Abstract
Endobronchial ultrasound (EBUS)-guided transbronchial needle aspiration (TBNA) has diagnostic accuracy and negative predictive value for the diagnosis of mediastinal tubercular lymphadenitis, especially when culture and cytological diagnosis is combined with high clinical suspicion. Both sarcoidosis and tuberculosis (TB) demonstrate granulomatous inflammation on cytology. Diagnosis of sarcoidosis in regions with a high burden of TB is challenging. We conducted a prospective study in 179 cases of suspected granulomatous pathology in mediastinal lymphadenopathy cases to evaluate the role of EBUS-TBNA in diagnosis of sarcoidosis and TB. It was found that extensive caseous necrosis, acid-fast bacilli positivity on Ziehl–Neelsen staining, and/or microbiological culture positivity have high positive predictive value for the diagnosis of TB.
Keywords: Endobronchial ultrasound-transbronchial needle aspiration, epithelioid cell granulomas, granulomatous inflammation, sarcoidosis, tuberculosis
Sarcoidosis and tuberculosis (TB) are the major causes of intrathoracic granulomatous lymphadenopathy. Endobronchial ultrasound (EBUS)-guided transbronchial needle aspiration (TBNA) is currently the preferred initial modality for evaluating intrathoracic lymphadenopathy. The most definite evidence of TB is demonstration of Mycobacterium tuberculosis by culture or molecular methods. However, the diagnostic sensitivity of microbiologic techniques is low. Whether cytomorphologic features of granuloma can diagnose TB and distinguish it from sarcoidosis, its close mimic, remains unclear. We performed a prospective observational study of subjects undergoing EBUS-TBNA to evaluate the same.
A single cytopathologist (NG), who was blinded to the clinical data and final diagnosis, reported the TBNA. The following features were recorded: adequacy (either diagnostic or shows lymphocyte preponderance), the presence of granulomas, number of granulomas, average number of epithelioid cells in granulomas, necrosis [graded as 1 (focal), 2, and 3 (extensive)], stain for acid-fast bacilli (AFB), and the final impression (TB vs. sarcoidosis). The final diagnosis was made after 6 months' of follow-up.
The diagnosis of TB was based on the demonstration of two of the following: (a) consistent clinicoradiological presentation; (b) positive culture for Mycobacterium tuberculosis or Xpert MTB/Rif positivity; and (c) clinicoradiological response to anti-TB treatment. Sarcoidosis was diagnosed when all the following criteria were satisfied: (a) consistent clinicoradiological presentation; (b) non-necrotizing epithelioid cell granulomas on TBNA, TBLB, or EBB along with no AFB on Ziehl–Neelsen stain and no growth of mycobacteria on MGIT; and (c) clinicoradiological response after treatment with glucocorticoids. The procedural details and data of some patients included in this study have been described previously.[1]
Of the 179 consecutive subjects enrolled (January 2014 to March 2015), sarcoidosis and TB were diagnosed in 145 (81%) and 34 (19%), respectively. Granulomas were identified in 135 (75.4%), including 113 (77.9%) and 22 (67.6%) cases of sarcoidosis and TB, respectively [Table 1; Figures 1 and 2]. Necrosis was rare in sarcoidosis (n = 9, 6.2%), and it was never extensive. Based on the cytomorphology, a correct diagnosis was favored by the cytologist in 83 (61%) subjects, whereas misdiagnosis occurred in 40 (29.4%), when compared with the final diagnosis (after 6 months of follow-up).
Table 1.
EBUS-TBNA cytology features of subjects with granulomatous intrathoracic lymphadenopathy
| Parameter | Sarcoidosis (n=145) | Tuberculosis (n=34) | Total (n=179) | P |
|---|---|---|---|---|
| Age in years | 44.1 (13.4) | 34.2 (15.2) | 42.2 (15.2) | <0.0001 |
| Male gender | 86 (59.3) | 21 (61.8) | 97 (54.2) | 0.79 |
| TST ≥10 mm | 7 (4.9) | 23 (67.6) | 30 (16.8) | <0.0001 |
| Adequate material on cytology | 132 (91) | 33 (97.1) | 165 (92.2) | 0.16 |
| Granuloma on EBUS-TBNA | 113 (77.9) | 22 (64.7) | 135 (75.4) | 0.69 |
| Necrosis | 0.0001 | |||
| None | 136 (93.8) | 15 (44.1) | 151 (84.4) | |
| Grade 1 (focal) | 9 (6.2) | 7 (20.6) | 16 (8.9) | |
| Grade 2 (neither 1 or 3) | 0 | 9 (26.5) | 9 (5) | |
| Grade 3 (extensive) | 0 | 3 (8.8) | 3 (1.7) | |
| AFB-positive | 0 | 15 (44.2) | 15 (8.4) | 0.0001 |
| Cytologists final impression based on the morphology of granuloma* | 0.02 | |||
| Correct diagnosis | 70 (61.9) | 13 (56.5) | 83 (61) | |
| Misdiagnosis | 34 (30.1) | 6 (2.6) | 40 (29.4) | |
| Difficult to differentiate | 9 (8) | 3 (17.4) | 13 (9.6) |
EBUS-TBNA: Endobronchial ultrasound-guided transbronchial needle aspiration; TST: Tuberculin skin test; AFB: Acid-fast bacilli. *n=135 was used to calculate the percentages of correct diagnosis and misdiagnosis
Figure 1.
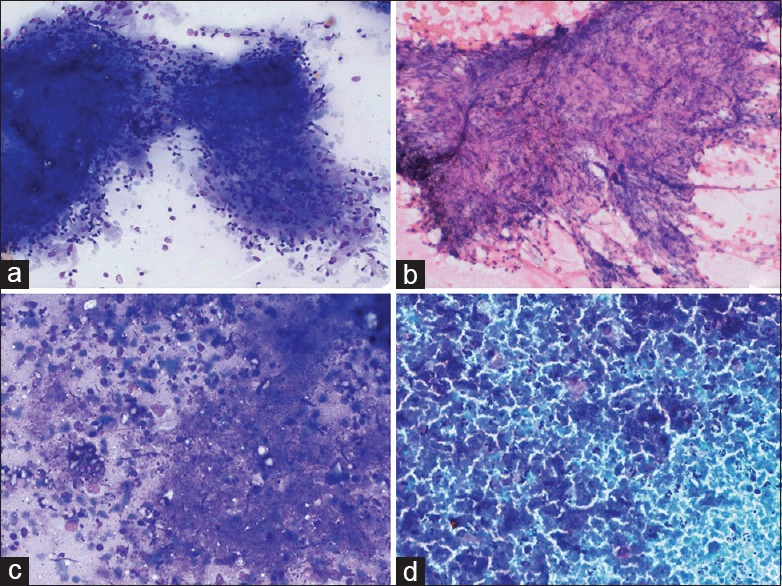
A panel of microphotographs showing epithelioid cell granulomas (a and b) and necrotizing inflammation (c and d) in tuberculosis (a: MGG 20×; b: H and E 20×, MGG: 20×, Pap 20×)
Figure 2.
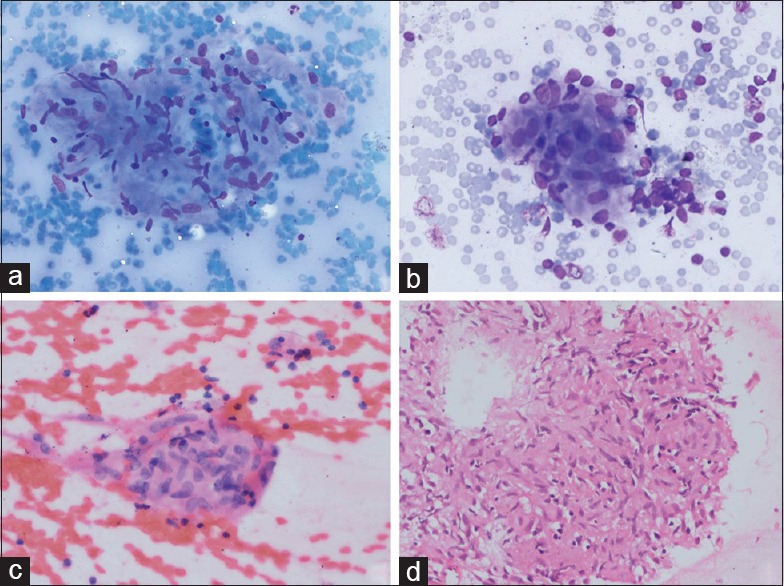
A panel of microphotographs showing epithelioid cell granulomas in sarcoidosis (a: MGG 20×; b: MGG 20×, H & E 40×, H & E in cell block 40×)
Diagnosing sarcoidosis in countries with a high TB burden poses a great challenge, and multiple features (clinical, imaging, microbiology, and cytology) should be taken into account. Despite decades of research, differentiating these two entities remains difficult, as both of them share similar clinical, radiological, and even pathological features.[2] A small retrospective study concluded that the morphology of granuloma did not help in differentiating TB and sarcoidosis.[3] Navani et al. in their study showed high diagnostic accuracy in diagnosing TB on EBUS-TBNA samples.[4] This study had more cases of sarcoidosis as EBUS-TBNA was done in a majority of suspected sarcoidosis cases and TB could be diagnosed by other investigations. This could be a reason for having lower diagnostic accuracy in this study. Though the cytomorphology in sarcoidosis and TB can overlap significantly, our observation suggests that certain features such as the presence of extensive necrosis may be highly suggestive of TB than sarcoidosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Muthu V, Gupta N, Dhooria S, Sehgal IS, Bal A, Aggarwal AN, et al. A Prospective, Randomized, Double-Blind Trial Comparing the Diagnostic Yield of 21- and 22-Gauge Aspiration Needles for Performing Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration in Sarcoidosis. Chest. 2016;149(4):1111–3. doi: 10.1016/j.chest.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 2.Gupta D, Agarwal R, Aggarwal AN, Jindal SK. Sarcoidosis and tuberculosis: the same disease with different manifestations or similar manifestations of different disorders. Curr Opinion Pulmonary Med. 2012;18(5):506–16. doi: 10.1097/MCP.0b013e3283560809. [DOI] [PubMed] [Google Scholar]
- 3.Kaur G, Dhamija A, Augustine J, Bakshi P, Verma K. Can cytomorphology of granulomas distinguish sarcoidosis from tuberculosis? Retrospective study of endobronchial ultrasound guided transbronchial needle aspirate of 49 granulomatous lymph nodes. CytoJ. 2013;10:19. doi: 10.4103/1742-6413.119008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Navani N, Molyneaux PL, Breen RA, Connell DW, Jepson A, Nankivell M, et al. Utility of endobronchial ultrasound-guided transbronchial needle aspiration in patients with tuberculous intrathoracic lymphadenopathy: A multicentre study. Thorax. 2011;66:889–93. doi: 10.1136/thoraxjnl-2011-200063. [DOI] [PMC free article] [PubMed] [Google Scholar]


