Abstract
Objectives
The aim of this study was to evaluate the clinical and radiological results of the surgical treatment of acetabular fractures using modified Stoppa approach.
Methods
A total of 57 patients (mean age 37.8 years; range 15–84) who underwent surgical treatment for acetabular fracture with modified Stoppa approach from February 2013 to June 2016 were included into the study. The mean follow-up time was 28.1 months (range 24–35). The records were reviewed for fracture patterns, time to surgery, operative time, blood loss, reduction quality, and perioperative complications. Reduction quality was graded as anatomic, imperfect, or poor. The Harris Hip Score (HHS) and Merle d'Aubigné score were used for functional evaluation.
Results
Among the 63 acetabulum fractures of the 57 patients, 27 were associated with both columns, 12 were T-type fractures, 10 were transverse, 7 were anterior column/posterior hemitransverse, 5 were anterior column, and 2 were anterior wall fracture. A single surgeon performed all operations. Pfannenstiel incision was used in the first 19 cases while vertical midline incision in the remaining 38 cases. Average time to operation was 5.5 days, and supplemental lateral windows were used in 17 (29.8%) patients. Average blood loss and operation times were 660 mL and 152 min, respectively. Radiological outcomes were anatomic, imperfect, and poor in 52 (82.5%), 9 (14.2%), and 2 (3.2%) of the acetabulum fractures, respectively. Clinical outcomes at 2 years with HHS and Merle d’Aubigné scores were mean 86.6 (range 66–96) (Excellent in 27, good in 23, fair in 4, poor in 3 patient) and 16.7 (range 10–18) (Excellent in 25, very good in 18, good in 6, fair in 5, poor in 3 patient), respectively. There was a significant relation between the reduction quality and clinical outcome (p < 0.001), while there was no significant relation between the clinical outcome and the fracture type (p > 0.05). Iatrogenic external iliac vein damage was noted in 2 patients. Obturator nerve palsy was noted in 3 patients, who recovered spontaneously at mean time of 3.7 months (range 3–5). Rectus abdominus paralysis was noted in 2 of the 19 (10.5%) Pfannenstiel-incision patients but not in the vertical-incision patients.
Conclusion
Our experience in 57 patients shows that satisfactory results can be obtained, even in bilateral fractures with vertical midline incision.
Level of evidence
Level IV Therapeutic Study
Keywords: Acetabulum, Stoppa, Modified, Pelvic, Fracture, Result
Introduction
The basic aim of the various surgical approaches used in fractures of the acetabulum is to be able to provide anatomic reduction with minimum complications,1, 2 since morbidity is high in cases of inappropriate reduction.3 The poor clinical outcome of non-anatomic reduction will eventually require total hip arthroplasty.1 Different surgical approaches can be used for acetabular fractures, including the Kocher-Langenbeck, iliofemoral, ilioinguinal, combined anterior/posterior, extended iliofemoral, transtrochanteric, modified Stoppa, and triradiate approaches.4, 5, 6, 7, 8, 9, 10, 11 These approaches can be classified as anterior, posterior, extensile, or combined approaches. In choosing the approach to be made, the fracture configuration, the experience of the surgeon and the soft tissue conditions such as Morel-Lavallee lesions are important considerations.12 Of these approaches, the modified Stoppa technique, which Cole and Bolhofner presented in 1994, has begun to be used more widely in recent years.13
The modified Stoppa approach has many advantages: it provides a sufficient area of visualisation for pelvic ring exposure, does not involve iliac artery vein or femoral nerve exposure, provides sufficient reduction in anterior wall and column fractures, and can be used when an anterior fracture exists together with a posterior hemitransverse fracture, in addition to fractures of both columns.14 Moreover, the application of a plate to the quadrilateral surface is feasible in the Stoppa approach, and this facilitates anatomic reduction.15, 16 In addition to anatomic reduction, decreased intraoperative blood loss and shorter operating times have been reported with the modified Stoppa approach.15, 16, 17
The aim of this study is to demonstrate the effectiveness of the modified Stoppa approach in treating fractures of the acetabulum by evaluating the postoperative radiological and clinical results of patients who had a minimum 24-month follow-up, and then to compare the results to those from other studies in the literature that have used the modified Stoppa technique.
Patients and methods
Approval for this study was granted by the local ethics committee. A retrospective evaluation was conducted of patients who had undergone the modified Stoppa technique for an acetabular fracture at a medical faculty hospital between February 2013 and June 2016, with a minimum 24-month follow-up period. Demographic data, mechanism of trauma, associated injuries, Injury Severity Score (ISS), time to surgery, surgery time, intraoperative bleeding, and intraoperative or perioperative complications were obtained from the patients' medical records. The indications for surgery were an unstable fracture in the weight-bearing region, a displacement of ≥2 mm in the non-weight-bearing region, a dislocation together with fracture, and young and active patients.15 The exclusion criteria were as follows: patients who were lost in follow-up or with incomplete follow-up and medical records (n = 8), patients with associated acetabular posterior wall fractures and/or those who had undergone the Kocher-Langenbeck approach in addition to a modified Stoppa approach (n = 7), patients with associated posterior pelvic ring injuries (n = 13), patients who had suffered head trauma that caused prolonged immobilisation (n = 3), patients with open fracture (n = 4) and patients with a history of ipsilateral hip injury that may interfere with the results (n = 1).
The approach for patients with detected acetabular fractures admitted to the emergency department starts with a complete clinical and neurological examination. Pelvic anteroposterior (AP) radiographs, pelvic computed tomography (CT), and three-dimensional (3D) CT reconstructions were the standard radiological protocol for these patients in order to classify the fractures according to the Judet and Letournel classification system, determine associated pelvic ring injuries, and describe specific fracture characteristics (such as impaction of the acetabular roof or femoral head) that may have had an effect on surgical planning.9 Anticoagulation prophylaxis with low-molecular heparin was used preoperatively if no contraindication was present due to concomitant injuries. Limb traction was applied until surgery to avoid pressure necrosis on the femoral head cartilage, to reduce instability, and to facilitate intraoperative reduction. Skin traction was applied to patients with simpler fractures and to those who expected to have earlier surgery in the absence of additional major injuries.
Surgical technique
Transverse incision (Pfannenstiel incision) was used in the first 19 patients. After that, we preferred vertical midline incision from approximately 2 cm below the umbilicus to 1 cm above the symphysis pubis joint to a transverse incision in all remaining patients (n = 38); see Fig. 1. After dissection to the anterior rectus fascia, it was deepened in the midline by splitting the rectus abdominus muscle along the linea alba. The potential space of Retzius was then reached by detaching the tissues surrounding the bladder using blunt-finger dissection and by mobilising the bladder away with a malleable retractor to improve visualisation. The exposure continued laterally by releasing the periosteum and iliopectineal fascia along the superior ramus and pubic root extending to the pelvic brim and the internal iliac fossa. During this exposure, the anastomotic branches between the internal and external iliac vessels (called the corona mortis) were explored and then tied or cauterised to avoid bleeding (Fig. 2). The external iliac vessels were then located with the aid of palpation, then elevated and protected with the iliopsoas muscle by a blunt retractor without the application of excessive force. The exposure could then be continued posteriorly along the pelvic brim to the sacroiliac joint. The obturator neurovascular bundle may also be located in the fat on the medial surface of the obturator internus muscle, which can then be dissected and mobilised with a retractor and another blunt-end retractor in the greater sciatic notch if necessary to achieve a better working area, especially for quadrilateral surface and posterior column fractures.18 In these cases, a Schanz screw or T-handle in the proximal femur can be useful for fracture reduction by lateral distraction and indirect manipulation; alternatively, a supplemental lateral window (a lateral window using the ilioinguinal approach) can be combined with a modified Stoppa approach for fractures with high anterior column involvement.
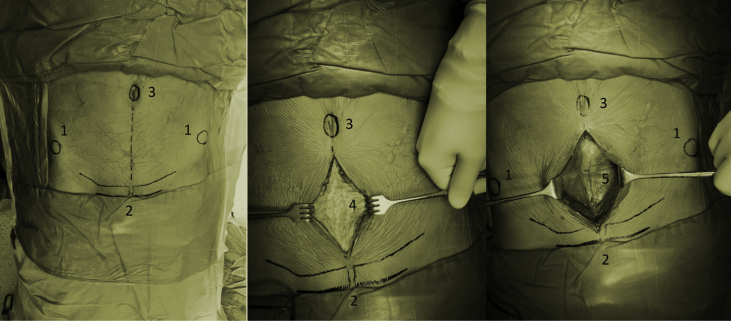
Fig. 1.
Vertical incision on a patient:(1) anterior superior iliac spine; (2) symphysis pubis; (3) umbilicus; (4) anterior rectus fascia; (5) bladder.
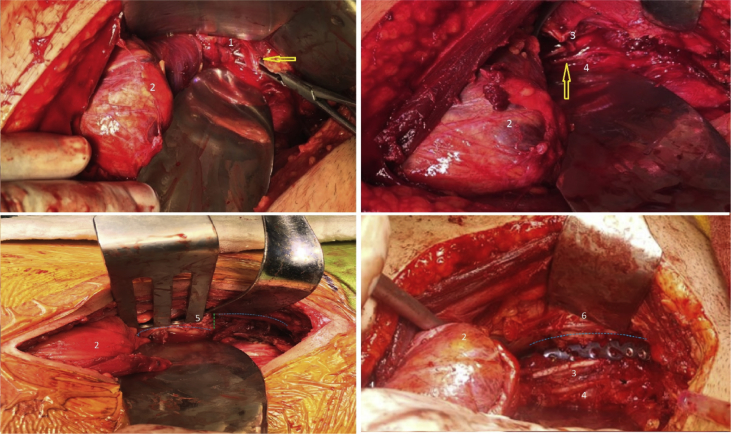
Fig. 2.
(1) corona mortis; (2) bladder; (3) obturator nerve; (4) obturator artery; (5) displaced quadrilateral plate; (6) quadrilateral surface fixation with a reconstruction plate.
Lateral window is made with a second incision starting 1–2 cm lateral to the anterior superior iliac spine along the iliac crest posteriorly, followed by submuscular dissection along the internal iliac wing to access the iliac crest and the upper iliac fossa. Using this supplemental window, it is possible to reduce and fixate the high anterior column fracture as well as to place the reduction clamps or Schanz screws to apply the reduction manoeuvre (e.g. internal hemipelvis reduction). For the fracture fixation, reconstruction plates and 3.5-mm-diameter cortical screws were used in a ‘J’ or ‘C’ shape from the pubic arm towards the iliac wing (Fig. 2, Fig. 3). Additional fixation with reconstruction plates positioned related to the fracture configuration may be required for quadrilateral surface fractures, posterior column fractures, and high anterior column fractures with iliac wing exit. The number and shape of the plates used were adjusted according to fracture configuration. Lag screws can also be used with reconstruction plates, especially for posterior column fixation. Special instruments such as ball spike pushers, pelvic reduction clamps, and collinear reduction clamps are important auxiliary tools in this type of surgery.
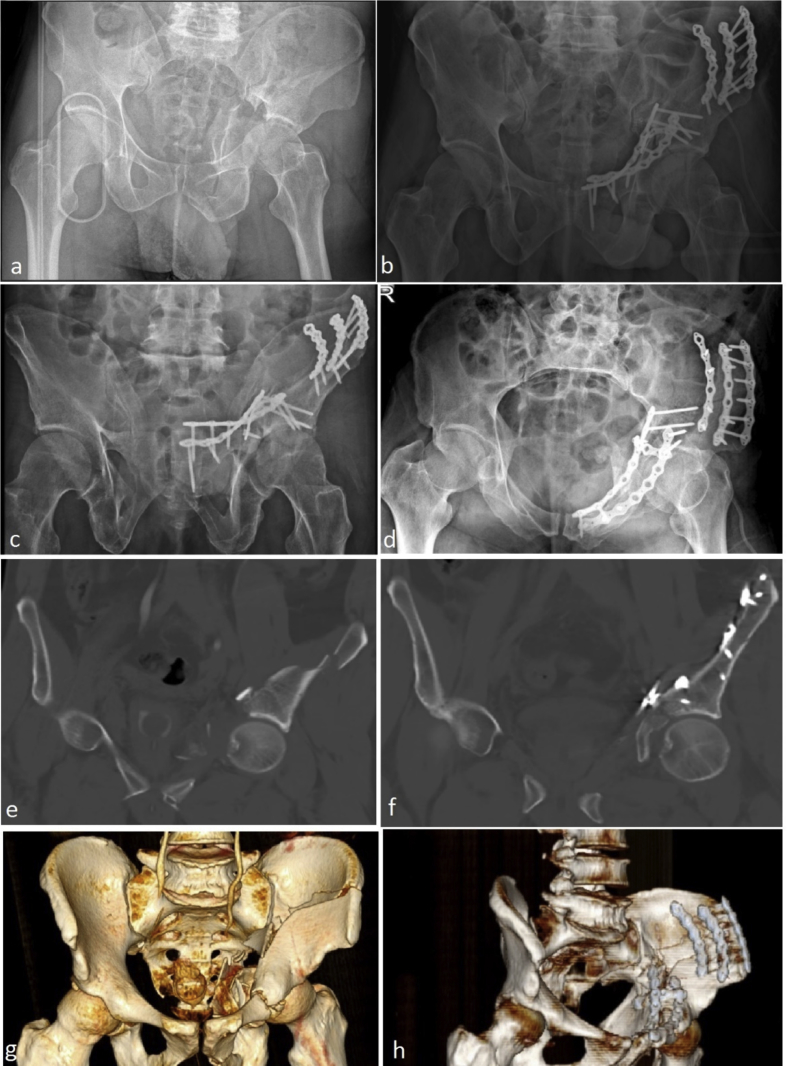
Fig. 3.
A 42-year-old male patient who sustained a both-column fracture treated with a modified Stoppa approach: (a) preoperative pelvic AP radiograph; (b) postoperative pelvic AP radiograph; (c) postoperative pelvic outlet radiograph; (d) postoperative pelvic inlet radiograph; (e) preoperative coronal CT; (f) postoperative coronal CT; (g) preoperative pelvic 3-D CT; (h) postoperative pelvic 3-D CT.
Postoperative care
Postoperatively, an intravenous antibiotic prophylaxis of 3 × 1 gr/day cefuroxime was administered routinely until the 3rd postoperative day, unless another indication for its continuation. As antithrombotic prophylaxis, 2 × 0.4 cc/day enoxaparin sodium was administered starting from 6 h postoperatively to the 4th week postoperatively. Antithrombotic compression stockings were applied in addition to pharmacologic deep venous thrombosis (DVT) prophylaxis. Heterotrophic ossification prophylaxis was not routinely administered. Drains were removed on the 2nd day postoperatively if the drainage did not exceed 50 mL/day.
After drain removal, in-bed passive hip movement exercises were begun. Patients were then encouraged to engage in touch-down weight-bearing mobilisation as early as possible for the operative side by taking into account each patient's general condition and concomitant injuries. Until the 8th week postoperatively, touch-down weight bearing was permitted and continued with partial weight bearing with two crutches and then one crutch until full weight bearing was achieved at the 12–16th week by considering each patient's radiological findings. Those patients who had bilateral acetabular fractures engaged in in-bed and bedside exercises, starting with passive hip movement exercises and then continuing with hip strengthening exercises with no weight-bearing until week 6–8 postoperatively. Mobilisation was then continued with partial weight-bearing after considering each patient's radiological findings.
Radiological and clinical evaluation
The initial plain radiographs routinely obtained postoperatively were AP, iliac oblique and obturator oblique pelvis radiographs. CT scans of the pelvis were also obtained from the patients before their discharge (Fig. 3). Radiologic views were examined to assess fracture reduction, and were graded according to the criteria described by Matta19 as anatomic (0–1 mm displacement), imperfect (2–3 mm displacement), or poor (>3 mm displacement). All patients were followed in the outpatient clinic at weeks 2 and 6, months 3 and 6, and years 1 and 2, and follow-up pelvis AP, iliac oblique and obturator oblique radiographs were obtained for radiologic evaluation. All radiological measurements were evaluated by both a radiologist experienced in extremities and a study author rather than by the operating surgeon. Functional evaluation of the patients was conducted by a physiotherapist using the postoperative application of the Harris Hip Score (HHS),20, 21 as well as by using the clinical grading system according to Merle d’Aubigné and Postel, modified by Letournel and Judet and then subsequently by Matta.19 Radiographic and clinical results were thereby classified as excellent, good, fair, or poor.
Clinical outcomes were divided into two groups: excellent to good and fair to poor. Radiological outcomes were graded as excellent, good, fair, and poor. Statistical analysis of the data was performed using SPSS version 20.0 statistical software (SPSS Inc., Chicago, Illinois, USA). The level of significance was set at a p-value < 0.05. The relationship between clinical outcomes and radiological outcomes was statistically analysed using Fisher's exact testing. Chi-squared testing was used for categorical variables, and Fisher's exact testing was used when the expected cell counts were lower than 5.
Results
After implementation of the exclusion criteria, 36 patients were excluded and the study included a total of 57 patients (36 males and 21 females), with a mean age of 37.8 years (range 15–84 years). Of these 57 patients, 6 had bilateral acetabular fractures. According to the Judet and Letournel classification system, the 63 acetabulum fractures of the 57 patients were categorised as transverse (10 patients), both columns (27 patients), anterior column and posterior hemitransverse (7 patients), T-type (12 patients), anterior column (five patients) and anterior wall (two patients); see Table 1.9 Classification of all the fractures according to the Judet and Letournel system was done by the operating surgeon and was also confirmed preoperatively by a radiologist experienced in extremity imaging.
Table 1.
Patient demographics, mechanism of injury, and types of fractures according to the Judet and Letournel classification system9; the study includes 63 acetabulum fractures in 57 patients.
| Demographics | Male | 36 |
| Female | 21 | |
| Age | 37.8 (15–84) | |
| ISS score | 18.3 (9–41) | |
| Trauma types | Motor vehicle crushing | 18 |
| Motor vehicle accident | 25 | |
| Fall from height | 10 | |
| Tractor accident (crushing) | 4 | |
| Acetabulum fracture types | Anterior column | 5 |
| Transverse | 10 | |
| Both columns | 27 | |
| Anterior column and posterior hemitransverse | 7 | |
| T-type | 12 | |
| Anterior wall | 2 |
All patients suffered high-energy trauma, with a mean ISS of 18.3 (range 9–41); see Table 1. A total of 13 patients were transferred from the emergency department to the intensive care unit (ICU) for close monitoring due to head trauma (n = 2), thoracic injury (n = 4), intra-abdominal pathology (n = 6), and associated multiple fractures (n = 1). After the clinical stabilisation of these patients (mean 5.3 days, range 2–10 days), they were transferred to the orthopaedics clinic. The timing of the operation was planned after ensuring that the patients were clinically stable. The mean time from trauma to surgery was 5.5 days (range 0–11 days). The mean time to operation for those patients with concomitant injuries was 6.9 days (range 6–11 days); in the remaining patients, the mean time was 4.7 days (range 0–7 days). All operations were performed by a single surgeon. The mean surgery time was determined to be 152 min (range 95–250). The mean intraoperative blood loss was determined to be 660.4 ml (range 150–1600 ml). Mean intraoperative blood loss was determined to be 733.3 ml (range 400–1200 ml) in the bilateral cases and 651.8 ml (range 150–1600 ml) in the unilateral cases. According to previous literature by Bose et al, each saturated small swab was accepted as containing 60 mL of blood, and the amount of blood aspirated intraoperatively was calculated by subtracting the amount of saline used intraoperatively from the accumulated material in the suction bottle. The amount of intraoperative bleeding was calculated from these two values and recorded routinely by anesthesia team.22
The patients were followed up for a mean of 28.1 months (range 24–35 months). Radiological outcomes after fracture fixation were anatomic, imperfect, and poor in 52 (82.5%), 9 (14.2%), and 2 (3.2%) of the acetabulum fractures, respectively (Table 2). The mean preoperative displacement in the sagittal, coronal, and axial planes was 4.1 mm, 4.4 mm, and 3.9 mm, respectively. The mean postoperative displacement values were 0.4 mm, 0.4 mm, and 0.2 mm, respectively (Table 2). The intra-class correlation coefficient was above 0.90 for all items measured and suggest that there is a perfect agreement among the raters. The relationship between reduction quality and clinical outcomes was statistically significant (p < 0.001), although no statistically significant difference was found between clinical outcomes and fracture type when evaluated according to fracture types (p > 0.05). Six of the 57 patients had bilateral acetabulum fractures, and 5 had excellent radiological outcomes for both right- and left-sided fractures, whereas excellent and good outcomes for right- and left-sided fractures were found in the remaining patient.
Table 2.
Amount of intraoperative bleeding, quality of reduction, and clinical outcomes.
| Amount of bleeding | Mean bleeding | 660.4 (150–1600) | |
| Bilateral acetabulum fractures | 773.3 (400–1200) | ||
| Unilateral acetabulum fractures | 651.8 (150–1600) | ||
| Mean displacement values (mm) | Radiologic plane | Preoperative | Postoperative |
| Sagittal | 4.1 | 0.4 | |
| Coronal | 4.4 | 0.4 | |
| Axial | 3.9 | 0.2 | |
| Quality of reduction | ≤1 mm | 53 | 84.1% |
| >1 to < 3 mm | 8 | 12.7% | |
| ≥3 mm | 2 | 3.2% | |
| Harris Hip Score (mean 86.6) | Excellent (≥90 points) | 27 | 47.4% |
| Good (80–89) | 23 | 40.3% | |
| Fair (70–79) | 4 | 7% | |
| Poor (≤70) | 3 | 5.3% | |
| Modified clinical grading system (mean 16.7) | Excellent (18 points) | 25 | 43.9% |
| Very good (17 points) | 18 | 31.6% | |
| Good (15–16) | 6 | 10.1% | |
| Fair (13–14) | 5 | 9.2% | |
| Poor (13) | 3 | 5.2% | |
At 2 years after the surgery using the modified Stoppa approach, functional hip evaluations using the HHS had a mean of 86.6 and a range of 66–96 (excellent in 27 patients, good in 23 patients, fair in 4 patients, and poor in 3 patients); with Matta's modified clinical grading system, the mean was 16.7, with a range of 10–18 (excellent in 25 patients, very good in 18 patients, good in 6 patients, fair in 5 patients, and poor in 3 patients); see Table 2. Excellent, very good, and good outcomes all occurred with anatomic reduction (p < 0.001). Five of the six patients with bilateral fractures had excellent clinical results, and the remaining patient had very good results. Three patients resulted with poor clinical outcomes and all of them were over the age of 65 years. These patients had T-type, anterior colon-hemitransverse, and both-column fractures, and they had poor, imperfect, and poor postoperative reduction quality, respectively. Two of these patients with T-type and anterior colon-hemitransverse fractures also had deep infection postoperatively, which was treated with surgical irrigation and prolonged antibiotic treatment. As a result of these, they experienced a loss of reduction due to fixation failure. The remaining patient with poor result was with both column fracture and postoperative poor reduction quality had also fixation failure postoperatively These patients underwent total hip arthroplasty in the 11th, 17th and 8th month postoperatively, respectively. Moreover, we had five patients with fair clinical outcome. Two of them were also over 65 years of age and with transverse column and anterior column fracture, had fair clinical outcomes due to fixation loss after anatomic reduction. The remaining three patients with fair clinical outcomes had both columns fracture in two and T-type fracture in one patient. They had imperfect radiological outcome postoperatively and consequently resulted with fair clinical outcome (Table 3).
Table 3.
Fracture type, age, postoperative quality of reduction and reason for clinical outcome of the patients with poor and fair clinical outcome.
| Clinical Outcome | Age (year's) | Fracture type | Quality of reduction | Reason for Clinical outcome |
|---|---|---|---|---|
| Poor | 66 | T-type | Poor | Deep infection |
| 69 | Anterior column-posterior hemitransverse | Imperfect | Deep infection | |
| 66 | Both-column | Poor | Both poor reduction quality and fixation failure | |
| Fair | 67 | Transverse column | Anatomic | Fixation loss |
| 72 | Anterior column | Anatomic | Fixation loss | |
| 51 | Both-column | Imperfect | Imperfect reduction quality | |
| 39 | T-type | Imperfect | Imperfect reduction quality | |
| 46 | Both-column | Imperfect | Imperfect reduction quality |
Intraoperatively, external iliac vein iatrogenic damage was noted in 2 patients and was repaired by the cardiovascular surgeon (Table 4); 1 of these 2 patients had previous laparotomy history. The corona mortis could not be located in 13 (22.8%) patients.23 In 17 (29.8%) patients, a supplemental lateral window was used to access the upper ilium and crest and was made with a second incision starting 1–2 cm lateral to the anterior superior iliac spine along the iliac crest posteriorly.
Table 4.
Postoperative complications.
| Complication | Patient (n) |
|---|---|
| External iliac vein injury | 2 |
| Deep vein thrombosis | 4 |
| Deep infection | 2 |
| Fixation failure | 1 |
| Neuropraxia of the obturator nerve | 3 |
| Hardware in acetabular joint space | 1 |
Postoperatively, a patient was reoperated on the second postoperative day due to articular penetration of a screw detected with pelvic CT. Obturator nerve palsy was observed in three patients. Two of these patients recovered spontaneously at three months, and the remaining patient recovered at five months; no sciatic or lateral cutaneous nerve injury was encountered in any cases. No postoperative ileus was encountered following surgery, perhaps due to the extraperitoneal approach that was used. Rectus abdominus paralysis was noted in 2 of the first 19 patients (10.5%) who had undergone Pfannenstiel incision, whereas rectus abdominus paralysis was not observed in any of the remaining 38 patients who had undergone vertical incision. No incisional hernias or groin hernias were encountered during the postoperative period. Heterotrophic ossification was not encountered in any of the patients. Deep vein thrombosis developed in 4 patients postoperatively. Deep infection was found in 2 diabetic patients aged 66 and 69 years, which was successfully treated with irrigation and prolonged antibiotic therapy (Table 4). But, unfortunately resulted with poor outcome due to fixation failure.
Discussion
Cole and Bolhofner first described the modified Stoppa approach by splitting the rectus abdominis muscle along the linea alba as an alternative approach for the fixation of acetabular and pelvic girdle fractures.13 The most important difference in the Stoppa technique is that dissection is directed to the inner pelvic girdle and the quadrilateral surface. Infrapectineal applications to the area using the modified Stoppa technique in quadrilateral surface fractures were soon reported in the literature.23, 24 In comparison with the extra-pelvic ilioinguinal approach, the major advantages of the modified Stoppa technique include the easier approach due to the lack of dissection of the inguinal canal and the better view that is afforded of all anterior elements, especially for the quadrilateral plate (QLP), which enables fixation and buttress plating of the QLP; this step cannot be performed when using an ilioinguinal approach.14 Moreover, with the help of direct visualization and approach of posterior column, reduction and fixation with a support plate can be applied.17
In cases with acetabulum fractures where the modified Stoppa approach has been applied, 69–93% of excellent or good clinical results have been reported at the end of at least a one-year follow-up (Table 5). In a study of 57 cases by Sagi et al,18 excellent or good acetabulum fracture reduction was achieved in 92% of cases; the clinical outcomes were reported as being good/excellent, with a Merle d’Aubigné score of 91%. Isaacson et al25 obtained anatomic or satisfactory reduction in 92% of 36 cases and good/excellent clinical results, with a Merle d’Aubigné score of 82%. In another series of 36 cases, Elmadağ et al26 reported anatomic reduction in 80% of cases and good/excellent clinical results (according to Merle d’Aubigné score) in 90% of cases. Ma et al15 reported anatomic or satisfactory reduction in 86% of 30 patients and good/excellent clinical outcomes using the HHS. Hirvensolo et al24 obtained excellent or good acetabulum fracture reduction in 84% of a series of 164 cases and good/excellent HHS results in 75% of cases. In 24 cases reported by Liu et al,16 excellent or good acetabulum fracture reduction was obtained in 92% of cases, and good/excellent clinical HHS results in 93%.
Table 5.
Comparison of excellent/good clinical outcomes with reduction quality.
| Authors | Date | Patient number (n) | Anatomic reduction (%) | Excellent/good clinical outcome (%) |
|---|---|---|---|---|
| Hirvensolo et al.20 | 2007 | 164 | 84 | 75 |
| Sagi et al.22 | 2010 | 50 | 92 | 88 |
| Laflamme et al.25 | 2011 | 21 | 90 | 71 |
| Bastian et al.26 | 2013 | 43 | 88 | 69 |
| Ma et al.14 | 2013 | 30 | 86 | 83 |
| Liu et al.15 | 2013 | 24 | 82 | 93 |
| Isaacson et al.23 | 2014 | 36 | 92 | 82 |
| Elmadağ et al.24 | 2016 | 36 | 80 | 90 |
| This study | 2018 | 57 | 81 | 87 |
Similarly, in the current study, anatomic reduction of the acetabular fracture was obtained in 52 (82.45%) of the acetabulum fractures. The clinical results were good/very good/excellent in 49 (85.9%) cases using the modified clinical grading score and good/excellent in 50 (87.7%) cases using HHS. The clinical results were also parallel to the success of anatomical reduction (p < 0.001). Contrary to the previous literature, Laflamme et al27 and Bastian et al28 reported poor clinical outcomes, although the rates of anatomic reduction were high. Because the age of most of the patients in these two studies was >65 years, these results may be interpreted such that the clinical outcome in the osteoporotic patient group may be poor, even if anatomic reduction can be obtained.27, 28 In our study, 7 of the patients were above 65 years of age, and 3 of these had poor clinical outcomes according to the modified clinical grading score. These patients had T-type, anterior colon-hemitransverse, and both-column fractures, and they had poor, imperfect, and poor postoperative reduction quality, respectively. Two of these patients with T-type and anterior colon-hemitransverse fractures also had diabetes, which could have made them susceptible to infection; these patients had deep infection postoperatively, which was treated with surgical irrigation and prolonged antibiotic treatment. As a result of these, they experienced a loss of reduction due to fixation failure and underwent total hip arthroplasty on the 11th and 17th months postoperatively. The remaining patient with poor result was with both column fracture and postoperative poor reduction quality had also fixation failure postoperatively. But this patients was with hepatic cirrhosis and was seen intraoperatively to have low bone quality. He had undergone total hip arthroplasty on 8th month postoperatively. But we still have all our poor clinical outcomes in patients over 65 years of age. But in these patients there was no poor result despite anatomic reduction contrary to Laflamme et al.‘s and Bastian et al.‘s studies.27, 28 However, another two patients aged 67 and 72 years were with transverse column and anterior column fracture respectively, had fair clinical outcomes due to fixation loss after anatomic reduction. Low bone quality with osteopenia can be blamed for this. Potential inability of elderly patients for controlled partial weight bearing can also be blamed for failure of osteosynthesis.28 These patients may also be candidates for hip arthroplasty in the near future. The remaining three patients with fair clinical outcomes were under 65 years of age; two of them had both columns fracture and one of them had T-type fracture. They had imperfect radiological outcome postoperatively and consequently resulted with fair clinical outcome (Table 3).
In this study, a statistically significant difference was found between reduction quality and clinical outcomes (p < 0,001), although no statistically significant difference was found between clinical outcomes and fracture type when evaluated according to fracture types (p > 0.05). In addition, no statistically significant difference was found in the current study between males and females in terms of clinical outcomes, which agrees with the literature.18, 19, 20, 21, 23, 24, 25, 26, 27, 28 Three patients (5.3%), with a mean age of 69 years, had poor results and underwent total hip arthroplasty. The conversion to total hip replacement after acetabulum fracture operation using a modified Stoppa approach has been reported in the range of 0–14%.13, 18, 24, 27, 29 We must keep in mind, however, that 2–3 years of follow-up are required for posttraumatic coxarthrosis development, and the duration of follow-ups varies in the literature.30 The patients were followed up for a mean of 28.1 months (range 24–35 months) in our study, and the number of patients who had total hip arthroplasty may increase in the near future.
Cole and Bolhofner, who first described acetabular fracture fixation by using the Stoppa approach in their series with 55 fractures, used the posterior approach in 18 (33%) patients and the lateral window of the ilioinguinal approach in 5 (9%) patients in combination with the Stoppa approach, whereas they used only the Stoppa approach in 32 (58%) patients.13 Other authors have also reported on the need to extend the modified Stoppa approach by combination with the lateral window of the ilioinguinal approach, the modified Smith-Petersen approach, or conversion to the ilioinguinal approach.18, 27, 28, 29, 30 The majority of studies have reported a combination with the lateral window of the ilioinguinal approach in a range of 28%28 to 93%,30 whereas some authors have reported the use of this supplemental lateral window to be their routine practice.18, 30 In our study, we used a supplemental lateral window in 17 (29.8%) of the patients, which is lower than the literature has reported. According to our experience, vertical midline incision provides better access to the pelvic ring than transverse Pfannenstiel incision does. We recognised this situation in the 20th patient who was the first case used vertical midline incision. We then started to use vertical incision for all the remaining patients. Ponsen et al and Hirvensalo et al also reported on the advantage of vertical midline skin incision, which provides better access to the pelvic ring due to the easier retraction of the peritoneal sac and abdominal musculature without the need for detachment of the rectus abdominus muscle.23, 24 Liu et al, however, reported that the exposure of the acetabulum was restricted due to obstruction of the rectus abdominus muscle and the subcutaneous fatty layer through the vertical midline incision, especially in obese patients.16 They modified the technique by performing the approach between the rectus muscle and the iliopsoas after a horizontal incision, which maintains the advantages of the Stoppa approach and allows even closer access to the acetabulum.16 Until now, we have not used the newly modified Stoppa technique described by Liu et al. But similarly to Ponsen et al and Hirvensalo et al, we experienced better access to the pelvic ring with vertical midline incision than with a transverse incision.23, 24 A relatively lower ratio (29.8%) of supplemental lateral window use may be the result of this better access with a midline incision. Furthermore, bilateral anterior dissections can be performed for both-sided fracture sides by a single midline vertical incision. Ponsen et al reported a case in their series with bilateral transverse acetabular fracture and unilateral sacroiliac disruption, approached through a single vertical incision.23 In our series, we had 6 bilateral cases with bilateral acetabulum fractures, and all were approached through a single vertical incision. Five of the 6 patients showed bilateral anatomic radiological results (the remaining patient had an anatomic right side and a left side that showed imperfect results), which suggests that the modified Stoppa approach through midline vertical incision could be a reasonable solution. Rectus abdominus paralysis was seen in 2 of the first 19 patients (10.5%) who had undergone a Pfannenstiel incision, whereas such paralysis was not observed in any of the following 38 patients with a vertical incision. Based on this result, we believe that two factors are involved. First, with a transverse Pfannenstiel incision using the modified Stoppa approach, the length of the cephalad-caudad split in the rectus abdominus through the linea alba is the limiting factor in the extent of exposure25; therefore, excessive traction to overcome this limitation can be a cause for rectus abdominus paralysis. Second, the need to detach any part of the rectus abdominus muscle becomes unnecessary with a vertical midline incision, which differs from Pfannenstiel incision.15, 18, 23, 24 Contrary to the advantages of vertical midline incision, the difficulty in converting to the classic ilioinguinal approach may cause discouragement at the beginning of the learning curve.
Deep infection was reported by Sagi et al18 in 1 patient (1.8%), in 1 patient (5.9%) by Anderson et al,29 in 1 patient (1.8%) by Cole et al,13 in 1 patient (3.3%) by Ma et al,14 and in 5 patients (3%) by Hirvensolo et al.24 Similarly, deep infection was observed in 2 (3.5%) patients in the current study and was treated with irrigation and prolonged antibiotic therapy. These patients had poor clinical outcomes due to fixation failure, so deep infection appears to be a poor prognostic factor, as expected.
Until now, no incidences of heterotopic ossification have been reported in the literature following the treatment of acetabular fractures through the modified Stoppa approach. Heterotropic ossification was not encountered in the current study. Furthermore, we had 3 patients with obturator nerve palsy; these patients spontaneously recovered at a mean of 3.7 months (range 3–5 months) and thus did not affect the clinical outcome. Similar results have been reported in the literature. In Sagi et al.'s18 study of acetabulum fractures, extreme weakening in the hip adductors with a paralysed obturator nerve was reported in 13 patients (26%) postoperatively; with the exception of 1 case, all recovered within 6 months. Obturator nerve damage was reported in 2 (6.7%) patients in Ma et al.'s study15 and in 1 (4.8%) patient by Laflamme et al.27
There have been limited publications in the current literature about the techniques used in the management of acetabular fractures with quadrilateral plate involvement and fixation stability.31, 32 Suprapectineal plating versus subpectineal plating constitutes the main point of the discussion. Technical modifications in fixation such as addition of periarticular lag screws over a suprapectineal plate, vertical or horizontal infrapectineal plate use are the other points of the interest. May et al reported a biomechanical study to compare the performances of four different fixation constructs (Group 1:A suprapectineal reconstruction plate only bridging the QLP; Group 2: Same instrumentation as in Group 1 but with additional periarticular screws along the QLP; Group 3: Same instrumentation as in Group 1 but with an additional 6-hole buttress plate below the pelvic brim; Group 4: Combination of the instrumentation used in Groups 2 and 3) in acetabular fractures involving anterior column with quadrilateral plate (QLP) distruption.31 During simulation of inadvertent supraphysiologic load, the median load to failure was higher in Group 2 and Group 4 compared with Group 1 and Group 3. They concluded that, only additional periarticular screws along the QLP increased the fixation strength and periarticular long screws were superior to infrapectineal buttress plates in preventing medial redisplacement of the QLP.31 However, unlike our study, it was seen that the infrapectineal plate did not cross along the all fracture line in quadrilateral surface (not applied from sciatic buttress to the inner side of the upper pubic arm) and may be the technical weakness of the study. Tanoğlu et al reported another biomechanical study that compare three different fixation techniques (Group 1: posterior column lag screws over a suprapectineal plate; Group 2: Posterior column lag screws over a suprapectineal plate and an infrapectineal plate; Group 3: A suprapectineal plate and a vertical infrapectineal plate) for anterior column posterior hemitransverse acetabular fractures.32 In the dynamic and static tests, Group 3 showed the less stable fixation compared to Group 2. In the static tests, there was no statistically significant difference between Group 1 and 2, although less displacements were obtained in Group 2. So, they concluded better stability with less fracture displacement with the combination of posterior lag screws over a suprapectineal plate and an infrapectineal plate supporting the pelvic brim along both sides of the linea terminalis than a suprapectineal plate accompanying with a vertical infrapectineal plate.32 Similar to our study, the infrapectineal plate along the inferior side of the pelvic brim was applied from sciatic buttress to the inner side of the upper pubic arm in this study. Even though with no statistically significant stiffness values difference between posterior column lag screws over a suprapectineal plate and addition of an infrapectineal plate fixation to this construct, less displacements can be obtained with this addition. According to our experience, additional infrapectieal plate fixation facilitates reduction in acetabulum fractures with disrupted QLP with its butress effect. In the study of May et al, if the biomechanical set up had done with a infrapectineal plate applied from sciatic butress to the inner side of the upper pubic arm, we believe the results would be different.31
The major limitations of the current study include the small sample size and the fact that it is a retrospective analysis. Due to its retrospective nature, the study is prone to various forms of bias, such as selection bias and recall bias. Absence of patient related health quality of life measurement is also a limitation of the study. The current study's inclusion of 57 cases with no control group is another limitation for understanding the advantages and disadvantages of this technique. Comparison of the 19 patients with Pfannenstiel incision to the 38 patients with vertical midline incision could be considered. But it was thought that this comparison would not be healthy when the randomization was not done and the learning curve was taken into consideration.
Conclusion
Our experience with the modified Stoppa approach in 57 patients shows that satisfactory results can be obtained with this exposure, even with bilateral fractures with vertical midline incision, although the literature disagrees if the modified Stoppa approach should be used with a vertical incision or a Pfannenstiel incision. To determine the effectiveness of the modified Stoppa approach, long-term, prospective, randomised, controlled studies are warranted to compare the effectiveness of this approach with vertical or Pfannenstiel incision, as well as with other standard approaches.
Disclaimers
None.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Cem Yalin Kilinc, Email: cykilinc@gmail.com.
Ahmet Emrah Acan, Email: dremrahacan@hotmail.com.
Emre Gultac, Email: emregultac@yahoo.com.
Rabia Mihriban Kilinc, Email: rguner@hotmail.com.
Onur Hapa, Email: onurhapa@gmail.com.
Nevres Hurriyet Aydogan, Email: nhaydogan@gmail.com.
References
- 1.Briffa N., Pearce R., Hill A.M., Bircher M. Outcomes of acetabular fracture fixation with ten years' follow-up. J Bone Joint Surg Br. 2011;93(2):229–236. doi: 10.1302/0301-620X.93B2.24056. [DOI] [PubMed] [Google Scholar]
- 2.Tannast M., Najibi S., Matta J.M. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Br. 2012;94(17):1559–1567. doi: 10.2106/JBJS.K.00444. [DOI] [PubMed] [Google Scholar]
- 3.Arazi M., Kutlu A., Eristi Y., Ögün T.C., Kapıcıoglu M.I.S. Open reduction and internal fixation of the displaced fractures of the acetabulum with single-nonextensile approaches. J Bone Joint Surg Br. 2001;83(suppl 2):118. Issn Print: 0301-620X. [Google Scholar]
- 4.Bray T.J., Esser M., Fulkerson L. Osteotomy of the trochanter in open reduction and internal fixation of acetabular fractures. J Bone Joint Surg. 1987;69(5):711–717. PMID:3597472. [PubMed] [Google Scholar]
- 5.Goulet J.A., Bray T.J. Complex acetabular fractures. Clin Orthop Relat Res. 1989;240:9–20. PMID: 2492912. [PubMed] [Google Scholar]
- 6.Helfet D.L., Schmeling G.J. Management of complex acetabular fractures through single nonextensile exposures. Clin Orthop Relat Res. 1994;305:58–68. PMID: 8050248. [PubMed] [Google Scholar]
- 7.Kebaish A.S., Roy A., Rennie W. Displaced acetabular fractures: long-term follow-up. J Trauma. 1991;31(11):1539–1542. [PubMed] [Google Scholar]
- 8.Kloen P., Siebenrock K.A., Ganz R. Modification of the ilioinguinal approach. J Orthop Trauma. 2002;16(8):586–593. doi: 10.1097/00005131-200209000-00008. PMID: 12352568. [DOI] [PubMed] [Google Scholar]
- 9.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;151:81–106. PMID: 7418327. [PubMed] [Google Scholar]
- 10.Matta J.M. Operative treatment of acetabular fractures through the ilioinguinal approach: a 10-year perspective. J Orthop Trauma. 2006;20(suppl 1):20–29. [PubMed] [Google Scholar]
- 11.Routt M.L., Swiontkowski M.F. Operative treatment of complex acetabular fractures: combined anterior and posterior exposures during the same procedure. J Bone Joint Surg Am. 1990;72(6):897–904. PMID: 2114408. [PubMed] [Google Scholar]
- 12.Sagi H.C., Dziadosz D., Mir H., Virani N., Olson C. Obesity, leukocytosis, embolization, and injury severity increase the risk for deep postoperative wound infection after pelvic and acetabular surgery. J Orthop Trauma. 2013;27(1):6–10. doi: 10.1097/BOT.0b013e31825cf382. [DOI] [PubMed] [Google Scholar]
- 13.Cole J.D., Bolhofner B.R. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach: description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;305:112–123. PMID: 8050220. [PubMed] [Google Scholar]
- 14.Khoury A., Weill Y., Mosheiff R. The Stoppa approach for acetabular fracture. Oper Orthop Traumatol. 2012;24(4–5):439–448. doi: 10.1007/s00064-011-0093-z. [DOI] [PubMed] [Google Scholar]
- 15.Ma K., Luan F., Wang X. Randomized, controlled trial of the modified Stoppa versus ilioinguinal approach for acetabular fractures. Orthopedics. 2013;36(10):1307–1315. doi: 10.3928/01477447-20130920-25. [DOI] [PubMed] [Google Scholar]
- 16.Liu Y., Yang H., Li X., Yang S.H., Lin J.H. Newly modified Stoppa approach for acetabular fractures. Int Orthop. 2013;37(7):1347–1353. doi: 10.1007/s00264-013-1920-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shazar N., Eshed I., Ackshota N., Hershkovich O., Khazanov A., Herman A. Comparison of acetabular fracture reduction quality by the ilioinguinal or the anterior intrapelvic (modified Rives-Stoppa) surgical approaches. J Orthop Trauma. 2014;28(6):313–319. doi: 10.1097/01.bot.0000435627.56658.53. [DOI] [PubMed] [Google Scholar]
- 18.Sagi H.C., Afsari A., Dziadosz D. The anterior intra-pelvic (modified Rives-Stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24(5):263–270. doi: 10.1097/BOT.0b013e3181dd0b84. [DOI] [PubMed] [Google Scholar]
- 19.Matta J.M. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–1645. PMID: 8934477. [PubMed] [Google Scholar]
- 20.Haddad R.J., Cook S.D., Brinker M.R. A comparison of three varieties of noncemented porous-coated hip replacement. J Bone Joint Surg Br. 1990;72(1):2–8. doi: 10.1302/0301-620X.72B1.2298788. PMID: 2298788. [DOI] [PubMed] [Google Scholar]
- 21.Kavanagh B.F., Fitzgerald J.R.H. Clinical and roentgenographic assessment of total hip arthroplasty: a new hip score. Clin Orthop Relat Res. 1985;13:3–40. [PubMed] [Google Scholar]
- 22.Bose P., Regan F., Brown S.P. Improving the accuracy of estimated blood loss at obstetric hemorrhage using clinical reconstructions. Int J Obstetrics Gynaecol. 2006;113(8):919–924. doi: 10.1111/j.1471-0528.2006.01018.x. [DOI] [PubMed] [Google Scholar]
- 23.Ponsen K.J., Joosse P., Schigt A., Goslings C.J., Luitse S.K. Internal fracture fixation using the Stoppa approach in pelvic ring and acetabular fractures: technical aspects and operative results. J Trauma. 2006;61(3):662–667. doi: 10.1097/01.ta.0000219693.95873.24. [DOI] [PubMed] [Google Scholar]
- 24.Hirvensalo E., Lindahl J., Kiljunen V. Modified and new approaches for pelvic and acetabular surgery. Injury. 2007;38(4):431–441. doi: 10.1016/j.injury.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 25.Isaacson M.J., Taylor B.C., French B.G., Poka A. Treatment of acetabulum fractures through the modified Stoppa approach: strategies and outcomes. Clin Orthop Relat Res. 2014;472(11):3345–3352. doi: 10.1007/s11999-014-3460-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elmadag M., Guzel Y., Aksoy Y., Arazi M. Surgical treatment of displaced acetabular fractures using a modified Stoppa approach. Orthopedics. 2016;39(2):340–345. doi: 10.3928/01477447-20160222-07. [DOI] [PubMed] [Google Scholar]
- 27.Laflamme G.Y., Hebert-Davies J., Rouleau D., Benoit B., Leduc S. Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury. 2011;42(10):1130–1134. doi: 10.1016/j.injury.2010.11.060. [DOI] [PubMed] [Google Scholar]
- 28.Bastian J.D., Tannast M., Siebenrock K.A., Keel M.J.B. Mid-term results in relation to age and analysis of predictive factors after fixation of acetabular fractures using the modified Stoppa approach. Injury. 2013;44(12):1793–1798. doi: 10.1016/j.injury.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 29.Andersen R.C., O'Toole R.V., Nascone J.W., Sciadini M.F., Frisch H.M., Turen C.W. Modified Stoppa approach for acetabular fractures with anterior and posterior column displacement: quantification of radiographic reduction and analysis of interobserver variability. J Orthop Trauma. 2010;24(5):271–278. doi: 10.1097/BOT.0b013e3181b2b4ca. [DOI] [PubMed] [Google Scholar]
- 30.Jakob M., Droeser R., Zobrist R., Messmer P., Regazzoni P. A less invasive anterior intrapelvic approach for the treatment of acetabular fractures and pelvic ring injuries. J Trauma. 2006;60(6):1364–1370. doi: 10.1097/01.ta.0000208139.97474.f7. [DOI] [PubMed] [Google Scholar]
- 31.May C., Egloff M., Butscher A. Comparison of fixation techniques for acetabular fractures involving the anterior column with disruption of the quadrilateral plate: a biomechanical study. J Bone Joint Surg Am. 2018;100(12):1047–1054. doi: 10.2106/JBJS.17.00295. [DOI] [PubMed] [Google Scholar]
- 32.Tanoğlu O., Alemdaroğlu K.B., İltar S., Özmeriç A., Demir T., Erbay F.K. Biomechanical comparison of three different fixation techniques for anterior column posterior hemitransverse acetabular fractures using anterior intrapelvic approach. Injury. 2018;49(8):1513–1519. doi: 10.1016/j.injury.2018.06.020. [DOI] [PubMed] [Google Scholar]