Abstract
Background: Burnout is a psychological syndrome characterized by emotional exhaustion, feelings of cynicism and reduced personal accomplishment. In the past years there has been disagreement on whether burnout and depression are the same or different constructs, as they appear to share some common features (e.g., loss of interest and impaired concentration). However, the results so far are inconclusive and researchers disagree with regard to the degree to which we should expect such overlap. The aim of this systematic review and meta-analysis is to examine the relationship between burnout and depression. Additionally, given that burnout is the result of chronic stress and that working environments can often trigger anxious reactions, we also investigated the relationship between burnout and anxiety.
Method: We searched the online databases SCOPUS, Web of Science, MEDLINE (PubMed), and Google Scholar for studies examining the relationship between burnout and depression and burnout and anxiety, which were published between January 2007 and August 2018. Inclusion criteria were used for all studies and included both cross-sectional and longitudinal designs, published and unpublished research articles, full-text articles, articles written in the English language, studies that present the effects sizes of their findings and that used reliable research tools.
Results: Our results showed a significant association between burnout and depression (r = 0.520, SE = 0.012, 95% CI = 0.492, 0.547) and burnout and anxiety (r = 0.460, SE = 0.014, 95% CI = 0.421, 0.497). However, moderation analysis for both burnout–depression and burnout–anxiety relationships revealed that the studies in which either the MBI test was used or were rated as having better quality showed lower effect sizes.
Conclusions: Our research aims to clarify the relationship between burnout–depression and burnout–anxiety relationships. Our findings revealed no conclusive overlap between burnout and depression and burnout and anxiety, indicating that they are different and robust constructs. Future studies should focus on utilizing more longitudinal designs in order to assess the causal relationships between these variables.
Keywords: burnout, depression, anxiety, meta-analysis, systematic review
Introduction
One of the most common psychological symptoms modern people increasingly experience is burnout, i.e., the outcome of chronic, work-related stress (Melamed et al., 2006). Burnout descriptions can be found in the historical record and they appear to be apparent across different times and cultures (reports of burnout feelings can be found from the Old Testament to Shakespeare's writings) (Kaschka et al., 2011). However, it was not until the mid 1970s that researchers have started investigating burnout feelings. In particular, two independent researchers, Herbert Freudenberger, a psychiatrist, and Christina Maslach, a social psychologist, were the first researchers who began examining burnout. Specifically, Freudenberger (1974) was the first to describe the concept of staff burnout. The basic elements of his definition of burnout described these experiences as to fail, wear out, or become exhausted by making excessive demands on energy, strength or resources, and can still be seen in the modern definitions of job burnout. Maslach et al. (1996) defined burnout as the experience of exhaustion, where the individuals who suffer from it become cynical toward the value of their occupation and doubt their ability to perform. According to Maslach et al. (1996), burnout is composed of three dimensions i.e., exhaustion, cynicism, and lack of professional efficacy. In more particular, exhaustion refers to feelings of stress, specifically chronic fatigue resulting from excessive work demands. The second dimension, depersonalization or cynicism, refers to an apathetic or a detached attitude toward work in general and the people with whom one works; leading to the loss of interest in work, and feeling that work has lost its meaning. Finally, lack of professional efficacy refers to reduced feelings of efficiency, successful attainment, and accomplishment both in one's job and the organization.
As Maslach and Leiter (2016) later highlighted, burnout is the result of prolonged interpersonal stressors at work. Research has shown that burnout is related to reduced performance in the workplace (Ruotsalainen et al., 2015) often leading to several forms of withdrawal, such as absenteeism and intention to leave the job (Alarcon, 2011; Kim and Kao, 2014). To put it in other words, it is the worker's inability or lack of resources to meet with the demands that are associated with the job tasks (Weber and Jaekel-Reinhard, 2000; Maslach et al., 2001; Bianchi et al., 2015a). It has been argued, for instance, that burnout is not only associated with difficulties related to the working environment, but also other factors, such as learned helplessness, learning theory, environmental and/or personality factors (for a review see Kaschka et al., 2011). To quote Bühler's and Land's (2003) question “why under the same working conditions one individual burns out, whereas another shows no symptoms at all?” we need to keep in mind that burnout is in fact a response to stressful events (Cherniss, 1980) and how each individual responds to such events depends on how he/she evaluates them (Sarason, 1972; Lazarus and Folkman, 1984); therefore, a person's reaction to a work stressor might range from minor to significant stimulation. In other words, while there are employees who report that they experience burnout, there are others who do not, although they all work within the same working environment. A possible mechanism that differentiates employees' reaction to a stressful working environment is personality characteristics. Personality can either be a coping mechanism which allows individuals to acquire/conserve resources and protect themselves from deviant behavior (Ghorpade et al., 2007) or it can make someone more susceptible and vulnerable to stressors. Two crucial psychological phenomena which are related with personality, are depression and anxiety. As Middeldorp et al. (2006) mention neuroticism, i.e., emotional instability and proneness to anxiety (Eysenck and Rachman, 2013), and low extraversion are positively correlated with both depression and anxiety. Indeed, emotional stability has been shown to be negatively related to the core component of burnout, i.e., emotional exhaustion, and depersonalization and positively related to personal accomplishment (Ghorpade et al., 2007), whereas extroversion has been found to be negatively related to emotional exhaustion and positively related to personal accomplishment (Ghorpade et al., 2007). That is to say, individuals who are more extroverted and more emotionally stable, are less likely to develop burnout and vice versa. However, the question as to what degree burnout is differentiated from depression and anxiety, or whether they complement each other, remains unanswered; and this question is crucial as burnout might be falsely labeled as depression and/or anxiety disorders, leading to inappropriate treatment techniques.
Burnout and Depression
There is disagreement among researchers who study burnout as to whether there is an overlap between burnout and depression (Bianchi et al., 2015a). As Freudenberger (1974) mentions, people who suffer from burnout look and act as if they were depressed. Indeed, we cannot overlook the fact that some of the burnout symptoms appear to resemble the ones of depression; as it is characterized by anhedonia, i.e., the loss of interest or pleasure, depressed mood, fatigue or loss of energy, impaired concentration, and feelings of worthlessness, decreased or increased appetite, sleep problems (hypersomnia or insomnia) and suicidal ideation (American Psychiatric Association, 2013). However, despite its severity and resemblance to depression characteristics, burnout is not mentioned in DSM-V and still no diagnostic criteria exist for identifying it (Bakusic et al., 2017). It is worth noting that in clinical practice, exhausted employees are being diagnosed with burnout and frequently, in order for the clinicians to proceed with their treatment, they turn to alternative diagnoses like the ones of depression or exhaustion (Kaschka et al., 2011). Yet, the question is still an open one, to what degree can we differentiate burnout from depression and anxiety?
Bianchi and Brisson (2017), for instance, examined to what extent individuals with burnout and depression attribute their feelings to their job. What the researchers found was that the number of the participants who attributed their burnout feelings to their job was proportional to the ones who attributed their depressive symptoms to their job as well, indicating that there might be an overlap between burnout and depression in relation to their antecedents. Many studies have also shown that there is a positive correlation between burnout and depression (Glass and McKnight, 1996; Schaufeli and Enzmann, 1998; Bianchi et al., 2013, 2014, 2015b; Bianchi and Laurent, 2015). Indeed, as Bianchi et al. (2015a) mention in their systematic review, it has been found that inventories that assess burnout, and more specifically the subscale of emotional exhaustion–the core component of burnout–are positively correlated with depressive symptoms (Takai et al., 2009; Bianchi et al., 2013; Ahola et al., 2014). Several researchers have argued that because studies have found a consistent medium to high correlation between the two concepts, this might suggest an overlap and that burnout might not be a distinct psychological phenomenon but a dimension of depression (Bianchi et al., 2015b). Additionally in terms of consequences, in a recent study by Bianchi et al. (2018a) it was observed that both burnout and depression were associated not only with the increased recall of negative words, but also with the decreased recall of positive words. The authors concluded that burnout and depression overlap with each other and this overlap extends also to emotional memory. It is worth noting, and regarding the diagnostic differentiation between burnout and depression, in their review Kaschka et al. (2011) mention that correlations between burnout and depression appear frequently among relevant studies, showing that either there is an overlap between burnout and depression, or burnout probably might be a risk factor of developing depression. As it regards to the similarity of the two constructs at a biological level, in their systematic review, Bakusic et al. (2017) found that burnout and depression appear to share a common biological basis. In particular, according to the researchers', the epigenetics studies so far appear to advocate toward a probable mediator, i.e., DNA methylation, which might act as a biomarker of stress-related mental disorders, such as depression, burnout and chronic stress. Therefore, we can observe that besides the psychological common characteristics these two constructs appear to share, they also seem to share a common biological basis.
On the other hand, not all researchers seem to agree with the above notion. Although burnout and depression appear to share some common features (e.g., loss of energy), several researchers believe that burnout and depression are two separate constructs (Ahola and Hakanen, 2007) and that emotional exhaustion is not related to depression (Schaufeli and Enzmann, 1998). There are quite a few studies which have shown that burnout and depression do not overlap with each other and that burnout is differentiated from depression (Bakker et al., 2000; Schaufeli et al., 2001; Toker and Biron, 2012). Furthermore, one major factor that appears to distinguish burnout from depression is the fact that burnout is work related and situation specific, whereas depression is context free and pervasive (Freudenberger and Richelson, 1980; Maslach et al., 2001; Iacovides et al., 2003). That is, burnout is specifically related to someone's working environment, while depression can show up regardless of the circumstances of the environment (e.g., social or family environment). Nevertheless, it should be noted that this distinction might not be very accurate as depression at its first stages might be domain specific (Rydmark et al., 2006). Thus, it is plausible that depression might start as work-related stress or it might evolve as burnout, as this work-related stress gets stronger.
The existing literature is still inconclusive as to whether burnout and depression are the same or different constructs and, although most of the research studies are cross-sectional, longitudinal studies also provide mixed results (McKnight and Glass, 1995; Hakanen and Schaufeli, 2012). As Bianchi et al. (2015b) note, the aim of most longitudinal studies is not to examine the casual relationship between the two variables, but they are designed in order to predict whether burnout can predict depression or vice versa. All in all, despite the majority of the research studies that examine the relationship between burnout and depression, we are not still able to answer whether the two phenomena are the same or different constructs. By conducting the present meta-analysis, we aim to provide more clarification concerning this relationship. Additionally, by knowing if burnout in its essence falls under the umbrella of depression diagnosis, it would provide valuable information as to whether it should be included in the diagnostic criteria of depression or it should be integrated as a different diagnostic entity.
Burnout and Anxiety
One other factor that appears to be related with burnout, but is not as frequently investigated in relation to it as depression, is anxiety (Sun et al., 2012). Anxiety is a common psychological condition which acts as a protective factor against threatening situations (Cole, 2014). However, prolonged anxiety might result in psychological distress affecting an individual's everyday functioning (Cole, 2014). According to Ahmed et al. (2009), anxiety is “a psychological and physiologic state characterized by cognitive, somatic, emotional, and behavioral components.” Nevertheless, although anxiety is considered a general reaction to threatening situations, it is divided into two related constructs; trait and state anxiety (Turnipseed, 1998). In particular, trait anxiety is an individual's stable characteristic and the degree to which he/she perceives stressful situations as threatening, i.e., a person's proneness to anxiety (Spielberger, 1966). On the other hand, state anxiety is the individual's reaction toward a situation after having appraised it as threatening (Spielberger, 1966). That is, an individual's proneness to anxiety reflects trait anxiety, whereas state anxiety is the reaction after a situation has been appraised as threatening. Some researchers suggest that occupational stress might in fact be a risk factor for anxiety symptoms (DiGiacomo and Adamson, 2001; Sun et al., 2012). For example, in the study of Vasilopoulos (2012) the participants who reported high social anxiety levels reported high burnout levels as well. Additionally, Mark and Smith (2012) found that job demands, extrinsic effort, and over-commitment were associated with increased anxiety levels. Similarly, Ding et al. (2014) found that emotional exhaustion and cynicism were positively related to anxiety symptoms, whereas professional efficacy was negatively related to anxiety symptoms. That is, the more emotionally exhausted, cynical, and less efficient toward his/her work an individual feels, the more anxious he/she will be. Turnipseed (1998) also found that burnout and anxiety symptoms are significantly correlated with each other, with the strongest link existing between anxiety and emotional exhaustion. According to Turnipseed (1998), this interaction between work situations and individuals' personalities –as mentioned earlier– creates a state of anxiety and, by extension, contributes to burnout onset. However, to our knowledge it is still unclear the exact relationship between burnout and anxiety. Specifically, are people with higher trait anxiety more prone to developing burnout or do burnout feelings compound anxiety symptoms? Furthermore, is there an overlap between burnout and anxiety?
Objectives
Overall, the evidence regarding the relation between burnout and depression and burnout and anxiety are still inconclusive. The purpose of this systematic review and meta-analysis is to investigate and clarify the association between the above variables. Our goal is to clarify the existing evidence and have a better understanding of the relationship between burnout and depression and burnout and anxiety.
Research Questions
Our research questions were the following:
Is there an overlap between burnout and depression?
Is there a potential moderator underlying the relationship between burnout and depression?
Is there an overlap between burnout and anxiety?
Is there a potential moderator underlying the relationship between burnout and anxiety?
Methods
Systematic Review Protocol
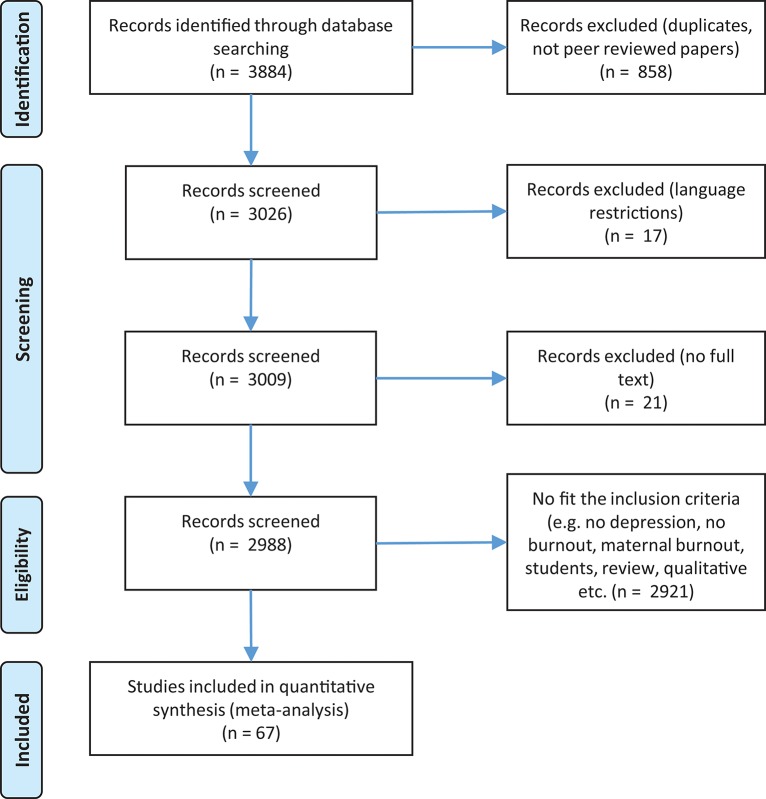
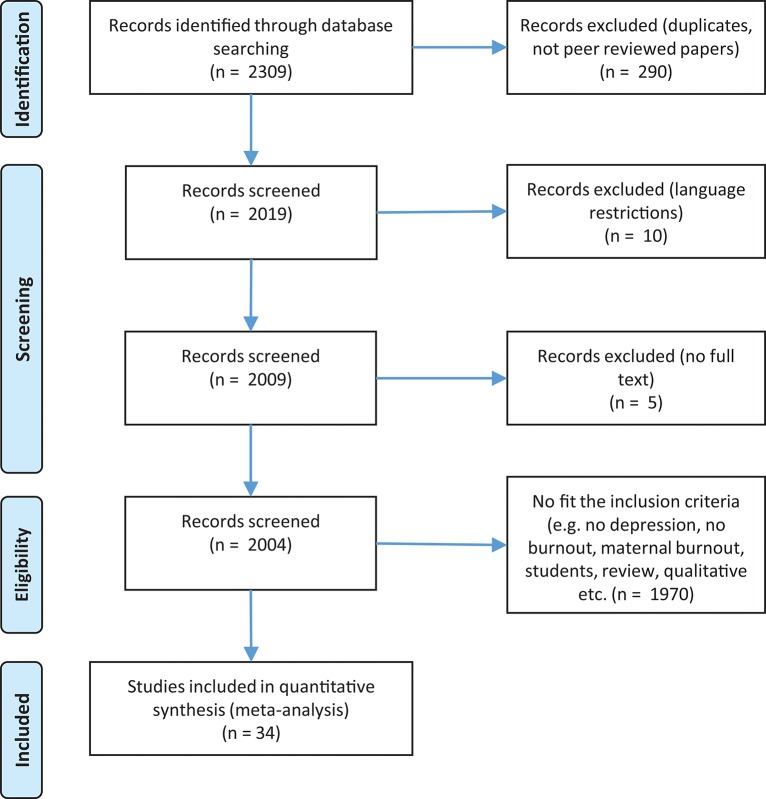
Before we began our database search, firstly we searched PROSPERO's database for possible registered protocol reviews that might have been conducting the same meta-analysis. As no such protocol review was found at PROSPERO's database, we wrote and registered a systematic protocol review in which we stated our purpose with the current meta-analysis, our eligibility criteria and our search strategy. After the registration of our systematic protocol review (CRD42018090505), we continued with the database search. Specifically, selection procedure, study identification, and critical appraisal of the research studies was conducted according to the checklist presented in the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (Moher et al., 2009; see Figures 1, 2), Supplementary Data Sheet S1. For burnout and depression, 67 papers were identified which resulted in 69 studies for analysis. For burnout and anxiety 34 papers were identified which resulted in 36 studies for analysis.
Figure 1.
Flow diagram for burnout and depression.
Figure 2.
Flow diagram for burnout and anxiety.
Search Strategy
We searched the online databases SCOPUS, Web of Science, MEDLINE (PubMed) and Google Scholar for research published between January 2007 and August 2018. The combinations of the key words we used were the following: burnout, depression, anxiety. Additionally, we used MeSH terms with the term “burnout” being the major topic of the meta-analysis and our search was formed as follows: burnout/depression [majr] AND burnout/anxiety [majr]; burnout/depression [majr] OR burnout/anxiety [majr]. After we completed the electronic database search, a manual scoping of the cited studies by all articles found was also done in case some of them did not show up in our search.
Our eligibility criteria included; (i) all types of studies, both cross-sectional and longitudinal, (ii) published and unpublished research articles, (iii) full-text articles, (iv) research articles written in the English language, (v) studies that present the effects sizes of their results and (vi) studies that used reliable research tools. Additionally, all studies had to describe the types of methods they used in order to assess burnout, depression and anxiety. Regarding the type of the populations used in the studies, we included studies that examined employed individuals and professional athletes as well.
Furthermore, we categorized the research studies into five moderators, depending on the type of the assessment tools that were used and the type of the studies (cross-sectional or longitudinal) in which they were utilized. Specifically, and after we conducted frequencies analyses, it was found that the most widely used tools for assessing our variables of interest were the Maslach Burnout Inventory (MBI) (Maslach et al., 2006) for assessing burnout, the Patient Health Questionnaire (PHQ) for assessing depression (Spitzer et al., 1994; Kroenke et al., 2001) and the Hospital Anxiety Depression Scale (HADS) (Zigmond and Snaith, 1983) for assessing anxiety. Consequently, the three moderator variables that were created were: (i) the MBI vs. Non-MBI studies, (ii) the PHQ vs. Non-PHQ studies, and (iii) the HADS vs. Non-HADS studies. The fourth moderator was the type of the study, i.e., cross-sectional or longitudinal. This way we were able to examine whether the assessment tools and/or the type of the studies had different effect on the results or not. Lastly, the fifth moderator was occupation.
Quality Assessment
Quality assessment was performed based on the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (Feng et al., 2014). The tool contains 14 criteria and the evaluator is asked to answer whether the study in question meets the criterion. The possible answers are Yes, No, Cannot Determine, Not applicable, and Not Reported. A score of >11 corresponds to good quality, 7–10 to fair quality and <7 to poor quality. Of the 67 studies measuring burnout and depression that were included in the meta-analysis 28 were rated by two independent evaluators as fair and 40 as good (one paper contained 2 studies - each one of the two studies was evaluated differently). Of the 34 studies measuring burnout and anxiety that were included in the meta-analysis 15 were rated by two independent evaluators as fair and 19 as good.
Analysis
All analyses were guided by Lipsey and Wilson (2001) and conducted using Comprehensive Meta-Analysis software (Lipsey and Wilson, 2001; Borenstein et al., 2005). In deriving effect sizes and confidence intervals, random-effects models were used. Random-effects models assume variation in effect sizes between studies, and this is due to both sampling error and true random variance arising from differences between studies in terms of their procedures and settings (as opposed to only sampling error stipulated in a fixed effect model). In comparison to fixed-effects models, then, random-effects models are generally considered to be preferable and allow generalization beyond the set of studies examined to future studies (Schmidt et al., 2009).
The summary statistic reported is the weighted r. Cohen provided rules of thumb for interpreting these effect sizes, suggesting that an r of 0.10, represents a “small” effect size, 0.30 represents a “medium” effect size and 0.50 represents a “large” effect size (Cohen, 1992). However, researchers have suggested that the indiscriminate use of Cohen's generic small, medium, and large effect size values to characterize effect sizes in domains in which normative values do not apply is inappropriate and misleading (Lipsey et al., 2012). Therefore, it is important that effect sizes are grounded in the context by assessing their contribution to knowledge.
Moderation Analysis
The following moderators were examined as possible reasons for heterogeneity; burnout measure (MBI vs. Non-MBI measurement of burnout), the emotional exhaustion dimension of the MBI vs. the other two dimensions vs. the dimensions of the Non-MBI scales (Emotional exhaustion vs. Non-Emotional exhaustion scales vs. other burnout scales), the depression measure (PHQ vs. Non-PHQ), the anxiety measure (HADS vs. Non-HADS), the type of study (Cross-sectional vs. Longitudinal), the occupational status (Healthcare vs. Educational vs. Other professionals), and their quality as described above (Fair vs. Good quality). The selection of the above measurements as moderators was decided after taking into consideration the frequency in which they were used in the studies.
Moderation was assessed by calculating the degree of inconsistency in the observed relationship across studies (I2). This index is interpreted as the percentage of total variation across studies due to “true” heterogeneity rather than sampling error (Higgins et al., 2003). As I2 increases, the level of true heterogeneity increases (0 to 100%). Values of 25, 50, and 75% have been identified as low, medium, and high levels of heterogeneity.
Results
Studies Retrieved for the Meta-Analysis
As it regards the number of records that were originally identified, concerning burnout, and depression a total of 3,884 records were found. After refining the search results, 3,026 records were screened, 21 of them were excluded as they were not full-texts, 17 were excluded due to language restrictions (non-English), and 2,921 because they didn't fit the inclusion criteria (e.g., no depression, no burnout, maternal burnout, students, review, qualitative etc.) or were excluded because the appropriate statistics were not provided. In total 67 papers (69 studies) were included in the meta-analysis (see Figure 1).
Concerning burnout and anxiety, 2,309 records were identified. After refining the results, 2,019 available records were screened; 10 of them were excluded due to non-use of the English language, 5 were not full-texts and 1,970 were excluded because they didn't fit the inclusion criteria (e.g., no depression, no burnout, maternal burnout, students, review, qualitative etc.) or because the appropriate statistics were not provided. In total 34 papers (36 studies) were eligible for the meta-analysis (see Figure 2).
Study Selection and Characteristics
Tables 1, 2 provide a detailed summary of all the studies that were included in the meta-analysis for both depression and anxiety, respectively. In total 101 studies were included in this review; 67 studies for burnout and depression and 34 studies for burnout and anxiety. Table 3 provides a list of all the questionnaires used in the studies included in the meta-analysis (includes the abbreviations).
Table 1.
Studies measuring burnout and depression included in the meta-analysis (69 studies).
| Studies (in alphabetical order) | n | Burnout measure | Depression measure | Design | |
|---|---|---|---|---|---|
| 1 | Ahola et al., 2014 | 1,964 | MBI-HS | BDI-SF | Longitudinal |
| 2 | Bakir et al., 2010 | 377 | MBI | BDI | Cross-sectional |
| 3 | Bauernhofer et al., 2018 | 103 | MBI-GS | BDI | Cross-sectional |
| 4 | Bianchi and Brisson, 2017 | 468 | SMBM | PHQ9 | Cross-sectional |
| 5 | Bianchi and Laurent, 2015 | 54 | MBI | BDI-II | Cross-sectional |
| 6 | Bianchi and Laurent, 2015 | 54 | BM | BDI-II | Cross-sectional |
| 7 | Bianchi and Schonfeld, 2016 | 323 | SMBM | PHQ9 | Cross-sectional |
| 8 | Bianchi and Schonfeld, 2018 | 911 | MBI-GS | PHQ-8 | Cross-sectional |
| 9 | Bianchi et al., 2013 | 1,658 | MBI | BDI-II | Cross-sectional |
| 10 | Bianchi et al., 2014 | 5,575 | MBI | PHQ-9 | Cross-sectional |
| 11 | Bianchi et al., 2015b | 627 | MBI | PHQ-9 | Longitudinal |
| 12 | Bianchi et al., 2016a | 1,046 | SMBM | PHQ-9 | Cross-sectional |
| 13 | Bianchi et al., 2016b | 184 | SMBM | PHQ-9 | Cross-sectional |
| 14 | Bianchi et al., 2018a | 1,056 | SMBM | PHQ-9 | Cross-sectional |
| 15 | Bianchi et al., 2018b | 222 | SMBM | PHQ-9 | Cross-sectional |
| 16 | Bianchi et al., 2018c | 1,015 | SMBM | PHQ-9 | Cross-sectional |
| 17 | Capone and Petrillo, 2018 | 285 | MBI-GS | CES-D | Cross-sectional |
| 18 | Cardozo et al., 2012 | 212 | MBI-HS | HSCL-25 | Longitudinal |
| 19 | Choi et al., 2018 | 386 | MBI-GS | PHQ | Cross-sectional |
| 20 | Choi et al., 2018 | ProQOL | PHQ | Cross-sectional | |
| 21 | da Silva Valente et al., 2018 | 1,046 | MBI | PHQ-9 | Cross-sectional |
| 22 | De Stefano et al., 2018 | 26 | MBI | BDI | Cross-sectional |
| 23 | Duan-Porter et al., 2018 | 281 | OLBI | PHQ-9 | Longitudinal |
| 24 | Favrod et al., 2018 | 208 | MBI | HADS | Cross-sectional |
| 25 | Fong et al., 2016 | 312 | CBI | HADS | Longitudinal |
| 26 | Garrouste-Orgeas et al., 2015 | 1,534 | MBI | CES-D | Cross-sectional |
| 27 | Grover et al., 2018 | 445 | MBI | PHQ-9 | Cross-sectional |
| 28 | Hakanen et al., 2008 | 2,555 | MBI | BDI | Longitudinal |
| 29 | Hakanen and Schaufeli, 2012 | 1,964 | MBI | BDI | Longitudinal |
| 30 | Hemsworth et al., 2018 | 273 | ProQOL | DASS-21 | Cross-sectional |
| 31 | Hintsa et al., 2014 | 3,283 | MBI-GS | BDI | Cross-sectional |
| 32 | Idris and Dollard, 2014 | 117 | MBI | PHQ-9 | Longitudinal |
| 33 | Johnson et al., 2017 | 323 | MBI | DASS-21 | Cross-sectional |
| 34 | Karaoglu et al., 2015 | 74 | MBI | HADS | Cross-sectional |
| 35 | Lebensohn et al., 2013 | 168 | MBI | CES-D | Cross-sectional |
| 36 | Lee et al., 2018 | 464 | MBI-GS | HADS | Cross-sectional |
| 37 | Lobo, 2018 | 10 | MBI | HADS | Cross-sectional |
| 38 | Malmberg-Gavelin et al., 2018 | 119 | SMBQ | HADS | Cross-sectional |
| 39 | Mather et al., 2016 | 5,093 | PBM | SCID | Cross-sectional |
| 40 | Melchers et al., 2015 | 944 | MBI-GS | BDI-II | Cross-sectional |
| 41 | Metlaine et al., 2018 | 140 | MBI | HADS | Cross-sectional |
| 42 | Moore and Schellinger, 2018 | 62 | PQLS | CES-D | Cross-sectional |
| 43 | Mosing et al., 2018 | 10,120 | MBI-GS | SCL-90 | Cross-sectional |
| 44 | Mutkins et al., 2011 | 80 | MBI | DASS-21 | Cross-sectional |
| 45 | Oe et al., 2018 | 158 | MBI | HADS | Cross-sectional |
| 46 | Penz et al., 2018 | 412 | MBI | PHQ-9 | Cross-sectional |
| 47 | Pereira-Lima and Loureiro, 2015 | 400 | BSI | PHQ-4 | Cross-sectional |
| 48 | Peterson et al., 2008 | 3,719 | OLBI | HADS | Cross-sectional |
| 49 | Plieger et al., 2015 | 755 | MBI-GS | BDI-II | Cross-sectional |
| 50 | Richardson et al., 2018 | 119 | CBI | IDAS-II | Cross-sectional |
| 51 | Rogers et al., 2014 | 349 | CBI | PHQ | Cross-sectional |
| 52 | Samios, 2017 | 69 | ProQOL | DASS-21 | Cross-sectional |
| 53 | Santa Maria et al., 2018 | 811 | CBI | PHQ-2 | Cross-sectional |
| 54 | Schiller et al., 2018 | 51 | SMBM | HADS | Cross-sectional |
| 55 | Schonfeld and Bianchi, 2016 | 1,386 | SMBM | PHQ-9 | Cross-sectional |
| 56 | Silva et al., 2018 | 100 | BSI | PHQ-9 | Cross-sectional |
| 57 | Steinhardt et al., 2011 | 267 | MBI | CES-D | Cross-sectional |
| 58 | Takai et al., 2009 | 84 | PBM | BDI-II | Cross-sectional |
| 59 | Talih et al., 2016 | 118 | BM | PHQ-9 | Cross-sectional |
| 60 | Talih et al., 2018 | 91 | BM | PHQ-9 | Cross-sectional |
| 61 | Toker and Biron, 2012 | 1,632 | SMBM | PHQ | Longitudinal |
| 62 | Tourigny et al., 2010 | 550 | MBI | CES-D | Cross-sectional |
| 63 | Trockel et al., 2018 | 250 | PFI | PROMIS | Cross-sectional |
| 64 | Tzeletopoulou et al., 2018 | 72 | MBI | CES-D | Cross-sectional |
| 65 | van Dam, 2016 | 113 | MBI | SCL-90 | Cross-sectional |
| 66 | Vasconcelos et al., 2018 | 91 | MBI-HS | BDI | Cross-sectional |
| 67 | Weigl et al., 2016 | 313 | MBI | STDS | Cross-sectional |
| 68 | Wurm et al., 2016 | 5,897 | HBI | MDI | Cross-sectional |
| 69 | Yeh et al., 2018 | 172 | OBI | EPDS | Cross-sectional |
Table 2.
Studies measuring burnout and anxiety included in the meta-analysis (36 studies).
| Studies (in alphabetical order) | n | Burnout measure | Depression measure | Design | |
|---|---|---|---|---|---|
| 1 | Andreassen et al., 2018 | 988 | MBI-GS | GHQ-28 | Cross-sectional |
| 2 | Bianchi and Laurent, 2015 | 54 | MBI | HADS | Cross-sectional |
| 3 | Bianchi and Laurent, 2015 | 54 | BM | HADS | Cross-sectional |
| 4 | Bianchi and Schonfeld, 2018 | 911 | MBI-GS | Self-constr. | Cross-sectional |
| 5 | Cardozo et al., 2012 | 212 | MBI-HS | HSCL-25 | Longitudinal |
| 6 | Choi et al., 2018 | 386 | MBI-GS | GAD-7 | Cross-sectional |
| 7 | Choi et al., 2018 | 386 | ProQOL | GAD-7 | Cross-sectional |
| 8 | Craiovan, 2015 | 60 | CBI | HAM-A | Cross-sectional |
| 9 | De Stefano et al., 2018 | 26 | MBI | STAI | Cross-sectional |
| 10 | Demir, 2018 | 335 | BSI-SV | IPIP | Cross-sectional |
| 11 | Diestel and Schmidt, 2010 | 324 | MBI | STAI | Cross-sectional |
| 12 | Ding et al., 2014 | 1,243 | MBI-GS | SAS | Cross-sectional |
| 13 | Favrod et al., 2018 | 208 | MBI | HADS | Cross-sectional |
| 14 | Gallego-Alberto et al., 2018 | 101 | MBI | POMS | Cross-sectional |
| 15 | Gillet et al., 2018 | 521 | SMBM | JAS | Cross-sectional |
| 16 | Hemsworth et al., 2018 | 273 | ProQOL | DASS-21 | Cross-sectional |
| 17 | Karaoglu et al., 2015 | 74 | MBI | HADS | Cross-sectional |
| 18 | Katkat, 2015 | 336 | MBI | SSAI | Cross-sectional |
| 19 | Lee et al., 2018 | 464 | MBI-GS | HADS | Cross-sectional |
| 20 | Lobo, 2018 | 10 | MBI | HADS | Cross-sectional |
| 21 | Malmberg-Gavelin et al., 2018 | 119 | SMBQ | HADS | Cross-sectional |
| 22 | Mather et al., 2016 | 5,093 | PBM | SCID | Cross-sectional |
| 23 | Metlaine et al., 2018 | 140 | MBI | HADS | Cross-sectional |
| 24 | Mutkins et al., 2011 | 80 | MBI | DASS-21 | Cross-sectional |
| 25 | Oe et al., 2018 | 158 | MBI | HADS | Cross-sectional |
| 26 | Pereira-Lima and Loureiro, 2015 | 400 | BSI | PHQ-4 | Cross-sectional |
| 27 | Peterson et al., 2008 | 3,719 | OLBI | HADS | Cross-sectional |
| 28 | Schiller et al., 2018 | 51 | SMBM | HADS | Cross-sectional |
| 29 | Shi et al., 2018 | 696 | MBI-GS | Self-constr. | Cross-sectional |
| 30 | Talih et al., 2016 | 118 | BM | GAD-7 | Cross-sectional |
| 31 | Talih et al., 2018 | 91 | BM | GAD-7 | Cross-sectional |
| 32 | Trockel et al., 2018 | 250 | PFI | PROMIS | Cross-sectional |
| 33 | van Dam, 2016 | 113 | MBI | SCL-90 | Cross-sectional |
| 34 | Yazicioglu and Kizanlikli, 2019 | 284 | MBI | STAI | Cross-sectional |
| 35 | Zhou et al., 2016 | 1,274 | MBI | SAS | Cross-sectional |
| 36 | Zhou et al., 2018 | 1,354 | MBI | SAS | Cross-sectional |
Table 3.
Questionnaires used for measuring burnout, depression and anxiety in the studies included in the meta-analysis.
| Short name | Name |
|---|---|
| BURNOUT | |
| BSI | Burnout Syndrome Inventory |
| CBI | Copenhagen Burnout Inventory |
| HBI | Hamburg Burnout Inventory |
| MBI | Maslach Burnout Inventory |
| OBI | Occupational Burnout Inventory |
| OLBI | Oldenburg Burnout Inventory |
| PBM | Pines Burnout Measure |
| PFI | Professional Fulfillment Index |
| PQLS | Professional Quality of Life Scale |
| ProQOL | Professional Quality of Life |
| SMBM | Shirom–Melamed Burnout Measure |
| SMBQ | Shirom-Melamed Burnout Questionnaire |
| DEPRESSION | |
| BDI | Beck Depression Inventory |
| CES-D | Center for Epidemiologic Studies Depression Scale |
| DASS-21 | Depression Anxiety Stress Scales |
| EDPS | Edinburgh Postnatal Depression Scale |
| HADS | Hospital Anxiety and Depression Scale |
| HSCL-25 | Hopkins Symptom Checklist-25 |
| IDAS-II | Inventory of Depression and Anxiety Symptoms-II |
| MDI | Major Depression Inventory |
| PHQ | Patient Health Questionnaire |
| PROMIS | Patient-Reported Outcomes Measurement Information System |
| SCID | Structured Clinical Interview for DSM-IV Disorders |
| SCL-90 | Symptom Checklist |
| STDS | State-TraitDepressionScales |
| ANXIETY | |
| – | 1 Item Self-Constructed |
| DASS-21 | Depression Anxiety Stress Scales |
| GAD-7 | Generalized Anxiety Disorder-7 |
| GHQ-28 | General Health Questionnaire-28 |
| HADS | Hospital Anxiety and Depression Scale |
| HAM-A | Hamilton Anxiety Rating Scale |
| HSCL-25 | Hopkins Symptom Checklist-25 |
| IPIP | International Personality Item Pool |
| JAS | Job-Anxiety-Scale |
| PHQ-4 | Patient Health Questionnaire-4 |
| POMS | Profile of Moods State |
| PROMIS | Patient-Reported Outcomes Measurement Information System |
| SAS | Zung Self-Rating Anxiety Scale |
| SCID | Structured Clinical Interview for DSM-IV Disorders |
| SCL-90 | Symptom Checklist |
| SSAI | Spielberger State Anxiety Inventory |
| STAI | State and Trait Anxiety Scales |
Concerning the publication year of the studies about burnout and depression, 43.3% of them were published during 2018 (until August), followed by 13.4% of them which were published in 2016 and 11.9% in 2015; 7.5% of the studies were published in 2014, 5.6% in 2017, 4.5% in 2012, 15.6% were published in each of the following years: 2008, 2010, 2011, and 2013 (3.9% each), and 1.5% in 2009. In relation to publication year of the studies about burnout and anxiety, 52.9% were published in 2018 (until August), 11.8% studies were published in 2015, 11.8% in 2016, 5.8% in 2014 and 5.8% 2017; 11.6% were published during the years of 2007, 2010, 2011, and 2012 (2.9% each).
Regarding the studies relating to burnout and depression, the overall sample size for the 67 studies was 84,169 participants, 30,942 (37%) men, and 49,898 (59%) women (three studies did not include gender characteristics). Of the studies that measured burnout, 55% of them used the MBI and variations of it (i.e., MBI-GS, MBI-HS), 14.5% used the SMBM test, 5.8% used the CBI test, 4.3% used the BM, and 4.3% the ProQOL tests, 8.7% of them used the BSI, the OLBI and the PBM tests, and 7% used other measures of burnout (HBI, OBI, PFI, PQLS, and SMBQ); in two studies burnout was measured with two tests, MBI and PBM and MBI and ProQOL test.
Most of the studies (36.1%) used the PHQ to measure depression, 20.2 % of them used the BDI, 14.5% used the HADS, another 10.1% of the studies used the CES-D, 5.8% used the DASS-21, 2.9% used the SCL-90 and, lastly, 1.4% used the EPDS, HSCL-25, IDAS-II, MDI, PROMIS, SCID, and STDS tests.
Respectively, in the studies relating to burnout and anxiety, the overall sample size for the 34 studies were 40,751 participants, 15,561 (38%) were men, and 23,915 (59%) were women (in two studies gender characteristics were not included). Concerning the burnout tool which was used across the studies, 63.9% of them used the MBI test and its variations (i.e., MBI-GS, MBI-HS), 8.3% used the BM test, 5.6% used the BSI, ProQOL and SMBM tests and 2.8% used the BSI, CBI, OLBI, PBM, PFI, and SMBQ tests. In two studies burnout was measured with two tests, MBI and PBM, and MBI and ProQOL test.
In relation to the measurement of anxiety, 30.6% of the studies used the HADS, 11.1% used the GAD-7, 8.3% used the STAI and the SAS, 5.6% of the studies used the DASS-21 and 1-item self-constructed test, and 2.8% of the studies used the GHQ-28, HAM-A, HSCL-25, IPIP, JAS, PHQ-4, POMS, PROMIS, SCID, SCL-90, and SSAI tests.
Concerning the design of the studies, 87% of them examining the burnout and depression relationship utilized a cross-sectional design, and 13% were longitudinal; 97.2% of the studies measuring burnout and anxiety utilized a cross-sectional design and 2.8% were longitudinal.
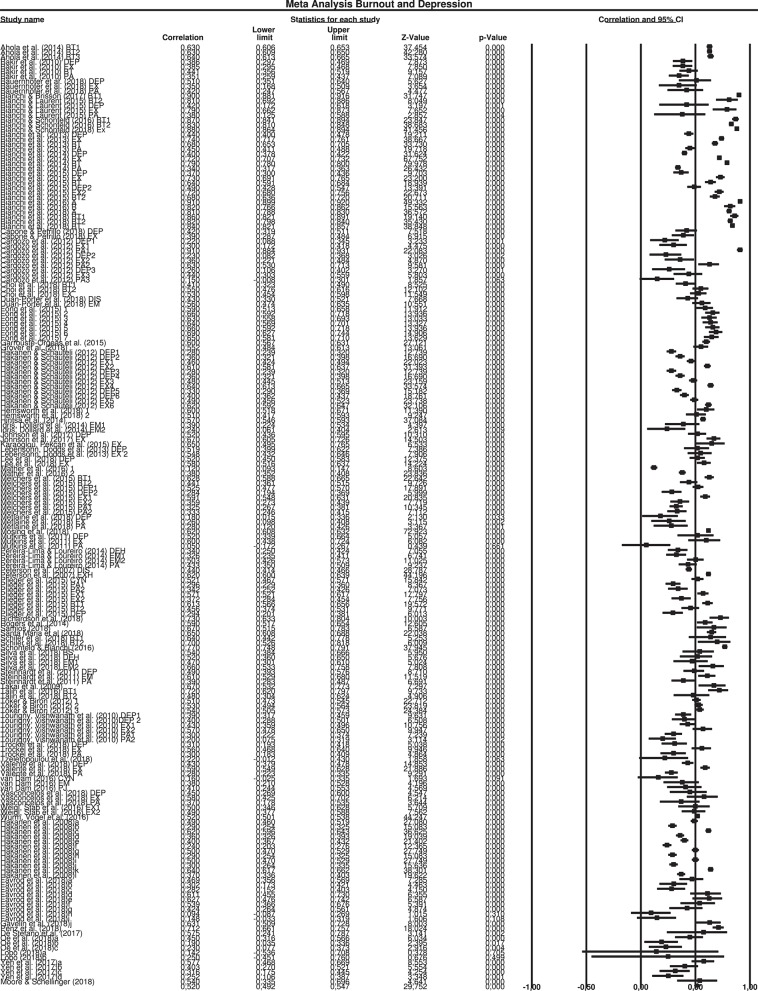
Main Meta-Analysis: Association Between Burnout and Depression
Overall results indicated a significant effect (r = 0.520, SE = 0.012, 95% CI = 0.492, 0.547). The confidence intervals around the effect sizes for each study are presented in the forest plot (see Figure 3).
Figure 3.
Meta analysis burnout and depression.
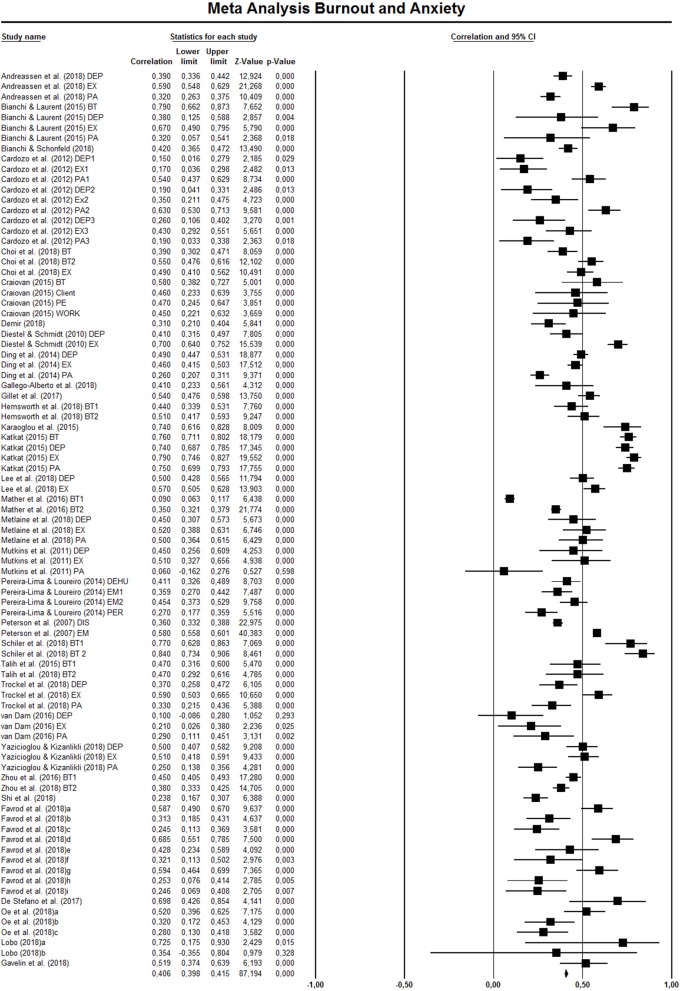
Main Meta-Analysis: Association Between Burnout and Anxiety
Overall results indicated a significant effect (r = 0.460, SE = 0.014, 95% CI = 0.421, 0.497). The confidence intervals around the effect sizes for each study are presented in the forest plot (see Figure 4).
Figure 4.
Meta analysis burnout and anxiety.
Sub-group Analysis: Measure and Context
The meta-analysis indicated significant heterogeneity with the I-squared = 98.432 and I-squared = 95.367 for both depression and anxiety respectively, suggesting that moderation analysis was appropriate.
In terms of context, the depression studies that used the MBI reported lower effect sizes (r = 0.472, SE = 0.011, 95% CI = 0.441, 0.503) in comparison with other scales (r = 0.622, SE = 0.042, 95% CI = 0.564, 0.675). Likewise, anxiety studies that used the MBI reported slightly lower effect sizes as well (r = 0.451, SE = 0.011, 95% CI = 0.406, 0.493) in comparison with other scales (r = 0.482, SE = 0.029, 95% CI = 0.408, 0.549).
Concerning the burnout dimension, in the burnout—depression relationship the effect sizes of the emotional exhaustion dimension were higher (r = 0.508, SE = 0.012, 95% CI = 0.467, 0.546) comparing to the other dimensions of the MBI test (r = 0.409, SE = 0.006, 95% CI = 0.380, 0.437), but lower compared to the other burnout measurements that report total burnout scores (r = 0.749, SE = 0.136, 95% CI = 0.643, 0.827) and those that report scores from individual subscales (r = 0.608, SE = 0.005, 95% CI = 0.574, 0.639). With respect to the burnout—anxiety relationship, the effect sizes of the emotional exhaustion dimension were slightly higher (r = 0.472, SE = 0.012, 95% CI = 0.417, 0.524), compared to the other dimensions of the MBI test (r = 0.426, SE = 0.017, 95% CI = 0.369, 0.479) and slightly lower compared to the other burnout measurements that report total scores (r = 0.494, SE = 0.060, 95% CI = 0.318, 0.637) and those that report scores from individual subscales (r = 0.499, SE = 0.052, 95% CI = 0.379, 0.602).
Additionally, the studies that used the PHQ scale reported higher effect sizes (r = 0.628, SE = 0.040, 95% CI = 0.565, 0.684) in comparison with other scales (r = 0.481, SE = 0.009, 95% CI = 0.453, 0.507). Likewise, in relation to anxiety, studies that used the HADS scale reported higher effect sizes as well (r = 0.507, SE = 0.023, 95% CI = 0.448, 0.562) in comparison with other scales (r = 0.437, SE = 0.016, 95% CI = 0.387, 0.484).
With respect to the design of the studies (cross-sectional or longitudinal), concerning the burnout—depression relationship, the cross-sectional studies reported higher effect sizes (r = 0.526, SE = 0.022, 95% CI = 0.488, 0.562) comparing to the longitudinal ones (r = 0.505, SE = 0.009, 95% CI = 0.466, 0.543). Concerning the burnout—anxiety relationship, sub-group analysis regarding the design of the studies was not conducted as there was only one longitudinal study in the meta-analysis.
As it regards the occupational status, and specifically the burnout—depression relationship, educational staff reported higher effect sizes (r = 0.679, SE = 0.049, 95% CI = 0.609, 0.738) comparing to healthcare workers (r = 0.495, SE = 0.008, 95% CI = 0.466, 0.524) and the general employed population (r = 0.449, SE = 0.020, 95% CI = 0.399, 0.496). Regarding the burnout—anxiety relationship, healthcare professionals reported slightly lower effect sizes (r = 0.436, SE = 0.010, 95% CI = 0.396, 0.475) comparing to the general employed population (r = 0.492, SE = 0.035, 95% CI = 0.418, 0.559). Sub-group analysis with the educational staff was not conducted as there were only two studies in which the participants fitted in the occupational status.
Lastly, with respect to the quality of the studies (see section Quality Assessment), concerning the burnout—depression relationship, the studies with fair quality reported slightly higher effect sizes (r = 0.565, SE = 0.032, 95% CI = 0.515, 0.610) comparing to the good quality studies (r = 0.488, SE = 0.009, 95% CI = 0.456, 0.518). Concerning the burnout—anxiety relationship, the studies with fair quality reported slightly higher effect sizes (r = 0.466, SE = 0.009, 95% CI = 0.418, 0.511) comparing to the good quality studies (r = 0.453, SE = 0.018, 95% CI = 0.402, 0.502).
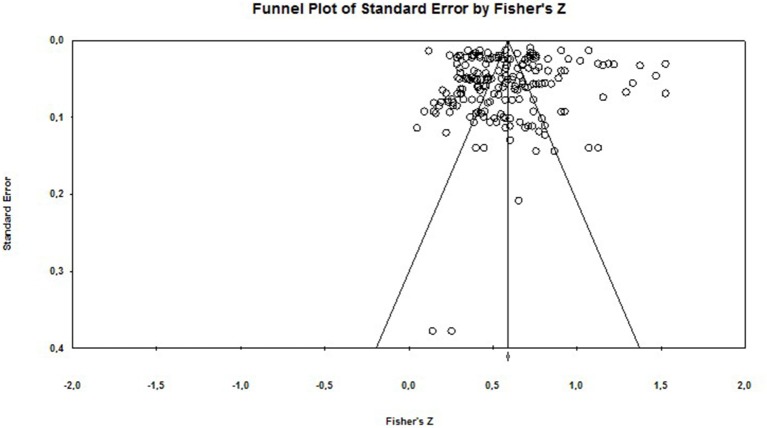
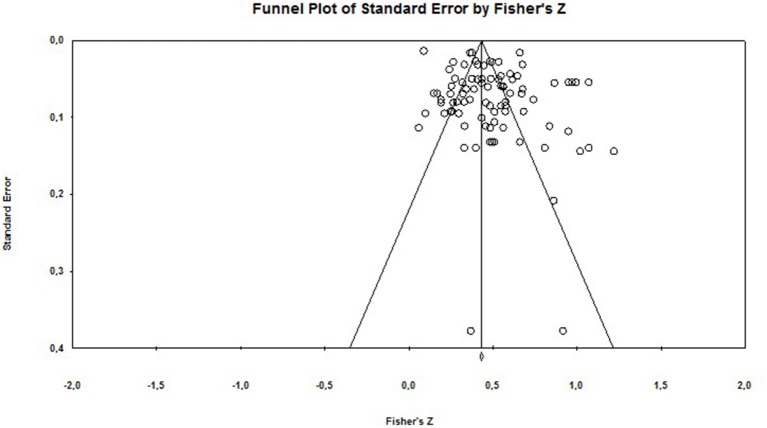
Publication Bias
In order to assess publication bias (the “file-drawer” problem) we adopted a number of strategies. We examined the fail-safe number (fail-safe N) for each effect size. We also inspected funnel plots (a scatterplot of effect sizes against the reciprocal of its standard error).
Rosenthal (1979) recommends that the fail-safe number should be >5 k + 10, where k equals the number of observed effect sizes (Rosenthal, 1979). In the present analysis the classic fail-safe N is 8,603 and 5,932 for the burnout—depression relationship and the burnout—anxiety relationships, respectively. Rosenthal's method has been critiqued on the grounds that it fails to take into account the bias in the “file drawer” of unpublished studies, and thus can give misleading results (Scargle, 1999). Therefore, we also calculated Orwin's fail-safe N, which was equal to 944 (depression) and 288 (anxiety) (using 0.10 as a criterion for a trivial correlation).
In terms of publication bias, the funnel plots (see Figures 5, 6) indicate a degree of asymmetry. However, funnel plots are not a good way to investigate publication bias per se, as there can be a number of reasons for asymmetrical funnel plots (also called small study effects), which are due to heterogeneity, reporting bias and poor methodological design (Sterne et al., 2011; Sedgwick, 2013).
Figure 5.
Funnel plot of Standard Error for burnout and depression.
Figure 6.
Funnel plot of Standard Error for burnout and anxiety.
Discussion
Summary of Main Findings
During the last decade, research regarding the relationship of burnout and depression, and burnout and anxiety, has grown. As we observed from our database search on the studies that measure the aforementioned relationships, the research in this field of area has increased in recent years, with the majority of the studies being conducted during the last year (43.5 and 52.8% for the burnout—depression and burnout—anxiety relationships, respectively). The interest on clarifying these relationships appears to be growing stronger and by conducting the present meta-analysis we wanted to clarify whether there is an overlap between burnout and depression, and an overlap between burnout and anxiety. Overall, burnout research is growing—particularly when it comes to small-scale occupational studies, but the research tends to be varied, and applies a range of different instruments to measure burnout (Eurofound, 2018). It is possible that employees who have been diagnosed with a depressive and/or an anxiety disorder might also suffer from burnout (Eurofound, 2018). Indicatively, Maske et al. (2016) found that 59% of individuals who have been diagnosed with burnout they were also diagnosed with an anxiety disorder, 58% with an affective disorder, i.e., depression or a depressive episode and 27% with a somatoform disorder. In other words, the similarities between burnout and depression and burnout and anxiety might lead to false diagnosis or it is possible that burnout might be overlooked on the account of these similarities, resulting in false treatments of the individuals who suffer from it.
Regarding the burnout-depression relationship, i.e., whether there is an overlap between burnout and depression, the results of our meta-analysis showed that there is an association between these two variables. Although burnout and depression are associated with each other, the effect size is not so strong that it would suggest they are the same construct. In other words, burnout and depression are more likely to be two different constructs rather than one. Additionally, as the MBI test was the one which was used in more of the half of the studies (55.1%), we examined the burnout–depression relationship in terms of context. According to our results, the studies that used the MBI test reported a lower association between burnout and depression compared to the studies that used other burnout measures, where the association between burnout and depression was higher.
Concerning the burnout—anxiety relationship, i.e., whether there is an overlap between burnout and anxiety, our results indicated a relationship between the two variables as well. In particular, although there appears to be an association between burnout and anxiety, this association is not so strong that it indicates an overlap between the two variables. This result indicates that although burnout is associated with anxiety, they are in fact different constructs. This finding can help us also answer the question of why some people develop burnout while others do not (Bühler and Land, 2003). According to our results, it is possible that individuals who are more prone to experiencing higher levels of anxiety (trait anxiety) are also more likely to develop burnout as well. As it regards the burnout-anxiety relationship in terms of context, likewise with the burnout-depression relationship, we found that in the studies that used the MBI test (63.9%) the effect between burnout and anxiety was lower compared to the ones that used a different burnout measure. However, it should be noted that there was variability in the inventories that were used in the research studies for assessing anxiety. It is possible that the effect sizes between burnout and anxiety would differ if there was a common widely used tool for assessing anxiety.
Overall, our results suggest that the studies that used measures other than the MBI burnout tool could potentially be artificially inflating the association between burnout and depression and burnout and anxiety as well. Burnout is an occupationally-specific dysphoria that is distinct from depression as a broadly based mental illness (Maslach et al., 2001). Maslach and Leiter (2016) have argued that while studies confirm that burnout and depression are not independent, claiming that they are simply the same mental illness is not supported by the accumulated evidence.
Another interesting finding of our meta-analysis was that the majority of the research studies that measured the relationship between burnout and depression, and burnout and anxiety, utilized cross- sectional designs (87% and 97% of the studies for depression and anxiety respectively).We noticed that there was a lack of longitudinal designs examining the burnout–depression and the burnout—anxiety relationship. Moreover, most of the longitudinal designs that were eligible for our meta-analysis did not examine directly the association between these two relationships, but they were focused mostly on whether burnout predicts depression or anxiety, or the opposite. As Bianchi et al. (2015b) aptly note, most longitudinal studies are not designed to examine casual relationships, but they mainly aim to investigate whether burnout can predict depression or vice versa. Therefore, although the burnout—depression and the burnout—anxiety relationships are found to be related, we are still not able to know whether these relationships are casual. Future studies need to focus more on utilizing longitudinal designs which will mostly aim at examining the causality of these relationships.
Overall, according to our results burnout and depression and burnout and anxiety appear to be different constructs that share some common characteristics and they probably develop in tandem, rather they fall into the same category with different names being used to describe them. However, further studies examining the psychosocial and neurobiological basis of these constructs are needed as well as their relationship with other illnesses (e.g., physical problems), as this field of research area is under investigated (Kaschka et al., 2011). It is worth noting that in their review Kaschka et al. (2011) mention that there appears to be a connection between burnout and cardiovascular musculoskeletal and cutaneous diseases and even with type II diabetes mellitus; and as burnout increases, the somatic co-morbidity appear to increase as well. Interestingly, a meta-analysis by Salvagioni et al. (2017) showed that burnout is a predictor of 12 somatic diseases, among which are; coronary heart disease, headaches, respiratory diseases and mortality under the age of 45 years old. Consequently, we can understand that burnout can have multifactorial psychological and somatic effects upon individuals.
Another field of research area, that would contribute further to the clarification of the association of these constructs, is the biological studies examining the neurobiological mechanisms behind burnout, depression, and anxiety. To this date such studies are scarce, however, researchers that have examined burnout, depression and anxiety at a biological level showed that these constructs appear to be similar. In particular, Korczak et al. (2010) found that neuroendocrine changes in individuals who suffer from burnout do not differ from the ones that suffer from depression or other stress related disorders; a finding that seems to be in accordance with Bakusic et al. (2017) review, as the authors suggest that burnout and depression share a common biological basis. Nevertheless, according to our meta-analysis results, burnout and depression and burnout and anxiety appear to be different rather the same constructs. These findings appear to be very crucial regarding medical diagnosis. Interestingly, only two European countries, i.e., Italy and Latvia, have recognized and classified burnout as an “occupational disease” (Eurofound, 2018), by distinguishing burnout from depression and anxiety, this will lead to more optimized practical implications to all experts who study burnout and work-stressors in general, and build more focused treatment plans.
All in all, we believe that our meta-analysis findings have helped toward the clarification of the relationship between burnout and depression, and burnout and anxiety. Additionally, another finding that emerged is that further studies need to be conducted which will be focusing on these two relationships and their behavioral, psychosomatic, and biological patterns as well. The findings of these studies will lead to the elucidation of the relationship of these constructs. Furthermore, it is worth mentioning that according to Eurofound (2018), during the past decade only a few countries across Europe have conducted surveys which focus exclusively on burnout and other European countries have mainly examined burnout related constructs, such as work stress and/or work-related exhaustion. Hence, we can realize that, besides the growing interest regarding the examination of both occupational work stressors and exhaustion and the clarification between burnout and depression and burnout and anxiety, more relevant studies are still lacking.
Limitations
Our meta-analysis has some limitations. Firstly, we searched only for research studies that were conducted during the past decade. We cannot be certain if our results would be different if we were to include earlier studies as well. A second limitation is that the studies that did not provide appropriate statistical results were not included in the meta-analysis, therefore, again, we cannot be certain whether the inclusion of these studies would change our results. The problems of finding appropriate data to conduct analyses and the reluctance/inability of authors to provide such data when directly contacted has been identified within the literature as a significant barrier to conducting comprehensive meta-analysis (Hardwicke and Ioannidis, 2018). Lastly, a third limitation of our meta- analysis is that, although our database search was conducted through four well–known databases, we still cannot be certain whether all the studies that examined the burnout–depression and burnout–anxiety relationships are reported; a limitation which is also known as the “file–drawer problem” (Rosenthal, 1979). That is, we are not able to know if/and to what extent there was a selective publication bias and whether there were studies that remained unpublished due to non–statistically significant results. Hence, it is possible that studies in which these two relationships were examined but did not provide statistically significant results remained unpublished and, therefore, they were not included in our meta-analysis.
Conclusions
In conclusion, our results showed that while there is statistical relationship between burnout and depression and burnout and anxiety, and while they are interconnected, they are not the same constructs. However, future studies examining these two relationships are still required in order to be able to draw safer conclusions. More longitudinal studies that focus on the causality of the burnout-depression and burnout—anxiety relationships are needed, as they will be able to clarify these two relationships. By conducting this meta-analysis, we aimed to examine the association between burnout and depression and burnout and anxiety. With our results we hope to inform potential effective interventions for treating burnout symptoms; by knowing the nature of a problem this can lead to more targeted solutions.
The modern workplace is characterized by significant proportions of people who feel exhausted, suffer from health problems, may be taking antidepressants or other medication, which can all contribute to feelings of diminished efficacy. The confluence of the aforementioned highlights the importance of clarifying the relationship between burnout and depression/anxiety, so as to avoid a one-dimensional approach to worker well-being.
Author Contributions
PK developed and designed the methodology, conducted data collection, applied statistical techniques to analyze and synthesize the study data, prepared the published work, specifically writing the initial draft and acquired the financial support for the project leading to this publication. AM formulated the research goals and aims, developed and designed the methodology, applied statistical techniques to analyze and synthesize the study data, provided the analysis tool and prepared the published work, specifically with critical reviews, editing, and revisions. KG conducted data collection, applied statistical techniques to analyze and synthesize study data and prepared the published work, specifically with critical reviews, editing and revisions.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This research is co-financed by Greece and the European Union (European Social Fund- ESF) through the Operational Programme Human Resources Development, Education and Lifelong Learning in the context of the project Strengthening Human Resources Research Potential via Doctorate Research (MIS-5000432), implemented by the State Scholarships Foundation (IKY).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2019.00284/full#supplementary-material
References
- Ahmed I., Banu H., Al-Fageer R., Al-Suwaidi R. (2009). Cognitive emotions: depression and anxiety in medical students and staff. J. Crit. Care 24, e1–e7. 10.1016/j.jcrc.2009.06.003 [DOI] [PubMed] [Google Scholar]
- Ahola K., Hakanen J. (2007). Job strain, burnout, and depressive symptoms: a prospective study among dentists. J. Affect. Disord. 104, 103–110. 10.1016/j.jad.2007.03.004 [DOI] [PubMed] [Google Scholar]
- Ahola K., Hakanen J., Perhoniemi R., Mutanen P. (2014). Relationship between burnout and depressive symptoms: a study using the person-centred approach. Burnout Res. 1, 29–37. 10.1016/j.burn.2014.03.003 [DOI] [Google Scholar]
- Alarcon G. M. (2011). A meta-analysis of burnout with job demands, resources, and attitudes. J. Vocation. Behav. 79, 549–562. 10.1016/j.jvb.2011.03.007 [DOI] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, DC: American Psychiatric Pub. [Google Scholar]
- Andreassen C. S., Pallesen S., Torsheim T. (2018). Workaholism as a mediator between work-related stressors and health outcomes. Int. J. Environ. Res. Public Health 15:73. 10.3390/ijerph15010073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakir B., Ozer M., Ozcan C. T., Cetin M., Fedai T. (2010). The association between burnout, and depressive symptoms in a Turkish military nurse sample. Bull. Clin. Psychopharmacol. 20, 160–163. 10.1080/10177833.2010.11790651 [DOI] [Google Scholar]
- Bakker A. B., Schaufeli W. B., Demerouti E., Janssen P. P., Van Der Hulst R., Brouwer J. (2000). Using equity theory to examine the difference between burnout and depression. Anxiety Stress Coping 13, 247–268. [Google Scholar]
- Bakusic J., Schaufeli W., Claes S., Godderis L. (2017). Stress, burnout and depression:A systematic review on DNA methylation mechanisms. J. Psychosom. Res. 92, 34–44. 10.1016/j.jpsychores.2016.11.005 [DOI] [PubMed] [Google Scholar]
- Bauernhofer K., Bassa D., Canazei M., Jiménez P., Paechter M., Papousek I., Weiss E. M. (2018). Subtypes in clinical burnout patients enrolled in an employee rehabilitation program: differences in burnout profiles, depression, and recovery/resources-stress balance. BMC Psychiatry 18:10. 10.1186/s12888-018-1589-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianchi R., Boffy C., Hingray C., Truchot D., Laurent E. (2013). Comparative symptomatology of burnout and depression. J. Health Psychol. 18, 782–787. 10.1177/1359105313481079 [DOI] [PubMed] [Google Scholar]
- Bianchi R., Brisson R. (2017). Burnout and depression: causal attributions and construct overlap. J. Health Psychol. 10.1177/1359105317740415. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Bianchi R., Laurent E. (2015). Emotional information processing in depression and burnout: an eye-tracking study. Eur. Arch. Psychiatry Clin. Neurosci. 265, 27–34. 10.1007/s00406-014-0549-x [DOI] [PubMed] [Google Scholar]
- Bianchi R., Laurent E., Schonfeld I. S., Bietti L. M., Mayor E. (2018a). Memory bias toward emotional information in burnout and depression. J. Health Psychol. 10.1177/1359105318765621. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Bianchi R., Laurent E., Schonfeld I. S., Verkuilen J., Berna C. (2018c). Interpretation bias toward ambiguous information in burnout and depression. Pers. Indiv. Differ. 135, 216–221. 10.1016/j.paid.2018.07.028 [DOI] [Google Scholar]
- Bianchi R., Rolland J.-P., & Salgado J. F. (2018b). Burnout, depression, and borderline personality: A 1,163-participant study. Front. Psychol. 8:2336. 10.3389/fpsyg.2017.02336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianchi R., Schonfeld I. S. (2016). Burnout is associated with a depressive cognitive style. Pers. Individ. Dif. 100, 1–5. 10.1016/j.paid.2016.01.008 [DOI] [Google Scholar]
- Bianchi R., Schonfeld I. S. (2018). Burnout-depression overlap: Nomological network examination and factor-analytic approach. Scand. J. Psychol. 59, 532–539. 10.1111/sjop.12460 [DOI] [PubMed] [Google Scholar]
- Bianchi R., Schonfeld I. S., Laurent E. (2014). Is burnout a depressive disorder? A reexamination with special focus on atypical depression. Int. J. Stress Manage. 21:307 10.1037/a0037906 [DOI] [Google Scholar]
- Bianchi R., Schonfeld I. S., Laurent E. (2015a). Burnout–depression overlap: a review. Clin. Psychol. Rev. 36, 28–41. 10.1016/j.cpr.2015.01.004 [DOI] [PubMed] [Google Scholar]
- Bianchi R., Schonfeld I. S., Laurent E. (2015b). Is burnout separable from depression in cluster analysis? A longitudinal study. Soc. Psychiatry Psychiatr. Epidemiol. 50, 1005–1011. 10.1007/s00127-014-0996-8 [DOI] [PubMed] [Google Scholar]
- Bianchi R., Schonfeld I. S., Mayor E., Laurent E. (2016a). Burnout-Depression overlap: A study of New Zealand schoolteachers. NZ. J. Psychol. 45, 4–11. [Google Scholar]
- Bianchi R., Verkuilen J., Brisson R., Schonfeld I. S., Laurent E. (2016b). Burnout and depression: label-related stigma, help-seeking, and syndrome overlap. Psychiatry Res. 245, 91–98. 10.1016/j.psychres.2016.08.025 [DOI] [PubMed] [Google Scholar]
- Borenstein M., Hedges L., Higgins J., Rothstein H. (2005). Comprehensive Meta-Analysis Version 3.3. Biostat, Englewood, NJ 2013. [Google Scholar]
- Bühler K. E., Land T. (2003). Burnout and personality in intensive care: an empirical study. Hosp. Top. 81, 5–12. 10.1080/00185860309598028 [DOI] [PubMed] [Google Scholar]
- Capone V., Petrillo G. (2018). Mental health in teachers: relationships with job satisfaction, efficacy beliefs, burnout and depression. Curr. Psychol. 1:10 10.1007/s12144-018-9878-7 [DOI] [Google Scholar]
- Cardozo B. L., Crawford C. G., Eriksson C., Zhu J., Sabin M., Ager A., et al. (2012). Psychological distress, depression, anxiety, and burnout among international humanitarian aid workers: a longitudinal study. PLoS ONE 7:e44948 10.1371/journal.pone.0044948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherniss C. (1980). Staff burnout: Job Stress in the Human Services. Beverly Hills, CA: Sage Publications. [Google Scholar]
- Choi B.-S., Kim J. S., Lee D.-W., Paik J.-W., Lee B. C., Lee J. W., et al. (2018). Factors associated with emotional exhaustion in south korean nurses: a cross-sectional study. Psychiatry Investig. 15:670. 10.30773/pi.2017.12.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1992). A power primer. Psychol. Bull. 112:155. 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Cole A. H. (2014). Anxiety, in Encyclopedia of Psychology and Religion, ed. Leeming D. A. (Boston, MA: Springer; ), 95–99. 10.1007/978-1-4614-6086-2_38 [DOI] [Google Scholar]
- Craiovan P. M. (2015). Burnout, depression and quality of life among the Romanian employees working in non-governmental organizations. Proc. Soc. Behav. Sci. 187, 234–238. 10.1016/j.sbspro.2015.03.044 [DOI] [Google Scholar]
- da Silva Valente M. d,. S Wang Y.-P. Menezes P. R. (2018). Structural validity of the Maslach Burnout Inventory and influence of depressive symptoms in banking workplace: unfastening the occupational conundrum. Psychiatry Res. 267, 168–174. 10.1016/j.psychres.2018.05.069 [DOI] [PubMed] [Google Scholar]
- De Stefano C., Philippon A. L., Krastinova E., Hausfater P., Riou B., Adnet F., et al. (2018). Effect of emergency physician burnout on patient waiting times. Intern. Emerg. Med. 13, 421–428. 10.1007/s11739-017-17069 [DOI] [PubMed] [Google Scholar]
- Demir S. (2018). The relationship between psychological capital and stress, anxiety, burnout, job satisfaction, and job involvement. Eur. J. Educ. Res. 75, 137–153. 10.14689/ejer.2018.75.8 [DOI] [Google Scholar]
- Diestel S., Schmidt K.-H. (2010). Interactive effects of emotional dissonance and self-control demands on burnout, anxiety, and absenteeism. J. Vocat. Behav. 77, 412–424. 10.1016/j.jvb.2010.05.006 [DOI] [Google Scholar]
- DiGiacomo M., Adamson B. (2001). Coping with stress in the workplace: Implications for new health professionals. J. Allied Health 30, 106–111. [PubMed] [Google Scholar]
- Ding Y., Qu J., Yu X., Wang S. (2014). The mediating effects of burnout on the relationship between anxiety symptoms and occupational stress among community healthcare workers in China: a cross-sectional study. PLoS ONE 9:e107130. 10.1371/journal.pone.0107130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan-Porter W., Hatch D., Pendergast J. F., Freude G., Rose U., Burr H., et al. (2018). 12-month trajectories of depressive symptoms among nurses—Contribution of personality, job characteristics, coping, and burnout. J. Affect. Disord. 234, 67–73. 10.1016/j.jad.2018.02.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eurofound (2018) Burnout in the Workplace: A Review of Data and Policy Responses in the EU, Publicatios Office of the European Union. Luxembourg. [Google Scholar]
- Eysenck H. J., Rachman S. (2013). The Causes and Cures of Neurosis (Psychology Revivals): An Introduction to Modern Behaviour Therapy Based on Learning Theory and the Principles of Conditioning. New York, NY: Routledge; 10.4324/9780203766767 [DOI] [Google Scholar]
- Favrod C., du Chêne L. J., Soelch C. M., Garthus-Niegel S., Tolsa J. F., Legault F., Horsch A. (2018). Mental health symptoms and work-related stressors in hospital midwives and NICUnurses: a mixed methods study. Front. Psychiatry 9:364. 10.3389/fpsyt.2018.00364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng S., Shu-Xun H., Jia-Liang Z., Dong-Feng R., Zheng C., Jia-Guang T. (2014). Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. PLoS ONE. 10.1371/journal.pone.0111695.t001 [DOI] [Google Scholar]
- Fong T. C., Ho R. T., Au-Yeung F. S., Sing C., Law K., Lee L., et al. (2016). The relationships of change in work climate with changes in burnout and depression: a 2-year longitudinal study of Chinese mental health care workers. Psychol. Health Med. 21, 401–412. 10.1080/13548506.2015.1080849 [DOI] [PubMed] [Google Scholar]
- Freudenberger H. J. (1974). Staff burn-out. J. Soc. Issues 30, 159–165. 10.1111/j.1540-4560.1974.tb00706.x [DOI] [Google Scholar]
- Freudenberger H. J., Richelson G. (1980). Burn-Out: The high Cost of High Achievement. Garden City, NY: Anchor Press. [Google Scholar]
- Gallego-Alberto L., Losada A., Vara C., Olazarán J., Muñiz R., Pillemer K. (2018). Psychosocial predictors of anxiety in nursing home staff. Clin. Gerontol. 41, 282–292. 10.1080/07317115.2017.1370056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrouste-Orgeas M., Perrin M., Soufir L., Vesin A., Blot F., Maxime V., et al. (2015). The Iatroref study: medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture. Intensive Care Med. 41, 273–284. 10.1007/s00134-014-3601-4 [DOI] [PubMed] [Google Scholar]
- Ghorpade J., Lackritz J., Singh G. (2007). Burnout and personality: evidence from academia. J. Career Assess. 15, 240–256. 10.1177/1069072706298156 [DOI] [Google Scholar]
- Gillet N., Fouquereau E., Vallerand R. J., Abraham J., Colombat P. (2018). The role of workers' motivational profiles in affective and organizational factors. J. Happ. Stud. 19, 1151–1174. 10.1007/s10902-017-9867-9 [DOI] [Google Scholar]
- Glass D., McKnight J. (1996). Perceived control, depressive symptomatology, and professional burnout: a review of the evidence. Psychol. Health 11, 23–48. 10.1080/08870449608401975 [DOI] [Google Scholar]
- Grover S., Sahoo S., Bhalla A., Avasthi A. (2018). Psychological problems and burnout among medical professionals of a tertiary care hospital of North India: a cross-sectional study. Indian J. Psychiatry 60:175. 10.4103/psychiatry.IndianJPsychiatry_254_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakanen J. J., Schaufeli W. B. (2012). Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J. Affect. Disorder. 141, 415–424. 10.1016/j.jad.2012.02.043 [DOI] [PubMed] [Google Scholar]
- Hakanen J. J., Schaufeli W. B., Ahola K. (2008). The Job Demands-Resources model: A three-year cross-lagged study of burnout, depression, commitment, and work engagement. Work Stress 22, 224–241. 10.1080/02678370802379432 [DOI] [Google Scholar]
- Hardwicke T. E., Ioannidis J. P. (2018). Populating the data ark: an attempt to retrieve, preserve, and liberate data from the most highly-cited psychology and psychiatry articles. PLoS ONE 13:e0201856. 10.1371/journal.pone.0201856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemsworth D., Baregheh A., Aoun S., Kazanjian A. (2018). A critical enquiry into the psychometric properties of the professional quality of life scale (ProQol-5) instrument. Appl. Nurs. Res., 39, 81–88. 10.1016/j.apnr.2017.09.006 [DOI] [PubMed] [Google Scholar]
- Higgins J. P., Thompson S. G., Deeks J. J., Altman D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327:557. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hintsa T., Elovainio M., Jokela M., Ahola K., Virtanen M., Pirkola S. (2014). Is there an independent association between burnout and increased allostatic load? Testing the contribution of psychological distress and depression. J. Health Psychol. 21, 1576–1586. 10.1177/1359105314559619 [DOI] [PubMed] [Google Scholar]
- Iacovides A., Fountoulakis K., Kaprinis S., Kaprinis G. (2003). The relationship between job stress, burnout and clinical depression. J. Affect. Disord. 75, 209–221. 10.1016/S0165-0327(02)00101-5 [DOI] [PubMed] [Google Scholar]
- Idris M. A., Dollard M. F. (2014). Psychosocial safety climate, emotional demands, burnout, and depression: a longitudinal multilevel study in the Malaysian private sector. J. Occup. Health Psychol. 19:291. 10.1037/a0036599 [DOI] [PubMed] [Google Scholar]
- Johnson J., Louch G., Dunning A., Johnson O., Grange A., Reynolds C., et al. (2017). Burnout mediates the association between depression and patient safety perceptions: a cross-sectional study in hospital nurses. J. Adv. Nurs. 73, 1667–1680. 10.1111/jan.13251 [DOI] [PubMed] [Google Scholar]
- Karaoglu N., Pekcan S., Durduran Y., Mergen H., Odabasi D., Ors R. (2015). A sample of paediatric residents' loneliness-anxiety-depression-burnout and job satisfaction with probable affecting factors. JPMA. J. Pak. Med. Assoc. 65, 183–191. [PubMed] [Google Scholar]
- Kaschka W. P Korczak D. Broich K. (2011). Burnout: a fashionable diagnosis. Deutsches Ärzteblatt Int. 108:781. 10.3238/arztebl.2011.0781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katkat D. (2015). Level of Anxiety and Burnout among Martial Athletes into 17th Mediterranean Games. Anthropologist 19, 673–678. 10.1080/09720073.2015.11891702 [DOI] [Google Scholar]
- Kim H., Kao D. (2014). A meta-analysis of turnover intention predictors among US child welfare workers. Child. Youth Serv. Rev. 47, 214–223. 10.1016/j.childyouth.2014.09.015 [DOI] [Google Scholar]
- Korczak D., Huber B., Kister C. (2010). Differential diagnostic of the burnout syndrome. GMS Health Technol. Assess. 6:Doc09. 10.3205/hta000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R. S., Folkman S. (1984). Stress, Appraisal and Coping. New York, NY: Springer. [Google Scholar]
- Lebensohn P., Dodds S., Benn R., Brooks A. J., Birch M. (2013). Resident wellness behaviors. Fam. Med. 45, 541–549. [PubMed] [Google Scholar]
- Lee J.-Y., Kim S.-Y., Bae K.-Y., Kim J.-M., Shin I.-S., Yoon J.-S., et al. (2018). The association of gratitude with perceived stress and burnout among male firefighters in Korea. Pers. Individ. Dif. 123, 205–208. 10.1016/j.paid.2017.11.010 [DOI] [Google Scholar]
- Lipsey M. W., Puzio K., Yun C., Herbert M. A., Steinka-Fry K., Cole M. W., et al. (2012). Translating the Statistical Representation of the Effects of Education Interventions Into More Readily Interpretable Forms. United States: U.S: Dept of Education, National Center for Special Education Research, Institute of Education Sciences. [Google Scholar]
- Lipsey M. W., Wilson D. B. (2001). Practical Meta-Analysis. Sage Publications, Inc. [Google Scholar]
- Lobo D. A. (2018). Investigating the Effects of an ACT-Based Mobile Application on Stress, Anxiety, and Burnout in the Workplace (Doctoral dissertation, The University of Waikato: ). [Google Scholar]
- Malmberg-Gavelin H., Eskilsson T., Boraxbekk C. J., Josefsson M., Stigsdotter Neely A., SlungaJärvholm L. (2018). Rehabilitation for improved cognition in patients with stress-related exhaustion disorder: RECO–a randomized clinical trial. Stress 21, 279–291. 10.1080/10253890.2018.1461833 [DOI] [PubMed] [Google Scholar]
- Mark G., Smith A. P. (2012). Occupational stress, job characteristics, coping, and the mental health of nurses. Br. J. Health Psychol. 17, 505–521. 10.1111/j.2044-8287.2011.02051.x [DOI] [PubMed] [Google Scholar]
- Maske U. E., Riedel-Heller S. G., Seiffert I., Jacobi F., Hapke U. (2016). Häufigkeit und psychiatrischeKomorbiditäten von selbstberichtetemdiagnostiziertem Burnout Syndrom. Psychiatr. Prax. 43, 18–24. 10.1055/s-0035-1552702 [DOI] [PubMed] [Google Scholar]
- Maslach C., Jackson S. E., Leiter M. P. (1996). MBI: Maslach Burnout Inventory. Sunnyvale, CA: CPP, Incorporated. [Google Scholar]
- Maslach C., Jackson S. E., Leiter M. P. (2006). Maslach Burnout Inventory. CPP. [Google Scholar]
- Maslach C., Leiter M. P. (2016). Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry 15, 103–111. 10.1002/wps.20311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach C., Schaufeli W. B., Leiter M. P. (2001). Job burnout. Annu. Rev. Psychol. 52, 397–422. 10.1146/annurev.psych.52.1.397 [DOI] [PubMed] [Google Scholar]
- Mather L., Blom V., Bergström G., Svedberg P. (2016). An underlying common factor, influenced by genetics and unique environment, explains the covariation between major depressive disorder, generalized anxiety disorder, and burnout: a Swedish twin study. Twin Res. Hum. Genet. 19, 619–627. 10.1017/thg.2016.73 [DOI] [PubMed] [Google Scholar]
- McKnight J. D., Glass D. C. (1995). Perceptions of control, burnout, and depressive symptomatology: a replication and extension. J. Consult. Clin. Psychol. 63:490. 10.1037/0022-006X.63.3.490 [DOI] [PubMed] [Google Scholar]
- Melamed S., Shirom A., Toker S., Berliner S., Shapira I. (2006). Burnout and risk of cardiovascular disease: evidence, possible causal paths, and promising research directions. Psychol. Bull. 132:327. 10.1037/0033-2909.132.3.327 [DOI] [PubMed] [Google Scholar]
- Melchers M. C., Plieger T., Meermann R., Reuter M. (2015). Differentiating burnout from depression: personality matters! Front. Psychiatry 6:113. 10.3389/fpsyt.2015.00113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metlaine A., Sauvet F., Gomez-Merino D., Boucher T., Elbaz M., Delafosse J. Y., et al. (2018). Sleep and biological parameters in professional burnout: a psychophysiological characterization. PLoS ONE 13:e0190607. 10.1371/journal.pone.0190607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middeldorp C. M., Cath D. C., Berg M.v.d., Beem A. L., Dyck R. V., Boomsma D. I. (2006). The association of personality with anxious and depressive psychopathology, in Biology of Personality and Individual Differences, ed Canli T. (New York, NY: The Guilford Press; ), 251–272. [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 151, 264–269. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- Moore B. M., Schellinger K. (2018). An examination of the moderating effect of proactive coping inNICU Nurses. J. Perinat. Neonatal Nurs. 32, 275–285. 10.1097/JPN.0000000000000353 [DOI] [PubMed] [Google Scholar]
- Mosing M. A., Butkovic A., Ullen F. (2018). Can flow experiences be protective of work-related depressive symptoms and burnout? A genetically informative approach. J. Affect. Disord. 226, 6–11. 10.1016/j.jad.2017.09.017 [DOI] [PubMed] [Google Scholar]
- Mutkins E., Brown R., Thorsteinsson E. (2011). Stress, depression, workplace and social supports and burnout in intellectual disability support staff. J. Intell. Disabil. Res. 55, 500–510. 10.1111/j.1365-2788.2011.01406.x [DOI] [PubMed] [Google Scholar]
- Oe M., Ishida T., Favrod C., Martin-Soelch C., Horsch A. (2018). Burnout, psychological symptoms, and secondary traumatic stress among midwives working on perinatal wards: a cross-cultural study between Japan and Switzerland. Front. Psychiatry 9:387. 10.3389/fpsyt.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penz M., Stalder T., Miller R., Ludwig V. M., Kanthak M. K., Kirschbaum C. (2018). Hair cortisol as a biological marker for burnout symptomatology. Psycho. Neuro. Endocrinol. 87, 218–221. 10.1016/j.psyneuen.2017.07.48 [DOI] [PubMed] [Google Scholar]
- Pereira-Lima K., Loureiro S. (2015). Burnout, anxiety, depression, and social skills in medical residents. Psychol. Health Med. 20, 353–362. 10.1080/13548506.2014.936889 [DOI] [PubMed] [Google Scholar]
- Peterson U., Demerouti E., Bergström G., Samuelsson M., Åsberg M., Nygren Å. (2008). Burnout and physical and mental health among Swedish healthcare workers. J. Adv. Nurs. 62, 84–95. 10.1111/j.1365-2648.2007.04580.x [DOI] [PubMed] [Google Scholar]
- Plieger T., Melchers M., Montag C., Meermann R., Reuter M. (2015). Life stress as potential risk factor for depression and burnout. Burnout Res. 2, 19–24. 10.1016/j.burn.2015.03.001 [DOI] [Google Scholar]
- Richardson C. M., Trusty W. T., George K. A. (2018). Trainee wellness: self-critical perfectionism, self-compassion, depression, and burnout among doctoral trainees in psychology. Counsel. Psychol. Q. 1–12. 10.1080/09515070.2018.1509839 [DOI] [Google Scholar]
- Rogers M. E., Creed P. A., Searle J. (2014). Emotional labour, training stress, burnout, and depressive symptoms in junior doctors. J. Vocat. Educ. Train. 66, 232–248. 10.1080/13636820.2014.884155 [DOI] [Google Scholar]
- Rosenthal R. (1979). The file drawer problem and tolerance for null results. Psychol. Bull. 86:638 10.1037/0033-2909.86.3.638 [DOI] [Google Scholar]
- Ruotsalainen J. H., Verbeek J. H., Mariné A., Serra C. (2015). Preventing occupational stress in healthcare workers. Cochr Library 4:CD002892 10.1002/14651858.CD002892.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rydmark I., Wahlberg K., Ghatan P. H., Modell S., Nygren Å., Ingvar M., et al. (2006). Neuroendocrine, cognitive and structural imaging characteristics of women on longtermsickleave with job stress–induced depression. Biol. Psychiatry 60, 867–873. 10.1016/j.biopsych.2006.04.029 [DOI] [PubMed] [Google Scholar]
- Salvagioni D. A. J., Melanda F. N., Mesas A. E., González A. D., Gabani F. L., de Andrade S. M. (2017). Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS ONE 12:e0185781. 10.1371/journal.pone.0185781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samios C. (2017). Burnout and psychological adjustment in mental health workers in rural Australia: the roles of mindfulness and compassion satisfaction. Mindfulness 9, 1088–1099. 10.1007/s12671-017-0844-5 [DOI] [Google Scholar]
- Santa Maria A., Wolter C., Gusy B., Kleiber D., Renneberg B. (2018). The Impact of Health-Oriented Leadership on Police Officers' Physical Health, Burnout, Depression and Well-Being. Policing: A Journal of Policy and Practice. Oxford University Press; 10.1093/police/pay067 [DOI] [Google Scholar]
- Sarason I. G. (1972). Experimental approaches to test anxiety: attention and the uses of information. Anxiety 2, 383–403. 10.1016/b978-0-12-657402-9.50010-7 [DOI] [Google Scholar]
- Scargle J. D. (1999). Publication bias (the “file-drawer problem”) in scientific inference. eprint arXiv:physics/9909033. [Google Scholar]
- Schaufeli W., Enzmann D. (1998). The Burnout Companion to Study and Practice: A Critical Analysis. Philadelphia, PA: CRC press. [Google Scholar]
- Schaufeli W. B., Bakker A. B., Hoogduin K., Schaap C., Kladler A. (2001). On the clinical validity of the Maslach Burnout Inventory and the Burnout Measure. Psychol. Health 16, 565–582. 10.1080/08870440108405527 [DOI] [PubMed] [Google Scholar]
- Schiller H., Söderström M., Lekander M., Rajaleid K., Kecklund G. (2018). A randomized controlled intervention of workplace-based group cognitive behavioral therapy for insomnia. Int. Arch. Occup. Environ. Health 91, 413–424. 10.1007/s00420-018-1291-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt F. L., Oh I. S., Hayes T. L. (2009). Fixed-versus random-effects models in meta-analysis: model properties and an empirical comparison of differences in results. Br. J. Math. Statist. Psychol. 62, 97–128. 10.1348/000711007X255327 [DOI] [PubMed] [Google Scholar]
- Schonfeld I. S., Bianchi R. (2016). Burnout and depression: two entities or one? J. Clin. Psychol. 72, 22–37. 10.1002/jclp.22229 [DOI] [PubMed] [Google Scholar]
- Sedgwick P. (2013). Meta-analyses: how to read a funnel plot. BMJ 346:f1342 10.1136/bmj.f1342 [DOI] [PubMed] [Google Scholar]
- Shi Y., Guo H., Zhang S., Xie F., Wang J., Sun Z., et al. (2018). Impact of workplace incivility against new nurses on job burn-out: a cross-sectional study in China. BMJ Open 8:e020461. 10.1136/bmjopen-2017-020461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva N. R., Bolsoni-Silva A. T., Loureiro S. R. (2018). Burnout e depressãoemprofessores do ensino fundamental: um estudocorrelacional. Rev. Brasil. Educ. 23:e230048 10.1590/s1413-24782018230048 [DOI] [Google Scholar]
- Spielberger C. D. (1966). Theory and research on anxiety. Anxiety Behav. 1:3 10.1016/B978-1-4832-3131-0.50006-8 [DOI] [Google Scholar]
- Spitzer R. L., Williams J. B., Kroenke K., Linzer M., VerloindeGruy F., Hahn S. R., et al. (1994). Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. JAMA 272, 1749–1756. 10.1001/jama.1994.03520220043029 [DOI] [PubMed] [Google Scholar]
- Steinhardt M. A., Smith Jaggars S. E., Faulk K. E., Gloria C. T. (2011). Chronic work stress and depressive symptoms: assessing the mediating role of teacher burnout. Stress and Health 27, 420–429. 10.1002/smi.1394 [DOI] [Google Scholar]
- Sterne J. A., Sutton A. J., Ioannidis J. P., Terrin N., Jones D. R., Lau J., et al. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343:d4002. 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- Sun W., Fu J., Chang Y., Wang L. (2012). Epidemiological study on risk factors for anxiety disorder among Chinese doctors. J. Occup. Health 54, 1–8. 10.1539/joh.11-0169-OA [DOI] [PubMed] [Google Scholar]
- Takai M., Takahashi M., Iwamitsu Y., Ando N., Okazaki S., Nakajima K., et al. (2009). The experience of burnout among home caregivers of patients with dementia: relations to depression and quality of life. Arch. Gerontol. Geriatr. 49, e1–e5. 10.1016/j.archger.2008.07.002 [DOI] [PubMed] [Google Scholar]
- Talih F., Ajaltouni J., Farhood L. (2018). Depression and burnout among nurses in a Lebanese academic medical center. J. Med. Liban. 66, 92–97. 10.12816/0047826 [DOI] [Google Scholar]
- Talih F., Warakian R., Ajaltouni J., Tamim H. (2016). Correlates of depression and burnout among residents in a lebanese academic medical center: a cross-sectional study. Academ. Psychiatry 40, 38–45. 10.1007/s40596-015-0400-3 [DOI] [PubMed] [Google Scholar]
- Toker S., Biron M. (2012). Job burnout and depression: unraveling their temporal relationship and considering the role of physical activity. J. Appl. Psychol. 97:699. 10.1037/a0026914 [DOI] [PubMed] [Google Scholar]
- Tourigny L., Baba V. V., Wang X. (2010). Burnout and depression among nurses in Japan and China: the moderating effects of job satisfaction and absence. Int. J. Hum. Resour. Manage. 21, 2741–2761. 10.1080/09585192.2010.528656 [DOI] [Google Scholar]
- Trockel M., Bohman B., Lesure E., Hamidi M. S., Welle D., Roberts L., et al. (2018). A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Academ. Psychiatry 42, 11–24. 10.1007/s40596-017-0849-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnipseed D. L. (1998). Anxiety and burnout in the health care work environment. Psychol. Reports 82, 627–642. 10.2466/pr0.1998.82.2.627 [DOI] [PubMed] [Google Scholar]
- Tzeletopoulou A., Alikari V., Zyga S., Tsironi M., Lavdaniti M., Theofilou P. (2018). Are burnout syndrome and depression predictors for aggressive behavior among mental health care professionals? Med. Arch. 72, 244–8. 10.5455/medarh.2018.72.244-248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dam A. (2016). Subgroup analysis in burnout: relations between fatigue, anxiety, and depression. Front. Psychol. 7:90. 10.3389/fpsyg.2016.00090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasconcelos E. M., Martino M. M. F. D., França S. P. (2018). Burnout and depressive symptoms in intensive care nurses: relationship analysis. Revistabrasil. Enferm. 71, 135–141. 10.1590/0034-7167-2016-0019 [DOI] [PubMed] [Google Scholar]
- Vasilopoulos S. (2012). Job burnout and its relation tosocial anxiety in primary school teachers. Hell. J. Psychol. 9, 18–44. [Google Scholar]
- Weber A., Jaekel-Reinhard A. (2000). Burnout syndrome: a disease of modern societies? Occup. Med. 50, 512–517. 10.1093/occmed/50.7.512 [DOI] [PubMed] [Google Scholar]
- Weigl M., Stab N., Herms I., Angerer P., Hacker W., Glaser J. (2016). The associations of supervisor support and work overload with burnout and depression: a cross-sectional study in two nursing settings. J. Adv. Nurs. 72, 1774–1788. 10.1111/jan.12948 [DOI] [PubMed] [Google Scholar]
- Wurm W., Vogel K., Holl A., Ebner C., Bayer D., Mörkl S., et al. (2016). Depression-burnout overlap in physicians. PLoS ONE 11:e0149913. 10.1371/journal.pone.0149913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yazicioglu I., Kizanlikli M. M. (2019). The effects of trait anxiety on the intention of leaving and burnout of restaurant employees. Turizm Akademik Dergisi 5, 247–259. Available online at: http://dergipark.gov.tr/touraj/issue/37924/431983 [Google Scholar]
- Yeh S. S., Lee C. N., Wu Y. H., Tu N. C., Guo Y. L., Chen P. C., et al. (2018). Occupational hazard exposures and depressive symptoms of pregnant workers. J. Occup. Environ. Med. 60, e134–8. 10.1097/JOM.0000000000001255 [DOI] [PubMed] [Google Scholar]
- Zhou J., Yang Y., Qiu X., Yang X., Pan H., Ban B., et al. (2016). Relationship between anxiety and burnout among Chinese physicians: a moderated mediation model. PLoS ONE 11:e0157013. 10.1371/journal.pone.0157013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Yang Y., Qiu X., Yang X., Pan H., Ban B., et al. (2018). Serial multiple mediation of organizational commitment and job burnout in the relationship between psychological capital and anxiety in Chinese female nurses: a cross-sectional questionnaire survey. Int. J. Nurs. Stud. 83, 75–82. 10.1016/j.ijnurstu.2018.03.016 [DOI] [PubMed] [Google Scholar]
- Zigmond A. S., Snaith R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–370. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.