Abstract
Background and Purpose
Two conversion scales between the Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MoCA) have been validated for Korean patients with Parkinson's disease. The aim of the present study was to validate these conversion scales for all patients with cognitive impairments regardless of dementia subtype.
Methods
Medical records of 323 subjects who completed both MMSE and MoCA on the same day were retrospectively reviewed. Mean, median, and root mean squared error (RMSE) of the difference between true and equivalent MMSE scores were calculated. Intraclass correlation coefficients (ICCs) between true and equivalent MMSE scores were also calculated. The validity of MoCA-MMSE conversion scales was evaluated according to educational level (low educated: ≤6 years; high educated: ≥7 years) and subtypes of cognitive impairment.
Results
The difference between true and equivalent MMSE scores had a median value of 0, a mean value of 0.19 according to the van Steenoven scale, a mean value of 0.57 according to the Lawton scale, RMSE value of 2.2 according to the van Steenoven scale, and RMSE value of 0.42 according to the Lawton scale. Additionally, ICCs between true and equivalent MMSE scores were 0.92 and 0.90 on van Steenovan and Lawton conversion scales, respectively. These results were maintained in subgroup analyses.
Conclusions
Findings of the present study suggest that both van Steenovan and Lawton MoCA-MMSE conversion scales are applicable to transforming MoCA scores into MMSE scores in patients with cognitive impairments regardless of dementia subtype or educational level.
Keywords: Mini Mental State Examination, Montreal Cognitive Assessment, Cognitive Impairments, Dementia
INTRODUCTION
As dementia is becoming a major health issue worldwide, it has been increasingly important to develop and validate effective tools for assessing cognitive function in aging populations. Although several types of imaging technology and a variety of biomarkers have recently emerged, brief cognitive screening tests remain the most important component of a dementia diagnosis. The most widely used cognitive screening instrument is the Mini-Mental State Examination (MMSE) which has been very well validated by previous studies.1,2,3,4 However, MMSE is under copyright restrictions.5,6 In addition, it is unsuitable for detecting mild cognitive impairment (MCI) in highly educated people.7 As a result, the Montreal Cognitive Assessment (MoCA)8 has been increasingly used to diagnose dementia, especially Parkinson's disease (PD) dementia.9,10 This tool was developed to screen for MCI including expanded assessments of executive and visuospatial functions.11
Transitioning MMSE score into MoCA score can be complicated because MoCA is generally more difficult than MMSE.12 Scores of these two measures have never been regarded as equivalent. Thus, a reliable conversion algorithm between these screening tests needs to be developed. Over the last few years, several studies have been performed to establish a MoCA-MMSE conversion scale.4,13,14,15 Two MoCA-MMSE conversion scales developed by van Steenoven et al.15 and Lawton et al.14 have reasonable validity. Recently, it has been shown that both of these MoCA-MMSE conversion scales are useful for transforming MoCA scores into converted MMSE scores in Korean patients with PD.16 However, patients with other subtypes of dementia were not assessed. Thus, the objective of the present study was to validate these 2 conversion scales for PD patients as well as patients with a wide variety of dementia subtypes.
METHODS
Patients
Medical records of patients who visited our hospital from October 2017 to September 2018 due to cognitive complaints were retrospectively reviewed. We included all patients who completed the Korean version of the MMSE (K-MMSE) and the Korean version of the MoCA (K-MoCA) on the same day. Because the purpose of this study was to validate conversion scores for all patients, not merely those with PD, the present sample encompassed a wide range of cognitive disorders, including Alzheimer's disease (AD), vascular dementia (VD), MCI, and other dementia such as Parkinson related or frontotemporal lobe dementia. This study was approved by the Institutional Review Board of the Bundang Jesaeng General Hospital. Patient consent was obtained.
Neuropsychological assessments
MMSE and MoCA are simple and multidomain cognitive screening tools with scores ranging from 0 to 30. The MMSE includes items assessing time and place orientation (10 points), memorization and immediate recall (6 points), attention and concentration (5 points), oral and written language ability (8 points), and visuospatial function (1 point). The MoCA includes items assessing visuospatial and executive function (5 points), naming (3 points), memory (5 points), attention (6 points), abstraction (2 points), language (3 points), and orientation (6 points). In the present study, the K-MoCA was adjusted by adding 1 point to scores of patients with an education level ≤6 years.
Statistical analyses
First, the correlation between MMSE score and MoCA score was analyzed by Pearson correlation coefficient. To convert MoCA scores to MMSE scores, the same equipercentile method described by van Steenoven et al.15 and Lawton et al.14 (Table 1) was used. This method matches scores on MMSE and MoCA tests according to percentile ranks following a long-linear smoothing of distribution. We calculated the mean, standard deviation, median, interquartile range (IQR), and root mean squared error (RMSE) based on the difference between real and equivalent MMSE scores. Smaller mean, median, and RMSE values were indicative of a more accurate MoCA-MMSE conversion. Additionally, intraclass correlation coefficient (ICC) and confidence interval (CI) between real and equivalent MMSE scores were evaluated.
Table 1. Conversion from MoCA to MMSE score by van Steenoven et al.15 and Lawton et al.14 .
| Adjusted K-MoCA score | Equivalent MMSE score | Equivalent MMSE score |
|---|---|---|
| 1 | 6 | 1 |
| 2 | 9 | 2 |
| 3 | 11 | 4 |
| 4 | 12 | 10 |
| 5 | 13 | 13 |
| 6 | 14 | 14 |
| 7 | 15 | 15 |
| 8 | 15 | 16 |
| 9 | 16 | 17 |
| 10 | 17 | 18 |
| 11 | 18 | 18 |
| 12 | 18 | 19 |
| 13 | 19 | 20 |
| 14 | 20 | 20 |
| 15 | 21 | 21 |
| 16 | 22 | 22 |
| 17 | 22 | 22 |
| 18 | 23 | 23 |
| 19 | 24 | 24 |
| 20 | 25 | 24 |
| 21 | 26 | 25 |
| 22 | 26 | 26 |
| 23 | 27 | 26 |
| 24 | 28 | 27 |
| 25 | 28 | 28 |
| 26 | 29 | 28 |
| 27 | 29 | 29 |
| 28 | 30 | 29 |
| 29 | 30 | 30 |
| 30 | 30 | 30 |
MoCA scores were adjusted by adding 1 point in patients with 6 or fewer years of education.
MoCA: Montreal Cognitive Assessment, MMSE: Mini-Mental State Examination, K-MoCA: Korean version of the Montreal Cognitive Assessment.
RESULTS
Demographic and clinical characteristics
The present study included 323 patients (199 females, 124 males) with a mean age of 72.91±1.35 years and mean MMSE and MoCA scores of 21.92±5.92 and 15.75±7.05, respectively. These participants were divided into two groups based on educational level; low educated (≤6 years, n=153, mean age: 76.89±7.65 years) and high educated (≥7 years, n=170, mean age: 69.26±13.29 years). Mean scores on K-MMSE and K-MoCA in the low educated group were 19.12±5.43 and 11.81±5.82, respectively, whereas those in the high educated group were 24.5±5.15 and 19.35±6.01, respectively. Based on subtypes of cognitive impairments, about half of patients had MCI (49.2%), with more MCI patients in the high educated group (65.9%) than those in the low educated group (30.7%). On the contrary, both AD and VD were more prevalent in the low educated group than in the high educated group (47.1% vs. 24.1% and 19.0% vs. 7.1%, respectively). The number of patients with AD was 113 (35.0%) and that of patients with VD was 41 (12.7%). Detailed demographic characteristics of each group are presented in Table 2.
Table 2. Demographics and clinical characteristics of study subjects.
| Characteristics | Low educated (≤6 yr, n=153) | High educated (≥7 yr, n=170) | Total patients (n=323) | |
|---|---|---|---|---|
| Age (yr) | 76.89±7.65 | 69.26±13.29 | 72.91±11.35 | |
| Sex (M:F) | 38:115 | 86:84 | 124:199 | |
| Education years | 3.53±2.54 | 12.19±2.81 | 8.04±5.07 | |
| K-MMSE | 19.12±5.43 | 24.5±5.15 | 21.92±5.92 | |
| K-MoCA | 11.81±5.82 | 19.35±6.01 | 15.75±7.05 | |
| BDI score | 6.88±4.49 | 5.49±4.52 | 6.16±4.55 | |
| Subtype | ||||
| AD | 72 (47.1) | 41 (24.1) | 113 (35.0) | |
| VD | 29 (19.0) | 12 (7.1) | 41 (12.7) | |
| Other dementia | 5 (3.3) | 5 (3.0) | 10 (3.1) | |
| MCI | 47 (30.7) | 112 (65.9) | 159 (49.2) | |
Data are presented as means±standard deviations or number (%).
K-MMSE: Korean version of the Mini-Mental Status Examination, K-MoCA: Korean version of the Montreal Cognitive Assessment, BDI: Beck Depression Inventory, AD: Alzheimer's disease, VD: vascular dementia, MCI: mild cognitive impairment.
Validation of the MoCA-MMSE conversion scale
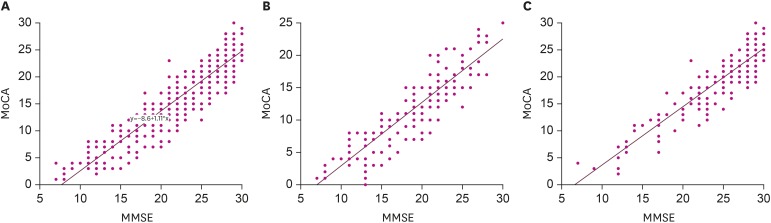
MoCA scores were highly and positively correlated with MMSE scores in all patients (r=0.922; p<0.001). This trend maintained in both high educated group (r=0.910; p<0.001) and low educated group (r=0.897; p<0.001) (Fig. 1). Table 3 shows validation results of MoCA-MMSE conversions. Using the van Steenoven conversion scale, the mean difference between real and equivalent MMSE scores was 0.19 and the median difference was 0 (IQR: −1, 2). Similarly, using the Lawton conversion scale, the mean of difference was 0.57 and the median difference was 0 (IQR: −1, 2). In subgroup analysis according to education level, using the Lawton conversion scale, mean differences for high educated group and low educated group were 0.26 and 0.84, respectively, and median values were 0 (IQR: −2, 2) and 1 (IQR: −1, 2), respectively. In terms of subgroups of cognitive impairment, the mean difference was 0.49 in AD, 0.39 in VD, and 0.47 in MCI using the van Steenoven conversion scale. Median differences were 0 (IQR: −2, 1), −1 (IQR: −2, 1.5), 1 (IQR: 0, 2), respectively. Using the Lawton conversion scale, mean differences, median differences, and RMSEs were very similar to results using the Steenoven conversion scale. ICCs between true and equivalent MMSE scores were 0.92 (95% CI, 0.90–0.93) using the van Steenonven conversion scale and 0.9 (95% CI, 0.88–0.92) using the Lawton conversion scale. In sub-analysis based on educational level, the van Steenoven conversion scale had an ICC of 0.89 (95% CI, 0.85–0.92) for the low educated group and an ICC of 0.91 (95% CI, 0.88–0.93) for the high educated group. Similarly, the Lawton conversion scale had an ICC of 0.87 (95% CI, 0.82–0.90) for the low educated group and an ICC of 0.89 (95% CI, 0.85–0.92) for the high educated group. In terms of cognitive impairment subtypes, the van Steenoven conversion scale had an ICC of 0.85 (95% CI, 0.79–0.89) for AD, 0.82 (95% CI, 0.88–0.93) for VD, and 0.86 (95% CI, 0.81–0.90) for MCI. Similarly, the Lawton conversion scale had an ICC of 0.80 (95% CI, 0.72–0.86) for AD, 0.80 (95% CI, 0.67–0.89) for VD, and 0.77 (95% CI, 0.70–0.83) for MCI.
Fig. 1. Scatterplots of MMSE and MoCA scores in all patients (A), low educated group (B), and high educated group (C).
MMSE: Mini-Mental State Examination, MoCA: Montreal Cognitive Assessment.
Table 3. Validation of MoCA-MMSE conversion.
| Difference between MMSE and equivalent MMSE | By van Steenoven et al.15 | By Lawton et al.14 | |
|---|---|---|---|
| Total (n=323) | |||
| Mean (SD) | 0.19 (2.19) | 0.57 (2.56) | |
| Median (IQR) | 0 (−1, 2) | 0 (−1, 2) | |
| RMSE | 2.2 | 2.62 | |
| Low educated (≤6 yr, n=153) | |||
| Mean (SD) | 0.06 (2.32) | 0.26 (2.78) | |
| Median (IQR) | 0 (−2, 1) | 0 (−2, 2) | |
| RMSE | 2.31 | 2.79 | |
| High educated (≥7 yr, n=170) | |||
| Mean (SD) | 0.40 (2.06) | 0.84 (2.30) | |
| Median (IQR) | 0 (−1, 2) | 1 (−1, 2) | |
| RMSE | 2.09 | 2.45 | |
| AD (n=113) | |||
| Mean (SD) | 0.49 (2.22) | 0.22 (2.94) | |
| Median (IQR) | 0 (−2, 1) | 0 (−2, 1) | |
| RMSE | 2.27 | 2.51 | |
| VD (n=41) | |||
| Mean (SD) | 0.39 (2.44) | 0.31 (3.17) | |
| Median (IQR) | −1 (−2, 1.5) | 0 (−2, 3) | |
| RMSE | 2.43 | 3.15 | |
| MCI (n=159) | |||
| Mean (SD) | 0.47 (1.8) | 0.54 (1.64) | |
| Median (IQR) | 1 (0, 2) | 1 (0, 2) | |
| RMSE | 2.04 | 2.15 | |
MoCA: Montreal Cognitive Assessment, MMSE: Mini-Mental State Examination, SD: standard deviation, IQR: interquartile range, RMSE: root mean squared error, MCI: mild cognitive impairment.
DISCUSSION
The present study retrospectively evaluated data to validate MoCA-MMSE conversion scales developed by van Steenoven et al.15 and Lawton et al.14 for all patients with cognitive impairments. Mean and median differences between real and equivalent MMSE scores were close to 0 for both conversion scales. Both scales had good correlations between true and equivalent MMSE scores. Thus, van Steenoven and Lawton conversion scales both exhibited good validity for transformation of MoCA scores into equivalent MMSE scores for all dementia patients regardless of subtype of cognitive impairment.
The MMSE is a tool most widely used to evaluate multiple cognitive domains for identifying cognitive dysfunction. However, the accuracy of the MMSE has been questioned due to its poor sensitivity in terms of identifying mild cognitive dysfunction in highly educated patients. In addition, it does not reflect decreasing levels of attention, executive function, or visuospatial function. Several studies have reported that MoCA can assess all cognitive domains and that it is sensitive to cognitive abnormalities in patients with MCI or dementia.9 In particular, PD patients with dementia exhibit impaired attention and executive function. As a result, the MoCA has been officially adopted as a screening instrument for cognitive impairments in PD.1 Due to its high sensitivity to MCI, lack of copyright issues, and free accessibility, MoCA is a more useful tool than MMSE for screening cognitive dysfunction not only in PD patients, but also in patients with other subtypes of dementia.1
Direct conversion of MoCA score to MMSE score would be helpful given the large quantity of clinical data collected using MMSE. MoCA-MMSE conversion scales for AD and MCI were investigated from 2013 to 2015.4,12,17 MoCA-MMSE conversion scales for PD were later established by van Steenoven et al.15 and Lawton et al.14 MMSE-equivalent MoCA scores in these two studies were similar, regardless of subtype of dementia. It has been reported that a score of 26 on the MMSE, the cut-off value for MCI, is equivalent to a score of 22 on the MoCA for PD-related dementia14,15 and a score of 20 on the MoCA for AD-related dementia.4,12 A MMSE score of 20 is approximately equivalent to a MoCA score of 13–15 and a MMSE score of 10 is approximately equivalent to a MoCA score of 3–4 in all papers.4,12,14,15 A recent study by Kim et al.16 has validated these conversion tables in Korean patients with PD and suggested that Both van Steenoven and Lawton MoCA-MMSE conversion tables are useful for transforming MoCA scores into converted MMSE scores regardless of educational level. However, it is virtually impossible for primary clinicians to classify dementia subtype at a patient's first visit. Therefore, MoCA-MMSE conversion scales for all subtypes of dementia are necessary. MoCA-MMSE conversions scales previously validated in Korean patients with PD might be also applicable to patients with other subtypes of dementia. Thus, the present study evaluated conversion scales developed by van Steenoven et al.15 and Lawton et al.14 previously validated in Korean patients.
Previously published data from MMSE and MoCA were obtained from well-educated subjects because educational level might influence scores on both screening tests. Some studies have shown that MMSE and MoCA can be useful for screening cognitive impairment in less educated patients.18 In study on Koreans by Kim et al.,16 approximately 30% of patients had 6 or fewer years of education. Although conversion scales have satisfactory validity in highly educated and less educated patients, it is also necessary to confirm validity in patients with low levels of education. In our study, approximately half of patients had 6 or fewer years of education. This group had higher mean age, greater proportion of females, and lower MMSE and MoCA scores than expected. However, mean, median, and RMSE values for the group with low level of education were similar to those for all patients. In addition, ICCs between true and equivalent MMSE score for the low educated group were reasonably similar to those for the high educated group. These results showed that MoCA-MMSE conversion scales exhibited adequate validity even in low educated patients. Thus, both conversion scales were useful regardless of educational level.
This study has several limitations that should be considered. The sample was collected from a single center with relatively small (n=323) subjects. In addition, this study had a retrospective design. Moreover, patients with lower MoCA scores required more validation because previous studies of conversion scales were performed with narrow distributions of MoCA scores. Finally, subjects in this study were heterogenous because all patients with cognitive impairments were enrolled regardless of dementia subtype. Some studies have reported that the MMSE-MoCA relationship differs somewhat according to dementia subtype.12 Therefore, large studies including all dementia subtypes and detailed analyses according to dementia subtype are needed in the future. However, the aim of the present study was to document the validity of MoCA-MMSE conversion scales in all patients with cognitive impairments drawn from a primary clinic center. Therefore, this study might suggest that MoCA-MMSE conversion scales could be widely used in all patients regardless of education level or subtype of cognitive impairment.
In conclusion, this study showed that both van Steenoven et al.15 and Lawton et al.14 conversion scales were useful for transforming MoCA scores into equivalent MMSE scores for patients with PD as well as for those with cognitive impairments. Moreover, these scales can be applied to individuals with low levels of education. These results will be helpful for applying MoCA scores to those with general dementia.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Jeong E, Yu HJ.
- Data curation: Jung YI, Lee H, Seo J.
- Formal analysis: Lee H, Seo J, Yu HJ.
- Investigation: Jung YI, Hong JY.
- Methodology: Hong JY.
- Supervision: Jeong E.
- Writing - original draft: Sunwoo MK.
- Writing - review & editing: Sunwoo MK.
References
- 1.Freitas S, Simões MR, Alves L, Santana I. Montreal Cognitive Assessment: validation study for mild cognitive impairment and Alzheimer disease. Alzheimer Dis Assoc Disord. 2013;27:37–43. doi: 10.1097/WAD.0b013e3182420bfe. [DOI] [PubMed] [Google Scholar]
- 2.Arevalo-Rodriguez I, Smailagic N, Roqué I Figuls M, Ciapponi A, Sanchez-Perez E, Giannakou A, et al. Mini-Mental State Examination (MMSE) for the detection of Alzheimer's disease and other dementias in people with mild cognitive impairment (MCI) Cochrane Database Syst Rev. 2015:CD010783. doi: 10.1002/14651858.CD010783.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 4.Roalf DR, Moberg PJ, Xie SX, Wolk DA, Moelter ST, Arnold SE. Comparative accuracies of two common screening instruments for classification of Alzheimer's disease, mild cognitive impairment, and healthy aging. Alzheimers Dement. 2013;9:529–537. doi: 10.1016/j.jalz.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newman JC. Copyright and bedside cognitive testing: why we need alternatives to the Mini-Mental State Examination. JAMA Intern Med. 2015;175:1459–1460. doi: 10.1001/jamainternmed.2015.2159. [DOI] [PubMed] [Google Scholar]
- 6.Newman JC, Feldman R. Copyright and open access at the bedside. N Engl J Med. 2011;365:2447–2449. doi: 10.1056/NEJMp1110652. [DOI] [PubMed] [Google Scholar]
- 7.Tombaugh TN, McIntyre NJ. The Mini-Mental State Examination: a comprehensive review. J Am Geriatr Soc. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 8.Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 9.Dalrymple-Alford JC, MacAskill MR, Nakas CT, Livingston L, Graham C, Crucian GP, et al. The MoCA: well-suited screen for cognitive impairment in Parkinson disease. Neurology. 2010;75:1717–1725. doi: 10.1212/WNL.0b013e3181fc29c9. [DOI] [PubMed] [Google Scholar]
- 10.Hoops S, Nazem S, Siderowf AD, Duda JE, Xie SX, Stern MB, et al. Validity of the MoCA and MMSE in the detection of MCI and dementia in Parkinson disease. Neurology. 2009;73:1738–1745. doi: 10.1212/WNL.0b013e3181c34b47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Julayanont P, Tangwongchai S, Hemrungrojn S, Tunvirachaisakul C, Phanthumchinda K, Hongsawat J, et al. The Montreal Cognitive Assessment-basic: a screening tool for mild cognitive impairment in illiterate and low-educated elderly adults. J Am Geriatr Soc. 2015;63:2550–2554. doi: 10.1111/jgs.13820. [DOI] [PubMed] [Google Scholar]
- 12.Bergeron D, Flynn K, Verret L, Poulin S, Bouchard RW, Bocti C, et al. Multicenter validation of an MMSE-MoCA conversion table. J Am Geriatr Soc. 2017;65:1067–1072. doi: 10.1111/jgs.14779. [DOI] [PubMed] [Google Scholar]
- 13.Falkowski JA, Hynan LS, Krishnan K, Carter K, Lacritz L, Weiner M, et al. Conversion of MoCA to MMSE scores. Alzheimers Dement (Amst) 2015;1:125. doi: 10.1016/j.dadm.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lawton M, Kasten M, May MT, Mollenhauer B, Schaumburg M, Liepelt-Scarfone I, et al. Validation of conversion between Mini-Mental State Examination and Montreal Cognitive Assessment. Mov Disord. 2016;31:593–596. doi: 10.1002/mds.26498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Steenoven I, Aarsland D, Hurtig H, Chen-Plotkin A, Duda JE, Rick J, et al. Conversion between Mini-Mental State Examination, Montreal Cognitive Assessment, and dementia rating scale-2 scores in Parkinson's disease. Mov Disord. 2014;29:1809–1815. doi: 10.1002/mds.26062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim R, Kim HJ, Kim A, Jang MH, Kim HJ, Jeon B. Validation of the Conversion between the Mini-Mental State Examination and Montreal Cognitive assessment in Korean patients with Parkinson's Disease. J Mov Disord. 2018;11:30–34. doi: 10.14802/jmd.17038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trzepacz PT, Hochstetler H, Wang S, Walker B, Saykin AJ Alzheimer's Disease Neuroimaging Initiative. Relationship between the Montreal Cognitive Assessment and Mini-Mental State Examination for assessment of mild cognitive impairment in older adults. BMC Geriatr. 2015;15:107. doi: 10.1186/s12877-015-0103-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim JI, Sunwoo MK, Sohn YH, Lee PH, Hong JY. The MMSE and MoCA for screening cognitive impairment in less educated patients with Parkinson's disease. J Mov Disord. 2016;9:152–159. doi: 10.14802/jmd.16020. [DOI] [PMC free article] [PubMed] [Google Scholar]