Abstract
The objective of the current study was to determine the factors associated with delayed isolation of pulmonary tuberculosis (TB). In this retrospective study, data of patients newly diagnosed with pulmonary TB from January 2015 through December 2017 at a referral hospital were reviewed. Delayed recognition of pulmonary TB was defined as failure to initiate airborne isolation within the first 3 days of admission. We analyzed the clinical, microbiological, and radiological factors associated with delayed isolation of pulmonary TB. A total of 134 patients with positive sputum acid-fast bacilli (AFB) cultures were analyzed, of which 44 (33%) were isolated within 3 days after admission. In multivariate logistic regression analysis, older age (p = 0.01), admission to departments other than Infectious Disease or Pulmonology (p = 0.005), and presence of malignancy (p = 0.02) were associated with delayed isolation. Patients with a radiologic diagnosis of active pulmonary TB were likely to be isolated early (p = 0.01). Better awareness of pulmonary TB among attending practitioners in hospital settings is required. Delay in isolation is associated with older age, malignancy, hospitalization to departments other than Infectious Disease or Pulmonology, and non-confident radiologic diagnosis of active pulmonary TB.
Introduction
Tuberculosis (TB) is a major global health problem. Approximately 6.3 million new cases of TB and 1.3 million related deaths are recorded annually1. TB outbreaks are known to occur in institutional settings including hospitals2. In the Korean health care system, patient care during hospitalization is often communal, which can lead to an easy spread of TB3. In addition, immunocompromised patients who acquire TB as a nosocomial infection can develop severe disease. The World Health Organization’s policy on TB-infection control recommends administrative controls that reduce exposure to patients with presumptive TB4. Prompt diagnosis of active pulmonary TB is critical for early treatment and preventing disease transmission among patients and healthcare workers5.
In a previous study, the initial diagnosis of active pulmonary TB in almost 50% of the hospitalized patients was missed, and treatment was delayed for ≥7 days in 30% of the patients6. According to a systematic review, the diagnosis of pulmonary TB was delayed by an average of 68 days in low-income countries and 61 days in high-income countries7. A delay in TB treatment can result in progression and increased transmission of the disease6. Previous studies have reported certain factors associated with the delayed diagnosis of active pulmonary TB8–10. However, those studies were limited to a specific population8 or did not focus on hospitalized patients with a potential risk of causing in-hospital TB transmission9,10. Thus, knowledge of the factors associated with delayed isolation of patients with unexpected active pulmonary TB in acute-care hospitals is lacking.
This study aimed to determine the clinical and microbiological factors responsible for prolonged exposure before isolation of patients with TB in a health care setting. In addition, we evaluated the role of radiologists in the rapid diagnosis and isolation of patients with unexpected active pulmonary TB.
Results
Baseline demographics and clinical characteristics
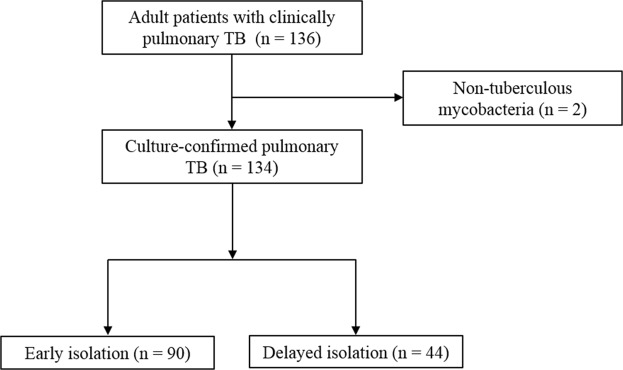
During the study period (January 2015 to December 2017), a total of 134 patients with sputum cultures positive for Mycobacterium tuberculosis were identified, of which 44 (33%) had delayed isolation (Fig. 1). Table 1 shows the comparison of the baseline patient characteristics between the early and delayed isolation groups. Patients with delayed isolation were older than those with early isolation (mean 72 vs. 55 years, P < 0.001). A smaller proportion of patients with early isolation showed disease comorbidity (38% vs. 14%, P = 0.004), which included hypertension (32% vs. 52%, P = 0.03), chronic obstructive pulmonary disease (2% vs. 14%, P = 0.02), and malignancies (7% vs. 23%, P < 0.01) compared to patients with delayed isolation. In addition, patients with early isolation had more clinical symptoms and features of pulmonary TB such as cough, sputum, night sweats, and weight loss. These patients were more often admitted to the Infectious Disease or Pulmonology Departments than to other departments (76% vs. 41%, P < 0.001). The median number of hospitalization days were higher in patients with delayed isolation than in those with early isolation (10 vs. 19 days, P < 0.001). The overall in-hospital mortality was 13% (17/134), and in-hospital mortality was not significantly different between the two groups (12% in the early isolation group vs. 14% in the delayed isolation group, P = 0.82).
Figure 1.
Flow diagram of the study.
Table 1.
Demographic and descriptive profiles of patients with pulmonary TB grouped according to the isolation period.
| Characteristics | Total number of patients (n = 134) | Early isolation (within 3 days, n = 90) | Delayed isolation (after 3 days, n = 44) | p |
|---|---|---|---|---|
| Age, mean (SD) | 61 (22) | 55 (22) | 72 (17) | <0.001 |
| Male sex | 90 (67) | 65 (72) | 25 (57) | 0.08 |
| Comorbidity | ||||
| None | 40 (30) | 34 (38) | 6 (14) | 0.004 |
| Hypertension | 52 (39) | 29 (32) | 23 (52) | 0.03 |
| Diabetes | 41 (31) | 25 (28) | 16 (36) | 0.31 |
| COPD | 8 (6) | 2 (2) | 6 (14) | 0.02 |
| Asthma | 5 (4) | 2 (2) | 3 (7) | 0.33 |
| Cerebrovascular accident | 11 (8) | 7 (8) | 4 (9) | 0.75 |
| Coronary artery disease | 10 (7) | 7 (8) | 3 (7) | 1.00 |
| HIV | 2 (2) | 2 (2) | 0 (0) | 1.00 |
| Chronic kidney disease | 10 (7) | 5 (6) | 5 (11) | 0.30 |
| Malignancy | 16 (12) | 6 (7) | 10 (23) | <0.01 |
| TB history | 18 (13) | 12 (13) | 6 (14) | 0.96 |
| TB medication history | 14 (10) | 9 (10) | 5 (11) | 0.77 |
| Clinical features | ||||
| Fever | 36 (27) | 20 (22) | 16 (36) | 0.08 |
| Chill | 21 (16) | 15 (17) | 6 (14) | 0.65 |
| Cough | 69 (52) | 54 (60) | 15 (34) | 0.01 |
| Sputum | 43 (32) | 35 (39) | 8 (18) | 0.02 |
| Dyspnea | 31 (23) | 17 (19) | 14 (32) | 0.10 |
| Chest pain | 12 (9) | 8 (9) | 4 (9) | 1.00 |
| Other pain | 21 (16) | 9 (10) | 12 (27) | 0.01 |
| Hemoptysis | 6 (5) | 5 (6) | 1 (2) | 0.66 |
| Night sweats | 10 (7) | 10 (11) | 0 (0) | 0.03 |
| Loss of appetite | 24 (18) | 19 (21) | 5 (11) | 0.16 |
| Weight loss | 23 (17) | 21 (23) | 2 (5) | <0.01 |
| Laboratory findings | ||||
| Positive AFB smear | 84 (63) | 66 (73) | 18 (41) | <0.001 |
| Positive TB PCR | 107 (87) | 78 (93) | 29 (74) | 0.007 |
| Radiological findings (chest radiograph) | ||||
| Diagnosis of TB | 94 (70) | 74 (82) | 20 (46) | <0.001 |
| Active TB | 76 (57) | 66 (73) | 10 (23) | <0.001 |
| Typical findings of TB in adults | 76 (57) | 61 (68) | 15 (34) | <0.001 |
| New disease on follow-up examination | 37 (28) | 25 (28) | 12 (27) | 0.04 |
| Hospitalization course | ||||
| Admission to the Infectious Disease or Pulmonology Department | 86 (64) | 68 (76) | 18 (41) | <0.001 |
| Length of hospitalization (days, median (range)) | 13 (6–22) | 10 (3–17) | 19 (12–51) | <0.001 |
| Exposure days, median (range) | 1 (0–6) | 0 (0–1) | 9 (6–14) | <0.001 |
| In-hospital mortality | 17 (13) | 11 (12) | 6 (14) | 0.82 |
Data are numbers (%) of patients, unless otherwise indicated.
Abbreviations: SD, standard deviation; COPD, chronic obstructive pulmonary disease; HIV, human immunodeficiency virus; TB, tuberculosis; AFB, acid-fast bacilli; PCR, polymerase chain reaction.
Radiological findings
The radiological findings of pulmonary TB in our patients are presented in Table 2. Pulmonary TB was diagnosed by experienced radiologists after a retrospective review of chest radiographs in 70% (94/134) of the patients. In the remaining 40 patients, chest radiographic diagnoses were pneumonia (n = 17), bronchiectasis (n = 3), lung cancer (n = 2), pleural effusion (n = 2), nontuberculous mycobacterial disease (n = 1), pulmonary fibrosis (n = 1), septic lung (n = 1), lung abscess (n = 1), and nonspecific features including normal findings (n = 12). In the delayed isolation group, TB was retrospectively diagnosed on the basis of chest radiography in approximately half (45%, 20/44) of the patients. Furthermore, chest radiographic findings of active TB and typical findings of TB in adults were observed in only 23% and 34% of patients, respectively. On review of chest radiographs and CT scans, four patients (3%, 4/134) who showed negative findings on chest radiographs were subsequently diagnosed with TB by CT.
Table 2.
Radiological findings of pulmonary TB.
| Characteristic | Total number of patients (n = 134) | Early isolation (within 3 days, n = 90) | Delayed isolation (after 3 days, n = 44) | p |
|---|---|---|---|---|
| Chest radiograph (n = 134) | ||||
| Diagnosis of TB | 94 (70) | 74 (82) | 20 (45) | <0.001 |
| Active TB | 76 (57) | 66 (73) | 10 (23) | <0.001 |
| Typical findings of TB in adults | 76 (57) | 61 (68) | 15 (34) | <0.001 |
| New disease on follow-up examination | 37 (28) | 25 (28) | 12 (27) | 0.03 |
| Chest CT (n = 122) | ||||
| Active TB | 98 (73) | 76 (84) | 22 (50) | 0.89 |
| Typical findings of TB in adults | 66 (49) | 55 (61) | 11 (25) | 0.001 |
| Airway involvement | 22 (16) | 16 (18) | 6 (14) | 0.59 |
Abbreviations: TB, tuberculosis; CT, computed tomography
Factors associated with delayed isolation of TB
Table 3 shows the results of multivariate logistic regression for factors associated with delayed isolation with pulmonary TB during hospitalization. Patients of older age, with comorbid malignancy, and who were hospitalized in departments other than Infectious Disease or Pulmonology were significantly associated with delayed isolation. Patients who were diagnosed with active pulmonary TB on chest radiographs were more likely to be isolated earlier. The adjusted odd ratios after adjusting for potential confounders by excluding factors in the multivariate model subgroups of comorbidity, hospitalization course, and microbiological results are presented in Table 3.
Table 3.
Multivariate logistic regression for factors associated with delayed isolation of patients with pulmonary TB during hospitalization.
| Variables | Total | Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p* | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Demographic | ||||||||
| Age | 1.04 (1.01–1.07) | 0.01 | 1.04 (1.01–1.08) | 0.002 | 1.04 (1.01–1.06) | 0.01 | 1.04 (1.01–1.08) | 0.01 |
| Comorbidity | ||||||||
| Malignancy | 4.75 (1.30–17.39) | 0.02 | 5.95 (1.54–23.03) | 0.01 | 4.86 (1.37–17.19) | 0.01 | ||
| Clinical features | ||||||||
| Other pain | 4.11 (1.27–13.25) | 0.02 | 3.97 (1.26–12.51) | 0.02 | ||||
| Microbiological findings | ||||||||
| AFB smear | 0.31 (0.12–0.83) | 0.02 | ||||||
| Hospitalization course | ||||||||
| Admission department | 4.03 (1.52–10.74) | 0.005 | 3.51 (1.39–8.85) | 0.008 | 7.09 (2.34–21.46) | 0.001 | ||
| Radiological findings (chest radiograph) | ||||||||
| Activity | 0.22 (0.08–0.66) | 0.01 | 0.23 (0.08–0.64) | 0.005 | 0.19 (0.07–0.57) | 0.003 | 0.18 (0.06–0.52) | 0.002 |
*All variables from Table 1 with P < 0.05 were included in the first step of multivariate analyses. Only significant variables in the final multivariate logistic regression model after backward selection are presented.
Model 1: Without comorbidity.
Model 2: Without hospitalization course.
Model 3: Without microbiological results.
Abbreviations: CI, confidence interval; SD, standard deviation; COPD, chronic obstructive pulmonary disease; HIV, human immunodeficiency virus; TB, tuberculosis; AFB, acid-fast bacilli; PCR, polymerase chain reaction.
Discussion
Our study showed that older age, presence of comorbid malignancy, no confirmed diagnosis of active TB on chest radiograph, and admission to departments other than Infectious Disease or Pulmonology can contribute to the delayed isolation of patients with active pulmonary TB in an acute-care hospital. In addition, delayed isolation was associated with prolonged hospitalization and exposure days, which could lead to a potentially threatening hospital TB outbreak. On retrospective review of chest radiographs, pulmonary TB was diagnosed by experienced radiologists in 70% of all patients and approximately half (43%) of the patients in the delayed isolation group.
We found that older age was an important factor associated with delayed isolation, which was consistent with the results from previous population-based studies in developed countries11,12. In elderly patients, active pulmonary TB can manifest with unusual clinical features and co-exist with aspiration pneumonia13. According to 2017 nationwide data from the Korea Centers for Disease Control and Prevention, 41.9% of newly diagnosed TB cases were patients aged ≥65 years, and this value has been increasing. The number of patients with newly diagnosed TB who are aged ≥80 years has been increasing since 200114. In an aging society, elderly patients with unusual symptoms or signs should be examined for possible TB infection. In the population aged ≥65 years, 1 in 10 persons has a malignant disease15. In this study, malignancy was a risk factor for delayed isolation. In the delayed isolation group, approximately one-fourth (22.72%, 10/44) of our patients had comorbid malignancies. Therefore, TB should be considered in the differential diagnosis of hospitalized patients, particularly in elderly patients with malignancy.
In this study, the initial department of admission for each patient was associated with a delayed diagnosis of TB. In previous studies, the type of hospital on initial visit or the level of the attending practitioner was associated with a delayed diagnosis of TB. Supplemental Table 1 show the detailed cause of admission or presenting symptom/sign. Most common department other than Infectious Diseases or Pulmonology was Gastroenterology followed by Orthopedic, Nephrology, and Thoracic surgery (see Supplemental Table 2). Among the patients who admitted to departments other than Infectious Diseases or Pulmonary, 54% (26/48) patients had delayed isolation. Of these 26 patients, 5 had extrapulmonary TB such as TB spondylitis (n = 3), meningitis (n = 1), and peritonitis (n = 1). In patients with extrapulmonary TB, physician should carefully check whether they are accompanied by pulmonary TB and isolate if necessary.
Patients with delayed isolation had symptoms indicating diseases other than pulmonary TB, such as pneumonia, lung mass, urinary tract infection, and liver cirrhosis with complications (see Supplemental Table 3). These patients had clinical features of systemic infectious disease, but the diagnosis of TB was delayed, possibly because of low AFB smear yield and decreased burden of pulmonary TB. Among the 44 patients who had delayed isolation, active pulmonary TB was diagnosed from the specimen collected during bronchoscopy (n = 6), subsequent chest CT (n = 7), and sputum specimen collected for evaluation of other disease such as pneumonia (n = 8). This result suggests that initial admission to an inappropriate department can delay the detection of active pulmonary TB and contribute to prolonged in-hospital airborne exposures.
Previous reports describe factors associated with a diagnostic delay of pulmonary TB8,9,16–18. In a Japanese study, male gender, absence of chronic cough, and presence of non-cavitary lesion on chest radiograph were associated with delayed isolation of patients with smear-positive pulmonary TB8. However, the Japanese study was limited by its inclusion of only AFB smear-positive patients. The present study included all patients with active TB who were isolated to prevent further transmission and reduce the burden of infection control. Pulmonary TB was confirmed by culture positivity in all our patients, but 50 (37%) patients had negative AFB smear results. Thus, negative AFB smear results might not reveal a patient who has contagious active pulmonary TB that can be transmitted to others and lead to a possible outbreak19.
This study highlights the importance of chest radiographic information and diagnosis by a radiologist for patients with pulmonary TB. A chest radiograph with pulmonary TB may be inaccurately interpreted by a physician20. Recent studies have reported that high-resolution CT screening is useful for detecting culture positive pulmonary TB21,22. However, those image studies have limited diagnostic performance when clinical information is lacking. In the present study, we found that 46% of our delayed isolation group were retrospectively diagnosed with pulmonary TB by chest radiologists during review of the examination results. In addition, confirmed active pulmonary TB by a radiologist was significantly associated with early isolation. Therefore, we expect that rapid interpretation of chest radiograph by a radiologist can reduce an unexpected exposure period. Because this interpretation is inferred by retrospective review of chest radiographs, the role of the radiologist in reducing an unexpected exposure to pulmonary TB needs to be evaluated in prospective studies.
Despite our important findings, there are a few limitations to this study. First, our study was based on a single-center cohort. Therefore, the clinically delayed decisions leading to exposure before isolation might have been made by clinicians at differing levels of experience, and our results may not be generalized to other institutions with different prevalence or incidence rates of TB. Second, owing to the retrospective nature of the study, the accuracy of documented charts is limited. Further prospective studies that involve multiple institutions are required to confirm our findings.
Although the incidence of pulmonary TB is decreasing worldwide, pulmonary TB outbreaks are reported consistently. These cause disease transmission and increasing hospital costs. Therefore, practitioners should be more careful and aware of the factors associated with delayed isolation of patients of older age, with malignancy, hospitalized to departments other than Infectious Disease or Pulmonology, and showing uncertain activity of pulmonary TB on chest radiography.
Methods
Study setting and population
This retrospective study included all hospitalized patients who were diagnosed with culture-positive active pulmonary TB at a university-affiliated referral center in Seoul, Republic of Korea, between January 2015 and December 2017. At our institution, patients with respiratory diseases such as pulmonary TB are usually admitted to the Pulmonology or Infectious Disease Department. If a patient is initially suspected of active pulmonary TB, preemptive airborne isolation with negative air pressure is performed at admission. If it is unclear whether the patient has active pulmonary TB, the patient can be isolated under suspicion, depending on the physician’s clinical decision. This study was approved by the Institutional Review Board (serial number 2018-04-033) of the hospital, and the need for informed consent was waived owing to the retrospective nature of the study.
Data collection and definitions
Electronic medical records of patients diagnosed with active pulmonary TB were reviewed. A diagnosis of active pulmonary TB was confirmed via AFB culture of respiratory specimens positive for Mycobacterium tuberculosis. We divided the patients with active pulmonary TB into the early or the delayed isolation group based on being isolated within 3 days, or after 3 days, of hospitalization respectively23,24. We focused on factors that might contribute to delayed isolation of such patients after 3 days of admission, which could lead to continued exposure during their hospital stay. We collected data on potential confounders such as patient-related demographics (age, sex, chief complaints, presenting symptoms and signs of illness, past medical history, and admission department), microbiological results (AFB staining and culture, and TB DNA polymerase chain reaction test), and radiologic findings (chest radiograph and/or chest computed tomography). Axillary measured body temperature >37.8 °C was considered a fever. Weight loss of ≥10% of body weight or ≥5 kg in the last 6 months was noted. Malignancies included all solid and hematologic types. The time from admission to adequate airborne isolation was defined as the exposure period.
Evaluation of radiological findings
The initial chest radiographs (134/134) and CT scans (122/134) of enrolled patients were reviewed by two chest radiologists, one with 26, and the other with 7, years of experience. Radiological diagnosis, including that of TB, and evaluation for disease activity, were performed without clinical information to eliminate preconceived bias. Final decisions were reached by consensus. Radiological findings of active pulmonary TB included cavities, nodules, and micronodules with segmental distribution, airspace consolidation, diffuse miliary nodules, and new appearance or progression of these findings on follow-up when the previous study was available. Findings of stable or inactive pulmonary TB included absence of active disease, mostly calcified small granulomas or lymph nodes, and stable fibronodular scarring for at least 6 months. Radiological diagnosis of TB activity was classified as active, inactive, and indeterminate. In addition, typical and relatively atypical radiological manifestations of TB in adults were evaluated. The typical findings included upper lung involvement, cavities with nodules or micronodules, and unilateral pleural effusion suggesting TB pleurisy. The atypical findings included middle and lower lung involvement, lobar or segmental airspace consolidation, diffuse miliary disease, bilateral pleural effusions, lymphadenopathy with no definite lung diseases, and airway involvement25,26.
Statistical analysis
Continuous variables were compared using the non-parametric Mann-Whitney and Kruskal-Wallis tests. Categorical variables were compared using Chi-square test or Fisher’s exact test. Factors possibly associated with early TB diagnosis were identified using univariate analysis (p < 0.05) and entered into multivariate models. The final model was selected using backward selection, and factors that did not improve the adequacy of the model were discarded. In addition, we have implemented virtual settings for clinically important variables with three situations by adjusting all significant values without comorbidity (model 1), hospitalization course (model 2), and microbiologic results (model 3). Data were analyzed using SPSS version 19.0 (Statistical Package for the Social Sciences Inc.; Chicago, IL, USA). Variables with a P-value of <0.05 were considered to be statistically significant.
Supplementary information
Acknowledgements
This research was supported by the Soonchunhyang University Research Fund.
Author Contributions
Conceptualization: Park S.Y., Lee E.J., Kim T.H. Investigation: Han J., Nam B.D., J. Park, Hwang J.H., S.Y. Park. Formal analysis: Han J., Nam B.D. Methodology: Han J., Nam B.D., Park S.Y., Hwang J.H. Supervision: S.Y. Park. Writing-original draft: Han J., Nam B.D., Park S.Y. Writing-review & editing: Han J., Nam B.D., Park S.Y., Lee E., E.J. Lee, Hwang J.H., Kim T.H.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jaijun Han and Bo Da Nam contributed equally.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-41086-4.
References
- 1.World Health Organization. Global tuberculosis report, 2017. WHO/HTM/TB/2017.23. Geneva, Switzerland. WHO, 2017. Accessed on October 18 (2018).
- 2.Humphreys H. Control and prevention of healthcare-associated tuberculosis: the role of respiratory isolation and personal respiratory protection. J. Hosp. Infect. 2007;66:1–5. doi: 10.1016/j.jhin.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Lee JE, et al. What strategy can be applied to the patients with culture positive tuberculosis to reduce treatment delay in a private tertiary healthcare center? Infect. Chemother. 2011;43:42–47. doi: 10.3947/ic.2011.43.1.42. [DOI] [Google Scholar]
- 4.World Health Organization. WHO policy on TB infection control in health-care facilities, congregate settings and households, 2009. WHO/HTM/TB2009.419. Geneva, Switzerland: WHO, 2009. Accessed on October 18 (2018). [PubMed]
- 5.Centers for Disease Control and Prevention. Recommendations and reports. Guidelines for preventing the transmission of mycobacterium tuberculosis in health-care facilities. MMWR. Recomm. Rep. 43, 1–132 (1994). [PubMed]
- 6.Greenway C. Delay in diagnosis among hospitalized patients with active TB-predictors and outcomes. Am. J. Resp. Crit. Care. Med. 2002;165:927–933. doi: 10.1164/ajrccm.165.7.2107040. [DOI] [PubMed] [Google Scholar]
- 7.Sreeramareddy CT, Panduru KV, Menten J, Ende JV. Time delays in diagnosis of pulmonary tuberculosis: a systematic review of literature. BMC. Infect. Dis. 2009;9:91. doi: 10.1186/1471-2334-9-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sho N, Shusaku T, Izumi K. Delayed isolation of smear-positive pulmonary tuberculosis patients in a Japanese acute care hospital. BMC. Pulm. Med. 2018;18:94. doi: 10.1186/s12890-018-0653-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu X, et al. Delays in care seeking, diagnosis and treatment among pulmonary TB patients in Shenzhen, China. Int. J. Tuberc. Lung. Dis. 2013;17:615–620. doi: 10.5588/ijtld.12.0231. [DOI] [PubMed] [Google Scholar]
- 10.Bogale S, Diro E, Shiferaw AM, Yenit MK. Factors associated with the length of delay with tuberculosis diagnosis and treatment among adult tuberculosis patients attending at public health facilities in Gondar town, Northwest, Ethiopia. BMC. Infect. Dis. 2017;17:145. doi: 10.1186/s12879-017-2240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rao VK, et al. Delays in the suspicion and treatment of tuberculosis among hospitalized patients. Ann. Intern. Med. 1999;130:404–411. doi: 10.7326/0003-4819-130-5-199903020-00004. [DOI] [PubMed] [Google Scholar]
- 12.Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC. Public. Health. 2008;15:8. doi: 10.1186/1471-2458-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rajagopalan S, Yoshikawa TT. Tuberculosis in the elderly. Z. Gerontol. Geriatr. 2000;33:374–38. doi: 10.1007/s003910070034. [DOI] [PubMed] [Google Scholar]
- 14.Park, W., Cha, J.O., Jang, S., Kim, J.H., Cho, K.S. Tuberculosis notification status in Korea in 2017. Division of TB and HIV/AIDS Control, Center for DiseasePrevention, KCDC. Available at http://www.cdc.go.kr/CDC/cms/content/mobile/35/79335_view.html. Accessed on October 18 (2018).
- 15.Jung KW, et al. Cancer status in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer. Res. Treat. 2018;50:303–316. doi: 10.4143/crt.2018.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takarinda KC, Harries AD. Tuberculosis treatment delays and associated factors within the Zimbabwe national tuberculosis programme. BMC. Public. Health. 2015;15:29. doi: 10.1186/s12889-015-1437-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rojpibulstit M, Kanjanakiritamrong J, Chongsuvivatwong V. Patient and health system delays in the diagnosis of tuberculosis in Southern Thailand after health care reform. Int. J. Tuberc. Lung. Dis. 2006;10:422–428. [PubMed] [Google Scholar]
- 18.Li Y, et al. Factors associated with patient, and diagnostic delays in Chinese TB patients: a systematic review and meta-analysis. BMC. Med. 2013;11:156. doi: 10.1186/1741-7015-11-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lipsky BA, Gates J, Tenover FC, Plorde JJ. Factors affecting the clinical value of microscopy for acid-fast bacilli. Rev. Infect. Dis. 1984;6:214–222. doi: 10.1093/clinids/6.2.214. [DOI] [PubMed] [Google Scholar]
- 20.Waitt CJ, et al. The effect of a tuberculosis chest X-ray image reference set on non-expert reader performance. Eur. Radiol. 2013;23:2459–2468. doi: 10.1007/s00330-013-2840-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kowada A. Cost effectiveness of high resolution computed tomography with interferon-gamma release assay for tuberculosis contact investigation. Eur. J. Radiol. 2013;82:1353–1358. doi: 10.1016/j.ejrad.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 22.Yeh JJ, et al. A high-resolution computer tomography scoring system to predict culture-positive pulmonary tuberculosis in the emergency department. PLoS. One. 2014;11:e93874. doi: 10.1371/journal.pone.0093847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Erkens CG, et al. Tuberculosis contact investigation in low prevalence countries: a European consensus. Eur. Respir. J. 2010;36:925–949. doi: 10.1183/09031936.00201609. [DOI] [PubMed] [Google Scholar]
- 24.Menzies D. Interpretation of repeated tuberculin tests. Boosting, conversion, and reversion. Am. J. Respir. Crit. Care. Med. 1999;159:15–21. doi: 10.1164/ajrccm.159.1.9801120. [DOI] [PubMed] [Google Scholar]
- 25.Nachiappan AC, et al. Pulmonary tuberculosis: role of radiology in diagnosis and management. Radiographics. 2017;37:52–72. doi: 10.1148/rg.2017160032. [DOI] [PubMed] [Google Scholar]
- 26.Jeong YJ, Lee KS. Pulmonary tuberculosis: Up-to-date imaging and management. AJR. Am. J. Roentgenol. 2008;191:834–844. doi: 10.2214/AJR.07.3896. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.