Abstract
Objective
The aim of the study was to evaluate the loss of truncal rotation over 54 hours after removing Chêneau brace.
Methods
The studied groups consisted of 39 girls aged 10–18 years old, diagnosed with adolescent idiopathic scoliosis (AIS) and treated with Chêneau brace (CAST) and 20 AIS girls aged 10–18 years old, not treated with bracing. Posterior-anterior radiographs were obtained from the clinical assessment of all subjects and were subsequently used to determine Cobb angles. The measurements of the angle of trunk rotation (ATR) were taken with the Scoliometer® and back-contour device during Adams forward bending test by the two evaluators. The changes in ATRs during 54 hours of observation were performed after the brace had been taken off (0, 2, 24, 30, 48 and 54 hours after debracing). This was described using VATR variable, defined as the change in the absolute Scoliometer® readings in the time intervals against the time interval Δt between the measurements. During back-contour assessment the differential factor (kra) has been used for the digital analysis. The changes in kra over 54 hours of observation were expressed as Vkra factor, defined as the difference in the absolute value of the amplitude differential factor (kra) in the time intervals against the time interval Δt between the measurements.
Results
The highest changes were observed in the thoracic as well as in lumbar spine in patients with Cobb angle ≥30°, axial rotation of the apical vertebrae within 5–15°, Risser sign 0–2. The biggest change in the trunk rotation after Chêneau brace had been taken off was noted within the first two hours of observation.
Conclusion
The patients should be advised to take the brace off for a minimum of two hours before the scheduled x-ray, to allow full relaxation of the trunk in order to obtain reliable radiological images of the deformation.
Level of Evidence
Level III Therapeutic study.
Keywords: Adolescent idiopathic scoliosis, Chêneau brace, Trunk rotation, X-ray, Spinal curvatures
Introduction
Adolescent idiopathic scoliosis (AIS) is defined as a persistent lateral curvature of the spine greater than 10° and/with associated rotation of the vertebrae in the upright or standing position.1
The most reliable and widely used diagnostic tool for the identification of scoliosis and thus the selection of treatment is the method of Cobb.2, 3 Recently, newly designed digital contour-based approaches has been proposed in the measurements of spinal curvature.4
The Society of Scoliosis Orthopedic Rehabilitation and Treatment (SOSORT) guidelines provide clear, scientific indications as to what type of treatment (observation, physical therapy, bracing, surgery) is appropriate for patients with scoliosis.5 For patients with curves of 20–40° (larger than 25°) the most common method used is a brace, especially of Chêneau-type. For curves of 20°–30°, bracing is commenced only when progression of 5° or more occurs between consecutive visits. However, when a patient is skeletally immature (Risser grade 2 or lower) and presents with a 30°–45° curve, bracing is commenced at the first visit.6
The implementation of the orthopaedic braces could be useful for preventing curvature progression in patients with AIS.7 Moreover, braces are still the best solution to avoid surgery.
The Chêneau brace is intended to de-rotate the apical segment of the curve and provide a 3D correction of the spinal deformity.8, 9 The major mechanism of this orthosis is 3D correction of the spinal deformity through a system of multipoint pressure zones and expansion chambers.8
Hopefully in the future there will be more studies not only on the efficacy but also on the biomechanics of bracing, evaluation tools, informatics in bracing etc.10 These aims made the main part of the scope of this research.
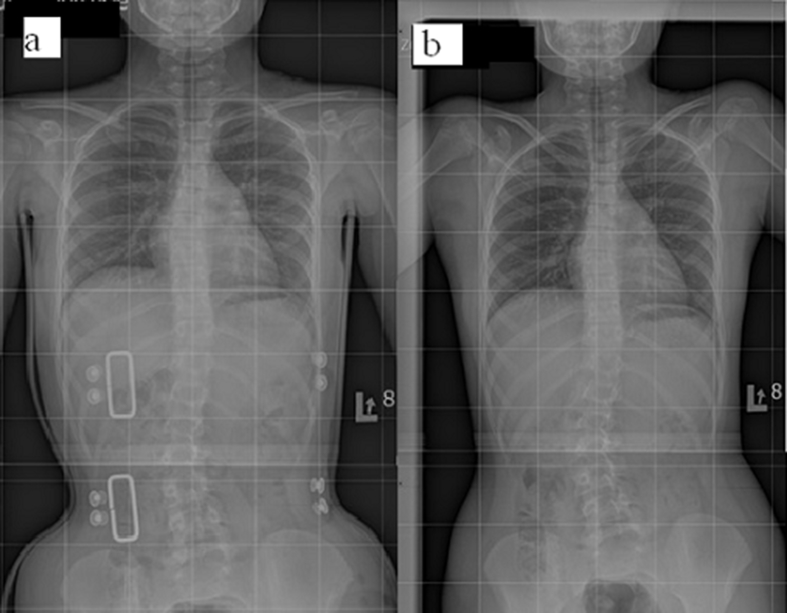
The treatment of AIS with an orthopaedic brace must be closely supervised by a specialist. The control visits require the assessment of curve progression. Generally, an x-ray imaging is the method of choice for the evaluation of the degree of correction, fit, and overall spinal balance and for further management decisions. It is regarded as the most reliable diagnostic tool which precisely reflects the current angle of curvature. Unfortunately, quite often the first x-ray is taken when the brace in on the body and the second one is performed immediately after removing the brace. This practice usually results in two almost identical images [Fig. 1 – no difference in the Cobb angle (24°) has been observed].
Fig. 1.
10-year-old girl with an adolescent idiopathic scoliosis (Risser sign = 0). A standing anteroposterior radiograph of the patient in the brace (a) and when the brace has been removed (b) (own data).
This may suggest inappropriate correction of the angle of the curve in patient wearing brace and lead to hasty conclusions about poor-fitting.
There has been many studies showing that bracing can improve the angle of curvature (effectively stop curvature progression) as well as the trunk deformity. The long-term stabilization of curve correction has been shown and no change with respect to trunk deformity has been observed when compared to the intermediate result achieved after two years of treatment. After Chêneau light brace weaning half of the Cobb angle (compared to the start of treatment) has been achieved.11
On the other hand, short stabilization of correction has not been discussed yet. The time when the spine comes back to uncorrected posture depends on many factors. Successful use of a brace depends on the amount of time the patient is wearing the brace. The brace is worn until growth is complete between 16 and 23 hours a day. Thus, the aim of the study was to evaluate the relationship between the above mentioned factors and the duration of the correction of the trunk rotation effect after the brace is taken off.
Methods
It has been hypothesized that after removing the Chêneau brace (CAST), the changes in trunk rotation could occur. However, the duration of the correction hasn't been known. Moreover, specific factors e.g. Cobb angle, Risser sign and axial rotation of the apical vertebrae could affect the reverse of the back contour after taking the brace off.
Participants
The target population for this study was patients (59 girls) diagnosed and treated with progressing adolescent idiopathic scoliosis (AIS) at the Department and Clinic of Rehabilitation (University of Warmia and Mazury in Olsztyn, Poland).
Patients were divided into two groups: the brace-wearing group (B) and control group (C). The characteristics of these two groups has been shown in Table 1.
Table 1.
Characteristics of the population studied.
| Variable | Subgroup | Na | MEAN | Standard deviation |
|---|---|---|---|---|
| Age [years] | B-Th | 32 | 14,50 | 1,52 |
| B-L | 21 | 15,14 | 1,20 | |
| C-Th | 16 | 13,90 | 2,50 | |
| C-L | 15 | 14,00 | 2,20 | |
| Cobb angle [°] | B-Th | 32 | 31,31 | 6,71 |
| B-L | 21 | 29,86 | 9,26 | |
| C-Th | 16 | 36,70 | 13,10 | |
| C-L | 15 | 31,90 | 9,90 | |
| Rotation angle [°] | B-Th | 32 | 10,63 | 5,79 |
| B-L | 21 | 17,38 | 7,35 | |
| C-Th | 16 | 12,10 | 6,40 | |
| C-L | 15 | 13,60 | 7,60 |
N – total number of curves.
Thirty nine girls, aged 10–18 years old, diagnosed with AIS and treated with Chêneau brace (CAST) formed group B. The patients from B group had thoracic (n = 17), thoracolumbar (n = 3), lumbar (n = 5) and double curve (n = 14) scoliosis.
Group C consisted of twenty girls, aged 10–18 years old, diagnosed with AIS, who have not been braced yet. The patients were diagnosed with: thoracic (n = 4), thoracolumbar (n = 3), lumbar (n = 2) and double curve (n = 11) scoliosis.
The total number of curves (n = 84, Table 1) has been calculated and used for the statistical analyses.
The inclusion criteria consisted of: AIS confirmed in the clinical and radiological assessment. Patients were either premenarcheal or <1 year postmenarcheal, had no history of brace treatment, no co-morbidities affecting the course of AIS such as genetic defects, neuromuscular disorders, metabolic disorders, history of severe trauma. Additional requirements for the B group were: Chêneau brace treatment for a minimum of 6 months, compliance with the number of hours of brace wearing 20h/day, x-ray confirmed good brace fitting and for the C group: no history of brace treatment.
Patients who had been treated previously12; who didn't comply with bracing recommendations or prematurely stopped the brace; who were simultaneously using another brace; and with Risser sign more than 4 were excluded from the study.
Additionally, the B group was subdivided for the purpose of statistical analysis into: thoracic curve subgroup (B-Th) which included 32 curves and lumbar curve subgroups (B-L) with 21 curves (Table 1). Within each subgroup, (i.e. B-Th and B-L), the patients were further classified based on: Cobb angle: a) < 30°, b) ≥ 30°, longitudinal axial rotation of the apical vertebrae according to the method of Perdriolle: a) rotation of 5°–15°, b) rotation of 16°–25°, Risser sign (RS): a) RS 0–2, b) RS 3–4. The intrarater reliability as well as the average intrarater error of the method of Perdriolle showed that this method was a useful tool for the follow-up of vertebral rotation.13
Group C was also subdivided into: thoracic curve subgroup (C-Th), which included 16 curves, and lumbar curve subgroups (C-L) with 15 curves. Within each subgroup, (i.e. C-Th and C-L), the patients were classified based on: Cobb angle: a) < 30°, b) > = 30°, longitudinal axial rotation of the apical vertebrae according to the method of Perdriolle: a) rotation of 5°–15°, b) rotation of 16°–25°, Risser sign (RS): a) RS 0–2, b) RS 3–4.
Experimental design
All the procedures involving human participants conformed to the ethical guidelines of the 1975 World Medical Association Declaration of Helsinki (and its later amendments or comparable ethical standards) as reflected in a priori approval by the institution's human research committee and followed the Adapted Physical Activity (APA) Ethics Standard. This research was approved by the Ethics Committee. The experiment was conducted with the understanding of each subject. All subjects as well as their parents gave written informed consent to participate in this study.
The diagnostic tests of both studied groups were performed six times: after 0, 2, 24, 30, 48 and 54 hours. The girls from B group were tested immediately after the brace had been taken off, and the girls from C group were diagnosed after a night rest, both groups at about 7 a.m.
The measurements of the patients took place during their hospitalization at the Clinic of Rehabilitation and the hours of tests correlated with the ward procedures in order to exclude any influence on the angle of trunk rotation (ATR) measurements.
Measurements
Posterior-anterior radiographs were obtained from the clinical assessment of all subjects and were subsequently used to determine Cobb angles.14 The measurements of the trunk rotation were taken with the Scoliometer® and back-contour device during Adams forward bending test by the two evaluators/diagnosticians.15
Scoliometer® assessment
The reliability of the measurements obtained with the Scoliometer® was determined as very good to excellent in a previous study.16
Thus, in this study the Scoliometer® was used to analyse the axial rotation of the trunk (i.e. ATR) in patients with idiopathic scoliosis. The Scoliometer® was placed over spinous processes of the back and was drawn along them to measure the axial trunk rotation. During the first measurement the spinous process with the highest value of ATR was marked with a waterproof marker. This space was used during next measurements in order to reproduce the same level as in previous examination. The evaluation performed with the Scoliometer® with the participants standing in trunk flexion was shown in Fig. 2.
Fig. 2.
The measurement of angle of trunk rotation using Bunnell scoliometer during forward bending – posterior view (own data).
The changes in ATRs during 54 hours of observation were performed after the brace had been taken off (t 0, 2, 24, 30, 48 and 54 hours after debracing). This was described using VATR variable, defined as the change in the absolute Scoliometer® readings in the time intervals against the time interval Δt between the measurements (equations (1), (2), (3), (4), (5))).
| (1) |
| (2) |
| (3) |
| (4) |
| (5) |
The above mentioned formulas define the angular velocity/change of angular displacement calculated at t time after removing the brace, and compared to the value measured at t0.
Back-contour assessment
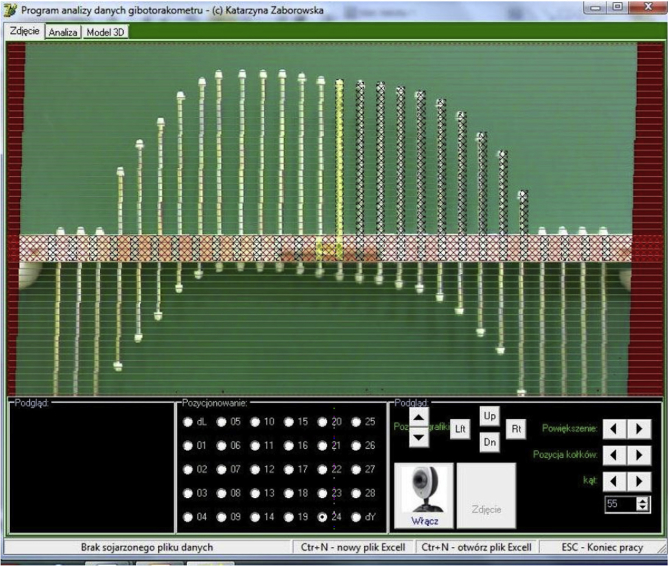
Back-contour device was employed as an alternative to invasive imaging.14 In this study, it was used to evaluate the rotation of the trunk and for the assessment of the topographic changes along a chosen linear axis. Back-contour device consists of 28 movable spikes placed at the distance of 1 cm from each other. The evaluation of the hump on the thoracic region during forward bending was shown in Fig. 3.
Fig. 3.
Clinical photograph during the evaluation of rib hump deformity with the back-contour device (own data).
Back-contour device was placed on a specially designed board where the position of spikes was captured with a digital camera. The picture was then imported into specific software (Polish version of the “Program analizy danych gibotorakometru”) for picture calibration and data collection (Fig. 4).
Fig. 4.
Back-contour device software (own data).
The differential factor (kra) has been used for the digital analysis. The changes in kra over 54 hours of observation were expressed as Vkra factor, defined as the difference in the absolute value of the amplitude differential factor (kra) in the time intervals against the time interval Δt between the measurements (Equations (6), (7), (8), (9), (10))).
| (6) |
| (7) |
| (8) |
| (9) |
| (10) |
The above mentioned formulas define the velocity of kra change as calculated at t time after removing the brace, compared to the previous value measured at t0 after debracing.
Statistical methods
Statistical analysis was performed using Statistica 12.0 software.17 The distribution of variables in samples were tested using the Shapiro–Wilks test. The data were presented as mean and standard deviation (SD). The statistical significance was set at p < 0.05. The non-parametric U-Mann–Whitney test was used for the comparisons between the studied groups.
Results
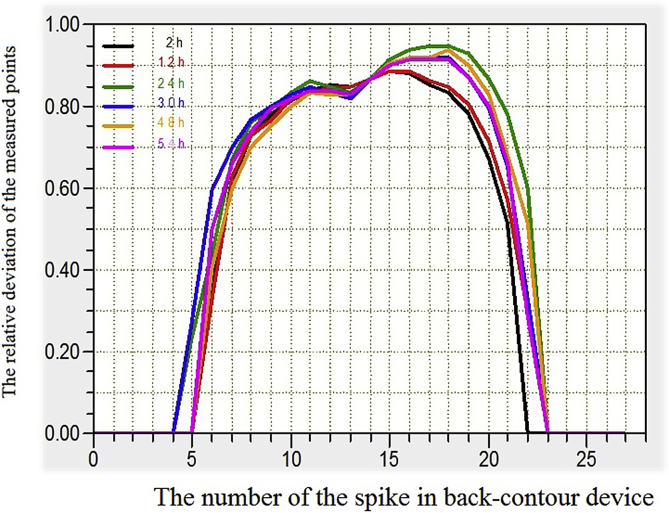
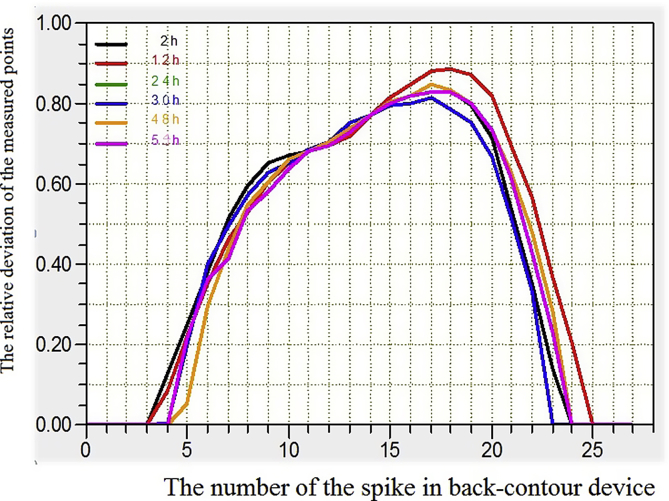
The dynamics of the trunk contour changes in thoracic and lumbar region of the spine in relation to the time after brace removal was shown in Fig. 5 and Fig. 6.
Fig. 5.
The sample of geometrical changes of the trunk contour in patients from B-Th group dependent on the time after removing the brace.
Fig. 6.
The sample of geometrical changes of the trunk contour in patients from B-L group dependent on the time after removing the brace.
The significant changes in the trunk rotation after Chȇneau brace had been taken off took place over the first two hours of observation (see Table 2, Table 3). Statistically significant differences were shown in the thoracic as well as at the lumbar region in patients with Cobb angle ≥30°, longitudinal axial rotation of the apical vertebrae from 5 to 15° and Risser sign from 0 to 2. After twenty four hours, the statistically significant changes were noted only within the lumbar region when the Cobb angle was lower than 30° and at the rotation angle from 5 to 15°. In patients with Risser sign from 0 to 2 the changes were noted after two and after thirty hours after debracing, both in the group of lumbar and thoracic curvatures (Table 2, Table 3).
Table 2.
The results of the U-Mann–Whitney test in patients wearing the brace (B) vs. control (C) groups at the thoracic region of the spine.
| Time [h] | Cobb angle |
Axial rotation |
Risser sign |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <30° |
≥30° |
5°–15° |
16°–25° |
0–2 |
3–5 |
|||||||
| VATR | Vkra | VATR | Vkra | VATR | Vkra | VATR | Vkra | VATR | Vkra | VATR | Vkra | |
| 2 | 1,00 | 0,55 | 0,28 | 0,02∗ | 0,28 | 0,03∗ | 0,55 | 0,86 | 0,10 | 0,05 | 0,51 | 0,18 |
| 24 | 0,31 | 0,81 | 0,38 | 0,63 | 0,54 | 0,94 | 0,35 | 1,00 | 0,25 | 0,74 | 0,44 | 0,81 |
| 30 | 0,13 | 0,72 | 0,82 | 0,90 | 0,50 | 0,71 | 0,69 | 1,00 | 0,74 | 0,03∗ | 0,51 | 0,14 |
| 48 | 0,61 | 1,00 | 0,93 | 0,33 | 0,94 | 0,30 | 0,45 | 0,11 | 0,50 | 0,96 | 0,34 | 0,87 |
| 54 | 0,13 | 0,81 | 0,98 | 0,26 | 0,11 | 0,32 | 0,85 | 0,22 | 0,74 | 0,11 | 0,16 | 0,31 |
∗p < 0.05 – a statistically significant differences between studied groups.
Table 3.
The results of the U-Mann–Whitney test in patients wearing the brace (B) group vs. control (C) groups in the lumbar region of the spine.
| Time [h] | Cobb angle |
Axial rotation |
Risser sing |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <30° |
≥30° |
5°–15° |
16°–25° |
0–2 |
3–5 |
|||||||
| VATR | Vkra | VATR | Vkra | VATR | Vkra | VATR | Vkra | VATR | Vkra | VATR | Vkra | |
| 2 | 0,01∗ | 0,20 | 0,01∗ | 0,00∗ | 0,02∗ | 0,01∗ | 0,02∗ | 0,11 | 0,10 | 0,05∗ | 0,51 | 0,18 |
| 24 | 0,05∗ | 0,30 | 0,37 | 0,70 | 0,01∗ | 0,27 | 0,83 | 0,55 | 0,25 | 0,74 | 0,44 | 0,81 |
| 30 | 0,94 | 0,74 | 0,46 | 0,35 | 0,56 | 1,00 | 0,56 | 0,23 | 0,74 | 0,03∗ | 0,51 | 0,14 |
| 48 | 0,61 | 0,90 | 0,06 | 0,81 | 0,79 | 0,96 | 0,17 | 0,62 | 0,50 | 0,96 | 0,34 | 0,87 |
| 54 | 0,33 | 0,06 | 0,47 | 0,66 | 0,14 | 0,40 | 1,00 | 0,55 | 0,74 | 0,11 | 0,16 | 0,31 |
∗p <0.05 – a statistically significant differences between studied groups.
When the subgroup of patients with the longitudinal axial rotation of the apical vertebrae within 16°–25° range was analysed, a statistically significant difference was noted only within the first time interval (i.e. after two hours). In this study, the patients with low values of Risser sign (from 0 to 2) proved to be less geometrically stable after removing the brace, compared with the group with advanced Risser sign (from 4 to 5).
Discussion
As we hypothesized the dynamic changes in trunk rotation over the first 2 and 24 hours after removing the Chêneau brace were observed. The highest changes during short period of time has been noted in thoracic region. Our previous experiences show that it could be explained by geometrical instability of upper body. Moreover, the specific asymmetry of upper body (e.g. in acromion and scapula) are less prone for correction when compared to the pelvic complex. These changes rapidly comes to the initial state before the correction (data yet not published). It could be assumed that it is associated with more stable complex of lower body in comparison with upper body (more stable kinematic chains).
This study also showed that the dynamic changes in trunk deformation appears faster in patients with Cobb angle >30° and the Risser sign 1–2. The scoliotic changes in these patients are considered as being more progressing and the correction is more difficult. Taking this into account, the treatment should be introduced immediately without waiting for the deformation progression. The short period of de-correction should change the recommendations in these patients in order to have the brace on for a longer period of time.
The latter was highly crucial from the clinical point of view. The clinicians should pay more attention to patients who do not follow medical recommendations and exceed the time without the Chêneau brace by more than what is needed for personal hygiene or exercise. Patients should be instructed that the correction of the spine takes place only when the brace is on the body. Morevoer, the effectiveness of the Chêneau brace in halting the progression of the AIS has been experimentally proven.18 Although full-time bracing has the longest history, some negative psychosocial effects of daytime bracing have led to the study of part-time bracing protocols (using e.g. the Providence brace). However, this alternative has resulted in slight progression of the AIS.19
The magnitude of the trunk rotation significantly depends on Cobb angle and longitudinal axial rotation of the apical vertebrae. It is well known that the higher values of Cobb angle are associated with greater rotation angles.20 In this study, the transverse plane deformation was analysed by assessing changes in the trunk rotation angle (VATR) and geometrical outline of the trunk (Vkra). Other authors showed a strong correlation in thoracic curvatures between ATR and Cobb angle as well as the longitudinal axial rotation21, 22 of the apical vertebrae measured according to the method of Perdriolle.23 However, this relationship has been less evident in the lumbar region.24
The Cobb method is the most widely used to determine the angular value of scoliosis and it is defined as the “gold standard”. However, this requires an x-ray examination as well as a qualified specialist. It was shown that there was a poor correlation between the Cobb measurements taken by spine orthopaedists and orthopaedic residents. That demonstrated difficulties in the method, which cannot even be overcome by expertise.25 Thus, in this study only clinical measurements were performed and the patients were not exposed to the additional dose of ionising radiation. Taking the potential harmful effect of an x-ray into consideration the number of radiological evaluations should be limited to the necessary minimum.26 Moreover, a controlled x-ray during the first visit (e.g. in the group of patients treated with Chêneau brace) should not be taken before the time the spine returns to its uncorrected shape.
Earlier studies showed a high27 or moderate28 correlation between the axial trunk rotation (ATR) values and the Cobb angles [scoliometer measurements vs. radiograph analyses was considered good (r = 0.7, p < 0.05)]. It was also shown that this correlation is stronger in the case of thoracic region compare to lumbar region.24 Thus, in this study the implementation of back-contour assessment has been crucial for overall diagnosis of the patient.
The discussions over the advantages and disadvantages of bracing have been going on for many years but they seem to have come to a halt with the results of a multicentre, prospective controlled study (BRAIST) published in 2013.29 The data clearly indicate that the use of orthopaedic braces alter the natural history of scoliosis and the final result of the curve correction correlates with the time of bracing.18
The latest cutting edge technology standards lead to the reduction of time in brace.30 From the patients' perspective it is reasonable to assume the proper time that improvements of Cobb angle and trunk deformity could be achieved. Thus, in this study the time interval, when the spine comes to its preliminary state, after taking the brace off, has been studied.
Moreover, we do understand that the level of correction (e.g. 20% in comparison with 60%) could have an impact on the results obtained. Earlier studies cleared only the correlation between rtg in-brace correction and short time results of brace (significant correlation range 0.64–0.98). Low in-brace correction had a low correlation coefficient between in-brace correction and out of brace (after 6 month treatment) for thoracic and lumbar curves showing the best results for thoracic curves.31 Furthermore, the in-brace correction seems able to predict the short time results of treatment.32
The long-term correction of brace treatment has been studied widely. The latest research showed only slight loss of correction 15 years post bracing. Moreover, contrary to this studies, no difference in terms of long-term results and progression has been found between patients with ≤30° vs > 30° Cobb angles.33
The results of this study have also another clinical rehabilitation impact. The patients as well as their parents, who do not follow the recommendations of 23-hour brace treatment, should realize that after 2 hours from removing the brace the back contour correction is lost. The main aim of the bracing is to reduce the angle of trunk rotation as well as the cosmetic improvement of posture (cosmetic effect). Thus, the time of bracing is the main priority.
Conclusions
The highest dynamics of the trunk rotation (after the experimental removing the Chȇneau brace) was observed within the first two hours of the 24 hours of observation. The results have a clinical implication. The patients should be advised to take the brace off for a minimum of two hours before the scheduled x-ray, to allow full relaxation of the trunk in order to obtain reliable radiological images of the deformation.
Conflicts of interest
The authors declare that there is no conflict of interests regarding the publication of this article.
Acknowledgements
This project was supported financially for the conduct of the research by the Ministry of Science and Higher Education research grant number No NN518288940 (for the years 2011–2014).
The authors would like to thank Rafał Sadowski, MA, for a critical reading of the manuscript and a writing assistance. We also thank the dedicated group of girls who made this study possible.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.The Terminology Committee of the Scoliosis Research Society A glossary of scoliosis terms. Spine. 1976;1(1):57–58. [Google Scholar]
- 2.Cobb J. Outline for the study of scoliosis. AAOS Instr Course Lec. 1948;5:261–275. [Google Scholar]
- 3.Mehta S.S., Modi H.N., Srinivasalu S. Interobserver and intraobserver reliability of Cobb angle measurement: endplate versus pedicle as bony landmarks for measurement: a statistical analysis. J Pediatr Orthop. 2009;29(7):749–754. doi: 10.1097/BPO.0b013e3181b72550. [DOI] [PubMed] [Google Scholar]
- 4.Bonanni P.G. Contour and angle-function based scoliosis monitoring: relaxing the requirement on image quality in the measurement of spinal curvature. Int J Spine Surg. 2017;11(3):173–182. doi: 10.14444/4022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Negrini S., Aulisa A.G., Aulisa L. 2011 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis. 2012;7(3):3. doi: 10.1186/1748-7161-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silva F.E., Lenke L.G. Adolescent idiopathic scoliosis. In: Errico T.J., Lonner B.S., Moulton A.W., editors. Surgical Management of Spinal Deformities. Saunders Elsevier; Philadelphia, Pa: 2009. pp. 97–118. [Google Scholar]
- 7.Fang M.Q., Wang C., Xiang G.H., Lou C., Tian N.F., Xu H.Z. Long-term effects of the Chêneau brace on coronal and sagittal alignment in adolescent idiopathic scoliosis. J Neurosurg Spine. 2015;23(4):505–509. doi: 10.3171/2015.2.SPINE14970. [DOI] [PubMed] [Google Scholar]
- 8.Chêneau J., Corset-Chêneau . Frison-Roche; Paris: 1994. Manuel dórtopedic des scolioses suivant la technique originale. [Google Scholar]
- 9.Rigo M., Weiss H.R. The Chêneau concept of bracing—biomechanical aspects. Stud Health Technol Inf. 2008;135:303–319. [PubMed] [Google Scholar]
- 10.Negrini S. Bracing adolescent idiopathic scoliosis today. Disabil Rehabil Assist Technol. 2008;3(3):107–111. doi: 10.1080/17483100801942887. [DOI] [PubMed] [Google Scholar]
- 11.Weiss H.R. Bracing can lead to a persistent correction in the treatment of Adolescent Idiopathic Scoliosis: a case report. Hard Tissue. 2014;3(1):8–12. [Google Scholar]
- 12.Richards B.S., Bernstein R.M., D'Amato C.R., Thompson G.H. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine (Phila Pa 1976) 2005;30(18):2068–2077. doi: 10.1097/01.brs.0000178819.90239.d0. [DOI] [PubMed] [Google Scholar]
- 13.Weiss H.R. Measurement of vertebral rotation: Perdriolle versus Raimondi. Eur Spine J. 1995;4(1):34–38. doi: 10.1007/BF00298416. [DOI] [PubMed] [Google Scholar]
- 14.Pearsall D.J., Reid J.G., Hedden D.M. Comparison of three noninvasive methods for measuring scoliosis. Phys Ther. 1992;72(9):648–657. doi: 10.1093/ptj/72.9.648. [DOI] [PubMed] [Google Scholar]
- 15.Bunnell W. Selective screening for scoliosis. Clin Orthop Relat Res. 2005;434:40–45. doi: 10.1097/01.blo.0000163242.92733.66. [DOI] [PubMed] [Google Scholar]
- 16.Bonagamba G.H., Coelho D.M., Oliveira A.S. Inter and intra-rater reliability of the scoliometer. Braz J Phys Ther. 2010;14(5):432–438. [Article in English, Portuguese] [PubMed] [Google Scholar]
- 17.StatSoft, Inc . 2014. STATISTICA (Data Analysis Software System), Version 12.www.statsoft.com [Google Scholar]
- 18.De Giorgi S., Piazzolla A., Tafuri A., Borracci C., Martucci A., De Giorgi G. Chêneau brace for adolescent idiopathic scoliosis: long-term results. Can it prevent surgery? Eur Spine J. 2013;(Suppl 6):S815–S822. doi: 10.1007/s00586-013-3020-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bohl D.D., Telles C.J., Golinvaux N.S., Basques B.A., DeLuca P.A., Grauer J.N. Effectiveness of Providence nighttime bracing in patients with adolescent idiopathic scoliosis. Orthopedics. 2014;37(12):e1085–e1090. doi: 10.3928/01477447-20141124-56. [DOI] [PubMed] [Google Scholar]
- 20.Carlson B.B., Burton D.C., Asher M.A. Comparison of trunk and spine deformity in adolescent idiopathic scoliosis. Scoliosis. 2013;8(1):2–6. doi: 10.1186/1748-7161-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krawczyński A., Kotwicki T., Szulc A., Samborski W. Kliniczny i radiologiczny pomiar rotacji kręgów u chorych ze skoliozą idiopatyczną. Ortopedia Traumatologia Rehabilitacja. 2006;6(1):602–607. [Article in Polish] [PubMed] [Google Scholar]
- 22.Korovesis P., Stamatakis M. Prediction of scoliotic Cobb angle with the use of scoliometer. Spine. 1996;21(14):1661–1666. doi: 10.1097/00007632-199607150-00010. [DOI] [PubMed] [Google Scholar]
- 23.Perdriolle R., Vidal J. Morphology of scoliosis: three dimensional evolution. Orthopedics. 1987;10(6):909–915. doi: 10.3928/0147-7447-19870601-10. [DOI] [PubMed] [Google Scholar]
- 24.Kotwicki T., Frydryk K., Lorkowska M., Krawczyński A., Szulc A. Powtarzalność i zgodność pomiaru rotacji tułowia skoliometrem Bunnella u dzieci ze skoliozą idiopatyczną. Fizjoterapia Polska. 2006;2(4):111–116. [Google Scholar]
- 25.Ritter R., Nagasse Y., Ribeiro I., Yamazato C., Oliveira de Fabio M., Kusabara R. Comparison of Cobb angle measurement in scoliosis by residents and spine experts. Coluna/Columna. 2016;15(1):13–16. [Google Scholar]
- 26.Ronckers C.M., Land C.E., Miller J.S., Stovall M., Lonstein J.E., Doody M.M. Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat Res. 2010;174(1):83–90. doi: 10.1667/RR2022.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Griffet J., Leroux M.A., Badeaux J., Coillard C., Zabjek K.F., Rivard C.H. Relationship between gibbosity and Cobb angle during treatment of idiopathic scoliosis with the SpineCor brace. Eur Spine J. 2000;9(6):516–522. doi: 10.1007/s005860000175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coelho D.M., Bonagamba G.H., Oliveira A.S. Scoliometer measurements of patients with idiopathic scoliosis. Braz J Phys Ther. 2013;17(2):179–184. doi: 10.1590/S1413-35552012005000081. [DOI] [PubMed] [Google Scholar]
- 29.Grivas T.B., Kotwicki T., Maruyama T., Obrien J., Labelle H., Hresko T. The BrAIST study and the implications for scoliosis screening: our duty for raising awareness and advocacy. Scoliosis. 2014;9(Suppl 1):O42. [Google Scholar]
- 30.Weiss H.R., Seibel S., Kleban A. Deformity-related stress in a sample of patients with adolescent idiopathic scoliosis (AIS) after brace weaning: a cross-sectional investigation. OA Musculoskelet Med. 2014;12(1):1–6. [Google Scholar]
- 31.Zaina F., Donzelli S., Lusini M., Negrini S. Correlation between in-brace radiographic correction and short time brace results. Stud Health Technol Inform. 2012;176:342–345. [PubMed] [Google Scholar]
- 32.Landauer F., Wimmer C., Behensky H. Estimating the final outcome of brace treatment for idiopathic thoracic scoliosis at 6-month follow-up. Pediatr Rehabil. 2003;6(3-4):201–207. doi: 10.1080/13638490310001636817. [DOI] [PubMed] [Google Scholar]
- 33.Aulisa A.G., Guzzanti V., Falciglia F., Galli M., Pizzetti P., Aulisa L. Curve progression after long-term brace treatment in adolescent idiopathic scoliosis: comparative results between over and under 30 Cobb degrees - SOSORT 2017 award winner. Scoliosis Spinal Disord. 2017;12:36–42. doi: 10.1186/s13013-017-0142-y. [DOI] [PMC free article] [PubMed] [Google Scholar]