Abstract
Hemorrhagic occlusive retinal vasculitis (HORV) is a condition associated with intraocular vancomycin during surgical intervention, most frequently following bilateral sequential cataract surgery. Because of the high rate of ophthalmic vascular complications in this condition, gonioscopic evaluation for identification of neovascularization of the angle and iris is essential. Careful examination can reveal previously asymptomatic and unassociated lesions of the iris or ciliary body. We present the case of a 71-year-old female who was diagnosed with a ciliary body melanoma secondary to complete ophthalmic examination associated with HORV. She reported decreased vision to light perception in the left eye (OS) following sequential, bilateral cataract surgery. Fundus examination OS demonstrated diffuse retinal vasculitis, retinal ischemia, and extensive hemorrhage. Evaluation included inflammatory and coagulopathy laboratory evaluation, carotid ultrasonography and magnetic resonance imaging (MRI) of the brain and orbits, all of which proved unrevealing, except for an enhancing mass OS on MRI. Further evaluation revealed a pigmented mass with features of melanoma in the anterior chamber angle extending into the ciliary body. Fine needle aspiration biopsy revealed high risk cytogenetic characteristics, and plaque radiotherapy was successfully employed.
Keywords: Ciliary body, Hemorrhagic occlusive retinal vasculitis, Intracameral vancomycin, Malignant melanoma, Plaque radiotherapy, Uvea
Introduction
Early diagnosis and treatment of uveal melanoma can reduce metastatic risk and result in survival benefit.1, 2, 3, 4 Ciliary body melanoma is particularly concerning because of the independent elevated risk for metastatic disease compared to iris or choroidal melanoma.1, 2, 3, 4 Some speculate the worse prognosis is secondary to a rich vascular supply potentiating hematogenous spread and the cryptic location masking the tumor until it achieves large size.1, 2, 3, 4
Hemorrhagic occlusive retinal vasculitis (HORV) is a rare ischemic retinal vasculitis that has been temporally associated with intraocular vancomycin used during bilateral sequential cataract surgery or intravitreal injection.5 The features of HORV include delayed onset painless decreased vision, mild to moderate anterior chamber and vitreous inflammation, sectoral intraretinal hemorrhage in areas of nonperfusion and sectoral retinal vasculitis and vascular occlusion on fluorescein angiography.5 Herein, we describe a case of HORV that led to timely and fortuitous discovery of an asymptomatic unrelated ciliary body melanoma.
Case report
A 71-year-old woman with visual acuity of 20/70 in the right (OD) and left (OS) eye underwent uneventful cataract surgery OD then OS over a two-week interval. Following surgery OS, on post-operative day one, visual acuity was 20/25 OD and 20/70 OS with normal post-operative clinical examination. On post-operative day two, visual acuity decreased to hand motions OS with mild vitreous haze, diffuse retinal hemorrhages, and sectoral retinal ischemia. An extensive laboratory and imaging evaluation for retinal vasculitis was performed including magnetic resonance imaging (MRI) and angiogram (MRA) of the brain and orbits, all of which were negative. The patient was presumed to have a central retinal vein occlusion and referred for second opinion.
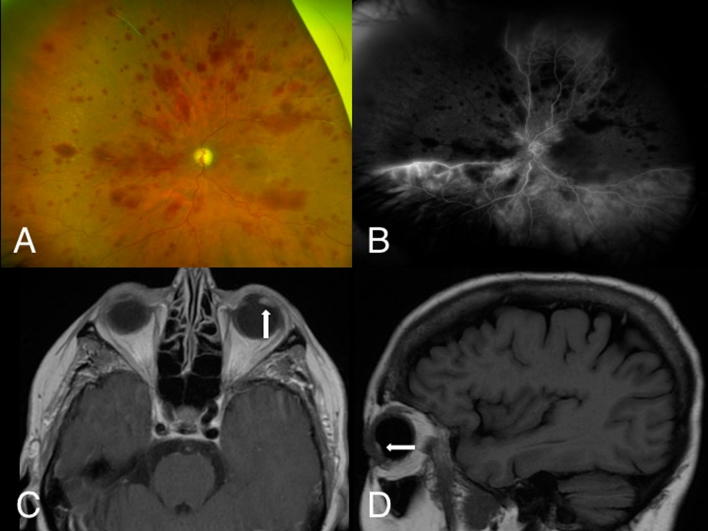
On examination, OD was within normal limits. Examination OS revealed optic nerve pallor, slight venous tortuosity, arterial vascular stasis with boxcarring, arterial and venous sclerosis in the superonasal and superotemporal peripheral retina, and diffuse intraretinal hemorrhage (Fig. 1A). Optical coherence tomography (OCT) was normal OD and showed thin disorganized retinal layers OS. Fluorescein angiography was normal OD but revealed non-perfusion in nearly the entire nasal and temporal quadrants OS with diffuse small vessel leakage (Fig. 1B). Gonioscopy OS disclosed no angle or iris neovascularization, but a pigmented ciliary body mass with angle invasion was found. Further review of the prior MRI revealed a small enhancing ciliary body mass OS (Fig. 1C, D).
Fig. 1.
(a) On our examination after cataract surgery, the left eye demonstrated optic nerve pallor, slight venous tortuosity, vascular boxcarring, (b) angiographic sclerosis with non-perfusion of arteries and veins in the superonasal and superotemporal retina and diffuse intraretinal hemorrhage throughout the macula and periphery. (c) T1 axial post-contrast magnetic resonance image (MRI) demonstrated a small enhancing ciliary body mass in the left eye (arrow). (d) A T1 sagittal post-contrast MRI showed the same lesion (arrow).
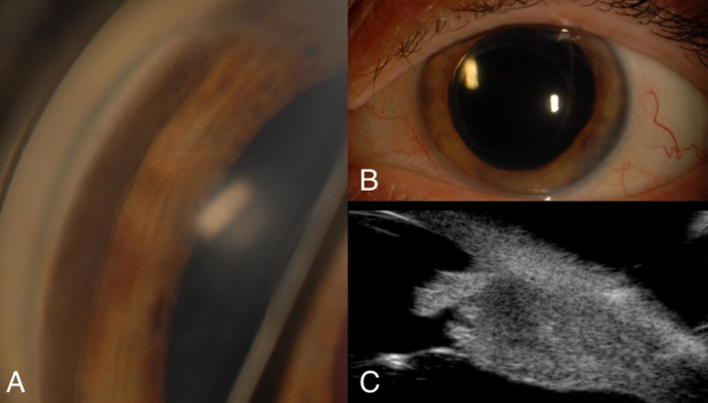
The patient was sent to our service for opinion regarding the ciliary body mass. Examination was consistent with the findings of the referring ophthalmologist. Gonioscopy documented the iridociliary mass (Fig. 2A, B), which caused a shadow measuring nine mm in basal diameter on transillumination. Ultrasound biomicroscopy demonstrated 4.4 mm in thickness (Fig. 2C). These findings were consistent with ciliary body melanoma OS.
Fig. 2.
(a) Gonioscopy revealed a pigmented mass in the inferotemporal anterior chamber angle. (b) Slit lamp evaluation revealed increased pigmentation of the peripheral iris from 3 to 5o’clock. (c) Ultrasound biomicroscopy of the ciliary body lesion demonstrated an acoustically dense lesion measuring approximately 4.4 mm in thickness.
A review of the cataract surgery operative notes revealed exposure to intracameral vancomycin (0.25 mg) at both surgeries. The hemorrhagic retinopathy OS was consistent with HORV OS. This case was reported to the American Society of Cataract and Refractive Surgery and American Society of Retina Specialists joint HORV task force.
The melanoma was treated with I-125 plaque radiotherapy with tumor apex dose of 70 Gy over 104 hours. Transscleral fine needle aspiration biopsy for cytogenetics revealed mosaic monosomy of chromosome three, amplification of chromosome six (6p and 6q), and disomy of chromosome eight, imparting increased risk for metastasis. Lifelong screening for systemic metastasis was advised.
At six months follow-up, visual acuity was 20/25 OD and no light perception OS with normal intraocular pressures and regression of the melanoma to 2.4 mm in thickness. There was partial resolution of the hemorrhage, optic nerve atrophy, and segmental retinal vascular occlusion without retinal neovascularization.
Discussion
In a study of 36 eyes in 23 patients with HORV, ten patients were found to have unilateral disease.5 Of these, only two patients presented in a similar fashion to ours with HORV developing only in the second operated eye despite vancomycin exposure in both eyes during cataract surgery.5 It has been suggested that HORV is caused by a delayed hypersensitivity to vancomyin and this may explain why our patient did not develop changes in the right eye after the initial surgery.5 In the same series, overall visual results were poor with 61% of eyes having 20/200 or worse visual acuity and 22% with no light perception. Neovascular glaucoma (NVG) developed in 56% of eyes with HORV, frequently within two months of presentation.5 Early treatment with corticosteroids may be beneficial in HORV while anti-vascular endothelial growth factor injections and panretinal photocoagulation can help prevent NVG.5 In uveal melanoma, these treatments may also limit the effects of radiation damage after plaque radiotherapy.6, 7 Unfortunately, the combination of HORV and radiation therapy in this patient strongly predisposes to ischemia and NVG, emphasizing the need for close follow up and possible prophylactic measures.
In uveal melanoma, every millimeter of increasing tumor thickness adds 5% increased risk of metastasis.1 Tumor growth also allows for the accumulation of genetic alterations that increase the risk of metastasis.2 In a series of 136 patients with ciliary body melanoma, the average size at presentation was 13 mm in basal diameter and seven mm in thickness.4 While the tumor presented here was relatively small (nine mm in base and four mm in thickness) at presentation, it unfortunately had already accumulated one high risk cytogenetic feature (mosaic monosomy of chromosome three). In a series of 1059 patients with uveal melanoma, Kaplan-Meier estimates for melanoma-associated metastasis at one, three, five, and seven years for partial loss of chromosome three was 1%, 3%, 14%, and 17% respectively.3 In the same series, the greatest prognostic impact on metastasis was found with 8p loss, 8q gain, and complete monosomy three.3 Fortunately, the tumor in our patient did not exhibit these more risky chromosomal mutations, possibly reflecting the early detection and treatment of the tumor.
In this case, the diagnosis of HORV, while devastating for vision, led to early diagnosis of ciliary body melanoma, allowing for prompt treatment with plaque radiotherapy. While the tumor genetics revealed an increased risk for metastasis, a delay in diagnosis and management could have imparted a more unfavorable life prognosis.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Support provided by the Eye Tumor Research Foundation, Philadelphia, PA (CLS). Supported in part by an unrestricted/challenge award to Yale Eye Center from the Research to Prevent Blindness, Inc. (KHN). The funders had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review or approval of the manuscript. Carol Shields, M.D. has had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. No conflicting relationship exists for any author.
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
Contributor Information
Basil K. Williams, Jr., Email: basilkwilliams@gmail.com.
R. Joel Welch, Email: r.joel.welch@gmail.com.
Kristen H. Nwanyanwu, Email: k.nwanyanwu@yale.edu.
Carol L. Shields, Email: carolshields@gmail.com.
References
- 1.Shields C.L., Furuta M., Thangappan A. Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch Ophthalmol. 2009;127:989–998. doi: 10.1001/archophthalmol.2009.208. [DOI] [PubMed] [Google Scholar]
- 2.Shields C.L., Say E.A.T., Hasanreisoglu M. Cytogenetic abnormalities in uveal melanoma based on tumor features and size in 1059 patients: The 2016 W richard green lecture. Ophthalmology. 2017;124:609–618. doi: 10.1016/j.ophtha.2016.12.026. [DOI] [PubMed] [Google Scholar]
- 3.Shields C.L., Say E.A.T., Hasanreisoglu M. Personalized prognosis of uveal melanoma based on cytogenetic profile in 1059 patients over an 8-year period: The 2017 Harry S. Gradle lecture. Ophthalmology. 2017;124:1523–1531. doi: 10.1016/j.ophtha.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 4.Gunduz K., Shields C.L., Shields J.A., Cater J., Freire J.E., Brady L.W. Plaque radiotherapy of uveal melanoma with predominant ciliary body involvement. Arch Ophthalmol. 1999;117:170–177. doi: 10.1001/archopht.117.2.170. [DOI] [PubMed] [Google Scholar]
- 5.Witkin A.J., Chang D.F., Jumper J.M. Vancomycin-associated hemorrhagic occlusive retinal vasculitis: clinical characteristics of 36 eyes. Ophthalmology. 2017;124:583–595. doi: 10.1016/j.ophtha.2016.11.042. [DOI] [PubMed] [Google Scholar]
- 6.Materin M.A., Bianciotto C.G., Wu C., Shields C.L. Sector laser photocoagulation for the prevention of macular edema after plaque radiotherapy for uveal melanoma: a pilot study. Retina. 2012;32:1601–1607. doi: 10.1097/IAE.0b013e3182437e70. [DOI] [PubMed] [Google Scholar]
- 7.Shah S.U., Shields C.L., Bianciotto C.G. Intravitreal bevacizumab at 4-month intervals for prevention of macular edema after plaque radiotherapy of uveal melanoma. Ophthalmology. 2014;121:269–275. doi: 10.1016/j.ophtha.2013.08.039. [DOI] [PubMed] [Google Scholar]