d | 1.0 |
| Cefiximeb | N/D | N/D | N/D | 2.0d | 2.0 |
| Azithromycin | 0.064 | 0.064 | 1.0c | N/D | N/D |
| Cefotaxime | 0.004 | 0.004 | 0.004 | N/D | N/D |
| Ampicillin | 0.125 | 0.064 | 0.125 | N/D | N/D |
| Tetracycline | 0.125 | 0.125 | 0.125 | N/D | N/D |
| Benzylpenicillin | 0.064 | 0.064 | 0.064 | N/D | N/D |
| Gentamicin | 4 | 4 | 4 | N/D | N/D |
| Tobramycin | 8 | 8 | 8 | N/D | N/D |
| Ceftazidime | 0.032 | 0.032 | 0.032 | N/D | N/D |
aMIC values are presented in μg/mL.
bPreliminary testing indicated FA1090 was too sensitive to this antibiotic for the MIC to be evaluated with Etests.
cVector for PldA overexpression encodes erythromycin resistance, which also provides resistance against azithromycin.
dPrior MIC determination performed on solid medium supplemented with hemoglobin and IsoVitalex [26]. N/D, not determined.
Fig 6. Loss of MlaA results in a reduction in gonococcal colony size that is exacerbated in the presence of the antimicrobial peptide polymyxin B.
(A) Supernatants from mid-logarithmic cultures of WT and ΔmlaA bacteria were separated by low-speed centrifugation and filtration, treated with DNAseI, and precipitated with a pyrogallol red-molybdate-methanol procedure. Precipitated supernatants and whole cell lysates were standardized by the OD600 of the source culture, separated by SDS-PAGE, and probed with indicated antisera. (B) WT FA1090, isogenic knockout ΔmlaA, complementation strain ΔmlaA/Plac::mlaA, and PldA overexpression strain ΔmlaA/Plac::pldA were cultured aerobically in liquid medium for 3 h, back diluted to an OD600 of 0.1, cultured 2 h longer, serially diluted, and spotted onto GCB without (left column) or with (right column) polymyxin B (800 U/mL) and either without (top row) or with (bottom row) 0.5 mM IPTG. Dilution spots from each condition were imaged with a Bio-Rad ImageDoc system. (C) CFUs for permissive and restrictive conditions with or without IPTG were counted and relative viability was calculated. Experiment was performed on three separate occasions (mean ± SEM on graph; *p < 0.05), and typical plate images are presented. (D) Representative micrographs from 10−4 dilution taken with a Zeiss AxioObserver.D1 microscope at 10× magnification 0.25 Phase Contrast 1 of WT (Row 1), ΔmlaA (Row 2), and ΔmlaA/Plac::mlaA (Row 3). MlaA expression was induced by inclusion of 0.1 mM IPTG in the solid medium for the complementation strain. (E) Images of 10−4 dilution were also taken at 2.5× magnification 0.06 Phase Contrast 1 and colony diameters were measured with ImageJ software. Colonies were measured for each of two independent experiments for the − polymyxin B condition (WT, n = 548; ΔmlaA, n = 755; ΔmlaA/Plac::mlaA, n = 664) and for the + polymyxin B condition (WT, n = 836; ΔmlaA, n = 1197; ΔmlaA/Plac::mlaA, n = 1121; mean ± SEM on graphs; *p < 0.05). (F) Rapidly growing liquid cultures of WT, ΔmlaA, ΔmlaA/Plac::mlaA, and ΔmlaA/Plac::pldA incubated in the presence or absence of polymyxin B were lysed and treated with proteinase K to isolate LOS. Subsequently, LOS was separated by SDS-PAGE and visualized by silver staining. IPTG was added to ΔmlaA/Plac::mlaA and ΔmlaA/Plac::pldA cultures to 0.5 mM as indicated. DF, dilution factor; OD600, optical density at 600 nm; IPTG, isopropyl β-D-thiogalactopyranoside; LOS, lipooligosaccharide; SDS-PAGE, sodium dodecyl sulfate–polyacrylamide gel electrophoresis.
Overexpression of the phospholipase PldA rescued SDS/EDTA sensitivity in E. coli ΔmlaC and in ΔmlaA/ΔmlaC knockouts, presumably by removal of phospholipids accumulated at the cell surface [6]. We therefore determined whether PldA overproduction would rescue the antibiotic sensitivity phenotypes observed for the N. gonorrhoeae ΔmlaA mutant. While WT resistance to ampicillin was restored in the ΔmlaA/Plac::pldA strain, the vancomycin MIC was the same as the ΔmlaA strain. However, when PldA was overexpressed, the strain’s polymyxin B sensitivity increased two- and four-fold in comparison to the ΔmlaA mutant and the WT strain, respectively (Table 2). Finally, follow-up agar dilution MIC assessment confirmed the fold decrease in MIC for each strain for polymyxin B and vancomycin but not for ampicillin. Complementation with MlaA was sufficient to restore resistance to polymyxin B but not to vancomycin (Table 2 in S1 Text). In all cases, the MICs were higher by agar dilution than by Etest, an effect noted previously [45].
Loss of MlaA results in reduction of gonococcal colony size
Our antibiotic susceptibility testing indicated ΔmlaA exhibited an outer membrane defect that was exacerbated upon overproduction of PldA in the presence of polymyxin B. To examine these effects more closely, viability was assessed for WT, ΔmlaA, ΔmlaA/Plac::mlaA, and ΔmlaA/Plac::pldA grown on solid medium supplemented with 800 U/mL (~84 μg/mL) polymyxin B and either 0 or 0.5 mM IPTG for the expression of MlaA or PldA. Visual inspection revealed an apparent decrease in ΔmlaA viability from the -5 to the -3 dilution during exposure to polymyxin B (Fig 6B, top panels). Upon examination with a stereo-microscope, colonies of the ΔmlaA mutant were noticeably smaller than those of the WT, although colony counting revealed no significant difference in CFUs compared to the absence of polymyxin B for the ΔmlaA mutant (106.2% ± 6.8 for WT compared to 73.6% ± 24.5 for ΔmlaA). In the absence of PldA induction, the viability of the ΔmlaA/Plac::pldA strain was not significantly different from that of the WT when exposed to polymyxin B (54.2% ± 17.42 for ΔmlaA/Plac::pldA). However, upon pldA overexpression in the ΔmlaA background, survival was significantly lower than WT bacteria (117.2 ± 5.7 for WT; 0.04% ± 0.01 for ΔmlaA/Plac::pldA), dropping by 99.96% compared to cells cultured in the absence of polymyxin B (Fig 6C).
Measurement of colony diameters (Fig 6D, left column) revealed that lack of MlaA resulted in significantly decreased colony size, even in the absence of the antimicrobial peptide (282.7 ± 2.66 μm for WT, 223.2 ± 2.19 μm for ΔmlaA). This phenotype was not reversed in the ΔmlaA mutant by expression of MlaA from a heterologous location (219.1 ± 2.91 μm; Fig 6E, left panel). The difference in colony size between WT and ΔmlaA was aggravated in the presence of polymyxin B (148.6 ± 2.35 μm for WT, 63.28 ± 1.02 μm for ΔmlaA; Fig 6D, right column), and was partially restored in the ΔmlaA/Plac::mlaA strain (115.4 ± 2.45 μm; Fig 6E, right panel). Analysis of LOS isolated from WT, ΔmlaA, ΔmlaA/Plac::mlaA, and with PldA at either native levels or overproduced in ΔmlaA/Plac::pldA bacteria in the presence or absence of polymyxin B revealed that neither loss of MlaA nor overproduction of PldA in the ΔmlaA background resulted in alterations to LOS abundance or migration (Fig 6F). Likewise, the presence of the antimicrobial peptide had no effect on LOS in any of the strains tested. Thus, the polymyxin B phenotype was not due to LOS defects.
Our experiments provided the first evidence that in N. gonorrhoeae, absence of MlaA affects outer membrane permeability to compounds acting against the cell wall, which can be partly rescued by the action of PldA, and alters colony morphology. Further, the relatively low levels of MlaA present in the ΔmlaA/Plac::mlaA strain partially alleviated the polymyxin B sensitivity phenotype resulting from this defect (Fig 3E). We conclude that MlaA is more important to the bacteria during exposure to cell envelope stress conditions than under standard laboratory growth.
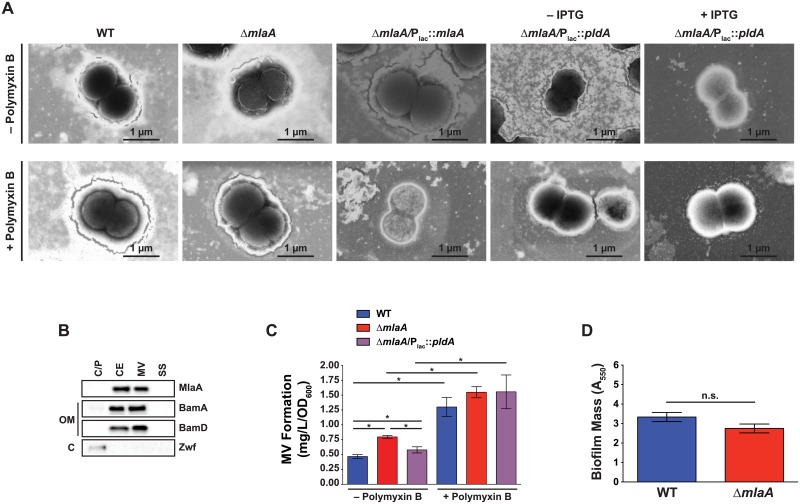
Gonococcal cell morphology is unaltered in the absence of MlaA
To determine whether the loss of MlaA either alone or combined with PldA expression would alter cell morphology and thus result in increased sensitivity to polymyxin B, we employed transmission electron microscopy. Cells from the ΔmlaA mutant typically appeared identical to WT cells, although the mutant occasionally exhibited ruffled membranes (Fig 7A, top row). Additionally, the ΔmlaA/Plac::pldA strain was indistinguishable from WT, either in the presence or absence of PldA overexpression (Fig 7A, top row). To determine whether any of the strains exhibited morphological differences in the presence of polymyxin B, we also imaged diplococci collected from cultures supplemented with the antimicrobial peptide. The presence of polymyxin B did not alter the overall morphology of any of the strains examined (Fig 7A, bottom row). Finally, we occasionally observed numerous blebs on cell surfaces, as shown for WT bacteria cultured without polymyxin B and ΔmlaA bacteria collected from both conditions (Fig 7A).
Fig 7. Investigations of MlaA effects on cell structure, membrane vesicles, and biofilm formation.
(A) Strains as indicated were cultured in liquid medium without (top row) or with (bottom row) polymyxin B until approximately mid-logarithmic growth. ΔmlaA/Plac::pldA was cultured in the presence or absence of 0.5 mM IPTG, as indicated. Bacteria were subsequently washed twice with PBS, spotted onto 300 mesh copper grids, negatively stained with phosphotungstic acid, and imaged using scanning electron microscopy. (B) Cytoplasmic/periplasmic (C/P), cell envelope (CE), membrane vesicle (MV), and soluble supernatant (SS) subcellular fractions of WT FA1090 collected under standard aerobic conditions were prepared and normalized based on protein concentration, separated by SDS-PAGE, and probed with indicated antisera. (C) MVs collected by ultracentrifugation of culture supernatants derived from strains indicated were quantified by protein concentration (n = 6 for WT and ΔmlaA for − polymyxin B condition; n = 3 for all others; mean ± SEM). (D) WT FA1090 and ΔmlaA bacteria were suspended to an OD550 of 1.5 in GCBL, added to 96 well microtiter plates, and cultured without shaking in 5% CO2 at 37 °C for 24 h. Planktonic bacteria were removed and biofilms were washed with PBS. Biofilms were allowed to dry at room temperature, then stained in 0.1% crystal violet in 2% ethanol. After staining, wells were washed with PBS and dried. Biofilms were dissolved in 30% acetic acid and quantified by A550 measurement. Biofilm experiments were performed 12 times, each with 3 or 4 technical replicates, for a total of 46 datapoints. Mean ± SEM is presented. IPTG, isopropyl β-D-thiogalactopyranoside; C/P, cytoplasmic/periplasmic; C, cytoplasm; CE, cell envelope; OM, outer membrane; MV, membrane vesicle; SS soluble supernatant; SDS-PAGE, sodium dodecyl sulfate-polyacrylamide gel electrophoresis; OD550, optical density at 550 nm; A550, absorbance at 550 nm, GCBL, gonococcal base liquid medium.
MlaA localizes to the cell envelope and naturally released membrane vesicles
We identified MlaA within CE and MV fractions isolated from four different N. gonorrhoeae strains in proteomic investigations using isobaric Tagging for Relative and Absolute Quantification coupled with Mass Spectrometry [22]. To validate these results and to determine to which cellular compartment(s) N. gonorrhoeae MlaA associates, we performed an immunoblotting analysis of subcellular fractions using anti-MlaA antiserum and control antisera against the periplasmic-facing lipoprotein member of the BAM complex, BamD [46]; BamA [25, 33]; and the cytoplasmic enzyme Zwf [47–49]. This analysis revealed that none of the proteins were detected in the supernatant (SS). MlaA exclusively localized to the CE and MV fractions, similar to BamD. BamA was detected primarily in the CE and MV fractions, but was also found in small amounts in the cytoplasmic/periplasmic fraction, which reflects the presence of five periplasmic polypeptide transport associated domains [25, 33]. Finally, as expected [49], Zwf was detected solely in the cytoplasmic/periplasmic fraction (Fig 7B).
Cell envelope and membrane vesicle composition is altered in the ΔmlaA mutant
The presence of membrane blebs on the surface of ΔmlaA cells both under permissive and stress conditions (Fig 7A), combined with the proposed role of MlaA in vesicle biogenesis [13], prompted us to assess whether this mechanism was conserved in N. gonorrhoeae. We examined vesicle formation by WT, ΔmlaA, and ΔmlaA/Plac::pldA bacteria during standard growth in liquid medium, as well as under polymyxin B exposure. Indeed, quantitation of MVs revealed that the ΔmlaA mutant produced significantly more vesicles than WT under standard conditions (0.80 ± 0.02 mg L-1OD600-1 compared to 0.47 ± 0.03 mg L-1OD600-1 for WT, Fig 7C). Overexpression of PldA partially decreased MV production, although the ΔmlaA/Plac::pldA strain still released significantly more MVs than WT bacteria (0.58 ± 0.03 mg L-1OD600-1, Fig 7C). However, in the presence of polymyxin B, all three strains produced significantly more MVs than under non-stress conditions (2.8-, 1.9-, and 2.7-fold increases for WT, ΔmlaA, and ΔmlaA/Plac::pldA, respectively). No significant differences were observed in MV secretion between strains during polymyxin B exposure (Fig 7C). The hypervesiculation phenotype of the ΔmlaA mutant did not translate into increased biofilm formation (Fig 7D, S6 Fig) despite the fact that gonococcal biofilms are primarily membranous material generated by the release of MVs [50].
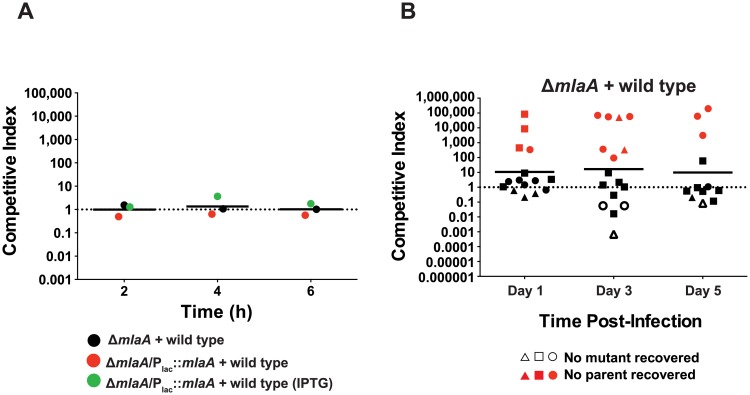
MlaA reduces gonococcal fitness in the female mouse lower genital tract
The increased blebbing, sensitivity to antimicrobial peptides, and the differential expression pattern of MlaA during iron deprivation and anaerobiosis led us to test whether the lack of MlaA impacts N. gonorrhoeae survival during infection. We chose to establish a competitive index (CI) as it provides a relative measure of bacterial fitness in comparison to a reference strain (in this case, WT bacteria) that takes the starting inoculum into account (see Materials and methods for calculation). A CI equal to 1 indicates that both strains are comparably fit whereas CI values greater or lower than 1 show that the mutant is able to outcompete the WT strain or displays decreased fitness, respectively. We first established that MlaA does not affect bacterial fitness using in vitro competitive experiments (Fig 8A) then used the female mouse model of gonococcal lower genital tract infection as a measure of in vivo fitness [51, 52]. In three biological replicates, each with at least seven mice, we observed a 9.8- to 16.9-fold increase in the competitive index for the ΔmlaA strain. Additionally, only mutant bacteria were isolated from several mice at each time point (Fig 8B). Expectedly, the same phenotype was observed in the ΔmlaA/Plac::mlaA strain (S7 Fig) due to the inability to restore MlaA expression to WT levels in this complemented strain (Fig 3E).
Fig 8. MlaA influences gonococcal fitness in vivo.
(A) In vitro competition assays were performed by combining WT FA1090 bacteria with approximately equal numbers of ΔmlaA or ΔmlaA/Plac::mlaA (~106 CFU total bacteria). Competitions were carried out in liquid medium, and output CFUs were assessed at 2, 4, and 6 h post-inoculation. Competitions with the complemented strain were performed in liquid medium both with and without IPTG. (B) Female BALB/c mice were inoculated intravaginally with approximately equal numbers of CFUs of WT and ΔmlaA bacteria (~106 CFU total N. gonorrhoeae; 7 mice per group). Vaginal swabs were taken on days 1, 3, and 5 post-infection and were cultured for CFU/mL enumeration on solid media containing streptomycin (total bacteria) or media containing streptomycin and kanamycin (ΔmlaA bacteria). Experiments were repeated three times and results are expressed as the geometric mean of the competitive index (CI): [mutant CFU (output) / WT CFU (output)] / [mutant CFU (input) / WT CFU (input)]. A CI > 1 indicates that the mutant was more fit during the competition. 1 CFU was assigned for any strain not recovered from an infected mouse. IPTG, isopropyl β-D-thiogalactopyranoside; CFU, colony forming unit.
Quantitative proteomic profiling reveals significant differences in the cell envelope and membrane vesicles upon loss of MlaA
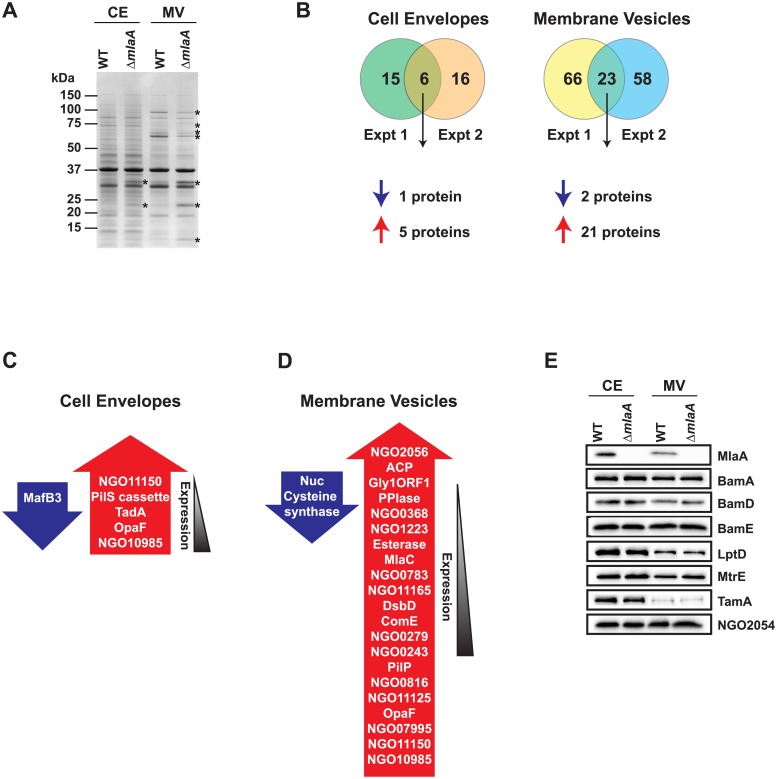
We hypothesized that the enhanced fitness of the ΔmlaA strain may be due to increased MV formation, as well as specific changes to CE and MV subproteomes (Fig 9A). To quantitatively examine these alterations, we utilized Tandem Mass Tag (TMT) 6plex isobaric mass tags to label trypsinized proteins from CE and MV fractions collected from WT and ΔmlaA bacteria on two separate occasions. Proteins were considered differentially expressed in the mutant if the ratio of ΔmlaA protein abundance to WT protein abundance was greater than 1.5-fold (increased in ΔmlaA) or less than 0.67-fold (decreased in ΔmlaA). Differentially expressed proteins in CE and MV fractions are listed in Table 3 and Fig 9C and 9D, and proteomic data are presented in S2 and S3 Files, respectively. All MS data are also available via ProteomeXchange with identifier PXD008673.
Fig 9. Proteomic investigations of MlaA influence on cell envelope and membrane vesicles.
(A) CE and MV fractions isolated from WT FA1090 and isogenic knockout ΔmlaA were normalized based on protein concentration, separated by SDS-PAGE, and proteins were visualized by coomassie staining. The migration of a molecular weight marker is shown on the left in kDa. Proteins that appeared differentially abundant in the ΔmlaA mutant by visual inspection are labeled with an asterisk. (B) Trypsinized CE and MV proteins from WT and ΔmlaA were labeled with TMT6plex isobaric mass tags, fractionated by strong cation exchange and reverse phase chromatography, and subjected to peptide identification by tandem mass spectrometry. The number of differentially abundant proteins in the ΔmlaA CE or MV protein profiles is noted in the Venn diagrams. (C, D) Lists of differentially abundant proteins in the CE (C) or MVs (D) of the ΔmlaA mutant. Proteins in blue arrows are downregulated in the mutant, while those listed in red arrows are upregulated in the mutant. Proteins are arranged by the magnitude of the mutant:WT ratio. (E) Validation of quantitative proteomics results. CE and MV fractions from WT FA1090 and ΔmlaA were normalized by protein concentration, separated by SDS-PAGE, and probed with antisera against indicated proteins. SDS-PAGE, sodium dodecyl sulfate-polyacrylamide gel electrophoresis; TMT, tandem mass tag.
Table 3. Differentially expressed proteins in ΔmlaA cell envelopes and membrane vesicles identified in two biological replicate experiments.
| Accession | Protein Name | Locus | Molecular Mass (kDa) | Expt. 1a,b | Expt. 2a,b | Informationc |
|---|---|---|---|---|---|---|
| Cell Envelopes | ||||||
| Q5F6H3 | Septum formation inhibitor MafB3 | NGO_1585 | 63.2 | 0.50 | 0.51 | MafB3, a toxin present on the maf genomic island 1. Contact dependent growth inhibition system. Contains intein domain. endoU ribonuclease. System also encodes immunity protein. Increases fitness in competition assay [53]. |
| A0A0H4IWJ8 | Uncharacterized protein | NGO_11150 | 10.2 | Pilin. Likely pilS. Involved in antigenic variation of PilE through recombination of pilE with “silent” copy of pilS. pilS loci produce sense and antisense RNA. [54, 55] | ||
| A0A0H4ISA9 | Large pilS cassette protein | NGO_10975 | 24.2 | Pilin. Involved in antigenic variation of PilE through recombination of pilE with “silent” copy of pilS. pilS loci produce sense and antisense RNA [54, 55]. | ||
| Q5F851 | tRNA-specific adenosine deaminase TadA | NGO_0941 | 25.9 | Catalyzes the deamination of adenosine to inosine at the wobble position 34 of tRNA(Arg2). Binds 1 zinc ion per subunit (Uniprot). | ||
| A0A0H4IS55 | Opacity protein Opa54 | NGO_04980 | 26.2 | Opacity associated protein (also known as OpaF). Binds to CD66a and CD66e receptors on apical side of T84 cells. Mediates attachment to PMNs and monocytes. Recognized by CEACAM1 and CEACAM5. Receptor specificity studied in strain MS11 [56–59]. | ||
| A0A0H4IWJ0 | Uncharacterized protein | NGO_10985 | 15.0 | PilA (FtsY). Signal recognition particle for protein translocation. [60] | ||
| Membrane vesicles | ||||||
| Q5F832 | Thermonuclease | NGO_0969 | 24.7 | 0.64 | 0.65 | Staphylococcal nuclease-like. Allows GC to degrade and escape from NETs. Involved in biofilm structuring [61, 62]. |
| Q5F9Q2 | Cysteine synthase | NGO_0340 | 32.7 | 0.64 | 0.67 | Member of pathway that synthesizes cysteine. May induce protective immune response in N. meningitidis, with subpopulation of cells exhibiting surface exposure, despite typically cytoplasmic function [63]. |
| Q5F574 | ABC transporter substrate-binding protein | NGO_2056 | 36.3 | Thiamine transport system substrate binding protein. Upregulated in response to hydrogen peroxide according to transcriptomics. May be transcriptionally linked to NGO2057 [64]. | ||
| Q5F5E8 | Adhesin complex protein | NGO_1981 | 20.4 | Upregulated under anaerobiosis and on exposure to hydrogen peroxide. Adhesin complex protein. Lysozyme inhibitor [64–67]. | ||
| Q5F9N5 | Gly1ORF1 | NGO_0358 | 15.7 | Knockout of Gly1 was more toxic to fallopian cells [68]. Annotated as chitinase. May enhance virulence by binding to glycoproteins or glycolipids that contain GlcNAc [69]. | ||
| Q5F6A4 | Peptidylprolyl isomerase | NGO_1656 | 31.5 | Meningococcal homolog described as cell binding protein, sera from colonized individuals cross-reacted with NMB0345. [70] | ||
| Q5F9M5 | Uncharacterized protein | NGO_0368 | 13.8 | Contains DUF302 domain of unknown function (KEGG) | ||
| Q5F7F5 | Membrane protein | NGO_1223 | 24.1 | Contains DUF3108 domain of unknown function (KEGG) | ||
| Q5F5H6 | Esterase | NGO_1949 | 31.4 | Uncharacterized | ||
| Q5F520 | MlaC | NGO_2119 | 21.1 | Involved in maintenance of lipid asymmetry; periplasmic component of Mla system. Transposon insertion into NGO2119 decreases pilin antigenic variation, DNA repair, and DNA transformation [6, 71] | ||
| Q5F8J0 | Uncharacterized protein | NGO_0783 | 18.5 | Uncharacterized | ||
| A0A0H4IVN2 | Uncharacterized protein | NGO_11165 | 13.9 | Likely PilA (FtsY). Signal recognition particle for protein translocation [60]. | ||
| Q5F823 | Thiol:disulfide interchange protein DsbD | NGO_0978 | 64.9 | Uses cytoplasmic thioredoxin to reduce DsbC. Expression is controlled by MisR/MisS two-component system [72]. | ||
| Q5F5M0 | DNA-binding competence protein 2 | NGO_1304 | 10.1 | Competence protein ComE. DNA binding protein necessary for DNA uptake. Binds without sequence specificity. Deletion does not affect piliation [73]. | ||
| Q5F9W6 | Uncharacterized protein | NGO_0270 | 17.4 | Uncharacterized protein. No meningococcal homolog. Closest match N. lactamica hypothetical protein. | ||
| Q5F9Z1 | Uncharacterized protein | NGO_0243 | 19.7 | Contains DUF2059 domain of unknown function. May have a Correia repeat enclosed element disrupting the coding sequence [74]. | ||
| Q5FAD1 | Pilin assembly protein | NGO_0095 | 20.1 | Pilus assembly protein PilP. Ubiquitously expressed in cell envelope, upregulated in response to normal human serum, iron deprivation, anaerobiosis [25]. | ||
| Q5F8F9 | Uncharacterized protein | NGO_0816 | 10.8 | Contains DUF4124 domain of unknown function. Hypothetical protein. Closest match is hypothetical protein from N. lactamica. N. meningitidis homolog has domain with homology to C-terminal proteolytic portion of LonC protease (KEGG). | ||
| A0A0H4ITA9 | Uncharacterized protein | NGO_11125 | 10.0 | Pilin. Likely PilE. Forms pilus fiber [75]. | ||
| A0A0H4IS55 | Opacity protein Opa54 | NGO_04980 | 26.2 | Opacity associated protein (also known as OpaF). Binds to CD66a and CD66e receptors on apical side of T84 cells. Mediates attachment to PMNs and monocytes. Recognized by CEACAM1 and CEACAM5. Receptor specificity studied in strain MS11 [56–59]. | ||
| A0A0H4IVG5 | Uncharacterized protein | NGO_07995 | 13.6 | Pilin. Likely PilS. Involved in antigenic variation of PilE through recombination of pilE with “silent” copy of pilS. pilS loci produce sense and antisense RNA [54, 55]. | ||
| A0A0H4IWJ8 | Uncharacterized protein | NGO_11150 | 10.2 | Pilin. Likely PilS. Involved in antigenic variation of PilE through recombination of pilE with “silent” copy of pilS. pilS loci produce sense and antisense RNA [54, 55] | ||
| A0A0H4IWJ0 | Uncharacterized protein | NGO_10985 | 15.0 | Likely PilA (FtsY). Signal recognition particle for protein translocation [60]. |
aRatios represent fold change in each experiment.
bRatios for upregulated proteins are shown in red.
cInformation gathered from bioinformatics tools and literature searches.
Of the 884 CE proteins identified in both replicates (S2 File), 21 and 22 were differentially abundant in the mutant in the first and second experiments, respectively, with 6 common proteins between the two experiments (Fig 9B, left, and Fig 9C). In this group, five proteins showed increased levels and one protein was decreased in the mutant. As expected from our previous proteomic mining of MVs [22], fewer proteins were present in this sub-proteome fraction (568; S3 File). However, the MV protein profile was more dramatically affected by the loss of MlaA than the CE proteome, similar to the qualitative results of coomassie staining (Fig 9A). In the first and second biological replicate, 89 and 81 proteins were differentially expressed in the mlaA null strain, respectively, with 23 proteins in common (Fig 9B, right, and Fig 9D). Of the common differentially expressed proteins, 21 increased in abundance in the absence of MlaA, and two proteins showed decreased levels. Additionally, the amounts of NGO2119 (MlaC) were augmented in the MVs isolated from ΔmlaA, whereas a corresponding increase was not observed in the CE fraction. Importantly, this result demonstrated that no immediate upstream or downstream effects were introduced to the NGO2116-NGO2124 operon (Fig 2C) during construction of the ΔmlaA mutant.
Subsequently, we performed an immunoblot analysis of CE and MV fractions isolated from WT and ΔmlaA using available antisera against eight outer membrane proteins including MlaA; BamA, D, and E; LptD; MtrE; TamA; and NGO2054 [25, 76]. As expected, MlaA was not detected in the CE or MVs of ΔmlaA. None of the other proteins examined were differentially regulated in the ΔmlaA CE or MVs (Fig 9E), which further corroborated the quantitative proteomic investigation (S2 and S3 Files).
One of the proteins that was most highly abundant in the ΔmlaA CE compared to WT was the tRNA adenosine deaminase TadA. This essential protein catalyzes an adenosine-to-inosine transition in RNA. A recent report provided the first evidence of mRNA modification in prokaryotes and demonstrated that the modifications were mediated by TadA, although TadA was originally thought to act exclusively on tRNA. E. coli TadA modifies over 250 proteins, including cell envelope proteins BamA, TamA, and PldA [77]. The tyrosine-to-cysteine transitions induced by TadA modification altered the toxicity of one of the target proteins, the toxin HokB [77], which may suggest that the biological activities of gonococcal TadA substrates are affected by TadA upregulation in the ΔmlaA mutant.
The increased presence of protein products with homology to pilS (NGO10975, NGO11150, and NGO07995; Table 3) in the mutant CE and MVs may indicate that pilin antigenic variation is enhanced in mlaA null bacteria. pilS cassettes are transcriptionally silent loci involved in antigenic variation of PilE through RecA-mediated recombination [54]. Also upregulated in the ΔmlaA CE and MVs was the opacity-associated protein Opa54 (NGO04980; OpaF). Opa proteins interact with members of the carcinoembryonic antigen-related cell adhesion molecule (CEACAM) family of receptors to mediate bacterial attachment to epithelial cells, neutrophils, and monocytes [56–59].
In addition to pilus-related proteins, several other potential virulence factors within the MVs of the ΔmlaA mutant were elevated. Across the two experiments, the Neisseria adhesin complex protein (ACP) was present in higher quantities in the mutant MVs by an average of 1.7-fold. ACP is involved in meningococcal adhesion to human cells [67] and possesses a secondary function as a lysozyme inhibitor [66]. Originally discovered in a screen for gonococcal hemolysins [68], Gly1ORF1 (NGO0358) was also increased 1.7-fold in the ΔmlaA MVs. The ngo0358 locus is annotated as a putative chitinase. While overexpression of gly1ORF1 has not been studied in N. gonorrhoeae, chitinases play roles in the virulence of other bacterial species by binding to the N-acetyl-glucosamine moiety of glycolipids and glycoproteins [69].
Together, our studies are the first to address the expression and function of MlaA in gonococcal physiology and pathogenesis, revealing that the loss of MlaA not only affects colony morphology, CE and MV subproteomes, resistance to certain antimicrobials, and MV formation, but also increases the fitness of N. gonorrhoeae under in vitro conditions relevant to infection and in the murine female genital tract. Cumulatively, our findings highlighted a new mechanism of N. gonorrhoeae pathogenesis and a better understanding of the function(s) of MlaA in this clinically relevant pathogen.
Discussion
The asymmetry of the Gram-negative outer membrane is responsible for its formidable barrier function. When this asymmetry is disrupted, phospholipids accumulate in the outer leaflet and the cell becomes more vulnerable to both hydrophilic and lipophilic antimicrobial compounds [3, 6]. Thus, bacteria have developed several systems to maintain the asymmetry of the outer membrane. Two systems, PagP and PldA, destroy outer-leaflet phospholipids, while the Mla system removes intact phospholipids and re-integrates them into the inner membrane [6]. MlaA, located within the outer membrane in complex with OmpF, forms a channel through which the head groups of phospholipids are able to travel [10]. Our bioinformatics searches did not identify a PagP homolog in the gonococcal genome, indicating that N. gonorrhoeae relies solely on PldA and the Mla system to maintain phospholipid homeostasis. This aspect of bacterial physiology has not been well studied in Neisseria, and reports on PldA mainly focus on its role during autolysis [78–80].
Bioinformatic analyses revealed the existence of two separate classes of MlaA homologs (Fig 2A). N. gonorrhoeae MlaA is a member of the class composed primarily of proteins lacking a lipoprotein signal peptide, with the exception of K. pneumoniae and F. tularensis. In vivo assessments with MlaA (VacJ) knockout strains revealed virulence defects in members of the lipoprotein-containing phylogenetic cluster: S. flexneri, H. parasuis, and S. enterica enterica serovar Typhimurium [11, 13–15]. In contrast, P. aeruginosa deficient in VacJ, which lacks a lipoprotein signal peptide, was more virulent than WT bacteria [12]. The opposing results suggest that MlaA may play a different moonlighting role(s) in certain aspects of pathogenesis for bacteria, depending on its association with the CE.
We also provide the first report of differences between the genetic location and organization of mlaA in N. gonorrhoeae, N. meningitidis, and N. lactamica compared to those in other bacteria. In the Neisseria species examined, mlaA appears to be part of a polycistronic operon composed of the other components of the Mla system, while mlaA is physically separated from the other Mla members in E. coli (Fig 2C and S2 Fig). Therefore, Neisseria may employ a different regulation strategy for MlaA. Due to its genomic organization, complementation of individual mla components is technically challenging, if not entirely impossible, without a greater understanding of mla system regulation. This hindrance was illustrated by low levels of MlaA in the ΔmlaA/Plac::mlaA strain regardless of the high amount of the inducer used (Fig 3E, S4 Fig). The little amount of MlaA was sufficient to return mutant colonies to nearly WT size during polymyxin B exposure (Fig 6B, 6D and 6E), but was not able to complement the competitive infection phenotype (Fig 8A and 8B; S6 Fig). The difficulty of complementing knockouts in a polycistronic operon, even in a fairly well-studied system in which many of the regulatory elements are already known, has been recognized [81–83]. For instance, in the soil bacterium Agrobacterium tumefaciens, a virulence plasmid, pTi, carries an operon composed of 11 virB genes that are each essential for tumor formation in plants [84–86]. A complementation study to examine each member of the virB operon revealed additional regulatory requirements for six of the 11 genes, including switching the constitutive (in the A. tumefaciens system) lacZ promoter for the native virB promoter for VirB1 and VirB2, adding 55 or 230 bp of upstream sequence for VirB6 and VirB9, or co-expressing VirB7 and VirB8 on the same complementation plasmid [86].
Mla is a relatively recently discovered protein complex and limited information is available regarding expression of the Mla components, including MlaA [10, 13]. To address this gap, we examined MlaA expression patterns throughout the growth of WT N. gonorrhoeae in liquid media, during exposure to host-relevant conditions, and in a panel of diverse Neisseria (Figs 4–5). We demonstrated that the amount of MlaA was decreased in the absence of iron and increased during anaerobic growth (Fig 5C and 5G). The down-regulation in the absence of iron is consistent with the Fur-dependent vacJ transcription pattern in H. influenzae during in vitro growth and in vivo in a mouse model of nasopharyngeal colonization [13]. While MlaA has not been described as part of the N. gonorrhoeae iron regulon, transcription of MlaF (NGO2116) decreases under iron restriction in a Fur-dependent manner [87], which suggests that the entire Mla system may be under Fur transcriptional control in the gonococcus. Our investigation into the effects of Fur on MlaA suggest that Fur’s influence has diminished over the intervening five genes. Free iron concentrations are maintained in the attomolar range (10−18 M) in bodily fluids to prevent microbial growth, and infection induces lactoferrin secretion to further restrict iron availability [88], including in the reproductive tract. Transcriptomic studies of gonococci isolated from active infections have shown that mlaA is transcribed during cervical infections after recent exposure to an infected male partner, and mlaA transcripts are typically lower during infection than during growth in defined medium [89]. Together, these lines of evidence suggest that the downregulation of mlaA in response to iron restriction, but not the complete abrogation of expression, is part of the infection strategy employed by the gonococcus.
Overexpression of the phospholipase PldA in the ΔmlaA background reduced MV formation but strongly enhanced bacterial vulnerability to polymyxin B (Figs 7C and 6B and 6C, respectively). An identical experiment has not been performed in E. coli. Differences in phospholipid composition between N. gonorrhoeae and E. coli explain our results (Table 4). E. coli membranes contain ~87% phosphatidylethanolamine (PE) and 4.7% phosphatidylglycerol (PG) in late-stage cultures [90], while PE and PG comprise 69% and 19% of the membrane of N. gonorrhoeae, respectively [91]. In both species, PldA predominantly destroys PE [79, 92]. In contrast, the Mla system does not appear to exhibit a preference for specific phospholipids [93]. In N. gonorrhoeae, only the Mla system and PldA contribute to outer membrane asymmetry as no PagP homolog exists. Thus, in our proposed model, in the absence of MlaA, with native PldA levels, the overall phospholipid composition is largely preserved [13], but the outer membrane will contain phospholipids that have invaded the CE outer leaflet (Fig 1B). PldA dimerization and activation will likely increase upon detection of perturbed phospholipid homeostasis [8], although evidence from E. coli suggests that PldA expression will not be altered in the absence of membrane stress [6]. The enhanced activation of endogenous PldA levels may alter the phospholipid profile slightly. However, upon PldA overproduction in the ΔmlaA mutant, the substrate preference of PldA towards PE will result in a higher abundance of PG within the surface of N. gonorrhoeae (Fig 1C; Table 4). Polymyxin B preferentially targets PG [94, 95]. Gonococci overexpressing PldA in the absence of MlaA are therefore more sensitive to the antimicrobial peptide.
Table 4. Phospholipid composition of N. gonorrhoeae and E. coli membranes.
| Phospholipid | N. gonorrhoeae [91] | E. coli [90] |
|---|---|---|
| Phosphatidylethanolamine (PE) | 69% | 87% |
| Phosphatidylglycerol (PG) | 19% | 4.7% |
| Cardiolipin | 0.8% | 7.1% |
| Phosphatidylcholine (PC) | 11% | N.D.a |
| Phosphatidic acid | N.D.a | 0.8% |
aN.D., Not detected
Downregulation and deletion of VacJ in H. influenzae and V. cholerae increased MV formation, and accumulation of phospholipids in the outer leaflet has been proposed as a general mechanism of MV biogenesis [13]. Corroborating this suggestion, the N. gonorrhoeae ΔmlaA strain produced significantly more MVs than WT bacteria and PldA overproduction partly reduced their amounts (Fig 7C). However, dramatic increases in MV release for both WT and ΔmlaA bacteria under polymyxin B stress (Fig 7C) provided evidence that invading phospholipids are not the primary factor in MV biogenesis.
Why do we observe increased fitness of the ΔmlaA during competitive infection in the surrogate host? We propose that it is due to the altered CE and MV protein contents (Fig 9A). Quantitative proteomics of these fractions revealed alterations in proteins with significant implications in bacterial physiology and virulence (Fig 9B, 9C and 9D). Among the most upregulated proteins in the ΔmlaA CE was an essential enzyme, TadA, which edits mRNA without changing its expression and recodes protein sequences, potentially affecting their function and cell physiology [77]. Our proteomic profiling revealed a previously unrecognized link between phospholipid homeostasis and RNA editing, which should be examined in future studies, in addition to the role of TadA-mediated protein modification in bacterial pathogenesis. Further, several adhesins were also elevated in the CE and MV fractions of the ΔmlaA mutant (Fig 9C and 9D, Table 3). Of these, adherence mediated by pili and Opa proteins is host-restricted, although a CEACAM receptor-independent advantage is observed for Opa-positive gonococci in the mouse model [51, 96]. Elevated Opa levels in the ΔmlaA mutant may therefore have contributed to the mutant’s enhanced fitness. Heightened pilin antigenic variation in the absence of MlaA may also have played a role. However, one or more of the other proteins may contribute more substantially to the increased fitness of the mutant in the mouse model (Fig 8B), possibly through elevated ACP acting as a lysozyme inhibitor [97, 98] within the MVs [56–59, 67]. MVs have been shown to act as decoys against components of the innate immune system, by adsorbing antimicrobial peptides, for example [99], and are often packages for virulence factors [100]. The ΔmlaA mutant appears to exploit both of these functions, as illustrated by the presence of heightened levels of ACP within MVs, which could protect the bacteria from lysozyme attack [66, 97]. We have not assessed lysozyme sensitivity in the ΔmlaA mutant, as two gonococcal lysozyme inhibitors, ACP and SliC, are responsible for lysozyme resistance and compensate for each other in vitro [97, 98]. However, lack of SliC was sufficient to significantly impact bacterial fitness in the mouse genital tract [97]. Thus, the loss of MlaA results in multifactorial alterations to gonococcal CE and MV protein composition that likely act in concert to enhance the fitness of the ΔmlaA mutant in the mouse model. The primary function of MlaA is in cell envelope biogenesis and homeostasis. However, alterations to the MlaA cellular pool in response to host conditions would modulate the CE and MV protein composition, as well as the amount of blebs released.
Our study presents MlaA as an intriguing protein with an inverse effect on gonococcal pathogenesis. We propose that N. gonorrhoeae adjusts virulence through changes in MlaA levels in response to iron availability in the host, as both the human [88] and murine [101] genital tracts are iron-restricted. Downstream effects of MlaA depletion involve alterations to the CE and MV protein composition, including elevated levels of known and potential virulence factors, as well as the possibility of post-translational protein modification. It is exciting to consider that other host/bacterial effectors may also be involved in MlaA-triggered MV biogenesis and in fine-tuning the bacteria-host interaction.
Materials and methods
Bacterial strains and growth conditions
For this study, laboratory strain FA1090 [102] and contemporary clinical isolate WHO X [26] were used as wild type (WT) strains. Isogenic null mutants of ngo2121 were previously constructed in both strain backgrounds by replacement of the locus with the kanamycin resistance cassette [22, 23], and a complemented strain with ngo2121 under the control of the Plac promoter was also previously constructed in the FA1090 strain background [23]. For this study, we also generated a conditional knockout of the Fur transcriptional regulator, Δfur/Plac::fur, described below. To analyze expression of MlaA in clinical strains, we used a panel of isolates collected from two public health clinics in Baltimore from 1991 to 1994 (LGB1, LG14, LG20, LG26); the Public Health-Seattle & King County Sexually Transmitted Disease clinic from 2011 to 2013 (UW01-UW13); and the 2016 WHO reference strains [25]. Frozen stocks of N. gonorrhoeae strains stored at -80 °C were streaked onto gonococcal base agar solid medium (GCB, Difco) supplemented with Kellogg’s supplements I and II diluted 1:100 and 1:1,000, respectively [25]. After incubation for 18–20 h at 37 °C in a 5% CO2 atmosphere, colonies were subcultured onto GCB. Transparent piliated cells were used for transformation, while transparent, non-piliated variants were used for all other experiments. Unless otherwise specified, after 18–20 h of subsequent culturing as described above, colonies were collected from solid medium with a polyester-tipped sterile applicator (Puritan) and suspended to a final OD600 of 0.1 in gonococcal base liquid medium (GCBL) supplemented with 0.042% sodium bicarbonate and Kellogg’s supplements as above. Bacteria were then cultured at 37 °C with agitation (220 rpm) for 3 h, diluted to a final OD600 of 0.1 in supplemented GCBL, and cultured as previously.
E. coli NEB5α was used for genetic manipulations, while E. coli BL21(DE3) was used for heterologous expression of MlaA and DsbA for protein purification. E. coli was maintained at 37 °C in Luria-Bertani (LB, Difco) media or LB agar supplemented with the appropriate antibiotic. Concentrations of antibiotics used are as follows: N. gonorrhoeae kanamycin (40 μg/mL for FA1090, 50 μg/mL for WHO X) and erythromycin (0.5 μg/mL for FA1090, 4 μg/mL for WHO X); E. coli kanamycin (50 μg/mL).
DNA manipulations
MlaA120-277 was amplified from purified FA1090 genomic DNA using primers MlaA-trunc-F, TTCATCCATATGCCCGACAATAAAAACACTTTGG and MlaA-trunc-R, TTCATCCTCGAGGGGTTGTGTTCCAGGTTG. The PCR product was digested with NdeI and XhoI restriction enzymes (New England Biolabs; restriction sites are underlined), inserted into similarly-digested pET28a to place a 6 × His-tag on the C-terminus, and transformed into E. coli BL21(DE3).
The gene encoding dsbA missing the signal peptide was amplified using primers DsbA-f, GACTCCATGGTGACGGAAGGGGAAGACT and DsbA-r, GACTAAGCTTCGGCTATTTCTGTACAGCAG. The subsequent PCR product was digested with NcoI and HindIII, as indicated, and ligated into similarly cut pRSF-NT to create a tobacco etch virus protease-cleavable C-terminal-6 × His-tagged fusion. PldA was amplified using primers PldA-F, GATCTTAATTAAAAAATGCCGTTTGAAAACCAATATG and PldaA-R, CGGTATTCAGATGCCGTC. PCR product was digested with PacI, ligated into pGCC4 digested with PacI and PmeI (New England Biolabs; PacI restriction site underlined), and transformed into E. coli NEB5α. After sequence verification, pGCC4-PldA was transformed into piliated ΔmlaA as previously [22].
The conditional fur knockout was created using a strategy described previously [25]. An additional copy of the fur gene was initially placed under the control of an IPTG-inducible promoter within the intergenic region between lctP and aspC in the FA1090 chromosome. fur was subsequently replaced in its native chromosomal locus with the nonpolar kanamycin resistance cassette. Specifically, the fur gene was amplified using primers fur-F, GATCTTAATTAATTACAGGGATATTGAATATTATGGAAAAATTC and fur-R, ACAACAAACCGTCCGGAT. The PCR product was cut with PacI and ligated into PacI/PmeI cut pGCC4 to create pGCC4-fur. The resulting plasmid was used for transformation of FA1090 to create FA1090Plac::fur. To generate the knockout plasmid, pNEB193 was linearized by PCR using primers pNEB-F, GTTTAAACCTGCAGGCATGCAAG and pNEB-R, TCTAGACTTAATTAAGGATCCGGCG. One thousand bp upstream and downstream of fur were amplified using primers fur-up-F, CGCCGGATCCTTAATTAAGTCTAGATTTCGGCGGCGGCGC; fur-up-R, TCTGAGCGGGACTCCCTGTAAAATAATAGACGCTATAATACGCAATTTCAG; fur-down-F, GTGAAGCTAGCTATCCGGACGGTTTGTTGTTCAG; and fur-down-R, AGCTTGCATGCCTGCAGGTTTAAACTTTCCAATTTTATAGTGGATTAAATTTAAACCGGTACGG. The kanamycin resistance cassette was amplified using primers kan-F, TATTTTACAGGGAGTCCCGCTCAGAAGAACTCG and kan-R, AAACCGTCCGGATAGCTAGCTTCACGCTGCC. All fragments were purified and assembled using NEBuilder HiFi DNA Assembly Master Mix (NEB). pNEB193-Δfur was linearized with ScaI and used to transform FA1090Plac::fur. Clones were selected on solid medium supplemented with kanamycin and 0.1 mM IPTG and verified by PCR.
All plasmid insert sequences were confirmed by the Oregon State University Center for Genome Research and Biocomputing.
Protein purification
Truncated, recombinant 6 × His tagged MlaA (MlaA120-277) was expressed in E. coli BL21(DE3) harboring pET28-MlaA120-277. An overnight culture was used to inoculate 1.5 L LB medium supplemented with kanamycin. Protein overproduction was induced with 500 mM IPTG when cultures had reached OD600 ~0.5. After 3 h of growth at 37 °C, cells were pelleted by centrifugation (6,000 rpm for 20 min at 4 °C) and stored at -80 °C until use. Pellets were resuspended in lysis buffer (20 mM Tris pH 8.0, 500 mM NaCl, 10 mM imidazole, 1% Triton-X) in which a Pierce protease inhibitor mini tablet (ThermoFisher Scientific) had been dissolved. Cells were lysed by six passages through a French Press pressure cell at 1,200 psi. Crude lysate was clarified by centrifugation, incubated with DNAseI, and filtered through a 0.45 μm filter. Protein was purified on a Bio-Rad NGC scout system through a Bio-Rad Bio-Scale Mini Nuvia IMAC cartridge (Bio-Rad). Non-specifically bound proteins were washed off the column by 10 column volumes of wash buffer (20 mM Tris pH 8.0, 500 mM NaCl, 40 mM imidazole, 1% Triton-X). Protein was eluted over a 40–250 mM imidazole gradient and fractions were monitored for protein purity by SDS-PAGE. Triton was removed from protein solution by 2 h of end-over-end incubation with Bio-Rad Bio-Beads SM-2 adsorbent polystyrene beads (Bio-Rad) at room temperature. Glycerol was added to a final concentration of 10% and protein was stored at -80 °C.
For the overproduction of DsbA, 1 L of LB supplemented with kanamycin was inoculated with E. coli BL21(DE3) carrying pRSF-dsbA. Protein overproduction was induced by the addition of 1 mM IPTG when the culture reached an OD600 of about 0.5. After 3 h of growth at 37 °C, bacterial cells were pelleted by centrifugation at 6,000 × g for 20 min at 4 °C and cell pellets were stored at -80 °C until used. Recombinant DsbA was purified under native conditions using the NGC Scout Chromatography system (Bio-Rad). Bacterial cells were resuspended in lysis buffer (20 mM Tris pH 8.0, 500 mM NaCl, 10 mM imidazole) and lysed by five passages through a French pressure cell at 1,200 psi. Cell lysates were clarified by centrifugation and loaded onto a Bio-Scale Mini Profinity IMAC cartridge (Bio-Rad). Loosely bound proteins were removed with 10 column volumes of wash buffer (20 mM Tris pH 8.0, 500 mM NaCl, 40 mM imidazole) and DsbA was eluted with a 40–250 mM imidazole gradient. To remove the 6 × His tag the eluted DsbA was incubated overnight at 4° C with TEV protease at a 1:20 ratio. The proteins were concentrated to 5 mL using a Vivaspin 20 centrifuge concentrator (GE HealthCare). Proteins were subjected to size exclusion chromatography using HiLoad 16/600 Superdex 75 pg (GE HealthCare) and phosphate buffered saline (PBS) as running buffer. Fractions containing DsbA were concentrated using a Vivaspin 20 centrifuge concentrator (GE HealthCare).
Antisera preparation
Polyclonal rabbit antisera were prepared by Pacific Immunology using about 2 mg of purified MlaA120-277 or DsbA. A 13-week antibody production protocol was approved by IACUC Animal Protocol #1 and the National Institute of Health Animal Welfare Assurance Program (#A4182-01), and was performed in a certified animal facility (USDA 93-R-283).
SDS-PAGE and immunoblotting
Samples as indicated in the text were standardized by OD600 values (whole cell lysates) or by protein concentration (subcellular fractionation samples, i.e. C/P, CE, MV, and SS fractions). Standardized samples were separated by 1 dimensional sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) on 4–12% Novex NuPAGE (ThermoFisher Scientific) or 4–15% Bio-Rad Criterion TGX (Bio-Rad) protein gels. Proteins were visualized by colloidal coomassie G-250 staining. For immunoblotting, proteins were transferred to Trans-Blot Turbo nitrocellulose 0.2 μm membranes (Bio-Rad) using a Trans-Blot Turbo transfer system (Bio-Rad) at 25 V for 7 min. Membranes were blocked in blocking buffer (5% skim milk in phosphate buffered saline with 0.1% Tween-20 [PBST]) for 1 h at room temperature on a rocking table or at 4 °C overnight. Primary antisera were diluted in blocking buffer as follows: α-MlaA: 1: 5,000; α-TbpB: 1: 1,000 [25]; α-MtrE: 1: 5,000 [25]; α-BamA: 1: 10,000 [25]; α-BamD: 1: 20,000 [25]; α-LptD: 1: 5,000 [25]; α-TamA: 1: 10,000 [25]; α-NGO2054: 1: 10,000 [25]; α-SurA: 1:10,000 [46]; α-DsbA: 1:10,000; and α-Zwf: 1: 10,000 [49]. Membranes were incubated in horseradish peroxidase-conjugated goat anti-mouse (MtrE) or–rabbit (all other antigens) secondary antibody diluted 1:10,000. Blots were developed in Clarity Western ECL Substrate (Bio-Rad) and imaged on a ChemiDoc MP (Bio-Rad). Densitometry analyses were performed with Image Lab software (Bio-Rad).
Exposure to host-relevant conditions
FA1090 (WT) and ΔmlaA bacteria cultured as above were collected from rapidly-growing liquid cultures, diluted to OD600 = 0.2, serially diluted, and spotted on GCB plates supplemented with 7.5% NHS or 5 μM of the iron chelator deferoxamine mesylate (desferal). Inoculated plates were incubated at 37 °C in a 5% CO2 environment for 22 h or anaerobically at 37 °C in the presence of 1.2 mM sodium nitrite as a terminal electron acceptor, and either 0, 5, 10, 20, or 25 μM desferal for immunoblotting, for 48 h. The anaerobic environment was generated using BD GasPaks (BD) in an anaerobic jar. Colonies were counted for colony forming unit (CFU)/mL enumeration. Bacteria were collected from plates for immunoblotting analysis.
Desferal titration was performed in liquid media. Non-piliated FA1090 WT or ΔmlaA were suspended to OD600 = 0.1 in GCBL supplemented with Kellogg’s supplement I and sodium bicarbonate, but without Kellogg’s supplement II. Strains were cultured at 37 °C for 3 h with agitation (220 rpm). Cultures were diluted to OD600 = 0.1 in media supplemented with Kellogg’s supplement I and sodium bicarbonate and split. Daughter cultures were supplemented either with Kellogg’s supplement II or Desferal (5 to 25 μM). Suspensions were cultured at 37 °C with agitation for 6 h. Every hour, including 0 h, samples of each culture were serially diluted. Five microliters of each dilution were spotted onto a GCB plate, which was subsequently cultured at 37 °C for 18–20 h at 5% CO2. Colonies were counted for CFU/mL enumeration after incubation. Samples of WT and ΔmlaA liquid cultures with different desferal concentrations were taken at the 6 h timepoint and subjected to immunoblot analysis.
MlaA Fur regulation assessment
MlaA regulation by Fur was evaluated using the conditional Fur knockout strain Δfur/Plac::fur. Initial liquid cultures of WT FA1090, ΔmlaA, and Δfur/Plac::fur were prepared without Kellogg’s supplement II. Fur expression was induced by the addition of 0.1 mM IPTG. After three hours of growth, Δfur/Plac::fur cultures were washed by centrifugation at 5,000 × g for 5 minutes to remove IPTG, the supernatant was decanted, and bacteria were resuspended in fresh medium without IPTG. All strains were back diluted to an OD600 of 0.1 and supplemented with either Kellogg’s supplement II or 25 μM desferal. Fur expression was induced at different levels by the addition of 10, 50, or 100 μM IPTG under both iron-deplete and–replete conditions. Bacteria were cultured for 6 h at 37 °C with shaking (220 rpm), and growth was monitored every hour by OD600 measurement. At the experimental endpoint, samples of each culture were collected and centrifuged at 6,000 × g for 10 minutes. The supernatant was discarded and pellets were prepared for SDS-PAGE and immunoblotting analysis.
Serum sensitivity
Assessment of bacterial serum sensitivity was essentially as previously described [37]. Non-piliated strains as indicated in the text were suspended to OD600 = 0.1 in supplemented GCBL and cultured for 3 h at 37 °C with shaking (220 rpm). Bacterial cultures were suspended to OD600 = 0.05 in sterile PBS, then diluted 1:1000 in Eagle’s minimal essential medium (EMEM). Seventy microliters of this suspension, corresponding to approximately 103 CFU, was added to 70 μL NHS (Quidel, San Diego, CA; Ref# A113), heat-inactivated NHS (inactivated at 56 °C for 30 min), or EMEM alone, for final serum concentrations of 0% or 50% in a 96 well microtiter plate (initial testing indicated that bacterial survival was not altered in the presence of 8%, 10%, 12%, or 24% NHS). Plates were incubated at 37 °C in 5% CO2 for 1 h, after which 20 μL from each well were spotted onto a GCB plate. CFU/mL were enumerated following 18–20 h incubation as above.
Exposure to human defensin
HBD1 (AnaSpec Inc. 510791–9560) was solubilized to 100 μM in 0.01% acetic acid. Rapidly growing liquid cultures of WT and ΔmlaA bacteria were diluted to 105 cells/mL, and 45 μL of this suspension were transferred to a 1.5 mL tube. Volumes were adjusted to 50 μL with either GCBL, 0.01% acetic acid (vehicle), or HBD1 (final concentration, 10 μM). Bacteria were incubated for 3 h at 37 °C, serially diluted, and spotted onto GCB. CFUs were enumerated following 22 h incubation, and the relative survival was calculated. Experiments were performed on at least four independent occasions.
Etest antimicrobial sensitivity testing
Antimicrobial susceptibility was assessed by Etests according to manufacturer’s instructions. Briefly, non-piliated colonies of FA1090 or WHO X WT, ΔmlaA bacteria in either strain background, or ΔmlaA/Plac::pldA in the FA1090 knockout background were collected from GCB plates and suspended in brain heart infusion liquid medium to a turbidity equivalent to that of a 0.5 McFarland standard. Suspensions were spread on 150 mm tissue culture dishes containing 50 mL GCB solid medium (~4 mm thick), and test strips were laid on the surface of the plates. 0.5 mM IPTG was added to ΔmlaA/Plac::pldA plates. MICs were measured after approximately 22 h of incubation as above. Experiments were performed on three occasions and consensus MICs from at least two out of the three replicates are presented.
Sensitivity to polymyxin B
FA1090 WT, ΔmlaA, ΔmlaA/Plac::mlaA, and ΔmlaA/Plac::pldA were suspended to OD600 = 0.1 in GCBL supplemented as above and cultured for 3 h at 37 °C with agitation (220 rpm). Cultures were subsequently diluted to an OD600 of 0.1 in supplemented GCBL and cultured at 37 °C with agitation for 2 h. Bacteria were serially diluted and spotted on plates with or without 800 U/mL polymyxin and 0, 0.05, 0.1, or 0.5 mM IPTG. Plates were cultured at 37 °C in a 5% CO2 environment for approximately 18 h. Overall colony morphology was documented with a Chemi-Doc MP (Bio-Rad). Colonies were counted to determine overall survival under polymyxin B exposure. Images of colonies were taken with a Zeiss AxioObserver.D1 microscope at 10× magnification 0.25 Phase Contrast 1 and at 2.5× magnification 0.06 Phase Contrast 1. Colony diameters from images taken at 2.5× magnification were measured using ImageJ software. Results were similar for all induction levels. For clarity, % survival data is presented only for the 0.5 mM IPTG level. Microscopy for the complemented strain was performed with 0.1 mM IPTG.
LOS isolation and silver staining
LOS was isolated from WT, ΔmlaA, ΔmlaA/Plac::mlaA, and ΔmlaA/Plac::pldA using a method described previously [49]. Strains were harvested from either standard liquid cultures or cultures containing 100 U/mL polymyxin B by suspension in 1.5 mL GCBL to an OD600 of 0.2 and centrifugation at 15,000 × g for 1.5 min. The expression of MlaA in the ΔmlaA/Plac::mlaA strain was induced with 0.5 mM IPTG, and ΔmlaA/Plac::pldA was cultured either with or without 0.5 mM IPTG, as indicated. Cell pellets were resuspended in 50 μL lysis buffer (2% SDS, 4% β-mercaptoethanol, 10% glycerol, 1 M Tris pH 6.8, and 0.01% bromophenol blue) and boiled at 100 °C for 10 minutes to lyse bacteria. After samples were allowed to cool to room temperature, proteins were digested by proteinase K (25 μg in 10 μL lysis buffer) at 60 °C for 1 h. SDS-PAGE was performed on isolated LOS using an 18% gel, and LOS was visualized by silver staining [49].
Supernatant protein profiling
Membrane leakiness was assessed as previously described [23], using filtered supernatants from mid-logarithmic liquid cultures. Soluble supernatant proteins were precipitated with a pyrogallol red-molybdate-methanol procedure after DNAse I treatment. Membrane vesicles were not separated prior to precipitation. Precipitated proteins, standardized by OD600 values of the source cultures, were separated by SDS-PAGE and analyzed by immunoblotting. Whole cell lysates of source cultures were analyzed simultaneously.
Electron microscopy
Strains indicated in the text were cultured in GCBL as above, either with or without 100 U/mL polymyxin B, until approximately mid-logarithmic growth (OD600 of 0.5). The ΔmlaA/Plac::mlaA and ΔmlaA/Plac::pldA strains were cultured in the presence (both strains) or absence (ΔmlaA/Plac::pldA only, as indicated) of 0.5 mM IPTG. Bacteria were collected by centrifugation at 4000 × g for 3 min, washed twice and resuspended with PBS sterilized by filtration through a 0.1 μm filter. 2.5 μL of suspension were spotted onto 300 mesh copper grids and cells were allowed to attach to the grid for 15 min before excess PBS was removed. Cells were negatively stained with phosphotungstic acid and visualized with a FEI Helios NanoLab 650 electron microscope housed at the Oregon State University Electron Microscopy Facility. Experiments were performed at least twice, and representative micrographs are presented.
Subcellular fractionation
C/P, CE, MV, and SS fractions were isolated as described previously [22, 25]. Briefly, strains as indicated in the text were suspended in 500 mL GCBL supplemented as above and cultured at 37 °C with agitation (220 rpm) until cultures reached OD600 of ~0.8. Where indicated in the text, cultures were also supplemented with 100 U/mL polymyxin B. PldA overproduction was induced by the addition of 0.5 mM IPTG. Supernatants were separated from bacteria by low speed centrifugation and filtration and treated with DNaseI and protease inhibitors. Naturally released MVs were isolated by high-speed ultracentrifugation. Supernatants of MV isolation contain soluble supernatant proteins, which were precipitated by incubation with 15% trichloroacetic acid at 4 °C for 1 h and centrifugation at 14,000 × g for 20 min at 4°C. Precipitated proteins were washed with ice-cold acetone and centrifuged at 14,000 × g for 20 min at 4 °C. MV and SS fractions were resuspended in PBS + 0.8% SDS for SDS-PAGE, immunoblotting, and quantitative proteomics analyses as indicated. The CE was isolated by cold sodium carbonate extraction and ultracentrifugation [22, 25], and suspended in PBS + 0.8% SDS. Samples of supernatants from CE isolation were collected for the cytoplasmic/periplasmic fraction.
Quantitative proteomics
The quantitative proteomics studies were performed as we described previously [103]. Briefly, CE or MV were isolated from WT and ΔmlaA bacteria when the OD600 of each culture reached 0.6–0.8, as described above. The total protein amount in each CE and MV fraction was assessed using a Protein Assay Kit (Bio Rad) and were subjected to labeling with TMT6plex reagent (Thermo Scientific) according to manufacturer recommendations. Eighty μg of proteins were placed in a 1.5 mL tube and the volume was adjusted to 100 μL using 100 mM triethylammonium bicarbonate (TEAB) buffer. Proteins were reduced by addition of 11.3 mM tris(2-carboxyethyl)phosphine hydrochloride (TCEP) and incubation at 55 °C for 1 h, and alkylated by addition of 20.1 mM iodoacetamide for 30 min in the dark. Proteins were precipitated overnight in 90% acetone at -20°C, spun down at 15,000 × g for 10 min at 4°C and washed once with ice cold acetone. Protein pellets were resuspended in 100 μL of 100 mM TEAB and digested with trypsin at a 1:40 ratio overnight at 37°C. TMT Reagents were reconstituted in 41 μL of acetonitrile (ACN) and were added to the digested samples. Wild type CE samples were labeled with reagent TMT126 and TMT128 for replicates 1 and 2, respectively. CE proteins isolated from ΔmlaA were labeled with TMT127 and TMT129 for replicates 1 and 2, respectively. To label the MV proteins, TMT128 and TMT130 were used for wild type and TMT129 and 131 for ΔmlaA. The reaction was allowed to proceed for 1 h at room temperature and was quenched by addition of 8 μL of 5% hydroxylamine. Samples were pooled and subsequently fractionated by strong cation exchange (SCX) with a Paradigm (Michrom Biosciences) HPLC using 5 mM potassium phosphate monobasic in 30% ACN/70% water (v/v) pH 2.7 (buffer A) and 5 mM potassium phosphate monobasic in 30% ACN/70% water (v/v) pH 2.7 with 500 mM potassium chloride (buffer B) as the mobile phases. The sample was brought up in 200 μL buffer A. Peptides were separated over 60 min with a 2.1 mm x 100 mm Polysulfoethyl A column (PolyLC) at a 200 μL/min flow rate using the following separation profile: hold 2% B for 5 min, 2% to 8% B in 0.1 min, 8% to 18% B in 14.9 min, 18% to 34% B in 12 min, 34% to 60% B in 18 min, 60% to 98% B in 0.1 min and hold for 10 min. We collected 1 min fractions in 96-well microtiter plates. Twelve pools were generated from 60 fractions, and the pools were dried with a speed vac. Oasis HLB 1cc cartridges were subsequently used to desalt the samples. Cartridges were initially washed with 70% ACN/0.1% trifluoroacetic acid (TFA), then equilibrated with 0.1% TFA. Fractionated samples were hydrated in 0.1% TFA to load onto the cartridge, washed with 0.1% TFA, eluted in 1 mL 70% ACN/0.1% TFA, and dried by vacuum centrifugation.
Desalted samples were subsequently analyzed by LC/ESI MS/MS with a Thermo Scientific Easy-nLC II (Thermo Scientific, Waltham, MA) nano HPLC system coupled to a hybrid Orbitrap Elite ETD (Thermo Scientific, Waltham, MA) mass spectrometer at the Proteomic Core at The Fred Hutchinson Cancer Research Center, Seattle, WA. Samples were further desalted in-line using a reversed-phase trap column (100 μm × 20 mm) packed with Magic C18AQ (5 μm 200 Å resin; Michrom Bioresources) and peptides were separated on a reversed phase column directly mounted to the electrospray ion source [75 μm × 250 mm column packed with Magic C18AQ resin (5 μm 200 Å resin; Michrom Bioresources)]. Chromatographic separations were performed at a flow rate of 400 nL/min to apply a 90 min gradient of 7% to 35% ACN in 0.1% formic acid. The capillary temperature was set to 300 °C, and a 2750 V spray voltage was applied to the electrospray tip. The Orbitrap Elite instrument’s data dependent mode was used to switch automatically between MS survey scans [automatic gain control (AGC) target value 1,000,000; resolution 120,000; and injection time 250 msec] and MS/MS spectra acquisition (AGC target value of 50,000; 15,000 resolution; and injection time 250 msec). From the Fourier-transform full scan, the 15 most intense ions were selected for fragmentation by higher-energy collisional dissociation in the higher-energy C-trap dissociation (HCD) cell. The normalized collision energy was set to 40%. Selected ions were dynamically excluded for 30 sec with a list size of 500 and exclusion mass by mass width +/- 10ppm.
Proteomic data analysis
Data analysis was performed using Proteome Discoverer 1.4 (Thermo Scientific, San Jose, CA) and the data were searched against the N. gonorrhoeae FA1090 database (UniProt, downloaded May 11, 2017) with the common Repository of Adventitious Proteins (cRAP,http://www.thegpm.org/crap/) FASTA file. Trypsin was set as the enzyme with 2 mis-cleavages allowed. Variable modifications included TMT6Plex (+229.163 Da) on any N-Terminus, oxidation on methionine (+15.995 Da), carbamidomethyl on cysteine (+57.021 Da), and TMT6Plex on lysine (+229.163 Da). Ten ppm was set as the precursor ion tolerance, and 0.8 Da was established as the fragment ion tolerance.
Experimental design and statistical rationale
All experiments described above were performed using CE and MVs isolated from the N. gonorrhoeae wild type and ΔmlaA mutant in biological duplicates. Data were searched using Sequest HT. All search results were run through Percolator for scoring. Quantification was performed using the canned TMT6plex method through Proteome Discoverer to compare the normalized total reporter ion intensity between WT and ΔmlaA CE or MV fractions for each biological replicate. The mass spectrometry proteomics data have been deposited to the ProteomeXchange Consortium via the PRIDE [104] partner repository with the dataset identifier PXD008673. A False Discovery Rate of 1% was applied, and only proteins identified by ≥1 unique and ≥2 total peptides with a score ≥ 1 for every detected peptide were included for further analysis. Proteins were considered differentially expressed when the calculated ratios were below 0.67 or above 1.50.
Biofilm characterization
The ability of strains to produce biofilms was assessed using a method adapted from Anderson et al. [105]. Non-piliated bacteria, cultured as above, were collected from plates and suspended to OD550 = 1.5 in supplemented GCBL. One hundred microliters of this suspension were added to the wells of a 96-well flat-bottomed microtiter plate (Corning #3370). Water was added to all remaining wells to minimize the effects of evaporation. The plate was wrapped in plastic wrap and incubated at 37 °C in a 5% CO2 environment for 24 h without shaking. After incubation, samples from each well were serially diluted and spotted onto GCB plates for CFU/mL enumeration of viable planktonic bacteria. Planktonic bacteria and spent media were removed and biofilm wells were washed once with PBS. Plates were allowed to dry for ~4 h at room temperature, after which 65 μL of 0.1% crystal violet were added to each well and incubated for 15 min at room temperature. Wells were then washed 3 times with PBS and allowed to dry overnight at room temperature. Biofilms were dissolved by the addition of 125 μL 30% acetic acid, incubation at room temperature for 30 min, and shaking on a microplate vortexer. Biofilm mass was measured on a BioTek Synergy HT plate reader (BioTek) at 550 nm.
Competitive infection of the murine lower genital tract
Female BALB/c mice (6 to 8 weeks old; Charles River Laboratories Inc., Wilmington, MA; NCI Frederick strain of inbred BALB/cAnNCr mice, strain code 555) were treated with 0.5 mg of Premarin given two days prior to, the day of, and two days after bacterial inoculation to increase susceptibility to N. gonorrhoeae. Mice were also given antibiotics to suppress the overgrowth of commensal flora that occurs under the influence of estrogen [106]. Groups of mice were inoculated vaginally with similar numbers of WT FA1090 and either isogenic ΔmlaA or ΔmlaA/Plac::mlaA bacteria (total dose 106 CFU; 7 mice/group). Vaginal swabs were collected on days 1, 3, and 5 post-inoculation and suspended in 100 μL GCBL. Swab suspensions and inocula were cultured quantitatively on GCB supplemented with streptomycin (total number of CFUs) and GCB with streptomycin and kanamycin (ΔmlaA, ΔmlaA/Plac::mlaA; CFU). Results are expressed as the competitive index (CI) using the equation CI = [mutant CFU (output)/wild-type CFU (output)]/[mutant CFU (input)/wild-type CFU (input)]. The limit of detection of 1 CFU was assigned for a strain that was not recovered from an infected mouse. A CI of >1 indicates that the mutant is more fit than the WT strain.
Bioinformatic analyses
The MlaA amino acid sequence was used to search the non-redundant NCBI protein database to search for homologous proteins, and the ClustalOmega online tool was used to align sequences to generate a distance matrix. Signal peptides recognized by Signal Peptidase I or II were predicted with the SignalP 4.1 server (http://www.cbs.dtu.dk/services/SignalP/) or the LipoP 1.0 server (http://www.cbs.dtu.dk/services/LipoP/). MEGA7 software was employed to align sequences with the ClustalW tool for examination of phylogenetic relationships. Subsequently, a maximum likelihood tree was generated in MEGA using the Jones-Taylor-Thornton model to calculate a pairwise distance matrix [107]. To generate the initial tree, Neighbor-Join and BioNJ algorithms were applied to the matrix, and the tree was heuristically searched with the Nearest-Neighbor-Interchange method. Five hundred bootstrap replicates were applied to test the phylogenies, and the lowest log-likelihood tree is presented. The mlaA nucleic acid sequence was used to query the Neisseria Multilocus Sequence typing Database for SNP analysis of the locus (NEIS1933) across the 44,289 isolates deposited as of December 2, 2017. Phylogenetic analyses of MlaA among N. gonorrhoeae and between all Neisseria isolates were performed as above. Amino acid sequences of proteins identified through our quantitative proteomic investigations were used to query the NCBI non-redundant protein database using BLASTp (https://blast.ncbi.nlm.nih.gov/Blast.cgi?PAGE=Proteins) to gain insights into their functions.
Statistical analyses
All statistical analyses were performed using GraphPad Prism software (version 6.0h for Mac OS X) with the exception of proteomic data and animal studies described above. Built-in two-way ANOVA (using Sidak’s multiple comparisons test) or unpaired t-test analyses were used to test for statistical significance at p<0.05.
Ethics statement
Animal experiments were conducted at the Uniformed Services University of the Health Sciences (USUHS) according to the guidelines of the Association for the Assessment and Accreditation of Laboratory Animal Care under protocol no. MIC16-488 that was approved by the University’s Institutional Animal Care and Use Committee. The USUHS animal facilities meet the housing service and surgical standards set forth in the “Guide for the Care and Use of Laboratory Animals” NIH Publication No. 85–23, and the USU Instruction No. 3203, “Use and Care of Laboratory Animals”. Animals are maintained under the supervision of a full-time veterinarian. For all experiments, mice were humanely euthanized by trained personnel upon reaching the study endpoint using a compressed CO2 gas cylinder in LAM as per the Uniformed Services University (USU) euthanasia guidelines (IACUC policy 13), which follow those established by the 2013 American Veterinary Medical Association Panel on Euthanasia (https://www.usuhs.edu/mps/facilities-resources).
Supplemental Materials and Methods are described in S1 Text.
Supporting information
Phylogenetic trees of MlaA alleles were constructed for alleles found in all Neisseria isolates (A) and among N. gonorrhoeae (B). Maximum likelihood trees were generated in MEGA7 using the Jones-Taylor-Thornton method. FA1090 MlaA allele (allele 42) is boxed in red for each tree.
(TIF)
N. gonorrhoeae FA1090 mlaA was used to query the BioCyc database (biocyc.org) to align mlaA homologs in the genomes of the bacterial strains shown. MlaA is shown in yellow hashed boxes in the top panel and in purple hashed boxes in the bottom panel. Orthologous proteins are the same color in each panel.
(EPS)
(A) MBP-MlaA was purified by affinity chromatography with a MBPTrap column. The MBP tag was subsequently cleaved by overnight incubation with TEV protease, and the cleaved protein products were subjected to nickel affinity chromatography. Elution fractions were analyzed by SDS-PAGE and coomassie staining. (B) Nickel column fractions were pooled, concentrated, and subjected to size exclusion chromatography. Elutions were separated by SDS-PAGE and silver stained. Migration of molecular mass markers (in kDa) is indicated on the left. Major protein bands are marked by arrows. MBP, maltose binding protein; TEV, Tobacco Etch Virus; SDS-PAGE, sodium dodecyl sulfate-polyacrylamide gel electrophoresis.
(EPS)
(A) Five complementation strains were constructed in the FA1090 and WHO X strain backgrounds, as indicated. WT and isogenic ΔmlaA knockouts in FA1090 or WHO X, as well as all complementation strains, were cultured aerobically in GCBL in the absence or presence of the indicated concentrations of IPTG until mid-logarithmic growth (OD600 of 0.6–0.8) and collected for immunoblot analysis. Equivalent OD600 units were separated by SDS-PAGE, transferred to nitrocellulose membranes, and probed with anti-MlaA antiserum. MlaA is indicated by an arrow, and a non-specific cross-reactive band observed in the FA1090 strain is indicated with an asterisk. (B) Coomassie stained gel of samples presented in Fig 3E in the main text, acting as a loading control. GCBL, gonococcal base liquid medium; IPTG, isopropyl β-D-thiogalactopyranoside; OD600, optical density at 600 nm; SDS-PAGE, sodium dodecyl sulfate-polyacrylamide gel electrophoresis.
(EPS)
(A) Demonstration of Fur’s essential role in FA1090 viability. Δfur/Plac::fur was plated on GCB supplemented with (bottom plate) or without (upper plate) 0.1 mM IPTG. Robust growth was observed only in the presence of IPTG. (B) WT FA1090, isogenic knockout ΔmlaA, and conditional knockout Δfur/Plac::fur were cultured for 6 h in the presence (Fe-) or absence (SGC) of 25 μM desferal. Fur expression was induced by the addition of 10, 50, or 100 μM IPTG. Bacterial growth was monitored every hour by OD600 measurement. Mean ± SEM is presented, n = 3. Timepoints at which all strains’ OD600 values under iron starvation were significantly different from WT under iron repletion are indicated with an asterisk, p<0.05. (C) TbpB immunoblot as presented in Fig 5I, with the exception that the blot was overexposed to demonstrate low TbpB expression levels in WT under SGC and in Δfur/Plac::fur under SGC with increasing Fur induction. GCB, gonococcal base medium; IPTG, isopropyl β-D-thiogalactopyranoside; OD600, optical density at 600 nm; SGC, standard growth conditions; SEM, standard error of the mean.
(EPS)
Suspensions of WT FA1090 and isogenic knockout ΔmlaA bacteria standardized to an OD600 of 1.5 in GCBL were cultured in 96 well plates for 24 h in 5% CO2 at 37°C. Planktonic bacteria were removed prior to biofilm processing, serially diluted, and spotted onto GCB for CFU/mL enumeration. Mean ± SEM is presented for 12 biological replicates, each with 3 or 4 technical replicates, for a total of 46 datapoints. GCBL, gonococcal base liquid medium; GCB, gonococcal base medium; OD600, optical density at 600 nm.
(EPS)
Female BALB/c mice were inoculated intravaginally with approximately equal numbers of CFUs of WT and ΔmlaA/Plac::mlaA bacteria (~106 CFU total N. gonorrhoeae; 7 mice per group). Vaginal swabs taken on days 1, 3, and 5 post-infection were cultured for CFU/mL enumeration on solid media containing streptomycin (total bacteria) or media containing streptomycin and kanamycin (ΔmlaA/Plac::mlaA bacteria). Experiments were repeated three times and results are expressed as the geometric mean of the competitive index (CI): [mutant CFU (output) / WT CFU (output)] / [mutant CFU (input) / WT CFU (input)]. A CI > 1 indicates that the mutant was more fit during the competition. A value of 1 CFU was assigned for any strain not recovered from an infected mouse. CFU, colony forming unit.
(EPS)
Table 1 in S1 Text: Amino acid identity of members of the N. gonorrhoeae Mla operon with their E. coli homologs. Table 2 in S1 Text: Agar dilution assessment of WT, ΔmlaA, ΔmlaA/Plac::mlaA, and ΔmlaA/Plac::pldA MICs.
(DOCX)
(XLSX)
(XLSX)
(XLSX)
Acknowledgments
The authors would like to thank Dr. Stacey Harper for the use of the Zeiss AxioObserver microscope. We are grateful to Dr. Josephine Bonventre for technical assistance with the microscope. We would also like to thank Dr. Igor Wierzbicki for generating the MlaA120-277-His purification construct. Anti-TbpB antiserum was a generous gift from Dr. Cynthia Cornelissen. We are also grateful to Dr. Hank Seifert for helpful discussions on gonococcal pilins.
Data Availability
Data are available via ProteomeXchange with identifier PXD008673.
Funding Statement
Funding was provided to AES by grant R01-AI117235 from the National Institute of Allergy & Infectious Diseases, National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Vollmer W, Blanot D, de Pedro MA. Peptidoglycan structure and architecture. FEMS Microbiol Rev. 2008;32(2):149–67. Epub 2008/01/16. 10.1111/j.1574-6976.2007.00094.x . [DOI] [PubMed] [Google Scholar]
- 2.Silhavy TJ, Kahne D, Walker S. The bacterial cell envelope. Cold Spring Harbor perspectives in biology. 2010;2(5):a000414 10.1101/cshperspect.a000414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nikaido H. Restoring permeability barrier function to outer membrane. Chemistry & biology. 2005;12(5):507–9. Epub 2005/05/25. 10.1016/j.chembiol.2005.05.001 . [DOI] [PubMed] [Google Scholar]
- 4.Snijder HJ, Ubarretxena-Belandia I, Blaauw M, Kalk KH, Verheij HM, Egmond MR, et al. Structural evidence for dimerization-regulated activation of an integral membrane phospholipase. Nature. 1999;401(6754):717–21. 10.1038/44890 . [DOI] [PubMed] [Google Scholar]
- 5.Bishop RE, Gibbons HS, Guina T, Trent MS, Miller SI, Raetz CR. Transfer of palmitate from phospholipids to lipid A in outer membranes of gram-negative bacteria. EMBO J. 2000;19(19):5071–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malinverni JC, Silhavy TJ. An ABC transport system that maintains lipid asymmetry in the gram-negative outer membrane. Proc Natl Acad Sci U S A. 2009;106(19):8009–14. 10.1073/pnas.0903229106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bishop RE. Structural biology of membrane-intrinsic beta-barrel enzymes: sentinels of the bacterial outer membrane. Biochim Biophys Acta. 2008;1778(9):1881–96. 10.1016/j.bbamem.2007.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dekker N. Outer-membrane phospholipase A: known structure, unknown biological function. Mol Microbiol. 2000;35(4):711–7. Epub 2000/02/26. . [DOI] [PubMed] [Google Scholar]
- 9.May KL, Silhavy TJ. The Escherichia coli Phospholipase PldA Regulates Outer Membrane Homeostasis via Lipid Signaling. mBio. 2018;9(2). 10.1128/mBio.00379-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abellon-Ruiz J, Kaptan SS, Basle A, Claudi B, Bumann D, Kleinekathofer U, et al. Structural basis for maintenance of bacterial outer membrane lipid asymmetry. Nature microbiology. 2017;2(12):1616–23. 10.1038/s41564-017-0046-x . [DOI] [PubMed] [Google Scholar]
- 11.Zhao L, Gao X, Liu C, Lv X, Jiang N, Zheng S. Deletion of the vacJ gene affects the biology and virulence in Haemophilus parasuis serovar 5. Gene. 2017;603:42–53. Epub 2016/12/19. 10.1016/j.gene.2016.12.009 . [DOI] [PubMed] [Google Scholar]
- 12.Shen L, Gao X, Wei J, Chen L, Zhao X, Li B, et al. PA2800 plays an important role in both antibiotic susceptibility and virulence in Pseudomonas aeruginosa. Curr Microbiol. 2012;65(5):601–9. 10.1007/s00284-012-0196-2 . [DOI] [PubMed] [Google Scholar]
- 13.Roier S, Zingl FG, Cakar F, Durakovic S, Kohl P, Eichmann TO, et al. A novel mechanism for the biogenesis of outer membrane vesicles in Gram-negative bacteria. Nat Commun. 2016;7:10515 10.1038/ncomms10515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carpenter CD, Cooley BJ, Needham BD, Fisher CR, Trent MS, Gordon V, et al. The Vps/VacJ ABC transporter is required for intercellular spread of Shigella flexneri. Infect Immun. 2014;82(2):660–9. 10.1128/IAI.01057-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suzuki T, Murai T, Fukuda I, Tobe T, Yoshikawa M, Sasakawa C. Identification and characterization of a chromosomal virulence gene, vacJ, required for intercellular spreading of Shigella flexneri. Mol Microbiol. 1994;11(1):31–41. . [DOI] [PubMed] [Google Scholar]
- 16.Nakamura S, Shchepetov M, Dalia AB, Clark SE, Murphy TF, Sethi S, et al. Molecular basis of increased serum resistance among pulmonary isolates of non-typeable Haemophilus influenzae. PLoS pathogens. 2011;7(1):e1001247 10.1371/journal.ppat.1001247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garenaux A, Guillou S, Ermel G, Wren B, Federighi M, Ritz M. Role of the Cj1371 periplasmic protein and the Cj0355c two-component regulator in the Campylobacter jejuni NCTC 11168 response to oxidative stress caused by paraquat. Res Microbiol. 2008;159(9–10):718–26. 10.1016/j.resmic.2008.08.001 . [DOI] [PubMed] [Google Scholar]
- 18.Santos PM, Benndorf D, Sa-Correia I. Insights into Pseudomonas putida KT2440 response to phenol-induced stress by quantitative proteomics. Proteomics. 2004;4(9):2640–52. 10.1002/pmic.200300793 . [DOI] [PubMed] [Google Scholar]
- 19.Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, et al. Global Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2012 Based on Systematic Review and Global Reporting. PloS one. 2015;10(12):e0143304 10.1371/journal.pone.0143304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Unemo M, Del Rio C, Shafer WM. Antimicrobial Resistance Expressed by Neisseria gonorrhoeae: A Major Global Public Health Problem in the 21st Century. Microbiol Spectr. 2016;4(3):213–37. 10.1128/microbiolspec.EI10-0009-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lefebvre B, Martin I, Demczuk W, Deshaies L, Michaud S, Labbe AC, et al. Ceftriaxone-Resistant Neisseria gonorrhoeae, Canada, 2017. Emerg Infect Dis. 2018;24(2). Epub 2017/11/14. 10.3201/eid2402.171756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zielke RA, Wierzbicki IH, Weber JV, Gafken PR, Sikora AE. Quantitative proteomics of the Neisseria gonorrhoeae cell envelope and membrane vesicles for the discovery of potential therapeutic targets. Mol Cell Proteomics. 2014;13(5):1299–317. 10.1074/mcp.M113.029538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baarda BI, Emerson S, Proteau PJ, Sikora AE. Deciphering the function of new gonococcal vaccine antigens using phenotypic microarrays. J Bacteriol. 2017;199(17):1–24. 10.1128/JB.00037-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nakayama H, Kurokawa K, Lee BL. Lipoproteins in bacteria: structures and biosynthetic pathways. The FEBS journal. 2012;279(23):4247–68. 10.1111/febs.12041 . [DOI] [PubMed] [Google Scholar]
- 25.Zielke RA, Wierzbicki IH, Baarda BI, Gafken PR, Soge OO, Holmes KK, et al. Proteomics-driven Antigen Discovery for Development of Vaccines Against Gonorrhea. Mol Cell Proteomics. 2016;15(7):2338–55. 10.1074/mcp.M116.058800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Unemo M, Golparian D, Sanchez-Buso L, Grad Y, Jacobsson S, Ohnishi M, et al. The novel 2016 WHO Neisseria gonorrhoeae reference strains for global quality assurance of laboratory investigations: phenotypic, genetic and reference genome characterization. J Antimicrob Chemother. 2016;71(11):3096–108. 10.1093/jac/dkw288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chan YA, Hackett KT, Dillard JP. The lytic transglycosylases of Neisseria gonorrhoeae. Microb Drug Resist. 2012;18(3):271–9. Epub 2012/03/22. 10.1089/mdr.2012.0001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Velez Acevedo RN, Ronpirin C, Kandler JL, Shafer WM, Cornelissen CN. Identification of regulatory elements that control expression of the tbpBA operon in Neisseria gonorrhoeae. J Bacteriol. 2014;196(15):2762–74. 10.1128/JB.01693-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ducey TF, Carson MB, Orvis J, Stintzi AP, Dyer DW. Identification of the iron-responsive genes of Neisseria gonorrhoeae by microarray analysis in defined medium. J Bacteriol. 2005;187(14):4865–74. Epub 2005/07/05. 10.1128/JB.187.14.4865-4874.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cornelissen CN. Identification and characterization of gonococcal iron transport systems as potential vaccine antigens. Future microbiology. 2008;3(3):287–98. Epub 2008/05/29. 10.2217/17460913.3.3.287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hagman KE, Shafer WM. Transcriptional control of the mtr efflux system of Neisseria gonorrhoeae. J Bacteriol. 1995;177(14):4162–5. Epub 1995/07/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Edwards JL, Apicella MA. The molecular mechanisms used by Neisseria gonorrhoeae to initiate infection differ between men and women. Clin Microbiol Rev. 2004;17(4):965–81, table of contents. Epub 2004/10/19. 10.1128/CMR.17.4.965-981.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ricci DP, Silhavy TJ. The Bam machine: a molecular cooper. Biochim Biophys Acta. 2012;1818(4):1067–84. 10.1016/j.bbamem.2011.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thomas CE, Sparling PF. Isolation and analysis of a fur mutant of Neisseria gonorrhoeae. J Bacteriol. 1996;178(14):4224–32. Epub 1996/07/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agarwal S, King CA, Klein EK, Soper DE, Rice PA, Wetzler LM, et al. The gonococcal Fur-regulated tbpA and tbpB genes are expressed during natural mucosal gonococcal infection. Infect Immun. 2005;73(7):4281–7. 10.1128/IAI.73.7.4281-4287.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kandler JL, Acevedo RV, Dickinson MK, Cash DR, Shafer WM, Cornelissen CN. The genes that encode the gonococcal transferrin binding proteins, TbpB and TbpA, are differentially regulated by MisR under iron-replete and iron-depleted conditions. Mol Microbiol. 2016;102(1):137–51. Epub 2016/06/30. 10.1111/mmi.13450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garvin LE, Bash MC, Keys C, Warner DM, Ram S, Shafer WM, et al. Phenotypic and genotypic analyses of Neisseria gonorrhoeae isolates that express frequently recovered PorB PIA variable region types suggest that certain P1a porin sequences confer a selective advantage for urogenital tract infection. Infect Immun. 2008;76(8):3700–9. Epub 2008/06/11. 10.1128/IAI.00265-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ganz T. Defensins: antimicrobial peptides of innate immunity. Nat Rev Immunol. 2003;3(9):710–20. 10.1038/nri1180 . [DOI] [PubMed] [Google Scholar]
- 39.Porter E, Yang H, Yavagal S, Preza GC, Murillo O, Lima H, et al. Distinct defensin profiles in Neisseria gonorrhoeae and Chlamydia trachomatis urethritis reveal novel epithelial cell-neutrophil interactions. Infect Immun. 2005;73(8):4823–33. Epub 2005/07/26. 10.1128/IAI.73.8.4823-4833.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yu Z, Qin W, Lin J, Fang S, Qiu J. Antibacterial mechanisms of polymyxin and bacterial resistance. Biomed Res Int. 2015;2015:679109 10.1155/2015/679109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kohanski MA, Dwyer DJ, Collins JJ. How antibiotics kill bacteria: from targets to networks. Nature reviews Microbiology. 2010;8(6):423–35. 10.1038/nrmicro2333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sklar JG, Wu T, Kahne D, Silhavy TJ. Defining the roles of the periplasmic chaperones SurA, Skp, and DegP in Escherichia coli. Genes Dev. 2007;21(19):2473–84. 10.1101/gad.1581007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lazar SW, Kolter R. SurA assists the folding of Escherichia coli outer membrane proteins. J Bacteriol. 1996;178(6):1770–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Denoncin K, Vertommen D, Paek E, Collet JF. The protein-disulfide isomerase DsbC cooperates with SurA and DsbA in the assembly of the essential beta-barrel protein LptD. J Biol Chem. 2010;285(38):29425–33. 10.1074/jbc.M110.119321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu H, Taylor TH Jr., Pettus K, Trees D. Assessment of Etest as an alternative to agar dilution for antimicrobial susceptibility testing of Neisseria gonorrhoeae. J Clin Microbiol. 2014;52(5):1435–40. 10.1128/JCM.02131-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sikora AE, Wierzbicki IH, Zielke RA, Ryner RF, Korotkov KV, Buchanan SK, et al. Structural and functional insights into the role of BamD and BamE within the beta-barrel assembly machinery in Neisseria gonorrhoeae. J Biol Chem. 2018;293(4):1106–19. Epub 2017/12/13. 10.1074/jbc.RA117.000437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sandoval JM, Arenas FA, Vasquez CC. Glucose-6-phosphate dehydrogenase protects Escherichia coli from tellurite-mediated oxidative stress. PloS one. 2011;6(9):e25573 10.1371/journal.pone.0025573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lundberg BE, Wolf RE Jr., Dinauer MC, Xu Y, Fang FC. Glucose 6-phosphate dehydrogenase is required for Salmonella typhimurium virulence and resistance to reactive oxygen and nitrogen intermediates. Infect Immun. 1999;67(1):436–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wierzbicki IH, Zielke RA, Korotkov KV, Sikora AE. Functional and structural studies on the Neisseria gonorrhoeae GmhA, the first enzyme in the glycero-manno-heptose biosynthesis pathways, demonstrate a critical role in lipooligosaccharide synthesis and gonococcal viability. Microbiologyopen. 2017;6(2). 10.1002/mbo3.432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Steichen CT, Shao JQ, Ketterer MR, Apicella MA. Gonococcal cervicitis: a role for biofilm in pathogenesis. J Infect Dis. 2008;198(12):1856–61. Epub 2008/11/01. 10.1086/593336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jerse AE. Experimental gonococcal genital tract infection and opacity protein expression in estradiol-treated mice. Infect Immun. 1999;67(11):5699–708. Epub 1999/10/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jerse AE, Sharma ND, Simms AN, Crow ET, Snyder LA, Shafer WM. A gonococcal efflux pump system enhances bacterial survival in a female mouse model of genital tract infection. Infect Immun. 2003;71(10):5576–82. Epub 2003/09/23. 10.1128/IAI.71.10.5576-5582.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jamet A, Jousset AB, Euphrasie D, Mukorako P, Boucharlat A, Ducousso A, et al. A new family of secreted toxins in pathogenic Neisseria species. PLoS pathogens. 2015;11(1):e1004592 10.1371/journal.ppat.1004592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hill SA, Davies JK. Pilin gene variation in Neisseria gonorrhoeae: reassessing the old paradigms. FEMS Microbiol Rev. 2009;33(3):521–30. Epub 2009/04/28. 10.1111/j.1574-6976.2009.00171.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wachter J, Masters TL, Wachter S, Mason J, Hill SA. pilS loci in Neisseria gonorrhoeae are transcriptionally active. Microbiology. 2015;161(Pt 5):1124–35. 10.1099/mic.0.000061 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang J, Gray-Owen SD, Knorre A, Meyer TF, Dehio C. Opa binding to cellular CD66 receptors mediates the transcellular traversal of Neisseria gonorrhoeae across polarized T84 epithelial cell monolayers. Mol Microbiol. 1998;30(3):657–71. Epub 1998/11/21. . [DOI] [PubMed] [Google Scholar]
- 57.Knepper B, Heuer I, Meyer TF, van Putten JP. Differential response of human monocytes to Neisseria gonorrhoeae variants expressing pili and opacity proteins. Infect Immun. 1997;65(10):4122–9. Epub 1997/10/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Popp A, Dehio C, Grunert F, Meyer TF, Gray-Owen SD. Molecular analysis of neisserial Opa protein interactions with the CEA family of receptors: identification of determinants contributing to the differential specificities of binding. Cell Microbiol. 1999;1(2):169–81. Epub 2001/02/24. . [DOI] [PubMed] [Google Scholar]
- 59.Bos MP, Kao D, Hogan DM, Grant CC, Belland RJ. Carcinoembryonic antigen family receptor recognition by gonococcal Opa proteins requires distinct combinations of hypervariable Opa protein domains. Infect Immun. 2002;70(4):1715–23. 10.1128/IAI.70.4.1715-1723.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Arvidson CG, Powers T, Walter P, So M. Neisseria gonorrhoeae PilA is an FtsY homolog. J Bacteriol. 1999;181(3):731–9. Epub 1999/01/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Juneau RA, Stevens JS, Apicella MA, Criss AK. A Thermonuclease of Neisseria gonorrhoeae Enhances Bacterial Escape From Killing by Neutrophil Extracellular Traps. J Infect Dis. 2015;212(2):316–24. 10.1093/infdis/jiv031 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Steichen CT, Cho C, Shao JQ, Apicella MA. The Neisseria gonorrhoeae biofilm matrix contains DNA, and an endogenous nuclease controls its incorporation. Infect Immun. 2011;79(4):1504–11. Epub 2011/02/09. 10.1128/IAI.01162-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mendum TA, Newcombe J, McNeilly CL, McFadden J. Towards the Immunoproteome of Neisseria meningitidis. PloS one. 2009;4(6). 10.1371/journal.pone.0005940 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stohl EA, Criss AK, Seifert HS. The transcriptome response of Neisseria gonorrhoeae to hydrogen peroxide reveals genes with previously uncharacterized roles in oxidative damage protection. Mol Microbiol. 2005;58(2):520–32. Epub 2005/10/01. 10.1111/j.1365-2958.2005.04839.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Isabella VM, Clark VL. Deep sequencing-based analysis of the anaerobic stimulon in Neisseria gonorrhoeae. BMC Genomics. 2011;12:51 Epub 2011/01/22. 10.1186/1471-2164-12-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Humbert MV, Awanye AM, Lian LY, Derrick JP, Christodoulides M. Structure of the Neisseria Adhesin Complex Protein (ACP) and its role as a novel lysozyme inhibitor. PLoS pathogens. 2017;13(6):e1006448 10.1371/journal.ppat.1006448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hung MC, Heckels JE, Christodoulides M. The adhesin complex protein (ACP) of Neisseria meningitidis is a new adhesin with vaccine potential. mBio. 2013;4(2). Epub 2013/02/28. 10.1128/mBio.00041-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Arvidson CG, Kirkpatrick R, Witkamp MT, Larson JA, Schipper CA, Waldbeser LS, et al. Neisseria gonorrhoeae mutants altered in toxicity to human fallopian tubes and molecular characterization of the genetic locus involved. Infect Immun. 1999;67(2):643–52. Epub 1999/01/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Frederiksen RF, Paspaliari DK, Larsen T, Storgaard BG, Larsen MH, Ingmer H, et al. Bacterial chitinases and chitin-binding proteins as virulence factors. Microbiology. 2013;159(Pt 5):833–47. 10.1099/mic.0.051839-0 . [DOI] [PubMed] [Google Scholar]
- 70.Williams JN, Weynants V, Poolman JT, Heckels JE, Christodoulides M. Immuno-proteomic analysis of human immune responses to experimental Neisseria meningitidis outer membrane vesicle vaccines identifies potential cross-reactive antigens. Vaccine. 2014;32(11):1280–6. Epub 2014/02/04. 10.1016/j.vaccine.2013.12.070 . [DOI] [PubMed] [Google Scholar]
- 71.Sechman EV, Rohrer MS, Seifert HS. A genetic screen identifies genes and sites involved in pilin antigenic variation in Neisseria gonorrhoeae. Mol Microbiol. 2005;57(2):468–83. Epub 2005/06/28. 10.1111/j.1365-2958.2005.04657.x . [DOI] [PubMed] [Google Scholar]
- 72.Kumar P, Sannigrahi S, Scoullar J, Kahler CM, Tzeng YL. Characterization of DsbD in Neisseria meningitidis. Mol Microbiol. 2011;79(6):1557–73. Epub 2011/01/12. 10.1111/j.1365-2958.2011.07546.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen I, Gotschlich EC. ComE, a competence protein from Neisseria gonorrhoeae with DNA-binding activity. J Bacteriol. 2001;183(10):3160–8. Epub 2001/04/28. 10.1128/JB.183.10.3160-3168.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Snyder LA, Cole JA, Pallen MJ. Comparative analysis of two Neisseria gonorrhoeae genome sequences reveals evidence of mobilization of Correia Repeat Enclosed Elements and their role in regulation. BMC Genomics. 2009;10:70 Epub 2009/02/11. 10.1186/1471-2164-10-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Scheuerpflug I, Rudel T, Ryll R, Pandit J, Meyer TF. Roles of PilC and PilE proteins in pilus-mediated adherence of Neisseria gonorrhoeae and Neisseria meningitidis to human erythrocytes and endothelial and epithelial cells. Infect Immun. 1999;67(2):834–43. Epub 1999/01/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lee EH, Shafer WM. The farAB-encoded efflux pump mediates resistance of gonococci to long-chained antibacterial fatty acids. Mol Microbiol. 1999;33(4):839–45. . [DOI] [PubMed] [Google Scholar]
- 77.Bar-Yaacov D, Mordret E, Towers R, Biniashvili T, Soyris C, Schwartz S, et al. RNA editing in bacteria recodes multiple proteins and regulates an evolutionarily conserved toxin-antitoxin system. Genome Res. 2017;27(10):1696–703. 10.1101/gr.222760.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cacciapuoti AF, Wegener WS, Morse SA. Cell envelope of Neisseria gonorrhoeae: phospholipase activity and its relationship to autolysis. Infect Immun. 1978;20(2):418–20. Epub 1978/05/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Senff LM, Wegener WS, Brooks GF, Finnerty WR, Makula RA. Phospholipid composition and phospholipase A activity of Neisseria gonorrhoeae. J Bacteriol. 1976;127(2):874–80. Epub 1976/08/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bos MP, Tefsen B, Voet P, Weynants V, van Putten JP, Tommassen J. Function of neisserial outer membrane phospholipase a in autolysis and assessment of its vaccine potential. Infect Immun. 2005;73(4):2222–31. Epub 2005/03/24. 10.1128/IAI.73.4.2222-2231.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kuldau GA, De Vos G, Owen J, McCaffrey G, Zambryski P. The virB operon of Agrobacterium tumefaciens pTiC58 encodes 11 open reading frames. Mol Gen Genet. 1990;221(2):256–66. Epub 1990/04/01. . [DOI] [PubMed] [Google Scholar]
- 82.Ward JE, Akiyoshi DE, Regier D, Datta A, Gordon MP, Nester EW. Characterization of the virB operon from an Agrobacterium tumefaciens Ti plasmid. J Biol Chem. 1988;263(12):5804–14. Epub 1988/04/25. . [PubMed] [Google Scholar]
- 83.Ward JE, Dale EM, Christie PJ, Nester EW, Binns AN. Complementation analysis of Agrobacterium tumefaciens Ti plasmid virB genes by use of a vir promoter expression vector: virB9, virB10, and virB11 are essential virulence genes. J Bacteriol. 1990;172(9):5187–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Smith EF, Townsend CO. A Plant-Tumor of Bacterial Origin. Science. 1907;25(643):671–3. Epub 1907/04/26. 10.1126/science.25.643.671 . [DOI] [PubMed] [Google Scholar]
- 85.Chilton MD, Drummond MH, Merio DJ, Sciaky D, Montoya AL, Gordon MP, et al. Stable incorporation of plasmid DNA into higher plant cells: the molecular basis of crown gall tumorigenesis. Cell. 1977;11(2):263–71. Epub 1977/06/01. . [DOI] [PubMed] [Google Scholar]
- 86.Berger BR, Christie PJ. Genetic complementation analysis of the Agrobacterium tumefaciens virB operon: virB2 through virB11 are essential virulence genes. J Bacteriol. 1994;176(12):3646–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yu C, Genco CA. Fur-mediated activation of gene transcription in the human pathogen Neisseria gonorrhoeae. J Bacteriol. 2012;194(7):1730–42. 10.1128/JB.06176-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Valenti P, Rosa L, Capobianco D, Lepanto MS, Schiavi E, Cutone A, et al. Role of Lactobacilli and Lactoferrin in the Mucosal Cervicovaginal Defense. Front Immunol. 2018;9:376 10.3389/fimmu.2018.00376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McClure R, Nudel K, Massari P, Tjaden B, Su X, Rice PA, et al. The Gonococcal Transcriptome during Infection of the Lower Genital Tract in Women. PloS one. 2015;10(8):e0133982 10.1371/journal.pone.0133982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Furse S, Wienk H, Boelens R, de Kroon AI, Killian JA. E. coli MG1655 modulates its phospholipid composition through the cell cycle. FEBS Lett. 2015;589(19 Pt B):2726–30. Epub 2015/08/15. 10.1016/j.febslet.2015.07.043 . [DOI] [PubMed] [Google Scholar]
- 91.Sud IJ, Feingold DS. Phospholipids and fatty acids of Neisseria gonorrhoeae. J Bacteriol. 1975;124(2):713–7. Epub 1975/11/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Audet A, Nantel G, Proulx P. Phospholipase A activity in growing Escherichia coli cells. Biochim Biophys Acta. 1974;348(3):334–43. Epub 1974/06/26. . [DOI] [PubMed] [Google Scholar]
- 93.Ekiert DC, Bhabha G, Isom GL, Greenan G, Ovchinnikov S, Henderson IR, et al. Architectures of Lipid Transport Systems for the Bacterial Outer Membrane. Cell. 2017;169(2):273–85 e17. 10.1016/j.cell.2017.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.El Mashak EM, Tocanne JF. Polymyxin B-phosphatidylglycerol interactions. A monolayer (pi, delta V) study. Biochim Biophys Acta. 1980;596(2):165–79. Epub 1980/02/28. . [DOI] [PubMed] [Google Scholar]
- 95.Domingues MM, Inácio RG, Raimundo JM, Martins M, Castanho MARB, Santos NC. Biophysical characterization of polymyxin b interaction with LPS aggregates and membrane model systems. Biopolymers. 2012;98(4):338–44. 10.1002/bip.22095 [DOI] [PubMed] [Google Scholar]
- 96.Cole JG, Fulcher NB, Jerse AE. Opacity proteins increase Neisseria gonorrhoeae fitness in the female genital tract due to a factor under ovarian control. Infect Immun. 2010;78(4):1629–41. Epub 2010/01/27. 10.1128/IAI.00996-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zielke RA, Le Van A, Baarda BI, Herrera MF, Acosta CJ, Jerse AE, et al. SliC is a surface-displayed lipoprotein that is required for the anti-lysozyme strategy during Neisseria gonorrhoeae infection. PLoS pathogens. 2018;14(7):e1007081 Epub 2018/07/06. 10.1371/journal.ppat.1007081 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ragland SA, Humbert MV, Christodoulides M, Criss AK. Neisseria gonorrhoeae employs two protein inhibitors to evade killing by human lysozyme. PLoS pathogens. 2018;14(7):e1007080 10.1371/journal.ppat.1007080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Manning AJ, Kuehn MJ. Contribution of bacterial outer membrane vesicles to innate bacterial defense. BMC microbiology. 2011;11:258 Epub 2011/12/03. 10.1186/1471-2180-11-258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Toyofuku M, Tashiro Y, Hasegawa Y, Kurosawa M, Nomura N. Bacterial membrane vesicles, an overlooked environmental colloid: Biology, environmental perspectives and applications. Adv Colloid Interface Sci. 2015;226(Pt A):65–77. 10.1016/j.cis.2015.08.013 . [DOI] [PubMed] [Google Scholar]
- 101.Jerse AE, Crow ET, Bordner AN, Rahman I, Cornelissen CN, Moench TR, et al. Growth of Neisseria gonorrhoeae in the female mouse genital tract does not require the gonococcal transferrin or hemoglobin receptors and may be enhanced by commensal lactobacilli. Infect Immun. 2002;70(5):2549–58. Epub 2002/04/16. 10.1128/IAI.70.5.2549-2558.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cohen MS, Cannon JG, Jerse AE, Charniga LM, Isbey SF, Whicker LG. Human experimentation with Neisseria gonorrhoeae: rationale, methods, and implications for the biology of infection and vaccine development. J Infect Dis. 1994;169(3):532–7. Epub 1994/03/01. . [DOI] [PubMed] [Google Scholar]
- 103.El-Rami FE, Zielke RA, Wi T, Sikora AE, Unemo M. Quantitative Proteomics of the 2016 WHO Neisseria gonorrhoeae Reference Strains Surveys Vaccine Candidates and Antimicrobial Resistance Determinants. Mol Cell Proteomics. 2019;18(1):127–50. Epub 2018/10/26. 10.1074/mcp.RA118.001125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Vizcaino JA, Csordas A, del-Toro N, Dianes JA, Griss J, Lavidas I, et al. 2016 update of the PRIDE database and its related tools. Nucleic Acids Res. 2016;44(D1):D447–56. 10.1093/nar/gkv1145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Anderson MT, Byerly L, Apicella MA, Seifert HS. Seminal Plasma Promotes Neisseria gonorrhoeae Aggregation and Biofilm Formation. J Bacteriol. 2016;198(16):2228–35. 10.1128/JB.00165-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jerse AE, Wu H, Packiam M, Vonck RA, Begum AA, Garvin LE. Estradiol-Treated Female Mice as Surrogate Hosts for Neisseria gonorrhoeae Genital Tract Infections. Frontiers in microbiology. 2011;2:107 Epub 2011/07/13. 10.3389/fmicb.2011.00107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jones DT, Taylor WR, Thornton JM. The rapid generation of mutation data matrices from protein sequences. Comput Appl Biosci. 1992;8(3):275–82. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Phylogenetic trees of MlaA alleles were constructed for alleles found in all Neisseria isolates (A) and among N. gonorrhoeae (B). Maximum likelihood trees were generated in MEGA7 using the Jones-Taylor-Thornton method. FA1090 MlaA allele (allele 42) is boxed in red for each tree.
(TIF)
N. gonorrhoeae FA1090 mlaA was used to query the BioCyc database (biocyc.org) to align mlaA homologs in the genomes of the bacterial strains shown. MlaA is shown in yellow hashed boxes in the top panel and in purple hashed boxes in the bottom panel. Orthologous proteins are the same color in each panel.
(EPS)
(A) MBP-MlaA was purified by affinity chromatography with a MBPTrap column. The MBP tag was subsequently cleaved by overnight incubation with TEV protease, and the cleaved protein products were subjected to nickel affinity chromatography. Elution fractions were analyzed by SDS-PAGE and coomassie staining. (B) Nickel column fractions were pooled, concentrated, and subjected to size exclusion chromatography. Elutions were separated by SDS-PAGE and silver stained. Migration of molecular mass markers (in kDa) is indicated on the left. Major protein bands are marked by arrows. MBP, maltose binding protein; TEV, Tobacco Etch Virus; SDS-PAGE, sodium dodecyl sulfate-polyacrylamide gel electrophoresis.
(EPS)
(A) Five complementation strains were constructed in the FA1090 and WHO X strain backgrounds, as indicated. WT and isogenic ΔmlaA knockouts in FA1090 or WHO X, as well as all complementation strains, were cultured aerobically in GCBL in the absence or presence of the indicated concentrations of IPTG until mid-logarithmic growth (OD600 of 0.6–0.8) and collected for immunoblot analysis. Equivalent OD600 units were separated by SDS-PAGE, transferred to nitrocellulose membranes, and probed with anti-MlaA antiserum. MlaA is indicated by an arrow, and a non-specific cross-reactive band observed in the FA1090 strain is indicated with an asterisk. (B) Coomassie stained gel of samples presented in Fig 3E in the main text, acting as a loading control. GCBL, gonococcal base liquid medium; IPTG, isopropyl β-D-thiogalactopyranoside; OD600, optical density at 600 nm; SDS-PAGE, sodium dodecyl sulfate-polyacrylamide gel electrophoresis.
(EPS)
(A) Demonstration of Fur’s essential role in FA1090 viability. Δfur/Plac::fur was plated on GCB supplemented with (bottom plate) or without (upper plate) 0.1 mM IPTG. Robust growth was observed only in the presence of IPTG. (B) WT FA1090, isogenic knockout ΔmlaA, and conditional knockout Δfur/Plac::fur were cultured for 6 h in the presence (Fe-) or absence (SGC) of 25 μM desferal. Fur expression was induced by the addition of 10, 50, or 100 μM IPTG. Bacterial growth was monitored every hour by OD600 measurement. Mean ± SEM is presented, n = 3. Timepoints at which all strains’ OD600 values under iron starvation were significantly different from WT under iron repletion are indicated with an asterisk, p<0.05. (C) TbpB immunoblot as presented in Fig 5I, with the exception that the blot was overexposed to demonstrate low TbpB expression levels in WT under SGC and in Δfur/Plac::fur under SGC with increasing Fur induction. GCB, gonococcal base medium; IPTG, isopropyl β-D-thiogalactopyranoside; OD600, optical density at 600 nm; SGC, standard growth conditions; SEM, standard error of the mean.
(EPS)
Suspensions of WT FA1090 and isogenic knockout ΔmlaA bacteria standardized to an OD600 of 1.5 in GCBL were cultured in 96 well plates for 24 h in 5% CO2 at 37°C. Planktonic bacteria were removed prior to biofilm processing, serially diluted, and spotted onto GCB for CFU/mL enumeration. Mean ± SEM is presented for 12 biological replicates, each with 3 or 4 technical replicates, for a total of 46 datapoints. GCBL, gonococcal base liquid medium; GCB, gonococcal base medium; OD600, optical density at 600 nm.
(EPS)
Female BALB/c mice were inoculated intravaginally with approximately equal numbers of CFUs of WT and ΔmlaA/Plac::mlaA bacteria (~106 CFU total N. gonorrhoeae; 7 mice per group). Vaginal swabs taken on days 1, 3, and 5 post-infection were cultured for CFU/mL enumeration on solid media containing streptomycin (total bacteria) or media containing streptomycin and kanamycin (ΔmlaA/Plac::mlaA bacteria). Experiments were repeated three times and results are expressed as the geometric mean of the competitive index (CI): [mutant CFU (output) / WT CFU (output)] / [mutant CFU (input) / WT CFU (input)]. A CI > 1 indicates that the mutant was more fit during the competition. A value of 1 CFU was assigned for any strain not recovered from an infected mouse. CFU, colony forming unit.
(EPS)
Table 1 in S1 Text: Amino acid identity of members of the N. gonorrhoeae Mla operon with their E. coli homologs. Table 2 in S1 Text: Agar dilution assessment of WT, ΔmlaA, ΔmlaA/Plac::mlaA, and ΔmlaA/Plac::pldA MICs.
(DOCX)
(XLSX)
(XLSX)
(XLSX)
Data Availability Statement
Data are available via ProteomeXchange with identifier PXD008673.