Abstract
Objective
The aim of this study was to analyze the survivorship and clinical outcome of Cementless Spotorno (CLS) stem in young patients.
Methods
A total of 99 consecutive hip arthroplasties using CLS stem were performed on 84 patients younger than 50 years of age between 1993 and 2001. 63 patients were available for final follow-up (mean age: 39 ± 7.8 (range: 22–50)). Patients' Harris Hip Scores (HHS) and survivorship estimates were calculated. Radiographs were analyzed for acetabular implant status, canal fill index (CFI), stem alignment, osteolysis, and stress shielding.
Results
Mean follow-up time was 18 years (13–3), and mean HHS was 88.7 (58–100). Patients with femoral neck fracture had a more favorable functional outcome (p = 0.027), while those with stems in varus had lower scores (p = 0.017). 31 stems (49%) were undersized and 30 hips (47%) had perifemoral osteolysis. Acetabular impairment was strongly associated with osteolysis in Gruen zones 1 and 7 (p < 0.01). Seventeen of the osteolytic lesions occurred in Gruen zone 1, 4 lesions in zone 2, 9 in zone 6 and 22 in zone 7. Forty nine stems were well aligned, 10 were in varus and 5 in valgus. Six patients presented with grade 1 stress shielding, 42 with grade 2, 9 with grade 3 and 7 with grade 4. Pedestal formation was evident in 13 cases. Kaplan-Meier survivorship estimates at 18 years with revision for any reason as the end point and with septic revisions excluded were 91.2% (95% CI: 83.7%–98.7%) and 95.1% (95% CI: 89.5%–100%), respectively. There was no difference between survival estimates of patients with different etiologies.
Conclusion
CLS stems in young patients have high survival estimates in the long term with good-excellent results. Spotorno stems perform equally well in all etiologies with no difference in terms of survivorship.
Level of Evidence
Level IV Therapeutic study.
Keywords: Hip arthroplasty, Spotorno, Survivorship, Gruen, Osteolysis
Introduction
Total hip arthroplasty is one of the most successful orthopedic procedures ever developed, hence described by some authors as “operation of the century”.1 With good to excellent functional outcome, results remain satisfactory into the third decade. However, hip replacement in young patients remains a challenge, as high activity levels of these individuals increase risk of component wear and loosening, and the patients are likely to outlive their prosthesis.2, 3
CementLessSpotorno (CLS) stem is a tapered design introduced in 1983. Initially coupled with a CLS titanium expanding cup, it is not uncommon to combine Spotorno stems with various types of both cemented and cementless acetabular components.4, 5 Despite the problems associated with acetabular cups, Spotorno stems yielded good patient outcomes in mid-term and performed better than their acetabular companion, whether be it cemented or cementless, in terms of survivorship and need for revision.2, 3, 4, 6
Although used for more than two decades, studies on CLS stem survival cementless extending into third decade in young patients are relatively rare compared to cemented implants.7, 8, 9, 10, 11, 12, 13 We performed a retrospective study to report the mid-long term results and survivorship analysis of CLS stem in patients younger than 50 years of age. In addition, we analyzed the factors that might affect implant survival.
Patients and methods
99 consecutive hip arthroplasties using Spotorno stem (CementLess Spotorno; Protek/Zimmer, Zurich, Switzerland) and CLS expansion cup (CementLess Spotorno; Protek/Zimmer, Zurich, Switzerland) were performed on 84 patients younger than 50 years of age at the time surgery between 1993 and 2001 at single institution. Informed consent for surgery was obtained from all patients. Both acetabular and femoral components were implanted using the press-fit technique. Stem sizes ranging from 7 to 15 mm were available during the study period. 32 mm metal heads and polyethylene liners were used in all cases. All patients were operated using the posterolateral approach. No prophylaxis for heterotopic ossification was used. Patients were called for monthly follow-ups for the first 6 months and annually after two years. Following approval from institutional review board, patients were called by phone for a final follow-up.
Of the 84 patients (99 hips), 21 were lost to follow-up. 77 hips of 63 patients were either available for final follow-up with early postoperative radiographs or patient records indicated stem revision at certain time point. Minimum follow-up time was 13 years.
All 77 stems were included in survivorship analysis. Twelve femoral components had been revised, leaving 64 hips of 56 patients with unrevised stems available for clinical and radiological assessment. Patients' Harris Hip Scores (HHS) were calculated to determine clinical outcome, and radiographs were analyzed for acetabular implant status, canal fill index (CFI), stem alignment, osteolysis and stress shielding. One patient who was not willing revision surgery despite a dislocated hip with total stem loosening was excluded from stem assessment but included in the survivorship analysis. Patient demographics and indications for hip arthroplasty are listed in Table 1.
Table 1.
Previous studies on cementless arthroplasty in young patients.
| Series | Stem | Patients (Hips) | Etiology | Age | FU (yr) | Stem Survival |
|
|---|---|---|---|---|---|---|---|
| Aseptic/Radiographic Loosening | Revision/Failure for Any Reason | ||||||
| Carlson 20177 | Prodigy | 69 (82) | Mixed | 47 (18–72) | 11.4 (10–12) | 100% at 10 years | 88% at 10 years |
| Schmolders 20178 | SL-Plus | 77 (81) | Mixed | 48 (30–50) | 13.5 (10–17) | NA | 96.8% at 10 years. |
| McLaughlin 20169 | Taperloc | 91 (108) | Mixed | 36 (20–49) | 25 (20–29) | 100% at 29 years | 90% at 29 years |
| Biemond 201510 | CLS | 85 (100) | Mixed | 44 (16–50) | 18.4 (16–21) | 90.7% at 19 years | 88.6% at 19 years |
| Takenaga 201211 | Prodigy | 73 (82) | Mixed | 40 (17–50) | 12.0 (10–17) | 100% at 10–15 years | NA |
| Kim 201112 | Profile | 79 (110) | Mixed | 47 (21–49) | 18.4 (16–19) | 96% at 20 years | 96% at 20 years |
| Aldinger 200913 | CLS | 141 (154) | Mixed | 47 (13–55) | 17 (15–20) | 95% at 20 years | 90% at 20 years |
FU (yr); mean follow-up time in years.
All survival analyses are reported within 95% confidence limits.
Kaplan–Meier survivorship analysis with endpoint as revision/failure of the stem for any reason.
Kaplan–Meier survivorship analysis with endpoint as revision for aseptic/radiographic loosening.
Carlson et al 's study included because mean age of the patients is relatively young.
Prodigy (DePuy, Warsaw, Indiana), SL-Plus (Smith-Nephew Inc, Memphis, TN, USA), Taperloc (Zimmer Biomet, Warsaw, IN), CLS Spotorno (Zimmer, Warsaw, Indiana), Profile (DePuy, Warsaw, Indiana).
NA: not reported.
Radiographic analysis
At the final follow-up, AP and lateral radiographs of the hip and pelvis were taken and the following parameters were evaluated; acetabular cup migration, liner wear, femoral osteolysis, stress shielding and pedestal formation.
Evaluation of femoral stem stability was performed using the criteria described by Engh et al, and a femoral stem was regarded as loose if there was more than 2 mm radiolucency around the entire implant.14 Perifemoral osteolysis in forms of demarcated localized bone resorption or endosteal erosion was assessed with respect to zones described by Gruen et al5, 15, 16, 17, 18 (Fig. 1) CFI was defined as the ratio of stem and medullary canal width at the level of lesser trochanter and stems with CFI <0.80 were considered undersized.5 Severity of the femoral stress shielding was graded according to the criteria described by Engh et al19 Varus or valgus malalignment was defined as an angle of 2 or more between the longitudinal axes of femur and prosthesis stem.5 Pedestal formation was defined as formation of endosteal bone traversing the medullary canal and reaching the stem tip.
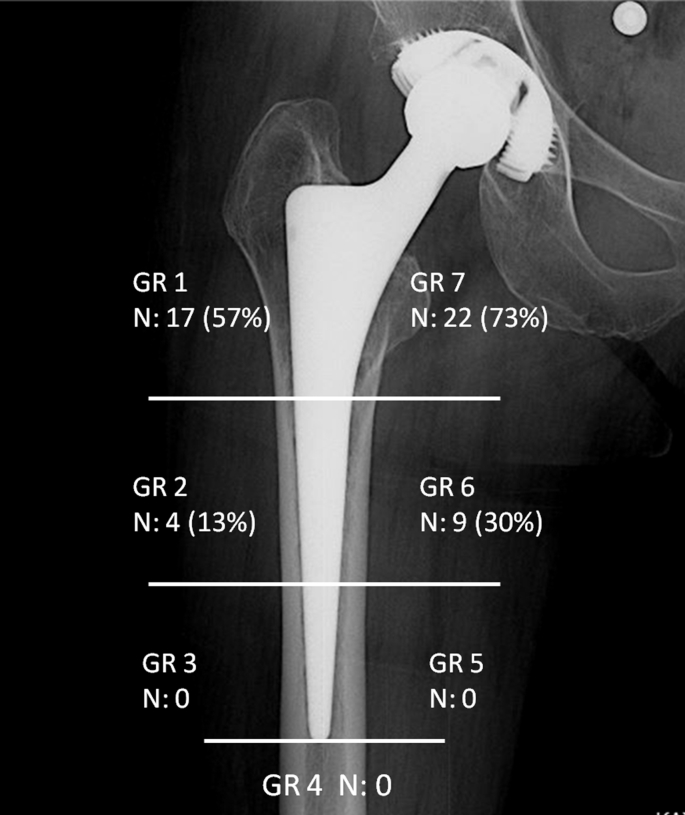
Fig. 1.
Distribution of femoral osteolysis according to zones described by Gruen.
Inter-teardrop line or inter-ischial line was used as fixed landmark to assess acetabular cup migration.20 Acetabular components that were revised, those that had broken wings or more than 4 mm linear insert wear as described by Livermore et al on plain radiographs, >5 mm migration or >5° tilting compared to initial postoperative radiograph were defined as impaired.5, 21
Statistical analysis
Shapiro Wilk test was used as normality test. Continuous variables were compared using Mann–Whitney U and Kruskal Wallis test when the data were not normally distributed Pearson chi-square and Fisher's exact tests were used to analyze categorical data. Correlations between variables were tested using Spearman correlation coefficients. Survivorship estimates for femoral stem were calculated using the Kaplan–Meier method, first with revision for any reason as end point and then with revision for aseptic loosening as the other end point. Influence of the etiology on survival rates was tested for statistical significance using log-rank test. IBM SPSS ver.23.0 software was used for statistical analysis. P < 0.05 was considered to be statistically significant.
Results
Twelve of the 77 hips required femoral revision. Five stems were revised due to periprosthetic infection; whereas 7 stems were revised because of aseptic loosening. Acetabular components were removed in all cases revised for periprosthetic infection. Of the 7 cases revised for aseptic reasons, 5 of them also required concurrent acetabular revision. One patient with a dislocated hip and a radiologically loose stem was offered revision surgery but declined. Patient demographics (gender, etiology, age at the time of operation and age at the time of last follow-up) were similar between patients with and without stem revision.
Of the 77 hips included in the study, 32 acetabular components (41.6%) had to be revised for aseptic reasons; whereas only 7 stems (9.1%) had to be removed during the study period for aseptic reasons.
Thirty one (49%) stems were undersized. Thirty hips (47%) had perifemoral osteolysis in various Gruen zones. Seventeen of the osteolytic lesions occurred in Gruen zone 1, 4 lesions in zone 2, 9 in zone 6 and 22 in zone 7 (Fig. 1). Forty nine stems were well aligned, 10 were in varus and 5 in valgus. Six patients presented with grade 1 stress shielding, 42 with grade 2, 9 with grade 3 and 7 with grade 4. Pedestal formation was evident in 13 cases.
Patients without femoral revision had a mean HHS of 88.7 (58–100). Patient HHSs were not correlated with age at the time of operation or at the time of last follow-up, whereas patient scores declined significantly with longer periods of follow-up (Spearman's rho with correlation significant at 0.01 level). Patients who had been operated for femoral neck fracture had a more favorable functional outcome than patients with DDH, primary coxarthrosis or inflammatory arthropathy (p = 0.027). Gender, history of acetabular revision, osteolysis, acetabular impairment and stem size did not influence HHSs. Patients whose stems were in varus malalignment had significantly lower scores compared to well aligned cases (p = 0.017).
Etiology, stem alignment, history of acetabular revision, gender and CFI did not affect prevalence of perifemoral osteolysis, whereas acetabular impairment was strongly associated with osteolysis in Gruen zones 1 (p < 0.01) and 7 (p < 0.01). Acetabular impairment did not seem to influence the lesions in zones 2 and 6.
Kaplan–Meier survivorship estimate for Spotorno stems with revision for any reason as the end point was 91.2% (95% CI: 83.7%–98.7%) at 18 years (Fig. 2). Log-rank regression analysis revealed lower survival rates for patients with femoral neck fracture compared to cases with primary coxarthrosis (p < 0.01) or DDH (p < 0.01). Survivorship of patients with rheumatoid arthritis was also compromised compared to patients with primary coxarthrosis (p = 0.042) (Fig. 3).
Fig. 2.
Kaplan–Meier survivorship estimates with 95% confidence intervals. Upper curve depicts survival with revision for aseptic reasons as the end point (95.1% at 18 years). Lower curve illustrates survival with revision for any reason as the end point (91.2% at 18 years).
Fig. 3.
Kaplan–Meier survivorship curves for different diagnoses with 95% confidence intervals. Survival estimates significantly lower for patients with femoral neck fracture compared to cases with primary coxarthrosis (p < 0.01) or DDH (p < 0.01). Survivorship of patients with rheumatoid arthritis significantly compromised compared to patients with primary coxarthrosis (p = 0.042). RA: Rheumatoid arthritis, CFF: Collum femoris fracture, DDH: Developmental dysplasia of the hip, OA: Osteoarthritis.
With infectious cases excluded and end point defined as revision for only mechanical reasons, stem survival was 95.1% (95% CI: 89.5%–100%) at 18 years (Fig. 2). Etiology of patients with aseptic loosening was rheumatoid arthritis in 3 cases, DDH in 3 cases, osteonecrosis in 1 case and hip fracture in another. Etiology and distribution of the patients with aseptic loosening are outlined in Table 2. There was no significant difference between survival estimates of patients with different etiologies.
Table 2.
Patient demographics and Diagnoses.
| Number of patients | 63 (77 hips) |
|---|---|
| Gender | |
| Female | 38 (60%) |
| Male | 25 (40%) |
| Mean age at surgery | 39 (22–50) |
| Mean age at last FU | 56.8 (37–73) |
| Mean FU (yr) | 18 (13–23) |
| Diagnosis | |
| DDH | 25 (31 hips) |
| Rheumatoid arthritis | 16 (20 hips) |
| Primary OA | 12 (13 hips) |
| CFF | 5 |
| Ankylosing spondilitis | 2 (3 hips) |
| Osteonecrosis | 2 |
| DDH with muscular dystrophy | 1 (2 hips) |
| Juvenile RA | 1 |
FU: Follow-up.
Yr: Years.
OA: Osteoarthritis.
CFF: Collum femoris fracture.
DDH: Developmental dysplasia of the hip.
RA: Rheumatoid arthritis.
Discussion
Total hip replacement in high demand patients remains a challenge, as younger age at surgery is related to increased polyethylene wear and decreased implant survivorship. Femoral components generally outperform their acetabular counterparts in terms of survivorship, and acetabular component survivorship is affected by patient age to a larger extend than the femoral side.2, 22, 23 Low revision rates of femoral components (9.1%) compared to acetabular revisions (41.6%) for aseptic complications in our series of young patients further extends the general notion. All of the acetabular components in our series were expansive cups with slits between metal lobes which expose pelvic bone to potential polyethylene debris.
Stem survivorship in our series was in parallel with the previous studies reporting good-excellent results with CLS Spotorno stem. Our results at 18 year with 95.1% survivorship estimate for aseptic loosening were the same as Evola et al 's at 23 years and were slightly inferior to studies with shorter follow-ups with 98–99% survivorship at 12–17 years.2, 4, 5, 6, 23 Results of our patient sample were not conclusive for 23 years survival estimate, making a direct comparison with Evola et al 's study difficult; however it is not wrong to assume that survivorship in our series will deteriorate below Evola et al 's with time. The main reason for the lower survival estimate in our series is due to younger age at the time of operation. Our patient series is limited to those younger than 50 years old (mean age 39 years), younger than in previous studies in the literature with mean age ranging from 47 to 60 years.2, 4, 5, 6 (Table 3). Longer time of follow-up was also a confounding factor, as survivorship estimates of shorter periods (97% at 15 years) were comparable to 99% survival in de Witte et al 's study whose follow-up was 8 years.2 The only study reporting higher survivorship estimate at longer follow-up is Terré’s, with 97% survival at 21 years.3 It is of particular interest that mean patient age at the time of implantation was 66, highest amongst the aforementioned studies, emphasizing the correlation between young age and increased rate of revision.
Table 3.
Diagnoses of patients with aseptic loosening.
| Failed stem | Stem Fail Ratio | |
|---|---|---|
| Osteonecrosis N:2 |
n: 1 | %50 |
| Hip fracture N:5 |
n: 1 | %20 |
| DDH N:31 |
n: 3 | %9.7 |
| Rheumatoid arthritis N:20 |
n: 3 | %15 |
N: Total number.
n: number of failed stems.
DDH: developmental dysplasia of the hip.
Several factors such as indications for surgery are reported to influence stem survivorship.22 When effect of etiological factors on implant survivorship was evaluated, our results yielded decreased stem survival in patients with femoral neck fracture or rheumatoid arthritis. With infectious cases excluded and end point defined as revision for only mechanical reasons, there was no significant difference between survival estimates of patients with different etiologies. Periprosthetic infection was more than 4 times more common in rheumatoid arthritis patients than non-rheumatoid patients, explaining the decreased survivorship estimates if infectious cases are not excluded. Higher prevalence of periprosthetic infections in cases with rheumatoid arthritis seems to be the reason behind relatively higher infection rate in our sample. Because our study focused on patients younger than 50 years old, prevalence of primary osteoarthritis decrease and relative rate of inflammatory arthritis increase.
There was only one revision for femoral neck fracture, and it was for septic reasons. Including the only revision case for CFF was statistically acceptable, however no conclusion should be derived from a single case and this result must be interpreted with caution. Spotorno stem performed equally well in all etiologies, and no difference was observed in terms of survivorship with infectious cases excluded. When grouping patients based on underlying disease, certain etiologies tend to cluster in certain age groups, with patients with primary coxarthrosis being generally older than those with rheumatoid arthritis. Because our patient sample was restricted to patients younger than 50 years, a more homogenous group was formed, eliminating the affect of age that would be otherwise evident between different etiologies.
Proximal femur is the first region on the femoral side that wear products and polyethylene debris can reach, and there is a tendency for macrophage induced bone resorption to begin in these regions in forms of linear radiolucencies or scalloping osteolytic regions.4, 23 In contrast to our cases with osteolysis in various Gruen zones in thirty hips (47%), femoral osteolysis was relatively rare and limited to Gruen zone 7 (6.6%) in Evola et al 's series.4 This is most likely to attributable to differences in acetabular wear between two studies, where only 5.4% of acetabular components were revised in Evola et al 's study. Similarly, Aldinger et al have reported no osteolysis and stress shielding around the stem.5 Even though several acetabular components in their series were revised, none of the intact cups had signs of polyethylene insert wear. The reason for lack of osteolysis around the stem despite high number of acetabular revision may be that weak initial stability and inadequate osteointegration are the primary factors in early loosening whereas wear products related osteolysis and loosening occur at a later period. Patients in our series were younger with longer time of follow-up, potential culprits for accelerated insert wear and subsequent acetabular loosening both inducing perifemoral lysis.2, 6 Acetabular impairment was strongly associated with osteolysis in Gruen zones 1 and 7, implicating the relation between acetabular wear products and perifemoral osteolysis as documented in previous studies.21
Importance of CFI index in implant survival is a point of debate.4, 6, 13 Muller et al have attributed the high survival rate of even the undersized stems to good initial stability and osteointegration provided by trapezoidal component design with microporous surface and longitudinal flutes.
Mean HHS in our series was 88.7 (58–100), slightly higher than majority of the previous studies on Spotorno stem with scores ranging from 84 to 87.4, 5, 6 Our study has the youngest sample of patients (mean 39 years) with one of the longest follow-up periods (mean 18 years). As Muller et al stated, since HHS is influenced by patients' activity level significantly, hip scores of young patients may reflect their overall health point to a greater extent than the outcome of their joint replacement procedure and may account for this difference. The fact that a direct correlation between patient age and functional outcome could not be drawn in this study should not be considered a potential flaw of this explanation since age range was relatively narrow. Patients clustered in narrow age range tend to have homogenous activity levels and the differences that would be otherwise observed in a group with wider age range do not occur. Young age of the patients serve to achieve higher HHSs which are partially trimmed as follow-up periods lengthen. Thus, longer follow-up may account for the lower HHS in our series despite the fact that our patient sample was younger compared to Streit et al 's study who reported mean HHS of 91.23
Main limitation of our study is the large numbers of patients lost to follow-up. In authors' institution in the early 2000s, patient files were transferred to digital media, and a substantial amount of patient data was either lost or inaccurately transcripted. It might be possible that number of patients lost to follow-up did not affect the failure rates since data loss was random and not based on patient satisfaction or surgical results. Still, the results of this study would be much more accurate and representative of general population if we could include the lost cases.
This study is retrospective in design and has all the limitations of a retrospective study. Not a real limitation but a confounding factor would be high incidence of periprosthetic infections. Although beyond the scope of this study, since survivorship analysis were based on aseptic failure, we believe that the discordance between the periprosthetic infection rates in our study and the literature results from higher number of patients with inflammatory arthritis. It is possible that high number of patients lost to follow-up caused the results to err on the side of increased infection rates. In our clinical practice, we have realized that arthroplasty patients with complications tend to refer to their surgeons rather than undergoing revision in other institutions. Patients with good outcome are more likely to get lost to follow-up and many do not show up for clinical evaluation till complications occur.
Conclusion
CLS stems in patients younger than 50 years of age have high survival estimates in the long term with good-excellent results. They outperform their acetabular counterparts in terms of survivorship with significantly lower revision rates. Spotorno stems perform equally well in all etiologies with no difference in terms of survivorship. Stem design provides good initial stability with low rates of loosening despite presence of numerous undersized femoral components.
Conflicts of interest
None of the authors have any conflict of interest.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Learmonth I.D., Young C., Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007 Oct 27;370(9597):1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 2.de Witte P.B., Brand R., Vermeer H.G., van der Heide H.J., Barnaart A.F. Mid-term results of total hip arthroplasty with the CementLessSpotorno (CLS) system. J Bone Joint Surg Am. 2011 Jul 6;93(13):1249–1255. doi: 10.2106/JBJS.I.01792. [DOI] [PubMed] [Google Scholar]
- 3.Terré R.A. Estimated survival probability of the Spotorno total hip arthroplasty after a 15- to 21-year follow-up: one surgeon's results. Hip Int. 2010;20(suppl 7):S70–S78. doi: 10.1177/11207000100200s713. [DOI] [PubMed] [Google Scholar]
- 4.Evola F.R., Evola G., Graceffa A. Performance of the CLS Spotorno uncemented stem in the third decade after implantation. Bone Joint J. 2014 Apr;96-B(4):455–461. doi: 10.1302/0301-620X.96B4.32607. [DOI] [PubMed] [Google Scholar]
- 5.Aldinger P.R., Thomsen M., Mau H., Ewerbeck V., Breusch S.J. Cementless Spotorno tapered titanium stems: excellent 10-15-year survival in 141 young patients. Acta Orthop Scand. 2003 Jun;74(3):253–258. doi: 10.1080/00016470310014157. [DOI] [PubMed] [Google Scholar]
- 6.Müller L.A., Wenger N., Schramm M., Hohmann D., Forst R., Carl H.D. Seventeen-year survival of the cementless CLS Spotorno stem. Arch Orthop Trauma Surg. 2010 Feb;130(2):269–275. doi: 10.1007/s00402-009-0969-7. [DOI] [PubMed] [Google Scholar]
- 7.Carlson S.W., Liu S.S., Callaghan J.J. Not all cementless femoral stems are created equal but the results may be comparable. Bone Joint J. 2017 Jan;99-B(1 supple A):14–17. doi: 10.1302/0301-620X.99B1.BJJ-2016-0269.R1. [DOI] [PubMed] [Google Scholar]
- 8.Schmolders J., Amvrazis G., Pennekamp P.H. Thirteen year follow-up of a cementless femoral stem and a threaded acetabular cup in patients younger than fifty years of age. Int Orthop. 2017 Jan;41(1):39–45. doi: 10.1007/s00264-016-3226-z. [DOI] [PubMed] [Google Scholar]
- 9.McLaughlin J.R., Lee K.R. Total hip arthroplasty with an uncemented tapered femoral component in patients younger than 50 Years of age: a minimum 20-year follow-up study. J Arthroplasty. 2016 Jun;31(6):1275–1278. doi: 10.1016/j.arth.2015.12.026. [DOI] [PubMed] [Google Scholar]
- 10.Biemond J.E., Venkatesan S., van Hellemondt G.G. Survivorship of the cementless Spotorno femoral component in patients under 50 years of age at a mean follow-up of 18.4 years. Bone Joint J. 2015 Feb;97-B(2):160–163. doi: 10.1302/0301-620X.97B2.34926. [DOI] [PubMed] [Google Scholar]
- 11.Takenaga R.K., Callaghan J.J., Bedard N.A., Liu S.S., Klaassen A.L., Pedersen D.R. Cementless total hip arthroplasty in patients fifty years of age or younger: a minimum ten-year follow-up. J Bone Joint Surg Am. 2012 Dec 5;94(23):2153–2159. doi: 10.2106/JBJS.L.00011. [DOI] [PubMed] [Google Scholar]
- 12.Kim Y.H., Kim J.S., Park J.W., Joo J.H. Comparison of total hip replacement with and without cement in patients younger than 50 years of age: the results at 18 years. J Bone Joint Surg Br. 2011 Apr;93(4):449–455. doi: 10.1302/0301-620X.93B4.26149. [DOI] [PubMed] [Google Scholar]
- 13.Aldinger P.R., Jung A.W., Pritsch M. Uncemented grit-blasted straight tapered titanium stems in patients younger than fifty-five years of age. Fifteen to twenty-year results. J Bone Joint Surg Am. 2009 Jun;91(6):1432–1439. doi: 10.2106/JBJS.H.00297. [DOI] [PubMed] [Google Scholar]
- 14.Engh C.A., McGovern T.F., Bobyn J.D., Harris W.H. A quantitative evaluation of periprosthetic bone-remodeling after cementless total hip arthroplasty. J Bone Joint Surg Am. 1992 Aug;74(7):1009–1020. [PubMed] [Google Scholar]
- 15.Gruen T.A., McNeice G.M., Amstutz H.C. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979 Jun;(141):17–27. [PubMed] [Google Scholar]
- 16.Willert H.G., Bertram H., Buchhorn G.H. Osteolysis in alloarthroplasty of the hip. The role of ultra-high molecular weight polyethylene wear particles. Clin Orthop Relat Res. 1990 Sep;258:95–107. [PubMed] [Google Scholar]
- 17.Zicat B., Engh C.A., Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg Am. 1995 Mar;77(3):432–439. doi: 10.2106/00004623-199503000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Johnston R.C., Fitzgerald R.H., Jr., Harris W.H., Poss R., Müller M.E., Sledge C.B. Clinical and radiographic evaluation of total hip replacement. A standard system of terminology for reporting results. J Bone Joint Surg Am. 1990 Feb;72(2):161–168. [PubMed] [Google Scholar]
- 19.Engh C.A., Bobyn J.D., Glassman A.H. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987 Jan;69(1):45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 20.Gokhale S., Soliman A., Dantas J.P. Variables affecting initial stability of impaction grafting for hip revision. Clin Orthop Relat Res. 2005 Mar;432:174–180. doi: 10.1097/01.blo.0000150103.75134.10. [DOI] [PubMed] [Google Scholar]
- 21.Livermore J., Ilstrup D., Morrey B. Effect of femoral head size on wear of the polyethylene acetabular component. J Bone Joint Surg Am. 1990 Apr;72(4):518–528. [PubMed] [Google Scholar]
- 22.Berry D.J., Harmsen W.S., Cabanela M.E., Morrey B.F. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002 Feb;84-A(2):171–177. doi: 10.2106/00004623-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Streit M.R., Schröder K., Körber M. High survival in young patients using a second generation uncemented total hip replacement. Int Orthop. 2012 Jun;36(6):1129–1136. doi: 10.1007/s00264-011-1399-z. [DOI] [PMC free article] [PubMed] [Google Scholar]