Abstract
Objective To evaluate nutrition-only, exercise-only, and nutrition-plus-exercise interventions for optimizing gestational weight gain (GWG) based on the 2009 Institute of Medicine (IOM) guidelines.
Study PubMed, Google Scholar, and 2015 Cochrane Review were searched. Analysis of variance was used to determine if significant GWG differences exist between strategies, with additional subanalyses on overweight (OV) or obese women based on 2009 IOM guidelines.
Results Of 66 identified studies, 31 contributed data ( n = 8,558). Compared with routine prenatal care, nutrition-only interventions were significantly associated with reduced GWG and are most likely to produce weight gain within IOM recommendations ( p = 0.013). Exercise-only ( p = 0.069) and nutrition-plus-exercise ( p = 0.056) interventions trended toward GWG within IOM guidelines, but did not reach statistical significance. Supervised ( p = 0.61) and unsupervised ( p = 0.494) exercise programs had similar effectiveness. Subanalyses on OV or obese women produced similar results to studies that did not differentiate results based on body mass index: nutrition only ( p = 0.011), exercise only ( p = 0.308), and nutrition plus exercise ( p = 0.129).
Conclusion Preventing excessive GWG is crucial, especially for OV or obese women. In the current study, nutrition-based intervention is the health system strategy that showed significant impact on preventing excessive GWG compared with routine prenatal care. Among women who are OV or have obesity, nutrition-only interventions hold the most promise compared with routine prenatal care.
Keywords: nutrition intervention, exercise intervention, pregnancy, weight gain, obesity
More women are entering pregnancy as overweight (OV) or having obesity (OB) than in the past, and many are gaining excessive weight during pregnancy. During 2011 to 2014, 34.4% of the U.S. women of childbearing age (aged 20–39 years) are OV or have OB. 1 For women who gave birth in 2016, 21% aged 18 to 24 years, 23% aged 25 to 34 years, and 24% aged 35 to 44 years had OB. 2 Weight gain exceeding the Institute of Medicine (IOM) recommendations, known as excessive gestational weight gain (GWG), increases the burden of chronic disease and can put the mother and her infant's health at risk. These burdens include, but are not limited to, gestational hypertension, preeclampsia, gestational diabetes, cesarean section delivery, and preterm birth. 2 Additionally, children of mothers who gain more weight during pregnancy are at higher risk of being OV in early childhood. 3
Based on the 2009 IOM guidelines, the recommended amount of GWG for underweight women (body mass index [BMI] <18.5 kg/m 2 ) is 12.5 to 18 kg (28–40 lb), normal weight (NW) women (BMI 18.5–24.9 kg/m 2 ) is 11.5 to 16 kg (25–35 lb), OV women (BMI 25.0–29.9 kg/m 2 ) is 7 to 11.5 kg (15–25 lb), and women who have OB (BMI >30.0 kg/m 2 ) is 5 to 9 kg (11–20 lb). 4 Previous studies have addressed the ability to control GWG and prevent weight exceeding IOM recommendations where all forms of interventions were considered statistically significant: nutrition only, 5 6 7 8 nutrition only for OV/OB women, 9 10 11 12 nutrition plus exercise, 5 13 14 15 16 17 18 19 20 21 nutrition plus exercise for OV/OB women, 10 22 23 24 25 26 exercise only, 17 and exercise only for OV/OB women. 10 27 28 29 The study expands on the 2015 Cochrane Review (Muktabhant et al [2015]) assessment of methods involving nutrition, exercise, and combination of nutrition-plus-exercise intervention studies to prevent excessive pregnancy weight gain based on studies published after the 2009 IOM recommendations. The Cochrane Review found that whether women participated in nutrition, exercise, or both interventions, their risk of excessive GWG was reduced by an average of 20% and women of intervention groups were more likely to experience low GWG than those in control groups. 30 The Cochrane Review and other previous reviews included studies prior to 2009, which could not have used the updated IOM guidelines. A review of interventions that only includes studies published after 2009 is necessary. This meta-analysis exclusively uses studies published after updated IOM guidelines were available. The objective of this study is to quantitatively assess the effect of three health system strategies on GWG: nutrition-only, exercise-only, and combination of nutrition-plus-exercise interventions.
Methods
PubMed and Google Scholar databases were searched weekly from September 20, 2016, through October 29, 2016. All studies included in 2015 Cochrane Review were examined.
Initial key terms search produced 5,528,591 results. Key terms include “pregnancy,” “body mass index (BMI),” “nutrition,” “exercise,” “counseling,” “obesity,” “overweight,” or “intervention.” Limiting publish dates from 2009 to 2016 produced 1,199,520 results. Studies published before 2009 were assumed to not have used the 2009 IOM recommendations for GWG, and therefore, ineligible for this meta-analysis. “Gestational weight gain” filters narrowed results to 14,827. All studies were assessed: 12,363 excluded based on irrelevant title; 2,398 excluded based on irrelevant abstract. Full articles for the remaining 66 studies were obtained. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework was used for search and reporting of studies. Search was performed by primary author (K.A.C.). Not all aspects of PRISMA were addressed, including risk of bias across studies, due to single person data collection.
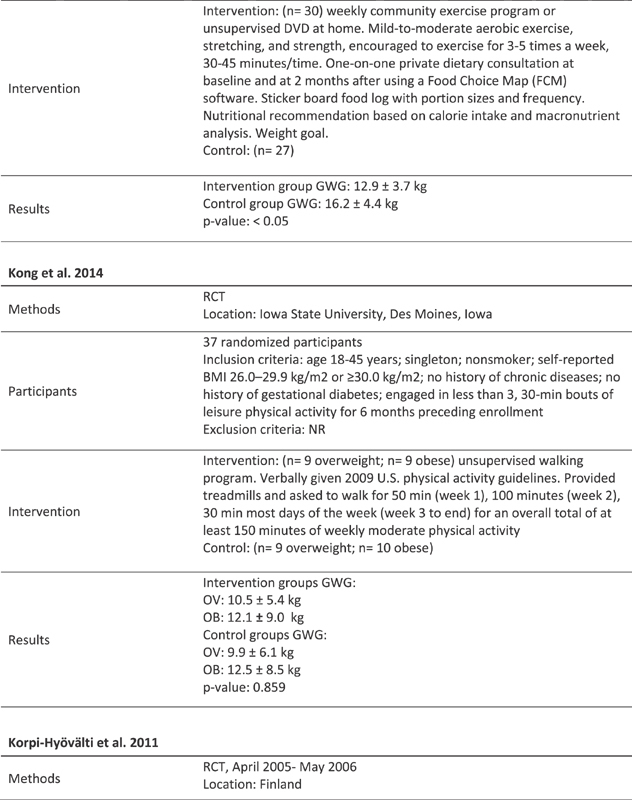
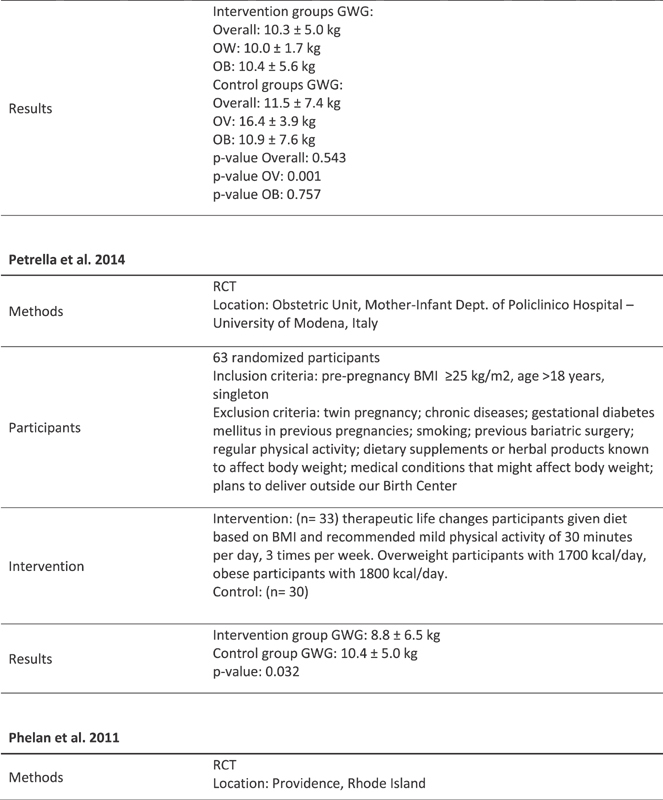
Reasons for exclusion include: mean GWG not reported, study published before 2009, and study in trial state ( Fig. 1 ). Inclusion criteria: randomized controlled parallel or cross-sectional study; at least 20 singleton pregnant women; women aged 18 years or older; control group with standard obstetric care; report means of GWG based on baseline BMI or pre-pregnancy BMI; and use 2009 IOM guidelines for GWG. For studies that did not use the 2009 IOM guidelines, additional analysis was made based on the reported mean GWG.
Fig. 1.
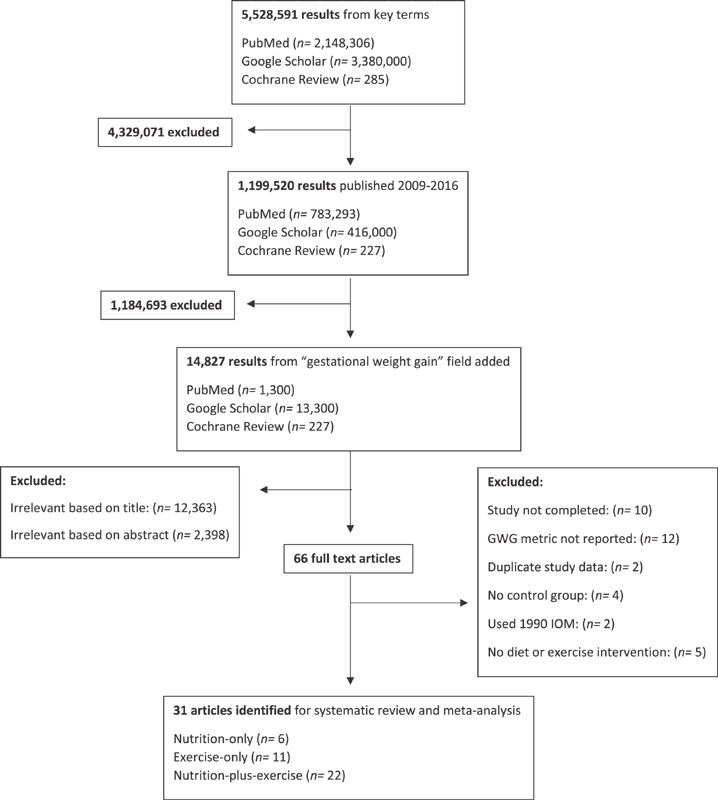
Electronic search strategy and inclusion criteria for studies used in meta-analysis.
Data were collected for total GWG in kilogram based on the BMI (kg/m 2 ) of women prior to pregnancy, age at the beginning of gestation, and pre-pregnancy BMI. Statistical analysis was done using Excel Version 2016 (Microsoft, Santa Rosa, CA, United States) and online Vassar Stats application a . Due to strong evidence of heterogeneity between studies, using the random effect approach, we addressed the source of this heterogeneity using subgroup analyses. Analysis of variance (ANOVA) was performed using Vassar Stats to compare effect of intervention and control groups within each study and relative effectiveness of health system strategies. The summary measure in this meta-analysis was the standardized mean difference, defined as the ratio of the difference in mean outcome between the groups and the standard deviation of the outcome among participants. Additional analysis on supervised versus unsupervised exercise was completed. Furthermore, we provided the average GWG means for interventions and subgroups, mean differences, and 95% confidence intervals in the results section.
Results
Study Search
Using the search terms, 66 results were identified. Thirty-five were excluded for not meeting criteria. Thirty-one involving 8,558 participants met criteria and contributed data to these analyses. Of these 31 studies, 6 were nutrition only, 31 32 33 34 35 36 22 were nutrition plus exercise, 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 and 11 were exercise only. 51 56 57 58 59 60 61 Four were used twice because data of participants with NW, OV, and having OB were analyzed separately. 48 59 60 61 Two were used twice because they reported data of different interventions within studies. 51 52 One included interventions based on exercise only and nutrition plus exercise. 51 One included interventions based on low intensity (LI) and moderate intensity (MI) exercise. 52 Results for all interventions reported separately were treated as separate studies. After separation of data, the 31 studies are analyzed as 39 studies.
Participants
These 39 studies involved 8,558 pregnant participants. Each study included 23 to 1,108 participants. No statistically significant differences in maternal age were reported. All studies required participants to be >18 years old and have singleton pregnancies. Studies recruited up to 26 weeks of gestation. Two recruited at the first prenatal visit. 36 61 One recruited at the 12th week of clinic. 47 One recruited at 6 to 16 weeks. 38 One required 7 to 21 weeks. 55 One recruited at eight to nine weeks. 46 Two required 8 to 12 weeks. 44 45 One required 10 to 14 weeks. 54 One required 10 to 16 weeks. 48 One required 10 to 18 weeks. 34 One required 10 to 20 weeks. 53 Two required <12 weeks. 39 56 One required <13 weeks. 33 One required <14 weeks. 37 One required 14 to 24 weeks. 60 Two required < 15 weeks. 40 59 One required 15 to 18 weeks. 49 Two required <16 weeks. 41 51 One required 16 to 20 weeks. 52 Two required <18 weeks. 50 57 One required <20 weeks. 43 One required <24 weeks. 58 One required <26 weeks. 42 Three studies did not report the gestational age requirement for participants. 31 32 35
Weight categories included NW (BMI 18.5–24.9 kg/m 2 ), OV (BMI 25.0–29.9 kg/m 2 ), and women with OB (BMI >30.0). Seventeen studies selected from general population without BMI specifications. 5 32 33 34 36 37 38 39 40 42 43 46 48 50 52 54 58 Three selected for OV participants. 31 47 53 Three selected for participants who are OV or have OB. 35 44 59 Eight selected for participants who have OB. 40 45 49 51 55 56 57 60 No significant differences in pre-pregnancy BMI.
Additional inclusion criteria include: nulliparous participants 32 37 ; secundigravida women previously given birth to macrosomic newborn 32 ; women expecting second pregnancy 36 ; healthy Caucasian mothers 54 ; no structured exercise program (>60 minutes once per week) 6 months before trial 58 ; sedentary (exercising for <20 minutes on <3 days/week) before study 61 ; not have engaged <3, 30-minute exercise per week for 6 months preceding enrollment, 60 nondiabetic 42 ; have at least one of the following risk factors: BMI >25 kg/m 2 ; gestational diabetes mellitus or any signs of glucose intolerance or newborn's macrosomia (>4,500 g) in early pregnancy; type 1 or 2 diabetes in first- or second-degree relatives; aged >40 years. 45
Setting
Based on World Bank classifications from 2017 economy, 28 studies occurred in high-income countries. 31 32 34 35 36 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 61 Three studies occurred in upper middle-income countries. 33 39 60 No studies occurred in low-income countries.
Eleven studies specified treatment locations: university hospitals 33 47 51 54 57 59 ; regular hospitals 32 55 56 ; eight multiethnic hospitals 49 ; obstetric clinic 38 60 ; and six primary care maternity health clinics. 46 All other studies did not specify treatment locations.
Intervention Implementation
Of the six nutrition-only studies, three focused on low glycemic index (LGI) foods. 32 34 36 All studies used a food diary to document past eating habits for nutrition plans and to detail food consumption during the trial. Three provided individual nutrition plans. 31 32 33 One provided focused nutritional advice based on the macronutrient composition of the participant's diet. 33 Three provided participants with lists of healthy foods based on local affordability 35 or LGI foods. 34 36 Three provided education in group settings. 34 35 36 General advice on nutrition, such as a pamphlet, is standard prenatal care and was not considered a nutrition-only intervention.
Of the seven exercise-only studies, four were supervised and three were unsupervised. Two studies included three supervised sessions per week, 57 60 one required participants to attend at least two sessions per week, 58 and one had one session per week. 60 Three supervised studies also had unsupervised exercise to be completed outside of the supervised sessions. 56 58 60 Types of exercise differed based on the study. One advised exercise based on an expenditure goal of 900 kcal/wk by means of a walking protocol that took place in five stages of VO2 measured for oxygen cost. 56 A heart rate monitor was provided to track exercise. One was based on a dance class and core exercises. 58 Two included aerobic and strength exercises. 57 60 One also included stretching. 60 One included aerobic, resistance, and core exercises. 61 One utilized pedometers 51 and one provided treadmills. 59 One registered daily steps on 7 consecutive days every 4 weeks and reminded participants of the recording period starting via text message. 51
Of the 19 nutrition-plus-exercise studies, 5 included group sessions and 14 provided one-on-one advice. Thirteen were unsupervised and six were supervised. Of the unsupervised interventions, three included DVD instructional videos for home exercise. 42 43 49 Additional implementations included: weight goal setting by the mother, 43 49 53 extrasupport for individuals not within IOM recommendations in which exercise and nutritional recommendations were revised, 38 39 48 food log, 39 40 43 48 50 pedometers, 48 51 text messages to remind participants when the daily steps recording period of 7 consecutive days every 4 weeks started, 51 profile-II nutritional program with six subscales to measure health behaviors, 39 exercises on reading food labels and shopping methods, 40 used Food Choice Map software, 42 43 free fitness membership, 54 heart rate monitors, 52 and calories calculated based on Dietary Approaches to Stop Hypertension (DASH) dietary pattern and reduced by 30% for participants without OB. 55 In addition to meeting the 2009 IOM recommendations, one study had the goal to keep weight within 3% of their weight at randomization. 55
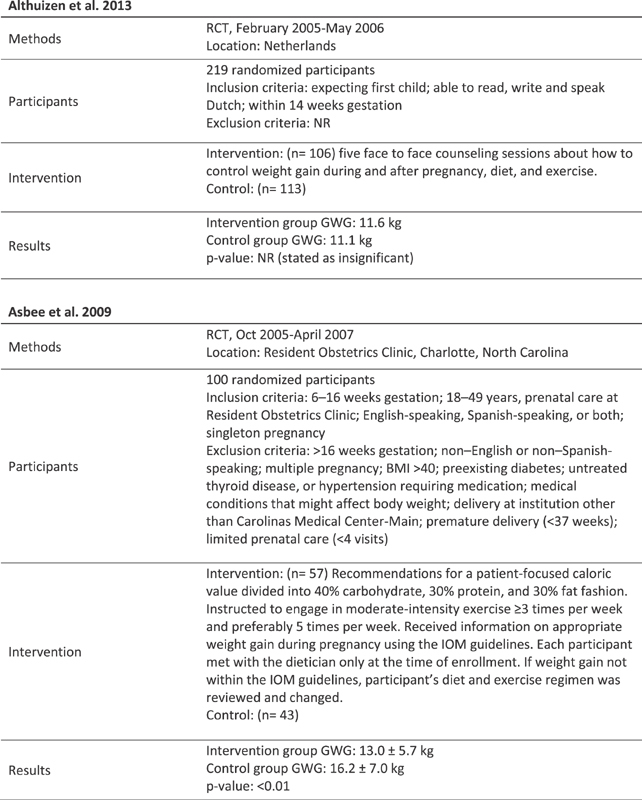
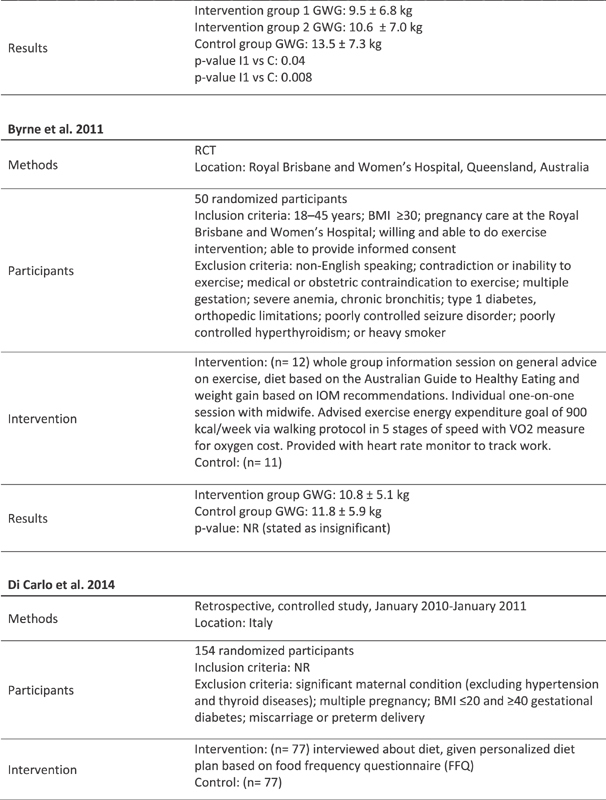
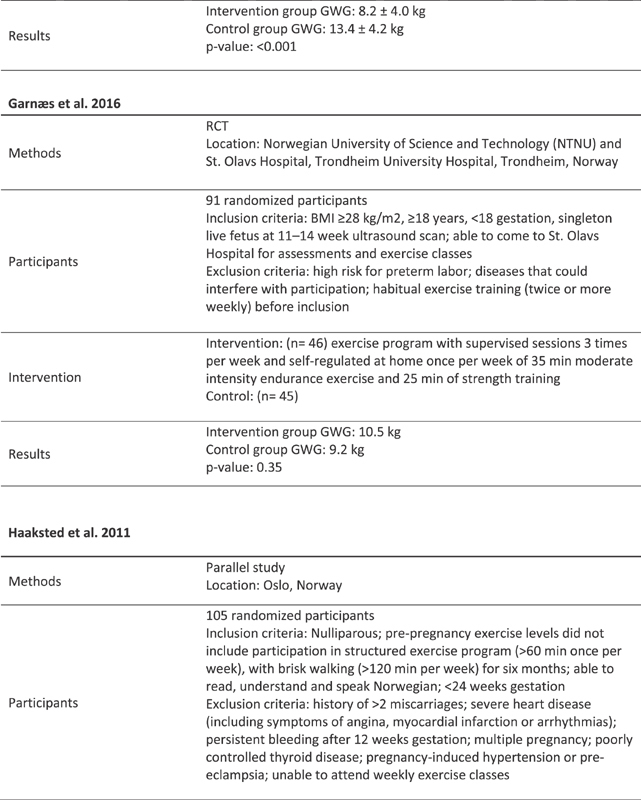
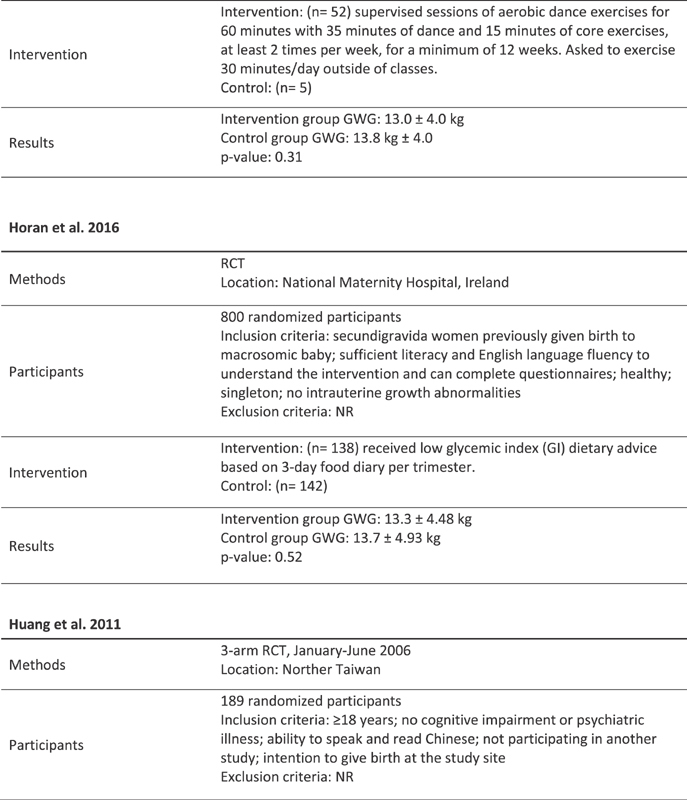
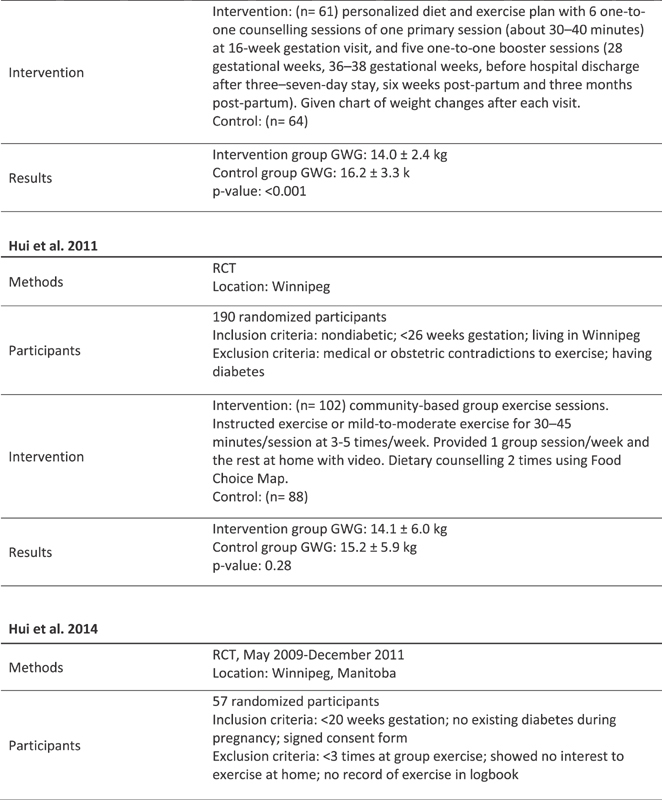
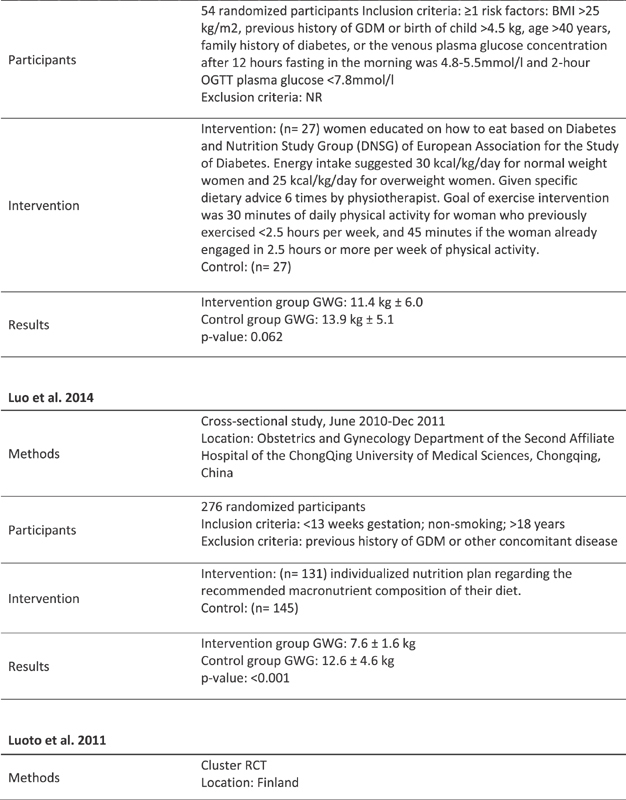
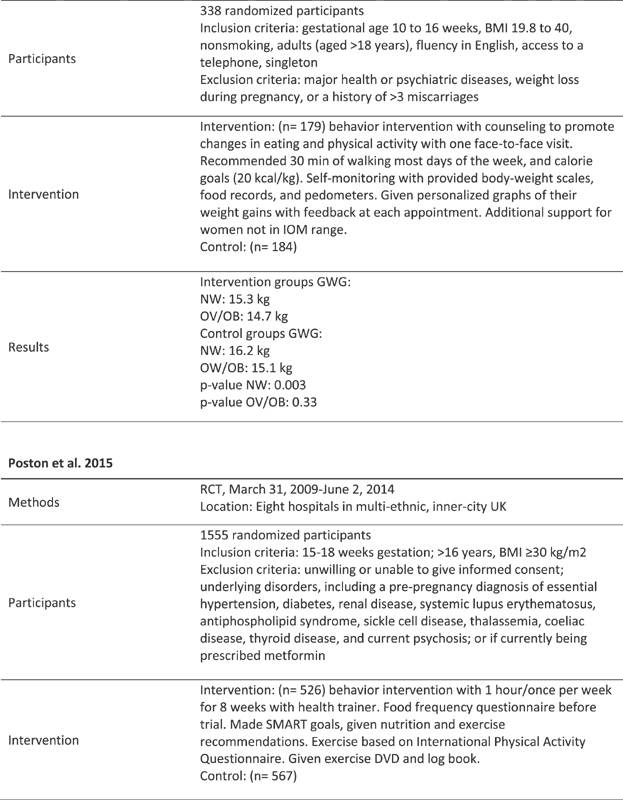
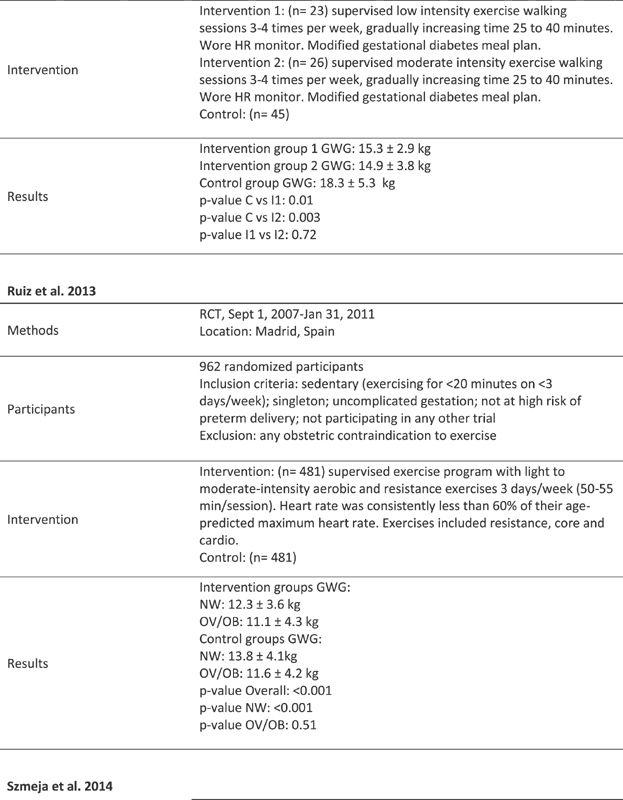
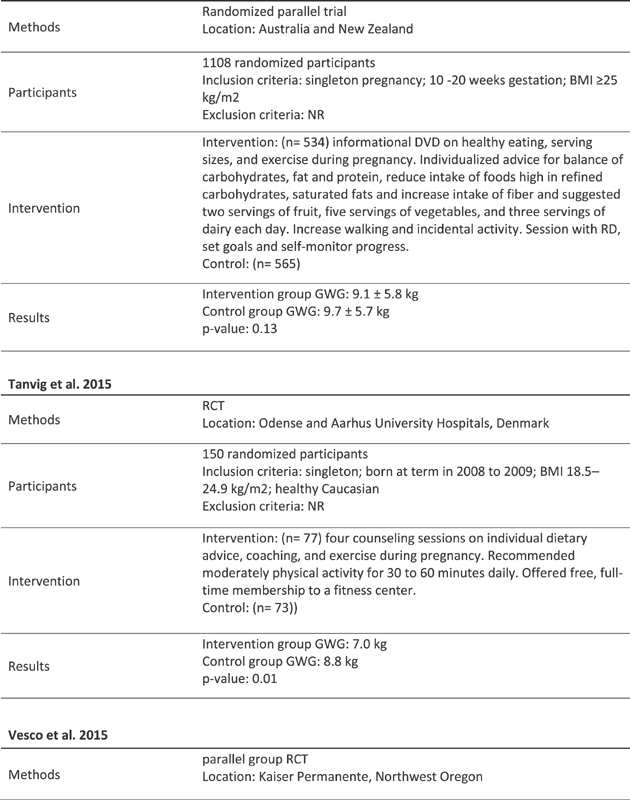
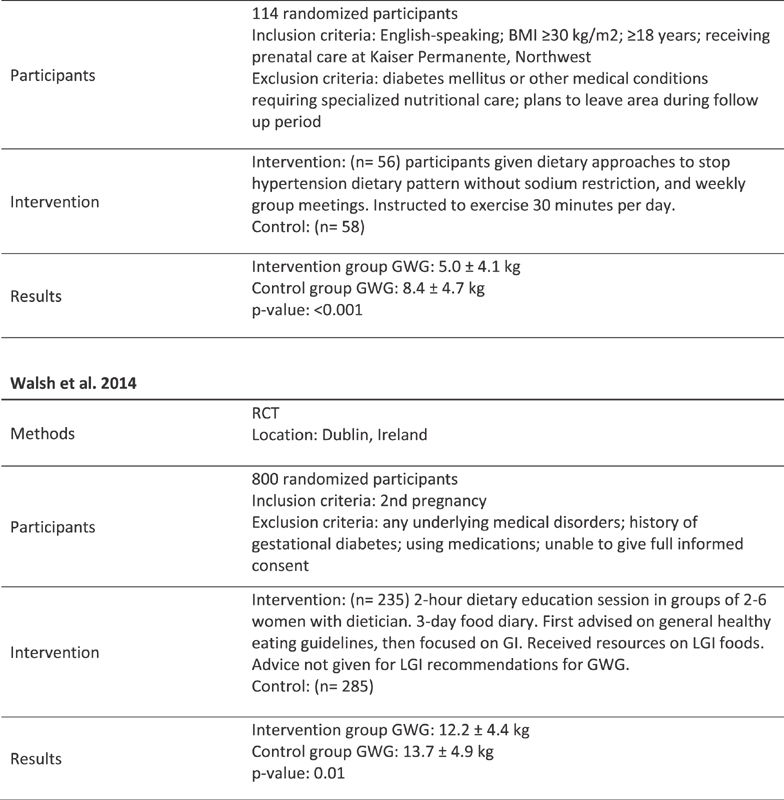
Fig. 2 provides an overview of the study design and characteristics of included studies.
Fig. 2.
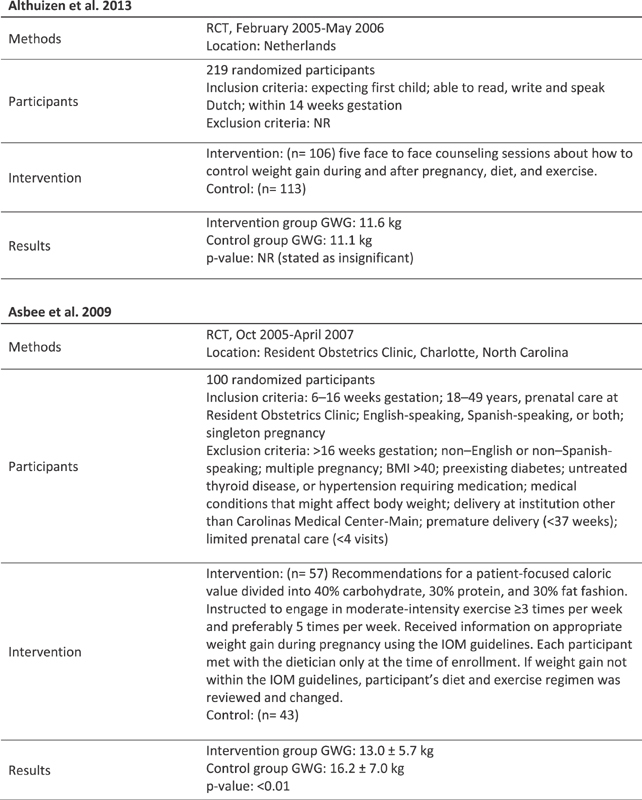
Characteristics of included studies.
Effects of Interventions
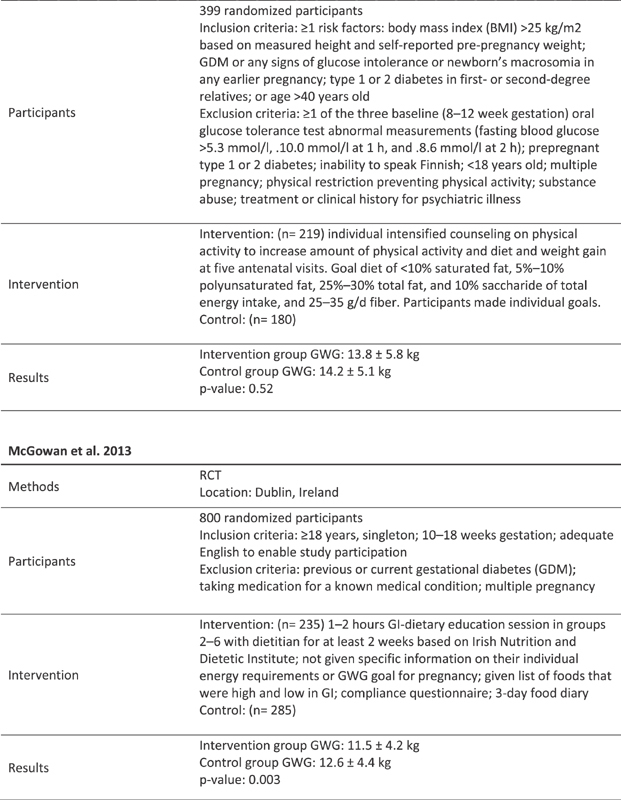
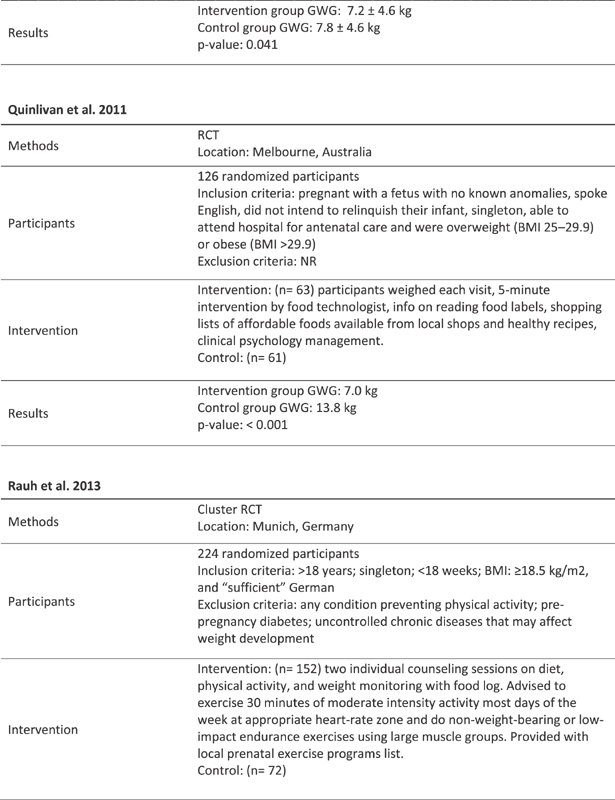
Among the total obstetric population studied, results of studies published after the 2009 IOM guidelines indicate that the nutrition-only intervention produced significant GWG differences between mean intervention and mean control groups ( p = 0.013). Nutrition-plus-exercise ( p = 0.056) and exercise-only ( p = 0.069) interventions trended toward statistical significance and show potential to control GWG ( Tables 1 and 2 ). ANOVA comparison of GWG between all intervention and control groups produced significant results ( p = 0.001) ( Table 1 ).
Table 1. Comparison of GWG (kg).
| Study or subgroup | Intervention | Control | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Nutrition | ||||
| Di Carlo et al (2014) | 8.2 | 4.0 | 13.4 | 4.2 |
| Horan et al (2016) | 13.3 | 4.5 | 13.7 | 4.9 |
| Luo et al (2014) | 7.6 | 1.6 | 12.6 | 4.6 |
| McGowan et al (2013) | 11.5 | 4.2 | 12.6 | 4.4 |
| Quinlivan et al (2011) | 7.0 | NR | 13.8 | NR |
| Walsh and McAuliffe (2015) | 12.2 | 4.4 | 13.7 | 4.9 |
| p -Value: 0.013 | ||||
| Nutrition plus exercise | ||||
| Althuizen et al (2013) | 11.1 | 3.2 | 11.6 | 4.6 |
| Asbee et al (2009) | 13.0 | 5.7 | 16.2 | 7.0 |
| Aşcı and Rathfisch (2016) | 12.5 | 5.0 | 12.3 | 4.8 |
| Bogaerts et al (2013) (1) | 9.5 | 6.8 | 13.5 | 7.3 |
| Bogaerts et al (2013) (2) | 10.6 | 7.0 | 13.5 | 7.3 |
| Huang et al (2011) | 14.0 | 2.4 | 16.2 | 3.3 |
| Hui et al (2012) | 14.1 | 6.0 | 15.2 | 5.9 |
| Hui et al (2014) | 12.9 | 3.7 | 16.2 | 4.4 |
| Korpi-Hyövälti et al (2011) | 11.4 | 6.0 | 13.9 | 5.1 |
| Luoto et al (2011) | 13.8 | 5.8 | 14.2 | 5.1 |
| Mustila et al (2012) | 13.6 | 5.1 | 14.1 | 4.5 |
| Petrella et al (2014) | 8.8 | 6.5 | 10.4 | 5.0 |
| Phelan et al (2011) (NW) | 15.3 | 4.4 | 16.2 | 4.6 |
| Phelan et al (2011) (OV/OB) | 14.7 | 6.9 | 15.1 | 7.5 |
| Poston et al (2015) | 7.2 | 4.6 | 7.8 | 4.6 |
| Rauh et al (2013) | 14.1 | 4.1 | 15.6 | 5.8 |
| Renault et al (2014) | 8.6 | NR | 10.9 | NR |
| Ruchat et al (2012) (LI) | 15.3 | 2.9 | 18.3 | 5.3 |
| Ruchat et al (2012) (MI) | 14.9 | 3.8 | 18.3 | 5.3 |
| Szmeja et al (2014) | 9.1 | 5.8 | 9.7 | 5.7 |
| Tanvig et al (2015) | 7.0 | NR | 8.8 | NR |
| Vesco et al (2014) | 5.0 | 4.1 | 8.4 | 4.7 |
| p -Value: 0.056 | ||||
| Exercise | ||||
| Byrne et al (2011) | 10.8 | 5.1 | 11.8 | 5.9 |
| Garnæs et al (2016) | 10.5 | NR | 9.2 | NR |
| Haakstad and Bø (2011) | 13.0 | 4.0 | 13.8 | 4.0 |
| Kong et al (2014) (OV) | 10.5 | 5.4 | 9.9 | 6.1 |
| Kong et al (2014) (OB) | 12.1 | 9.0 | 12.5 | 8.5 |
| Nascimento et al (2011) | 10.3 | 1.7 | 16.4 | 3.9 |
| Nascimento et al (2011) (OV) | 10.0 | 1.7 | 16.4 | 3.9 |
| Nascimento et al (2011) (OB) | 10.4 | 5.6 | 10.9 | 7.6 |
| Renault et al (2014) | 9.4 | NR | 10.9 | NR |
| Ruiz et al (2013) (NW) | 12.3 | 3.6 | 13.8 | 4.1 |
| Ruiz et al (2013) (OV/OB) | 11.1 | 4.3 | 11.6 | 4.2 |
| p -Value: 0.069 | ||||
| Supervised exercise | ||||
| Garnæs et al (2016) | 10.5 | 10.5 | 9.2 | NR |
| Haakstad and Bø (2011) | 13.0 | 4.0 | 13.8 | 4.0 |
| Nascimento et al (2011) | 10.3 | 1.7 | 16.4 | 3.9 |
| Nascimento et al (2011) (OV) | 10.0 | 1.7 | 16.4 | 3.9 |
| Nascimento et al (2011) (OB) | 10.4 | 5.6 | 10.9 | 7.6 |
| Ruiz et al (2013) (NW) | 12.3 | 3.6 | 13.8 | 4.1 |
| Ruiz et al (2013) (OV/OB) | 11.1 | 4.3 | 11.6 | 4.2 |
| p -Value: 0.61 | ||||
| Unsupervised exercise | ||||
| Byrne et al (2011) | 10.8 | 5.1 | 11.8 | 5.9 |
| Kong et al (2014) (OV) | 10.5 | 5.4 | 9.9 | 6.1 |
| Kong et al (2014) (OB) | 12.1 | 9.0 | 12.5 | 8.5 |
| Renault et al (2014) | 9.4 | NR | 10.9 | NR |
| p -Value: 0.494 | ||||
| Total p -value: 0.0014 | ||||
Abbreviations: GWG, gestational weight gain; LI, low intensity; MI, moderate intensity; NR not reported; NW, normal weight; OB, obesity; OV, overweight; SD, standard deviation.
Table 2. Comparison of GWG (kg) for studies that selected participants who are OV or have OB based on mean pre-pregnancy BMI.
| Study or subgroup | Intervention | Control | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Nutrition | ||||
| Di Carlo et al (2014) | 8.2 | 4.0 | 13.4 | 4.2 |
| Quinlivan et al (2011) | 7.0 | NR | 13.8 | NR |
| p -Value: 0.011 | ||||
| Nutrition plus exercise | ||||
| Bogaerts et al (2013) (1) | 9.5 | 6.8 | 13.5 | 7.3 |
| Bogaerts et al (2013) (2) | 10.6 | 7.0 | 13.5 | 7.3 |
| Korpi-Hyövälti et al (2011) | 11.4 | 6.0 | 13.9 | 5.1 |
| Luoto et al (2011) | 13.8 | 5.8 | 14.2 | 5.1 |
| Petrella et al (2014) | 8.8 | 6.5 | 10.4 | 5.0 |
| Phelan et al (2011) (OV/OB) | 14.7 | 6.9 | 15.1 | 7.5 |
| Poston et al (2015) | 7.2 | 4.6 | 7.8 | 4.6 |
| Renault et al (2014) | 8.6 | NR | 10.9 | NR |
| Szmeja et al (2014) | 9.1 | 5.8 | 9.7 | 5.7 |
| Tanvig et al (2015) | 7.0 | NR | 8.8 | NR |
| Vesco et al (2014) | 5.0 | 4.1 | 8.4 | 4.7 |
| p -Value: 0.129 | ||||
| Exercise | ||||
| Byrne et al (2011) | 10.8 | 5.1 | 11.8 | 5.9 |
| Garnæs et al (2016) | 10.5 | NR | 9.2 | NR |
| Kong et al (2014) (OV) | 10.5 | 5.4 | 9.9 | 6.1 |
| Kong et al (2014) (OB) | 12.1 | 9.0 | 12.5 | 8.5 |
| Nascimento et al (2011) | 10.3 | 1.7 | 16.4 | 3.9 |
| Does not differentiate between OV and obese | ||||
| Renault et al (2014) | 9.4 | NR | 10.9 | NR |
| p -Value: 0.308 | ||||
| Supervised exercise | ||||
| Garnæs et al (2016) | 10.5 | NR | 9.2 | NR |
| Nascimento et al (2011) | 10.3 | 1.7 | 16.4 | 3.9 |
| p -Value: 0.575 | ||||
| Unsupervised exercise | ||||
| Byrne et al (2011) | 10.8 | 5.1 | 11.8 | 5.9 |
| Kong et al (2014) (OV) | 10.5 | 5.4 | 9.9 | 6.1 |
| Kong et al (2014) (OB) | 12.1 | 9.0 | 12.5 | 8.5 |
| Renault et al (2014) | 9.4 | NR | 10.9 | NR |
| p -Value: 0.494 | ||||
| Total p -value: 0.0055 | ||||
Abbreviations: BMI, body mass index; GWG, gestational weight gain; LI, low intensity; MI, moderate intensity; NR not reported; NW, normal weight; OB, obesity; OV, overweight; SD, standard deviation.
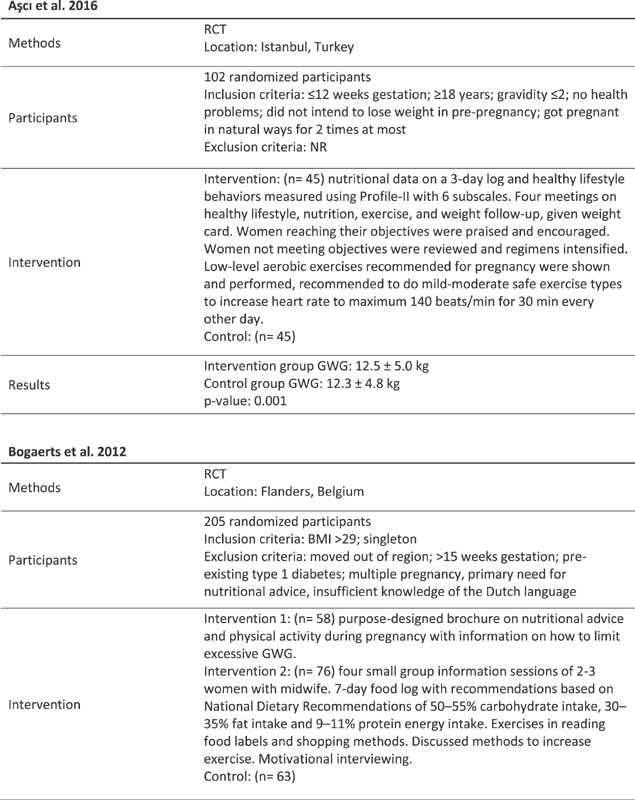
Graphically, there is a visually noticeable difference between mean control and mean intervention GWG for all intervention groups; however, nutrition ( p = 0.013) is the only statistically significant health system strategy ( Fig. 3 ). Exercise and nutrition plus exercise demonstrated some improvement; however, neither was statistically significant. When separated into supervised ( p = 0.61) and unsupervised ( p = 0.494) exercise programs, results were not significant.
Fig. 3.
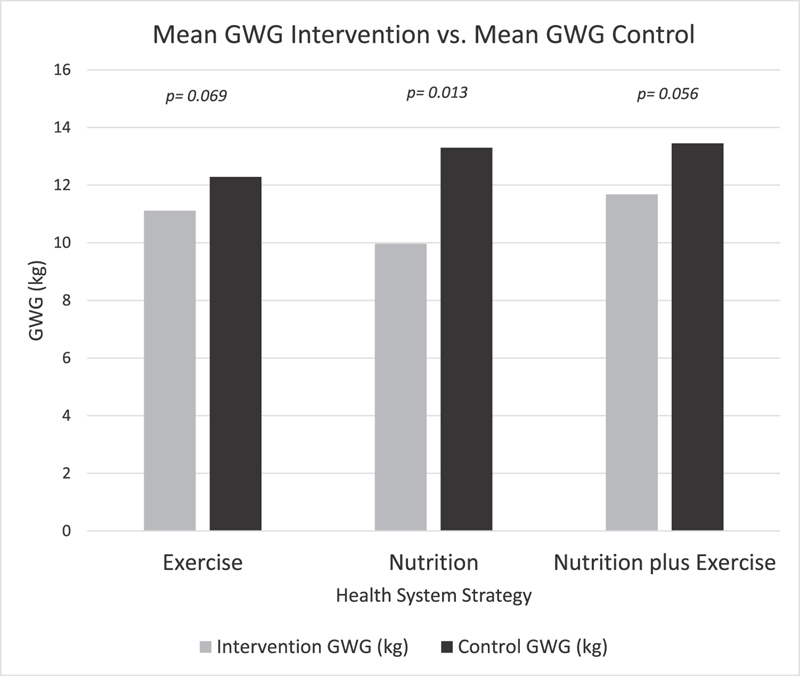
Mean gestational weight gain (GWG) (kg) of health system strategies intervention groups versus mean GWG control groups.
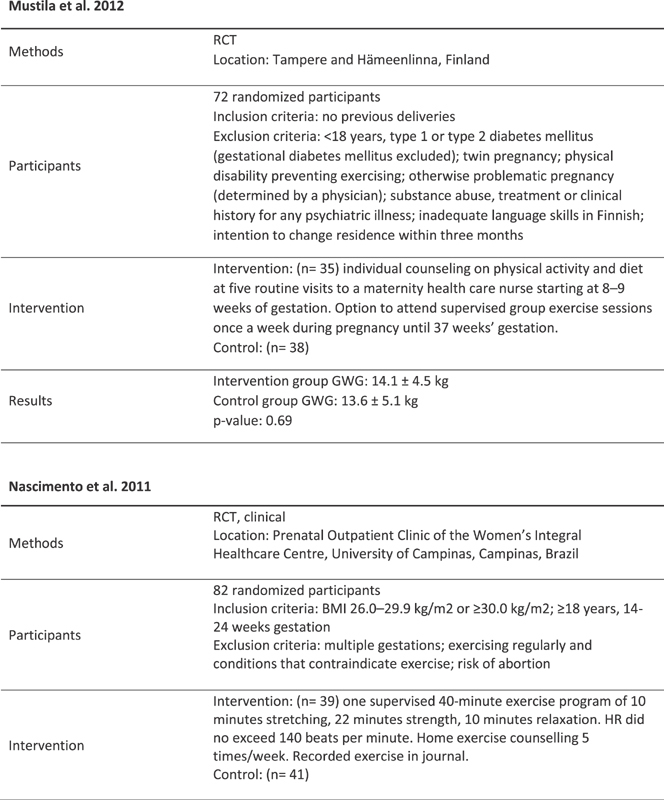
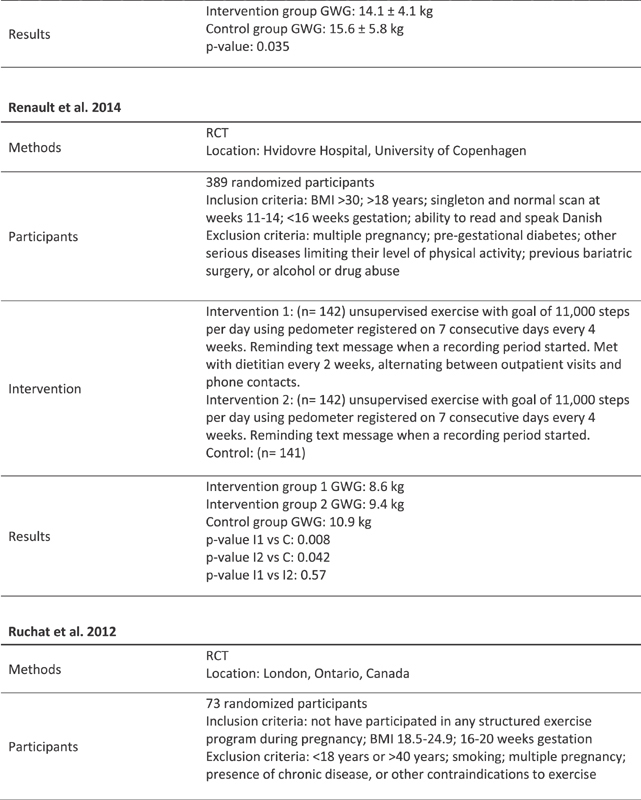
Table 3 depicts upper and lower 95% confidence intervals for each study based on population ( N ) and standard deviation (SD). Fig. 4 depicts the forest plot. Not all studies reported number of participants at, above, or below IOM recommendations, so odds ratio, risk ratio, nor weight could not be calculated.
Table 3. Comparison of mean intervention and control gestational weight gain (kg).
| Study or subgroup | Intervention | Control | p -Value | Mean difference | IV, random 95% CI | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | ||||
| Nutrition | |||||||||
| Di Carlo et al (2014) | 77 | 8.2 | 4.0 | 77 | 13.4 | 4.2 | <0.001 | −5.2 | −6.51, −3.89 |
| Horan et al (2016) | 138 | 13.3 | 4.5 | 142 | 13.7 | 4.9 | 0.52 | −0.4 | −1.51, 0.71 |
| Luo et al (2014) | 131 | 7.6 | 1.6 | 145 | 12.6 | 4.6 | <0.001 | −5.0 | −5.83, −4.17 |
| McGowan et al (2013) | 235 | 11.5 | 4.2 | 285 | 12.6 | 4.4 | 0.003 | −1.1 | −1.85, −0.35 |
| Quinlivan et al (2011) | 63 | 7.0 | NR | 61 | 13.8 | NR | <0.001 | −6.8 | NR |
| Walsh and McAuliffe (2015) | 235 | 12.2 | 4.4 | 285 | 13.7 | 4.9 | 0.01 | −1.5 | −2.31, −0.69 |
| Total events: 879 (intervention), 995 (standard care) | |||||||||
| Nutrition and exercise | |||||||||
| Althuizen et al (2013) | 106 | 11.1 | 3.2 | 113 | 11.6 | 4.6 | NR a | −0.5 | −1.56, 0.56 |
| Asbee et al (2009) | 57 | 13.0 | 5.7 | 43 | 16.2 | 7.0 | <0.01 | −3.2 | −5.72, −0.68 |
| Aşcı and Rathfisch (2016) | 45 | 12.5 | 5.0 | 45 | 12.3 | 4.8 | 0.001 | 0.2 | −1.85, 2.25 |
| Bogaerts et al (2013) (1) | 58 | 9.5 | 6.8 | 63 | 13.5 | 7.3 | 0.04 | −4.0 | −6.55, −1.45 |
| Bogaerts et al (2013) (2) | 76 | 10.6 | 7.0 | 63 | 13.5 | 7.3 | 0.008 | −2.9 | −5.30, −0.50 |
| Huang et al (2011) | 61 | 14.0 | 2.4 | 64 | 16.2 | 3.3 | <0.001 | −2.2 | −3.23, −1.17 |
| Hui et al (2012) | 102 | 14.1 | 6.0 | 88 | 15.2 | 5.9 | 0.28 | −1.1 | −2.81, 0.61 |
| Hui et al (2014) | 30 | 12.9 | 3.7 | 27.0 | 16.2 | 4.4 | <0.05 | −3.3 | −5.45, −1.15 |
| Korpi-Hyövälti et al (2011) | 27 | 11.4 | 6.0 | 27.0 | 13.9 | 5.1 | 0.062 | −2.5 | −5.54, 0.54 |
| Luoto et al (2011) | 219 | 13.8 | 5.8 | 180 | 14.2 | 5.1 | 0.52 | −0.4 | −1.49, 0.96 |
| Petrella et al (2014) | 33 | 8.8 | 6.5 | 30 | 10.4 | 5.0 | 0.032 | −1.6 | −4.54, 1.34 |
| Phelan et al (2011) (NW) | 92 | 15.3 | 4.4 | 94 | 16.2 | 4.6 | 0.003 | −0.9 | −2.20, 0.40 |
| Phelan et al (2011) (OV/OB) | 87 | 14.7 | 6.9 | 90 | 15.1 | 7.5 | 0.33 | −0.4 | −2.54, 1.74 |
| Poston et al (2015) | 526 | 7.2 | 4.6 | 567 | 7.8 | 4.6 | 0.041 | −0.6 | −1.15, −0.05 |
| Rauh et al (2013) | 152 | 14.1 | 4.1 | 72 | 15.6 | 5.8 | 0.035 | −1.5 | −2.83, −0.17 |
| Renault et al (2014) | 142 | 8.6 | NR | 141 | 10.9 | NR | 0.008 | −2.3 | NR |
| Ruchat et al (2012) (LI) | 23 | 15.3 | 2.9 | 45 | 18.3 | 5.3 | 0.01 | −3.0 | −5.37, −0.63 |
| Ruchat et al (2012) (MI) | 26 | 14.9 | 3.8 | 45 | 18.3 | 5.3 | 0.003 | −3.4 | −5.76, −1.04 |
| Szmeja et al (2014) | 543 | 9.1 | 5.8 | 565 | 9.7 | 5.7 | 0.13 | −0.6 | −1.28, 0.08 |
| Tanvig et al (2015) | 77 | 7.0 | NR | 73 | 8.8 | NR | 0.01 | −1.8 | NR |
| Vesco et al (2014) | 56 | 5.0 | 4.1 | 58 | 8.4 | 4.7 | <0.001 | −3.4 | −5.04, −1.76 |
| Total events: 2,538 (intervention), 2,493 (standard care) | |||||||||
| Exercise | |||||||||
| Byrne et al (2011) | 12 | 10.8 | 5.1 | 11 | 11.8 | 5.9 | NR a | −1.0 | −5.77, 3.77 |
| Garnæs et al (2016) | 46 | 10.5 | NR | 45 | 9.2 | NR | 0.35 | −1.3 | NR |
| Haakstad and Bø (2011) | 52 | 13.0 | 4.0 | 53 | 13.8 | 4.0 | 0.31 | −0.8 | −2.35, 0.75 |
| Kong et al (2014) (OV) | 9 | 10.5 | 5.4 | 9 | 9.9 | 6.1 | 0.859 | 0.6 | −5.16, 6.36 |
| Kong et al (2014) (OB) | 9 | 12.1 | 9.0 | 10 | 12.5 | 8.5 | 0.859 | −0.4 | −8.87, 8.07 |
| Nascimento et al (2011) | 39 | 10.3 | 1.7 | 41 | 16.4 | 3.9 | 0.543 | −6.1 | −7.45, −4.75 |
| Nascimento et al (2011) (OV) | 9 | 10.0 | 1.7 | 5 | 16.4 | 3.9 | 0.001 | −6.4 | −9.61, −3.19 |
| Nascimento et al (2011) (OB) | 30 | 10.4 | 5.6 | 36 | 10.9 | 7.6 | 0.757 | −0.5 | −3.84, 2.84 |
| Renault et al (2014) | 142 | 9.4 | NR | 141 | 10.9 | NR | 0.042 | −1.5 | NR |
| Ruiz et al (2013) (NW) | 335 | 12.3 | 3.6 | 352 | 13.8 | 4.1 | <0.001 | −1.5 | −2.08, −0.92 |
| Ruiz et al (2013) (OV/OB) | 146 | 11.1 | 4.3 | 129 | 11.6 | 4.2 | 0.51 | −0.5 | −1.51, 0.51 |
| Total events: 790 (intervention), 791 (standard care) | |||||||||
| Supervised exercise | |||||||||
| Garnæs et al (2016) | 46 | 10.5 | 10.5 | 45 | 9.2 | NR | 0.35 | 1.3 | NR |
| Haakstad and Bø (2011) | 52 | 13.0 | 4.0 | 53 | 13.8 | 4.0 | 0.31 | −0.8 | −2.35, 0.75 |
| Nascimento et al (2011) | 39 | 10.3 | 1.7 | 41 | 16.4 | 3.9 | 0.543 | −6.1 | −7.45, −4.75 |
| Nascimento et al (2011) (OV) | 9 | 10.0 | 1.7 | 5 | 16.4 | 3.9 | 0.001 | −6.4 | −9.61, −3.19 |
| Nascimento et al (2011) (OB) | 30 | 10.4 | 5.6 | 36 | 10.9 | 7.6 | 0.757 | −0.5 | −3.84, 2.84 |
| Ruiz et al (2013) (NW) | 335 | 12.3 | 3.6 | 352 | 13.8 | 4.1 | <0.001 | −1.5 | −2.08, −0.92 |
| Ruiz et al (2013) (OV/OB) | 146 | 11.1 | 4.3 | 129 | 11.6 | 4.2 | 0.51 | −0.5 | −1.51, 0.51 |
| Total events: 657 (intervention), 661 (standard care) | |||||||||
| Unsupervised exercise | |||||||||
| Byrne et al (2011) | 12 | 10.8 | 5.1 | 11 | 11.8 | 5.9 | NR a | −1.0 | −5.77, 3.77 |
| Kong et al (2014) (OV) | 9 | 10.5 | 5.4 | 9 | 9.9 | 6.1 | 0.859 | 0.6 | −5.16, 6.36 |
| Kong et al (2014) (OB) | 9 | 12.1 | 9.0 | 10 | 12.5 | 8.5 | 0.859 | −0.4 | −8.87, 8.07 |
| Renault et al (2014) | 142 | 9.4 | NR | 141 | 10.9 | NR | 0.042 | −1.5 | NR |
| Total events: 172 (intervention), 171 (standard care) | |||||||||
| Overall total events: 4 , 207 ( i ntervention), 4 , 279 ( standard care) | |||||||||
Abbreviations: CI, confidence interval; LI, low intensity; MI, moderate intensity; NR not reported; NW, normal weight; OB, obesity; OV, overweight; SD, standard deviation.
Stated as insignificant.
Fig. 4.
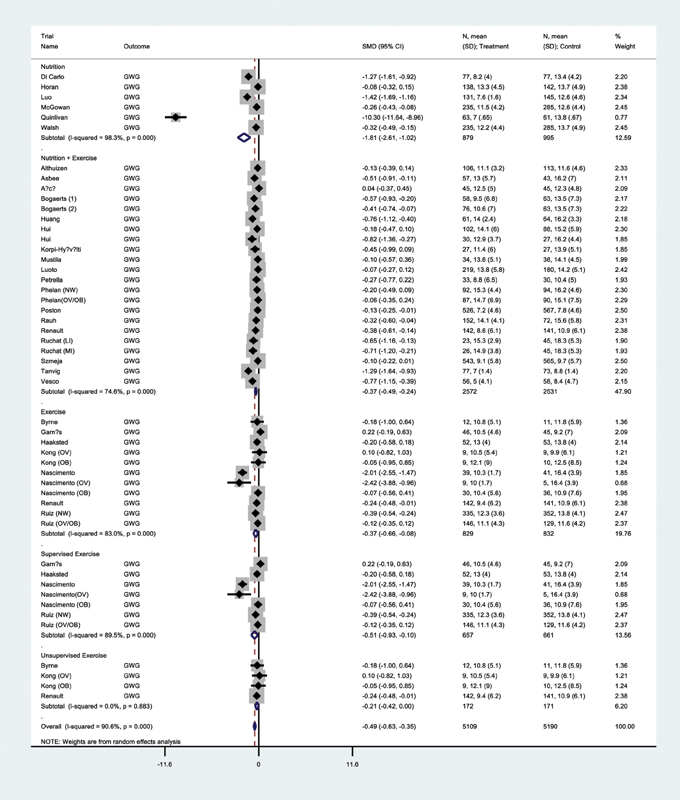
Forest plot divided by subgroups.
Eight studies categorized based on pre-pregnancy BMI and analyzed whether mean GWG, as adjusted for BMI, fell below, within, or above IOM recommendations. Three of 8 (37.5%) exercise-only, 3 of 6 (50%) nutrition-only, and 15 of 22 (68.18%) nutrition-plus-exercise interventions were within the IOM GWG recommendations. Compared with control groups within IOM, 3 of 8 (37.5%) exercise-only, 1 of 8 (12.5%) nutrition-only, and 6 of 22 (27.27%) nutrition-plus-exercise interventions produced GWG within IOM recommendation. For one of the nutrition-plus-exercise studies, the control GWG fell below the IOM recommendation. 37
Of the studies that reported percentage of participants exceeding IOM, 2 of 2 (100%) nutrition only, 9 of 13 (69.23%) nutrition plus exercise, and 4 of 6 (66.67%) exercise only reported that women in the intervention group exceeded the IOM recommendations less than control group. One exercise-only study on mothers with OB reported the same percentage exceeding IOM for intervention and control groups 59 ( Table 4 ).
Table 4. Per cent participants that exceed IOM recommendations.
| Study or subgroup | Intervention | Control |
|---|---|---|
| Nutrition | ||
| Di Carlo et al (2014) | NR | NR |
| Horan et al (2016) | NR | NR |
| Luo et al (2014) | NR | NR |
| McGowan et al (2013) | 33.2 | 44.7 |
| Quinlivan et al (2011) | NR | NR |
| Walsh and McAuliffe (2015) | 37.7 | 47.9 |
| Nutrition plus exercise | ||
| Althuizen et al (2013) | 70.4 | 72.4 |
| Asbee et al (2009) | 61.4 | 48.8 |
| Aşcı and Rathfisch (2016) | 51.1 | 28.9 |
| Bogaerts et al (2013) (1) | NR | NR |
| Bogaerts et al (2013) (2) | NR | NR |
| Huang et al (2011) | NR | NR |
| Hui et al (2012) | 35.2 | 54.5 |
| Hui et al (2014) | 10 | 37 |
| Korpi-Hyövälti et al (2011) | NR | NR |
| Luoto et al (2011) | NR | NR |
| Mustila et al (2012) | 35.5 | 27.0 |
| Petrella et al (2014) | 33.3 | 60.8 |
| Phelan et al (2011) (NW) | 40.2 | 52.1 |
| Phelan et al (2011) (OV/OB) | 66.7 | 61.1 |
| Poston et al (2015) | NR | NR |
| Rauh et al (2013) | 38.2 | 59.5 |
| Renault et al (2014) | NR | NR |
| Ruchat et al (2012) (LI) | 35 | 53 |
| Ruchat et al (2012) (MI) | 31 | 53 |
| Szmeja et al (2014) | NR | NR |
| Tanvig et al (2015) | NR | NR |
| Vesco et al (2014) | 44 | 82 |
| Exercise | ||
| Byrne et al (2011) | NR | NR |
| Garnæs et al (2016) | 58.3 | 44.4 |
| Haakstad and Bø (2011) | 33 | 38 |
| Kong et al (2014) (OV) | 44.4 | 50 |
| Kong et al (2014) (OB) | 77.8 | 77.8 |
| Nascimento et al (2011) | 47 | 57 |
| Nascimento et al (2011) (OV) | NR | NR |
| Nascimento et al (2011) (OB) | NR | NR |
| Renault et al (2014) | NR | NR |
| Ruiz et al (2013) (NW) | 23.8 | 32 |
| Ruiz et al (2013) (OV/OB) | NR | NR |
| Supervised exercise | ||
| Garnæs et al (2016) | 58.3 | 44.4 |
| Haakstad and Bø (2011) | 33 | 38 |
| Nascimento et al (2011) | 47 | 57 |
| Nascimento el al (2011) (OV) | NR | NR |
| Nascimento et al (2011) (OB) | NR | NR |
| Ruiz et al (2013) (NW) | 23.8 | 32 |
| Ruiz et al (2013) (OV/OB) | NR | NR |
| Unsupervised exercise | ||
| Byrne et al (2011) | NR | NR |
| Kong et al (2014) (OV) | 44.4 | 50 |
| Kong et al (2014) (OB) | 77.8 | 77.8 |
| Renault et al (2014) | NR | NR |
Abbreviations: IOM, Institute of Medicine; LI, low intensity; MI, moderate intensity; NR not reported; NW, normal weight; OB, obesity; OV, overweight.
Participants Who Are Overweight and/or Have Obesity
Additional analysis was completed on studies that selected for participants who are OV or have OB ( Table 2 ). When examined individually, 2 of 2 nutrition only (100%), 7 of 10 nutrition plus exercise (70%), and 1 of 6 exercise only produced significant results (16.67%). One of two supervised and one of four unsupervised exercise produced significant results. Like the overall analyses, nutrition-only strategy was significant ( p = 0.011). Overall, comparison between all interventions and controls was significant ( p = 0.004) in this population.
Exercise Interventions
Three studies reported statistically significant differences in mean GWG 51 60 61 ( Table 3 ). Five of eight studies subjects selected for pre-pregnancy BMI as obese or OV. 51 56 57 59 60 These studies produced GWG greater than IOM recommendation for both control and intervention groups, except when Kong et al (2014) was divided into participants with OV and OB; OV individuals had mean GWG within IOM recommendations. Three studies did not have BMI specifications and were classified as NW with GWG within IOM. 52 58 61
Studies were then divided into subgroups where exercise was either supervised or unsupervised. To be a supervised intervention, exercise must be performed under the supervision of a personal trainer or by attendance at an exercise class. Neither supervised ( p = 0.61) nor unsupervised ( p = 0.494) programs produced significant results. However, mean GWG for unsupervised intervention (10.7 kg) and control (11.275 kg) groups was lower than supervised (11.44 kg) intervention and control (12.96 kg) groups.
Nutrition Interventions
Five of six studies reported statistically significant differences in mean GWG 31 33 34 35 36 52 ( Table 3 ). Two studies selected subjects with OV or obese pre-pregnancy BMI. 31 35 The results of three studies demonstrated that the intervention group's average GWG was within IOM and the average GWG of control group exceed IOM. 31 34 35 All control groups' GWG exceeded IOM, except one that was within IOM recommendations. 34 One intervention group's GWG was below IOM recommendations. 33
Combination of Exercise-Plus-Nutrition Interventions
Thirteen of 19 studies reported statistically significant differences in mean GWG 38 39 40 41 43 47 49 50 51 52 54 55 ( Table 3 ). Three underwent multiple analyses. When divided into subgroups, interventions 1 and 2, 40 NW participants 48 and both LI and MI exercise programs were significant. 52 Ten studies selected participants with OV or obese pre-pregnancy BMI. 40 44 45 47 48 49 51 53 54 55 Of these studies, six interventions and three control groups were within IOM recommendations. All NW subjects produced GWG within the IOM recommendations for the intervention group. 37 39 41 42 43 46 48 50
Discussion
Based on results of this meta-analysis, nutrition-only interventions were associated with statistically significant lower rates of excessive GWG and therefore have the highest probability of helping women achieve target IOM GWG guidelines ( p = 0.013). Exercise-only ( p = 0.069) and nutrition-plus-exercise ( p = 0.056) interventions have potential to control GWG, but results did not reach statistical significance in the current study. In comparison to the Cochrane Review findings of studies published before the 2009 IOM guidelines which found all three intervention groups reduced GWG, the current meta-analysis study found that studies which utilized the 2009 IOM guidelines were more likely to produced reduced GWG with nutrition-only interventions. Nonsignificant findings from exercise and nutrition-plus-exercise health system strategies may be due to the inclusion of different exercise types. Exercise programs varied. Some included advice about exercise or discussed increased amount of physical activity, while others were more interventional, such as supervised dance programs or recommending a certain number of steps per day. The way in which these steps were achieved may and most likely differed between participants. Despite different nutritional advice, interventions universally recommend increased amounts of fruits and vegetables, and decreased consumption of food with high fat and sugar content. Additionally, retention to exercise programs may be more difficult than nutrition programs because one must eat to live, but exercise is not a fundamental need.
Previous studies have addressed the ability to control GWG and prevent weight exceeding IOM recommendations with mixed results. Since the study search for this article was completed, additional studies have been published with inconsistent results. Nutrition-only studies of the general population and of women who are OV/OB concur that nutrition-only interventions make significant differences for controlling GWG. 6 7 8 Walker et al's (2018) meta-analysis of general population concerning nutrition only, exercise only, and nutrition plus exercise claimed nutrition-only interventions are the best method to control GWG. Lamminpää et al's (2017) meta-analysis of OV/OB women only analyzed nutrition-only interventions because of previous reporting this as the best method. This meta-analysis found that nutrition-only results vary because of adherence inconsistency. Exercise-only interventions produced significant results for both general population 10 17 27 28 29 and OV/OB except for one study. 10 Nutrition-plus-exercise interventions for general population were statistically significant. 14 15 16 17 18 19 20 21 Nutrition plus exercise for OV/OB were inconsistent, including a meta-analysis determining nutrition plus exercise as insignificant impact on GWG. 20 Due to the variability of these findings, it is challenging to make a consensus regarding which intervention is best for clinical use. The results of this study confer with other studies that nutrition-only interventions are the best method to control GWG.
Limitations
Limitations include the inability to calculate risk ratio and weight. Based on heterogeneity of p -value greater than 0.10, 22 studies were determined to have excessive heterogeneity. Heterogeneity between subgroups was not significant; therefore, data were pooled between subgroups. Search did not explore worldwide databases such as EMBASE and LiLACS; therefore, some foreign studies may have been missed that would have otherwise met the inclusion criteria. Meta-analyses are generally limited due to selection bias and publication bias. No publication bias was detected.
Future Research
Evidence suggests that nutrition-only, exercise-only, and nutrition-plus-exercise interventions help control excessive GWG during pregnancy. Since the nutrition-only group was the only health system strategy to produce statistically significant results, this type of intervention should be favored as first line. Based on analysis, pre-pregnancy BMI is a better predictor of GWG than the type of intervention program studied. Pregnant individuals with a starting BMI categorized as OV or obese are more likely to exceed IOM recommendations regardless of intervention. Further research is needed on participants that are OV or have OB. Interventions on participants from middle-income or low-income countries should be analyzed because impact of interventions may differ based on several factors.
Conclusion
We found that nutrition-only interventions were more effective at decreasing rates of excessive GWG than exercise or nutrition-plus-exercise interventions. Time and resources are limited for all clinicians and clinics. Therefore, clinicians and clinical programs should focus efforts on nutrition education with health messages targeting increased consumption of fruits and vegetables and decreased consumption of foods with high fat or sugar content to maximize effectiveness. If additional resources are available, efforts may also be focused on exercise since such efforts are not harmful, but these efforts may be of lower yield.
Funding Statement
Funding This meta-analysis was not funded.
Conflict of Interest The authors of this study declare no conflict of interest.
One-way ANOVA. 2010. Vassarstars.net. [accessed October 9, 2016, to June 30, 2017]. http://vassarstats.net/anova1u.html
References
- 1.Ogden C L, Carroll M D, Fryar C D, Flegal K M. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015;219(219):1–8. [PubMed] [Google Scholar]
- 2.Stang J, Huffman L G. Position of the academy of nutrition and dietetics: obesity, reproduction, and pregnancy outcomes. J Acad Nutr Diet. 2016;116(04):677–691. doi: 10.1016/j.jand.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Oken E, Taveras E M, Kleinman K P, Rich-Edwards J W, Gillman M W. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol. 2007;196(04):3220–3.22E10. doi: 10.1016/j.ajog.2006.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rasmussen K M, Catalano P M, Yaktine A L. New guidelines for weight gain during pregnancy: what obstetrician/gynecologists should know. Curr Opin Obstet Gynecol. 2009;21(06):521–526. doi: 10.1097/GCO.0b013e328332d24e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gardner B, Wardle J, Poston L, Croker H. Changing diet and physical activity to reduce gestational weight gain: a meta-analysis. Obes Rev. 2011;12(07):e602–e620. doi: 10.1111/j.1467-789X.2011.00884.x. [DOI] [PubMed] [Google Scholar]
- 6.Koutelidakis A E, Alexatou O, Kousaiti S et al. Higher adherence to Mediterranean diet prior to pregnancy is associated with decreased risk for deviation from the maternal recommended gestational weight gain. Int J Food Sci Nutr. 2018;69(01):84–92. doi: 10.1080/09637486.2017.1330403. [DOI] [PubMed] [Google Scholar]
- 7.Walker R, Bennett C, Blumfield M et al. Attenuating pregnancy weight gain-what works and why: a systematic review and meta-analysis. Nutrients. 2018;10(07):944. doi: 10.3390/nu10070944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abdel-Aziz S B, Hegazy I S, Mohamed D A, Abu El Kasem M MA, Hagag S S. Effect of dietary counseling on preventing excessive weight gain during pregnancy. Public Health. 2018;154:172–181. doi: 10.1016/j.puhe.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 9.Quinlivan J A, Julania S, Lam L. Antenatal dietary interventions in obese pregnant women to restrict gestational weight gain to Institute of Medicine recommendations: a meta-analysis. Obstet Gynecol. 2011;118(06):1395–1401. doi: 10.1097/AOG.0b013e3182396bc6. [DOI] [PubMed] [Google Scholar]
- 10.Shieh C, Cullen D L, Pike C, Pressler S J. Intervention strategies for preventing excessive gestational weight gain: systematic review and meta-analysis. Obes Rev. 2018;19(08):1093–1109. doi: 10.1111/obr.12691. [DOI] [PubMed] [Google Scholar]
- 11.Robertson N, Ladlow B. Effect of individual dietetic intervention on gestational weight gain and associated complications in obese pregnant women. Aust N Z J Obstet Gynaecol. 2018;58(03):274–277. doi: 10.1111/ajo.12711. [DOI] [PubMed] [Google Scholar]
- 12.Dorise B, Byth K, McGee T, Wood A, Blumenthal C. A low intensity dietary intervention for reducing excessive gestational weight gain in an overweight and obese pregnant cohort. Eat Weight Disord. 2018;••• doi: 10.1007/s40519-018-0566-2. [DOI] [PubMed] [Google Scholar]
- 13.Streuling I, Beyerlein A, Rosenfeld E, Hofmann H, Schulz T, von Kries R. Physical activity and gestational weight gain: a meta-analysis of intervention trials. BJOG. 2011;118(03):278–284. doi: 10.1111/j.1471-0528.2010.02801.x. [DOI] [PubMed] [Google Scholar]
- 14.Shepherd E, Gomersall J C, Tieu J, Han S, Crowther C A, Middleton P. Combined diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2017;11:CD010443. doi: 10.1002/14651858.CD010443.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Y Q, Liu Y, Hua Y, Chen X L. Effect of diet and exercise intervention in Chinese pregnant women on gestational weight gain and perinatal outcomes: a quasi-experimental study. Appl Nurs Res. 2017;36:50–56. doi: 10.1016/j.apnr.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 16.Broekhuizen K, Simmons D, Devlieger R et al. Cost-effectiveness of healthy eating and/or physical activity promotion in pregnant women at increased risk of gestational diabetes mellitus: economic evaluation alongside the DALI study, a European multicenter randomized controlled trial. Int J Behav Nutr Phys Act. 2018;15(01):23. doi: 10.1186/s12966-018-0643-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nobles C, Marcus B H, Stanek E J, III et al. The effect of an exercise intervention on gestational weight gain: the Behaviors Affecting Baby and You (B.A.B.Y.) study: a randomized controlled trial. Am J Health Promot. 2018;32(03):736–744. doi: 10.1177/0890117117732409. [DOI] [PubMed] [Google Scholar]
- 18.Chan R S, Tam W H, Ho I C et al. Randomized trial examining effectiveness of lifestyle intervention in reducing gestational diabetes in high risk Chinese pregnant women in Hong Kong. Sci Rep. 2018;8(01):13849. doi: 10.1038/s41598-018-32285-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morison P N, Bacardi-Gascon M, Lopez-Corrales M, Jimenez-Cruz A. Combined dietary-exercise intervention for gestational weight gain and birthweight: a meta-analysis. Asia Pac J Clin Nutr. 2018;27(04):860–868. doi: 10.6133/apjcn.112017.02. [DOI] [PubMed] [Google Scholar]
- 20.Rogozińska E, Marlin N, Betrán A P et al. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: meta-analysis of individual participant data from randomised trials. BMJ. 2017;358:j3119. doi: 10.1136/bmj.j3119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sagedal L R, Øverby N C, Bere E et al. Lifestyle intervention to limit gestational weight gain: the Norwegian Fit for Delivery randomised controlled trial. BJOG. 2017;124(01):97–109. doi: 10.1111/1471-0528.13862. [DOI] [PubMed] [Google Scholar]
- 22.Cahill A G, Haire-Joshu D, Cade W T et al. Weight control program and gestational weight gain in disadvantaged women with overweight or obesity: a randomized clinical trial. Obesity (Silver Spring) 2018;26(03):485–491. doi: 10.1002/oby.22070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yeo S, Walker J S, Caughey M C, Ferraro A M, Asafu-Adjei J K. What characteristics of nutrition and physical activity interventions are key to effectively reducing weight gain in obese or overweight pregnant women? A systematic review and meta-analysis. Obes Rev. 2017;18(04):385–399. doi: 10.1111/obr.12511. [DOI] [PubMed] [Google Scholar]
- 24.Van Horn L, Peaceman A, Kwasny M et al. Dietary approaches to stop hypertension diet and activity to limit gestational weight: maternal offspring metabolics family intervention trial, a technology enhanced randomized trial. Am J Prev Med. 2018;55(05):603–614. doi: 10.1016/j.amepre.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 25.Peaceman A M, Clifton R G, Phelan S et al. Lifestyle interventions limit gestational weight gain in women with overweight or obesity: LIFE-Moms prospective meta-analysis. Obesity (Silver Spring) 2018;26(09):1396–1404. doi: 10.1002/oby.22250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haby K, Berg M, Gyllensten H, Hanas R, Premberg Å. Mighty Mums - a lifestyle intervention at primary care level reduces gestational weight gain in women with obesity. BMC Obes. 2018;5(01):16. doi: 10.1186/s40608-018-0194-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Daly N, Farren M, McKeating A, OʼKelly R, Stapleton M, Turner M J. A medically supervised pregnancy exercise intervention in obese women: a randomized controlled trial. Obstet Gynecol. 2017;130(05):1001–1010. doi: 10.1097/AOG.0000000000002267. [DOI] [PubMed] [Google Scholar]
- 28.Wang C, Wei Y, Zhang X et al. A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Am J Obstet Gynecol. 2017;216(04):340–351. doi: 10.1016/j.ajog.2017.01.037. [DOI] [PubMed] [Google Scholar]
- 29.Du M C, Ouyang Y Q, Nie X F, Huang Y, Redding S R. Effects of physical exercise during pregnancy on maternal and infant outcomes in overweight and obese pregnant women: a meta-analysis. Birth. 2018;••• doi: 10.1111/birt.12396. [DOI] [PubMed] [Google Scholar]
- 30.Muktabhant B, Ta L, Lumbiganon P, Laopaiboon M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy (review) summary of the findings for the main comparison. Cochrane. Database Syst Rev. 2015;(06):CD007145. doi: 10.1002/14651858.CD007145.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Di Carlo C, Iannotti G, Sparice S et al. The role of a personalized dietary intervention in managing gestational weight gain: a prospective, controlled study in a low-risk antenatal population. Arch Gynecol Obstet. 2014;289(04):765–770. doi: 10.1007/s00404-013-3054-y. [DOI] [PubMed] [Google Scholar]
- 32.Horan M K, McGowan C A, Gibney E R, Byrne J, Donnelly J M, McAuliffe F M. Maternal nutrition and glycaemic index during pregnancy impacts on offspring adiposity at 6 months of age analysis from the ROLO randomised controlled trial. Nutrients. 2016;8(01):13–15. doi: 10.3390/nu8010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luo X-D, Dong X, Zhou J. Effects of nutritional management intervention on gestational weight gain and perinatal outcome. Saudi Med J. 2014;35(10):1267–1270. [PMC free article] [PubMed] [Google Scholar]
- 34.McGowan C A, Walsh J M, Byrne J, Curran S, McAuliffe F M. The influence of a low glycemic index dietary intervention on maternal dietary intake, glycemic index and gestational weight gain during pregnancy: a randomized controlled trial. Nutr J. 2013;12(01):140. doi: 10.1186/1475-2891-12-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Quinlivan J A, Lam L T, Fisher J. A randomised trial of a four-step multidisciplinary approach to the antenatal care of obese pregnant women. Aust N Z J Obstet Gynaecol. 2011;51(02):141–146. doi: 10.1111/j.1479-828X.2010.01268.x. [DOI] [PubMed] [Google Scholar]
- 36.Walsh J M, McAuliffe F M. Impact of maternal nutrition on pregnancy outcome--does it matter what pregnant women eat? Best Pract Res Clin Obstet Gynaecol. 2015;29(01):63–78. doi: 10.1016/j.bpobgyn.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 37.Althuizen E, van der Wijden C L, van Mechelen W, Seidell J C, van Poppel M NM. The effect of a counselling intervention on weight changes during and after pregnancy: a randomised trial. BJOG. 2013;120(01):92–99. doi: 10.1111/1471-0528.12014. [DOI] [PubMed] [Google Scholar]
- 38.Asbee S M, Jenkins T R, Butler J R, White J, Elliot M, Rutledge A.Preventing excessive weight gain during pregnancy through dietary and lifestyle counseling: a randomized controlled trial Obstet Gynecol 2009113(2 Pt 1):305–312. [DOI] [PubMed] [Google Scholar]
- 39.Aşcı Ö, Rathfisch G. Effect of lifestyle interventions of pregnant women on their dietary habits, lifestyle behaviors, and weight gain: a randomized controlled trial. J Health Popul Nutr. 2016;35:7. doi: 10.1186/s41043-016-0044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bogaerts A F, Devlieger R, Nuyts E, Witters I, Gyselaers W, Van den Bergh B RH. Effects of lifestyle intervention in obese pregnant women on gestational weight gain and mental health: a randomized controlled trial. Int J Obes. 2013;37(06):814–821. doi: 10.1038/ijo.2012.162. [DOI] [PubMed] [Google Scholar]
- 41.Huang T T, Yeh C Y, Tsai Y C. A diet and physical activity intervention for preventing weight retention among Taiwanese childbearing women: a randomised controlled trial. Midwifery. 2011;27(02):257–264. doi: 10.1016/j.midw.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 42.Hui A, Back L, Ludwig S et al. Lifestyle intervention on diet and exercise reduced excessive gestational weight gain in pregnant women under a randomised controlled trial. BJOG. 2012;119(01):70–77. doi: 10.1111/j.1471-0528.2011.03184.x. [DOI] [PubMed] [Google Scholar]
- 43.Hui A L, Back L, Ludwig S et al. Effects of lifestyle intervention on dietary intake, physical activity level, and gestational weight gain in pregnant women with different pre-pregnancy body mass index in a randomized control trial. BMC Pregnancy Childbirth. 2014;14:331. doi: 10.1186/1471-2393-14-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Korpi-Hyövälti E A, Laaksonen D E, Schwab U S et al. Feasibility of a lifestyle intervention in early pregnancy to prevent deterioration of glucose tolerance. BMC Public Health. 2011;11:179. doi: 10.1186/1471-2458-11-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Luoto R, Kinnunen T I, Aittasalo M et al. Primary prevention of gestational diabetes mellitus and large-for-gestational-age newborns by lifestyle counseling: a cluster-randomized controlled trial. PLoS Med. 2011;8(05):e1001036. doi: 10.1371/journal.pmed.1001036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mustila T, Raitanen J, Keskinen P, Saari A, Luoto R. Lifestyle counseling during pregnancy and offspring weight development until four years of age: follow-up study of a controlled trial. J Negat Results Biomed. 2012;11:11. doi: 10.1186/1477-5751-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Petrella E, Malavolti M, Bertarini V et al. Gestational weight gain in overweight and obese women enrolled in a healthy lifestyle and eating habits program. J Matern Fetal Neonatal Med. 2014;27(13):1348–1352. doi: 10.3109/14767058.2013.858318. [DOI] [PubMed] [Google Scholar]
- 48.Phelan S, Phipps M G, Abrams B, Darroch F, Schaffner A, Wing R R. Randomized trial of a behavioral intervention to prevent excessive gestational weight gain: the Fit for Delivery Study. Am J Clin Nutr. 2011;93(04):772–779. doi: 10.3945/ajcn.110.005306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Poston L, Bell R, Croker H et al. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 2015;3(10):767–777. doi: 10.1016/S2213-8587(15)00227-2. [DOI] [PubMed] [Google Scholar]
- 50.Rauh K, Gabriel E, Kerschbaum E et al. Safety and efficacy of a lifestyle intervention for pregnant women to prevent excessive maternal weight gain: a cluster-randomized controlled trial. BMC Pregnancy Childbirth. 2013;13:151. doi: 10.1186/1471-2393-13-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Renault K M, Nørgaard K, Nilas L et al. The Treatment of Obese Pregnant Women (TOP) study: a randomized controlled trial of the effect of physical activity intervention assessed by pedometer with or without dietary intervention in obese pregnant women. Am J Obstet Gynecol. 2014;210(02):1340–1.34E11. doi: 10.1016/j.ajog.2013.09.029. [DOI] [PubMed] [Google Scholar]
- 52.Ruchat S M, Davenport M H, Giroux I et al. Nutrition and exercise reduce excessive weight gain in normal-weight pregnant women. Med Sci Sports Exerc. 2012;44(08):1419–1426. doi: 10.1249/MSS.0b013e31825365f1. [DOI] [PubMed] [Google Scholar]
- 53.Szmeja M A, Cramp C, Grivell R M, Deussen A R, Yelland L N, Dodd J M. Use of a DVD to provide dietary and lifestyle information to pregnant women who are overweight or obese: a nested randomised trial. BMC Pregnancy Childbirth. 2014;14:409. doi: 10.1186/s12884-014-0409-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tanvig M, Vinter C A, Jørgensen J S et al. Effects of lifestyle intervention in pregnancy and anthropometrics at birth on offspring metabolic profile at 2.8 years: results from the Lifestyle in Pregnancy and Offspring (LiPO) study. J Clin Endocrinol Metab. 2015;100(01):175–183. doi: 10.1210/jc.2014-2675. [DOI] [PubMed] [Google Scholar]
- 55.Vesco K K, Karanja N, King J C et al. Efficacy of a group-based dietary intervention for limiting gestational weight gain among obese women: a randomized trial. Obesity (Silver Spring) 2014;22(09):1989–1996. doi: 10.1002/oby.20831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Byrne N M, Groves A M, McIntyre H D, Callaway L K; BAMBINO group.Changes in resting and walking energy expenditure and walking speed during pregnancy in obese women Am J Clin Nutr 20119403819–830. [DOI] [PubMed] [Google Scholar]
- 57.Garnæs K K, Mørkved S, Salvesen Ø, Moholdt T. Exercise training and weight gain in obese pregnant women: a randomized controlled trial (ETIP trial) PLoS Med. 2016;13(07):e1002079. doi: 10.1371/journal.pmed.1002079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Haakstad L A, Bø K. Effect of regular exercise on prevention of excessive weight gain in pregnancy: a randomised controlled trial. Eur J Contracept Reprod Health Care. 2011;16(02):116–125. doi: 10.3109/13625187.2011.560307. [DOI] [PubMed] [Google Scholar]
- 59.Kong K L, Campbell C G, Foster R C, Peterson A D, Lanningham-Foster L. A pilot walking program promotes moderate-intensity physical activity during pregnancy. Med Sci Sports Exerc. 2014;46(03):462–471. doi: 10.1249/MSS.0000000000000141. [DOI] [PubMed] [Google Scholar]
- 60.Nascimento S L, Surita F G, Parpinelli MÂ, Siani S, Pinto e Silva J L. The effect of an antenatal physical exercise programme on maternal/perinatal outcomes and quality of life in overweight and obese pregnant women: a randomised clinical trial. BJOG. 2011;118(12):1455–1463. doi: 10.1111/j.1471-0528.2011.03084.x. [DOI] [PubMed] [Google Scholar]
- 61.Ruiz J R, Perales M, Pelaez M, Lopez C, Lucia A, Barakat R. Supervised exercise-based intervention to prevent excessive gestational weight gain: a randomized controlled trial. Mayo Clin Proc. 2013;88(12):1388–1397. doi: 10.1016/j.mayocp.2013.07.020. [DOI] [PubMed] [Google Scholar]


