Abstract
It is unclear whether impaired cognition is a risk factor for depression, a consequence of depression, or whether both depression and impaired cognition are caused by a third underlying process (e.g., stress). These three hypotheses were tested in 523 adolescents assessed annually for depression, attentional functioning, and childhood/recent life stress. Baseline switching, sustained, and selective attention did not predict first onset of depression (foD) or depressive symptoms. Divided attention predicted depressive symptoms only. Piecewise growth modelling indicated that the trajectory of switching attention declined prior to foD; there was evidence of significant recovery in switching attention following foD. Structural equation modelling indicated that impaired switching attention prospectively predicted higher depressive symptoms and that higher depressive symptoms predicted worse selective and switching attention. Further, childhood stress prospectively predicted higher depressive symptoms via switching attention and worse switching attention via depressive symptoms.
Introduction
Depression is a chronic, debilitating, and highly prevalent psychological disorder that frequently emerges in adolescence (Burcusa & Iacono, 2007; Hankin et al., 1998; Kessler et al., 2012; Whiteford et al., 2013). Depression is characterized by somatic (e.g. fatigue), behavioral (e.g. social withdrawal), emotional (e.g. sadness) and cognitive (e.g. excessive guilt, poor concentration) symptoms (American Psychiatric Association, 2013). Researchers have identified both cognitive biases and cognitive deficits in depression (Abramson, Metalsky, & Alloy, 1989; Burt, Zembar, & Niederehe, 1995). There is substantial evidence that individuals, both diagnosed with and at risk of developing depression, are more likely to exhibit negatively biased cognition, including negative views of themselves, those around them, and of the future as well as a negative bias in the way they recall and attend to their environment (Abramson et al., 1989; Beck, 1976; Gotlib & Joormann, 2010). Deficits in cognitive functioning (e.g., executive functioning, attention) were, until relatively recently, considered to be epiphenomena emerging from cardinal symptoms of depression, such as decreased motivation (Austin, Mitchell, & Goodwin, 2001; Gotlib & Joormann, 2010). There is increasing evidence, however, that cognitive deficits are core features of depression.
Cognitive Functioning in Adults with Depression
Recent well-powered meta-analyses find that individuals with major depressive disorder (MDD) are more likely to perform worse on a range of cognitive functions than healthy controls (Rock, Roiser, Riedel, & Blackwell, 2013; Snyder, 2013; Wagner, Doering, Helmreich, Lieb, & Tadić, 2012). Wagner et al. (2012) reported moderate to large deficits in semantic fluency, phonemic fluency, inhibition and shifting in non-psychotic MDD patients with current depression. Similarly, both Snyder (2013) and Rock et al. (2013) reported impaired performance across multiple domains of executive functioning in MDD, including updating working memory, planning, cognitive shifting and flexibility, inhibition and verbal fluency tasks; moreover, results in both studies held despite relying on substantially non-overlapping instruments for assessing cognitive function. Further, deficits also have been shown to exist during first onset of a depressive episode, indicating that deficits are not solely a product of recurrent depressive episodes (Lee, Hermens, Porter, & Redoblado-Hodge, 2012). Consequently, there is convincing evidence that depression is associated with generalized cognitive impairment and it is hypothesized that impaired cognition may be a consequence of depression.
The Complex Relationship between Cognition and Depression
Not only is cognition impaired during a depressive episode, but studies show that impairment persists beyond the duration of a depressive episode. Rock et al. (2013) reported that deficits in attention, memory and executive function persist in remission, results that are in accordance with a previous systematic review and meta-analysis (Bora, Harrison, Yücel, & Pantelis, 2013; Hasselbalch, Knorr, & Kessing, 2011). Further, there is also evidence from multiple studies using well-powered longitudinal designs that poorer premorbid cognitive functioning predicts first onset of depression (Franz et al., 2011; Koenen et al., 2009; Zammit et al., 2004). These studies suggest that the relationship between depression and cognition may be bi-directional; however, confidence in the conclusions being drawn from these studies is tempered by multiple confounding and moderator factors, such as age, severity of depressive symptoms, recurrence of depression and medication status. Indeed, higher depressive symptoms, repeated recurrence, older age and medication use all are associated with more significant cognitive dysfunction (Snyder, 2013). In sum, conceptualizing the relationship between cognitive deficits and depression is complicated by an ambiguous temporal relationship and the existence of multiple confounding and moderating factors.
Cognitive Functioning in Children and Adolescents with Depression
Hypothesis testing in younger samples can offer valuable insight into the relationship of depression and cognition by limiting the effect of two known confounds/moderators, namely older age and recurrent depression. There is strong, although more mixed, evidence of cognitive deficits in children and adolescents with depression. Case control studies report that higher depressive symptoms are associated with worse performance on measures of psychomotor speed, attention, memory and executive function in both children and adolescents (Baune, Czira, Smith, Mitchell, & Sinnamon, 2012; Günther, Holtkamp, Jolles, Herpertz-Dahlmann, & Konrad, 2004; Günther, Konrad, De Brito, Herpertz‐Dahlmann, & Vloet, 2011; Han et al., 2012; Wilkinson & Goodyer, 2006). These findings are supported by a recent meta-analysis in which Wagner, Müller, Helmreich, Huss, and Tadić (2015) reported generalized deficits across multiple cognitive functions in depressed youth. However, a separate meta-analysis on cognitive deficits in children and adolescents reported null results (Vilgis, Silk, & Vance, 2015). This inconsistency may be explained by stricter inclusion criteria used by Wagner et al. (2015) that only included samples with a current acute major depression diagnosis compared to the more liberal inclusion criteria of Vilgis et al. (2015) that allow greater variability in diagnoses and severity of depression at the time of neuropsychological evaluation. Only two studies have examined the temporal relationship between cognition and depression in children and adolescents. Connolly et al. (2014) found that measures of selective, sustained, and executive attention did not predict subsequent depression in adolescents, whereas Kertz, Belden, Tillman, and Luby (2016) reported that deficits in cognitive control did predict depressive symptoms in children. It is unclear why results, to date, have been more mixed in youth than in adults; however, inconsistencies may be attributable to differences in sample selection, developmental period, medication status, severity of symptoms, earlier age of onset, or greater developmental variability in the development of cognitive functioning in children and adolescents (Snyder, Miyake, & Hankin, 2015; Vilgis et al., 2015). Given the inconsistent results observed in youth samples, further research is needed to more accurately conceptualize the relationship between cognition and depression in youth.
Cognitive Functioning and Depression: Conceptual Issues
Snyder et al. (2015) proposed that the relationship between cognitive functioning and depression may be conceptualized in three ways. First, it is possible that cognitive deficits, while present during depression, actually precede and act as a risk factor for depression. Second, poor cognitive functioning may be a consequence of depression, worsening at and following the first incidence of depression. Finally, impaired cognition and depression may be related via a third underlying process (e.g., stress, inflammation). In particular, there is substantial and convergent evidence that stress could be a putative underlying process linking cognitive dysfunction with depression [see Lupien, McEwen, Gunnar, and Heim (2009) for a review]. Consequently, further research is needed that is capable of simultaneously testing these alternative accounts of the relationship between cognitive functioning and depression with a longitudinal design in a diverse, community sample of individuals who have never experienced depression, and consequently, are not exposed to many of the confounds present in case control studies.
The Present Study
Thus, the current study tested three hypotheses in a longitudinal study of a diverse adolescent community sample. The first hypothesis was that baseline levels of switching, sustained, divided, and selective attention are risk factors that prospectively predict future depressive symptoms and/or first onset of a depression diagnosis. The second hypothesis tested whether deficits in attentional functioning are only observable following a depressive episode by examining whether (i) prior to first onset of depression, the trajectory of attentional functioning differs for those who experience depression compared to non-depressed peers and (ii) the trajectories of attentional functioning following first diagnosis of depression differ significantly from non-depressed peers. The third hypothesis was that negative life events (both childhood and recent) (i) predict both negative changes in attentional functioning and increases in depressive symptoms, and (ii) represent indirect effects of attention on depression and/or depression on attention.
Methods
Participants
The Adolescent Cognition and Emotion Study (ACE) is a prospective, longitudinal study of adolescent-onset depression that tracked 642 adolescents and their caregivers (93% of whom were their biological mothers) every six months. At twelve month intervals, including baseline, a comprehensive assessment takes place, including semi-structured interviews to assess diagnostic status and life events, behavioral assessment of attentional functioning and multiple self-report measures. In between these comprehensive assessments, shorter assessments occur every six months during which recent life stress is assessed using self-report measures and interview. Participants were recruited from Philadelphia’s public and private middle schools (68% of the sample) as well as advertisement in Philadelphia-area newspapers (32% of the sample). Recruitment began in May 2009 and data collection is ongoing. English-speaking adolescents who identified as Caucasian/White, African American/Black, or Biracial, ages 12–13, were eligible to participate if their mother also was willing to participate. Participants were excluded if either the adolescent or mother had insufficient English reading/speaking skills to complete the assessments, or had a severe psychiatric, developmental, medical, or learning disorder. Detailed information on recruitment and sample characteristics have been published elsewhere (Alloy et al., 2012). The sample is 52.6% African-American, 53% female and 50% report being in receipt of free school lunch or possessing a family income of less than $15,000, indicative of low socio-economic status (SES).
The analytic sample was comprised of 523 adolescent participants. Individuals who met criteria for a DSM-IV-TR or Research Domain Criteria major depressive episode or dysthymia diagnosis at/before baseline (n = 72) were excluded because depression may cause impairment in cognitive functioning that may persist when depression is in remission. Additional participants who met study exclusion criteria after a baseline assessment (n = 9) or who had missing/invalid data on demographic variables, depressive symptoms, and/or cognitive assessment (n = 38) were also excluded. The analytic sample was aged 13.02 (SD = .86) at baseline, was 54% female, 53.7% African-American, and 50% were classified as low SES. Within the analytic sample, the typical participant was in the study for 3.11 years (SD = 2.56), during which time 176 participants were present for one comprehensive assessment only, 77 attended two comprehensive assessments, 76 attended three assessments, 92 attended four assessments, and 102 attended five or more assessments.
Measures
Dependent Variables
Depression diagnosis and symptoms are the dependent variables for hypothesis one, attentional functioning is the dependent variable for hypothesis two, while depressive symptoms and attentional functioning are the key dependent variables for hypothesis three. Details on each of these outcome variables are provided below.
Attention
Four sub-tests of the Test of Everyday Attention for Children (TEACh) and the Test of Everyday Attention (TEA) were administered assessing switching, sustained, divided and selective attention (Manly et al., 2001; Robertson, Ward, Ridgeway, & Nimmo-Smith, 1994). Both measures are age- and gender-normed behavioral assessments of three specific domains of attentional functioning: selective attention, sustained attention, and attentional switching. Scaled scores, where a score of 10 is indicative of performance in the 50th percentile (SD = 3), are reported for each domain of attention; higher scores are indicative of superior performance. The TEA was designed and normed to assess adults, while the TEAch was adapted from the TEA to assess attention in youth aged 6 – 16.
For both measures, ‘Sky search’ was administered to assess Selective Attention. The ‘Sky Search’ sub-test is a non-linguistic measure of selective attention, in which participants were asked to identify cases in which identical stimuli are paired together on a page. Different stimuli were used for the TEA and TEAch to improve the ecological validity for their respective samples. Additionally, in the TEAch, an observed difference in motor speed is controlled for by using a motor control version of the task. Both speed and accuracy are encouraged and the outcome is based both on the participant’s ability to correctly identify targets and the speed with which they complete the task, controlling for psychomotor speed in the case of adolescents. For the TEAch, sustained attention is assessed using the ‘Score!’ subtest. ‘Score!’ is a 10-item counting measure in which between 9 and 15 tones (345 ms) are presented, interspersed by silent intervals of variable duration (500–5000 ms) and participants were asked to count the number of tones. The TEA utilizes a comparable seven-item task. Sustained attention performance is assessed by the number of tones correctly identified. Since scaled scores are not provided for the TEA, raw scores were z-standardized for both the TEA and TEAch. ‘Sky Search DT’ is a measure of divided attention in both the TEA and TEAch that measures decrements under dual task conditions, combining both the ‘Sky Search’ and the ‘Score!’ sub-tests. A practice item is given before a test round. Performance is based upon the number of auditory tones correctly identified, the number of targets correctly identified, as well as the speed to complete the task. The final score is adjusted in both the TEAch and TEA to control for performance on ‘Sky Search’, before an age- and gender- normed score is calculated. Attentional switching is assessed in the TEAch using the ‘Creature Counting’ sub-test and in the TEA using the ‘Elevator Counting’ sub-test. Both tests measure the temporary slowing that is associated with temporarily switching from one task or mental set to another. For ‘Creature Counting’, a variable number of creatures are depicted in their burrows along a path with arrows pointing up and down interspersed between the creatures. Adolescents are asked to begin counting the creatures from the top-down using the arrows as a cue to switch the direction of their counting. The ‘Elevator Counting’ sub-test is a comparable test that substitutes creatures in a burrow with an elevator ascending and descending. Following demonstration of counting ability for youth only, participants complete two practice items as well as seven test items. Scores are determined by the speed and/or accuracy with which participants complete all test items.
When the current study was extended beyond the initial four years, the TEA was administered to youth older than sixteen years. Data examining the reliability and comparability of the TEAch and TEA over time are presented as supplemental material. These tests indicate adequate test-retest reliability for all measures of the TEAch. Test-retest reliability was considerably weaker for the sustained and divided attention measures of the TEA. When using the combined scores from both the TEAch and TEA over time, reliability for selective and switching attention is adequate, however divided and sustained attention is poor. See the supplementary section for complete information.
Depression Diagnosis
Depression diagnoses were assessed using The Schedule for Affective Disorders and Schizophrenia for School-Age Children - Epidemiologic Version (K-SADS-E), a semi-structured diagnostic interview that assesses DSM-IV-TR Axis I (DSM) and Research Diagnostic Criteria (RDC) psychopathology (Orvaschel, 1995). Diagnosis may be at the time of interview or since the time of the previous annual assessment. The K-SADS-E has demonstrated good test-retest and interrater reliability. The K-SADS-E was administered by the same interviewer first to the mother and then to the adolescent at baseline to assess current and lifetime Axis I psychopathology, and was re-administered at follow-ups to assess subsequent diagnoses. Inter-rater reliability for Project ACE was κ = .85 for 120 pairs of ratings (five raters for each of 24 diagnoses from 10 K-SADS-E interviews). The outcome variable in this study considered depression as those meeting criteria for DSM-IV-TR or Research Diagnostic Criteria major depression or dysthymia.
Depressive Symptoms
Depressive symptoms were measured using the Children’s Depression Inventory (CDI), a valid, reliable measure of current depressive symptoms in youth (Kovacs, 1992). This self-report instrument consists of 27 items, scored on a three-point scale ranging from zero to two. Items were summed, with higher scores indicative of higher levels of depressive symptoms. The CDI demonstrated good internal consistency with Cronbach’s α of .84 at Time 1, .85 at Time 2, .85 at Time 3, .85 at Time 4, .86 at Time 5, and .83 at Time 6.
Independent Variables
Stressful Childhood Life Events
The Childhood Life Events Scale – Parental Report (CLES-PR) measures the occurrence of stressful life events during childhood (e.g., between birth and time of questionnaire administration), as reported by a parent (Crossfield, Alloy, Gibb, & Abramson, 2002). Parents respond ‘yes’ or ‘no’ for 50 childhood events deemed to be moderate-to-majorly stressful, including items of physical and sexual abuse, bereavement, poor school performance, achievement failures and negative emotional feedback. A total score was calculated by summing all affirmative answers, with each affirmative answer scored as one so that values for this measure range from zero to fifty. The CLES-PR has demonstrable predictive validity and has been associated with the later development of negative inferential styles and impaired cognitive functioning (Crossfield et al., 2002).
Life Events Interview
Negative life events (NLEs) were measured using a semi-structured interview, the Life Events Interview (LEI) (Safford, Alloy, Abramson, & Crossfield, 2007). All LEI data used in analyses were gathered during the shorter six month assessments, but in cases where participants missed a shorter six month assessment, data were taken from the next comprehensive assessment. The LEI is administered in two steps. First, self-report questionnaires are completed by mother and child to estimate the number of NLEs experienced by the child over a given time period, and second, more information is gathered on each of the NLEs reported in the questionnaires by means of a semi-structured interview (LEI). Initially, both adolescents and their mothers completed separate versions of a self-report questionnaire, the Adolescent Life Events Questionnaire (ALEQ) (Hankin & Abramson, 2002), that ascertained the occurrence of 63 NLEs common in adolescence. Subsequently, the LEI was conducted to determine whether events endorsed on the ALEQ by adolescents and/or their mothers met event definition criteria for inclusion and occurred during the outlined time period. Objective criteria were designed to reduce the effect of a negative reporter bias. The current study examined total number of NLEs. Both the ALEQ and LEI are valid and reliable instruments (Hankin, 2008; Safford et al., 2007).
Emotional Maltreatment
The Childhood Trauma Questionnaire Short Form (CTQ) is a 28 item self-report questionnaire that has been shown to be a valid retrospective assessment of emotional maltreatment over the previous six months (Bernstein, Stein, & Newcomb, 2003). All CTQ data used in analyses were gathered during the shorter six month assessments, but in cases where participants missed a shorter six month assessment, data were taken from the next comprehensive assessment. Adolescents responded to items describing childhood maltreatment with responses ranging from 1 (Never True) to 5 (Very Often True). The CTQ yields five subscales- Emotional Abuse, Physical Abuse, Sexual Abuse, Emotional Neglect, and Physical Neglect. Project ACE only utilized the Emotional Abuse and Emotional Neglect subscales to specifically measure emotional maltreatment. These subscales have demonstrated good internal consistency in adolescent samples and a Cronbach’s α of .82 was reported for data leading up to Time 2, .85 leading up to Time 3, .86 leading up to Time 4, .88 leading up to Time 5, and .89 leading up to Time 6. The CTQ also demonstrates good concurrent validity with severity of psychopathology (Spinhoven et al., 2014).
Demographic variables
Sex and SES were assessed using self-report. Within sex, ‘female’ is coded as one and ‘male’ as zero. For SES, receipt of National School Lunch Program or a familial income less than $15,000, indicative of low SES, was coded as ‘one’ and all other participants were coded as ‘zero’.
Procedure
Adolescents completed two types of assessments. Comprehensive assessments occurred at baseline and at subsequent annual appointments. Comprehensive assessments included diagnostic interview (K-SADS-E), a behavioral assessment of attentional functioning (TEACh/TEA), an interview assessing NLEs (LEI), a self-report questionnaire assessing emotional maltreatment (CTQ), and a self-report questionnaire of depressive symptoms (CDI). Participants’ mothers completed a diagnostic interview of her child’s psychopathology at each comprehensive assessment and reported stressful childhood life events (CLES-PR) and demographic information at baseline. Comprehensive assessments were supplemented with shorter six month assessments that assessed life events, including a life event interview of general NLEs (LEI) and a self-report assessment of emotional maltreatment (CTQ). Data on depressive symptomology, diagnosis of a depressive disorder, and attentional functioning were gathered from baseline assessment (Time 1) or from any of the five subsequent comprehensive assessments (Time 2, Time 3, Time 4, Time 5, or Time 6). Life event data (LEI) were gathered from the shorter six-month assessments to ensure a prospective design; where participants were missing data from the shorter assessments, data were used from the following comprehensive assessment. Participants completed the TEAch from Time 1 until they turned 16, after which they began to take the adult version of the TEAch: the Test of Everyday Attention (TEA).
Data Analysis
Separate analyses were completed for each of the three hypotheses. All analyses were conducted using Mplus Version 7.4, with Full Information Maximum Likelihood used to handle missing data. Graphs were generated using R version 2.0.6.
Hypothesis One
The first hypothesis used (i) logistic regression to test whether lower scaled scores of switching, sustained, divided and selective attention predicted first onset of depression (DSM/RDC major depression or dysthymia) and (ii) comparable analyses used linear regression to predict to depressive symptoms. Analyses controlled for all variables that were significantly associated with the dependent variables (age, sex, childhood life stress, low SES, and number of years in the study/time to next assessment of depressive symptoms).
Hypothesis Two
The second hypothesis tested whether individuals who met criteria for a depression diagnosis experienced different trajectories of attentional functioning compared to those who did not meet criteria. This hypothesis was operationalized using within-person, piecewise latent growth models that estimated trajectories of attention functioning for those who did and did not experience depression. Piecewise latent growth curve models represented the rate of change in attentional functioning before depression onset and the rate of change in attentional functioning following first onset of depression, with the intercept being the level of the outcome at the onset of depression, or for those who never experienced depression, the final assessment. Piecewise latent growth curve models also included (i) the effect of depression diagnosis on attentional functioning as a main effect and (ii) relevant covariates. Covariates in these models were included if they were significantly associated with the dependent variable; covariates included: depression diagnosis, grand mean centered age, gender, socio-economic status, and stressful childhood life events. All predictors were mean-centered and time was coded as the number of years prior to a diagnosis/final assessment and number of years following a diagnosis.
The trajectory of attentional functioning was estimated jointly for adolescents who never experienced depression and for adolescents prior to a depression diagnosis. An interaction term (Depression Diagnosis x Trajectory of Attention (number of years prior to a depressive diagnosis/final assessment) was included to test whether the trajectory of attention differed leading up to first onset of depression for those who never experienced depression and those who met criteria for depression. Where a significant interaction was observed, this was taken to indicate within person difference in attention attributable to a depression diagnosis. Where a significant interaction was observed, the trajectory of attention following first onset was examined, comparing the trajectory of attention post-depression diagnosis to the trajectories of those with (i) no diagnosis and (ii) prior to diagnosis.
Hypothesis Three
The third hypothesis used path analysis within a structural equation modeling framework to examine the relationship between attentional functioning and depression, in particular testing whether (i) life stress (CLES-PR, LEI, CTQ) predicted both attentional functioning (switching, sustained, divided, and selective attention) and depressive symptoms, and (ii) whether indirect pathways existed between stress and depression via attention or between stress and attention via depression. In the first step, a basic model was estimated modeling the cross-lagged relationship between attention and depression across six time points. In the second step, measures of life stress were integrated into the models. See Figure 1 for a graphical representation of the modeled relationships. Depressive symptoms controlled for sex, while attention variables controlled for age and sex. In order to generate interpretable statistics across the six time points, equality constraints were applied, imposing the assumption that the hypothesized relationships across stressful life events, attentional functioning, and depressive symptoms are equivalent across all six time points. Finally, indirect pathways were tested where significant associations between attention and depression were observed. Indirect effects were estimated based on 5000 bootstrapped samples.
Figure 1.
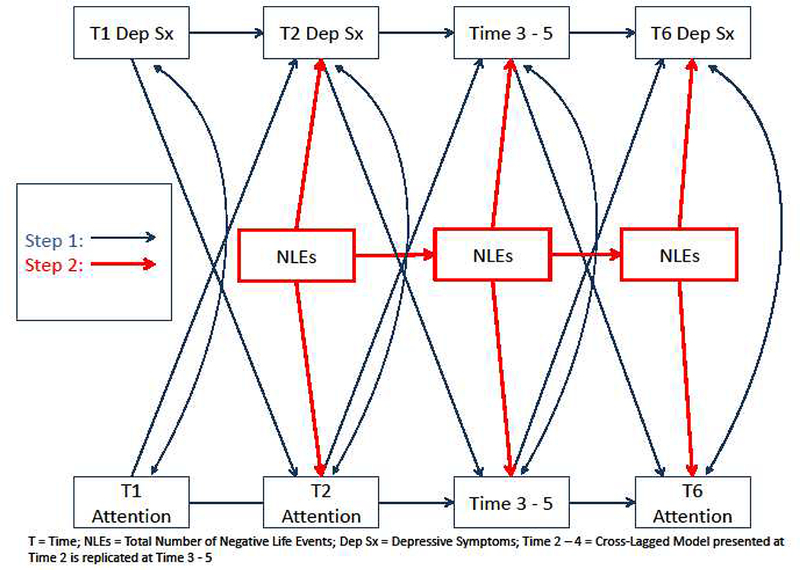
Structural Equation Path Analysis Model
Results
Bivariate correlations for the main study variables are presented in Table 1 for the 523 individuals who had complete data on diagnostic status, depressive symptoms, attention (switching, sustained, divided and selective), sex, SES and childhood stressful life events. Between baseline and the sixth annual prospective assessment, 347 adolescents were present for more than one assessment, of which 78 participants were diagnosed with a DSM-IV-TR/RDC major depressive episode or dysthymia.
Table 1.
Bivariate Correlations of Study Variables Across All Time Points for Participants with Complete Baseline Data (N = 523; Observations = 1596)
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1: DEP Dx | - | .26*** | .06* | .13*** | .01 | .07* | .00 | -.04 | .03 | .07* | .09** | .19*** |
| 2: Dep Sx | - | .11*** | -.01 | .06** | .16*** | --.05† | -.06* | -.08** | .03 | .30*** | .33*** | |
| 3: Sex (Female) | - | -.02 | .03 | .06*** | .03 | .08* | -.01 | .06* | .03 | .12*** | ||
| 4: Baseline Age | - | .03 | .02 | .20*** | .06* | .34*** | .44*** | .06* | -.10*** | |||
| 5: Low SES | - | .06** | -.12** | -.08* | -.12** | -.04 | .11*** | .02 | ||||
| 6: CLES-PR | - | -.06* | -.06* | -.10*** | -.03 | .12*** | .10*** | |||||
| 7: Selective Attention | - | .10*** | .27*** | -.02 | -.07* | -.06† | ||||||
| 8: Sustained Attention | - | .11* | .11* | -.01 | -.01 | |||||||
| 9: Switching Attention | - | .29*** | -.02 | -.09** | ||||||||
| 10: Divided Attention | - | .06† | .01 | |||||||||
| 11: LEI | - | .37*** | ||||||||||
| 12: CTQ |
Note: DEP Dx: Major or Dysthymic DSM Depression Diagnosis; Dep Sx: Children’s Depression Inventory score; SES = Socio-economic status; CLES-PR: Childhood Life Events Scale – Parental Report; Probability
= p<.10
= p<.05
= p<.01
= p<.001
Hypothesis One
Logistic regression analysis tested whether scaled scores of attention predicted first onset of a depressive episode between Time 1 and Time 6, controlling for length of time in study between baseline and Time 6, baseline depressive symptoms, baseline age, female sex, and childhood stressful life events. Scaled scores for selective (b = .04, s.e. = .03, p = .12), sustained (b = .15, s.e. = .09, p = .08), switching (b = .01, s.e. = .03, p = .86), and divided (b = .04, s.e. = .03, p = .18) attention did not predict first onset of a depressive episode. However, a relatively consistent pattern was observed in which baseline depressive symptoms, female sex, number of years participation in the study, and childhood stress predicted a greater likelihood of meeting depressive episode criteria. For selective attention, time in the study (b = .31, s.e. = .07, p < .001), baseline depressive symptoms (b = .13, s.e. = .07, p = .046), being female (at a trend level; b = .27, s.e. = .14, p = .056), and childhood life stress (b = .14, s.e. = .07, p = .04) predicted a greater likelihood of meeting depression criteria; baseline age did not, (b = −.03, s.e. = .08, p = .73). For sustained attention, time in the study (b = .31, s.e. = .07, p < .001), baseline depressive symptoms (b = .14, s.e. = .07, p = .03), being female (b = .28, s.e. = .14, p = .048), and childhood life stress (b = .15, s.e. = .07, p = .02) predicted a greater likelihood of meeting depression criteria; baseline age did not, (b = −.05, s.e. = .08, p = .55). For switching attention, time in the study (b = .33, s.e. = .07, p < .001), baseline depressive symptoms (b = .14, s.e. = .07, p = .04), being female (b = .31, s.e. = .14, p = .03), and childhood life stress (b = .14, s.e. = .07, p = .04) predicted a greater likelihood of meeting depression criteria; baseline age did not, (b = −.03, s.e =.08, p = .70). For divided attention, time in the study (b = .31, s.e. = .07, p < .001), baseline depressive symptoms (at a trend level; b = .13, s.e. = .07, p = .06), being female (at a trend level; b = .25, s.e. = .14, p = .08), and childhood life stress (b = .15, s.e. = .07, p = .03) predicted a greater likelihood of meeting depression criteria; baseline age did not, (b = −.02, s.e. = .08, p = .76)
Linear regression analysis tested whether scaled scores of attention predicted depressive symptoms at first follow-up after baseline, controlling for length of time to first follow-up, baseline depressive symptoms, baseline age, female sex, childhood stressful life events, and low SES. Scaled scores for selective (b = .02, s.e. = .04, p = .71), sustained (b = −.04, s.e. = .04, p = .35), and switching (b = −.08, s.e. = .10, p = .42) attention, did not predict depressive symptoms at follow-up. However, higher levels of divided attention (b = .11, s.e. = .04, p = .01) predicted higher levels of depressive symptoms at next follow-up.
For selective attention, time to first follow-up (b = .22, s.e. =.04, p < .001), baseline depressive symptoms (b = .48, s.e. = .04, p < .001), baseline age (b = .14, s.e. = .05, p = .005), being female (at a trend level; b = .15, s.e. = .09, p = .09), childhood life stress (b = .09, s.e. = .04, p = .046), and low SES (at a trend level; b = .−14, s.e. = .09, p = .095), predicted higher depressive symptoms. For sustained attention, time to first follow-up (b = .22, s.e. =.04, p < .001), baseline depressive symptoms (b = .48, s.e. = .04, p < .001), baseline age (b = .12, s.e. = .04, p = .005), childhood life stress (at a trend level; b = .09, s.e. = .04, p = .052), and low SES (at a trend level; b = .−16, s.e. = .09, p = .07), predicted higher depressive symptoms. However, being female did not, (b = .14, s.e. = .09, p = .11). For switching attention, time to first follow-up (b = .21, s.e. =.04, p < .001), baseline depressive symptoms (b = .48, s.e. = .04, p < .001), baseline age (b = .13, s.e. = .04, p = .004), childhood life stress (at a trend level; b = .08, s.e. = .04, p = .073), and low SES (at a trend level; b = .−15, s.e. = .09, p = .08), predicted greater depressive symptoms. However, being female did not, (b = .14, s.e. = .09, p = .11). For divided attention, time to first follow-up (b = .25, s.e. =.04, p < .001), baseline depressive symptoms (b = .47, s.e. = .04, p < .001), baseline age (b = .13, s.e. = .04, p = .003), and childhood life stress (b = .11, s.e. = .04, p = .02), predicted greater depressive symptoms. However, neither gender (b = .09, s.e. = .09, p = .29), nor low SES were associated with depressive symptoms, (b = −.13, s.e. = .09, p = .14).
Hypothesis Two
The second hypothesis examined whether individuals who met criteria for a depression diagnosis experienced different trajectories of attentional functioning compared to those who did not meet criteria. Piecewise latent growth curve models included three components. First, piecewise models estimated the rate of change in attentional functioning before depression onset/final assessment and after depression onset, where the intercept represents attentional functioning at the onset of depression for those diagnosed with depression and represents the final assessment for those who never became depressed. To test whether the trajectory of attentional functioning of depressed and non-depressed individuals differed, an interaction term was included in the model (slope leading up to depression onset/final assessment x depression diagnosis). Second, piecewise models tested the main effect of depression diagnosis on attentional functioning, namely whether depression diagnosis was significantly associated with attentional functioning at the level of the intercept. Finally, relevant covariates were included in the models when significantly associated with the outcome variables.
Data for these analyses were based on (i) 269 participants who never experienced depression and were tracked for an average of 4.11 years (SD = 1.91) and (ii) 78 participants who experienced the first onset of depression and were tracked for a mean length of 0.83 years prior to diagnosis (SD = 1.35) and 1.04 years following first diagnosis (SD = 1.48). Given the variability in the number of years in which participants were tracked in the study, analyses were replicated to reduce the potential effect of outliers – these more conservative analyses only included data gathered ±3 SDs in years prior/following first onset of depression, thereby removing observations occurring more than 4.88 years prior to depression onset/final assessment and after 5.48 years following first onset of depression.
Attentional functioning leading up to first onset of depression
In the piecewise latent growth curve model, a significant interaction (slope leading up to depression x depression diagnosis) was observed for the trajectory of selective attention comparing (i) adolescents leading up to a depression diagnosis and (ii) those who never experienced a depression diagnosis (b = −.30, s.e. = .14, p = .035), indicating a greater decline in selective attention for adolescents leading up to their first depression diagnosis. In more conservative analyses where observations ±3 SDs in years prior/following first onset of depression are removed, this effect was reduced to a non-significant association (b = −.26, s.e. = .17, p = .12). Likewise, the trajectory of switching attention for these two groups of adolescents also differed significantly, such that switching attention declined leading up to a depression diagnosis (b = −.37, s.e. = .13, p = .005). This replicated in a more conservative sample (observations ±3 SDs years prior/following first onset of depression removed), b = −.42, s.e. = .15, p = .006. No interaction was observed for sustained (b = .00, s.e. = .04, p = .93), or divided attention (b = −.19, s.e. = .14, p = .19), meaning that depression diagnosis did not predict the slope of sustained or divided attention leading up to first onset of depression. No main effect was observed for selective attention, indicating that selective attention did not differ at the level of the intercept (first onset of depression vs. final assessment; b = −.47, s.e. = .42, p = .25). A trend level main effect was observed for switching attention, such that onset of depression was associated with worse switching attention (b = −.62, s.e. = .37, p = .09). No main effect was observed for sustained (b = .11, s.e. = .10, p = .24) or divided attention (b = −.23, s.e. = .35, p = .52). When interpreting the main effect of depression diagnosis, it should be kept in mind that the vast majority of depressed individuals were diagnosed with a past, not current, depression diagnosis.
In the previous analyses depression diagnosis for the majority of participants consisted of a past depression diagnosis, however for a small percentage of participants, diagnosis was for a current depressive episode. Therefore, previous analyses did not parse apart the effect of a past versus current depression on the trajectory of attention leading up to first onset of depression. In order to more reliably test whether the trajectory of attention functioning declined prior to first diagnosis, significant results were replicated examining the trajectory of attentional functioning for depressed versus non-depressed adolescents prior to first diagnosis. These results indicated that the trajectory of selective attention did not decline prior to the assessment where a current or past depression diagnosis was confirmed, (b = −.22, s.e. = .28, p = .43); however the trajectory of switching attention did decline, (b = −.49, s.e. = .25, p = .047). It should be noted that these analyses relied on a smaller sample of 319 participants with 882 observations.
Attentional functioning prior to and following first onset of depression
Post-hoc analyses indicated that the slope of selective attention following depression diagnosis (i) differed at a trend level from the slope of depressed individuals leading up to a depression diagnosis (b = .51, s.e. = .28, p = .067), and (ii) did not significantly differ from the slope of those who never experienced a depression diagnosis (b = .21, s.e. = .19, p = .27). Post-hoc analyses indicated that the slope of switching attention following depression diagnosis differed significantly from both (i) the slope of depressed individuals leading up to a depression diagnosis (b = .70, s.e. = .23, p = .002), and (ii) those who never experienced a depression diagnosis (b = .33, s.e. = .14, p = .02). For post-hoc analyses in a more conservative sample, a significant difference was observed for (i) (b = .71, s.e. = .26, p = .006), but not (ii) (b = .29, s.e. =.16, p = .64). Visual depictions of the trajectories of selective and switching attention using the entire sample can be seen in Figure 2. Visual depictions of the trajectories of selective and switching attention using a more conservative sample are presented in Supplementary Figure 1 in the supplementary material. All beta coefficients, standard errors, and levels of significance estimated by piecewise latent growth curve models are reported in Supplementary Table 1.
Figure 2.

Piecewise Growth Model of Normed Attentional Development without MDD, prior to MDD and post MDD.
Hypothesis Three
The third hypothesis tested whether (i) prospective associations between attention and depression were observable, (ii) whether three forms of life stress (childhood, recent emotional maltreatment, and total number of NLEs) were associated with both attention and depression, in addition to whether (iii) indirect pathways existed between stress and depression via attention or between stress and attention via depression.
Step One: Prospective associations between attention and depression
For step one, a base model estimated the prospective relationship between attention and depression. Depressive symptoms prospectively predicted lower selective and switching attention, but not sustained or divided attention. Additionally, higher levels of switching attention prospectively predicted lower levels of depressive symptoms. Base model fit statistics (RMSEA/CFI) reported in Table 2 were estimated before equality constraints were imposed; however, fit statistics were almost identical following imposition of equality constraints. Overall, for base level models, model fit was adequate based on RMSEA; however, represented a poor fit based on CFI.
Table 2.
Structural Equation Model Testing Reciprocal Associations Between Attention and Depression as well as Types of Life Stress
| Step One: Base Model |
Step Two: + Childhood Stress
(CLES-PR) |
|||||||
|---|---|---|---|---|---|---|---|---|
| CTQ | Selective | Sustained | Switching | Divided | Selective | Sustained | Switching | Divided |
| Model Fit | ||||||||
| Chi-Squared Model Fit | 165.19*** | 117.55*** | 132.46*** | 136.11*** | 179.36*** | 130.07** | 153.73*** | 142.00*** |
| RMSEA: Estimate (90% CI) | .06(.05/.07) | .05 (.03/.06) | .05 (.04/.06) | 05 (.04/.06) | .06 (.05/.07) | .04 (.03/.05) | .05 (.04/.06) | .04 (.03/.05) |
| CFI | .84 | .88 | .88 | .86 | .85 | .92 | .89 | .88 |
| Outcome: Attention | ||||||||
| Dep Sx. (1 Year Prior) | −.05** | .00 | −.03* | .02 | −.05** | .00 | −.03* | .03 |
| Stress | −.02 | −.01 | −.04* | −.04* | ||||
| Outcome: Depression | ||||||||
| Attention (1 Year Prior) | −.01 | −.30† | −.11* | .02 | .02 | −.22 | −.12* | .01 |
| Stress | .08* | .07* | .07* | .07* | ||||
| Outcome: Stress | ||||||||
| Dep Sx. (6 Months Prior) | ||||||||
| Attention (6 Months Prior) | ||||||||
| Attention with Dep Sx. | .11 | −.20† | −.18 | .02 | .17 | −.19 | −.02 | .20 |
| LEI | ||||||||
| Step Two: + Recent Emotional
Maltreatment Stress (CTQ) |
Step Two: + Recent Total Life
Stress (LEI) |
|||||||
| Model Fit | Selective | Sustained | Switching | Divided | Selective | Sustained | Switching | Divided |
| Chi-Squared Model Fit | 290.45*** | 245.84*** | 254.68*** | 265.91*** | 322.77*** | 238.14*** | 269.67*** | 256.85*** |
| RMSEA: Estimate (90% CI) | .05(.04/.06) | .04 (.03/.05) | .04 (.03/.05) | .04(.04/.05) | .05(.04/.06) | .04(.03/.05) | .05(.04/.06) | .05(.04/.06) |
| CFI | .86 | .92 | .92 | .90 | .85 | .88 | .88 | .86 |
| Outcome: Attention | ||||||||
| Dep Sx. (1 Year Prior) | −.04* | .00 | −.02 | .03 | −.05** | .00 | −.03† | .01 |
| Stress | −.02 | −.01 | −.03 | −.02 | .00 | −.01† | −.02 | .00 |
| Outcome: Depression | ||||||||
| Attention (1 Year Prior) | .01 | −.11 | −.11* | .02 | −.02 | −.24 | −.11* | .02 |
| Stress | 21*** | 21*** | .21*** | .22*** | .24*** | .24*** | .24*** | .24*** |
| Outcome: Stress | ||||||||
| Dep Sx. (6 Months Prior) | 22*** | 21*** | .22*** | .22*** | .20*** | .20*** | .20*** | 19*** |
| Attention (6 Months Prior) | .02 | −49*** | .02 | .02 | .03 | −.02 | .04 | .03 |
| Attention with Dep Sx. | .20 | −.20† | −.03 | .10 | .16 | −.15 | −.04 | .04 |
RMSEA = Root Mean Square Error Of Approximation; CFI = Comparative Fit Index; Dep Sx = Depressive Symptoms; CTQ := Childhood Trauma Questionnaire
p<.10
p <.05
p <.01
<.001
Step Two: Addition of life stress to models of prospective associations between attention and depression
Step two involved the addition of three forms of life stress: childhood stress, recent emotional maltreatment, and recent NLEs to the base model. The addition of stress to the model is outlined in Figure 1, with the exception of the CLES-PR. Inasmuch as the CLES-PR is only administered at baseline, CLES-PR is simply added as a predictor to both attention and depression outcomes. For Step two, the overall pattern of results in the base model is replicated when childhood stress is included in the model. Additionally, greater exposure to childhood stress was associated with higher levels of depressive symptoms across all time points as well as worse switching and divided attention. When emotional maltreatment is added to the base model, previous results hold, with the exception of higher depressive symptoms prospectively predicting worse switching attention. Higher levels of emotional maltreatment are associated with more severe depressive symptoms, but not any form of attention. Additionally, higher levels of sustained attention are associated with significantly lower reports of emotional maltreatment. Finally, when recent negative life events (LEI) are introduced into the model, previous results hold, although higher depressive symptoms prospectively predict worse switching attention at a trend level (see Table 2).
Step Three: Indirect pathways linking attention and depression via stress
Higher depressive symptoms prospectively predicted worse selective attention, whereas a reciprocal association was observed between switching attention and depression. Consequently, indirect pathways linking selective and switching attention with depression were tested. Higher parent report of childhood stress was associated with both higher depressive symptoms and worse switching attention. Across all time points, a significant indirect pathway was observed from childhood stress to (i) switching attention via depressive symptoms (b = .005; 95% CI: .0001, .013), and (ii) depressive symptoms via switching attention (b = −.003; 95% CI: −.008, - .0001). In both cases, the precise value of the bootstrapped confidence interval approaching zero could not be precisely estimated due to it being such a small value; re-scaling variables to better estimate this small value was attempted, unsuccessfully, to be the point where the model could no longer be computed. No other significant indirect pathways linked childhood stress, emotional maltreatment, or total number of NLEs with either attention via depression, or depression via attention.
Discussion
The current study tested three hypotheses postulating how attentional functioning related to depression. The first hypothesis was that poor attention preceded and increased the likelihood that an individual would experience a depressive episode. The second hypothesis was that attentional deficits were a consequence of depression, which would consequently emerge following the first onset of depression. The third hypothesis was that both depression and impaired attention were explained by a third underlying variable: stress. The results of this paper suggest that the association between depression and attention is more complex than conceptualized by any of these three hypotheses alone. First, piecewise latent growth curve models that used data from the entire study indicate that switching attention declined leading up to first onset of depression, before subsequently recovering in the years following first onset; similar although less consistent patterns were also observed for selective attention. Second, there was good evidence that the relationship between attention and depression was not confined to a depressive episode. Switching attention declined prior to first onset of depression and further, outside of depressive episodes, higher depressive symptoms consistently predicted worse selective and switching attention, with higher switching attention also prospectively predicting lower depressive symptoms. These results suggest a complex, reciprocal interaction between depressive symptoms and attentional functioning that are not confined to a depressive episode. Finally, this paper provides evidence that childhood stress, but not recent negative life events or emotional maltreatment, predicted more severe depressive symptoms via impaired switching attention and worse switching attention via depressive symptoms, thereby suggesting that exposure to childhood stress may, in part, explain the close relationship between depression and at least one component of cognitive functioning: switching attention.
Depression and Attentional Functioning in Adolescents
A central finding of this study was that the trajectory of attention, particularly switching attention, declined leading up to a depression diagnosis and subsequently recovered. Although this study predominantly examined cognitive function in euthymic adolescents, these results are in line with previous studies that have found that (i) attention is impaired in both adults and youth with depression (Rock et al., 2013; Wagner et al., 2015), (ii) attentional deficits are observable in adolescents, and therefore are not simply artifacts explained by age or the cumulative effect of multiple depressive episodes (McClintock, Husain, Greer, & Cullum, 2010; Snyder, 2013), and (iii) that specific deficits in selective and switching attention are observed in depression (Gualtieri, Johnson, & Benedict, 2006; Rock et al., 2013; Snyder, 2013). The failure to observe decreases in sustained attention, however, is at odds with previous research (Wagner et al., 2015). It should be noted, however, that this discrepancy with sustained attention may be due to poor reliability for sustained attention across the TEA and TEAch or the low scoring ceiling of the ‘Score!’ subtest, thereby potentially not effectively discriminating different levels of aptitude in a community sample.
Interestingly, the temporal relationship between attentional functioning and depression was more complex than originally proposed by any single hypothesis. First, the recovery of attention following depression is largely at odds with previous meta-analyses (Bora et al., 2013; Rock et al., 2013). The cause of this discrepancy is unclear; however, it may be attributable to the longitudinal study design. For example, it is possible that recovery of attentional functioning may be an extended temporal process better detected in prospective, longitudinal studies. Alternatively, it may be that cognitive dysfunction is caused by the presence of sub-threshold depressive symptoms (Rock et al., 2013). Thus, recovery may be a process that extends beyond a depressive episode, with cognitive dysfunction enduring until persistent sub-threshold depressive symptoms dissipate - this hypothesis is supported by the linear, prospective relationship between depressive symptoms and selective/switching attention observed in this study. An additional competing hypothesis is that the recovery of attentional functioning in this study is attributable to specific clinical characteristics (e.g. medication history or number of depressive episodes) that are more characteristic of a community sample of adolescents than, say, inpatients in a psychiatric facility.
Attentional Functioning and Prospective Depression
There was no evidence that switching, sustained, divided or selective attention at baseline predicted first onset of depression during the years that participants were tracked in this study, although there was some evidence that higher divided attention predicted higher subsequent depressive symptoms at first follow-up. This association between divided attention and depression was not replicated across multiple time points, suggesting that this effect may reflect either type I error or, potentially, temporally bound increased risk that accompanies a surge in cognitive functioning characteristic of early adolescence. Overall, the failure to observe a relationship between baseline attention functioning and subsequent depression is at odds with a number of large, longitudinal studies that have found that general cognitive functioning prospectively predicts first onset of depression (Franz et al., 2011; Koenen et al., 2009; Zammit et al., 2004). It is possible that this study was underpowered to detect the small effects reported in these studies, that discrepant results were due to the substantially shorter follow-up period of this study, or that deficits in attentional functioning, as opposed to more generalized cognitive functioning, does not precede depression. Instead, results reported in this study support a recent meta-analysis that the prospective relationship between cognition and depression was largely attributable to the effect of sub-clinical depressive symptoms at the time of initial cognitive assessment on cognitive performance (Scult et al., 2017). Nonetheless, while there is no evidence that baseline attentional functioning predicted subsequent depression, higher levels of switching attention predicted lower levels of depressive symptoms across adolescence and switching attention declined prior to first onset of depression. These results, when combined with the null baseline results, suggest that the effect of cognitive functioning on subsequent depressive diagnosis is too small to be detected in this study, and is only detectable when examining a continuum of depressive symptomology. These results are in line with previous research reporting that, in youth, poor executive functioning (i.e. cognitive control) predicts higher depressive symptoms (Snyder & Hankin, 2016).
Stress and Prospective Attentional Functioning
Childhood stress, but not recent emotional maltreatment or negative life events, was associated with worse switching attention in addition to increased depressive symptoms across multiple time points. These findings are consistent with abundant research linking stress with depression (Hammen, 2005), and they also concur with a smaller body of research that has found that life adversity, particularly extreme stressors such as sexual abuse or early foster care, is associated with worse cognitive functioning (Pechtel & Pizzagalli, 2011). Moreover, these results extend previous studies by demonstrating that less severe stressors, such as general childhood stress, are associated with worse switching attention. Thus, the effect of childhood stress on attention may be more deleterious than subsequent stress during adolescence. Results also suggest that switching, rather than selective, divided, or sustained attention, was negatively associated with childhood stress. Given that switching attention is a measure of attention particularly reliant on pre-frontal functioning, it was not too surprising that switching attention was differentially susceptible to stress (Lupien et al., 2009).
However, not only was childhood stress predictive of worse switching attention, childhood stress predicted higher depressive symptoms via switching attention and worse switching attention via depressive symptoms, thereby indicating that childhood stress may be a mechanism explaining the close association between depression and cognition. Previous studies have suggested that an association between cognitive deficits and depression may reflect genetic liability (Christensen, Kyvik, & Kessing, 2006; Franz et al., 2011). Results from the current study suggest that, in addition to genetic liability, impaired cognition and depression may be linked via the deleterious effect of childhood stress (Lupien et al., 2009). Other studies report that executive functioning (cognitive control) predicts depressive symptoms via self-generated stressful life events and rumination (Snyder & Hankin, 2016). Two types of life stress measured in this study, emotional maltreatment and general negative life events, did not mediate a relationship between switching attention and depression. This discrepancy in results may be driven by the type of stress measured, which was not confined to self-generated negative life events. It should be noted that the overall effects of (i) switching attention on depression and (ii) the indirect effects of depression on switching and switching attention on depression via childhood stress were small, particularly the indirect effects. Thus, cognitive deficits in depression may be attributable to the effect of risk factors for depression as well as the effect of depression itself, however these effects are likely modest in size.
Limitations
Conclusions should be considered alongside the study’s limitations. First, two measures of attention (sustained and divided) demonstrated poor reliability, thereby weakening confidence in the conclusions pertaining to these measures. Second, both the TEA and TEAch are normed using small, non-U.S. samples, thereby increasing the risk that normed scores do not capture performance in a diverse adolescent/young adult population. This risk is somewhat offset by focus on within, rather than between, person longitudinal change in a truly prospective, diverse sample of adolescents with multiple behavioral assessments of attention as well as diagnostic assessments. Third, the absolute number of adolescents who experienced first onset of a DSM-IV-TR/RDC major depressive or dysthymic disorder was small, given the reliance on a community sample. This increases the risk that this group of adolescents who experienced first onset of depression differs significantly from adolescents generally. Nonetheless, a benefit of a community sample is that the results may be more generalizable to adolescents who are at risk of experiencing depressive symptoms. Fourth, indices of model fit were not uniformly acceptable across all of the models presented, thereby increasing the risk of unreliable parameter estimates. However, when considered as a whole, there was good indication of overall model fit and the analyses performed were intended to answer theoretical questions and, consequently, models representing better model fit were not sought. Finally, although the measure of attention used in this study is an ecologically valid and reliable assessment of attention that is both age and gender normed, we cannot exclude the possibility that higher levels of attention were, in fact, indicative of higher levels of general intelligence.
Conclusions
These data demonstrate that the relationship between attentional functioning and depression is more complex than previously thought. Similar to many previous studies, some components of attentional functioning were shown to decline prior to a depressive diagnosis, before subsequently recovering. However, a complex reciprocal relationship between attention, switching attention in particular, and depression also was observed outside of a depressive episode. This study demonstrates that this complex, reciprocal relationship between attention and depression may partially be attributable to a third underlying process: childhood stress. These results highlight the importance of conceptualizing the role that independent risk factors may play in elevating risk of both depression and impaired cognition.
Supplementary Material
Supplementary Table 1
All Parameter Estimates for Piecewise Latent Growth Curve Model
Supplementary Table 2
Pairwise Auto-Correlation of Selective, Sustained, Switching, and Divided Attention for the TEA and TEAch combined, the TEAch alone, and the TEA alone at consecutive time points using pairwise deletion
Supplementary Table 3
All Parameter Estimates for Piecewise Latent Growth Curve Model
Supplementary Figure 1
Piecewise Growth Model of Normed Attentional Development without MDD, prior to MDD and post MDD using data gathered 4.88 years prior to diagnosis/final assessment and 5.48 years following diagnosis.
Acknowledgments
This research was supported by National Institute of Mental Health Grants MH079369 and MH101168 to Lauren Alloy.
Authorship
Data were collected as part of NIMH grants awarded to L.B.A. and L.Y.A. N.M.G developed the study design with input from J.N. N.M.G. and J.N. conducted data analysis with considerable support from T.M.O. N.M.G. wrote the manuscript and all authors provided substantive revisions. All authors approved the final draft of the manuscript for submission.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Abramson LY, Metalsky GI, & Alloy LB (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96, 358–372. doi: 10.1037/0033-295x.96.2.358 [DOI] [Google Scholar]
- Alloy LB, Black SK, Young ME, Goldstein KE, Shapero BG, Stange JP, .. Abramson LY (2012). Cognitive vulnerabilities and depression versus other psychopathology symptoms and diagnoses in early adolescence. Journal of Clinical Child and Adolescent Psychology, 41, 539–560. doi: 10.1080/15374416.2012.703123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin MP, Mitchell P, & Goodwin GM (2001). Cognitive deficits in depression: Possible implications for functional neuropathology. The British Journal of Psychiatry, 178, 200–206. doi: 10.1192/bjp.178.3.200 [DOI] [PubMed] [Google Scholar]
- Baune BT, Czira ME, Smith AL, Mitchell D, & Sinnamon G (2012). Neuropsychological performance in a sample of 13–25 year olds with a history of non-psychotic major depressive disorder. Journal of Affective Disorders, 141, 441–448. doi: 10.1016/j.jad.2012.02.041 [DOI] [PubMed] [Google Scholar]
- Beck AT (1976). Cognitive therapy and the emotional disorders. New York:International Universities Press. [Google Scholar]
- Bernstein D, Stein J, & Newcomb M (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27, 169–190. [DOI] [PubMed] [Google Scholar]
- Bora E, Harrison BJ, Yücel M, & Pantelis C (2013). Cognitive impairment in euthymic major depressive disorder: a meta-analysis. Psychological Medicine, 43, 2017–2026. doi: 10.1017/s0033291712002085 [DOI] [PubMed] [Google Scholar]
- Burcusa SL, & Iacono WG (2007). Risk for recurrence in depression. Clinical Psychology Review, 27, 959–985. doi: 10.1016/j.cpr.2007.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt DB, Zembar MJ, & Niederehe G (1995). Depression and memory impairment: a meta-analysis of the association, its pattern, and specificity. Psychological Bulletin, 117, 285–305. doi: 10.1037/0033-2909.117.2.285 [DOI] [PubMed] [Google Scholar]
- Christensen MV, Kyvik KO, & Kessing LV (2006). Cognitive function in unaffected twins discordant for affective disorder. Psychological Medicine, 36(08), 1119–1129. [DOI] [PubMed] [Google Scholar]
- Connolly SL, Wagner CA, Shapero BG, Pendergast LL, Abramson LY, & Alloy LB (2014). Rumination prospectively predicts executive functioning impairments in adolescents. Journal of Behavior Therapy and Experimental Psychiatry, 45, 46–56. doi: 10.1016/j.jbtep.2013.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crossfield AG, Alloy LB, Gibb BE, & Abramson LY (2002). The development of depressogenic cognitive styles: The role of negative childhood life events and parental inferential feedback. Journal of Cognitive Psychotherapy, 16(4), 487–502. [Google Scholar]
- Franz CE, Lyons MJ, O’Brien R, Panizzon MS, Kim K, Bhat R, . . . Kremen WS (2011). A 35-year longitudinal assessment of cognition and midlife depression symptoms: the Vietnam era twin study of aging. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 19, 559–570.doi: 10.1097/JGP.0b013e3181ef79f1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotlib IH, & Joormann J (2010). Cognition and depression: current status and future directions. Annual Review of Clinical Psychology, 6, 285–312. doi: 10.1146/annurev.clinpsy.121208.131305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gualtieri CT, Johnson LG, & Benedict KB (2006). Neurocognition in depression: patients on and off medication versus healthy comparison subjects. The Journal of Neuropsychiatry and Clinical Neurosciences, 18(2), 217–225. doi: 10.1176/jnp.2006.18.2.217 [DOI] [PubMed] [Google Scholar]
- Günther T, Holtkamp K, Jolles J, Herpertz-Dahlmann B, & Konrad K (2004). Verbal memory and aspects of attentional control in children and adolescents with anxiety disorders or depressive disorders. Journal of Affective Disorders, 82(2), 265–269. [DOI] [PubMed] [Google Scholar]
- Günther T, Konrad K, De Brito SA, Herpertz‐Dahlmann B, & Vloet TD (2011). Attentional functions in children and adolescents with ADHD, depressive disorders, and the comorbid condition. Journal of Child Psychology and Psychiatry, 52(3), 324–331. [DOI] [PubMed] [Google Scholar]
- Hammen C (2005). Stress and depression. Annual Review of Clinical Psychology, 1, 293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938 [DOI] [PubMed] [Google Scholar]
- Han G, Klimes-Dougan B, Jepsen S, Ballard K, Nelson M, Houri A, . . . Cullen K (2012). Selective neurocognitive impairments in adolescents with major depressive disorder. Journal of Adolescence, 35, 11–20. doi: 10.1016/j.adolescence.2011.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL (2008). Stability of cognitive vulnerabilities to depression: a short-term prospective multiwave study. Journal of Abnormal Psychology, 117(2), 324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, & Abramson LY (2002). Measuring cognitive vulnerability to depression in adolescence: Reliability, validity, and gender differences. Journal of Clinical Child and Adolescent Psychology, 31(4), 491–504. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, & Angell KE (1998). Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology, 107(1), 128–140. [DOI] [PubMed] [Google Scholar]
- Hasselbalch BJ, Knorr U, & Kessing LV (2011). Cognitive impairment in the remitted state of unipolar depressive disorder: a systematic review. Journal of Affective Disorders, 134, 20–31. doi: 10.1016/j.jad.2010.11.011 [DOI] [PubMed] [Google Scholar]
- Kertz SJ, Belden AC, Tillman R, & Luby J (2016). Cognitive control deficits in shifting and inhibition in preschool age children are associated with increased depression and anxiety over 7.5 years of development. Journal of Abnormal Child Psychology, 44(6), 1185–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC (1997). The effects of stressful life events on depression. Annual Review of Psychology, 48(1), 191–214. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, . . Petukhova M (2012). Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry, 69(4), 372–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenen KC, Moffitt TE, Roberts AL, Martin LT, Kubzansky L, Harrington H, . . . Caspi, A. (2009). Childhood IQ and adult mental disorders: A test of the cognitive reserve hypothesis. American Journal of Psychiatry, 166, 50–57. doi: 10.1176/appi.ajp.2008.08030343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M (1992). The Children’s Depression Inventory. Psychopharmacology Bulletin, 21(4), 995–998. [PubMed] [Google Scholar]
- Lee R, Hermens DF, Porter M. a., & Redoblado-Hodge MA (2012). A meta-analysis of cognitive deficits in first-episode Major Depressive Disorder. Journal of Affective Disorders, 140, 113–124. doi: 10.1016/j.jad.2011.10.023 [DOI] [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, & Heim C (2009). Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience, 10, 434–445. doi: 10.1038/nrn2639 [DOI] [PubMed] [Google Scholar]
- Manly T, Anderson V, Nimmo-Smith I, Turner A, Watson P, & Robertson IH (2001). The differential assessment of children’s attention: The Test of Everyday Attention for Children (TEA-Ch), normative sample and ADHD performance. Journal of Child Psychology and Psychiatry, 42(08), 1065–1081. [DOI] [PubMed] [Google Scholar]
- McClintock SM, Husain MM, Greer TL, & Cullum CM (2010). Association between depression severity and neurocognitive function in major depressive disorder: a review and synthesis. Neuropsychology, 24(1), 9. [DOI] [PubMed] [Google Scholar]
- Orvaschel H (1995). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Epidemiologic Version, Fifth Edition (K-SADS-E; ). [Google Scholar]
- Pechtel P, & Pizzagalli DA (2011). Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacology (Berl), 214(1), 55–70. doi: 10.1007/s00213-010-2009-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson IH, Ward T, Ridgeway V, & Nimmo-Smith I (1994). The Test of Everyday Attention: TEA: Thames Valley Test Company Bury St. Edmunds; , UK. [Google Scholar]
- Rock PL, Roiser JP, Riedel WJ, & Blackwell a. D. (2013). Cognitive impairment in depression: A systematic review and meta-analysis. Psychological Medicine, 1–12. doi.org/10.1017/S0033291713002535 [DOI] [PubMed] [Google Scholar]
- Safford SM, Alloy LB, Abramson LY, & Crossfield AG (2007). Negative cognitive style as a predictor of negative life events in depression-prone individuals: A test of the stress generation hypothesis. Journal of Affective Disorders, 99(1), 147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scult MA, Paulli AR, Mazure ES, Moffitt TE, Hariri AR, & Strauman TJ (2017). The association between cognitive function and subsequent depression: a systematic review and meta-analysis. Psychological Medicine, 47(1), 1–17. doi: 10.1017/s0033291716002075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR (2013). Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychological Bulletin, 139, 81–132. doi: 10.1037/a0028727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, & Hankin BL (2016). Spiraling out of control: Stress generation and subsequent rumination mediate the link between poorer cognitive control and internalizing psychopathology. Clinical Psychological Science, 4(6), 1047–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Miyake A, & Hankin BL (2015). Advancing understanding of executive function impairments and psychopathology: Bridging the gap between clinical and cognitive approaches. Frontiers in Psychology, 6, 328. doi: 10.3389/fpsyg.2015.00328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinhoven P, Penninx BW, Hickendorff M, van Hemert AM, Bernstein DP, & Elzinga BM (2014). Childhood Trauma Questionnaire: Factor structure, measurement invariance, and validity across emotional disorders. Psychological Assessment, 26(3), 717. [DOI] [PubMed] [Google Scholar]
- Vilgis V, Silk TJ, & Vance A (2015). Executive function and attention in children and adolescents with depressive disorders: a systematic review. European Child & Adolescent Psychiatry, 24(4), 365–384. [DOI] [PubMed] [Google Scholar]
- Wagner Doering, B., Helmreich I, Lieb K, & Tadić A (2012). A meta-analysis of executive dysfunctions in unipolar major depressive disorder without psychotic symptoms and their changes during antidepressant treatment. Acta Psychiatrica Scandinavica, 125, 281–292. doi: 10.1111/j.1600-0447.2011.01762.x [DOI] [PubMed] [Google Scholar]
- Wagner S, Müller C, Helmreich I, Huss M, & Tadić A (2015). A meta-analysis of cognitive functions in children and adolescents with major depressive disorder. European Child & Adolescent Psychiatry, 24, 5–19. doi: 10.1007/s00787-014-0559-2 [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, . .Vos T (2013). Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet, 382, 1575–1586. doi: 10.1016/s0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- Wilkinson PO, & Goodyer IM (2006). Attention difficulties and mood‐related ruminative response style in adolescents with unipolar depression. Journal of Child Psychology and Psychiatry, 47(12), 1284–1291. [DOI] [PubMed] [Google Scholar]
- Zammit S, Allebeck P, David AS, Dalman C, Hemmingsson T, Lundberg I, & Lewis G (2004). A longitudinal study of premorbid IQ score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Archives of General Psychiatry, 61(4), 354–360. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1
All Parameter Estimates for Piecewise Latent Growth Curve Model
Supplementary Table 2
Pairwise Auto-Correlation of Selective, Sustained, Switching, and Divided Attention for the TEA and TEAch combined, the TEAch alone, and the TEA alone at consecutive time points using pairwise deletion
Supplementary Table 3
All Parameter Estimates for Piecewise Latent Growth Curve Model
Supplementary Figure 1
Piecewise Growth Model of Normed Attentional Development without MDD, prior to MDD and post MDD using data gathered 4.88 years prior to diagnosis/final assessment and 5.48 years following diagnosis.


