Abstract
Objective:
The number of individuals transitioning from correctional facilities to community in later life (age ≥50) is increasing. We sought to determine if later-life prison release is a risk factor for suicidal behavior and death by accidental injury, including drug overdose.
Design:
Retrospective cohort study.
Setting:
U.S. Department of Veterans Affairs and Medicare healthcare systems, 2012–2014.
Participants:
Veterans age ≤50 released from correctional facilities (N = 7,671 reentry veterans) and those never incarcerated (N = 7,671).
Methods:
Dates of suicide attempt and cause-specific mortality defined using the National Suicide Prevention Applications Network and the National Suicide Data Repository, respectively.
Results:
Later-life prison release was associated with increased risk of suicide attempt (599.7 versus 134.7 per 100,000per year; adjusted hazard ratio [HR] 3.45; 95% confidence interval [CI] 2.24–5.32; p < 0.001, Wald χ2=31.58, degrees of freedom [df] = 1), death by drug overdose (121.7 versus 43.5; adjusted HR 3.45; 95% CI 1.37–8.73; p = 0.009, Wald χ2 = 6.86, df=1), and other accidental injury (126.0 versus 39.1; adjusted HR 3.13; 95% CI 1.28–7.69;p = 0.013, Wald χ2 = 6.25, df= 1), adjusting for homelessness, traumatic brain injury, medical and psychiatric conditions, and accounting for competing risk of other deaths. Suicide mortality rates were observed as nonsignificant between re-entry veterans and those never incarcerated (30.4 versus 17.4, respectively; adjusted HR 2.40; 95% CI 0.51 –11.24; p = 0.266, Wald χ2 = 1.23, df= 1).
Conclusion:
Older re-entry veterans are at considerable risk of attempting suicide and dying by drug overdose or other accidental injury. This study highlights importance of prevention and intervention efforts targeting later-life prison-to-community care transitions.
Keywords: Suicide, suicide attempt, overdose, prisoners, veterans, late-life
INTRODUCTION
With minimum sentencing laws, more arrests in later age, and population aging, the number of incarcerated persons aged 50 and older in the United States has increased exponentially.1,2 As most inmates are eventually released (from prisons or jails) to the community,3 the number of middle- and older-aged individuals re-entering the community after incarceration can also be expected to grow. Considering that persons aged 50 and older have the highest suicide rates4 and that deaths by drug overdose, specifically opioid-related deaths, increased sixfold among those aged 55–64 between 1999 and 2011,5 it may be especially important to characterize risk of suicide and drug overdose in those transitioning from prison to community in later life. When further considering that the percentage of prisoners who are veterans increases with increasing age6 and that nearly 70% of veteran suicides are in veterans aged 50 and older,7 the impact of re-entry into community for older veterans may be particularly salient.
Although suicide attempt rates among incarcerated persons are up to six times higher than those living in the community,8 data on suicide attempt following community re-entry are essentially unknown. Whereas large national surveys, such as the National Survey on Drug Use and Health, have been used to estimate suicidal ideation in those recently released from prison,9 suicide attempts cannot be confirmed. However, in 2008, the U.S. Department of Veterans Affairs (VA) mandated that health system facilities track attempted suicides at local and national levels through oversight of local suicide prevention coordinators,10 providing the rare opportunity to reliably examine suicide attempts. Thus, because suicide attempt is a robust predictor of subsequent death by suicide, improved understanding of suicide attempts in older veterans may inform postrelease suicide prevention efforts.
The transition from prison to community has been shown to be associated with higher than expected allcause mortality rates,11 with evidence pointing towards deaths from suicide and accidental drug overdose as leading causes,12 as well as other accidental injuries (such as motor vehicle and falls).13 However, to the best of our knowledge, no studies have used a national sample to quantify mortality rates, and next to nothing is known regarding the likelihood of experiencing these outcomes following prison release in later life.12–16 A partnership between Centers for Medicare and Medicaid Services (CMS) and the VA offers a unique opportunity to link large national datasets to evaluate if release from prison is a risk factor for subsequent suicide-related outcomes and unintended death among middle- and older- aged veterans. Over 3 years (2012–2014), we determined risk of suicide attempt and death by suicide, drug overdose, and other accidental injury among those released from prison (i.e., older re-entry veterans) as compared with an age-matched nonincarcerated cohort. This study provides invaluable data on suicide attempt and injurious deaths in a large national sample of veterans and offers benchmark data regarding these outcomes among re-entry adults aged 50 and older.
METHODS
Data and Participants
By linking large national datasets, we created a cohort of all Medicare-eligible veterans aged 50 and older who were incarcerated between 2012 and 2014, following them from their most recent prison release date for a mean (± standard deviation [SD]) of 1.56 (±0.94) years, until death or study completion. We also created a matched cohort of nonincarcerated Medicare-eligible veterans with a mean (SD) of 1.58 (0.94) years’ follow-up. The following four databases were linked: 1) VA's National Patient Care Database, which includes all inpatient and outpatient VA services; 2) CMS data, which include medical claims/diagnoses and identify prison admission/release dates; 3)VA's Suicide Prevention Applications Network (SPAN), which contains information on suicide attempts;10,17 and 4) VA's National Suicide Data Repository (SDR), which includes cause-specific death information.7,18 Records were extracted for veterans aged 50 and older seen at inpatient or outpatient VA healthcare facilities fiscal year 2012 (October 1, 2011) through December 31, 2014, and also enrolled in Medicare services. Using an approach established by Wang et al.,19 Medicare data were used to identify older re-entry veterans and to create a matched cohort. For veterans aged 50–64 years, the sample entry was limited to those eligible for Medicare due to disability and/or end-stage renal disease (ESRD). For those aged 65 and older, when all veterans are Medicare-eligible, the sample included nearly all veterans. The study sample included 7,671 older re-entry veterans matched with 7,671 veterans with no incarceration history. Year of correctional facility release was used to match to a never-incarcerated beneficiary in the same year, with further matching on age (±1 year), sex, race, residential ZIP code, and Medicare eligibility status (including age, disability, and ESRD). If the older re-entry veteran was incarcerated more than once during the study period, the most recent release date was used for matching. Institutional review boards of the University of California, San Francisco, and the San Francisco VA Medical Center approved this study.
Suicide attempt
Suicide attempt was derived from the VA's National SPAN data, a suicide tracking system that uses a standardized method (i.e., Centers for Disease Control and Prevention's Self-Directed Violence Classification System) to record suicide attempts based on clinician reports from local SPAN databases.10,17 A key advantage of the SPAN data is that they include actual attempt date. Thus, we were able to assess suicide attempts occurring post–re-entry date/matching date.
Death by suicide, drug overdose, and other accidental injury
Data for death by suicide and drug overdose (i.e., suicide or accidental) were obtained using the International Classification of Diseases, Tenth Revision (ICD-10), codes included in the VA's SDR.7 We also used these data to determine death by accidental injury (i.e., deaths due to transport and nontransport accidents) other than accidental drug overdose. ICD-10 codes for suicide included X60–X84 and Y87.0. Death by drug overdose was defined as ICD-10 codes X60–X64 (which includes intentional injury by suicide), codes X40–X44 (accidental drug overdose), and codes Y10–Y14 (undetermined intent). Codes for death by all accidental injuries included V01–X59 and Y85–Y86, whereas codes X40–X44 were excluded when evaluating death by accidental injury other than drug overdose. Corresponding dates of death for these ICD-10 codes were included in VA SDR data.
Chronic medical conditions and psychiatric disorders
Chronic medical conditions and psychiatric disorders were determined using standard International Classification of Diseases, Ninth Revision (ICD-9), codes included in VA and/or CMS database records (2012–2014). Medical conditions included hypertension, myocardial infarction, congestive heart failure, stroke, diabetes mellitus, arthritis, hip fracture, chronic lung disease, cancer, liver disease, human immunodeficiency virus/acquired immunodeficiency syndrome, hepatitis C, and sexually transmitted disease. The sum of these 13 conditions was calculated for each participant. Psychiatric disorders included mood disorders (i.e., depression [major depression or depression not otherwise specified], dysthymia, and bipolar disorder), anxiety disorders (i.e., post-traumatic stress disorder, generalized anxiety disorder, panic, and phobia), schizophrenia, psychosis, and substance use disorders (i.e., alcohol abuse/dependence, drug abuse/dependence, and tobacco dependence).
Other variables
Evidence of homelessness was indicated by ICD-9 code V60.0 (lack of housing) as a primary or other code during a VHA visit or by having received a non-ICD VHA clinic or specialty code related to receiving homeless services during the study period.20 Finally, history of traumatic brain injury (TBI) was derived from ICD-9 codes included in VA and/or CMS database records and determined using the Defense and Veterans Brain Injury Center and the Armed Forces Health Surveillance Branch for TBI surveillance 2012 criteria.21
Statistical Analyses
To describe the sample, we conducted bivariate analyses of the characteristics across re-entry status. Characteristics were summarized using means and standard deviations or frequencies and proportions for re-entry veterans and for the never-incarcerated cohort. Statistical significance of differences between the two cohorts was tested by t tests for continuous variables and χ2 tests for categorical variables.
We determined cumulative incidence of suicide attempt and death by all injuries, then plotted these results according to age in years for the two cohorts. Fine-Gray proportional hazards regression was used to examine time to suicide attempt and time to death by suicide, drug overdose, and accidental injury, with age as the time scale, while accounting for competing risk of other deaths. Hazard ratios were estimated for the association between re-entry status and risk of outcomes in models, adjusting for the sum of 13 major medical conditions, homelessness, TBI, and any psychiatric disorder.
Proportional hazards assumptions were evaluated graphically and statistically and were satisfied for all models. Statistical tests for models were two-tailed, with p <0.05 defining statistical significance. All analyses were performed using SAS version 9.4 software (SAS Institute Inc., Cary, NC) and Stata version 15 (StataCorp, College Station, TX).
RESULTS
Descriptive Statistics
Table 1 presents descriptive characteristics of the older re-entry and never-incarcerated veterans. Groups each had an average age of approximately 62 years, were nearly all male (98.7%), and were 62.5% non-Hispanic white. Half were Medicare-eligible based on being aged 65 or older, and 48% qualified for Medicare due to disability without ESRD. Hip fracture, chronic lung disease, liver disease, human immunodeficiency virus/acquired immunodeficiency syndrome, hepatitis C, and sexually transmitted diseases were significantly more prevalent among older re-entry veterans than those never incarcerated (Table 1). Furthermore, older re-entry veterans were significantly more likely to have any of the psychiatric disorders, with the exception of dysthymia, panic, and phobia, where there were no differences between the groups. Older re-entry veterans were also more likely to be currently homeless and to have history of TBI (Table 1).
TABLE 1.
Characteristics of the Sample of 15,342 Medicare Beneficiaries: Re-entry Group (N = 7,671) and Never-Incarcerated Comparison Group (N = 7.671)
| Characteristics n (%) or mean (SD) | Re-entry (N = 7,671) | Never Incarcerated (N = 7,671) | t value/χ2 | df, p valuea |
|---|---|---|---|---|
| Demographicb | ||||
| Age at release/match time, years, mean (SD) | 62.85(7.17) | 62.19(7.03) | −5.78 | 15,334, <0.001 |
| Female | 100(1.30) | 100(1.30) | n/a | n/a |
| Race | n/a | n/a | ||
| Non-Hispanic white | 4,794 (62.50) | 4,794 (62.50) | ||
| Non-Hispanic black | 2,584 (33.69) | 2,584 (33.69) | ||
| Hispanic/Other | 293 (3.82) | 293 (3.82) | ||
| Mean income (SD)c | 51,989.98 (12,846.54) | 51,962.96 (12,792.69) | 0.13 | 15,325, 0.896 |
| >25% college educationc | 3,480 (45.37) | 3,463 (45.14) | 0.08 | 1, 0.783 |
| Medicare status | n/a | n/a | ||
| ≥65 years without ESRD | 3,900 (50.84) | 3,900 (50.84) | ||
| ≥65 years with ESRD | 28 (0.37) | 28 (0.37) | ||
| Disabled without ESRD | 3,712(48.39) | 3,712 (48.39) | ||
| Disabled with ESRD | 31 (0.40) | 31 (0.40) | ||
| ESRD only | 0 (0.00) | 0 (0.00) | ||
| Chronic medical conditions | ||||
| Hypertension | 5,642 (73.55) | 5,986 (78.03) | 42.04 | 1, <0.001 |
| Myocardial infarction | 758 (9.88) | 688 (8.97) | 3.74 | 1, 0.053 |
| Congestive heart failure | 906(11.81) | 958 (12.49) | 1.65 | 1, 0.199 |
| Stroke | 1,111 (14.48) | 1,236 (16.11) | 7.86 | 1, 0.005 |
| Diabetes mellitus | 2,445 (31.87) | 3,163 (41.23) | 144.89 | 1, <0.001 |
| Arthritis | 181 (2.36) | 161 (2.10) | 1.20 | 1, 0.274 |
| Hip fracture | 235 (3.06) | 187 (2.44) | 5.61 | 1, 0.018 |
| Chronic lung disease | 2,886 (37.62) | 2,413 (31.46) | 64.50 | 1, <0.001 |
| Cancer | 1,192 (15.54) | 1,453 (18.94) | 31.12 | 1, <0.001 |
| Liver disease | 515 (6.71) | 313 (4.08) | 52.09 | 1, <0.001 |
| HIV/AIDS | 200 (2.61) | 132 (1.72) | 14.24 | 1, <0.001 |
| Hepatitis C | 1,601 (20.87) | 719 (9.37) | 395.05 | 1, <0.001 |
| Sexually transmitted disease | 630 (8.21) | 238 (3.10) | 187.65 | 1, <0.001 |
| Sum of above 13, mean (SD) | 2.39 (1.62) | 2.30 (1.49) | −3.40 | 15,340, <0.001 |
| Psychiatric disorders | ||||
| Any Mood | 4,264 (55.59) | 3,467 (45.20) | 165.62 | 1, <0.001 |
| Depressiond | 3,724 (48.55) | 3,122 (40.70) | 95.59 | 1, <0.001 |
| Dysthymia | 521 (6.79) | 510 (6.65) | 0.13 | 1, 0.723 |
| Bipolar disorder | 1,344 (17.52) | 608 (7.93) | 317.96 | 1, <0.001 |
| Any Anxiety | 2,488 (32.43) | 2,011 (26.22) | 71.56 | 1, <0.001 |
| Post-traumatic stress disorder | 2,114 (27.56) | 1,690 (22.03) | 62.84 | 1, <0.001 |
| GAD | 460 (6.00) | 368 (4.80) | 10.81 | 1, 0.001 |
| Panic | 182 (2.37) | 169 (2.20) | 0.49 | 1, 0.483 |
| Phobia | 98(1.28) | 112 (1.46) | 0.95 | 1,0.331 |
| Schizophreniae | 1,213 (15.81) | 583 (7.60) | 250.29 | 1, <0.001 |
| Primary Psychotic Illnessesf | 1,618 (21.09) | 785 (10.23) | 342.39 | 1, <0.001 |
| Any SUDs | 5,529 (72.08) | 3,510 (45.76) | 1,097.71 | 1, <0.001 |
| Alcohol | 3,463 (45.14) | 1,372 (17.89) | 1,320.43 | 1, <0.001 |
| Drug | 3,218 (41.95) | 1,101 (14.35) | 1,444.24 | 1, <0.001 |
| Tobacco dependence | 4,188 (54.60) | 2,799 (36.49) | 507.05 | 1, <0.001 |
| Any psychiatric illness | 6,459 (84.20) | 5,322 (69.38) | 472.77 | 1, <0.001 |
| Homelessness | 550 (7.17) | 126 (1.64) | 278.20 | 1, <0.001 |
| Traumatic brain injury | 920 (11.99) | 477 (6.22) | 154.55 | 1, <0.001 |
Notes: ESRD: end-stage renal disease; GAD: generalized anxiety disorder; SUD: substance use disorder.
p value based on unpaired t test for continuous variables and χ2 test for categorical variables, comparing across re-entry status.
Variables matched on year of release from a correctional facility, age (±1 year), sex, race (non-Hispanic white, non-Hispanic black, Hispanic/Other), residential ZIP code, and Medicare eligibility status.
ZIP code tabulation area from 2013 census.
Depression includes major depression or depression NOS.
Schizophrenia includes schizophrenia or schizoaffective disorder (all-inclusive ICD-9 codes: 295.0–295.4 and 295.6–295.9).
Primary psychotic illnesses include ICD-9 codes 297.1 (delusional), 298.8 and 298.9 (brief psychotic and other psychotic), 295.9 (unspecified schizophrenia), 295.7 (schizoaffective), 295.4 (schizophreniform), 293.81 and 293.82 (psychosis due to medical condition).
Among the older re-entry veterans, approximately half were incarcerated at some point before their most recent incarceration. About 20% had two or more incarcerations over the 3-year study period (range: 1—5 incarcerations). Average (±SD) years in prison for the index incarceration was 1.3 (±2.3) years (Table 2).
TABLE 2.
Re-entry Characteristics in Older Re-entry Veterans (N = 7,671) Starting 2012 and Followed Until 2014
| Re-entry Characteristics | Re-entry (N = 7,671) |
|---|---|
| Study Yeara Baseline 2012, n (%) |
2,979 (38.8) |
| Follow-up 2013, n (%) | 2,370 (30.9) |
| Follow-up 2014, n (%) | 2,322 (30.3) |
| Years in prison, mean (SD) [range] | 1.3 (2.3) [1 day–36.8 years] |
| Number of Incarcerations 2012–2014 One, n (%) | 6,193 (80.7) |
| Two, n (%) | 1,082 (14.1) |
| Three, n (%) | 293 (3.8) |
| Four, n (%) | 79 (1.0) |
| ≥five, n (%) | 24 (0.3) |
| Prior History of Any Incarceration (Including 2012–2014) | |
| One, n (%) | 3,956 (51.6) |
| Two, n (%) | 1,759 (22.9) |
| Three, n (%) | 884 (11.5) |
| Four, n (%) | 535 (7.0) |
| ≥five, n (%) | 537 (7.0) |
Based on most recent (i.e., index) incarceration.
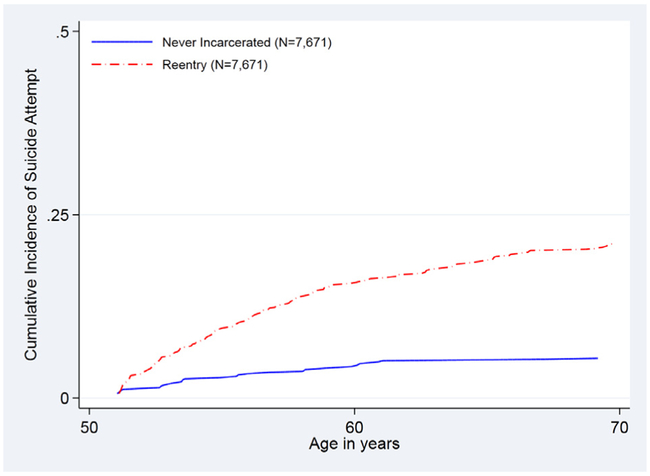
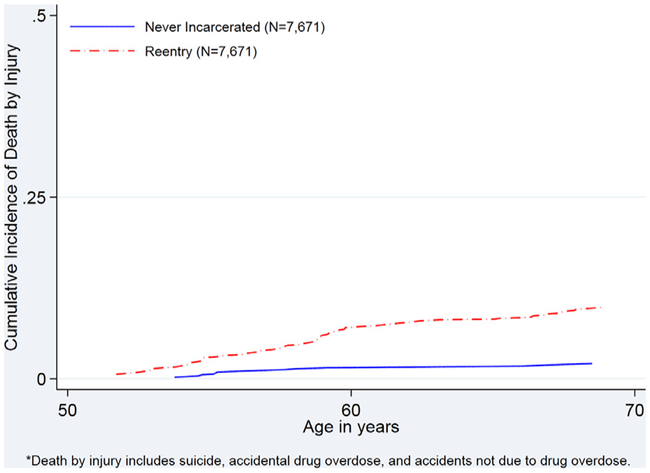
Cumulative Incidence
Cumulative incidence of suicide attempt (2012–2014) was consistently higher for older re-entry veterans than for those never incarcerated (Fig. 1). Similar results were found for death by all injuries, including suicide and accidental injury (Fig. 2).
FIGURE 1.
Cumulative incidence of suicide attempt in older re-entry veterans and a matched comparison group of veterans who were never incarcerated.
FIGURE 2.
Cumulative incidence of death by injury in older re-entry veterans and a matched comparison group of veterans who were never incarcerated.
Mortality Outcomes and Suicide Attempt
Annual incidence rates of all outcomes were higher among older re-entry veterans as compared with those who were never incarcerated (Table 3). Rate of suicide attempt was considerably higher among older re-entry veterans (599.7 versus 134.7 per 100,000 per year; adjusted hazard ratio [HR] 3.45; 95% confidence interval [CI] 2.24–5.32; p <0.001, Wald χ2 statistic = 31.58, df = 1). Regarding death, although a total of seven older re-entry veterans died by suicide as compared with four never-incarcerated veterans, there was no observed statistically significant difference in suicide mortality rates between the two groups (30.4 versus 17.4, respectively; adjusted HR 2.40; 95% CI 0.51–11.24; p = 0.266, Wald χ2 = 1.23, df = 1). However, as compared with veterans who were never incarcerated, older re-entry veterans had significantly higher rates of death by drug overdose (121.7 versus 43.5; adjusted HR 3.45; 95% CI 1.37–8.73; p = 0.009, Wald χ2 statistic = 6.86, df = 1) and other accidental injury (126.0 versus 39.1; adjusted HR 3.13; 95% CI 1.28–7.69; p = 0.013, Wald χ2 statistic = 6.25, df = 1). Whereas two of the older re-entry veteran suicide deaths were attributed to drug overdose, there were no suicides by drug overdose among the never incarcerated.
TABLE 3.
Suicide-Related Outcomes and Accidental Death in Older Veterans: Re-entry Versus Never-Incarcerated Comparison Group
| Outcomes | Re-entry (n = 7,671) |
Never Incarcerated (n = 7,671) |
Unadjusted Hazard Ratio (95% CI) Re-entry Versus Never Incarcerated (ref) |
Wald χ2 | df, p value |
Adjusted Hazard Ratioa (95% CI) Re-entry versus Never Incarcerated (ref) |
Wald χ2 | df, p value |
||
|---|---|---|---|---|---|---|---|---|---|---|
| N (%)over 3 years |
Rate/100,000 /year |
N(%)over 3 years |
Rate/100,000 /year |
|||||||
| Suicide | ||||||||||
| Attemptb | 138 (1.80) | 599.7 | 31 (0.41) | 134.7 | 4.59 (3.01–7.01) | 49.94 | 1, <.001 | 3.45 (2.24–5.32) | 31.58 | 1, <0.001 |
| Deathc | 7 (0.09) | 30.4 | 4 (0.05) | 17.4 | 2.33 (0.56–9.60) | 1.37 | 1, 0.242 | 2.40(0.51–11.24) | 1.23 | 1, 0.266 |
| Drug Overdosed | ||||||||||
| Death | 28 (0.37) | 121.7 | 10(0.13) | 43.5 | 3.93(1.72–8.99) | 10.51 | 1, 0.001 | 3.45 (1.37–8.73) | 6.86 | 1, 0.009 |
| Suicide | 2(0.03) | 8.7 | 0(0.00) | 0 | – | – | – | – | – | – |
| Accidental | 26(0.34) | 113.0 | 10(0.13) | 43.5 | 3.61(1.57–8.32) | 9.12 | 1, 0.003 | 3.13(1.22–8.05) | 5.62 | 1, 0.018 |
| Accidental Death (no drug overdose)e | 29(0.38) | 126.0 | 9(0.12) | 39.1 | 3.84(1.67–8.83) | 10.02 | 1, 0.002 | 3.13(1.28–7.69) | 6.25 | 1, 0.013 |
Adjusted for homelessness,sum of 13 medical conditions, TBI, and any psychiatric disorder.
SPAN, post-release/match time.
ICD-10=X60–X84,Y87.0.
ICD-10=suicide(X60–64),accident(X40–44),undetermined(Y10–14).
ICD-10=V01–X39, X45–X59, Y85–Y86.
We further determined prison release as a risk factor for near-term suicide attempt. Within the first 30 days following prison release, there were 24 attempts in the re-entry group as compared with 7 attempts in those never incarcerated, translating to a hazard ratio of 3.86 (95% CI 1.06–13.98; p = 0.040, Wald χ2 statistic = 4.22, df = 1). By 6 months, there were 59 and 11 attempts in the re-entry and comparison groups, respectively (HR 6.08; 95% CI 2.69–13.75; p <0.001, Wald χ2 statistic = 18.82, df = 1), and at 1 year there were 93 and 19 attempts in the re-entry and comparison groups, respectively (HR 5.08; 95% CI 2.89–8.93; p <0.001, Wald χ2 statistic =31.74, df = 1).
CONCLUSION
This study evaluated release from prison as a risk factor for suicide-related outcomes and unintended death in a national cohort of middle- and older-aged veterans. Our findings indicate that veterans released from prison in later life have a significantly increased risk of attempting suicide, as well as an increased risk of death by drug overdose and other accidental injury, as compared with matched comparisons. These findings are not accounted for by between-group differences in the occurrence of homelessness, TBI, and medical or psychiatric conditions.
Until now, risk of suicide attempt following prison release in later life has been largely unknown. Strikingly, we found that those released from prison in later life had nearly five times greater risk of a subsequent suicide attempt than those never incarcerated. This finding is not only statistically significant but also clinically meaningful, as the difference in the incidence of suicide attempts between the two groups translates to an additional 465 suicide attempts per 100,000 person-years among the older re-entry veterans. Thus, these results emphasize the need for suicide prevention efforts throughout the process of transitioning from prison to the community and beyond in later life—from prison discharge planning to the early re-entry period, and even after 1 year or more following re-entry. Prior studies of mixed-age samples have shown that the few weeks immediately following prison release are a high-risk time for death by suicide.13,22,23 Our findings add to that literature by demonstrating that suicide attempts also occur at a much higher rate soon after release. To our knowledge, we are the first to do such work. Findings from the present study also complement the growing body of research emphasizing the potential importance of care transitions to suicide risk and prevention efforts. For example, prior work has shown increased risk of suicide among subgroups of persons hospitalized in the past year, such as those hospitalized for psychiatric reasons or for self- or assault-related injuries.24–26 Future research is needed to determine the mechanisms by which transitions from “boundaried” settings (e.g., hospitals, prisons) to the community increase suicide risk. While our study has some similarities to prior research evaluating death by suicide, drug overdose, and accidental injury in those released from prison, there are important differences, the latter including studies conducted mainly on mixed-age samples outside the United States22,27,28 or those that used data from one state12–14 or city15,16 in the United States. Our study is the first to use national-level data and quantify these outcomes in the rapidly growing population of veterans released from prison in later life.
Our results regarding suicide attempt are also compelling considering the strengths of the SPAN data, particularly inclusion of suicide attempt date(s) as recorded by clinicians. Having accuracy in the timing of suicide attempts was vital, as it allowed us to determine actual date of an attempt after the prison release date. Other methods of capturing suicide attempt, such as using ICD-9 codes, are less precise. Because ICD-9 codes refer to visit dates and not event dates, it is unknown when actual attempts occurred, how long attempts have been in individuals’ medical records, and how many attempts occurred over time. Moreover, because veterans comprised the entire sample, both the re-entry group and the never-incarcerated comparison group had the opportunity for clinical assessment of suicidal behavior to be documented in SPAN, thereby substantially reducing the likelihood of differential case ascertainment between groups.
Over the past 2 decades in the United States, suicide rates among persons aged 65 and older have been consistently high. More recently, however, middle-aged persons have experienced the highest increase in suicide rates of any age group,29 and rates of drug-related deaths have also risen substantially in middle- and older-aged individuals.30 The largest increase in the rate of opioid-related deaths between 1999 and 2015 occurred among those aged 55–64 years,5,31 and between 2014 and 2015, the percent change in the rate of heroin-related deaths was highest among those aged 55 and older.31 These increases are attributed, at least in part, to the increase in opioid prescriptions for pain that began in the late 1990s and to stresses associated with economic insecurity.32However, further research is needed to evaluate where prison entry and subsequent release fall on the pathway from drug use and/or economic pressures to suicide or death by drug overdose in this age group.
Our findings also indicate that later-life prison release is a risk factor for death by accidental drug overdose and death due to accidental injury (other than drug overdose). The risk of experiencing each of these outcomes was three times greater in middle- and older-aged veterans recently released from prison when compared with never-incarcerated veterans. Together, differences in the incidences of these outcomes between the two groups translate to an additional 157 deaths per 100,000 person-years among the older re-entry veterans. A possible explanation for this risk difference may be deficits in prefrontal cortex functioning among the re-entry group that cannot be explained by between-group differences in the presence of TBI. For example, problems with executive functioning activities crucial for self-regulation, including impulsivity, inhibition, planning, and problem-solving, have been previously noted in incarcerated populations33,34 and found to be associated with suicidal behavior in the context of late-life depression.35,36 In addition, there is mounting concern regarding misclassification of suicides as accidental deaths resulting from drug-related poisoning or overdose.37,38 Thus, it is possible, and probably likely, that the rates of death by suicide reported in the present study may be artificially low for both re-entry veterans and those never incarcerated.
Our study has limitations. Data regarding suicide attempts and other suicide-related behaviors during incarceration were not available. Reason for incarceration was also not available. In addition, we did not have information regarding psychosocial factors, such as social support, that may impact risk of suicidal behavior following prison release, as prior research suggests that older prisoners are often estranged from family and friends.39,40 Similarly, we had limited information on marital status and were unable to determine employment status. Furthermore, although we assessed suicide attempts using SPAN data, which provided high specificity, it is possible that some veterans with only ICD-9 coded attempts were misclassified into the no-attempt group. However, this would have led to conservative estimates, biasing study findings towards the null. Finally, generalizability may be limited for women and nonveterans. Still, those in our sample who are eligible for Medicare fee-for-service based on age are likely representative of veterans aged 65 and older. In addition, representation of the larger population of Medicare beneficiaries aged 50–64 who have been released from prison is fairly good because individuals released from prison are more likely to be Medicare-eligible owing to disability than persons in the general population.19
The present research provides new evidence supporting prison release in later life as a risk factor for suicidal behavior and death by drug overdose and accidental injuries in veterans. Documenting the increased risk of these outcomes for older veterans released from prison has important implications for the VA and care transition models in general. Targeting suicide prevention efforts towards the transition from prison to community in later life may help to reduce the number of older veterans dying by suicide and related adverse outcomes. Furthermore, thinking of this transition as a longer term process may help to ensure that prevention efforts remain in place. These findings also encourage future research evaluating healthcare patterns that precede and follow nonfatal suicide attempts to determine environments, services, and supports that may help to decrease risk. Finally, future studies that evaluate older prisoners’ concerns about adapting to life “on the outside” upon release may help to inform age-specific prison-to-community transition care planning.
Highlights.
Question: Is transition from prison to community in later life a risk factor for suicidal behavior and death by drug overdose or other accidental injury?
Findings: In this retrospective cohort study that used linked, national-level datasets, the reentry sample, compared with a never-incarcerated matched comparison group, had higher suicide attempt rates (599.7 vs. 134.7 per 100,000/year) and death by drug overdose (121.7 vs. 43.5) and other accidental injury (126.0 vs. 39.1).
Meaning: Given their high rates of suicide attempts and injurious deaths, those transitioning from prison to community in later life may benefit from targeted suicide prevention efforts.
Acknowledgments
This work was supported by I01 CX001119 from the Clinical Science Research & Development Service of the Office of Research and Development, U.S. Department of Veterans Affairs (principal investigator: Amy L. Byers, Ph.D., M.P.H.), and by R01 MH106529 from NIMH (principal investigator: Lisa C. Barry, Ph.D., M.P.H.). Support for SDR and SPAN is provided by the Center of Excellence for Suicide Prevention, U.S. Department of Veterans Affairs. Support for VA/CMS data is provided by the U.S. Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development, VA Information Resource Center (SDR 02-237 and 98-004).
Footnotes
The sponsors had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or the preparation, review, or approval of the manuscript. Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the author(s) and do not necessarily reflect the views of the U.S. Government or the U.S. Department of Veterans Affairs, and no official endorsement should be inferred. There are no financial disclosures to report.
References
- 1.Carson EA, Golinelli D: Prisoners in 2012. Trends in Admissions and Releases, 1991–2012. NCJ 243920. Washington, DC: U.S. Department of Justice, Bureau of Justice Statistics, 2014 [Google Scholar]
- 2.Luallen J, Cutler C: The growth of older inmate populations: how population aging explains rising age at admission. J Gerontol B Psychol Sci Soc Sci 2015;72(5):888–900 [DOI] [PubMed] [Google Scholar]
- 3.U.S. Bureau of Justice Statistics:. Reentry Trends in the U.S: Inmates Returning to the Community After Serving Time in Prison. (online) Available at:Accessed October 17 https://www.bjs.gov/content/reentry/reentry.cfm; 2017. Accessed October 17
- 4.National Violent Death Reporting System:. Suicide Rates, All Mechanisms, All Races, Both Sexes, All Ages (2014). (online) Available at: https://wisqars.cdc.gov:8443/nvdrs/nvdrsDisplay.jsp. Accessed October 17, 2017
- 5.Chen LH, Hedegaard H, Warner M: Drug-poisoning deaths involving opioid analgesics: United States, 1999–2011. NCHS Data Brief 2014; 166:1–8 [PubMed] [Google Scholar]
- 6.Bronson J, Carson EA, Noonan M, et al. : Veterans in Prison and Jail, 2011 – 12. NCJ 249144. Washington, DC: U.S. Department of Justice, Bureau of Justice Statistics, 2015 [Google Scholar]
- 7.Kemp J, Bossarte RM: Suicide Data Report, 2012. Washington, DC: Department of Veterans Affairs Mental Health Services Suicide Prevention Program, 2012 [Google Scholar]
- 8.Jenkins R, Bhugra D, Meltzer H, et al. : Psychiatric and social aspects of suicidal behaviour in prisons. Psychol Med 2005;35(2):257–269 [DOI] [PubMed] [Google Scholar]
- 9.Yu SS, Sung HE, Mellow J, et al. : Prevalence and correlates of suicidal ideation among parolees. Psychiatr Serv 2014;65(3):381–386 [DOI] [PubMed] [Google Scholar]
- 10.Kemp J, Bossarte RM: Surveillance of suicide and suicide attempts among veterans: addressing a national imperative. Am J Public Health 2012;102(suppl 1):e4–e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zlodre J, Fazel S: All-cause and external mortality in released prisoners: systematic review and meta-analysis. Am J Public Health 2012;102(12):e67–e75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Binswanger IA, Blatchford PJ, Mueller SR, et al. : Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med 2013;159(9):592–600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Binswanger IA, Stern MF, Deyo RA, et al. : Release from prison—a high risk of death for former inmates. N Engl J Med 2007;356 (2):157–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosen DL, Schoenbach VJ, Wohl DA: All-cause and cause-specific mortality among men released from state prison, 1980–2005. AmJ Public Health 2008;98(12):2278–2284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lim S, Seligson AL, Parvez FM, et al. : Risks of drug-related death, suicide, and homicide during the immediate post-release period among people released from New York City jails, 2001–2005. Am J Epidemiol 2012;175(6):519–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alex B, Weiss DB, Kaba F, et al. : Death after jail release: matching to improve care delivery. J Correct Health Care 2017;23 (1):83–87 [DOI] [PubMed] [Google Scholar]
- 17.Hoffmire C, Stephens B, Morley S, et al. : VA Suicide Prevention Applications Network: a national health care system-based suicide event tracking system. Public Health Rep 2016;131(6):816–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Center of Excellence for Suicide Prevention:. Joint Department of Veterans Affairs (VA) and Department of Defense (DoD) Suicide Data Repository—National Death Index (NDI). (online) Available at: https://www.mirecc.va.gov/suicideprevention/ Accessed February 16, 2018
- 19.Wang EA, Wang Y, Krumholz HM: A high risk of hospitalization following release from correctional facilities in Medicare beneficiaries: a retrospective matched cohort study, 2002 to 2010. JAMA Intern Med 2013;173(17):1621–1628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peterson R, Gundlapalli AV, Metraux S, et al. : Identifying homelessness among veterans using VA administrative data: opportunities to expand detection criteria. PLoS One 2015; 10(7):e0132664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Armed Forces Health Surveillance Branch:. Surveillance Case Definitions, 2016. (online) Available at:Accessed January 5 http://www.health.mil/Military-Health-Topics/Health-Readiness/Armed-Forces-Health-Surveillance-Branch/Epidemiology-and-Analysis/Surveillance-Case-Definitions; 2018. Accessed January 5
- 22.Haglund A, Tidemalm D, Jokinen J, et al. : Suicide after release from prison: a population-based cohort study from Sweden. J Clin Psychiatry 2014;75(10):1047–1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kariminia A, Law MG, Butler TG, et al. : Suicide risk among recently released prisoners in New South Wales, Australia. Med J Aust 2007;187(7):387–390 [DOI] [PubMed] [Google Scholar]
- 24.Conner KR, Langley J, Tomaszewski KJ, et al. : Injury hospitalization and risks for subsequent self-injury and suicide: a national study from New Zealand. Am J Public Health 2003;93(7): 1128–1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersen UA, Andersen M, Rosholm JU, et al. : Contacts to the health care system prior to suicide: a comprehensive analysis using registers for general and psychiatric hospital admissions, contacts to general practitioners and practising specialists and drug prescriptions. Acta Psychiatr Scand 2000;102(2): 126–134 [DOI] [PubMed] [Google Scholar]
- 26.Chock MM, Bommersbach TJ, Geske JL, et al. : Patterns of health care usage in the year before suicide: a population-based case-control study. Mayo Clin Proc 2015;90(11):1475–1481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pratt D, Piper M, Appleby L, et al. : Suicide in recently released prisoners: a population-based cohort study. Lancet 2006;368 (9530):119–123 [DOI] [PubMed] [Google Scholar]
- 28.Spittal MJ, Forsyth S, Pirkis J, et al. : Suicide in adults released from prison in Queensland, Australia: a cohort study. J Epidemiol Community Health 2014;68(10):993–998 [DOI] [PubMed] [Google Scholar]
- 29.Curtin SC, Warner M, Hedegaard H: Increase in suicide in the UnitedStates, 1999–2014.NCHS Data Brief 2016; 241:1–8 [PubMed] [Google Scholar]
- 30.Hedegaard H, Warner M, Minino AM: Drug overdose deaths in the United States, 1999–2016. NCHS Data Brief 2017; 294:1–8 [PubMed] [Google Scholar]
- 31.Rudd RA, Seth P, David F, et al. : Increases in drug and opioid-involved overdose deaths - United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016;65(5051):1445–1452 [DOI] [PubMed] [Google Scholar]
- 32.Case A, Deaton A: Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A 2015;112(49):15078–15083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meijers J, Harte JM, Jonker FA, et al. : Prison brain? Executive dysfunction in prisoners. Front Psychol 2015; 6:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vadini F, Calella G, Pieri A, et al. : Neurocognitive impairment and suicide risk among prison inmates. J Affect Disord 2018; 225:273–277 [DOI] [PubMed] [Google Scholar]
- 35.Dombrovski AY, Szanto K, Clark L, et al. : Reward signals, attempted suicide, and impulsivity in late-life depression. JAMA Psychiatry 2013;70(10):1020–1030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gujral S, Dombrovski AY, Butters M, et al. : Impaired executive function in contemplated and attempted suicide in late life. Am J Geriatr Psychiatry 2014;22(8):811–819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rockett IR, Kapusta ND, Coben JH: Beyond suicide: action needed to improve self-injury mortality accounting. JAMA Psychiatry 2014;71(3):231–232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stone DM, Holland KM, Bartholow B, et al. : Deciphering suicide and other manners of death associated with drug intoxication: a Centers for Disease Control and Prevention consultation meeting summary. Am J Public Health 2017;107(8):1233–1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williams BA, McGuire J, Lindsay RG, et al. : Coming home: health status and homelessness risk of older pre-release prisoners. J Gen Intern Med 2010;25(10):1038–1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hayes AJ, Burns A, Turnbull P, et al. : Social and custodial needs of older adults in prison. Age Ageing 2013;42(5):589–593 [DOI] [PubMed] [Google Scholar]