Abstract
This extensive review summarizes clinical evidence on immunotherapy and targeted therapy currently available for endometrial cancer (EC) and reports the results of the clinical trials and ongoing studies. The research was carried out collecting preclinical and clinical findings using keywords such as immune environment, tumor infiltrating lymphocytes, programmed death-1 (PD-1)/programmed death-ligand 1 (PD-L1) expression, immune checkpoint inhibitors, anti-PD-1/PD-L1 antibodies and others' on PubMed. Finally, we looked for the ongoing immunotherapy trials on ClinicalTrials.gov. EC is the fourth most common malignancy in women in developed countries. Despite medical and surgical treatments, survival has not improved in the last decade and death rates have increased for uterine cancer in women. Therefore, identification of clinically significant prognostic risk factors and formulation of new rational therapeutic regimens have great significance for enhancing the survival rate and improving the outcome in patients with advanced or metastatic disease. The identification of genetic alterations, including somatic mutations and microsatellite instability, and the definition of intracellular signaling pathways alterations that have a major role in in tumorigenesis is leading to the development of new therapeutic options for immunotherapy and targeted therapy.
Keywords: Endometrial Cancer, Immunotherapy, Biological Therapy, Molecular Targeted Therapy
INTRODUCTION
Endometrial cancer (EC) is the fourth most common malignancy in women and the most common gynecologic cancer in developed countries, with an overall incidence of 7% and 63,230 estimated new cases in the United States in 2018 [1]. The most important risk factors are all related to an unbalanced increase of circulating estrogen as early menarche, late menopause, obesity, exposure to tamoxifen and nulliparity [2]. Most ECs are sporadic but 2%–5% of cases are familial, featuring specific germline mutations in the mismatch repair genes [3]. As in other types of cancer, genetic evaluation has acquired an increasingly important role in EC. In recent years, the definition of different cluster of genetic mutations and polymorphisms, the study of intracellular signaling pathways alterations in tumorigenesis and of tumor microenvironment, as well as the identification of important molecules for the control of tumor growth have led to the development of a number of potential strategies for targeted treatment. In this review, we will describe the immunotherapeutic options currently available for EC and report the results of the clinical trials and ongoing studies on targeted therapy.
BIOLOGICAL AND GENETIC BACKGROUND
According to Bokhman's model [4], EC has classically been divided in two subgroups: Type I, which includes the most common endometrioid cancer (60%–70% of cases), with a grading between 1 and 2, with high expression of hormonal receptors; and Type II, including high grade endometrioid cancer and other histological types like serous or clear cell carcinoma, generally negative for hormone receptors and with a worse prognosis.
The most frequent mutations in Type I involve PTENPIK3/AKT/mammalian target of rapamycin (mTOR) pathway (PTEN being mutated in 52%–78% of lesions), followed by KRAS mutations (15%–43%), ARID1A and Β-catenin alterations. One third of Type I EC also feature microsatellite instability (MSI), while TP53 is mutated in most of subtype II tumors [5].
In 2013 The Cancer Genome Atlas (TCGA) Research Network [6] suggested an integrated genomic classification of EC:
• Polymerase-ε (POLE) ultramutated, characterized by hotspot mutations of a catalytic subunit of DNA polymerase epsilon involved in nuclear DNA replication and repair, identified in 10% of endometrioid subtype.
• Microsatellite instability hypermutated (MSI-H), with high mutation rate related to alteration of MLH1, MSH2, MSH6, PMS2 genes involved in the mismatch repair system, both in sporadic and hereditary EC.
• Copy-number low, with low mutation rates, which include most endometrioid tumors and are frequently associated with mutations in PTEN, CTNNB1, PIK3CA, ARID1A and KRAS. This subtype seems to have similar pathogenesis as colo-rectal tumors.
• Copy-number high, including serous tumors and 25% of high-grade endometrioid tumors, characterized by extensive copy number variation and low mutation rate, frequent mutation of TP53, low estrogen and progesterone receptor expression. This subgroup shares the same features as basal-like breast cancer and serous ovarian carcinoma.
This genomic characterization allowed a reclassification of EC and may have impact on prognosis and guide treatment decisions. Unfortunately, genome sequencing methods used for the TCGA study are unsuitable for wider clinical application.
More recently, clinically applicable methodologies, which are less complex and expensive, have been applied to identify the same molecular subgroups. These novel approaches are based on next-generation sequencing (NGS) methods and investigate key epitopes evaluable by relatively simple molecular methods, adding prognostic information and directly impacting clinical management [7,8].
IMMUNOTHERAPEUTIC OPTIONS
Physiologically, endometrial immune system has unique characteristics, as its role is double: on one hand it should protect from infections and sexually transmitted pathogens, but on the other hand it should allow implantation of an allogenic embryo. To accomplish these tasks, endometrial microenvironment is influenced by sex hormones through menstrual cycle.
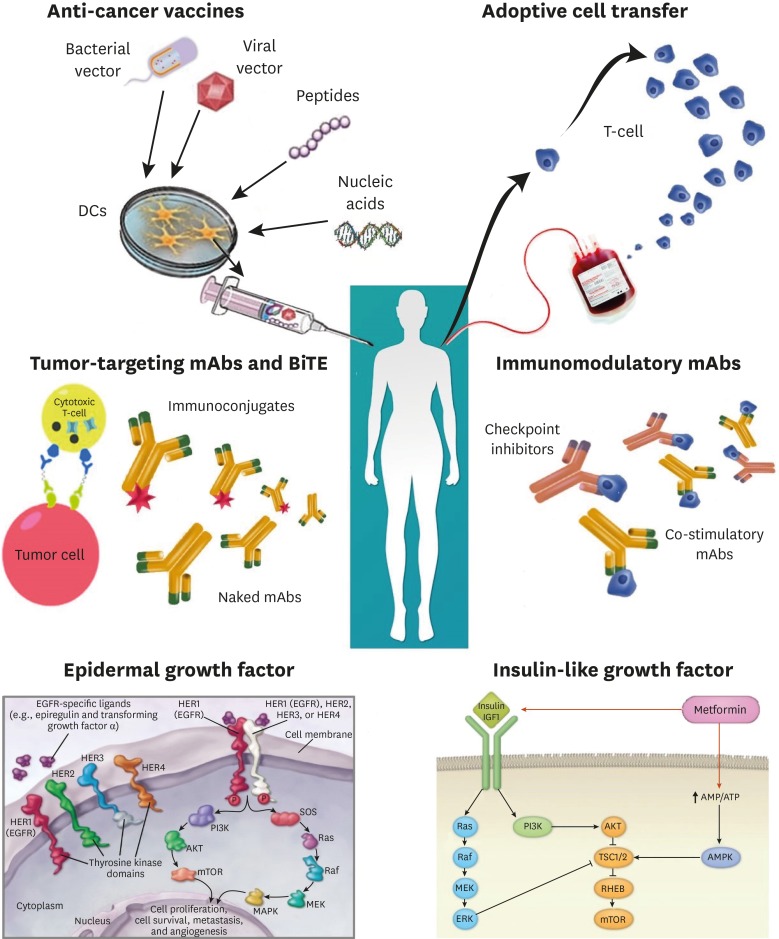
Immunotherapy basically consists in stimulating the endogenous immune response specifically against tumor cells and seems the new frontier of the anticancer treatment. Several compounds targeting different biological pathway are available. Some of these agents are already approved for treatment of non-gynecological malignancies like lung cancer and melanoma and could play a major role in treatment of EC as well. These therapies have been classified as active and passive therapy: the first consists in a stimulation of the host's own immune system against cancer cells, while the latter is based on administration of exogenously produced or manipulated immune system components promoting an anti-tumor immune response [9] (Fig. 1).
Fig. 1. Immunotherapeutic options available for treatment of EC.
BiTE, Bispecific T cell engager; DC, dendritic cell; EC, endometrial cancer; EGF, epidermal growth factor; EGFR, epidermal growth factor receptor; HER, human epidermal growth factor receptor; IGF, insulin-like growth factor; mAb, monoclonal antibody; mTOR, mammalian target of rapamycin; PI3K, phosphatidylinositol-3 kinase.
1. Anti-cancer vaccines
Therapeutic vaccination is considered a form of active immunotherapy that induce a cell-mediated immune response against tumor-associated antigens.
Peptide and protein-based vaccines contain manipulated tumor-associated antigens which are directly processed by dendritic cells to stimulate a CD8+ and CD4+ T cell mediated response. Whole cell vaccines include tumor cell-based and dendritic cell based: the first consist of inactivated tumor cells which induce a in vivo immune response, while the latter are made of dendritic cells which have been activated with tumor-associated antigens and can directly stimulate a cell-mediated immune response. Viral vector and nucleic acid-based vaccines have been found to trigger specific humoral and cellular immune responses [10].
As for EC, data concerning therapeutic vaccination are limited. Ohno et al. [11] evaluated the safety and tolerability of a Wilms' Tumor 1 (WT1) peptide vaccine in 12 patients with recurrent or progressive gynecologic cancers resistant to standard therapy in a phase II trial. Although the disease control rate in the initial 3 months was 25.0%, the only subject with uterine adenocarcinoma had disease progression after 3 months.
Coosemans et al. [12] studied six pre-treated patients with uterine cancer who received four weekly vaccines of autologous dendritic cells loaded with WT1 mRNA. Three out of four patients who were human leucocyte antigen (HLA)-A2-positive showed an oncological response after four injections, while two HLA-A2-negative patients had neither oncological nor immunological response.
Jäger et al. [13] analyzed serological and clinical responses of 36 patients with different tumors who received recombinant vaccinia NY-ESO-1 and a viral-based vaccine containing NY-ESO-1. The only patient affected by endometrial carcinoma showed immunological response after four vaccinations, but had clinical progression disease.
In a phase I trial, Kaumaya et al. [14] studied a dose escalating protocol with a combination vaccine of two chimeric, B-cell epitopes derived from the human epidermal growth factor receptor 2 (HER2) extracellular domain with a promiscuous T cell epitope in 24 oncological patients with metastatic disease. In the two patients affected by EC, one showed a clinical partial response.
2. Immune checkpoints blockade
In order to escape from the immune system, EC cells are able to stimulate immune checkpoints (inhibitory pathways that down-regulate T cells activation), activating negative feedback mechanisms and creating a locally immunosuppressed environment.
1) Targeting programmed death-ligand 1 (PD-L1)
EC cells have the ability to activate programmed death-1 (PD-1) signaling, by overexpressing PD-L1 and PDL-2, which can bind PD-1 receptors, expressed on tumor-infiltrating CD4 and CD8 T cells and inactivate them in the tumor microenvironment. EC cells overexpress PD-1 (present in 75% of cases) and PD-L1 (in 25%–100% of cases) the most among gynecological cancer. For this reason, targeting this pathway seems a promising strategy to enhance antitumor immune response [15].
Pembrolizumab, a humanized monoclonal antibody that targets PD-1, was proven clinically effective in tumors with mismatch-repair deficiency for the first time in a phase II study published in 2015 by Le et al. [16].
In 2017 results of KEYNOTE-028 (NCT02054806), a phase Ib trial investigating the effect of pembrolizumab in advanced EC patients, were published. In this study a small cohort of 24 patients with advanced or metastatic, PD-L1 positive EC progressing after standard therapy, was treated with intravenous pembrolizumab 10 mg/kg every 2 weeks up to 24 months or until disease progression or intolerable toxicity. Partial response was achieved in 3 patients and 1 of them had POLE mutations. Stable disease (SD) was achieved in 2 patients. Overall response rate (ORR) was 13%. Six-months progression-free survival (PFS) and overall survival (OS) rates reported were 19.0% and 68.8%, respectively. As for toxicity, only mild adverse effects, including fatigue, pruritus, pyrexia and anorexia, were observed in 54.2% of patients [17].
In a recent phase Ib/II trial [18], Pembrolizumab was used at the dosage of 200 mg intravenously every 3 weeks in combination with Lenvatinib, a multikinase-inhibitor with antiangiogenic activity, at the dosage of 20 mg/day orally, in 23 patients with metastatic EC in progression after conventional chemotherapy. An ORR of 48% was reported, while adverse effects were mild and manageable [18].
In 2016, Mehnert et al. [19] reported a case of a 53-years old woman with International Federation of Gynecology and Obstetrics (FIGO) high grade metastatic endometrioid type endometrial adenocarcinoma who was treated with pembrolizumab 10 mg/kg every 2 weeks with almost immediate clinical benefit and partial response after 8 weeks of treatment. Adverse effects were only mild grade and the therapy was well tolerated. Both the primary tumor and metastatic lymph nodes were tested for genomic profiling and both samples resulted POLE-mutated. In the TCGA data set [6], POLE-mutant cancers have higher expression of immune checkpoint-related proteins, including PD-L1 and PD-L2, CD8A, PD-1, and cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4). These results suggest that this subset of tumors may be particularly responsive to immunotherapy.
Similarly, anti-PD-1 monoclonal antibody Nivolumab was reported effective in two cases of recurrent POLE ultra-mutated and MSH6 hyper-mutated endometrial carcinoma refractory to conventional surgical and chemotherapeutic treatments [20]. In these patients Nivolumab was administrated in monotherapy intravenously at the dosage of 3 mg/kg biweekly, and a significant clinical response was observed in both cases after a few months.
Antibodies against PD-L1 were also tested for the treatment of endometrial carcinoma. Fleming et al. [21] reported the results of a phase I clinical trial in which Atezolizumab, an anti-PD-L1 antibody, was tested in 15 women with advanced EC with microsatellite stability (MSS) and MSI unknown or MSI-H status. Patients received Atezolizumab 15 mg/m2 intravenously in monotherapy every three weeks. The authors reported an ORR of 13%, a median PFS of 1.7 months and a median OS of 9.6 months.
Anti PD-L1 antibody Avelumab was also tested in a recent phase II trial in which, up until now, 16 patients were enrolled and divided in two cohorts, one including ECs with MSI and/or POLE mutations and one including ECs patients with MSS. Patients received Avelumab 10 mg/kg as 1-hour IV infusion every 2 weeks until disease progression or unacceptable toxicity. This trial is still ongoing and preliminary results have not been published yet [22].
2) Targeting CTLA-4
CTLA-4 is expressed by regulatory T cells and serves as a negative immune regulator, as it binds competitively ligands B7.1 and B7.2 expressed on antigen-presenting cells, preventing its binding with stimulatory receptor CD28 and therefore inhibiting the activation of cytotoxic T lymphocytes. CTLA-4 predominately regulates T cell activation within secondary lymphoid organs [5].
Although the use of CTLA-4 inhibitors has a strong rationale in EC, clinical data about the efficacy of molecules like Ipilimumab and Tremelimumab, two anti-CTLA-4 monoclonal antibodies, have not been reported so far.
3. Adoptive cell transfer (ACT)
ACT indicates a reinfusion of allogenic or autologous lymphocytes (T cells) isolated through leukapheresis, activated and expanded in vitro, into cancer patients in order to induce tumor regression. Firstly, patients undergo lympho-depleting therapy to decrease cells of immune system and to activate cytokines [23]. This treatment does not induce immunological memory, but offers immediate and short-term protection. Several types of ACT therapies exist, including lymphokine-activated killer (LAK) cells, tumor-infiltrating lymphocytes (TILs), natural killer (NK) cells. LAK cells are leukocytes cultured with autologous peripheral blood mononuclear cells and IL-2, whereas TILs recognize HLAs. TILs have been used in melanomas in preclinical studies, but have shown limiting features for their application in clinical practice [24,25]. Subsequently, advances in T cells engineering and culturing have introduced T cell receptors (TCRs) and chimeric antigen receptors (CARs) that recognize a wide range of potential cellular targets, so the use of ACT was applied in a larger population of patients [23,24]. TCR derives from patients' lymphocytes transfected with a viral vector that carries TCR genes and may recognize antigens specifically derived from a tumor-reactive T cell clone [25]. CARs are modified membrane receptors, composed of an extracellular antibody single-chain variable fragment (scFv), a TCR-derived internal domain and one or more intracellular co-stimulatory domains. Although in ovarian cancer it is known that the presence of TILs is related to a more favorable outcome, as demonstrated in a metanalysis and in recent studies [26,27], ACT in the treatment of EC has not been investigated yet.
The earliest preclinical studies in EC involved the infusion of LAK cells with and without additional immuno-stimulatory components (IL-2, lentinan) [28,29]. This therapy produced growth retardation of tumor in nude mice. Steis et al. [30] investigated intraperitoneal adoptive transfer of LAK cells with IL-2 in a phase I trial that enrolled 12 colorectal cancer patients, 10 ovarian cancer patients, and 1 EC patient with abdominal metastasis. Partial response was detected in thirty percent of patients, but no women with EC were included. Santin et al. [31] evaluated the infusion of peripheral blood T cells stimulated with tumor lysate-pulsed autologous dendritic cells in a 65-year-old patient with advanced, chemoresistant EC. During treatment, a SD response was obtained through cytotoxic T cell response.
4. Bispecific T cell engager (BiTE) Antibodies
BiTE antibodies are novel molecules that induce a transient cytolytic synapsis between a cytotoxic T cell and the cancer target [32]. After this interaction, cytotoxic T cell contents are discharged, resulting in direct tumor cell lysis. At present Blinatumomab (BiTE for CD19 and CD3) is approved by Food and Drug Administration (FDA) for patients with acute lymphoblastic leukemia (ALL), based on a complete remission rate in a phase 2 clinical trial [32].
Preclinical studies have shown interesting results on uterine serous carcinoma (USC) cells that overexpress epithelial-cell-adhesion-molecule (EpCAM) treated with BiTE antibodies [9]. Bellone et al. [33] investigated the role of Solitomab, a novel bispecific single-chain antibody construct which targets EpCAM on tumor cells expressed in 87.5% of USC, tested by flow cytometry. They demonstrated that Solitomab induces robust immunologic responses in vitro resulting in increased T cell activation with production of cytokines, and direct killing of tumor cells. For this reason it could be in the future a novel, potentially effective agent for treatment of recurrent/metastatic and/or chemo-resistant USC overexpressing EpCAM.
GENOMIC INSTABILITY
Serous EC appears to share similar genetic background to serous ovarian carcinoma, including deficiency in DNA repair systems, providing a rationale for use of poly ADP-ribose polymerase (PARP) inhibitors in this malignancy as well. PARP is an enzyme that catalyzes the poly ADP-ribosylation of proteins involved in DNA repair and has proven effective in treatment of ovarian cancers with homologous recombination deficiency and genomic instability due to somatic BRCA1 and BRCA2 mutations. Although PARP inhibitors have already demonstrated promising pre-clinical activity in EC [34], clinical trials data are not yet available.
Olaparib, an oral PARP inhibitor, proved to be clinically effective in a case of a 58 years old woman affected by metastatic endometrioid EC previously treated with surgery, adjuvant radiotherapy and several lines of chemotherapy. Olaparib was administrated orally at the dosage of 400 mg twice daily. After 10 weeks of treatment a significant reduction in the size of the brain metastases was observed, but unfortunately disease progression was observed after 8 months of therapy. Interestingly, genomic characterization of tumor biopsy showed absence of BRCA1 or BRCA2 mutations, but displayed loss of PTEN expression, suggesting that this alteration could be predictive of sensitivity to PARP inhibitors [35].
SUSTAINED PROLIFERATIVE SIGNALING
1. Targeting cytoplasmic tyrosine kinases and phosphates-AKT/mTOR pathway
The mTOR is a serine/threonine kinase involved in intracellular pathways that regulate cellular growth and proliferation. Over-activation of mTOR signaling has a central role in the pathogenesis of many types of cancer, including endometrial tumors.
Oza et al. [36] studied in a phase II trial the activity of Temsirolimus, an inhibitor of mTOR, in two groups of chemotherapy naive or treated recurrent or metastatic EC patients. Temsirolimus 25 mg was administrated intravenously weekly in monotherapy. In the chemotherapy naive group of 29 patients 14% had a partial response, 69% had SD and only 18% had progressive disease, while in the chemotherapy-treated group of 25 patients 4% had a confirmed partial response, 48% had SD, and 48% had progressive disease.
Another mTOR inhibitor, everolimus, was reported to be effective in recurrent chemotherapy treated EC in a phase II trial [37]. It was administrated in a group of 28 patients at the dosage of 10 mg daily until disease progression or unbearable toxicity. Although no complete or partial responses was observed, 43% of patients had SD, with a median duration of 4.5 months. The safety profile of everolimus was acceptable in the context of heavily pretreated patients with EC.
2. Targeting epidermal growth factor receptor (EGFR)
Members of the Type I receptor tyrosine kinase family which includes EGFR are frequently implicated in the occurrence and progression of a variety of tumors. High EGFR expression has been demonstrated in 43%–67% of patients with EC and positively correlates with the FIGO stage, differentiation degree, depth of myometrial invasion, and lymph node metastasis, and is associated to poor prognosis, low survival rate and shortened disease-free survival [38,39].
Selective inhibitors of the EGFR tyrosine kinase have showed concentration-dependent anti-proliferative effects in EC cell lines in in vitro studies [39].
However, two phase II clinical trials using EGFR inhibitors in monotherapy showed low response rate (RR), suggesting that the tumor heterogeneity and molecular instability has to be tackle with multi targeted therapies [40,41]. The first one was a two-stage phase II study that aimed to evaluate activity of Erlotinib in monotherapy in 33 women with advanced EC and recurrent or metastatic disease who were chemotherapy naive and had received up to one line of prior hormonal therapy. Erlotinib was administered at daily dose of 150 mg. Treatment was well tolerated and severe toxicity infrequent, with the only grade 4 toxicity being an elevation of transaminases (AST). There were 4 confirmed partial responses (12.5%; 95% confidence interval [CI]=3.5%–29%) lasting 2 to 36 months. Fifteen patients had SD, with median duration of 3.7 months and thirteen patients (40.6%) had PD on study [40]. The second study evaluated another selective inhibitor of EGFR tyrosine kinase activity, Gefitinib in a multicenter phase II open-label trial on 26 patients with recurrent or persistent EC from 16 participating institutions across the United States. Enrolled women were treated with 500 mg oral Gefitinib daily until progression or severe toxicity, with PFS at six months as the primary endpoint. Four patients experienced PFS ≥6 months, and one had a complete response which was not associated with an EGFR mutation [41].
In line with these findings, there are two ongoing trials of ado-trastuzumab emtasine and afatinib (irreversible EGFR, HER 2 and HER4 inhibitors) that are currently accruing patients with EC and HER2-amplified or mutant cancers (NCT02675829 and NCT02491099).
3. Targeting mitogen-activated protein kinase kinase (MEK)
Among the patterns which play an essential role in cell survival, proliferation, and differentiation, MEK is a critical kinase in the mitogen-activated protein (MAP) kinase signal transduction pathway for many growth factor receptors that provide growth signals to cancer cells, including epidermal growth factor (EGF) receptor, insulin-like growth factor (IGF)-1 receptor and platelet-derived growth factor (PDGF) receptor. A phase II evaluation of selumetinib (AZD6244, ARRY-142886), a selective MEK-1/2 inhibitor in the treatment of recurrent or persistent EC has shown very promising results [42]. In this single arm, open label study, Coleman et al. [42] evaluated response and 6-month event-free survival (EFS) as primary endpoints in 54 patients with recurrent EC. They demonstrated that selumetinib is well tolerated in patients with recurrent or persistent measurable epithelial EC, but has limited single-agent activity and did not meet their pre-specified efficacy parameters.
In line with the TGCA findings [6], which report frequent alternations in MAPK, phosphatidylinositol-3 kinase (PI3K) and beta-catenin pathways in EC subtypes, Aslan et al. [43] profiled 13 EC cell lines for their PI3K pathway and KRAS mutational and PTEN protein status and treated them with one MEK- and two PI3K-targeted inhibitors alone and in combination. Their results showed that PTEN protein loss and the absence of any tested pathway mutations are dominant negative predictors of sensitivity to MEK inhibition. KRAS-mutated cells were most sensitive to MEK inhibition, but significantly more resistant to PI3K inhibition than KRAS-wild-type cell lines. These in vitro data suggested that inhibition of MEK with cobimetinib alone or in combination with PI3K inhibitors (pictilisib and apitolisib) could be a promising treatment modality, not just for EC patients with mutated KRAS, but also for those with retained PTEN expression.
4. Targeting focal adhesion kinase (FAK)
PTEN mutation has found to be attractive also for its role in dephosphorylating FAK. FAK is a non-receptor protein tyrosine kinase that is overexpressed in many types of human cancer cells, portending a poor prognosis and decreased survival duration. Previous studies demonstrated a role for FAK in tumor angiogenesis, migration, invasion and metastasis. In fact, since 2015 in vitro and in vivo studies showed that FAK inhibition is most effective in treatment of PTEN-mutated EC, suggesting PTEN as a feasible biomarker for predicting tumoral response to this treatment [44].
5. Targeting IGF
Many studies focus on the role of the IGF and sex hormone axes in endometrial physiology [45,46]; in the most of them appear clear that these pathways are considerably dysregulated in diabetes as well as in EC development [47,48].
The IGFs (IGF-I, IGF-II) are a family of binding proteins involved in growth, resistance to apoptosis, and differentiation of cells [49].
Cyclic changes in IGF-I expression play a pivotal role in regulating the transition of premenopausal endometrium through the proliferative, secretory, and menstrual phases of the uterus cycle [50,51].
Even if the biological mechanisms of the connection between EC and diabetes is not well known, many epidemiological studies have demonstrated a correlation between activation of IGF axis components, serum IGF-I and insulin values and EC risk [50,51,52,53,54,55].
The insulin-like growth factor receptor I (IGF1R) signaling pathway starts with binding of IGF-I to its cell-surface receptor IGF1R. This link is able to activate PI3K/Akt signaling pathway, to stimulate cell growth and proliferation, and to inhibit programmed cell death [56].
Insulin receptor and insulin-like growth factor receptor (IGF-IR) are tyrosine kinase receptors with more than 50% structural homology. Both of them are covalent dimers composed of two transmembrane β-subunits enclosing tyrosine kinase domains and two extracellular α-subunits containing ligand binding sites. The two receptors have different biological effects; in fact, while insulin receptor activation has essentially metabolic effects, IGF-IR signaling has mainly mitogenic effects. Although may occur some interaction, insulin exerts its effect mostly through IR, and IGFs bind to IGF-IR with high affinity and bind to IR with much lower affinity (<1%) [56].
Both insulin and IGF-1 are known factors that promote cell growth, thus, decreasing insulin would have a negative effect on cell proliferation.
Metformin is one of the most widely prescribed oral hypoglycemic agents used to treat type 2 diabetes. This molecule seems to have both a direct and indirect effects on cell growth and metabolism. In the direct model, metformin activates AMPK, which induces phosphorylation of tuberous sclerosis 2 protein. As a result, mTOR signaling and ultimately cell growth are inhibited. Metformin can exert its effect indirectly by increasing insulin sensitivity and uptake of glucose in the cell, and by decreasing consequently circulating levels of insulin [57].
Both diabetes and insulin resistance are risk factors for EC; these evidences are confirmed by many studies [58,59]. Preclinical data have demonstrated that increasing doses of metformin were associated with a decrease in cell proliferation in several EC cell lines [60,61].
Based on these data, Soliman et al. [57] supposed that treatment with oral metformin would decrease EC cell growth by activation of AMPK and inhibition of mTOR.
In this prospective trial, newly diagnosed EC patients underwent pre-treatment blood draw and endometrial biopsy, were administered oral metformin 850 mg daily for ≥7 days, and underwent post-treatment blood draw and definitive surgery. Serum levels of IGF-1, omentin, insulin, C-peptide, and leptin significantly decreased between pre- and post-treatment samples and phosphorylation of AKT and MAPK were significantly decreased in EC cells after oral metformin. These results suggest that metformin may be of benefit in the treatment of EC. Although the data supporting a potential main role of metformin in the treatment of EC, it is unclear at this point if there is an impact on OS [62].
Ongoing clinical trials will help determine the appropriate role for metformin in the treatment of women with EC.
In this panorama also other new molecules have aroused interest.
Attias-Geva et al. [63] investigated Cixutumumab (IMC-A12), a fully human antibody that binds to the IGF-IR with high affinity and inhibits IGF-I- and IGF-II-stimulated proliferation in different cell types and xenograft tumor models with very high efficiency and specificity.
Their results demonstrated that cixutumumab was able to block the IGF-I-induced autophosphorylation of the IGF-IR and the PI3K and MAPK downstream signaling pathways were also inactivated in part of the cell lines. Furthermore prolonged (24 hours and 48 hours) exposures to cixutumumab reduced IGF-IR expression, by mediating IGF-IR internalization and degradation.
They evaluated also apoptotic effect; results obtained showed that cixutumumab increased caspase-3 and PARP cleavage, two markers of apoptosis.
In summary, in a cell line model of EC cixutumumab was able to bind specifically and cause internalization of IGF-IR and subsequently to inhibit the cell proliferation IGF-I induced. Taken together, these results suggest that cixutumumab might be a promising anticancer therapeutic strategy in EC.
Attias-Geva et al. [55] focused on the anti-proliferative potential of NVP-AEW541 as a targeted therapy approach against the IGF-IR in Type I and Type II ECs. NVPAEW541 is a pyrrolo (2,3-d) pyrimidine derivative with specific IGF-IR tyrosine kinase inhibitory activity. NVP-AEW541 has been shown to void IGF-I-induced IGF-IR autophosphorylation and to decrease activation of the IGF-IR signaling pathways. These data suggest that NVP-AEW541 may be of benefit in the treatment of EC.
Metformin was shown to reduce proliferation in a preoperative study in obese patients with EC with a mean reduction in Ki-67 of 11.75%. A total of 65% of patients responded to metformin as defined by a decrease in Ki-67 staining [64]. A randomized placebo-controlled phase II/III trial is ongoing to assess the interest to combine metformin to paclitaxel/carboplatin advanced EC (NCT02065687).
6. Targeting folate receptor
Novel target therapy for EC involves also folate, also known as vitamin B9, as a molecule highly needed by rapidly proliferating cells. Folate receptor α (FRα), whose main task is to transfer folate vitamin through the cell membrane, is known to be extremely needed by the cells of malignancies that proliferate rapidly, while is present in limited amounts in normal tissues [65]. FRα expression is associated with high-grade, advanced-stage EC and a poor prognosis, particularly in serous-type tumors [66], thus representing an innovative candidate for targeted therapeutic strategies in advanced EC. Mirvetuximab soravtansine is an antibody-drug conjugate (ADC) comprised of an FRα-binding antibody, cleavable linker, and the maytansinoid DM4, a potent tubulin-targeting agent. A phase 1 expansion study of mirvetuximab soravtansine in patients with EC is currently ongoing (NCT02606305) [67].
ANGIOGENESIS
Angiogenesis is one of the cardinal processes leading to invasion and metastasis in solid tumors. Vascular endothelial growth factor (VEGF), an endothelial cell-specific mitogen specifically acting on vascular endothelial cells and promoting their proliferation, is the strongest currently known growth factor that acts directly on vascular endothelial cells and plays a pivotal role in progression, invasion and metastasis in EC [38].
Several groups of study tested angiogenetic therapies targeting VEGF [68,69,70,71,72]. One of the first trials was proposed in 2011 by Aghajanian et al. [67], who conducted a phase II trial of Bevacizumab, a humanized monoclonal antibody that acts as a direct VEGF inhibitor, in recurrent or persistent EC. Fifty-six patients were enrolled. Seven patients (13.5%) experienced clinical responses (1 complete response and 6 partial responses; median response duration, 6 months), and 21 patients (40.4%) survived progression free for at least 6 months. Median PFS and OS times were 4.2 and 10.5 months, respectively. Adverse events were consistent with those expected with bevacizumab treatment. No gastrointestinal perforations or fistulae were seen. Since then, multiple phase II trials have demonstrated improved PFS with bevacizumab monotherapy or in combination with an mTOR inhibitor [69,70,71,72].
Viswanathan et al. [68] studied 15 EC patients who received concurrent bevacizumab and pelvic intensity modulated radiation therapy (IMRT), reporting a 1-year PFS and 3-year PFS of 80% and 67% respectively and confirming a good local disease control, in particular in patients with non-dissectible nodes. The OS after 1-year and 3-year were 93% and 80%, respectively. Adverse effects included thrombosis and 1 embolic event in the setting of metastatic disease, but no gastrointestinal perforations were reported. Alvarez et al. [69] studied the combination of bevacizumab 10 mg/kg every other week and temsirolimus 25 mg intravenously weekly in 49 patients with persistent or recurrent EC after one to two prior cytotoxic regimens and showed 24.5% of clinical responses and median PFS and OS times of 5.6 and 16.9 months, respectively.
Simpkins et al. [70] evaluated the response to a regimen consisting of paclitaxel 175 mg/m2, carboplatin (AUC 5) and bevacizumab 15mg/kg in 15 patients with stage III/IV or recurrent EC. Five complete responses and 6 partial responses were seen, with a median PFS of 18 months and a median OS of 58 months. The GOG-86P trial of bevacizumab with cytotoxic agents suggested a potential survival benefit. In this randomized phase II trial, patients with chemotherapy-naïve stage III/IVA and stage IVB or recurrent EC were randomly assigned to treatment with paclitaxel and carboplatin (PC) plus bevacizumab (Arm 1), PC plus temsirolimus (Arm 2) or ixabepilone and carboplatin (IC) plus bevacizumab (Arm 3). Three hundred forty-nine patients were randomized. OS was significantly increased in the PC plus bevacizumab Arm when compared to historical controls treated with PC. However, the lack of contemporaneous control and the lack of improvement in RR and PFS necessitates interpreting the OS results with caution [72].
Lately, very interesting results came from Lenvatinib, an oral multiple kinase inhibitor targeting VEGF receptors 1–3, fibroblast growth factor (FGF) receptors 1–4, and PDGF beta, carried on 133 patients affected by advanced or recurrent EC. Complete response was noted in 29% of patients with a median OS of 10.6 months. Lenvatinib in combination with immunotherapy is therefore being developed [73].
Also Cediranib, a multi-tyrosine kinase inhibitor targeting VEGF, PDGF, and FGF receptors, was tested as a second or third line of therapy in EC patients with measurable disease in a phase II study conducted by Bender et al. [73]. Of the 48 patients enrolled, 12.5% showed a partial response, with a median PFS of 3.65 months and a median OS of 12.5 months.
HORMONAL THERAPY
An important role in regulation of normal endometrial function is played by expression of sex steroid hormone receptors like estrogen receptor (ER) α and β and progesterone receptor (PR A and PR B). ERα, ERβ and PR A and PR B are nuclear receptors encoded by different genes. Today we know that estrogens, progesterone and their receptors are involved in the development of many types of malignant tumors and interest in the study of these receptors has been growing significantly for their prognostic and therapeutic importance. As for EC, mostly Type I tumors, which express ERα and PR are, associated with hyperestrogenism and characterized by low tumor grade and a good prognosis. On the other hand, type 2 tumors, are often negative for hormone receptors, are high-grade and have a relatively poor prognosis.
Hormonal therapy is the only target therapy approved for EC. Even though hormonal therapy has been considered standard for four decades, prediction of its efficacy with receptor evaluation and understanding mechanisms of resistance are still important challenges. For a long time, hormonal therapy has been available as an adjuvant treatment of hormone responsive advanced or recurrent EC. Hormonal therapy can be used at the same time or in sequence with chemotherapy, with a RR between 10%–20% and a survival shorter than 1 year. Progestin treatment is able to inhibit the gene expression of ERs and reverse estrogen-induced proliferation of EC cells. Nevertheless, in some cases resistance to progestin therapy occurs for reasons that that are unknown. Studies in literature have discovered the role of second mitochondria derived activator of caspase (SMAC) as capable to sensitize for apoptosis in gynecological cancer cells [74,75].
One preclinical study in literature investigated the role of SMAC in EC. Neubauer et al. [76] It evaluated the role of inhibitors of apoptosis (IAPs) in the progesterone receptors (PRB23) cells to promote cell survival using an antagonist to IAPs, SMAC, also known as DIABLO. Treatment of PRB23 cells with SMAC mimetic increased apoptosis. This study could be the starting point to explain resistance to progestin therapy.
At present, however, progestin-based adjuvant treatment in advanced or recurrent EC has not shown a clear advantage in terms of OS. The use of progestin for advanced-EC patients appears to increase non-cancer related adverse events and death. For this reason, progestin is considered a valid option only in Type I advanced or recurrent EC patients with several comorbidities and old age. Progestin-based drugs usually employed are: hydroxyprogesterone caproate, with a RR of 37%, medroxyprogesterone acetate (RR 9%–53%), and megestrol acetate (24%–46%). Several works describe the action of selective ER modulators (SERMs): tamoxifen, for example, can increase the progesterone activity against EC cells through the link with the corresponding receptor. Other works consider the role of gonadotrophin-releasing hormone analogs (GnRHa). GnRHa causes a reduction of the gonadotrophin level by means of pituitary receptor down-regulation and, consequently, the suppression of ovarian activity and the reduction of the estrogen level. At present, only a single randomized report on the neo-adjuvant use of aromatase inhibitor (AI) in EC patients have been done. Thangavelu et al. [77] showed a decrease of endometrial proliferation in 16 EC patients subjected to anastrozole therapy for 14 days, against 8 patients treated with placebo. The authors also demonstrated a significant decrease of the expression of glandular Ki-67. As previously reported for breast cancer patients, AI may find a clinical use in the treatment of EC, but they are mainly useful in the case of patients not eligible for surgery. Combination therapy with mTOR and an AI has been evaluated as well, based on preclinical evidence showing that mTOR inhibition overcomes hormonal resistance. The combination of letrozole 2.5 mg with everolimus 10 mg demonstrated a clinical benefit rate (CBR) of 40% and an objective response rate of 32% in the 35 evaluable patients among 38 patients enrolled in the trial.
However, up until now, the lack of clinical trials for EC patients in large populations does not clarify the benefit in terms of OS and PFS.
CONCLUSION
Immunotherapy represents the most promising therapeutic approach in gynecological cancer. Current and ongoing studies are trying to improve clinical responses through immunotherapies strategies.
IGF, EGF, genomic instability and angiogenesis represent the hallmarks of EC most investigated in the last decade, achieving significant clinical results (Table 1) and several ongoing studies will help determine the role of compounds targeting these biological targets in the management of EC patients (Table 2).
Table 1. Main published trials involving targeted therapy in endometrial cancer.
| Author | Study year | No. of patients | Cancer type | Compound | Pathway target | Clinical response |
|---|---|---|---|---|---|---|
| Ott et al. [17] | 2017 | 24 | Advanced/metastatic | Pembrolizumab | PD-L1 | PR: 3 patients |
| SD: 1 patient | ||||||
| ORR: 13% | ||||||
| PFS: 19% | ||||||
| OS: 68.8% | ||||||
| Makker et al. [18] | 2017 | 23 | Advanced/metastatic | Pembrolizumab | PD-L1 | ORR: 48% |
| Fleming et al. [21] | 2017 | 15 | Advanced | Atezolimumab | PD-L1 | ORR: 13% |
| Oza et al. [36] | 2011 | 34 (25 CT naïve + 29 CT treated) | Recurrent/metastatic | Temsirolimus | mTOR | CT-naïve group |
| PR: 14%, SD: 69%, PD 18% | ||||||
| CT-treated group | ||||||
| PR: 4%, SD: 48%, PD 48% | ||||||
| Slomovitz et al. [37] | 2010 | 28 | Recurrent CT-treated | Everolimus | mTOR | PR: 0% |
| SD: 43% | ||||||
| Oza et al. [40] | 2008 | 33 | Recurrent/metastatic | Erlotinib | EGFR | PR: 12% |
| SD: 46.9% | ||||||
| PD: 40.6% | ||||||
| Leslie et al. [41] | 2013 | 26 | Persistent/recurrent after at least one CT regimen | Gefitinib | EGFR | CR: 3.8% |
| SD: 26.9% | ||||||
| PFS (median): 1.8 months | ||||||
| OS (median): 7.1 months | ||||||
| Coleman et al. [42] | 2015 | 54 | Persistent/recurrent | Selumetinib | MEK 1/2 | CR: 1 patient |
| PR: 2 patients | ||||||
| SD: 13 patients | ||||||
| PFS (median): 2.3 months | ||||||
| OS (median): 8.5 months | ||||||
| Aghajanian et al. [67] | 2011 | 56 | Persistent/recurrent | Bevacizumab | VEGF | CR: 1 patient |
| PR: 6 patients | ||||||
| PFS (median): 4.2 months | ||||||
| OS (median): 10.5 months | ||||||
| Viswanathan et al. [68] | 2014 | 15 | Persistent/recurrent | Bevacizumab + IMRT | VEGF | 1-year PFS: 80% 3-year PFS: 67% |
| 1-year OS: 93% 3-year OS: 80% | ||||||
| Alvarez et al. [69] | 2013 | 49 | Persistent/recurrent | Bevacizumab + Temsirolimus | VEGF/mTOR | CR: 24.5% |
| PFS (median): 5.6 months | ||||||
| OS (median): 16.9 months | ||||||
| Simpkins et al. [70] | 2014 | 15 | Stage III/IV or recurrent EC | Bevacizumab + Paclitaxel/Carboplatin | VEGF | CR: 5 patients |
| PR: 6 patients | ||||||
| PFS (median): 18 months | ||||||
| OS (median): 58 months | ||||||
| Vergote et al. [72] | 2013 | 133 | Metastatic/unresectable endometrial cancer after 1 or 2 prior platinum-based treatments, ≤2 prior chemotherapies, and ECOG PS ≤2. | Lenvatinib | VEGFR1–3, FGFR1–4, RET, KIT, and PDGFRβ | CR + PR: 14.3% |
| PFS (median): 5.4 months | ||||||
| OS (median): 10.6 months | ||||||
| Bender et al. [73] | 2015 | 48 | Second or third line of therapy in EC patients with measurable disease | Cediranib | VEGF, PDGF, FGF | PR: 12.5 % |
| PFS (median): 3.65 months | ||||||
| OS (median): 12.5 months |
CR, clinical response; CT, chemotherapy; EC, endometrial cancer; ECOG Eastern Cooperative Oncology Group; EGFR, epidermal growth factor receptor; FGF, fibroblast growth factor; IMRT, intensity-modulated radiation therapy; MEK, mitogen-activated protein kinase kinase; mTOR, mammalian target of rapamycin; ORR, overall response rate; OS, overall survival; PD, progressive disease; PD-L1, programmed death-ligand 1; PDGF, platelet-derived growth factor; PFS, progression free survival; PR, partial response; PS, performance status; SD, stable disease; VEGF, vascular endothelial growth factor.
Table 2. Main ongoing clinical trials involving targeted therapy in endometrial cancerCTLA-4, cytotoxic T-lymphocyte-associated antigen 4; mTOR, mammalian target of rapamycin; PARP, poly ADP-ribose polymerase; PD, progressive disease; PD-L1, programmed death-ligand 1; VEGF, vascular endothelial growth factor.
| Compound | Target pathway | Pathway target |
|---|---|---|
| Pembrolizumab | PD-1 | NCT02899793 (phase II) |
| NCT02630823 (phase I/II) | ||
| NCT02549209 (phase II) | ||
| NCT02606305 (phase Ib) | ||
| NCT02501096 *plus Bevacizumab (phase Ib/II) | ||
| NCT03694834 (phase Ib) | ||
| NCT03276013 (phase II) | ||
| NCT03192059 (phase II) | ||
| NCT03517449 *plus Lenvatinib (phase III) | ||
| Atezolizumab | PD-L1 | NCT03603184 (phase III) |
| NCT03526432 *plus Bevacizumab (phase II) | ||
| NCT03694262 *plus Bevacizumab/Rucaparib (phase II) | ||
| NCT02914470 *plus CBDCA-CTX (phase Ib) | ||
| Avelumab | PD-L1 | NCT02912572 (phase II) |
| NCT03503786 (phase II) | ||
| Ipilimumab | CTLA-4 | NCT02982486 *plus Nivolumab (phase II) |
| Olaparib | PARP | NCT02755844 (phase I/II) |
| NCT03660826 *plus Adavosertib/Cediranib (phase II) | ||
| NCT03570437 *plus Paclitaxel/Cediranib (phase II) | ||
| Everolimus | mTOR | NCT03008408 *plus Ribociclib/Letrozole (phase II) |
| Bevacizumab | VEGF | NCT03526432 *plus Atezolizumab (phase II) |
| NCT03694262 *plus Rucaparib/Atezolizumab (phase II) | ||
| Lenvatinib | VEGF | NCT03517449 *plus Pembrolizumab (phase III) |
| Cediranib | VEGF | NCT03660826 *plus Olaparib/Cediranib (phase II) |
| NCT03570437 *plus Olaparib/Paclitaxel (phase II) |
The use of anti-angiogenetic agents, PARP-inhibitors and hormonal therapy is a promising strategy in the treatment of EC. POLE-mutated and MMR-deficient tumors exhibit TILs, high levels of neoantigens, and expression of immune checkpoint regulators, such as PD-1 or its ligand, PD-L1, that escape from immune surveillance [78]. Pembrolizumab, a humanized monoclonal antibody that targets PD-1, has been approved by FDA for metastatic cancers exhibiting MMR deficiency and in trials with advanced or metastatic EC the ORR ranges from 13% to 48% [19,79,80].
Adoptive T cell therapies are receiving increased attention as an immunotherapeutic approach for EC but BiTE antibodies treatment has not been implemented yet and only preclinical trials have been performed on USC cells. As single treatments modalities, chemotherapies and radiotherapies may be ineffective in advanced metastatic and recurrent cancer. In these cases, a combinatory approach may induce a synergistic effect of conventional therapies and immunotherapy [24]. Pathologic identification of new variants of EC continues to advance the phenotypic spectrum of these tumors inducing genomic studies to reveal new strategies for therapy. Hence, in the era of precision medicine, the future efforts will be focused on pathologic assessment of biomarkers (e.g., mismatch repair proteins), recognition of phenotypes that are amenable to specific targeted therapies (such as POLE-mutated tumors) and on the identification of the best therapeutic combination, and the more appropriate clinical setting in the management of women with endometrial carcinoma.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: D.T.C., S.M.C., D.D.V.
- Data curation: D.D.V.
- Formal analysis: C.C., G.G., I.V.
- Funding acquisition: D.T.C., C.C.
- Investigation: D.T.C.
- Resources: D.T.C., S.M.C.
- Supervision: D.T.C., M.L., P.P.B.
- Validation: D.T.C., M.L., P.P.B.
- Visualization: C.C.
- Writing - original draft: C.C., G.G., I.V.
- Writing - review & editing: D.T.C., S.M.C., D.D.V.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2.Ali AT. Reproductive factors and the risk of endometrial cancer. Int J Gynecol Cancer. 2014;24:384–393. doi: 10.1097/IGC.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 3.Lynch HT, Snyder CL, Shaw TG, Heinen CD, Hitchins MP. Milestones of Lynch syndrome: 1895–2015. Nat Rev Cancer. 2015;15:181–194. doi: 10.1038/nrc3878. [DOI] [PubMed] [Google Scholar]
- 4.Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983;15:10–17. doi: 10.1016/0090-8258(83)90111-7. [DOI] [PubMed] [Google Scholar]
- 5.Mittica G, Ghisoni E, Giannone G, Aglietta M, Genta S, Valabrega G. Checkpoint inhibitors in endometrial cancer: preclinical rationale and clinical activity. Oncotarget. 2017;8:90532–90544. doi: 10.18632/oncotarget.20042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cancer Genome Atlas Research Network. Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67–73. doi: 10.1038/nature12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bosse T, Nout RA, McAlpine JN, McConechy MK, Britton H, Hussein YR, et al. Molecular Classification of Grade 3 Endometrioid Endometrial Cancers Identifies Distinct Prognostic Subgroups. Am J Surg Pathol. 2018;42:561–568. doi: 10.1097/PAS.0000000000001020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Talhouk A, McConechy MK, Leung S, Li-Chang HH, Kwon JS, Melnyk N, et al. A clinically applicable molecular-based classification for endometrial cancers. Br J Cancer. 2015;113:299–310. doi: 10.1038/bjc.2015.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Longoria TC, Eskander RN. Immunotherapy in endometrial cancer - an evolving therapeutic paradigm. Gynecol Oncol Res Pract. 2015;2:11. doi: 10.1186/s40661-015-0020-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang A, Jeang J, Cheng K, Cheng T, Yang B, Wu TC, et al. Current state in the development of candidate therapeutic HPV vaccines. Expert Rev Vaccines. 2016;15:989–1007. doi: 10.1586/14760584.2016.1157477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohno S, Kyo S, Myojo S, Dohi S, Ishizaki J, Miyamoto K, et al. Wilms' tumor 1 (WT1) peptide immunotherapy for gynecological malignancy. Anticancer Res. 2009;29:4779–4784. [PubMed] [Google Scholar]
- 12.Coosemans A, Vanderstraeten A, Tuyaerts S, Verschuere T, Moerman P, Berneman ZN, et al. Wilms' Tumor Gene 1 (WT1)--loaded dendritic cell immunotherapy in patients with uterine tumors: a phase I/II clinical trial. Anticancer Res. 2013;33:5495–5500. [PubMed] [Google Scholar]
- 13.Jäger E, Karbach J, Gnjatic S, Neumann A, Bender A, Valmori D, et al. Recombinant vaccinia/fowlpox NY-ESO-1 vaccines induce both humoral and cellular NY-ESO-1-specific immune responses in cancer patients. Proc Natl Acad Sci U S A. 2006;103:14453–14458. doi: 10.1073/pnas.0606512103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaumaya PT, Foy KC, Garrett J, Rawale SV, Vicari D, Thurmond JM, et al. Phase I active immunotherapy with combination of two chimeric, human epidermal growth factor receptor 2, B-cell epitopes fused to a promiscuous T-cell epitope in patients with metastatic and/or recurrent solid tumors. J Clin Oncol. 2009;27:5270–5277. doi: 10.1200/JCO.2009.22.3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herzog TJ, Arguello D, Reddy SK, Gatalica Z. PD-1 and PD-L1 expression in 1599 gynecological malignanices-implications for immunotherapy. Gynecol Oncol. 2015;137:204–205. [Google Scholar]
- 16.Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015;372:2509–2520. doi: 10.1056/NEJMoa1500596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ott PA, Bang YJ, Berton-Rigaud D, Elez E, Pishvaian MJ, Rugo HS, et al. Safety and antitumor activity of pembrolizumab in advanced programmed death ligand 1-positive endometrial cancer: results from the KEYNOTE-028 study. J Clin Oncol. 2017;35:2535–2541. doi: 10.1200/JCO.2017.72.5952. [DOI] [PubMed] [Google Scholar]
- 18.Makker V, Rasco DW, Dutcus CE, Stepan DE, Li D, Schmidt EW, et al. A phase Ib/II trial of lenvatinib (LEN) plus pembrolizumab (Pembro) in patients (Pts) with endometrial carcinoma. J Clin Oncol. 2017;35:abstr5598 [Google Scholar]
- 19.Mehnert JM, Panda A, Zhong H, Hirshfield K, Damare S, Lane K, et al. Immune activation and response to pembrolizumab in POLE-mutant endometrial cancer. J Clin Invest. 2016;126:2334–2340. doi: 10.1172/JCI84940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santin AD, Bellone S, Buza N, Choi J, Schwartz PE, Schlessinger J, et al. Regression of chemotherapy-resistant polymerase ε (POLE) ultra-mutated and MSH6 hyper-mutated endometrial tumors with nivolumab. Clin Cancer Res. 2016;22:5682–5687. doi: 10.1158/1078-0432.CCR-16-1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fleming GF, Emens LA, Eder JP, Hamilton EP, Liu JF, Liu B, et al. Clinical activity, safety and biomarker results from a phase Ia study of atezolizumab (atezo)in advanced/recurrent endometrial cancer(rEC) J Clin Oncol. 2017;35:abstr5585 [Google Scholar]
- 22.Konstantinopoulos PA, Liu JF, Barry WT, Krasner CN, Buss MK, Birrer MJ, et al. Phase 2, two-group, two-stage, open-label study of avelumab in patients with microsatellite stable, microsatellite instable and POLE-mutated recurrent or persistent endometrial cancer. J Clin Oncol. 2017;35:TPS5615 [Google Scholar]
- 23.Ruella M, Kalos M. Adoptive immunotherapy for cancer. Immunol Rev. 2014;257:14–38. doi: 10.1111/imr.12136. [DOI] [PubMed] [Google Scholar]
- 24.Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature. 2011;480:480–489. doi: 10.1038/nature10673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang D, Zhang X, Zhang X, Xu Y. The progress and current status of immunotherapy in acute myeloid leukemia. Ann Hematol. 2017;96:1965–1982. doi: 10.1007/s00277-017-3148-x. [DOI] [PubMed] [Google Scholar]
- 26.Hwang WT, Adams SF, Tahirovic E, Hagemann IS, Coukos G. Prognostic significance of tumor-infiltrating T cells in ovarian cancer: a meta-analysis. Gynecol Oncol. 2012;124:192–198. doi: 10.1016/j.ygyno.2011.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gasparri ML, Attar R, Palaia I, Perniola G, Marchetti C, Di Donato V, et al. Tumor infiltrating lymphocytes in ovarian cancer. Asian Pac J Cancer Prev. 2015;16:3635–3638. doi: 10.7314/apjcp.2015.16.9.3635. [DOI] [PubMed] [Google Scholar]
- 28.Inoue M, Shimizu H, Shimizu C, Sasagawa T, Ueda G, Tanizawa O, et al. Antitumor efficacy of recombinant interleukin 2-activated killer cells against endometrial cancers. Nippon Sanka Fujinka Gakkai Zasshi. 1987;39:143–144. [PubMed] [Google Scholar]
- 29.Shimizu H, Inoue M, Tanizawa O. Adoptive cellular immunotherapy to the endometrial carcinoma cell line xenografts in nude mice. Gynecol Oncol. 1989;34:195–199. doi: 10.1016/0090-8258(89)90141-8. [DOI] [PubMed] [Google Scholar]
- 30.Steis RG, Urba WJ, VanderMolen LA, Bookman MA, Smith JW, 2nd, Clark JW, et al. Intraperitoneal lymphokine-activated killer-cell and interleukin-2 therapy for malignancies limited to the peritoneal cavity. J Clin Oncol. 1990;8:1618–1629. doi: 10.1200/JCO.1990.8.10.1618. [DOI] [PubMed] [Google Scholar]
- 31.Santin AD, Hermonat PL, Ravaggi A, Bellone S, Cowan C, Coke C, et al. Development and therapeutic effect of adoptively transferred T cells primed by tumor lysate-pulsed autologous dendritic cells in a patient with metastatic endometrial cancer. Gynecol Obstet Invest. 2000;49:194–203. doi: 10.1159/000010246. [DOI] [PubMed] [Google Scholar]
- 32.Wickramasinghe D. Tumor and T cell engagement by BiTE. Discov Med. 2013;16:149–152. [PubMed] [Google Scholar]
- 33.Bellone S, Black J, English DP, Schwab CL, Lopez S, Cocco E, et al. Solitomab, an EpCAM/CD3 bispecific antibody construct (BiTE), is highly active against primary uterine serous papillary carcinoma cell lines in vitro. Am J Obstet Gynecol. 2016;214:99.e1–99.e8. doi: 10.1016/j.ajog.2015.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miyasaka A, Oda K, Ikeda Y, Wada-Hiraike O, Kashiyama T, Enomoto A, et al. Anti-tumor activity of olaparib, a poly (ADP-ribose) polymerase (PARP) inhibitor, in cultured endometrial carcinoma cells. BMC Cancer. 2014;14:179. doi: 10.1186/1471-2407-14-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Forster MD, Dedes KJ, Sandhu S, Frentzas S, Kristeleit R, Ashworth A, et al. Treatment with olaparib in a patient with PTEN-deficient endometrioid endometrial cancer. Nat Rev Clin Oncol. 2011;8:302–306. doi: 10.1038/nrclinonc.2011.42. [DOI] [PubMed] [Google Scholar]
- 36.Oza AM, Elit L, Tsao MS, Kamel-Reid S, Biagi J, Provencher DM, et al. Phase II study of temsirolimus in women with recurrent or metastatic endometrial cancer: a trial of the NCIC Clinical Trials Group. J Clin Oncol. 2011;29:3278–3285. doi: 10.1200/JCO.2010.34.1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Slomovitz BM, Lu KH, Johnston T, Coleman RL, Munsell M, Broaddus RR, et al. A phase 2 study of the oral mammalian target of rapamycin inhibitor, everolimus, in patients with recurrent endometrial carcinoma. Cancer. 2010;116:5415–5419. doi: 10.1002/cncr.25515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cai S, Zhang YX, Han K, Ding YQ. Expressions and clinical significance of COX-2, VEGF-C, and EFGR in endometrial carcinoma. Arch Gynecol Obstet. 2017;296:93–98. doi: 10.1007/s00404-017-4386-9. [DOI] [PubMed] [Google Scholar]
- 39.Konecny GE, Venkatesan N, Yang G, Dering J, Ginther C, Finn R, et al. Activity of lapatinib a novel HER2 and EGFR dual kinase inhibitor in human endometrial cancer cells. Br J Cancer. 2008;98:1076–1084. doi: 10.1038/sj.bjc.6604278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Oza AM, Eisenhauer EA, Elit L, Cutz JC, Sakurada A, Tsao MS, et al. Phase II study of erlotinib in recurrent or metastatic endometrial cancer: NCIC IND-148. J Clin Oncol. 2008;26:4319–4325. doi: 10.1200/JCO.2007.15.8808. [DOI] [PubMed] [Google Scholar]
- 41.Leslie KK, Sill MW, Fischer E, Darcy KM, Mannel RS, Tewari KS, et al. A phase II evaluation of gefitinib in the treatment of persistent or recurrent endometrial cancer: a Gynecologic Oncology Group study. Gynecol Oncol. 2013;129:486–494. doi: 10.1016/j.ygyno.2013.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Coleman RL, Sill MW, Thaker PH, Bender DP, Street D, McGuire WP, et al. A phase II evaluation of selumetinib (AZD6244, ARRY-142886), a selective MEK-1/2 inhibitor in the treatment of recurrent or persistent endometrial cancer: an NRG Oncology/Gynecologic Oncology Group study. Gynecol Oncol. 2015;138:30–35. doi: 10.1016/j.ygyno.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aslan O, Cremona M, Morgan C, Cheung LW, Mills GB, Hennessy BT. Preclinical evaluation and reverse phase protein Array-based profiling of PI3K and MEK inhibitors in endometrial carcinoma in vitro. BMC Cancer. 2018;18:168. doi: 10.1186/s12885-018-4035-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thanapprapasr D, Previs RA, Hu W, Ivan C, Armaiz-Pena GN, Dorniak PL, et al. PTEN expression as a predictor of response to focal adhesion kinase inhibition in uterine cancer. Mol Cancer Ther. 2015;14:1466–1475. doi: 10.1158/1535-7163.MCT-14-1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rutanen EM. Insulin-like growth factors in endometrial function. Gynecol Endocrinol. 1998;12:399–406. doi: 10.3109/09513599809012842. [DOI] [PubMed] [Google Scholar]
- 46.Zhu L, Pollard JW. Estradiol-17beta regulates mouse uterine epithelial cell proliferation through insulin-like growth factor 1 signaling. Proc Natl Acad Sci U S A. 2007;104:15847–15851. doi: 10.1073/pnas.0705749104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kaaks R, Lukanova A, Kurzer MS. Obesity, endogenous hormones, and endometrial cancer risk: a synthetic review. Cancer Epidemiol Biomarkers Prev. 2002;11:1531–1543. [PubMed] [Google Scholar]
- 48.Merritt MA, Strickler HD, Einstein MH, Yang HP, Sherman ME, Wentzensen N, et al. Insulin/IGF and sex hormone axes in human endometrium and associations with endometrial cancer risk factors. Cancer Causes Control. 2016;27:737–748. doi: 10.1007/s10552-016-0751-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Werner H, Bruchim I. The insulin-like growth factor-I receptor as an oncogene. Arch Physiol Biochem. 2009;115:58–71. doi: 10.1080/13813450902783106. [DOI] [PubMed] [Google Scholar]
- 50.Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Manson JE, Li J, et al. A prospective evaluation of insulin and insulin-like growth factor-I as risk factors for endometrial cancer. Cancer Epidemiol Biomarkers Prev. 2008;17:921–929. doi: 10.1158/1055-9965.EPI-07-2686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pavelić J, Radaković B, Pavelić K. Insulin-like growth factor 2 and its receptors (IGF 1R and IGF 2R/mannose 6-phosphate) in endometrial adenocarcinoma. Gynecol Oncol. 2007;105:727–735. doi: 10.1016/j.ygyno.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 52.Hirano S, Ito N, Takahashi S, Tamaya T. Clinical implications of insulin-like growth factors through the presence of their binding proteins and receptors expressed in gynecological cancers. Eur J Gynaecol Oncol. 2004;25:187–191. [PubMed] [Google Scholar]
- 53.McCampbell AS, Broaddus RR, Loose DS, Davies PJ. Overexpression of the insulin-like growth factor I receptor and activation of the AKT pathway in hyperplastic endometrium. Clin Cancer Res. 2006;12:6373–6378. doi: 10.1158/1078-0432.CCR-06-0912. [DOI] [PubMed] [Google Scholar]
- 54.Renehan AG, Zwahlen M, Minder C, O'Dwyer ST, Shalet SM, Egger M. Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. Lancet. 2004;363:1346–1353. doi: 10.1016/S0140-6736(04)16044-3. [DOI] [PubMed] [Google Scholar]
- 55.Attias-Geva Z, Bentov I, Fishman A, Werner H, Bruchim I. Insulin-like growth factor-I receptor inhibition by specific tyrosine kinase inhibitor NVP-AEW541 in endometrioid and serous papillary endometrial cancer cell lines. Gynecol Oncol. 2011;121:383–389. doi: 10.1016/j.ygyno.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 56.Dai C, Li N, Song G, Yang Y, Ning X. Insulin-like growth factor 1 regulates growth of endometrial carcinoma through PI3k signaling pathway in insulin-resistant type 2 diabetes. Am J Transl Res. 2016;8:3329–3336. [PMC free article] [PubMed] [Google Scholar]
- 57.Soliman PT, Zhang Q, Broaddus RR, Westin SN, Iglesias D, Munsell MF, et al. Prospective evaluation of the molecular effects of metformin on the endometrium in women with newly diagnosed endometrial cancer: a window of opportunity study. Gynecol Oncol. 2016;143:466–471. doi: 10.1016/j.ygyno.2016.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Burzawa JK, Schmeler KM, Soliman PT, Meyer LA, Bevers MW, Pustilnik TL, et al. Prospective evaluation of insulin resistance among endometrial cancer patients. Am J Obstet Gynecol. 2011;204:355.e1–355.e7. doi: 10.1016/j.ajog.2010.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Friberg E, Mantzoros CS, Wolk A. Diabetes and risk of endometrial cancer: a population-based prospective cohort study. Cancer Epidemiol Biomarkers Prev. 2007;16:276–280. doi: 10.1158/1055-9965.EPI-06-0751. [DOI] [PubMed] [Google Scholar]
- 60.Cantrell LA, Zhou C, Mendivil A, Malloy KM, Gehrig PA, Bae-Jump VL. Metformin is a potent inhibitor of endometrial cancer cell proliferation--implications for a novel treatment strategy. Gynecol Oncol. 2010;116:92–98. doi: 10.1016/j.ygyno.2009.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Iglesias DA, Yates MS, van der Hoeven D, Rodkey TL, Zhang Q, Co NN, et al. Another surprise from Metformin: novel mechanism of action via K-Ras influences endometrial cancer response to therapy. Mol Cancer Ther. 2013;12:2847–2856. doi: 10.1158/1535-7163.MCT-13-0439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Al Hilli MM, Bakkum-Gamez JN, Mariani A, Cliby WA, Mc Gree ME, Weaver AL, et al. The effect of diabetes and metformin on clinical outcomes is negligible in risk-adjusted endometrial cancer cohorts. Gynecol Oncol. 2016;140:270–276. doi: 10.1016/j.ygyno.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 63.Attias-Geva Z, Bentov I, Ludwig DL, Fishman A, Bruchim I, Werner H. Insulin-like growth factor-I receptor (IGF-IR) targeting with monoclonal antibody cixutumumab (IMC-A12) inhibits IGF-I action in endometrial cancer cells. Eur J Cancer. 2011;47:1717–1726. doi: 10.1016/j.ejca.2011.02.019. [DOI] [PubMed] [Google Scholar]
- 64.Schuler KM, Rambally BS, DiFurio MJ, Sampey BP, Gehrig PA, Makowski L, et al. Antiproliferative and metabolic effects of metformin in a preoperative window clinical trial for endometrial cancer. Cancer Med. 2015;4:161–173. doi: 10.1002/cam4.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Brown Jones M, Neuper C, Clayton A, Mariani A, Konecny G, Thomas MB, et al. Rationale for folate receptor alpha targeted therapy in “high risk” endometrial carcinomas. Int J Cancer. 2008;123:1699–1703. doi: 10.1002/ijc.23686. [DOI] [PubMed] [Google Scholar]
- 66.Senol S, Ceyran AB, Aydin A, Zemheri E, Ozkanli S, Kösemetin D, et al. Folate receptor α expression and significance in endometrioid endometrium carcinoma and endometrial hyperplasia. Int J Clin Exp Pathol. 2015;8:5633–5641. [PMC free article] [PubMed] [Google Scholar]
- 67.Aghajanian C, Sill MW, Darcy KM, Greer B, McMeekin DS, Rose PG, et al. Phase II trial of bevacizumab in recurrent or persistent endometrial cancer: a Gynecologic Oncology Group study. J Clin Oncol. 2011;29:2259–2265. doi: 10.1200/JCO.2010.32.6397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Viswanathan AN, Lee H, Berkowitz R, Berlin S, Campos S, Feltmate C, et al. A prospective feasibility study of radiation and concurrent bevacizumab for recurrent endometrial cancer. Gynecol Oncol. 2014;132:55–60. doi: 10.1016/j.ygyno.2013.10.031. [DOI] [PubMed] [Google Scholar]
- 69.Alvarez EA, Brady WE, Walker JL, Rotmensch J, Zhou XC, Kendrick JE, et al. Phase II trial of combination bevacizumab and temsirolimus in the treatment of recurrent or persistent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol. 2013;129:22–27. doi: 10.1016/j.ygyno.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 70.Simpkins F, Drake R, Escobar PF, Nutter B, Rasool N, Rose PG. A phase II trial of paclitaxel, carboplatin, and bevacizumab in advanced and recurrent endometrial carcinoma (EMCA) Gynecol Oncol. 2015;136:240–245. doi: 10.1016/j.ygyno.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 71.Aghajanian C, Filiaci V, Dizon DS, Carlson JW, Powell MA, Secord AA, et al. A phase II study of frontline paclitaxel/carboplatin/bevacizumab, paclitaxel/carboplatin/temsirolimus, or ixabepilone/carboplatin/bevacizumab in advanced/recurrent endometrial cancer. Gynecol Oncol. 2018;150:274–281. doi: 10.1016/j.ygyno.2018.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vergote I, Teneriello M, Powell MA, Miller DS, Garcia AA, Mikheeva ON, et al. A phase II trial of lenvatinib in patients with advanced or recurrent endometrial cancer: angiopoietin-2 as a predictive marker for clinical outcomes. J Clin Oncol. 2013;31:abstr5520 [Google Scholar]
- 73.Bender D, Sill MW, Lankes HA, Reyes HD, Darus CJ, Delmore JE, et al. A phase II evaluation of cediranib in the treatment of recurrent or persistent endometrial cancer: an NRG Oncology/Gynecologic Oncology Group study. Gynecol Oncol. 2015;138:507–512. doi: 10.1016/j.ygyno.2015.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mao HL, Pang Y, Zhang X, Yang F, Zheng J, Wang Y, et al. SMAC peptide potentiates TRAIL- or paclitaxel-mediated ovarian cancer cell death in vitro and in vivo. Oncol Rep. 2013;29:515–522. doi: 10.3892/or.2012.2132. [DOI] [PubMed] [Google Scholar]
- 75.Petrucci E, Pasquini L, Bernabei M, Saulle E, Biffoni M, Accarpio F, et al. A small molecule SMAC mimic LBW242 potentiates TRAIL- and anticancer drug-mediated cell death of ovarian cancer cells. PLoS One. 2012;7:e35073. doi: 10.1371/journal.pone.0035073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Neubauer NL, Ward EC, Patel P, Lu Z, Lee I, Blok LJ, et al. Progesterone receptor-B induction of BIRC3 protects endometrial cancer cells from AP1-59-mediated apoptosis. Horm Cancer. 2011;2:170–181. doi: 10.1007/s12672-011-0065-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Thangavelu A, Hewitt MJ, Quinton ND, Duffy SR. Neoadjuvant treatment of endometrial cancer using anastrozole: a randomised pilot study. Gynecol Oncol. 2013;131:613–618. doi: 10.1016/j.ygyno.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 78.Howitt BE, Shukla SA, Sholl LM, Ritterhouse LL, Watkins JC, Rodig S, et al. Association of polymerase e-mutated and microsatellite-instable endometrial cancers with neoantigen load, number of tumor-infiltrating lymphocytes, and expression of PD-1 and PD-L1. JAMA Oncol. 2015;1:1319–1323. doi: 10.1001/jamaoncol.2015.2151. [DOI] [PubMed] [Google Scholar]
- 79.Gatalica Z, Snyder C, Maney T, Ghazalpour A, Holterman DA, Xiao N, et al. Programmed cell death 1 (PD-1) and its ligand (PD-L1) in common cancers and their correlation with molecular cancer type. Cancer Epidemiol Biomarkers Prev. 2014;23:2965–2970. doi: 10.1158/1055-9965.EPI-14-0654. [DOI] [PubMed] [Google Scholar]
- 80.Liao JB. Immunotherapy for gynecologic cancers. Gynecol Oncol. 2016;142:3–5. doi: 10.1016/j.ygyno.2016.05.029. [DOI] [PubMed] [Google Scholar]