Abstract
Background
National guidelines require programmes use subjective assessments of social support when determining transplant suitability, despite limited evidence linking it to outcomes. We examined how transplant providers weigh the importance of social support for kidney transplantation compared with other factors, and variation by clinical role and personal beliefs.
Methods
The National survey of the American Society of Transplant Surgeons and the Society of Transplant Social Work in 2016. Using a discrete choice approach, respondents compared two hypothetical patient profiles and selected one for transplantation. Conditional logistic regression estimated the relative importance of each factor; results were stratified by clinical role (psychosocial vs medical/surgical providers) and beliefs (outcomes vs equity).
Results
Five hundred and eighy-four transplant providers completed the survey. Social support was the second most influential factor among transplant providers. Providers were most likely to choose a candidate who had social support (OR=1.68, 95% CI 1.50 to 1.86), always adhered to a medical regimen (OR=1.64, 95% CI 1.46 to 1.88), and had a 15 years life expectancy with transplant (OR=1.61, 95% CI 1.42 to 1.85). Psychosocial providers were more influenced by adherence and quality of life compared with medical/surgical providers, who were more influenced by candidates’ life expectancy with transplant (p<0.05). For providers concerned with avoiding organ waste, social support was the most influential factor, while it was the least influential for clinicians concerned with fairness (p<0.05).
Conclusions
Social support is highly influential in listing decisions and may exacerbate transplant disparities. Providers’ beliefs and reliance on social support in determining suitability vary considerably, raising concerns about transparency and justice.
INTRODUCTION
Kidney transplantation provides a unique example of rationing life-saving treatment in USA, requiring clinicians to consider multiple factors when deciding which patients to list for transplant. With growing organ scarcity and increasing oversight of outcomes, transplant centres must balance concerns for fairness and medical utility when selecting candidates.1 To do so, transplant teams rely on guidelines that Centers for Medicare and Medicaid Policy (CMS) and professional societies promulgate to clarify the factors (medical, demographic, psychological and lifestyle) that should be used to determine eligibility.2–5 There is little information about how influential subjective criteria are compared with other factors when evaluating candidates for kidney transplantation, especially the requirement for adequate social support.6,7 Social support can be defined as the services, care or encouragement provided by social network members (eg, spouses or partners, family, and friends). Although no formal guidelines establish a threshold for social support, inadequate social support is designated as a relative contraindication to kidney transplantation in USA by CMS and professional transplant organisations.4 Accordingly, patients who cannot demonstrate sufficient social support may be excluded from kidney transplantation, resulting in differential access to care.
Compared with other evidence-based criteria used to determine transplant eligibility, social support remains controversial because of its subjectivity, lack of uniform standards for assessment7 and because its relationship to post-transplant outcomes remains uncertain.8 A 2017 meta-analysis found that social support was not predictive of post-transplant adherence, and was inconsistently associated with other post-transplant outcomes.8 Use of social support raises both procedural and distributive justice concerns. First, due to ambiguous guidance, clinicians may vary significantly in their reliance on social support in decision making. Inconsistent use of social support in patient evaluation and listing decisions may significantly increase variation between as well as within centres, undermining uniformity and transparency in transplantation and raising procedural justice concerns. Second, use of social support may disproportionately affect vulnerable populations which are less able to identify caregivers with flexibility to leave work, with more strained support systems, and less able to self-finance home-based assistance. Further disadvantaging vulnerable populations by increasing barriers to transplantation raises distributive justice concerns, including the potential for exacerbating socioeconomic disparities.9,10 Understanding how providers with diverse perspectives value different criteria and the relative importance of social support criterion is critical for minimising variation in clinical practice and socioeconomic disparities in access to care.
Clinicians’ personal ethical beliefs may influence the extent to which they rely on the social support criterion. Recent increased scrutiny of outcomes by CMS may influence some clinicians to use social support in an attempt to prioritise outcomes above all else (utilitarian concerns). At the same time, the potential for contributing to disparities in access to the transplant waitlist may influence clinicians’ against using social support (distributive justice/fairness concerns).11–14 Clinical role may also contribute to attitudes about using social support in transplant evaluations, especially between clinicians directly involved in psychosocial evaluations (eg, social workers, psychologists, psychiatrists) and other medical or surgical clinicians (eg, nephrologists, transplant surgeons).
There is little information about how influential subjective criteria are compared with other factors when evaluating candidates for kidney transplantation, especially the requirement for adequate social support.6,7,15,16 The absence of established definitions and thresholds for social support leaves significant discretion and interpretation to clinicians. Using a discrete choice experiment, this study examines which factors are most important to transplant clinicians when prioritising patients for kidney transplantation. We examine the relative importance of social support compared with other listing criteria, and assess whether use of social support varies based on clinical role in the transplantation process and ethical beliefs related to balancing fairness with utility.
METHODS
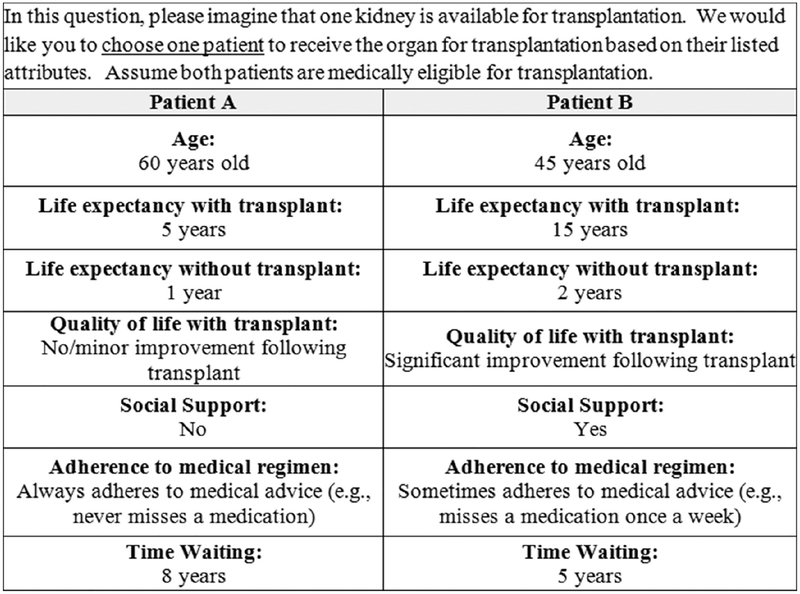
We developed a discrete choice experiment to examine how transplant clinicians rank the importance of social support when choosing a candidate for kidney transplantation, compared with other patient factors. The discrete choice experiment was included as part of a larger survey about transplant centres’ ongoing social support evaluation practices, and clinicians’ opinions about the evidence, importance and fairness of using social support in listing decisions. Discrete choice experiments are a well-established validated quantitative approach for eliciting preferences. They have been commonly used in the health policy context, especially in the context of complex medical decision making, where decision makers must consider multiple factors to arrive at a decision.17,18 A typical discrete choice question elicits preferences by asking respondents to choose between multiple attribute-based scenarios. In our survey, we asked respondents to choose between two hypothetical candidates to receive a kidney transplant, based on differences in key patient attributes (figure 1).
Figure 1.
Sample discrete choice question.
Sample
We surveyed the American Society of Transplant Surgeons (ASTS) and Society for Transplant Social Work in October 2016 to gain diverse perspectives from clinicians with different roles in listing decisions and candidate evaluations. Participants received an email containing a description of the study, consent form and anonymous survey link.
Survey development
Following established guidelines for conducting discrete choice expreiments (DCEs),19 we identified 20 possible attributes included in transplant listing decisions through a review of clinical guidelines and the literature. This attribute list was narrowed through iterative deliberations by a group of stake-holders (transplant surgeon, psychologist, social worker, ethicist and behavioural scientists; n=6) who ranked attributes by importance for transplant listing decisions and considered independence from other attributes.18 Rankings were qualitatively discussed until consensus was reached. In accordance with methodological recommendations to minimise respondents’ cognitive burden,20seven attributes were selected: life expectancy with transplant, life expectancy without transplant, quality of life with transplant, adherence to medial regimen, time on the waiting list, social support and age (table 1). Attributes were defined and two to three, levels representing meaningful differences within attributes, were assigned following a literature review and discussion among stakeholders (ie, 20 years, 40 years and 60 years for the ‘age’ attribute)18 (table 1). We conducted cognitive pretests with transplantation experts (n=6) to ensure that respondents understood the survey questions as intended, and revised the DCE attributes and levels based on feedback.
Table 1.
Discrete choice experiment: transplant candidate profile attributes and levels
| Attribute | Definition | levels |
|---|---|---|
| Life expectancy with transplant | Number of years patient is expected to live posttransplant | 5 years |
| 10 years | ||
| 15 years | ||
| Quality of life with transplant | Level of functioning achieved with transplant in the long term | No/slight improvement |
| Significant improvement | ||
| Time on waiting list | Time already spent waiting on the transplant list (time since candidacy for transplant) | 3 years |
| 5 years | ||
| 8 years | ||
| Life expectancy without transplant | Number of years patient is expected to live if he or she does not receive the organ | 3 years |
| 2 years | ||
| 1 year | ||
| Adherence to medical regimen | How well a patient follows medical advice for transplant medications | Sometimes |
| Often | ||
| Always | ||
| Age | Patient’s age at the time of transplant | 60 years |
| 40 years | ||
| 20 years | ||
| Social support | Whether a patient has someone to look after him/ her after organ transplantation and assist with needed post-transplant care | No |
| Yes |
Survey design
Respondents were presented with questions comparing two hypothetical transplant candidates described by varying levels of the seven attributes (hereafter ‘candidate profiles’). For each question, respondents were instructed, ‘Please imagine that one kidney is available for transplantation. We would like you to choose one patient to receive the organ for transplantation based on their listed attributes. Assume both patients are medically eligible for transplantation’. An example DCE question is shown in figure 1. Candidate profiles were generated using a fractional factorial design, selecting the subset of attribute and level combinations that ensured attribute balance and statistical efficiency.19 We identified the best orthogonal combination of attribute levels that minimised correlation between attributes and levels, and evaluated design efficiency using the relative D-efficiency Score in SAS.19 Using a simulation model prior to fielding, we tested the chosen design for balance, efficiency and to estimate needed sample size.21 Simulation results indicated a minimum sample of 270 respondents was needed. Respondents were evenly randomised into one of nine blocks of four discrete choice questions. To maintain statistical efficiency and design balance in subgroup analyses, randomisation was stratified by clinician involvement with psychosocial evaluation and familiarity with kidney transplantation.
Demographic information (organ transplant programme, United Network for Organ Sharing (UNOS) region, gender, years in practice) was collected. Personal beliefs related to social support were assessed based on dis/agreement with the following statements: ‘Using social support to determine transplant eligibility is fair’; and ‘Social support is especially important in listing decisions because of the need to avoid wasting organs.’ Responses were measured using a 5-point scale, from ‘strongly disagree’ to ‘strongly agree’. These questions are based on measures widely used in surveys about ethical beliefs and rationing of healthcare.22–24 We assessed respondents’ confidence in using social support to determine transplant eligibility; measured from ‘extremely confident’ to ‘not at all confident’. We also included a free text field for comments. The survey was fielded using Qualtrics (2015, Provo, Utah, USA) and analyses were conducted using Stata V.14, College Station, Texas, USA.
Statistical analyses
We used conditional logistic regression to calculate the odds that a respondent would choose a particular candidate profile given the attribute levels presented, accounting for matched comparisons. The dependent variable was the profile chosen by the respondent and independent variables included attribute levels in the profiles. We used effects coding to represent the presence or absence of each attribute level. With effects coding, the estimated independent effects for each attribute level represent the incremental effect over the mean for respondents.25 We adjusted for the within-subject correlation using bootstrapping with replacement methods.26 Conditional attribute importance reflects the difference between the highest and lowest regression parameter estimates for each attribute, divided by the sum of all differences. This metric gives an estimate of the overall importance of each attribute.27
We conducted stratified analyses based on clinical role (psychosocial provider vs not), belief that using the social support criterion is fair (agreed/disagreed), belief that social support is important to avoid wasting organs (agreed/disagreed) and confidence in the social support criterion (confident/not confident). Neutral responses were included into the disagree category for stratified regression analyses, and sensitivity analyses tested removing these responses from the analysis. Likelihood ratio tests were used to compare statistical differences in the importance of attributes between subgroups. Additional sensitivity analyses assessed the validity of responses from respondents who answered two or fewer discrete choice questions (n=96); those unfamiliar with kidney transplantation (n=73); and respondents who answered uniformly in the DCE (eg, always selecting ‘Patient B’; n=47).
RESULTS
Survey sample
Overall, 627 people completed the survey (41% response rate) of whom 93% completed the DCE (n=584). Respondent characteristics are displayed in table 2. Approximately half (52.6%) of respondents were male, and 48.3% (n=282) were involved in psychosocial evaluation of transplant candidates (hereafter psychosocial providers). Of psychosocial providers, 66% were social workers and 29% were medical doctors (MDs). Medical/surgical providers that were not involved directly in psychosocial evaluation comprised 51.7% of the sample (n=302). Most respondents were involved in kidney transplantation (71.6%), followed by liver (52.9%), pancreas (38.7%), heart (14.4%) and lung (7.5%), with most involved in multiple programmes.
Table 2.
Sample descriptive statistics
| Full sample | Involved In psychosocial evaluation | Not involved in psychosocial evaluation | ||||
|---|---|---|---|---|---|---|
| N | Per cent | N | Per cent | N | Per cent | |
| Total | 584 | 282 | 48.3 | 302 | 51.7 | |
| Gender (n=489) | ||||||
| Male | 257 | 52.7 | 82 | 14.4 | 175 | 30.0 |
| Female | 232 | 47.4 | 160 | 27.4 | 72 | 12.3 |
| UNOS region (n=462) | ||||||
| Region 1 | 49 | 10.6 | 23 | 3.9 | 26 | 4.5 |
| Region 2 | 54 | 11.7 | 22 | 3.8 | 32 | 5.5 |
| Region 3 | 25 | 5.4 | 12 | 2.1 | 13 | 2.2 |
| Region 4 | 36 | 7.8 | 24 | 4.1 | 12 | 2.1 |
| Region 5 | 62 | 13.5 | 31 | 5.3 | 31 | 5.3 |
| Region 6 | 23 | 4.8 | 10 | 1.7 | 12 | 2.1 |
| Region 7 | 40 | 8.6 | 19 | 3.3 | 21 | 3.6 |
| Region 8 | 33 | 7.2 | 13 | 2.2 | 20 | 3.4 |
| Region 9 | 29 | 6.3 | 15 | 2.6 | 14 | 2.4 |
| Region 10 | 48 | 10.4 | 26 | 4.5 | 22 | 3.8 |
| Region 11 | 63 | 13.7 | 36 | 6.2 | 27 | 4.6 |
| Organ programme* | ||||||
| Kidney | 418 | 71.6 | 180 | 30.8 | 238 | 40.8 |
| Liver | 309 | 52.9 | 114 | 19.5 | 195 | 33.4 |
| Heart | 84 | 14.4 | 65 | 11.1 | 19 | 3.3 |
| Lung | 44 | 7.5 | 26 | 4.5 | 18 | 3.1 |
| Pancreas | 226 | 38.7 | 81 | 13.9 | 145 | 24.8 |
| Other | 54 | 9.3 | 28 | 4.8 | 26 | 4.5 |
| Confident in listing guidelines (n=419) | ||||||
| Confident | 178 | 30.5 | 176 | 30.1 | 134 | 22.9 |
| Not confident | 241 | 41.3 | 94 | 16.1 | 144 | 24.7 |
| Believe using social support in listing is fair (n=562) | ||||||
| Agree | 422 | 72.3 | 214 | 36.6 | 200 | 34.2 |
| Disagree | 79 | 13.5 | 24 | 4.1 | 55 | 9.4 |
| Neutral | 61 | 10.5 | 34 | 5.8 | 35 | 6.0 |
| Believe using social support in listing is important to avoid organ waste (n=560) | ||||||
| Agree | 392 | 67.1 | 193 | 33.0 | 197 | 33.7 |
| Disagree | 54 | 9.2 | 26 | 4.5 | 28 | 4.8 |
| Neutral | 114 | 19.5 | 51 | 8.7 | 63 | 10.8 |
| Mean | SD | Mean | SD | Mean | SD | |
| Years in practice (n=484) | 16.5 | 11.2 | 16.1 | 10.9 | 16.9 | 11.4 |
| Years in transplantation (n=486) | 13.5 | 10.4 | 11.3 | 9.8 | 16.1 | 10.4 |
| Average psychosocial evaluations per month (n=238) | 19.9 | 20.2 | 20.0 | 20.4 | 0 | N/A |
Percentages are of full sample (n=584) and may add up to <100% as responses to questions were not required. Remaining respondents did not answer the question.
Percentage may add up to >100%, as respondents were allowed to select multiple organs.
Most providers (88.7%) reported having used inadequate social support along with other factors when making listing decisions. Most (86.3%) agreed or strongly agreed that patients with inadequate support are evaluated less favourably for transplantation than similar patients with greater support. Most providers (71.4%) perceived social support was important for preventing organ waste (utility). Yet, a quarter of respondents (24.3%) thought using social support to determine transplant eligibility was unfair or were unsure about its fairness. Nearly half of respondents (42.4%) were only somewhat or not at all confident in using social support to determine transplant suitability.
Discrete choice experiment results
Overall, a candidate’s life expectancy with transplant, adherence to medical regimen and social support were the most influential factors in transplant decision making (table 3; attribute importance estimates are shown as percentages and convey the overall influence each attribute had in the respondents’ profile choice, conditioned on the particular attributes and levels in the survey, with higher numbers conveying more relative influence). Compared with the mean rate of choosing a profile, respondents were 1.68 times more likely to choose a profile of a transplant candidate that had social support (95% CI 1.50 to 1.86), 1.64 times more likely to select a profile of a candidate who always adheres to his/her medical regimen (95% CI 1.46 to 1.88) and 1.61 times more likely to select a profile of a candidate with a 15 years life expectancy (CI 1.42 to 1.85).
Table 3.
Results from the discrete choice experiment conditional logistic regression
| Attribute | Level | or | P value | 95% CI | Conditional attribute importance |
|---|---|---|---|---|---|
| Life expectancy with transplant | 5 years | 0.56 | <0.001 | 0.49 to 0.62 | 21% |
| 10 years | 1.10 | <0.001 | 1.00 to 1.24 | ||
| 15 years | 1.61 | <0.001 | 1.42 to 1.85 | ||
| Quality of life with transplant | No/slight improvement | 0.66 | <0.001 | 0.49 to 0.62 | 16% |
| Significant improvement | 1.51 | <0.001 | 1.38 to 1.64 | ||
| Time waiting | 3 years | 0.76 | <0.001 | 0.68 to 0.87 | 11% |
| 5 years | 0.99 | 0.698 | 0.87 to 1.10 | ||
| 8 years | 1.33 | <0.001 | 1.18 to 1.50 | ||
| Life expectancy without transplant | 3 years | 0.86 | 0.011 | 0.76 to 0.97 | 5% |
| 2 years | 1.07 | 0.312 | 0.95 to 1.17 | ||
| 1 year | 1.09 | 0.134 | 0.97 to 1.25 | ||
| Adherence to medical regimen | Sometimes | 0.57 | <0.001 | 0.50 to 0.64 | 21% |
| Often | 1.07 | 0.329 | 0.94 to 1.19 | ||
| Always | 1.64 | <0.001 | 1.46 to 1.88 | ||
| Age | 60 years | 0.87 | 0.010 | 0.78 to 0.97 | 5% |
| 40 years | 1.01 | 0.746 | 0.91 to 1.14 | ||
| 20 years | 1.13 | 0.036 | 1.01 to 1.27 | ||
| Social support | No | 0.60 | <0.001 | 0.54 to 0.68 | 20% |
| Yes | 1.68 | <0.001 | 1.50 to 1.86 |
Modelled with effects coding. N = 497. Pseudo R2 = 0.2406. Attribute importance estimates are shown as percentages and convey the overall influence each attribute had in respondents’ profile choice, conditioned on the particular attributes and levels in the survey, with higher numbers conveying more relative influence.
Importantly, short expected life expectancy following transplantation and lack of social support were similarly influential in providers’ listing decisions. Respondents were less likely to select candidates who were expected to survive for only 5 years (OR=0.56; 95% CI 0.49 to 0.62) or who had no social support (OR=0.60; 95% CI 0.54 to 0.68). Life expectancy without transplant (a measure of urgency) and the age of the transplant candidate were the least influential attributes, and were not statistically significant. Sensitivity analyses with a more restricted sample yielded similar results.
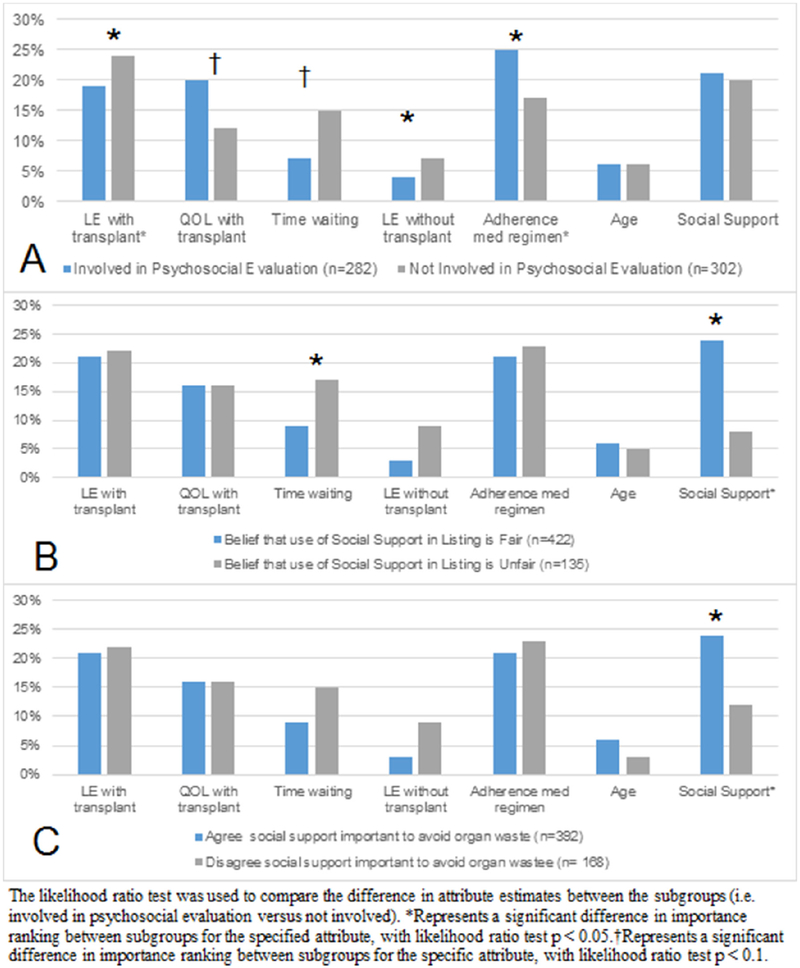
Results by personal beliefs
The influence of social support in transplant decisions varied significantly based on clinicians’ stated beliefs as well as their confidence in their centre’s listing guidelines (table 4, figure 2). Social support was the most influential factor (24% attribute importance) among clinicians who believed that social support criterion was important to avoid organ waste (n=392), while it was the third least influential factor (12% attribute importance) in decision making among respondents who disagreed that social support was important for preventing organ waste (n=168; p<0.05 for statistical difference between groups). Social support was one of the most influential factors in decision making among clinicians who believed the use of social support was fair, (24% conditional attribute importance; n=422) but was one of the least influential factors in decisions among clinicians who did not believe that social support is fair (8% conditional attribute importance; n=135; p<0.05 for difference between groups). Social support was also significantly less influential in the decision making of clinicians who lacked confidence in their centre’s listing guidelines compared with those who stated confidence in guidelines (table 4; 12% vs 26% conditional attribute importance, respectively; p<0.05 difference between groups).
Table 4.
Conditional attribute importance: subgroup results by involvement in psychosocial evaluation, belief in fairness of listing, agreement with importance of avoiding organ waste and guideline confidence
| Involvement in psychosocial evaluation | Believe social support in listing is fair | Believe social support is important in listing to avoid organ waste | Confidence in listing guidelines | |||||
|---|---|---|---|---|---|---|---|---|
| Involved | Not involved | Agree | Disagree | Agree | Disagree | Confident | Not confident | |
| N | 282 | 302 | 422 | 135 | 392 | 168 | 178 | 241 |
| Pseudo R2 | 0.244 | 0.265 | 0.259 | 0.244 | 0.260 | 0.236 | 0.267 | 0.247 |
| Attribute | % Importance | % Importance | % Importance | % Importance | ||||
| Life expectancy with transplant | 19* | 24* | 21 | 22 | 21 | 22 | 19 | 24 |
| Quality of life with transplant | 20† | 12† | 16 | 16 | 16 | 16 | 16 | 16 |
| Time waiting | 7† | 15† | 9* | 17 | 9 | 15 | 9 | 15 |
| Life expectancy without transplant | 4* | 7* | 3 | 9 | 3 | 9 | 2 | 8 |
| Adherence to medical regimen | 25* | 17* | 21% | 23 | 21 | 23 | 22 | 20 |
| Age | 6 | 6 | 6 | 5 | 6 | 3 | 5 | 5 |
| Social support | 21 | 20 | 24* | 8 | 24* | 12* | 26* | 12* |
Attribute importance estimates are shown as percentages and convey the overall influence each attribute had in respondents’ profile choice, conditioned on the particular attributes and levels in the survey, with higher numbers conveying more relative influence. The likelihood ratio test was used to compare the difference in attribute estimates between the subgroups (ie, involved in psychosocial evaluation versus not involved).
Represents a significant difference in importance ranking between subgroups for the specified attribute, with likelihood ratio test p<0.05.
Represents a significant difference in importance ranking between subgroups for the specific attribute, with likelihood ratio test p<0.1.
Figure 2.
Graphs of conditional logistic regression model results, stratified by clinical role (A), belief in fairness of using social support criteria (B), agreement with importance of avoiding organ waste (C). QOL, Quality of life; LE, Life expectancy.
Results by clinical role
When the sample was stratified by clinical role, comparing psychosocial providers and medical/surgical providers, differences emerged, although social support remained the second most influential attribute for both groups. Psychosocial providers were 1.69 times more likely (95% CI 1.41 to 1.92) and medical/surgical providers were 1.79 times more likely (95% CI 1.57 to 2.04) to select a candidate with social support (table 4). Overall, medical/surgical providers were most influenced by the candidate’s life expectancy with transplant (24% attribute importance), followed by social support (20% attribute importance) and adherence to medical regimen (17% attribute importance) (table 4, full analysis results online supplementary appendices 1–5). Among psychosocial providers, the most influential attributes were adherence to medical regimen (attribute importance score: 25%), social support (21%) and quality of life with transplant (20%). Compared with medical/surgical providers, psychosocial providers were significantly more likely to prioritise medication adherence (p<0.05) and quality of life (p<0.10) in their choices. By contrast, medical/surgical providers were significantly more likely to prioritise life expectancy with transplant (p<0.05), compared with psychosocial providers.
DISCUSSION
Clinicians assign significant importance to objectively measured factors influencing patient and graft survival rates, in accordance with regulatory agencies that require minimum risk-adjusted outcomes.28 Yet, little is known about how transplant clinicians consider subjective factors like social support when determining whether to waitlist patients for transplantation. Our findings reveal that social support is highly influential in shaping the opinions of medical/surgical providers and psychosocial evaluators alike. This finding is striking, given the limited evidence base confirming the impact of social support on transplant outcomes and its potential for increasing disparities.8 Vague, subjective criteria may result in shifting standards, and inconsistent treatment. Because reliance on social support is unpredictable, not evidence-based, and not always transparent, use of social support may contribute to unequal access to transplantation.
Social support was the second most important factor in listing decisions irrespective of clinical role. with psychosocial evaluators most influenced by adherence to medication, and medical/surgical providers most influenced by life expectancy post-transplant. Surgeons’ preferences for life expectancy after transplant may stem from concerns over transplanting too many high-risk patients, which can lead to lower than expected patient and graft survival rates, jeopardising the transplant programme’s status with regulatory agencies and payers, including centre of excellence designations. Preferences may also be affected by clinicians’ awareness of the organ shortage and the imperative of avoiding futile transplants. By contrast, concern over adherence and quality of life may be more salient to social workers given the scope of their practice and their role in supporting patients following transplantation.
Clinicians’ personal beliefs and confidence in their centre’s evaluation guidelines strongly determined their reliance on social support in listing decisions Clinicians who expressed more utilitarian values including perceived implications for organ waste were more likely to use social support in listing decisions, whereas others more concerned about fairness seldom used social support in listing decisions. Specifically, among clinicians who perceived the social support criterion to be unfair, social support was among the least influential factors, compared with the most influential factor among those concerned with utility (preventing organ waste). Greater confidence in procedures related to social support evaluations was associated with greater reliance on social support in listing decisions. These findings underscore procedural justice concerns associated with subjective criteria because patients seeking life-saving transplants may receive radically different treatment depending on clinicians’ personal beliefs and not on specified criteria.
Apparent discordance in use of social support by ethical beliefs and confidence in the social support criterion may result in significant variation in patient experiences and should be further examined in the context of persistent disparities in access to transplantation. Although the National Organ Transplant Act29 mandates equal access to life-saving organs, vulnerable populations continue to face barriers in access to the waitlist.30,31 Persons of low socioeconomic status, racial and ethnic minorities, and those living in rural areas face disproportionate difficulty successfully completing transplant evaluations.12,13,15,32–36 Because demonstrating social support may be correlated with socioeconomic status, race, ethnicity and age, this criterion may increase and reinforce barriers to care for underserved populations.34,37 The family structure and marriage rates seen in particular groups, both of which may influence the ability to demonstrate social support, may contribute to this.9 For example, blacks (32%) are less likely than whites (56%) to be married, and this gap has increased significantly over time.38 Patients in rural areas and those whose social network has limited job security or flexibility may also face greater difficulty demonstrating social support.11,39 Future research should examine differences in the ability of patients from undeserved backgrounds to meet the threshold for social support.
Lack of clarity about how to evaluate social support and its importance in determining listing status leaves this criterion increasingly susceptible to implicit bias and may also contribute to disparities. Implicit bias and subsequent reliance on stereotypes is particularly problematic when individuals face high levels of cognitive load and stress, as is the case in transplantation, limiting providers’ ability to filter bias from their thoughts and interactions.40 While attention is focused on the high stress, fast-paced medical environment and controlling explicit bias, physicians’ are vulnerable to implicit bias.41 Implicit bias refers to ‘the attitudes or stereotypes that affect our understanding, actions, and decisions in an unconscious manner. These biases, which encompass both favourable and unfavourable assessments, are activated involuntarily and without an individual’s awareness or intentional control’.42 Use of the social support criterion may reinforce implicit biases against people who are less socially connected, who do not have family or friends advocating on their behalf, and who may be part of a stigmatised population who often have fewer social contacts (ie, persons with persistent mental illness, history of substance abuse).43 As such, the social support criterion may amplify existing biases and sanction them, entrenching unequal treatment as part of the transplant evaluation process, undermining both procedural and distributive justice.
The impact of implicit bias in medicine and surgery is documented in a growing literature, offering new explanations for the paradox that well-intentioned clinicians sometimes treat marginalised patients worse than others.40,44,45 For example, Green et al found that, even among physicians with no explicit racial bias, most displayed negative implicit bias towards black patients.46 Moreover, while explicit bias did not affect behaviour, physicians with stronger implicit bias were less likely to recommend a preferred treatment for black compared with white patients, although both presented identical symptoms. Similarly, implicit bias has been associated with lower empathy towards marginalised patients, affecting care recommendations.45 Taken together, these findings suggest that the social support criterion reinforces a blind spot among clinicians by sanctioning non-evidence-based and potentially stigmatising criterion that aligns with clinicians’ implicit bias. Implicit bias operates on the subconscious level, making it difficult to recognise its existence and use. Studies linking bias to racial disparities in access to kidney transplantation illustrate the need for reviewing eligibility criteria and improving national standards, including those related to social support.47,48 Future studies should qualitatively examine how clinicians use social support to determine eligibility, and their beliefs around fairness, efficiency and equity to better understand the cognitive processes, emotions and organisational factors contributing to waitlisting decisions. Further exploration of the mechanisms by which clinicians legitimise the use of a criterion which they believe may be unfair is also needed to effectively tailor interventions to improve equity in evaluations.
Our study is not without limitations. Although our sample is balanced nationally, the ASTS membership did not include a sufficient number of nephrologists, and as such, we cannot examine whether they hold different preferences. However, although the medical/surgical providers and psychosocial providers in our sample have distinct roles, training and preferences for many factors, they did not differ with respect to their prioritisation of social support. Future work should examine preferences of nephrologists. While our study includes questions about ethical beliefs commonly discussed in the context of organ transplantation, our survey did not define fairness to avoid biasing providers’ responses. Future studies should examine differences in ethical ideologies more comprehensively to determine how these influence other aspects of clinical decision making. Finally, patient perspectives were not included in this paper. Future studies should examine public perceptions about using social support to determine transplant eligibility.
Our findings should be considered in conjunction with recent and proposed changes to regulatory oversight of solid organ transplantation in USA. Some suggest that greater regulatory scrutiny of transplant programmes with poorer than expected outcomes is harmful, and may lead to risk aversion on the part of transplant programmes.49 Risk averse programmes may undertake fewer high-risk transplants, turning away patients who could benefit, and resulting in unnecessary organ waste. While studies have examined potential harms of increased regulatory scrutiny on organ waste, the potential impact for vulnerable patients seeking transplantation remains unclear. One consequence of heightened scrutiny and lack of clear guidelines for using social support to determine eligibility for transplantation is greater susceptibility to implicit bias and lack of uniformity in care. Given the poor evidence base, lack of transparency and potential to increase disparities, the transplant community should re-examine use of social support in patient evaluation and improve definitions and assessments to ensure transparency and equity in access to transplantation.
Acknowledgements
The authors thank Meghan Olsen and Kelsey Berry for their dedicated and skilled research assistance, and Norma Terrin for statistical guidance.
Funding Financial support for this study was provided by the Greenwall Foundation through their “Making a Difference” grants. KL also received funding support from the Greenwall Faculty Scholars program from the National Center for Advancing Translational Sciences, National Institutes of Health, Award Number KL2TR001063. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Footnotes
Publisher's Disclaimer: Disclaimer The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Competing interests None declared.
Patient consent Not required.
Ethics approval This study was approved by the Tufts University Institutional Review Board in January 2016.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
- 1.United Network on Organ Sharing (UNOS). Ethical principles in the allocation of human organs. Virginia: United Network on Organ Sharing, 1992. [Google Scholar]
- 2.Thapar M, Bonkovsky HL. Indications for liver transplant and AASLD guidelines. Hepatology 2015;61:408. [DOI] [PubMed] [Google Scholar]
- 3.Weill D, Benden C, Corris PA, et al. A consensus document for the selection of lung transplant candidates: 2014--an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant 2015;34:1–15. [DOI] [PubMed] [Google Scholar]
- 4.Kasiske BL, Cangro CB, Hariharan S, et al. The evaluation of renal transplantation candidates: clinical practice guidelines. Am J Transplant 2001;2:5–95. [PubMed] [Google Scholar]
- 5.Centers for Medicare and Medicaid Services. Services DoHaHIn: , ed. Interpretive guidelines for the organ transplant Conditions of Participation (CoPs) 42 CFR. Baltimore, MD: Department of Health and Human Services, 2016. [Google Scholar]
- 6.Tong A, Hanson CS, Chapman JR, et al. The preferences and perspectives of nephrologists on patients’ access to kidney transplantation: a systematic review. Transplantation 2014;98:682–91. [DOI] [PubMed] [Google Scholar]
- 7.Batabyal P, Chapman JR, Wong G, et al. Clinical practice guidelines on waitlisting for kidney transplantation: consistent and equitable? Transplantation 2012;94:703–13. [DOI] [PubMed] [Google Scholar]
- 8.Ladin K, Daniels A, Osani M, et al. Is social support associated with post-transplant medication adherence and outcomes? A systematic review and meta-analysis. Transplant Rev 2018;32:16–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ladin K, Hanto DW. Understanding disparities in transplantation: do social networks provide the missing clue? Am J Transplant 2010;10:472–6. [DOI] [PubMed] [Google Scholar]
- 10.Moore G Structural Determinants of Men’s and Women’s Personal Networks. Am Sociol Rev 1990;55:726–35. [Google Scholar]
- 11.Ladin K, Rodrigue JR, Hanto DW. Framing disparities along the continuum of care from chronic kidney disease to transplantation: barriers and interventions. Am J Transplant 2009;9:669–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Norris KC, Agodoa LY. Reducing disparities in assessment for kidney transplantation. Clin J Am Soc Nephrol 2012;7:1378–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joshi S, Gaynor JJ, Bayers S, et al. Disparities among Blacks, Hispanics, and Whites in time from starting dialysis to kidney transplant waitlisting. Transplantation 2013;95:309–18. [DOI] [PubMed] [Google Scholar]
- 14.Patzer RE, Perryman JP, Schrager JD, et al. The role of race and poverty on steps to kidney transplantation in the Southeastern United States. Am J Transplant 2012;12:358–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johansen KL, Zhang R, Huang Y, et al. Association of race and insurance type with delayed assessment for kidney transplantation among patients initiating dialysis in the United States. Clin J Am Soc Nephrol 2012;7:1490–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tong A, Howard K, Wong G, et al. Nephrologists’ perspectives on waitlisting and allocation of deceased donor kidneys for transplant. Am J Kidney Dis 2011;58:704–16. [DOI] [PubMed] [Google Scholar]
- 17.Clark MD, Determann D, Petrou S, et al. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics 2014;32:883–902. [DOI] [PubMed] [Google Scholar]
- 18.Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health--a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health 2011;14:403–13. [DOI] [PubMed] [Google Scholar]
- 19.Reed Johnson F, Lancsar E, Marshall D, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR conjoint analysis experimental design good research practices task force. Value Health 2013;16:3–13. [DOI] [PubMed] [Google Scholar]
- 20.Abiiro GA, Leppert G, Mbera GB, et al. Developing attributes and attribute-levels for a discrete choice experiment on micro health insurance in rural Malawi. BMC Health Serv Res 2014;14:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuhfeld WF. Marketing Research Methods in the SAS: Experimental Design, Choice, Conjoint, and Graphical Techniques. North Carolina, USA: SAS Institute Inc, 2010. [Google Scholar]
- 22.Tyler T Why people obey the law. Princeton University Press: Princeton, 1990. [Google Scholar]
- 23.Boulware LE, Troll MU, Wang NY, et al. Perceived transparency and fairness of the organ allocation system and willingness to donate organs: a national study. Am J Transplant 2007;7:1778–87. [DOI] [PubMed] [Google Scholar]
- 24.Levi M, Sacks A, Tyler T, et al. measuring legitimating beliefs. Am Behav Sci 2009;53:354–75. [Google Scholar]
- 25.Bech M, Gyrd-Hansen D. Effects coding in discrete choice experiments. Health Econ 2005;14:1079–83. [DOI] [PubMed] [Google Scholar]
- 26.Efron B Better Bootstrap Confidence Intervals. J Am Stat Assoc 1987;82:171–85. [Google Scholar]
- 27.Hollin IL, Peay HL, Bridges JF. Caregiver preferences for emerging duchenne muscular dystrophy treatments: a comparison of best-worst scaling and conjoint analysis. Patient 2015;8:19–27. [DOI] [PubMed] [Google Scholar]
- 28.Adler JT, Axelrod DA. Regulations’ Impact on Donor and Recipient Selection for Liver Transplantation: How Should Outcomes be Measured and MELD Exception Scores be Considered? AMA J Ethics 2016;18:133–42. [DOI] [PubMed] [Google Scholar]
- 29.Stat. National Organ Transplantation Act of 1984, Pub L. 98–507, 98: Stat, 1984. 2339–2348 (October 19, 1984). [Google Scholar]
- 30.Salter ML, Gupta N, King E, et al. Health-related and psychosocial concerns about transplantation among patients initiating dialysis. Clin J Am Soc Nephrol 2014;9:1940–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salter ML, Orandi B, McAdams-DeMarco MA, et al. Patient- and provider-reported information about transplantation and subsequent waitlisting. J Am Soc Nephrol 2014;25:2871–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldfarb-Rumyantzev AS, Sandhu GS, Baird B, et al. Effect of education on racial disparities in access to kidney transplantation. Clin Transplant 2012;26:74–81. [DOI] [PubMed] [Google Scholar]
- 33.Schold JD, Gregg JA, Harman JS, et al. Barriers to evaluation and wait listing for kidney transplantation. Clin J Am Soc Nephrol 2011;6:1760–7. [DOI] [PubMed] [Google Scholar]
- 34.Axelrod DA, Guidinger MK, Finlayson S, et al. Rates of solid-organ wait-listing, transplantation, and survival among residents of rural and urban areas. JAMA 2008;299:202–7. [DOI] [PubMed] [Google Scholar]
- 35.Schold JD, Heaphy EL, Buccini LD, et al. Prominent impact of community risk factors on kidney transplant candidate processes and outcomes. Am J Transplant 2013;13:2374–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scholz U, Klaghofer R, Dux R, et al. Predicting intentions and adherence behavior in the context of organ transplantation: gender differences of provided social support. J Psychosom Res 2012;72:214–9. [DOI] [PubMed] [Google Scholar]
- 37.Browne T The relationship between social networks and pathways to kidney transplant parity: evidence from black Americans in Chicago. Soc Sci Med 2011;73:663–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taylor P The decline of marriage and rise of new families. social and demographic trends project. Washington, DC: Pew Research Center, 2010. [Google Scholar]
- 39.Axelrod DA, Dzebisashvili N, Schnitzler MA, et al. The interplay of socioeconomic status, distance to center, and interdonor service area travel on kidney transplant access and outcomes. Clin J Am Soc Nephrol 2010;5:2276–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.In: Smedley B, Stith A, Nelson A, eds. Unequal treatment: confronting racial and ethnic disparities in health care. Washington DC: National Academy Press, 2003. [PubMed] [Google Scholar]
- 41.Dovidio JF, Fiske ST. Under the radar: how unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. Am J Public Health 2012;102:945–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bias KIftSoraEUI. Implicit Bias. 2016. http://kirwaninstitute.osu.edu/research/understanding-implicit-bias.
- 43.Marotta S, Ladin K. Quality support: Evidence of bias against patients with non-traditional caregivers in transplant listing determinations Annual Meeting of the Association for Psychological Science. San Francisco, CA: Association for Psychological Science, 2018. [Google Scholar]
- 44.Mathur VA, Richeson JA, Paice JA, et al. Racial bias in pain perception and response: experimental examination of automatic and deliberate processes. J Pain 2014;15:476–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haider AH, Sexton J, Sriram N, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA 2011;306:942–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Green CR, Anderson KO, Baker TA, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med 2003;4:277–94. [DOI] [PubMed] [Google Scholar]
- 47.Ayanian JZ, Cleary PD, Weissman JS, et al. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med 1999;341:1661–9. [DOI] [PubMed] [Google Scholar]
- 48.Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation--clinically appropriate or due to underuse or overuse? N Engl J Med 2000;343:1537–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kasiske BL, Salkowski N, Wey A, et al. Potential Implications of Recent and Proposed Changes in the Regulatory Oversight of Solid Organ Transplantation in the United States. Am J Transplant 2016;16:3371–7. [DOI] [PMC free article] [PubMed] [Google Scholar]