Abstract
The identification of individual factors modulating clinical recovery after a stroke is fundamental to personalize the therapeutic intervention to enhance the final clinical outcome. In this framework, electrophysiological factors are promising since are more directly related to neuroplasticity, which supports recovery in stroke patients, than neurovascular factors. In this retrospective observational study, we investigated brain neuronal activity assessed via spectral features and Higuchi’s fractal dimension (HFD) of electroencephalographic signals in acute phase (2–10 days from symptom onset, T0) and sub-acute phase (2.5 months, T1) in 24 patients affected by unilateral middle cerebral artery stroke. Longitudinal assessment of the clinical deficits was performed using the National Institutes of Health Stroke Scale (NIHSS), together with the effective recovery calculated as the ratio between difference of NIHSS at T0 and T1 over the NIHSS value at T0. We observed that delta and alpha band electroencephalographic signal power changed between the two phases in both the hemispheres ipsilateral (ILH) and contralateral (CHL) to the lesion. Moreover, at T0, bilateral higher delta band power correlated with worse clinical conditions (Spearman’s rs = 0.460, P = 0.027 for ILH and rs = 0.508, P = 0.013 for CLH), whereas at T1 this occurred only for delta power in ILH (rs = 0.411, P = 0.046) and not for CHL. Inter-hemispheric difference (ILH vs. CLH) of alpha power in patients was lower at T0 than at T1 (P = 0.020). HFD at T0 was lower than at T1 (P = 0.005), and at both phases, ILH HFD was lower than CLH HFD (P = 0.020). These data suggest that inter-hemispheric low band asymmetry and fractal dimension changes from the acute to the sub-acute phase are sensitive to neuroplasticity processes which subtend clinical recovery. The study protocol was approved by the Bioethical Committee of Ospedale San Giovanni Calibita Fatebenefretelli (No. 40/2011) on July 14, 2011.
Keywords: mono-hemispheric stroke, delta band, fractal dimension, inter-hemispheric asymmetries, EEG, plasticity
Chinese Library Classification No. R448; R741
Introduction
Ischemic stroke is a leading cause of death and the primary cause of chronic disability in Western countries, mostly in the elderly (Crichton et al., 2016). Care in the hyper-acute and acute period after a stroke has improved over the last decades, with a remarkable increase of stroke survival rate (http://www.rcplondon.ac.uk/resources/stroke-guidelines). However, the clinical outcome shows a huge inter-individual variability, even with similar symptoms and features of the lesion (site/volume) at onset (Zeiler and Krakauer, 2013). Studies of global neural activity, neural circuitry and brain connectivity following an ischemic lesion in animals and humans represent the basis of our understanding of the biological mechanisms underpinning post-stroke recovery, and are important in orienting the clinical practice and to improve outcome. Indeed, a proper detection of neural markers of the neurological impairment in the acute phase, as well as of prognostic value and recovery abilities can provide information about the selection of therapies, medical and/or rehabilitative, that enhances the individual ability for post-stroke recovery.
In humans, several neuroimaging techniques have been used in the last decades to broaden knowledge of short and long-term changes of neural activity after stroke (for a review see Rossini et al., 2007). Previous evidence strongly supports the notion that stroke patients show an uncoupling of their neuronal activations from their hemodynamics (Rossini et al., 2004), suggesting that electrophysiological features of neural activity are better candidates to describe the functional state of neurons surviving cerebral ischemia after a stroke and to characterize their reaction capability. Electroencephalography (EEG) is a sensitive, non-invasive, low-cost and widely available technique able to detect neuronal functional changes following a brain lesion. Indeed, EEG studies in humans (Nagata et al., 1982; Sainio et al., 1983; Ahmed, 1988; Niedermeyer, 1997; Makela et al., 1998; Murri et al., 1998) reported that slow-frequency activity and interhemispheric asymmetries of delta and alpha activity are signs of a cerebral lesion. We previously demonstrated, by means of magnetoencephalography (MEG) and EEG, that in acute unilateral stroke a higher cortical activity in the delta frequency band (1–4 Hz), together with a lower amplitude of the somatosensory evoked fields in the ipsi-lesional hemisphere, is able to reliably predict most of the variability of the clinical status in the acute phase (Tecchio et al, 2005; Assenza et al., 2009).
In addition to features derived by the oscillatory nature of brain activity and extracted by spectral analysis, recent non-linear methods revealed neuronal dynamics dysfunction following a stroke lesion. Indeed, brain processes are highly non-linear (He, 2011; Buzsaki and Mizuseki, 2014; Roberts et al., 2014; Ramon and Holmes, 2015) and measures of system complexity have been proved to quantify critical aspects of the brain activity (Stam et al., 2005; Rodríguez-Bermúdez and García-Laencina 2015). Complexity has been associated to efficient processing and functional advantages (Garret et al., 2013). In particular, Higuchi’s fractal Dimension (HFD) of EEG at rest was found to be smaller in the first week after a mono-hemispheric stroke (Zappasodi et al., 2014) and this reduction was paired to a worse clinical status. It has been suggested that the HFD decrease in stroke patients describes the loss of complexity subsequent to the global system dysfunction due to the structural damage. This picture is coherent with neuronal activity complexity decrease paired to a reduced repertoire of functional abilities.
The present study aimed to characterize the evolution of electrophysiological features in acute (within 10 days from ischemic attack) and sub-acute (after 2 months) phases of brain activity in unilateral ischemic stroke in the middle cerebral artery (MCA) territory. Moreover, links between the electrophysiological alterations and the clinical status were evidenced, at both acute and sub-acute phases, as well as possible associations between changes in neural activity in sub-acute phase and clinical recovery.
Participants and Methods
Participants
Twenty-four patients (72.0 ± 9.5 years, 9 women and 15 men), admitted to our clinical centers (San Raffaele Hospital, Cassino; Università Campus Biomedico di Roma, Rome; Fatebenefratelli Isola Tiberina Hospital, Rome) from January 2010 to December 2011 were enrolled in this retrospective longitudinal observational study with a control group (Figure 1). The inclusion criteria were: first-ever mono-hemispheric and mono-lesional ischemic stroke in MCA territory; clinical evidence of motor/sensory deficit of the upper limb; neuroradiological diagnosis of MCA ischemia. The exclusion criteria were: a previous stroke revealed by clinical history; neuroradiological evidence of involvement of either hemispheres or brain hemorrhage; dementia or aphasia severe enough to impair patients’ compliance with the procedures; anti-epileptic and anti-psychotic treatments. Patients received a diagnostic/therapeutic approach following the Italian stroke guidelines (SPREAD – Stroke Prevention and Educational Awareness Diffusion. Ictus cerebrale: Linee guida italiane; www.spread.it). None of our patients received thrombolytic therapy. The rehabilitative treatment was organized as follows: in the acute hospitalization in campus Bio-Medico university of Rome, patients were examined by a medical doctor specialist in physical and rehabilitative medicine within 48 hours from the admission to the hospital to start active and passive therapy as soon as possible (but after 24 hour after stroke onset, Bernhardt et al, 2016) if not contraindicated. Once patient was admitted to the rehabilitation institute, all our patients received intensive physical therapy for 3 hours/day 7/7 for 40–45 days. No robotic or neuromodulatory therapies were provided in these patients.
Figure 1.
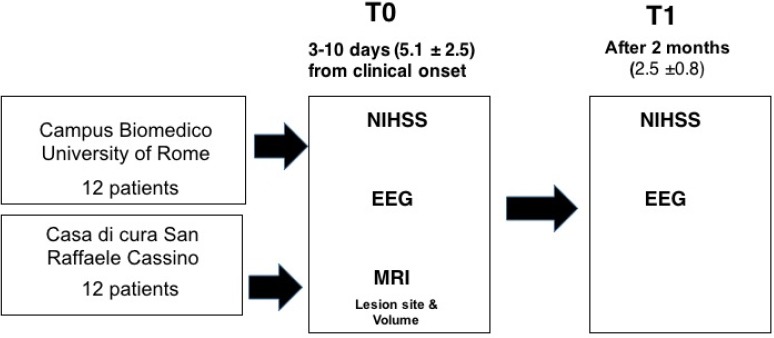
Study flow chart.
NIHSS: National Institutes of Health Stroke Scale; EEG: electroencephalogram; MRI: magnetic resonance imaging.
As a control group, 20 participants (8 females and 12 males) with age comparable to the patients (71.2 ± 6.2 years, P = 0.736) were enrolled from patients’ relatives. All healthy subjects had an unremarkable neurological examination and did not receive any pharmacological treatment at the time of recordings.
The experimental protocol was approved by the Bioethical Committee of Ospedale San Giovanni Calibita Fatebenefretelli (No. 40/2011) on July 14, 2011 (Additional file 1 (374KB, pdf) ), and all participants provided written informed consent (Additional file 2 (276.9KB, pdf) ).
PARERE ETICO ESPRESSO il 14 luglio 2011
PARTE INFORMATIVA dello studio “Promuovere il recupero da ictus: interventi riabilitativi in fase acuta arricchiti individualmente [ProSIA]” (PAZIENTE)
Clinical evaluation
Patients underwent clinical status evaluation by National Health Institute Stroke Scale (NIHSS) between days 2 and 10 after stroke onset (acute phase: T0, mean 5.1 ± 2.5 days from symptoms onset), as well as EEG and magnetic resonance imaging (MRI).
Clinical evaluations by NIHSS and EEG recordings were repeated after 2 months (sub-acute phase: T1, 2.5 ± 0.8 months). The same clinician assessed the NIHSS scores both at T0 and at T1 in each patient. To quantify clinical follow-up, the effective recovery (ER) was then calculated as:
ER = (NIHSS at T0 – NIHSS at T1)/NIHSS at T0 × 100%.
Neuroradiological evaluation
Brain MRI was taken at 1.5 T (MAGNETOM Avanto; Siemens, Erlangen, Germany), using Turbo Spin-Echo (TSE) and Spin-Echo (SE) T1- and T2-weighted sequences. All sequences provided contiguous 5 mm thick slices in sagittal, coronal and axial planes. These images allowed deriving a characterization of the ischemic lesion, which was classified according to lesion site as: ‘subcortical’ (S) when there was no visible cortical involvement and basal ganglia, thalamus, caudate nucleus, nucleus lenticularis or internal capsule were affected (Dromerick and Reding, 1995); ‘cortical’ (CS), if also cortical structures were involved.
EEG recordings and data analysis
Subjects were sitting on a comfortable armchair during relaxed closed-eyes rest. Five minutes of EEG activity was acquired by means of 19 Ag-AgCl electrodes positioned according to the 10-20 International system (Fp2, F4, F8, C4, T4, P4, P8, O2, Fz, Cz, Pz, Fp1, F3, F7, C3, T3, P3, P7, and O1) in fronto-central reference by a Micromed EEG recorder (Micromed, Mogliano Veneto, Italy). Two additional electrode pairs were used to monitor and record electro-oculogram and electrocardiogram. Data were sampled at 256 Hz (analogical filter 0.1–70 Hz).
EEG data were off-line filtered between 1 and 45 Hz (second order forward-backward Butterworth filter) and visually inspected to remove epochs contaminated by movements. To identify and eliminate artefacts (i.e., eye movements, cardiac activity, scalp muscles contraction), we applied a procedure based on Independent Component Analysis (Barbati et al., 2004). Scalp EEG recordings were re-referenced to a standardized reference by the Reference Electrode Standardization Technique (Marzetti et al., 2007). In this way, the reference is far from all possible neural sources and acts like a neutral virtual reference.
The power spectral density was estimated for each EEG channel via the Welch procedure (4-second epoch duration, resulting in a frequency resolution of 0.25 Hz, Hanning windowing, 60% overlap, about 180 artifacts free trials used). For each EEG electrode band power values were obtained as the mean of power spectral density in each frequency band. The investigated frequency bands were: 1–4 Hz (delta), 4.25–7.5 Hz (theta), 8–12.5 Hz (alpha), 13–25 Hz (beta). Spectral features were investigated in the classical frequency bands, instead of being settled on the basis of individual spectral characteristics (Klimesch, 1999), as spectral properties are known to be affected by stroke.
Band power in both the hemispheres ipsilateral (ILH) and contralateral (CHL) to the lesion was calculated as the average of the band power at the electrodes laying over the area covered by the MCA (F4, F8, C4, T4, P4, P8 for right hemisphere and F3, F7, C3, T3, P3, P7 for left hemisphere, Figure 2). Band power values were log-transformed to fit a Gaussian distribution.
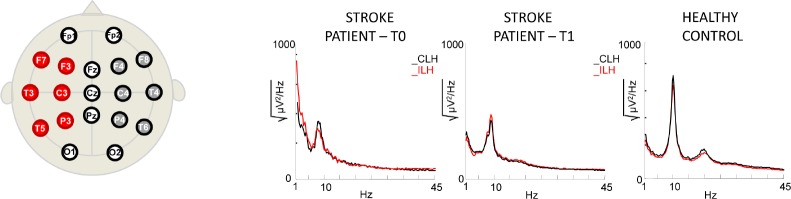
Figure 2.
Electroencephalographic montage and power spectrum densities
Up: Electrode spatial positioning of the international 10–20 system used in this study. Electrodes covering the middle cerebral artery vascular territory used for the analysis are evidenced (in red for the left, in blue for the right hemisphere). Bottom: Examples of power spectrum densities in both hemispheres of one patient (female, 86 years old, lesion with cortical involvement in the left temporal area), in both acute (T0) and sub-acute phase (T1), and a healthy control (male, 73 years old).
The interhemispheric asymmetry (IntAsy) between activities of affected and unaffected hemispheres was obtained for each band power as follows:
IntAsy = (XILH – XCLH) / (XILH + XCLH)
Being X the power in delta, theta, alpha or beta band.
HFD (Higuchi, 1988) was calculated for each EEG channel in time windows of 10 seconds (see Zappasodi et al., 2014, 2015 for details). A global measure of HFD was obtained by averaging HFD values over time and over all EEG channels. Separate values of HFD for the ILH and CLH were also calculated.
Statistical analysis
Statistical analysis was performed using the IBM SPSS Statistics for Windows (version 24.0; Armonk, NY, USA: IBM Corp., Released 2016). The significance level was set to alpha = 0.05. The first aim of the statistical analysis was to check for changes of electrophysiological features at rest in the sub-acute phase with respect to the acute phase of mono-hemispheric stroke. To evaluate possible differences of spectral features between the two phases, a repeated measure analysis of variance (ANOVA) was performed with Band (delta, theta, alpha, and beta), Hemisphere (ILH, CLH) and Time (T0, T1) as within-subject factors. Whenever an interaction Band × Time was found, reduced models were separately applied for each band with Hemisphere and Time as within-subject factors. Greenhouse-Geisser correction has been applied when the sphericity assumption was not valid. Significant main effect of Hemisphere, Time or interaction Time × Hemisphere was followed up by unpaired t-test, to compare ILH and CLH band power of patients with the values of the healthy control group, considered as the reference. For the control group values, we arbitrarily aligned right hemisphere with ILH and left with CLH for half of the subjects, and the contrary for the other half. The opposite matching was also verified in order to exclude the presence of inter-hemispheric asymmetries.
Differences between values of global HFD at T0 and T1 were tested by two-tail paired samples t-test. Independent sample t-tests were also used to evidence difference between HFD values of patients and of healthy controls.
The second aim of the analysis was to evidence relationship between electrophysiological alteration and clinical status, both at T0 and T1, as well as relationship between changes in T1 and recovery. Thus, once differences between the two phases or between patients and healthy controls were assessed, Spearman’s correlation was calculated between spectral features or fractal dimension values and NIHSS scores at T0 or at T1 or ER values. A percentile-based bootstrap, with 5000 replicated samples, was applied to assess the 95% confidence interval of correlation coefficients. Moreover, the patients were split into two groups according to recovery levels (lower than and equal to 75%; higher than 75%) and electrophysiological features compared between the two groups.
Finally, to take into account the difference due to lesion site, spectral values and HFD values of patients with subcortical lesions and patients with cortical lesions were compared with normative values of healthy control group. Since the number of patients in our study was not high enough to allow a finer classification in sub-groups, non-parametric Mann-Whitney U tests were used. Bonferroni correction was applied when needed.
Results
Clinical scores
Stroke was localized in the left hemisphere in 14 patients and in the right hemisphere in 10 patients. Ten patients had a lesion in subcortical areas, while 14 patients had a lesion with cortical involvement. NIHSS score in the acute phase (T0) ranged from 1 to 17 (median: 4; 5–95 percentile: 1–14) and from 0 to 12 at T1 (median: 1.5; 5–95 percentile: 0–8). Differences between NIHSS at T0 and NIHSS at T1 and ER values indicated that 7 patients (29% of patients; 3 with lesion in the right hemisphere, 4 with lesion in the left hemisphere) showed a complete recovery (ER = 100%), 13 patients (54%; 6 with right lesion, 7 with left lesion) showed some clinical recovery at T1, and 4 patients (17%; 1 with right lesion, 3 with left lesion) did not recovered (ER = –25%–0). No differences in NIHSS at T0 and T1, as well as in ER, were found between patients with right and left lesion (Mann-Whitney U test, P > 0.200). No difference in age, NIHSS at T0 and T1 and in ER was found between patients with subcortical or cortical lesion (Mann-Whitney U test, P > 0.200).
Spectral features
Repeated measures ANOVA with Band (delta, theta, alpha, and beta), Hemisphere (ILH, CLH) and Time (T0, T1) as within-subject factors showed a significant Band × Hemisphere interaction effect (F(2.3,52.5) = 3.742, P = 0.025), as well as a significant triple interaction Time × Band × Hemisphere (F(1.6, 38.2) = 3.644, P = 0.043). Reduced models applied on the separate bands based on repeated measures ANOVA Hemisphere (ILH, CLH) and Time (T0, T1) as within-subject factors were applied. Significant results were found only for delta and alpha bands, as we reported in the following. No differences were found for theta and beta bands between hemispheres, times and groups (both controls vs. patients and cortical vs. subcortical lesions).
Delta band
In the delta band, a significant main effect of hemisphere was found (F(1,23) = 4.536, P = 0.044), indicating that in both phases ILH delta power was greater than CLH delta power (Figure 3A). Neither Time main effect nor Time × Hemisphere interaction was present. Comparing delta power of both hemispheres with the values of healthy controls, only ILH delta at T0 was significantly different from delta of healthy controls (unpaired t-test, P = 0.036 for ILH and P = 0.092 for CLH). At T1, no differences between the two groups were observed (unpaired t-test, P = 0.130 for ILH, P = 0.276 for CLH, Figure 3A).
Figure 3.
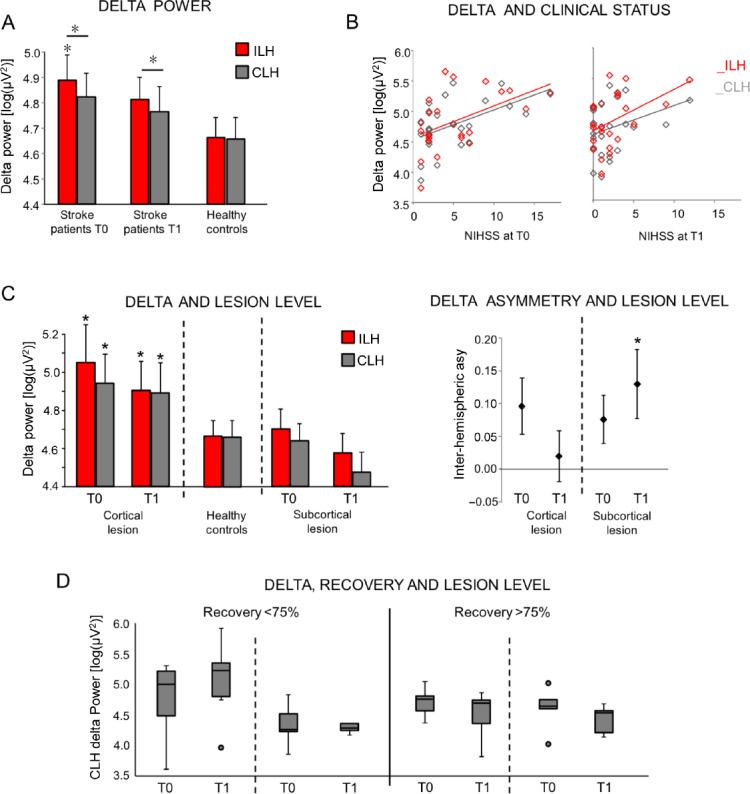
Electroencephalographic delta band power.
(A) Mean (standard error) of band power values in delta band for ILH and CLH in patients in the acute and sub-acute phases. Reference values of controls are also shown. Stars indicate a significant difference in patients with respect to the corresponding value in the control group, as indicated by unpaired t-test (*P < 0.05). Horizontal bars indicate significant difference between ILH and CLH values. (B) Scatterplot of the delta band power in ILH and CLH over NIHSS scores at both acute (T0) and sub-acute phase (T1). Regression lines are displayed. (C) Left: Mean (standard error) of band power values in delta band for ILH and CLH in patients in the acute and sub-acute phases, split in two groups on the basis of the lesion site: lesion with cortical involvement, subcortical lesion. Right: Mean (standard error) of inter-hemispheric asymmetries of delta activity at both phases in both groups of patients. Stars indicate a significant difference in patients with respect to the corresponding value in the control group (*P < 0.05), as assessed by Mann-Whitney U test (Bonferroni corrected). (D) Box-plot (median, 95% confidence interval) of CLH delta power in patients at both phases (T0 and T1), stratified in accordance to effective recovery (< 75% and > 75%) and lesion site (cortical involvement, subcortical lesion). ILH: Ipsilesional hemisphere; CLH: contralesional hemisphere; NIHSS: National Institutes of Health Stroke Scale.
Delta and clinical status
In the acute phase, delta band power of both hemispheres positively correlated with NIHSS scores (for ILH: Spearman’s rs = 0.460, P = 0.027, confidence interval: 0.062, 0.722; for CLH: rs = 0.508, P = 0.013, confidence interval: 0.128, 0.773; Figure 3B left), indicating a worse clinical status paired to an increase of delta power.
In the sub-acute phase, only ILH delta power positively correlated with NIHSS (rs = 0.411, P = 0.046, confidence interval: 0.010, 0.672; Figure 3B). No significant correlations were found between clinical scores and CLH delta power (rs = 0.346, P = 0.098, confidence interval: –0.041, 0.658). No correlation was found between ER and delta power in sub-acute phase (rs = –0.200, P = 0.348 and rs = –0.147, P = 0.493, respectively for ILH and CLH).
Delta: dependence on lesion site (cortical – subcortical)
Both ILH and CLH delta power values at T0 of patients with cortical involvement were higher than healthy control values (Mann-Whitney U test, P < 0.008). No differences between values of healthy controls and subcortical patients were found (Figure 3C, left). No differences between patient groups and healthy controls were found at T1 (Mann-Whitney U test, P > 0.05).
For the delta band inter-hemispheric asymmetries, while no differences depending on the lesion site were observed in the acute phase (Mann-Whitney U test, P > 0.05), at T1 delta activity was more symmetrical in cortical patients (Mann-Whitney U test, P > 0.05) than in subcortical one (Mann-Whitney U test, P < 0.05) (Figure 3C, right).
Delta power and recovery in sub-acute phase depending on lesion site
To investigate whether CLH delta power values at T1 is linked to effective recovery, we split the group of patients in patients with effective recovery lower than 75% (13 patients) and higher than 75% (11 patients). This analysis revealed that CLH delta power at T1 was higher in the group with a lower recovery and cortical lesion (Figure 3D, Mann-Whitney U test between the two groups: P = 0.048 for cortical lesion; P = 0.662 for subcortical lesion).
Alpha band
In the alpha band, a significant interaction Time × Hemisphere was found (F(1,23) = 6.200, P = 0.020), but neither Time nor Hemisphere main effects were present (Figure 4A).
Figure 4.
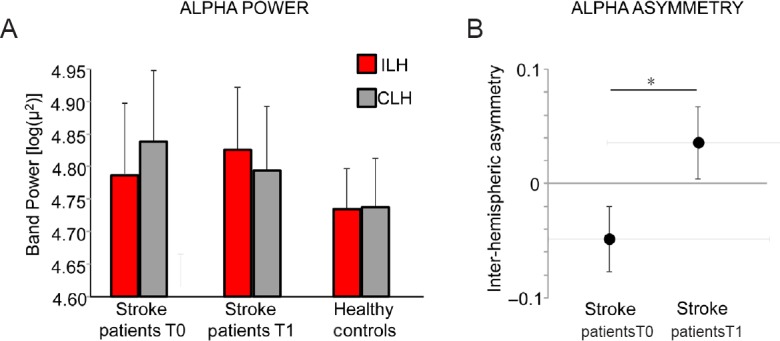
Electroencephalographic alpha band power.
(A) Mean (standard error) of band power values in alpha band for ILH and CLH in patients at both acute and sub-acute phases. Reference values of controls are also shown. (B) Mean (standard error) of inter-hemispheric asymmetries of alpha activity at both phases in both groups of patients. Star indicates significant difference between acute (T0) and sub-acute phase (T1) values, as assessed by two-tailed paired samples t-test (*P < 0.05). ILH: Ipsilesional hemisphere; CLH: contralesional hemisphere.
Indeed, the inter-hemispheric asymmetry in alpha power values in patients (ILH vs. CLH) was lower at T0 than at T1 (paired samples t-test: t(23) = –2.493, P = 0.020), indicating that ILH alpha values were lower than CLH values at T0 with respect to T1 (Figure 4B).
The values of patients’ alpha power were not significantly different from the values of healthy controls in both hemispheres and in both phases (unpaired t-test, P > 0.05).
Alpha and clinical status
No correlation was found between clinical scores and alpha power in both phases (NIHSS and alpha power at T0: rs = 0.001, P = 0.995; rs = 0.126, P = 0.557, respectively for ILH and CLH; NIHSS and alpha power at T1: rs = 0.008, P = 0.969; rs = 0.086, P = 0.691, respectively for ILH and CLH).
Alpha: dependence on lesion site
No difference in alpha activity or asymmetries depending on the lesion site was found (P > 0.05).
Fractal dimension
In both patients and healthy controls, a similar HFD topography on the scalp was observed. HFD values were lower in parieto-occipital and fronto-polar areas and higher in fronto-central and temporal areas (Figure 5A).
Figure 5.
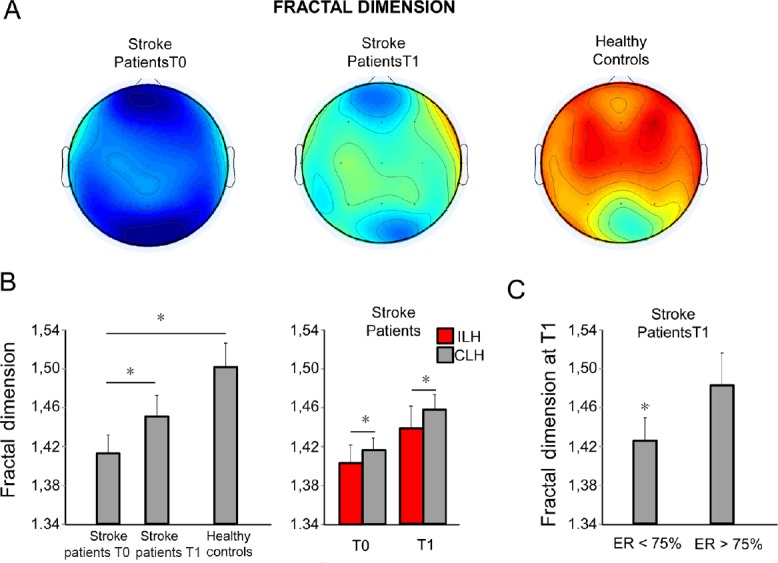
Electroencephalographic fractal dimension
(A) Topographies of mean values of fractal dimension in patients at T0 (acute phase, left) and T1 (sub-acute phase, center) and in healthy age-matched controls (right). Black dots indicate the position of electroencephalographic electrodes in the montage. (B) Left: mean (standard error) of global fractal dimension (average over all sensors) in patients at T0 and T1 and in healthy controls. Right: mean (standard error) of Higuchi’s fractal dimension (HFD) values in ILH and CLH of patients at both T0 and T1. Stars indicate a significant difference between groups, as assessed by two-tailed paired samples t-test (*P < 0.05). (C) In the sub-acute phase, mean and standard deviation of global fractal dimension in patients with ER lower than 75% (left) and patients with ER higher than 75%. Stars indicate a significative difference with respect to values in healthy controls. ILH: Ipsilesional hemisphere; CLH: contralesional hemisphere; ER: effective recovery [(NIHSS at T0 – NIHSS at T1)/NIHSS at T0 × 100%].
In patients, HFD at T0 was lower than at T1 (paired samples t-test: t(23) = –3.093, P = 0.005, Figure 5B, left panel). When comparing the HFD of stroke group with the reference values of the healthy control group, we observed that in the acute phase HFD was lower in patients than in healthy controls (independent samples t-test: t(42) = 2.878, P = 0.006), whereas no difference was observed in the sub-acute phase (independent sample t-test: t(42) = 1.585, P = 0.120). If we consider only the patients with effective recovery lower than 75% (13 patients: 5 with lesion in the right hemisphere, 8 in the left hemisphere), HFD at T1 was significantly lower than the HFD values of healthy control group (1.395 ± 0.077 vs. 1.501 ± 0.109, t(31) = 2.137, P = 0.032, Figure 5C).
Considering the HFD values of the two hemispheres, an ANOVA design was applied with Hemisphere (ILH, CLH) and Time (T0, T1) as within-subject factors. Significant main effects of Time (F(1,22) = 8.566, P = 0.006) and Hemisphere (F(1,22) = 6.311, P = 0.020) were found. The lack of interaction Hemisphere × Time indicated that both at T0 and T1 the HFD values of both hemispheres were different. In particular, ILH HFD was lower than CLH FD (HFD ILH and HFD CLH values: 1.406 ± 0.089 and 1.441 ± 0.098 at T0; 1.416 ± 0.081 and 1.458 ± 0.086 at T1, respectively). Moreover, in both hemispheres, HFD values in the acute phase were lower than those in the sub-acute phase.
ILH and CLH HFD values in patients were significantly lower at T0 than the corresponding values in healthy controls (unpaired t-test: t(42) = 3.337, P = 0.002 for ILH; t(42) = 3.247, P = 0.003 for CLH). In the sub-acute phase, this difference was found only in ILH (t(42) = 2.128, P = 0.039), although it did not survive Bonferroni correction (two hemispheres and two phases resulting in four comparisons), but not in CLH (t(42) = 1.733, P = 0.090). No correlation between ILH and CLH HFD values with clinical scores (NIHSS) was found at both times (P > 0.200 consistently).
Discussion
Data from our cohort of mono-hemispheric stroke patients provided confirmative evidence that normalization of electric neural activity at rest in both the ipsi- and contralesional hemisphere parallels clinical amelioration. Our study did not investigate the modifications occurring at cerebral organization level depending on diverse rehabilitative approaches; we investigated instead – as derived by EEG – the brain activity features associated with the recovery level. They can deepen understanding of recovery process, and provide an adjunctive indication prospectively to focus therapies in sustaining brain adaptive reorganizations.
Delta power as an index of clinical damage
A power increase in low frequency band (1–4 Hz, delta band) was the most evident hallmark of electrophysiological brain activity alteration at rest in stroke patients, clearly associated with the clinical status. Indeed, consistently with previous EEG literatures (Van der Drift and Kok, 1972; Sainio et al., 1983; Ahmed 1988; Jackel and Harner, 1989; Nagata et al., 1992; Niedermeyer 1997; Makela et al., 1998; Murri et al., 1998; Fernandez-Bouzas et al., 2000; Tecchio et al., 2005, 2006a), delta power was higher in ILH that in CLH, in both acute and sub-acute phase. Nevertheless, in our patient cohort, we observed also an increment of delta power in the CLH with respect to healthy control values. Delta activity is believed to be the hallmark of two distinct phenomena, i.e. cortico-thalamocortical network dysfunction and intracortical neuronal activity alteration, as a result of deafferentation (Amzica and Steriade, 1995; Blatow et al., 2003). In animal models, it has been proven that delta activity is cortical in origin, since it is still present after extensive ipsilateral thalamotomy (Steriade and Contreras, 1995) and cannot be recorded in the thalamus of decorticated animals or after cortical necrosis (Timofeev and Steriade, 1996). In humans, ILH delta activity in stroke has been described as a ‘perilesional’ rhythm (Butz et al., 2004; Machado et al., 2004) that increases in correspondence of neural tissue damage, necrosis or both structural or functional deafferentation. Additionally, ILH delta activity correlates with the lesion volume in acute phase (Harmony et al., 1995; Wu et al., 2016), as well as with a worse acute clinical status (Assenza et al., 2009; Wu et al., 2016). Our results are in line with these previous findings, as delta power in the ILH positively correlates with NIHSS scores both in the acute and sub-acute phases. ILH delta activity is a sign of cortical rearrangement accompanying a worse clinical status due to the damage. Thus, in patients, a reduction of ILH low-frequency activity at 2 months towards healthy normative values is a sign of a clinical amelioration. To be noted, a correlation of delta activity with the clinical status has been previously described also at six months from the ischemic attack (Tecchio et al., 2006a, b). However, delta activity, during both the sleep and the wakefulness, is a well-known sign of cortical plastic changes (Tononi and Cirelli, 2012; Assenza and Di Lazzaro, 2015, Giovanni et al., 2017), thus in stroke patients it can also be interpreted as a sign of ongoing cortical rearrangement. Its correlation with a worse clinical status makes difficult to understand to which extent this delta activity is symptomatic of the severity of the lesion and to which extent it marks an attempt to build a new cortical network to overcome the clinical deficits. We are aware that the present study cannot resolve this ambiguity. However, our observation of a high delta activity in the sub-acute phase in patients with either a complete or a partial recovery suggests that a prolonged follow-up could reveal whether subacute chronic delta is a sign that cortical plasticity is still ongoing.
The presence of a delta power increase in patients with respect to healthy controls also in the hemisphere contra-lateral to the lesion suggests an involvement of the CLH in post-stroke recovery. Actually, not only previous EEG and MEG findings (Tecchio et al., 2005, 2007; Zappasodi et al., 2007; Finnigan et al., 2008; Assenza et al., 2013; Van Kaam et al., 2018), but also magnetic stimulation studies (Di Lazzaro et al., 2010) and positron emission tomography (Calautti et al., 2001) demonstrated that the CLH over-activation in the post-stroke phase is detrimental for clinical recovery. Nevertheless, it is still unclear whether this is a compensatory mechanism activated by a severe lesion or an index of functional disconnection. As suggested in Assenza et al. (2013), from an electrophysiological point of view, the two main hypotheses that may explain the presence of an enhanced contra-lesional delta activity are an interhemispheric spreading from the ipsi- to the contralesional hemisphere or a breakdown of interhemispheric communication due to transcallosal diaschisis, i.e., a modification of functionality of a brain area remote from the lesion (Von Monakov, 1914). This modification is possibly mediated by cerebral blood flow and metabolism decrease, or by electrophysiological phenomena (Carrera and Tononi, 2014). Although in subacute stroke patients a decreased regional cerebral blood flow also in the CLH has been documented (Lagreze et al., 1987), to our knowledge no correlation between this reduction and low frequency activity increase has been found (Melamed et al., 1975).
Inter-hemispheric unbalance
Several studies in animal models and humans evidenced the functional role of interhemispheric unbalance in consequence of a brain lesion. In a rat model, interhemispheric connectivity and neurological improvement followed a parallel trend after cerebral ischemia, from acute to chronic stage (van Meer et al., 2010). In humans, both functional MRI and electrophysiological data in acute and chronic stroke patients demonstrated that the balancing is associated with a better clinical and functional picture (Carter et al., 2010; Pellegrino et al., 2012; Graziadio et al., 2013; Baldassarre et al., 2016). In our patient cohort, we found changes in inter-hemispheric asymmetry in the alpha band between T0 and T1. In particular, while alpha was lower in ILH than in CLH in the acute phase, in the sub-acute phase a restoration of ILH vs. CLH alpha activity balance was evidenced. Preservation of alpha activity in the acute phase has been associated to neuronal survival in ischemic regions (Juhász et al., 1997; Leon-Carrion et al., 2009). Moreover, the prognostic value of the ratio between delta and alpha activities has been described, with a better clinical condition associated to an increment of alpha with respect to delta activity (Leon-Carrion et al., 2009; Finnigan et al., 2016; Aminov et al., 2017).
Dependence of the electrophysiological features on lesion site
Recent studies pointed out the need to consider a stratification of patients based on the lesion site when studying inter-hemispheric balance in stroke (Cramer 2010; Di Pino et al., 2014). For example, Fanciullacci et al. (2017) showed that a brain injury from unilateral stroke resulted in a bilateral enhancement of delta activity, and thus in an enhancement of delta power also in the CLH, only in patients with cortical involvement and not in subcortical stroke, in which an ‘asymmetrical’ delta activity was found. This is an interesting hypothesis that cannot be evaluated in the present study because of the limited number of patients that does not allow any stratification. Nevertheless, in our cohort of patients, while we found no differences in inter-hemisperic asymmetry in relation to lesion site in the acute phase, in the sub-acute phase we found a more symmetrical delta in patients with cortical involvement, with respect to pure subcortical patients. This result may suggest a cortical origin of delta activity, in line with previous evidence (Butz et al., 2004; van Wijngaarden et al., 2016). Moreover, enhanced delta in the CLH was found in patients with a poorer clinical recovery, in which brain reorganization processes are possibly still more heavily occurring. van Wijngaarden et al. (2016) recently developed a biologically constrained model to explain the characteristic slowing of alpha peak and the increase of low frequency power in stroke, associated with a cortical lesion. They proposed that thalamic neurons switched from tonic spiking to a pathologic bursting regime in consequence of a de-inactivation of voltage-gated T-type Ca2+-channels. This inactivation derives from a thalamic relay neuron hyperpolarization, secondary to a cortical lesion. Bidirectional divergent connectivity between thalamic nuclei promotes propagation of bursting activity and further entrainment of thalamo-cortical circuits.
Fractal dimension
Our data confirmed previous results about fractal dimension of EEG signals in the acute phase of unilateral stroke (Zappasodi et al., 2014) and add evidence to the idea of the fractal nature of electrophysiological brain signals as a marker of brain complexity (Di Ieva et al., 2014), mirroring the system functionality. Indeed, in our sample the Higuchi FD globally decreased in the acute phase after the stroke as compared with healthy controls values. We can speculate that a loss of local neural activity, with a lesion induced damage in local functionality, reflects into a disruption of global brain processing and thus in a reduced complexity in spatially distributed areas. In other words, HFD discloses the intimate nature of structure-function unity, where an anatomical lesion, even if local and discrete, destroys the whole brain multi-scale self-similar activity. In the sub-acute phase, a general increment of HFD with respect to the acute phase was found and no difference between patients and healthy controls was noticed. Such HFD increment was proportional to the clinical recovery since patients with more than 75% of effective clinical recovery showed higher fractal dimension values. These signs indicate that the recovery of EEG-derived brain activity complexity parallels a restored repertoire of functional abilities.
Limitations
This study has some limitations. First, the number of enrolled patients is relatively low. However, our study has not the ambition to provide a new diagnostic tool for clinical stroke diagnostic and monitoring, rather it aims at strengthening the use of EEG technique in the clinical model of the stroke pathology and recovery. We will devote future studies to confirm our results in a larger independent patient group. Furthermore, wider cohorts with homogeneous lesion sites and volumes, together with an accurate MRI assessment, will be the basis for the deepening the significance of electrophysiological features in stroke and their relationship with clinical status and recovery. Second, we evaluated the clinical status through NIHSS which is the typical scale used to evaluate the clinical status in the acute phase. We are aware that other scales can be more suitable to measure the functional outcome in the period following the acute phase. Nevertheless, since one of our primary aim was to assess electrophysiological changes in relation to the ‘recovery potential’ somehow independently from the clinical status at T0, we used the Effective Recovery, which partly normalizes for the acute phase conditions. The definition of the Effective Recovery index required the use of the same scale for both phases (Tecchio et al., 2006b, 2007; Assenza et al., 2013; Squitti et al., 2018).
Conclusion
The present study offers an EEG longitudinal monitoring of cortical activity across the acute and subacute phases of stroke, describing electrophysiological rest activity changes paralleling the clinical recovery process. We confirmed the sensitivity of EEG signals to brain plasticity in stroke patients and thus we encourage new studies paralleling EEG modifications with clinical assessment to find electrophysiological markers able to identify patients destined to an incomplete recovery. In turn, these electrophysiological markers should lead new clinical trials of standard and enriched rehabilitation (e.g. robotic, neuromodulation) in stroke patients.
Additional file:
Additional file 1 (374KB, pdf) : Ethical approval documentation (in Italian).
Additional file 2 (276.9KB, pdf) : Model consent form (in Italian).
Additional file 3: Open peer review report 1 (75.6KB, pdf) .
Acknowledgments
We would like to thank Fabrizio Emma e Rita Fini for their technical assistance in EEG acquisition, Salvatore Assenza and Federica Assenza for his and her contributions to the enrollment and follow-up of patients.
Footnotes
Conflicts of interest: The authors declare no conflicts of interest.
Financial support: FZ and FT obtained financial support from the Italian Ministry of Health Cod. GR-2008-1138642 “Promoting recovery from Stroke: individually enriched therapeutic intervention in Acute phase”, and PNR-CNR Aging Program. The funding bodies played no role in the study design, in the collection, analysis and interpretation of data, in the writing of the paper, and in the decision to submit the paper for publication.
Institutional review board statement: This study protocol was approved by the Bioethical Committee of Ospedale San Giovanni Calibita Fatebenefretelli (No. 40/2011) on July 14, 2011, and performed in accordance with the Declaration of Helsinki. All participants provided written informed consent.
Declaration of participant consent: The authors certify that they have obtain all appropriate participant consent forms. In the form the participants will give their consent for their images and other clinical information to be reported in the journal. The participants understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Reporting statement: This study followed the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement.
Biostatistics statement: The statistical methods of this study were reviewed by the biostatistician of Campus Bio-Medico of Rome.
Copyright license agreement: The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement: The authors prefer to not share the data of this study.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer reviewer: Lijie Zhai, University of Illinois at Chicago, USA.
Funding: FZ and FT obtained financial support from the Italian Ministry of Health Cod. GR-2008-1138642 “Promoting recovery from Stroke: individually enriched therapeutic intervention in Acute phase”, and PNR-CNR Aging Program.
P-Reviewer: Zhai L; C-Editors: Zhao M, Li CH; T-Editor: Liu XL
References
- 1.Ahmed I. Predictive value of the electroencephalogram in acute hemispheric lesions. Clin Electroencephalogr. 1988;19:205–209. doi: 10.1177/155005948801900406. [DOI] [PubMed] [Google Scholar]
- 2.Aminov A, Rogers JM, Johnstone SJ, Middleton S, Wilson PH. Acute single channel EEG predictors of cognitive function after stroke. PLoS One. 2017;12:e0185841. doi: 10.1371/journal.pone.0185841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amzica F, Steriade M. Disconnection of intracortical synaptic linkages disrupts synchronization of a slow oscillation. J Neurosi. 1995;15:4658–4677. doi: 10.1523/JNEUROSCI.15-06-04658.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Assenza G, Zappasodi F, Squitti R, Altamura C, Ventriglia M, Ercolani M, Quattrocchi CC, Lupoi D, Passarelli F, Vernieri F, Rossini PM, Tecchio F. Neuronal functionality assessed by magnetoencephalography is related to oxidative stress system in acute ischemic stroke. NeuroImage. 2009;44:1267–1273. doi: 10.1016/j.neuroimage.2008.09.049. [DOI] [PubMed] [Google Scholar]
- 5.Assenza G, Zappasodi F, Pasqualetti P, Vernieri F, Tecchio F. A contralesional EEG power increase mediated by interhemispheric disconnection provides negative prognosis in acute stroke. Restor Neurol Neurosci. 2013;31:177–188. doi: 10.3233/RNN-120244. [DOI] [PubMed] [Google Scholar]
- 6.Assenza G, Di Lazzaro V. A useful electroencephalography (EEG) marker of brain plasticity: delta waves. Neural Regen Res. 2015;10:1216–1217. doi: 10.4103/1673-5374.162698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baldassarre A, Ramsey LE, Siegel JS, Shulman GL, Corbetta M. Brain connectivity and neurological disorders after stroke. Curr Opin Neurol. 2016;29:706–713. doi: 10.1097/WCO.0000000000000396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barbati G, Porcaro C, Zappasodi F, Rossini PM, Tecchio F. Optimization of ICA approach for artifact identification and removal in MEG signals. Clin Neurophys. 2004;115:1220–1232. doi: 10.1016/j.clinph.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 9.Bernhardt J, Dewey H, Collier J, Thrift A, Lindley R, Moodie M, Donnan G. A very early rehabilitation trial (AVERT) Int J Stroke. 2006;1:169–171. doi: 10.1111/j.1747-4949.2006.00044.x. [DOI] [PubMed] [Google Scholar]
- 10.Blatow M, Rozov A, Katona I, Hormuzdi SG, Meyer AH, Whittington MA, Caputi A, Monyer H. A novel network of multipolar bursting interneurons generates theta frequency oscillations in neocortex. Neuron. 2003;38:805–817. doi: 10.1016/s0896-6273(03)00300-3. [DOI] [PubMed] [Google Scholar]
- 11.Butz M, Gross J, Timmermann L, Moll M, Freund HJ, Witte OW, Schnitzler A. Perilesional pathological oscillatory activity in the magnetoencephalogram of patients with cortical brain lesions. Neurosci Lett. 2004;355:93–96. doi: 10.1016/j.neulet.2003.10.065. [DOI] [PubMed] [Google Scholar]
- 12.Buzsaki G, Mizuseki K. The log-dynamic brain: how skewed distributions affect network operations. Nat Rev Neurosci. 2014;15:264–278. doi: 10.1038/nrn3687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Calautti C, Leroy F, Guincestre JY, Marié RM, Baron JC. Sequential activation brain mapping after subcortical stroke: changes in hemispheric balance and recovery. Neuroreport. 2001;12:3883–3886. doi: 10.1097/00001756-200112210-00005. [DOI] [PubMed] [Google Scholar]
- 14.Carrera E, Tononi G. Diaschisis: past, present, future. Brain. 2014;137:2408–2422. doi: 10.1093/brain/awu101. [DOI] [PubMed] [Google Scholar]
- 15.Carter AR, Astafiev SV, Lang CE, Connor LT, Rengachary J, Strube MJ, Pope DL, Shulman GL, Corbetta M. Resting interhemispheric functional magnetic resonance imaging connectivity predicts performance after stroke. Ann Neurol. 2010;67:365–375. doi: 10.1002/ana.21905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cramer SC. Stratifying patients with stroke in trials that target brain repair. Stroke. 2010;41(10 Suppl):S114–116. doi: 10.1161/STROKEAHA.110.595165. [DOI] [PubMed] [Google Scholar]
- 17.Crichton SL, Bray BD, McKevitt C, Rudd AG, Wolfe CDA. Patient outcomes up to 15 years after stroke: survival, disability, quality of life, cognition and mental health. J Neurol Neurosurg Psychiatry. 2016;87:1091–1098. doi: 10.1136/jnnp-2016-313361. [DOI] [PubMed] [Google Scholar]
- 18.Di Ieva A, Grizzi F, Jelinek H, Pellionisz AJ, Losa GA. Fractals in the Neurosciences, Part I: General Principles and Basic Neurosciences. Neuroscientist. 2014;20:403–417. doi: 10.1177/1073858413513927. [DOI] [PubMed] [Google Scholar]
- 19.Di Lazzaro V, Profice P, Pilato F, Capone F, Ranieri F, Pasqualetti P, Colosimo C, Pravatà E, Cianfoni A, Dileone M. Motor cortex plasticity predicts recovery in acute stroke. Cereb Cortex. 2010;20:1523–1528. doi: 10.1093/cercor/bhp216. [DOI] [PubMed] [Google Scholar]
- 20.Di Pino G, Pellegrino G, Assenza G, Capone F, Ferreri F, Formica D, Ranieri F, Tombini M, Ziemann U, Rothwell JC, Di Lazzaro V. Modulation of brain plasticity in stroke: a novel model for neurorehabilitation. Nat Rev Neurol. 2014;10:597–608. doi: 10.1038/nrneurol.2014.162. [DOI] [PubMed] [Google Scholar]
- 21.Dromerick AW, Reding MJ. Functional outcome for patients with hemiparesis, hemihyposthesia and hemianopsia. Stroke. 1995;11:2023–2026. doi: 10.1161/01.str.26.11.2023. [DOI] [PubMed] [Google Scholar]
- 22.Fanciullacci C, Bertolucci F, Lamola G, Panarese A, Artoni F, Micera S, Rossi B, Chisari C. Delta power is higher and more symmetrical in ischemic stroke patients with cortical involvement. Front Hum Neurosci. 2017;11:385. doi: 10.3389/fnhum.2017.00385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fernandez-Bouzas A, Harmony T, Fernandez T, Silva-Pereyra J, Valdes P, Bosch J, Aubert E, Casián G, Otero Ojeda G, Ricardo J, Hernández-Ballesteros A, Santiago E. Sources of abnormal EEG activity in brain infarctions. Clin Electroencephalogr. 2000;31:165–169. doi: 10.1177/155005940003100403. [DOI] [PubMed] [Google Scholar]
- 24.Finnigan S, Wong A, Read S. Defining abnormal slow EEG activity in acute ischaemic stroke: Delta/alpha ratio as an optimal QEEG index. Clin Neurophysiol. 2016;127:1452–1459. doi: 10.1016/j.clinph.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 25.Finnigan SP, Rose SE, Chalk JB. Contralateral hemisphere delta EEG in acute stroke precedes worsening of symptoms and death. Clin Neurophysiol. 2008;119:1690–1694. doi: 10.1016/j.clinph.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 26.Garrett DD, Samanez-Larkin GR, MacDonald SW, Lindenberger U, McIntosh AR, Grady CL. Moment-to-moment brain signal variability: A next frontier in human brain mapping? Neurosci Biobehav Rev. 2013;37:610–624. doi: 10.1016/j.neubiorev.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Giovanni A, Capone F, di Biase L, Ferreri F, Florio L, Guerra A, Marano M, Paolucci M, Ranieri F, Salomone G, Tombini M, Thut G, Di Lazzaro V. Oscillatory activities in neurological disorders of elderly: biomarkers to target for neuromodulation. Front Aging Neurosci. 2018;9:189. doi: 10.3389/fnagi.2017.00189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Graziadio S, Tomasevic L, Assenza G, Tecchio F, Eyre JA. The myth of the ‘unaffected’ side after unilateral stroke: Is reorganisation of the non-infarcted corticospinal system to re-establish balance the price for recovery? Exp Neurol. 2013;238:168–175. doi: 10.1016/j.expneurol.2012.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harmony T, Fernández-Bouzas A, Marosi E, Fernández T, Valdés P, Bosch J, Riera J, Jackel RA, Harner RN. Computed EEG topography in acute stroke. Neurophysiol Clin. 1989;19:185–197. doi: 10.1016/s0987-7053(89)80036-x. [DOI] [PubMed] [Google Scholar]
- 30.He BJ. Scale-free properties of the functional magnetic resonance imaging signal during rest and task. J Neurosci. 2011;31:13786–13795. doi: 10.1523/JNEUROSCI.2111-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higuchi T. Approach to an irregular time series on the basis of the fractal theory. Physica D. 1988;31:277–283. [Google Scholar]
- 32.Jackel RA, Harner RN. Computed EEG topography in caute stroke. Neurophysiol Clin. 1989;19:185–197. doi: 10.1016/s0987-7053(89)80036-x. [DOI] [PubMed] [Google Scholar]
- 33.Juhász C, Kamondi A, Szirmai I. Spectral EEG analysis following hemispheric stroke: evidences of transhemispheric diaschisis. Acta Neurol Scand. 1997;96:397–400. doi: 10.1111/j.1600-0404.1997.tb00305.x. [DOI] [PubMed] [Google Scholar]
- 34.Lagreze HL, Levine RL, Pedula KL, Nickles RJ, Sunderland JS, Rowe BR. Contralateral flow reduction in unilateral stroke: evidence for transhemispheric diaschisis. Stroke. 1987;18:882–886. doi: 10.1161/01.str.18.5.882. [DOI] [PubMed] [Google Scholar]
- 35.Leon-Carrion J, Martin-Rodriguez JF, Damas-Lopez J, Barroso y Martin JM, Dominguez-Morales MR. Delta-alpha ratio correlates with level of recovery after neurorehabilitation in patients with acquired brain injury. Clin Neurophysiol. 2009;120:1039–1045. doi: 10.1016/j.clinph.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 36.Machado C, Cuspineda E, Valdés P, Virues T, Llopis F, Bosch J, Aubert E, Hernández E, Pando A, Alvarez MA, Barroso E, Galán L, Avila Y. Assessing acute middle cerebral artery ischemic stroke by quantitative electric tomography. Clin EEG Neurosci. 2004;35:116–124. doi: 10.1177/155005940403500303. [DOI] [PubMed] [Google Scholar]
- 37.Makela JP, Salmelin R, Kotila M, Salonen O, Laaksonen R, Hokkanen L, Hari R. Modification of neuromagnetic cortical signals by thalamic infarctions. Electroencephalogr Clin Neurophysiol. 1998;106:433–443. doi: 10.1016/s0013-4694(98)00005-4. [DOI] [PubMed] [Google Scholar]
- 38.Marzetti L, Nolte G, Perrucci MG, Romani GL, Del Gratta C. The use of standardized infinity reference in EEG coherency studies. Neuroimage. 2007;15:48–63. doi: 10.1016/j.neuroimage.2007.02.034. [DOI] [PubMed] [Google Scholar]
- 39.Melamed E, Lavy S, Portnoy Z, Sadan S, Carmon A. Correlation between regional cerebral blood flow and EEG frequency in the contralateral hemisphere in acute cerebral infarction. J Neurol Sci. 1975;26:21–27. doi: 10.1016/0022-510x(75)90110-0. [DOI] [PubMed] [Google Scholar]
- 40.Murri L, Gori S, Massetani R, Bonanni E, Marcella F, Milani S. Evaluation of acute ischemic stroke using quantitative EEG: a comparison with conventional EEG and CT scan. Neurophysiol Clin. 1998;28:249–257. doi: 10.1016/S0987-7053(98)80115-9. [DOI] [PubMed] [Google Scholar]
- 41.Nagata K, Mizukami M, Araki G, Kawase T, Hirano M. Topographic electroencephalographic study of cerebral infarction using computed mapping of the EEG. J Cereb Blood Flow Metab. 1982;2:79–88. doi: 10.1038/jcbfm.1982.9. [DOI] [PubMed] [Google Scholar]
- 42.National Institute of Health, National Institute of Neurological Disorders and Stroke. Stroke Scale. [Accessed December 2, 2018]. https://www.ninds.nih.gov/sites/default/files/NIH_Stroke_Scale_Booklet.pdf .
- 43.Niedermeyer E. Cerebrovascular disorders and EEG. In: Electroencephalography: Basic Principles, Clinical Applications and Related Fields. In: Niedermeyer E, Lopes Da Silva F, editors. 4th ed. Oxford, UK: Oxford University Press; 1997. pp. 320–321. [Google Scholar]
- 44.Pellegrino G, Tomasevic L, Tombini M, Assenza G, Bravi M, Sterzi S, Giacobbe V, Zollo L, Guglielmelli E, Cavallo G, Vernieri F, Tecchio F. Inter-hemispheric coupling changes associate with motor improvements after robotic stroke rehabilitation. Restor Neurol Neurosci. 2012;30:497–510. doi: 10.3233/RNN-2012-120227. [DOI] [PubMed] [Google Scholar]
- 45.Ramon C, Holmes MD. Spatiotemporal phase clusters and phase synchronization patterns derived from high density EEG and ECoG recordings. Curr Opin Neurobiol. 2015;31:127–132. doi: 10.1016/j.conb.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 46.Roberts J, Iyer K, Finnigan S, Vanhatalo S, Breakspear M. Scale-free bursting in human cortex following hypoxia at birth. J Neurosci. 2014;34:6557–6572. doi: 10.1523/JNEUROSCI.4701-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rodríguez-Bermúdez G, García-Laencina P. Analysis of EEG signals using nonlinear dynamics and chaos: a review. Appl Math Inf Sci. 2015;9:2309–2321. [Google Scholar]
- 48.Rossini PM, Altamura C, Ferretti A, Vernieri F, Zappasodi F, Caulo M, Pizzella V, Del Gratta C, Romani GL, Tecchio F. Does cerebrovascular disease affect the coupling between neuronal activity and local haemodynamics? Brain. 2004;127:99–110. doi: 10.1093/brain/awh012. [DOI] [PubMed] [Google Scholar]
- 49.Rossini PM, Altamura C, Ferreri F, Melgari JM, Tecchio F, Tombini M, Pasqualetti P, Vernieri F. Neuroimaging experimental studies on brain plasticity in recovery from stroke. Eura Medicophys. 2007;43:241–254. [PubMed] [Google Scholar]
- 50.Sainio K, Stenberg D, Keskimaki I, Muuronen A, Kaste M. Visual and spectral EEG analysis in the evaluation of the outcome in patients with ischemic brain infarction. Electroencephalogr Clin Neurophysiol. 1983;56:117–124. doi: 10.1016/0013-4694(83)90066-4. [DOI] [PubMed] [Google Scholar]
- 51.Squitti R, Siotto M, Assenza G, Giannantoni NM, Rongioletti M, Zappasodi F, Tecchio F. Prognostic value of serum copper for post-stroke clinical recovery: a pilot study. Front Neurol. 2018;9:333. doi: 10.3389/fneur.2018.00333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stam CJ. Nonlinear dynamical analysis of EEG and MEG: review of an emerging field. Clin Neurophysiol. 2005;116:2266–2301. doi: 10.1016/j.clinph.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 53.Steriade M, Contreras D. Spike-wave complexes and fast components of cortically generated seizures. I. Role played by neocortex and thalamus. J Neurophysiol. 1998;80:1439–1455. doi: 10.1152/jn.1998.80.3.1439. [DOI] [PubMed] [Google Scholar]
- 54.Tecchio F, Zappasodi F, Pasqualetti P, Tombini M, Salustri C, Oliviero A, Vittorio P, Vernieri F, Rossini PM. Rhythmic brain activity at rest from rolandic areas in acute mono-hemispheric stroke: A magnetoencephalographic study. Neuroimage. 2005;28:72–83. doi: 10.1016/j.neuroimage.2005.05.051. [DOI] [PubMed] [Google Scholar]
- 55.Tecchio F, Zappasodi F, Tombini M, Oliviero A, Pasqualetti P, Vernieri F, Ercolani M, Pizzella V, Rossini PM. Brain plasticity in recovery from stroke: an MEG assessment. Neuroimage. 2006a;32:1326–1334. doi: 10.1016/j.neuroimage.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 56.Tecchio F, Zappasodi F, Pasqualetti P, Tombini M, Caulo M, Ercolani M, Rossini PM. Long-term effects of stroke on neuronal rest activity in rolandic cortical areas. J Neurosci Res. 2006b;83:1077–1087. doi: 10.1002/jnr.20796. [DOI] [PubMed] [Google Scholar]
- 57.Tecchio F, Pasqualetti P, Zappasodi F, Tombini M, Lupoi D, Vernieri F, Rossini PM. Outcome prediction in acute monohemispheric stroke via magnetoencephalography. J Neurol. 2007;254:296–305. doi: 10.1007/s00415-006-0355-0. [DOI] [PubMed] [Google Scholar]
- 58.Timofeev I, Steriade M. Low-frequency rhythms in the thalamus of intact-cortex and decorticated cats. J Neurophysiol. 1996;76:4152–4168. doi: 10.1152/jn.1996.76.6.4152. [DOI] [PubMed] [Google Scholar]
- 59.Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron. 2014;81:12–34. doi: 10.1016/j.neuron.2013.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Van der Drift JHA, Kok NKD. The EEG in cerebrovascular disorders in relations to pathology. In: Remond A, editor. Handbook of Electroencephalography and Clinical Neuropysiology. Amsterdam, Netherlands: Elsevier; 1972. pp. 12–30. 30, 47-64. [Google Scholar]
- 61.Van Kaam RC, van Putten MJAM, Vermeer SE, Hofmeijer J. Contralesional brain activity in acute ischemic stroke. Cerebrovasc Dis. 2018;45:85–92. doi: 10.1159/000486535. [DOI] [PubMed] [Google Scholar]
- 62.van Meer MP, van der Marel K, Wang K, Wang K, Otte WM, El Bouazati S, Roeling TA, Viergever MA, Berkelbach van der Sprenkel JW, Dijkhuizen RM. Recovery of sensorimotor function after experimental stroke correlates with restoration of resting-state interhemispheric functional connectivity. J Neurosci. 2010;30:3964–3972. doi: 10.1523/JNEUROSCI.5709-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.van Wijngaarden JB, Zucca R, Finnigan S, Verschure PF. The impact of cortical lesions on thalamo-cortical network dynamics after acute ischaemic stroke: a combined experimental and theoretical study. PLoS Comput Biol. 2016;12:e1005048. doi: 10.1371/journal.pcbi.1005048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.von Monakov C. Die Lokalisation im Grosshirn und der Abbau der Funktion durch kortikale Herde. JAMA LXIII:797. 1914 [Google Scholar]
- 65.Wu J, Srinivasan R, Burke Quinlan E, Solodkin A, Small SL, Cramer SC. Utility of EEG measures of brain function in patients with acute stroke. J Neurophysiol. 2016;115:2399–2405. doi: 10.1152/jn.00978.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zappasodi F, Tombini M, Milazzo D, Rossini PM, Tecchio F. Delta dipole density and strength in acute monohemispheric stroke. Neurosci Lett. 2007;416:310–314. doi: 10.1016/j.neulet.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 67.Zappasodi F, Olejarczyk E, Marzetti L, Assenza G, Pizzella V, Tecchio F. Fractal dimension of EEG activity senses neuronal impairment in acute stroke. PLoS One. 2014;9:e100199. doi: 10.1371/journal.pone.0100199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zappasodi F, Marzetti L, Olejarczyk E, Tecchio F, Pizzella V. Age-related changes in electroencephalographic signal complexity. PLoS One. 2015;10:e0141995. doi: 10.1371/journal.pone.0141995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zeiler SR, Krakauer JW. The interaction between training and plasticity in the poststroke brain. Curr Opin Neurol. 2013;26:609–616. doi: 10.1097/WCO.0000000000000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PARERE ETICO ESPRESSO il 14 luglio 2011
PARTE INFORMATIVA dello studio “Promuovere il recupero da ictus: interventi riabilitativi in fase acuta arricchiti individualmente [ProSIA]” (PAZIENTE)