Abstract
Restoration of neutral mechanical alignment of the lower limb is an important factor in the treatment of unicompartmental arthrosis. Traditionally, medial opening wedge high tibial osteotomy has been widely performed to correct varus malalignment with unicompartmental arthrosis. However, an ideal indication for the high tibial osteotomy is the knee with metaphyseal tibial varus malalignment. The basic principle of corrective osteotomy is performing an osteotomy at the center of the deformity to prevent abnormal joint line obliquity. If pathologic distal femoral varus deformity is the cause of genu varum, the osteotomy should be performed in the distal femur. Reports of medial opening wedge distal femoral osteotomy (DFO) to correct varus malalignment are rare. We present a case of this very rare and challenging condition in a 47-year-old male, which was successfully treated by medial opening wedge DFO.
Keywords: Deformity, Varus, Osteotomy, Distal femoral, Medial opening
Restoration of neutral mechanical alignment of the lower limb is an important factor in the treatment of unicompartmental arthrosis. In particular, varus knee alignment is the most common pathologic condition in patients with medial compartmental knee osteoarthritis. As a surgical method to correct varus malalignment, medial opening wedge high tibial osteotomy has been widely performed because it is relatively easy to perform and causes less side effects than lateral closed wedge high tibial osteotomy with good mid-term clinical and radiological outcomes1). The ideal candidate for medial opening wedge high tibial osteotomy is a relatively young (less than 60 years old) and active patient with metaphyseal tibial varus malalignment and medial unicompartmental arthrosis2).
If genu varum is caused by distal femoral pathologic malalignment, distal femoral osteotomy (DFO) could be considered as a treatment option to correct the deformity and restore the mechanical axis. Candidates for DFO have been usually patients with genu valgum and concomitant unicompartmental lateral arthrosis although similar satisfactory outcomes have been reported in genu varum patients after lateral opening wedge or medial closed wedge DFO in a mid-term follow-up3). Medial closed wedge DFO is technically demanding, whereas the union period of the osteotomy site is shorter than opening wedge DFO and the risk of hinge fracture is relatively low. The lateral open wedge technique is relatively easy to perform in spite of disadvantages such as the need for bone grafting to enhance bony union of the opening gap and the risk of hinge fracture which may result in collapse of the osteotomy site3).
However, reports of medial opening wedge DFO to correct varus malalignment are rare. Here, we report a case of this very rare and challenging condition in a 47-year-old male, which was successfully treated by medial opening wedge DFO.
Case Report
A 47-year-old male patient complained of shortening of right leg and varus deformity. He also had medial side knee pain. He fell down from a chin-up bar in 198, and he was told that a linear fracture occurred in the distal femur at another hospital. Although he could not remember the exact treatment method, he denied any previous history of surgery around the knee joint.
On physical examination, varus thrust gait was observed. Medial joint line tenderness was obvious. The range of motion in the affected knee ranged from 0° to 130°. A standing whole limb scanogram showed pelvic tilting due to limb shortening of the right leg. The length of the femur from the highest point of the femoral head to the lowest point of the medial femoral condyle was measured to be 435 mm in the right and 455 mm in the left. The tibial length was 347 mm on both sides. The whole limb length from the top of the femoral head to the center of the tibial plafond was measured to be 781 mm in the right and 799 mm in the left.
The hip-knee-ankle (HKA) angle formed between the mechanical axis of the femur and tibia was measured to be varus 15° in the right and varus 5° in the left. The anatomical femorotibial angle (aFTA) was 190° in the right and 177° in the left. The anatomical lateral distal femoral angle (aLDFA) was 98° in the right and 82° in the left. The mechanical lateral distal femoral angle (mLDFA) formed between the femoral mechanical axis and the knee joint line of the distal femur was 101° in the right and 91° in the left. The mechanical medial proximal tibial angle (mMPTA) formed between the tibial mechanical axis and the knee joint line of the proximal tibia was 87° in both side (Fig. 1). The mMPTAs in both side were within normal limits, implicating that the proximal tibia was not the major cause of deformity in the right. On the other hand, based on increased aLDFA and mLDFA, distal femoral metaphysis was thought to be the center of the angulation.
Fig. 1.
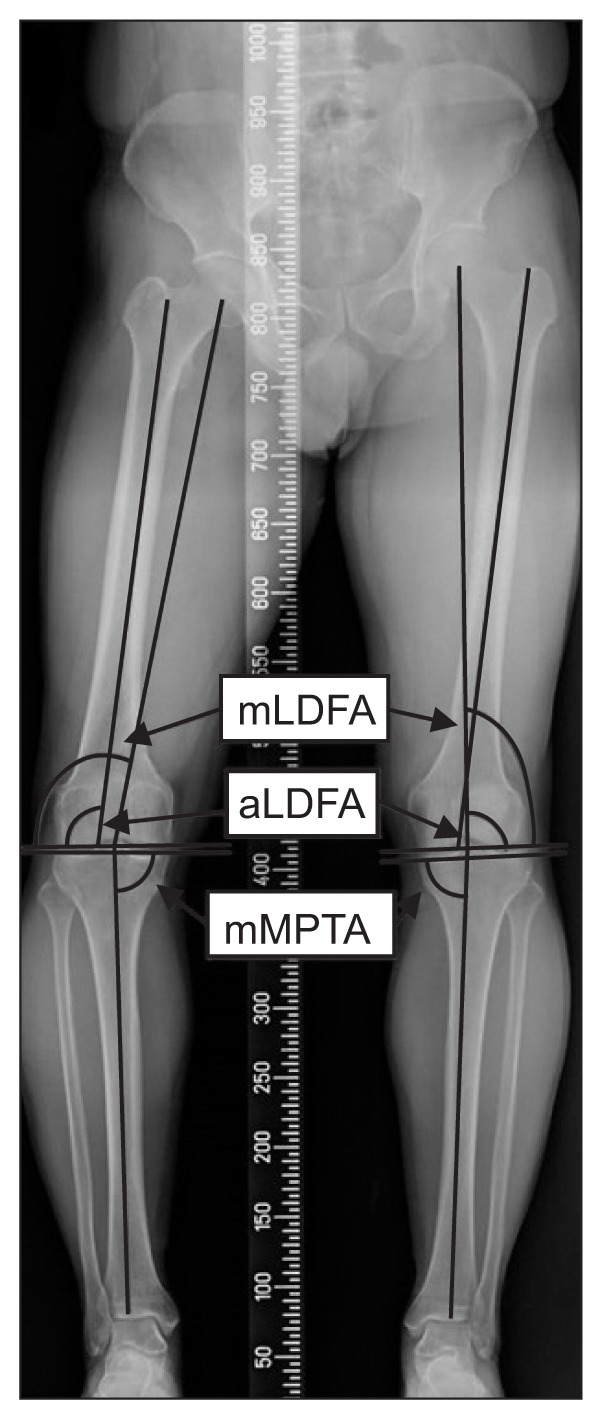
Preoperative whole limb standing scanogram. The anatomical lateral distal femoral angle (aLDFA) is 98° in the right leg and 82° in the left leg. The mechanical lateral distal femoral angle (mLDFA) is 101° in the right leg and 91° in the left leg. The mechanical medial proximal tibial angle (mMPTA) is 87° in both sides.
Standing anteroposterior knee X-ray showed Kellgren-Lawrence (KL) grade II arthrosis in the medial compartment of the right knee. The magnetic resonance imaging (MRI) scan showed that more than 50% of the thickness of the cartilage in the medial femoral condyle was lost (1.5 cm in the longest diameter), which was considered to be grade 2b according to the modified Noyes classification (Fig. 2)4).
Fig. 2.
(A) A 1.5 cm sized Noyes class IIB chondral lesion of the medial femoral condyle was found in a proton density sagittal and coronal magnetic resonance images (arrow). Kellgren-Lawrence grade II arthrosis in the medial compartment was found in the standing knee anteroposterior view (B) and 45° posteroanterior flexion view (C).
The final diagnosis was genu varum and limb shortening caused by an old distal femoral physeal injury with secondary medial osteoarthritis. The primary treatment goals were restoration of the limb alignment to unload the medial compartment with arthrosis and correction of leg length discrepancy.
Preoperative planning of the corrective osteotomy was made according to the method described by Dugdale et al.5). The estimated correction angle was formed by the line drawn from the center of the femoral head to cross the center of the width of the tibial plateau from medial to lateral (50% point) and the line drawn from the center of the talus to the center of the mediolateral width of the tibial plateau (50% point).
1. Operation Procedure and Outcome Assessment
The patient was operated in supine position under tourniquet control. First, arthroscopy was performed. A high anterolateral portal was made just lateral to the patellar tendon-bone junction for viewing portal. A 2×2 cm Outerbridge grade II chondral defect was revealed on the medial femoral condyle (Fig. 3). The unstable cartilage rim was trimmed using a shaver. Cartilage of the lateral femoral condyle, lateral meniscus, and anterior and posterior cruciate ligaments seemed to be relatively preserved.
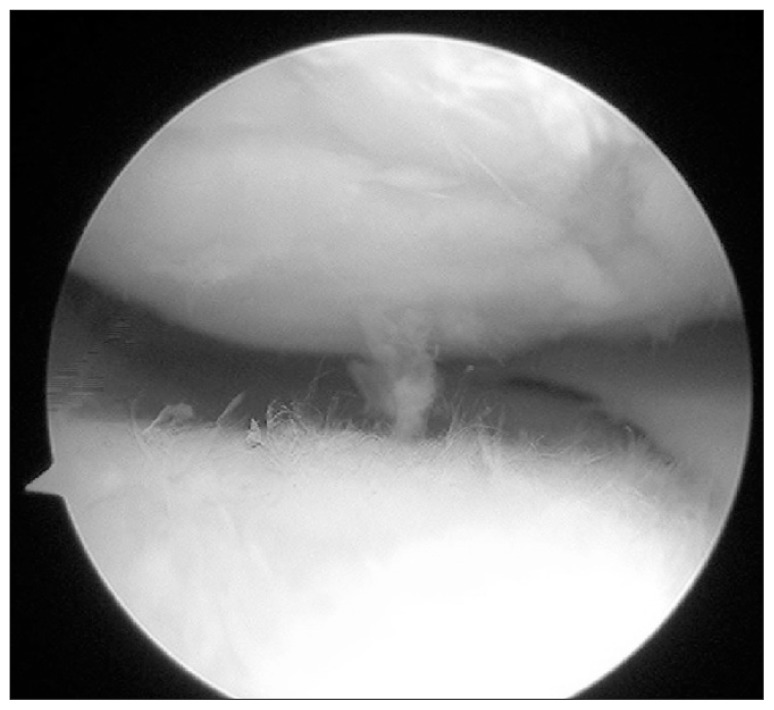
Fig. 3.
Arthroscopic view showing a 2×2 cm Outerbridge grade II chondral defect in the medial femoral condyle.
Then, a 20 cm longitudinal skin incision was made from the medial femoral epicondyle extending proximally. The exposed vastus medialis muscle was retracted anteriorly with a Hohmann retractor. The distal femur was identified and the locking plate (TomoFix; Synthes, Oberdorf, Switzerland) was placed for defining the desired osteotomy cut. The biplane osteotomy site was marked with an electrocautery device. Two anterior and posterior parallel 2.0-mm Kirschner wires (K-wires) were inserted obliquely from the previously marked osteotomy site to just above the lateral epicondyle under fluoroscopic guidance. A biplane osteotomy was performed with an oscillating saw blade leaving the lateral cortex. The osteotomy site was gently widened using osteotomy chisels and then a 15 mm opening gap was maintained using a bone spreader (Fig. 4A). The correction of the lower limb alignment was confirmed by the line of the electrocautery device under fluoroscopy. Two tricortical wedge-shaped bone blocks from the ipsilateral iliac crest were harvested and filled the osteotomy gap (Fig. 4B and C). Finally, the locking plate was applied and fixated.
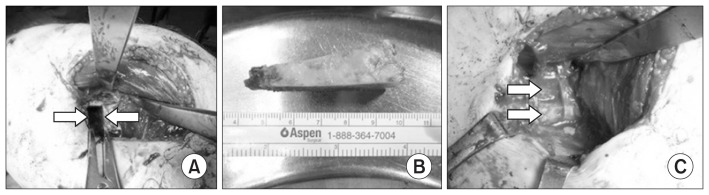
Fig. 4.
(A) An osteotomy gap that was maintained by a bone spreader (arrows). (B) A wedge-shaped tricortico-cancellous bone block that was harvested from the ipsilateral iliac crest. (C) Two tricortical blocks filled the osteotomy gap (arrows).
The operated leg was immobilized in a long leg splint for the first 2 weeks after the surgery. Thereafter, the knee was placed in an immobilizer for another 6 weeks. Continuous passive motion exercises were initiated at 1 week postoperatively and the range of motion was increased as tolerated. Partial weight bearing with bilateral crutches was started at postoperative 4 weeks. Partial weight bearing ambulation was maintained for postoperative 8 weeks. Weight bearing was progressively increased based on the patient’s symptom and radiological findings of the callus formation thereafter. Crutch weaning was started at 10 weeks postoperatively. Quadriceps and hamstring strengthening exercises were recommended for postoperative 8 weeks according to the patient’s symptoms. Closed kinetic chain exercises including lunge and squatting were permitted as tolerated thereafter. Light jogging was permitted at 6 months postoperatively.
The appropriate bone union was obtained 6 months postoperatively (Fig. 5). The range of knee motion measured at postoperative 2 years was from 0° to 145°. Cosmesis of the affected lower limb was also improved (Fig. 6). The International Knee Documentation Committee (IKDC) subjective knee score was improved from C to B. The Lysholm knee score was also improved from 62 to 88. The HKA angle was measured to be varus 2°. The aFTA was measured to be 179°. The aLDFA and mLDFA were measured to be 89° and 92°, respectively. The length of the femur was measured to be 450 mm in the right, which was 5 mm shorter than the left (Fig. 7).
Fig. 5.
Postoperative 6-month follow-up X-rays: anteroposterior view (A) and lateral view (B).
Fig. 6.
(A) Nearly full range of motion was obtained in the operated knee. (B) The appearance of the limb was also improved.
Fig. 7.
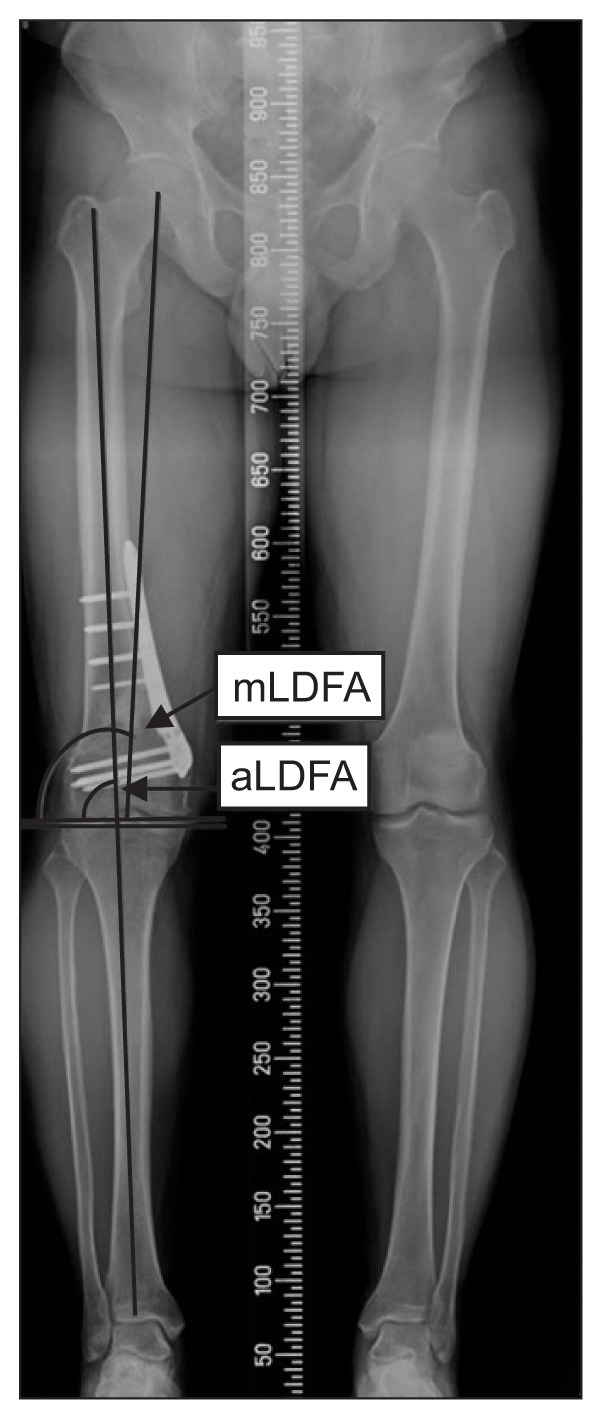
Postoperative 2-year follow-up X-rays. The anatomical lateral distal femoral angle (aLDFA) and mechanical lateral distal femoral angle (mLDFA) were measured to be 89° and 92°, respectively. The length of the femur was measured to be 450 mm in the right leg, which was 5 mm shorter than the left leg.
Discussion
Traditionally, varus malalignment has been treated by an osteotomy on the proximal tibia. However, the basic principle of corrective osteotomy is performing an osteotomy at the center of the deformity. If the osteotomy is performed at the tibia in the patient with a distal femoral varus deformity, the tibial osteotomy can be the cause of excessive knee joint line obliquity, resulting in non-uniformly distributed load transfer on the articular surface3).
In our patient, the mMPTA was 87° in both sides, which was within the normal limit, indicating that there was no metaphyseal tibia vara in the affected side. On the other hand, both aLDFA and mLDFA increased in the affected side compared to the opposite side where the parameters were relatively within the normal limit. This indicates that the varus malalignment in the patient was caused by distal femoral varus deformity. Furthermore, we sought possibility of rotational malalignment in the lower extremity by use of the hip and knee computed tomography to evaluate anteversion of the hip; it is difficult to determine the appropriate rotational alignment based on coronal and sagittal X-rays. In addition, several studies have revealed that rotational malalignment, which is more than 15°, may have negative effects on the cartilage, knee function, and gait6); the rotational difference in our patient was 5°, and it was considered to be within the acceptable range.
The varus deformity of the femur can be treated by lateral closed wedge osteotomy or medial opening wedge osteotomy of the distal femur. Among these two techniques, medial opening wedge osteotomy can obtain both correction of the varus deformity and limb lengthening.
The ideal postoperative lower limb alignment after valgization has yet to be clearly established; this is because the proposed mechanical axis crossing the tibial plateau at 62.5% is mainly based on clinical experience. Hence the postoperative alignment needs to be individualized according to the degree of cartilage injury in the medial compartment. In the case of patients with KL grade I and II osteoarthritis and focal cartilage defect, correction to neutral or slight valgus would be considered appropriate; in the case of advanced medical compartment osteoarthritis (KL grade III and IV), more correction would be needed based on previous reports7,8). Furthermore, a considerable amount of correction may potentially have a negative effect on the clinical outcomes by poor cosmesis and progression of arthrosis in the lateral compartment and delayed or nonunion of a large opening gap. We therefore aimed to correct the deformity to neutral alignment9). The postoperative lower limb alignment was measured to be 2° of varus, which seems to be slightly undercorrected. The patient showed improvement in pain and function of the affected knee.
As a part of the surgical planning of the opening wedge osteotomy, the potential side effects such as loss of correction and delayed or nonunion should be taken into consideration. To prevent these potential complications, maintaining the osteotomy gap provided by adequate stability within the osteotomy gap may be needed10). We used two tricortical bone blocks harvested from the iliac crest to promote mechanical stability and bone healing. The harvested tricortical bone block was shaped as a wedge to fit the osteotomy gap10). The cortical part of the bone block was expected to provide solid medial support in the osteotomy gap.
Preservation of the lateral cortex as a hinge is also an important factor for maintaining the stability of the osteotomy site. Violation of the lateral cortex could lead to micromotion of the osteotomy site, resulting in loss of correction and delayed union or nonunion. To prevent lateral cortical breakage, the depth of the saw blade cut was adjusted to be 10 mm shorter than the whole length of the desired osteotomy depth. The length of the K-wire was measured and used to calculate the length of the desired osteotomy cut.
A satisfactory result without donor site morbidity and delayed union or nonunion was obtained in our patient. Therefore, medial opening wedge DFO could be a reasonable treatment option for femoral varus deformity with limb shortening.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Schuster P, Geβlein M, Schlumberger M, Mayer P, Mayr R, Oremek D, Frank S, Schulz-Jahrsdörfer M, Richter J. Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and varus malalignment. Am J Sports Med. 2018;46:1362–70. doi: 10.1177/0363546518758016. [DOI] [PubMed] [Google Scholar]
- 2.Dettoni F, Bonasia DE, Castoldi F, Bruzzone M, Blonna D, Rossi R. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: a review of the literature. Iowa Orthop J. 2010;30:131–40. [PMC free article] [PubMed] [Google Scholar]
- 3.Kim YC, Yang JH, Kim HJ, Tawonsawatruk T, Chang YS, Lee JS, Bhandare NN, Kim KS, Delgado GDG, Nha KW. Distal femoral varus osteotomy for valgus arthritis of the knees: systematic review of open versus closed wedge osteotomy. Knee Surg Relat Res. 2018;30:3–16. doi: 10.5792/ksrr.16.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kijowski R, Blankenbaker DG, Davis KW, Shinki K, Kaplan LD, De Smet AA. Comparison of 1.5- and 3.0-T MR imaging for evaluating the articular cartilage of the knee joint. Radiology. 2009;250:839–48. doi: 10.1148/radiol.2503080822. [DOI] [PubMed] [Google Scholar]
- 5.Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;(274):248–64. [PubMed] [Google Scholar]
- 6.Gugenheim JJ, Probe RA, Brinker MR. The effects of femoral shaft malrotation on lower extremity anatomy. J Orthop Trauma. 2004;18:658–64. doi: 10.1097/00005131-200411000-00002. [DOI] [PubMed] [Google Scholar]
- 7.McNamara I, Birmingham TB, Fowler PJ, Giffin JR. High tibial osteotomy: evolution of research and clinical applications: a Canadian experience. Knee Surg Sports Traumatol Arthrosc. 2013;21:23–31. doi: 10.1007/s00167-012-2218-9. [DOI] [PubMed] [Google Scholar]
- 8.Gardiner A, Gutierrez Sevilla GR, Steiner ME, Richmond JC. Osteotomies about the knee for tibiofemoral malalignment in the athletic patient. Am J Sports Med. 2010;38:1038–47. doi: 10.1177/0363546509335193. [DOI] [PubMed] [Google Scholar]
- 9.Feucht MJ, Minzlaff P, Saier T, Cotic M, Südkamp NP, Niemeyer P, Imhoff AB, Hinterwimmer S. Degree of axis correction in valgus high tibial osteotomy: proposal of an individualised approach. Int Orthop. 2014;38:2273–80. doi: 10.1007/s00264-014-2442-7. [DOI] [PubMed] [Google Scholar]
- 10.Brinkman JM, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br. 2008;90:1548–57. doi: 10.1302/0301-620X.90B12.21198. [DOI] [PubMed] [Google Scholar]