Abstract
Objective
The aim of this study was to evaluate the radiologic outcomes of open reduction and lateral plating with wiring in the treatment of Vancouver B2 periprosthetic femoral fractures.
Methods
We retrospectively recruited 37 patients treated with ORIF with lateral plating and wiring for Vancouver B2 fractures. The 27 patients (15 men and 12 women; mean age: 70.8 ± 8.3 years) without follow-up loss had achieved complete bony union without notable complications. The average union period was checked after operation with radiologic findings. Radiologic outcomes were evaluated by ipsilateral limb length discrepancy (LLD) and subsidence between immediate postoperative length and length at postoperative 1 year after adjusting for magnification differences. The average distance to which the retained stem sunk down was investigated between immediate postoperative radiographs and final radiographs showing union.
Results
Ten patients could not be evaluated, because of mortality or failure to follow up. The average time to union was 18.3 weeks, and the average distance of stem sinking was 2.5 ± 1.7 mm (range: 0–7.2 mm), which was significantly different between immediate postoperative radiographs and final radiographs. There was no case with loss of reduction or loss of fixation, requiring revision surgery.
Conclusion
Open reduction and lateral plating with wiring as a treatment for Vancouver B2 periprosthetic femoral fractures produced good radiologic outcomes with successful bony union. ORIF can be considered the alternative option for treating patients with Vancouver B2 PPF, instead of stem revision surgery.
Level of evidence
Level IV, Therapeutic study.
Keywords: Arthroplasty, Replacement, Hip, Femur, Hip fractures, Periprosthetic fractures
Introduction
Periprosthetic femoral fractures (PFF) following hemiarthroplasty or total hip arthroplasty (THA) are significant, challenging, and complex surgical problems because the presence of an intramedullary prosthesis does compromise fixation of fractures.1, 2, 3 The incidence of post-operative periprosthetic fractures reported in the literature varies, ranging from less than 1% after primary arthroplasty to up to 4% after revision arthroplasty, and this number appears to be on the rise.3, 4, 5 This is because of increasing patient longevity, more demanding activity levels that persist into advanced age, and the increasing rate of revision arthroplasty.6 PFF has been associated with significant morbidity and mortality.7, 8 In cases of PFF, the surgeon must be an expert in both arthroplasty and fracture repair.
PFF treatment depends on the location and the stability of the fractures, the stability of the femoral stem, the quality of bone, and the medical conditions and functional demands of the patients.9, 10 The most commonly accepted classification scheme is the Vancouver system developed by Duncan and Masri.10 According to this system, type B fractures involve the area of the femoral prosthesis and are further subclassified depending on the stability of the stem and surrounding bone quality: type B1 fractures (stable prosthesis) are indications for osteosynthesis, while type B2 (unstable prosthesis but adequate bone stock) and type B3 (unstable prosthesis and inadequate bone stock) are generally indications for complex stem revision surgery.1, 11, 12 However, stem revision surgery is difficult and entails a high risk for combined perioperative complications, rather than ORIF. Furthermore, internal fixation is required for unstable type B fractures, in combination with femoral stem revision, to secure the stability of the femoral stem and the periprosthetic unstable bone stock.13, 14, 15 The purpose of this study was to investigate the radiologic outcomes for the treatment of Vancouver type B2 fractures by open reduction and internal fixation using lateral plating and wiring. (see Table 1).
Table 1.
Vancouver classification of postoperative periprosthetic femoral fracture.
| Type | Location | Recommended treatment |
|---|---|---|
| A | Around trochanter | |
| AG | Great trochanter | Conservative or surgical if associated with a loose stem |
| AL | Lesser trochanter | |
| B | Around or just distal to the stem | |
| B1 | Stable fixed stem | ORIF with cerclage and struts and plate |
| B2 | Loose stem | Long stem revision with or without ORIF |
| B3 | Loose stem with poor bone stock | Revision and structural allograft |
| C | Well below the stem | ORIF with plate systems |
Abbreviation; ORIF, open reduction and internal fixation.
Material and methods
The Institutional Review Board of – Hospital approved the design and protocol of this study. The inclusion criteria were: unstable periprosthetic fracture with loosening of the femoral stem around the proximal femur (Vancouver classification type B2 PFF), no contraindication to anesthesia, and the ability to walk independently pre-injury with or without aids. The exclusion criteria were: loosening of the stem and deficiency of the proximal femur because of osteolysis, osteoporosis, or fracture comminution (Vancouver classification type B3 PFF), or the patient died or was lost to follow up within postoperative 1 year. We treated 37 consecutive patients with lateral plating and wiring. Ten patients were excluded; 6 patients had died, and 4 patients were lost to follow-up within 1 year after the surgery. The average age of the remaining 27 patients (15 men and 12 women) at the time of the operation was 70.8 ± 8.3 years (range, 51–101 years). The type of femoral stem was cementless type in all cases. However, there were no cases of short stems or revision long stems. Mean body mass index (BMI) was 22.5 ± 4.3 kg/㎡, and mean bone mineral density (BMD) using dual-energy X-ray absorptiometry (DXA) T-score of L1-4 was −2.9 ± 1.3. All cases of this study were postoperative periprosthetic fractures, and occurred on average 71.1 ± 74.2 months (range 2–300 months) (Table 2). All patients were operated on by a single senior surgeon (J.S.P). For diaphyseal fracture reduction, the direct lateral approach was used. The patient was placed in the lateral decubitus position and the hip was flexed to 30°. The fracture site was exposed over the lateral thigh. After accurate reduction, internal fixation of the fracture was performed with a lateral locking plate (LCP plate, Depuy Synthes, West Chester, PA) and locking screws (5 mm diameter, bicortical self-tapping, Depuy Synthes, West Chester, PA) and cerclage wires. At postoperative 2 weeks, patients walked with restricted weight bearing and use of assistive devices. Patients were followed up at 6 weeks, 3, 6, and 9 months, and 1 year after surgery in our outpatient clinic. At the follow-up visits, radiographs were taken, and complete union was considered as cortical continuity in all 4 different views (femur AP, lateral view, and both oblique views). At each postoperative visit, stem subsidence and radiologic limb length shortening were measured, and magnification adjustment was performed.
Table 2.
Summary of patient characteristics.
| Patients (n = 27) | |
|---|---|
| Age (years)a | 70.8 ± 8.3 (50–101) |
| Gender | Male: 15 |
| Female: 12 | |
| BMI (kg/m2)a | 22.5 ± 4.3 (16.4–37.6) |
| BMD (DXA T-score; L1-4)a | −2.9 ± 1.3 (−5.4∼−1.2) |
| Occurrence of periprosthetic fracture after primary surgery (months) | 71.1 ± 74.2 (2–300) |
| Fracture pattern | Spiral: 19 |
| Comminuted: 5 | |
| oblique: 3 | |
| Operation time (min.)a | 120.3 ± 31.8 (85–200) |
| Type of femoral stem | Cementless stems in all cases |
n, number of patients; BMI, body mass index; BMD, bone mineral density; DXA, dual-energy X-ray absorptiometry; min, minute.
Data are presented as mean ± standard deviation (range).
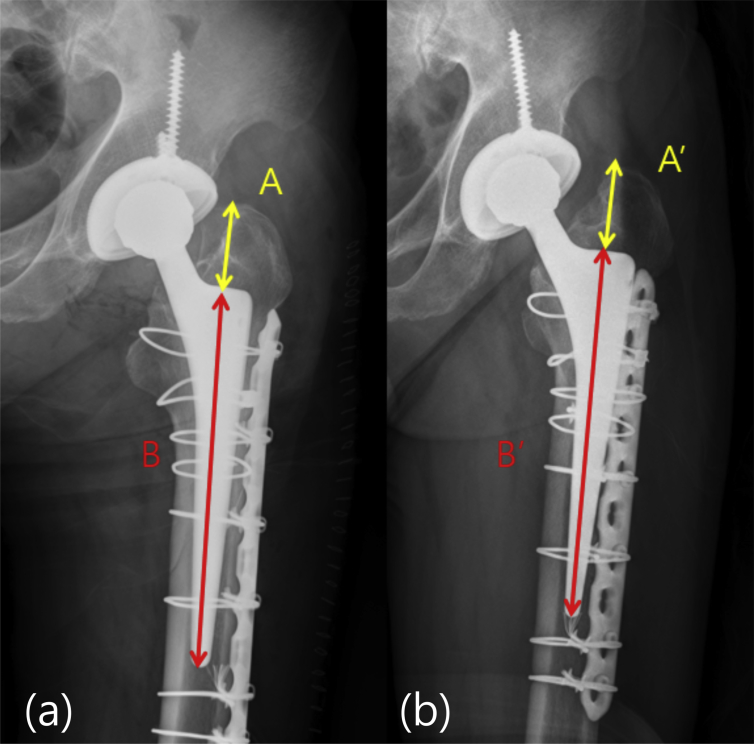
Radiologic outcomes were evaluated by ipsilateral limb length discrepancy (LLD) and subsidence between immediate postoperative length and length at postoperative 1 year after adjusting for magnification differences. Subsidence was assessed from the greater trochanter to the upper margin of the stem in PPF patients (See Fig. 1, A: immediate postoperative length; A’: length at postoperative 1 year). Magnification adjustment was performed using the ratio of stem length immediate following the operation to that 1 year later (See Fig. 1, B: immediate postoperative stem length; B’: the length of the stem at postoperative 1 year). Shortening of the limb (subsidence) was measured, considering differences in magnification. All measurements on radiographs were subsequently made on a 19-inch LCD monitor.
Fig. 1.
Measurement of limb length discrepancy using stem subsidence after 1 year. Adjusted for differences in magnification. (a) Immediate postoperative radiograph of a patient treated with open reduction and internal fixation with plate after periprosthetic fracture (b) After 1 year, substantial sinking of the stem can be seen on plain radiograph. B2 periprosthetic fractures with plate fixation. (A: immediate postoperative length, A’: length at postoperative 1 year) from greater trochanter to upper margin of femoral stem (B: immediate postoperative stem length, B’: stem length at postoperative 1 year), adjusted for magnification. *Radiologic limb length discrepancy (shortening) = {A × (B’/B)}- A’.
*Radiologic limb length discrepancy (shortening) = A x (B’/B)}- A’
Reliability was defined as the consistency of the measurement. Radiologic limb length discrepancy were checked by two examiners (JHN, SH). The intra-observer reliability of each method was assessed using the values measured by one examiner (JHN), who performed the reassessment three weeks later.16 The inter-observer reliability of each method was assessed by the same two examiners. All measurements were made without any knowledge of the patient's clinical information or the findings of the other examiners. The radiographs and scans were presented to each examiner in random order by a research assistant who did not participate in the reliability sessions.
Baseline patient characteristics and perioperative clinical data were analyzed for all patients, and by gender and operation type with descriptive statistics. Bi-variable tests of association were based on either Pearson's Chi-square or Fisher's exact test for categorical variables. Paired t-tests and Chi-square tests were used to assess differences between immediate postoperative radiographs and final radiographs. The ICCs and their 95% CIs were used to summarize the interobserver reliability in a single measurement. The ability of a test to show intra- and interobserver reliability was evaluated using the two-way random effects model assuming a single measurement and absolute agreement. An ICC of 1 means perfect reliability and an ICC of 0 means the opposite. All tests were two-sided, and statistical significance was taken as a p value < 0.05. Statistical analysis was performed using SPSS statistical software (version 21.0; IBM, Armonk, New York).
Results
Within 1 year after operation, 6 patients were excluded from the study, because they were expired due to other medical problems. An additional 4 patients were lost to follow-up (follow-up rate 79% (27/37).
The remaining 27 patients had achieved complete bony union without notable complications (Table 2). The average latency to union was 19.2 ± 3.9 weeks (range, 15–24 weeks) and the average extent of stem sinking was 2.5 ± 1.7 mm (range, 0–7.4 mm), which was statistically significant (p = 0.000). In radiologic measurements of two examiners, the intra-class correlation was 0.992 (95% CI 0.982 to 0.997), the inter-class correlation was 0.971 (95% CI 0.933 to 0.988) (Table 3).
Table 3.
Intraclass and interclass correlation coefficients.
| Intra-observer interaclass correlation coefficient | ||||
|---|---|---|---|---|
| ICC | 95% confidence interval |
F test with true value 0 |
||
| Lower bound | Upper bound | p-value | ||
| Single measure | 0.997 | 0.995 | 0.999 | 0.000 |
| Average measure |
0.992 |
0.982 |
0.997 |
0.000 |
| Inter-observer interaclass correlation coefficient | ||||
| Single measure | 0.944 | 0.875 | 0.975 | 0.000 |
| Average measure | 0.971 | 0.933 | 0.988 | 0.000 |
ICC, intraclass correlation.
Two-way random model where both people effects and measures effects are random. A single measurement and absolute agreement are used for intraclass correlation coefficients.
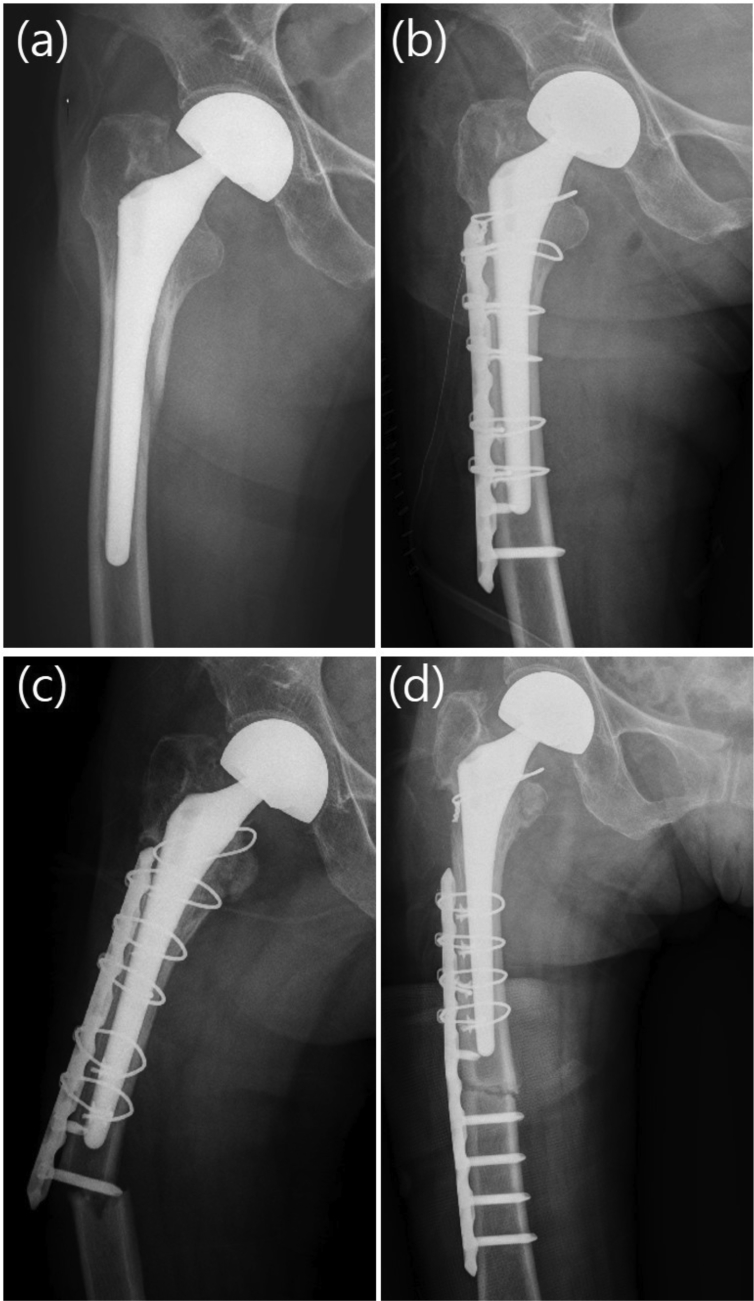
There was no case of reduction loss or fixation loss requiring revision surgery. There was no case of infection or nonunion. But, there is 1 complication after these operation, because of using insufficient length of plate. one patient, an 80-year-old woman, fell down while walking and she had fracture at the distal end of plate. The patient previously had undergone surgery using lateral plating and wiring due to Vancouver classification type B2 PFF 11 months ago, and reoperation was done and she achieved bony union again (Fig. 2). In addition, all patients enrolled in the study were described in Table 4.
Fig. 2.
Case: A 80-year-old woman. (a) Simple radiograph showed a Vancouver type B2 periprosthetic femoral fracture. (b) This patient treated by an osteosynthesis using a lateral plating and wiring. (c) Eleven months after surgery, bony union was obtained. She fell and sustained a femoral fracture at the distal end of plate, classified as Vancouver type C periprosthetic fracture. (d) Postoperative anteroposterior radiographs that was treated with a lateral plating and wiring.
Table 4.
Details of patient characteristics and implant designs.
| Case | Age (years) |
Gender | Fracture Pattern |
Union Period (month) |
Stem Subsidence (mm) |
Complication | Operation Time (min.) |
Type of femoral prosthesis |
||
|---|---|---|---|---|---|---|---|---|---|---|
| Cement | Coating | |||||||||
| 1 | 83 | Female | Comminuted | 24 | 3.2 | None | 115 | Cementless | Proximal | Taperlock stem (Biomet) |
| 2 | 66 | Male | Spiral | 16 | 1.1 | None | 125 | Cementless | Extensive | C2 stem (Lima) |
| 3 | 76 | Male | Spiral | 22 | 2.4 | None | 105 | Cementless | Extensive | CLS stem (Zimmer) |
| 4 | 71 | Female | Spiral | 18 | 3.3 | None | 130 | Cementless | Proximal | Omnifit stem (Stryker) |
| 5 | 68 | Male | Spiral | 16 | 0.2 | None | 120 | Cementless | Extensive | C2 stem (Lima) |
| 6 | 50 | Female | Spiral | 20 | 0.6 | None | 130 | Cementless | Extensive | C2 stem (Lima) |
| 7 | 72 | Male | Comminuted | 20 | 7.4 | None | 75 | Cementless | Extensive | CLS stem (Zimmer) |
| 8 | 66 | Male | Spiral | 16 | 0.8 | None | 140 | Cementless | Extensive | CLS stem (Zimmer) |
| 9 | 82 | Female | Spiral | 24 | 2.1 | None | 90 | Cementless | Proximal | Versys stem (Zimmer) |
| 10 | 54 | Female | Spiral | 15 | 2.3 | None | 105 | Cementless | Extensive | C2 stem (Lima) |
| 11 | 80 | Male | oblique | 20 | 3.8 | None | 120 | Cementless | Extensive | Omnifit stem (Stryker) |
| 12 | 63 | Male | Spiral | 16 | 1.7 | None | 155 | Cementless | Proximal | Revitan stem (Zimmer) |
| 13 | 74 | Female | Spiral | 24 | 0.7 | Refracture | 85 | Cementless | Extensive | Omnifit stem (Stryker) |
| 14 | 79 | Female | Spiral | 24 | 6.5 | None | 90 | Cementless | Proximal | CLS stem (Zimmer) |
| 15 | 57 | Female | Spiral | 16 | 1.3 | None | 150 | Cementless | Extensive | Omnifit stem (Stryker) |
| 16 | 64 | Male | oblique | 18 | 1.7 | None | 200 | Cementless | Extensive | Revitan stem (Zimmer) |
| 17 | 76 | Male | Comminuted | 20 | 2.8 | None | 135 | Cementless | Proximal | Taperlock stem (Biomet) |
| 18 | 68 | Male | Spiral | 20 | 2.9 | None | 155 | Cementless | Extensive | CLS stem (Zimmer) |
| 19 | 72 | Male | Comminuted | 24 | 3.7 | None | 195 | Cementless | Extensive | C2 stem (Lima) |
| 20 | 76 | Female | Spiral | 24 | 2.2 | None | 115 | Cementless | Extensive | Wagner cone stem (Zimmer) |
| 21 | 73 | Male | Comminuted | 18 | 2.0 | None | 90 | Cementless | Extensive | C2 stem (Lima) |
| 22 | 71 | Female | Spiral | 24 | 1.0 | None | 135 | Cementless | Proximal | Omnifit stem (Stryker) |
| 23 | 67 | Male | Spiral | 20 | 2.2 | None | 85 | Cementless | Extensive | Wagner cone stem (Zimmer) |
| 24 | 82 | Male | Oblique | 24 | 1.9 | None | 120 | Cementless | Proximal | Omnifit stem (Stryker) |
| 25 | 75 | Male | Spiral | 14 | 2.5 | None | 110 | Cementless | Extensive | C2 stem (Lima) |
| 26 | 73 | Female | Spiral | 12 | 4.5 | None | 85 | Cementless | Extensive | C2 stem (Lima) |
| 27 | 74 | Female | Spiral | 12 | 1.7 | None | 90 | Cementless | Extensive | C2 stem (Lima) |
Discussion
Recently, PFF after hip arthroplasty is a growing problem; it affects an increasing number of patients each year. Treatment options include traction, open reduction, and internal fixation of the fracture while leaving the stem in situ, and femoral revision with or without adjunctive internal fixation.2, 17, 18, 19, 20 Because of the advantages of early mobilization and more favorable results in terms of disunion and stem loosening, surgical management of PFF is generally preferable in patients who are medically stable.12, 21, 22 About 86% of all PFF cases are Vancouver type B fractures (type B2 or B3), and 70% of type B fractures that occur are associated with a loose stem (type B2) following primary THA.17 It is generally recommended that Vancouver B2 fractures should be treated with a long femoral stem revision to restore stability of the femoral prosthesis and to obtain sufficient intramedullary fixation of the fractures. This strategy permits early weight bearing and therefore improved mobility compared with treatment with osteosynthesis and protected weight bearing.1, 18, 23, 24, 25 However, no single surgical recommendation has gained universal acceptance.
Patients with PFF have increased mortality.26 In several studies, the rate of revision THA associated with periprosthetic fracture was found to be significantly higher than that of hip fractures requiring primary joint replacement surgery and revision for aseptic loosening.27, 28, 29 Generally, stem revision surgery requires a longer operation time, more blood loss, extensive soft tissue stripping, more loss of bone stock, and increased risk of infection, substantially increasing perioperative morbidity and mortality. In this study, which used ORIF to treat Vancouver type B2 PFF, rather than revision arthroplasty, minimized perioperative complications. Several authors have reported that fixation of PFF using plates is a reliable treatment option associated with a low rate of complications.13, 30, 31 Niikura et al treated select Vancouver type B2 patients with ORIF, achieved reliable outcomes, and suggested that decisions regarding the treatment of PFF should take into account not only the algorithmic approach of the Vancouver system but also on an assessment of each patient's physical status and activity level.12 To successfully apply this strategy, the fracture location relative to the femoral prosthesis, implant stability, surrounding bone quality, and the patient's medical and functional status must be considered.5, 11, 31 One of the challenges for ORIF of PFF is to achieve sufficient fixation in the proximal fragment around the zone of the femoral prosthesis.32 Cables are typically supplemented with screws in the trochanteric region or with unicortical locked screws in the zone of the prosthesis.12, 33, 34, 35 Relying on unicortical locked screws without cables should be avoided, as these constructs result in inadequate rotational control.1 In a biomechanical study, only proximal cable fixation was shown to provide significantly less axial stability compared with methods where cables and locked or unlocked screws were used, and proximal unicortical locking screws without cables were associated with a statistically significant difference in load failure compared with the cable group.33, 36 Gulsen et al investigate the biomechanics of periprosthetic fractures fixation, and noted B2 fractures union is not satisfactory and suggest additional allograft application concomitant with plating.37 The primary objective of this study was to determine the union rate of PFF using ORIF, rather than revision arthroplasty. In this study, all cases achieved bony union without notable complications that would have required additional surgery, except 1 patient of refracture at the distal tip of plate. Radiologic shortening by stem subsidence could arise physiologically during fracture healing.24, 38 Munro et al reported that subsidence was observed in 24% of patients, although the majority of cases were less than 3 mm, and only 9% subsided more than 3 mm.25 Mulay et al reported a mean subsidence of 5 mm (range, 2–10 mm) in 17 of 24 patients 48. It should be noted that a similar rate of subsidence has been reported after revision surgery for aseptic loosening.39, 40, 41
Our study has several limitations. First, it is retrospective in design and has no control group. Second, it involved a relatively short follow-up time, absence of cemented stem cases. Third, radiologic landmarks were somewhat ambiguous and depend on the patient's exact positioning, such as hip flexion or extension and internal or external rotation. Finally, we could not evaluate postoperative clinical outcomes such as ambulatory status and functional scoring. The mobility of these patients is so low, that it is difficult to come to the hospital for outpatient care and functional evaluation without a caregiver.
Conclusions
In this study, ORIF of unstable stem could lead slight subsidence of stem, however there was no case of reduction loss or fixation loss requiring revision surgery.
Despite of some limitations, treating Vancouver B2 cementless PFF with open reduction and internal fixation by lateral plating with wiring produced good radiologic outcomes with successful bony union, and minimized perioperative complications in our study. ORIF can be considered the alternative option for treating patients with Vancouver B2 PPF, instead of stem revision surgery.
Disclosure of conflicts of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgement
Jong-Seok Park and Sijohn Hong equally contributed to this work, and should be considered co-first authors. And this work was supported by the Soonchunhyang University Research Fund.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Ricci W.M. Periprosthetic femur fractures. J Orthop Trauma. 2015;29(3):130–137. doi: 10.1097/BOT.0000000000000282. [DOI] [PubMed] [Google Scholar]
- 2.Lewallen D.G., Berry D.J. Periprosthetic fracture of the femur after total hip arthroplasty: treatment and results to date. Instr Course Lect. 1998;47:243–249. [PubMed] [Google Scholar]
- 3.Younger A.D.J., Duncan C. Periprosthetic hip and knee fractures: the scope of the problem. Instr Course Lect. 1997;47:251–256. [PubMed] [Google Scholar]
- 4.Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury. 2007;38(6):651–654. doi: 10.1016/j.injury.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 5.Soenen M., Lautridou C., Lebel B. Periprosthetic fractures around total hip and knee arthroplasty. Review of the literature. Rev Chir Orthop Reparatrice Appar Mot. 2006;92(5 Suppl):2S44–42S51. [PubMed] [Google Scholar]
- 6.Haasper C., Enayatollahi M.A., Gehrke T. Treatment of Vancouver type B2 periprosthetic femoral fractures. Int Orthop. 2015;39(10):1989–1993. doi: 10.1007/s00264-015-2959-4. [DOI] [PubMed] [Google Scholar]
- 7.Klein G.R., Parvizi J., Rapuri V. Proximal femoral replacement for the treatment of periprosthetic fractures. J Bone Joint Surg Am. 2005;87(8):1777–1781. doi: 10.2106/JBJS.D.02420. [DOI] [PubMed] [Google Scholar]
- 8.Sidler-Maier C.C., Waddell J.P. Incidence and predisposing factors of periprosthetic proximal femoral fractures: a literature review. Int Orthop. 2015;39(9):1673–1682. doi: 10.1007/s00264-015-2721-y. [DOI] [PubMed] [Google Scholar]
- 9.Della Rocca G.J., Leung K.S., Pape H.C. Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma. 2011;25(Suppl 2):S66–S70. doi: 10.1097/BOT.0b013e31821b8c28. [DOI] [PubMed] [Google Scholar]
- 10.Duncan C.P., Masri B.A. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 11.Moazen M., Jones A.C., Jin Z., Wilcox R.K., Tsiridis E. Periprosthetic fracture fixation of the femur following total hip arthroplasty: a review of biomechanical testing. Clin Biomech (Bristol, Avon) 2011;26(1):13–22. doi: 10.1016/j.clinbiomech.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Niikura T., Lee S.Y., Sakai Y., Nishida K., Kuroda R., Kurosaka M. Treatment results of a periprosthetic femoral fracture case series: treatment method for Vancouver type b2 fractures can be customized. Clin Orthop Surg. 2014;6(2):138–145. doi: 10.4055/cios.2014.6.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lunebourg A., Mouhsine E., Cherix S., Ollivier M., Chevalley F., Wettstein M. Treatment of type B periprosthetic femur fractures with curved non-locking plate with eccentric holes: retrospective study of 43 patients with minimum 1-year follow-up. Orthop Traumatol Surg Res. 2015;10(3):277–282. doi: 10.1016/j.otsr.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 14.Masri B.A., Meek R.M., Duncan C.P. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res. 2004;(420):80–95. doi: 10.1097/00003086-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 15.O'Shea K., Quinlan J.F., Kutty S., Mulcahy D., Brady O.H. The use of uncemented extensively porous-coated femoral components in the management of Vancouver B2 and B3 periprosthetic femoral fractures. J Bone Joint Surg Br. 2005;87(12):1617–1621. doi: 10.1302/0301-620X.87B12.16338. [DOI] [PubMed] [Google Scholar]
- 16.McKelvie S.J. Does memory contaminate test-retest reliability? J Gen Psychol. 1992;119(1):59–72. doi: 10.1080/00221309.1992.9921158. [DOI] [PubMed] [Google Scholar]
- 17.Lindahl H., Malchau H., Herberts P., Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20(7):857–865. doi: 10.1016/j.arth.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Parvizi J., Vegari D.N. Periprosthetic proximal femur fractures: current concepts. J Orthop Trauma. 2011;25(Suppl 2):S77–S81. doi: 10.1097/BOT.0b013e31821b8c3b. [DOI] [PubMed] [Google Scholar]
- 19.Pike J., Davidson D., Garbuz D., Duncan C.P., O'Brien P.J., Masri B.A. Principles of treatment for periprosthetic femoral shaft fractures around well-fixed total hip arthroplasty. J Am Acad Orthop Surg. 2009;17(11):677–688. doi: 10.5435/00124635-200911000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Ricci W.M., Haidukewych G.J. Periprosthetic femoral fractures. Instr Course Lect. 2009;58:105–115. [PubMed] [Google Scholar]
- 21.Haddad F.S., Duncan C.P., Berry D.J., Lewallen D.G., Gross A.E., Chandler H.P. Periprosthetic femoral fractures around well-fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg Am. 2002;84-A(6):945–950. [PubMed] [Google Scholar]
- 22.Lee S.R., Bostrom M.P. Periprosthetic fractures of the femur after total hip arthroplasty. Instr Course Lect. 2004;53:111–118. [PubMed] [Google Scholar]
- 23.Broden C., Mukka S., Muren O. High risk of early periprosthetic fractures after primary hip arthroplasty in elderly patients using a cemented, tapered, polished stem. Acta Orthop. 2015;86(2):169–174. doi: 10.3109/17453674.2014.971388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drexler M., Dwyer T., Chakravertty R., Backstein D., Gross A.E., Safir O. The outcome of modified extended trochanteric osteotomy in revision THA for Vancouver B2/B3 periprosthetic fractures of the femur. J Arthroplasty. 2014;29(8):1598–1604. doi: 10.1016/j.arth.2014.03.020. [DOI] [PubMed] [Google Scholar]
- 25.Munro J.T., Garbuz D.S., Masri B.A., Duncan C.P. Tapered fluted titanium stems in the management of Vancouver B2 and B3 periprosthetic femoral fractures. Clin Orthop Relat Res. 2014;472(2):590–598. doi: 10.1007/s11999-013-3087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Franklin J., Malchau H. Risk factors for periprosthetic femoral fracture. Injury. 2007;38(6):655–660. doi: 10.1016/j.injury.2007.02.049. [DOI] [PubMed] [Google Scholar]
- 27.Anakwe R.E., Aitken S.A., Khan L.A. Osteoporotic periprosthetic fractures of the femur in elderly patients: outcome after fixation with the LISS plate. Injury. 2008;39(10):1191–1197. doi: 10.1016/j.injury.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 28.Bhattacharyya T., Chang D., Meigs J.B., Estok D.M., 2nd, Malchau H. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am. 2007;89(12):2658–2662. doi: 10.2106/JBJS.F.01538. [DOI] [PubMed] [Google Scholar]
- 29.Young S.W., Walker C.G., Pitto R.P. Functional outcome of femoral peri prosthetic fracture and revision hip arthroplasty: a matched-pair study from the New Zealand Registry. Acta Orthop. 2008;79(4):483–488. doi: 10.1080/17453670710015463. [DOI] [PubMed] [Google Scholar]
- 30.Kumar V., Kanabar P., Owen P.J., Rushton N. Less invasive stabilization system for the management of periprosthetic femoral fractures around hip arthroplasty. J Arthroplasty. 2008;23(3):446–450. doi: 10.1016/j.arth.2007.01.028. [DOI] [PubMed] [Google Scholar]
- 31.Park S.K., Kim Y.G., Kim S.Y. Treatment of periprosthetic femoral fractures in hip arthroplasty. Clin Orthop Surg. 2011;3(2):101–106. doi: 10.4055/cios.2011.3.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lever J.P., Zdero R., Nousiainen M.T., Waddell J.P., Schemitsch E.H. The biomechanical analysis of three plating fixation systems for periprosthetic femoral fracture near the tip of a total hip arthroplasty. J Orthop Surg Res. 2010;5(45):45. doi: 10.1186/1749-799X-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Demos H.A., Briones M.S., White P.H., Hogan K.A., Barfield W.R. A biomechanical comparison of periprosthetic femoral fracture fixation in normal and osteoporotic cadaveric bone. J Arthroplasty. 2012;27(5):783–788. doi: 10.1016/j.arth.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 34.Wood G.C., Naudie D.R., McAuley J., McCalden R.W. Locking compression plates for the treatment of periprosthetic femoral fractures around well-fixed total hip and knee implants. J Arthroplasty. 2011;26(6):886–892. doi: 10.1016/j.arth.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 35.Zdero R., Walker R., Waddell J.P., Schemitsch E.H. Biomechanical evaluation of periprosthetic femoral fracture fixation. J Bone Joint Surg Am. 2008;90(5):1068–1077. doi: 10.2106/JBJS.F.01561. [DOI] [PubMed] [Google Scholar]
- 36.Moazen M., Mak J.H., Etchels L.W. Periprosthetic femoral fracture--a biomechanical comparison between Vancouver type B1 and B2 fixation methods. J Arthroplasty. 2014;29(3):495–500. doi: 10.1016/j.arth.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 37.Gulsen M., Karatosun V., Uyulgan B. The biomechanical assessment of fixation methods in periprosthetic femur fractures. Acta Orthop Traumatol Turc. 2011;45(4):266–269. doi: 10.3944/AOTT.2011.2338. [DOI] [PubMed] [Google Scholar]
- 38.Suh Y.S., Nho J.H., Kim S.M., Hong S., Choi H.S., Park J.S. Clinical and radiologic outcomes among bipolar hemiarthroplasty, compression hip screw and proximal femur nail antirotation in treating comminuted intertrochanteric fractures. Hip Pelvis. 2015;27(1):30–35. doi: 10.5371/hp.2015.27.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kwong L.M., Miller A.J., Lubinus P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: a 2- to 6-year follow-up study. J Arthroplasty. 2003;18(3 Suppl 1):94–97. doi: 10.1054/arth.2003.50083. [DOI] [PubMed] [Google Scholar]
- 40.Ovesen O., Emmeluth C., Hofbauer C., Overgaard S. Revision total hip arthroplasty using a modular tapered stem with distal fixation: good short-term results in 125 revisions. J Arthroplasty. 2010;25(3):348–354. doi: 10.1016/j.arth.2008.11.106. [DOI] [PubMed] [Google Scholar]
- 41.Rodriguez J.A., Deshmukh A.J., Klauser W.U., Rasquinha V.J., Lubinus P., Ranawat C.S. Patterns of osseointegration and remodeling in femoral revision with bone loss using modular, tapered, fluted, titanium stems. J Arthroplasty. 2011;26(8):1409–1417. doi: 10.1016/j.arth.2011.06.021. e1401. [DOI] [PubMed] [Google Scholar]