Abstract
Purpose
The purposes of the present study were to review published studies that investigated arthroscopic meniscus repair to treat meniscus injury in young patients and to compare all-inside and inside-out suture techniques.
Methods
Various electronic databases were queried for published articles, and this search was updated in August 2017 for evaluating the outcomes of arthroscopic meniscus surgery in young patients. Data search, extraction, analysis, and quality assessment were performed according to the Cochrane Collaboration guidelines, and the clinical outcomes were evaluated using various outcome values in young patients according to suture techniques.
Results
Three randomized controlled trials and three prospective comparative studies were included in this systematic review and meta-analysis. There were no significant differences in clinical outcomes such as meniscus healing rate (risk ratio [RR], 1.11; 95% confidence interval [CI], 0.90 to 1.37; I2=39%) and perioperative complications (RR, 0.62; 95% CI, 0.23 to 1.72; I2=43%) between all-inside and inside-out techniques for meniscus repair.
Conclusions
The present study shows favorable results for clinical outcomes such as meniscus healing rate and perioperative complications in young patients. Furthermore, based on our results, both all-inside and inside-out meniscal suture techniques are equally effective in these patients.
Keywords: Knee, Meniscus, Tear, Repair, Suture technique
Introduction
A meniscus tear in young, active patients is critical because of its clinical consequences. The meniscus acts as a shock-absorbing, load-transmitting, and secondary anterior stabilizer of the knee, plays a role in proprioception, and contributes to the lubrication and nutrition of the articular cartilage1–5). For these reasons, a meniscal injury is a potential risk factor for knee osteoarthritis, and thus, many orthopedic surgeons advocate performing surgical meniscal procedures to treat these lesions.
Currently, the typical meniscus surgery is arthroscopically-assisted meniscectomy or meniscus repair. Compared with open meniscus surgery, arthroscopic meniscus surgery has various beneficial effects such as short operation time, early recovery, and minimal trauma. Despite these benefits, arthroscopic meniscectomy can cause disruption of the circumferential fibers, which can ultimately lead to the inability of the remaining meniscus to effectively control hoop stress6). In addition, removing meniscal tissue can directly increase contact stresses, which can cause degenerative knee disorders such as osteoarthritis7–9). Based on this theoretical evidence, a recent review10) suggested that meniscal repair has better long-term patient-reported outcomes and better activity levels than meniscectomy; thus, arthroscopic meniscus repair is recommended over meniscectomy in young patients.
Several recently developed meniscal suture devices are available for peripheral meniscus tears11–15). The development of these devices decreased the risk of meniscectomy, which led to less secondary osteoarthritis16–18). In particular, the all-inside technique has advantages such as low risk of neurovascular injury and short operation time19). However, despite these benefits, recent randomized controlled trials (RCTs)20) reported that there were no statistically significant differences in measured outcomes between the all-inside and inside-out suture techniques, whereas other RCTs21) suggested that arthroscopic meniscus repair with the inside-out technique was superior in comparison with the other methods. Many controversies remain, and therefore, the purposes of the present study were (1) to evaluate the effectiveness of arthroscopic meniscus repair in young patients and (2) to compare the clinical outcomes between the all-inside and inside-out suture techniques. We hypothesized that young patients treated with arthroscopic meniscus repair would also have favorable outcomes and that the two suture techniques were not significantly different in clinical outcomes.
Methods
1. Study Selection
To identify the relevant studies, we used the controlled vocabulary and free text provided in Appendix 1 to query MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials. This study is based on the Cochrane Review Methods, and reporting was carried out according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We attempted to identify all relevant studies in the English language literature irrespective of the publication type (articles, posters, conference articles, instructional course lectures, etc.), publication journal, and publication date. We updated this search in August 2017, and it now includes reference lists from the studies and any review articles that we identified. The reference lists of the investigated studies were scrutinized to identify any possible additional publications not found through electronic or manual searches. Since unpublished data have the risk of bias, they were not included in this study.
2. Eligibility Criteria
We included studies in our meta-analysis if (1) the subjects were patients who had received arthroscopic meniscus repair in young age (the subjects’ mean age in included studies was less than 30 years), (2) the studies investigated clinical outcomes after arthroscopic meniscus repair in young patients, (3) the studies reported on a minimum two-year follow-up data on clinical outcome, functional and imaging outcomes, and (4) the studies included only level I or II evidence. However, we excluded subjects who had degenerative meniscus lesions, studies that only described surgical techniques, studies regarding revision surgery, subjects who had congenital disease or congenital deformity such as discoid meniscus lesions, studies that reported on less than two years of follow-up data, intraoperative measures, or nonclinical outcome measures, levels III, IV, or V, and in vitro and animal studies. Detailed criteria are presented in Table 1.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| The subjects were young patients that received arthroscopic meniscus repair (the subjects’ mean age in included studies was less than 30 years) | Studies that did not compare the effect of arthroscopic meniscus repair |
| Studies regarding revision surgery | |
| Subjects who had congenital disease or congenital deformity | |
| The studies evaluated clinical outcomes after arthroscopic meniscus repair in young patients | Studies reporting less than 2-year follow-up data on clinical outcome, functional and imaging outcomes |
| Studies reporting a minimum 2-year follow-up data on clinical outcome, functional and imaging outcomes | Level III, IV and V evidence (case report, technical note, letters to editor), review articles |
| Only included level-I or -II evidence | Studies that only reported non-clinical outcome measures or intraoperative measures were excluded |
| No exclusions were made on the basis of language | |
| Human subjects | Animal studies or in vitro studies |
3. Data Collection and Analysis
We independently assessed the titles or abstracts of the studies identified via the query and then assessed the full papers for final inclusion through discussion and consensus. We independently abstracted the eligible data into predefined formats and checked them for accuracy. We collected information on the study characteristics (information about the authors, journal, country, surgical procedure, study design, level of evidence, publication year, sample size, subjects’ age, sex, and follow-up period) (Table 2). We evaluated the clinical results of the included studies with respect to the operated side, suture technique, tear length, tear zone, concomitant anterior cruciate ligament (ACL) reconstruction, time from injury to repair, complications, healing rate, and outcome scales at final follow-up (Table 3). We also investigated the numbers of subjects or means and standard deviations for the demographic data and clinical outcomes between the groups.
Table 2.
Characteristics of the Included Studies
| Study | Journal | Country | Surgical procedure | Study design | Level of evidence | Year | Sample size | Age (yr) | Sex (M:F) | Follow-up time (mo) |
|---|---|---|---|---|---|---|---|---|---|---|
| Albrecht-Olsen and Bak13) | Knee Surgery Sports Traumatology Arthroscopy | Denmark | MR | RCT | I | 1999 | 68 | 26.0 (18–40) | 55:13 | Not provided |
| Spindler et al.24) | American Journal of Sports Medicine | USA | MR | PCS | II | 2003 | 125 | 23.8±9.3 | 65:60 | 40.1 |
| Barber et al.26) | Arthroscopy | USA | MR | PCS | II | 2005 | 85 | 27.0 (15–48) | 54:31 | 26.5 (12–56) |
| Hantes et al.21) | Knee Surgery Sports Traumatology Arthroscopy | Greece | MR | RCT | II | 2006 | 57 | 27.1 | 13:44 | 22.3 (17–37) |
| Bryant et al.20) | American Journal of Sports Medicine | Canada | MR | RCT | I | 2007 | 100 | 25.4±8.0 | 62:38 | 28.0±8.4 (9–46) |
| Choi et al.27) | American Journal of Sports Medicine | Korea | MR | PCS | II | 2009 | 48 | 28.0 (15–55) | 44:4 | 35.7 (24–91) |
Values are presented as mean±standard deviation (range).
MR: meniscus repair, RCT: randomized controlled trial, PCS: prospective cohort study, M: male, F: female.
Table 3.
Characteristics of Meniscal Tear and Surgical Techniques for Meniscus Repair
| Study | Meniscus side (M/L) | Suture technique | Tear length (mm) | Tear zone (distance from capsule, mm) | Concomitant ACLR | Time from injury to repair | No. of complications (%) | No. of healing (%) | Outcome scale |
|---|---|---|---|---|---|---|---|---|---|
| Albrecht-Olsen and Bak13) | 21/13 | Arrow: 34 | 25.0 (12–40) | 1.9 (0–4) | 10 | <2 mo: 14 2 mo–1 yr: 6 >1 yr: 13 |
2 (5.9) | 30 (88.2) | N/P |
| 21/13 | IO: 34 | 25.1 (15–40) | 2.1 (0–4) | 9 | < 2 mo: 23 2 mo–1 yr: 8 >1 yr: 3 |
7 (20.6) | 24 (70.6) | ||
| Spindler et al.24) | 40/0 | IO: 40 | 16.0±4.7 | R-R (40), R-W(0) | 40 | N/P | 8 (20.0) | 33 (82.5) | IKDC, Lysholm score, SF-36, WOMAC, KOOS |
| 85/7 | Arrow: 85 | 15.7±3.5 | R-R (81), R-W (4) | 85 | 5 (5.9) | 78 (91.8) | |||
| Barber et al.26) | 66/23 | Arrow: 47 | 19.0±5.0 | R-R (31), R-W (15), W-W (2) | 41 | N/P | 2 (4.3) | 43 (91.5) | Lysholm score, Tegner score, IKDC, Cincinnati score |
| IO: 29 | 19.5±4.8 | R-R (20), R-W (7), W-W (2) | 24 | 0 | 29 (100) | ||||
| Arrow+IO: 13 | 29.6±4.1 | R-R (9), R-W (4), W-W (0) | 8 | 0 | 11 (84.6) | ||||
| Hantes et al.21) | 14/3 | OI: 17 | 28.8 | R-R (16), R-W (6) | 10/7 | >3 wk: 14 <3 wk 3 |
1 (5.9) | 17 (100.0) | IKDC |
| 17/3 | IO: 20 | 27.8 | R-R (12), R-W (8) | 13/7 | >3 wk: 16 <3 wk: 4 |
3 (15.0) | 19 (95.0) | ||
| 17/3 | AI: 20 | 25.0 | R-R (13), R-W (7) | 5/15 | >3 wk: 15 <3 wk: 5 |
1 (5.0) | 13 (65.0) | ||
| Bryant et al.20) | 46/5 | Arrow: 51 | 24.7±11 | Ramp (2), R-R (35), R-W (16) | 34 | 14.2±17 mo | 14 (27.5) | 40 (78.4) | QOL, WOMET, ROM |
| 40/11 | IO: 49 | 22.8±10 | Ramp (5), R-R (35), R-W (16) | 31 | 17.6±22 mo | 12 (24.5) | 38 (77.6) | ||
| Choi et al.27) | 20/14 | IO: 34 | N/P | Ramp (12), R-R (13), R-W (9) | N/P | >6 wk: 13 <6 wk: 21 |
5 (14.7) | 24 (70.6) | Lachman test, side-to-side difference, Lysholm score, Tegner score, Pivot shift test |
| 8/6 | AI: 14 | Ramp (4), R-R (5), R-W (5) | >6 wk: 6 <6 wk: 8 |
1 (7.1) | 10 (71.4) |
Values are presented as mean±standard deviation (range).
M/L: medial/lateral, ACLR: anterior cruciate ligament reconstruction, N/P: not provided, IO: inside-out, R-R: red-red, R-W: red-white, IKDC: International Knee Documentation Committee, SF-36: Short Form-36, WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index, KOOS: Knee Injury and Osteoarthritis Outcome Score, W-W: white-white, OI: outside-in, AI: all-inside, QOL: quality of life, WOMET: Western Ontario Meniscal Evaluation Tool, ROM: range of motion.
4. Assessing Methodological Quality
We independently assessed the methodological qualities of the RCTs using the PEDro critical appraisal scoring system, which is an 11-item scale that has previously demonstrated reliability and validity in assessing RCTs22). In addition, we assessed the methodological quality of comparative studies using the Newcastle-Ottawa quality assessment scale23). We resolved any disagreements between us through discussion or review by a third investigator, and we attempted to clarify any uncertainties in outcomes or methodologies through personal correspondence with the authors. We did not evaluate publication bias due to low statistical power because the number of studies included was less than 10 in each field of research.
5. Statistical Analysis
In this review, we evaluated the clinical outcomes of arthroscopic meniscus surgery in young patients and investigated the effects of different suture techniques; clinical outcomes mainly focused on meniscus healing rate and perioperative complications. To evaluate the two outcomes after arthroscopic meniscus surgery, we calculated the risk ratios (RRs) between the groups. We used Review Manager (RevMan) ver. 5.3 (The Cochrane Collaboration, London, UK) to estimate the overall pooled effect sizes for each outcome and conducted a meta-analysis of the included studies using a random effects model. For binary outcomes, we calculated the RRs between the groups using the Mantel-Haenszel method. We assessed statistical heterogeneity among the studies according to the I-squared (I2) value, with values of 25%, 50%, and 75% considered low, moderate, and high, respectively. We used the Cochrane Q statistic (chi-square test) to assess heterogeneity and defined p<0.10 as significant heterogeneity.
Results
1. Identifying the Studies
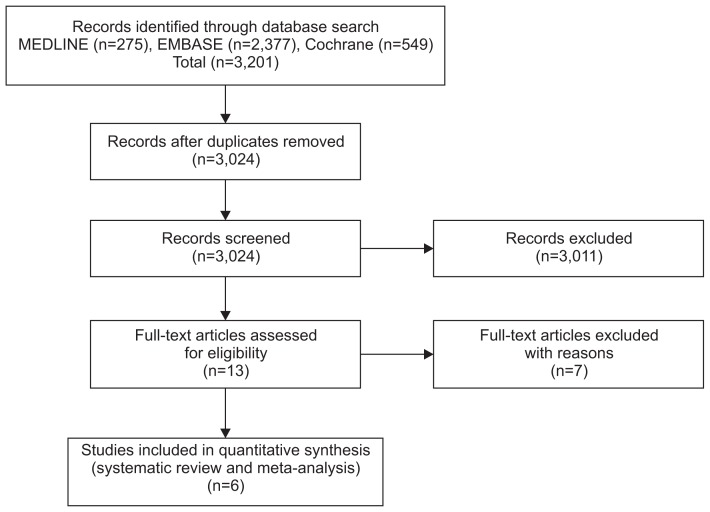
We initially identified a total of 3,201 relevant articles; of these, 177 were duplicated in the databases. After we screened the remaining 3,024 articles using titles and abstracts, we excluded all but 13 because they were not relevant to the purpose of the present study. A thorough full-text review of the 13 articles excluded 7 because they lacked vital data such as experimental or clinical outcomes. The majority of the excluded articles did not investigate the clinical outcomes of each technique, were inappropriate regarding the patients’ ages, evaluated meniscus suture techniques, were biomechanical studies of meniscus, or were animal studies. Finally, we included six studies for the data extraction and meta-analysis (Fig. 1)20,21,24–27).
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
2. Quality of the Included Studies
As mentioned above, we used the PEDro critical appraisal score to assess the methodological quality of the RCTs and assessed the methodological quality of comparative studies using the Newcastle-Ottawa Quality Assessment Scale. The mean PEDro score was 8.3 points (range, 8 to 9 points), indicating that most studies had good quality by the current scoring system. Furthermore, total scores of the Newcastle-Ottawa quality assessment scale are over 7.3 points (range, 7 to 8 points), which indicated a low risk of bias for the included studies, and therefore, we included all selected studies in this meta-analysis.
3. Clinical Results of the RCTs
The six studies were three RCTs and three prospective comparative studies. It is inappropriate to analyze RCTs with comparative studies because this increases the risk of bias, and thus, we only analyzed RCTs. We could not analyze outcome scales such as Lysholm knee score, Tegner activity score, International Knee Documentation Committee score, quality of life, or side-to-side differences because of insufficient data such as means or standard deviations. Based on tables and results of each study, we prepared a forest plot of healing rate and prevalence of perioperative complications.
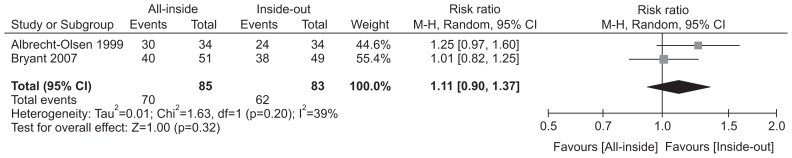
1) Healing rate
In qualitative analysis, regardless of suture technique, the healing rates for arthroscopic meniscus repair were 70.8%–93.3% across the studies. In the quantitative analysis, the two RCTs20,25) reported on the healing rates between the two techniques with a total of 168 patients (85 in the all-inside group and 83 in the inside-out group). There was no significant difference in the healing rate between the all-inside and inside-out techniques (RR, 1.11; 95% CI, 0.90 to 1.37; I2=39%) (Fig. 2).
Fig. 2.
Forest plot of meniscus healing rates of randomized controlled trials using the all-inside and inside-out techniques. CI: confidence interval.
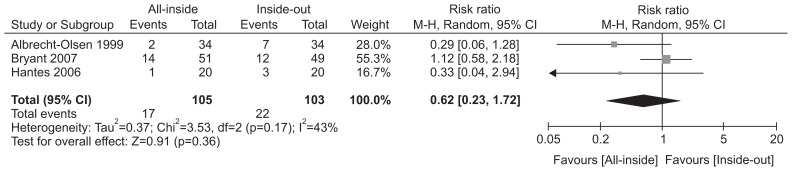
2) Perioperative complications
In the qualitative analysis, regardless of suture technique, the prevalence of perioperative complications was 2.2%–26.0% across studies. The three RCTs20,21,25) reported on the perioperative complications between the two techniques with a total of 208 patients (105 in the all-inside group and 103 in the inside-out group). There were no significant differences in the perioperative complications between the all-inside and inside-out techniques (RR, 0.62; 95% CI, 0.23 to 1.72; I2=43%) (Fig. 3).
Fig. 3.
Forest plot of the prevalence of perioperative complications in the randomized controlled trials using the all-inside and inside-out techniques. CI: confidence interval.
Discussion
In this meta-analysis, we assessed evidence from clinical studies that evaluated the outcomes of arthroscopic meniscus repair for meniscus tears in young patients, and we compared the effects between the all-inside and inside-out meniscal suture techniques. The most important finding of the present study was that the clinical outcomes such as meniscus healing rates and perioperative complications in these patients improved favorably after arthroscopic meniscus repair, and there were no significant differences between the two different suture technique groups. This indicates that arthroscopic meniscus repair should be considered a treatment of choice for traumatic meniscus tears in young patients and the suture technique can be selected based on the surgeon’s familiarity with the procedure.
In terms of anatomic characteristics of the meniscus, the peripheral one third of the meniscus has the best blood supply in adults28). For this reason, vertical tears <5 mm in length in the peripheral one third of the meniscus are generally stable, and conservative care is recommended6). However, whereas conservative treatment of stable meniscus tears can potentially result in complete healing, sometimes it leads to a reparable or irreparable tear if the tear progressed due to highly demanding activity or frequent trauma history, especially in young patients; in these cases, arthroscopic meniscus repair is recommended for conserving the remaining meniscus tissue. Meniscus repair preserves meniscus tissue, and it also offers biomechanical advantages7). In the same context, multiple studies have presented satisfactory outcomes after meniscus suture repair: in one meta-analysis, meniscus repair was associated with better long-term outcomes than those following meniscectomy10). Thus, despite the results of previous studies showing a failure rate of 15%–30% in repaired isolated meniscal tears without ACL injury, many authors advocate meniscus repair to preserve meniscus tissue29,30). Our results also showed favorable healing rates and perioperative complication rates after arthroscopic meniscus repair in young patients. This can strengthen the clinical evidence for arthroscopic meniscus repair in these patients.
Meniscus repair is globally accepted among orthopedic surgeons, and the inside-out technique has been used widely for posterior horn tears of the meniscus; however, this technique requires an additional skin incision and has a risk of neurovascular injuries and postoperative stiffness27). The new all-inside technique using bioabsorbable materials was developed to overcome the drawbacks19). The all-inside technique also has benefits such as short operation time and good healing rate with satisfactory outcomes31). Furthermore, this technique was especially useful in cases with ramp lesions27). Despite these various benefits of the all-inside technique, several complications are associated with this technique as well. For example, authors of one study reported complications such as chondral damage, device-induced irritation, device breakage, foreign body reaction, and synovitis32–35). Based on these discrepancies, one study36) demonstrated that the all-inside technique using arrows had significantly higher failure strength than did other meniscal repair devices; conversely, another study37) found that inside-out sutures had significantly higher mean loads to failure than meniscal arrows. In addition, Spindler et al.24) found no differences in failure rates between two groups, and Bryant et al.20) conducted RCTs on this topic and also reported that there were no statistically significant differences in measured outcomes between the meniscus inside-out suturing and arrows. In the same context, Spindler et al.24) and Bryant et al.20) reported that there were no differences in meniscus healing rates or perioperative complications between the two groups in their meta-analyses. Although we could not analyze clinical outcome scales in this meta-analysis due to insufficient data, our results strengthen previous study results and confirm the appropriateness of arthroscopic meniscus suture repair for treating meniscus tears in young patients. To verify which suture technique yields greater improvement in clinical outcomes, more high quality RCTs are needed.
We assessed the quality of the included studies using the PEDro critical appraisal scoring system or the Newcastle-Ottawa Quality Assessment Scale. By PEDro score, all RCTs scored ≥ 8 points (range, 8 to 9 points) and Newcastle-Ottawa Quality Assessment Scale for comparative studies scored ≥ 7 points (range, 7 to 8 points). These results indicate a low risk of bias of the included studies and their eligibility for the analysis. In addition, two independent, blinded reviewers performed the screening and data extraction, which is one of the strengths of our study.
However, despite its strengths, there are some limitations to the present study. First, we used a relatively small number of studies in this meta-analysis: a search of the literature revealed that the number of original, previously published articles on this topic is inadequate, which is a clear limitation. However, all of the included clinical studies were entirely level I or II (high-quality) studies, and this may carry a low risk of bias. Second, there was heterogeneity in the studies regarding the patient populations, the different scoring systems, the patterns of meniscus tears, the follow-up durations, and the surgical indications for arthroscopic meniscus surgery. Third, we did not fully consider other factors that could have affected clinical outcomes, such as patient gender, meniscus tear type, size, location (medial or lateral) and site, time from injury to arthroscopic surgery, and concomitant ACL injury. Of course, removing all confounding factors is ideal to reduce the risk of bias in the evaluation of one independent factor. However, strict control of all confounding factors affecting clinical outcomes is difficult in practice. Furthermore, permission to conduct more dissimilar heterogeneous studies will lead to improved external validity and generalizability. This concept is associated with “effectiveness”: heterogeneous, more practical, “real world” studies in normal clinical conditions likely encountered in practical clinical trials38). Hence, even though all of the included studies are prospective studies, the findings of the forest plots of the present study should be interpreted with great caution considering that the data were extracted from somewhat heterogeneous studies. Furthermore, despite these discrepancies, to minimize the risk of bias and compensate for heterogeneity, we used random effect model analysis according to the Cochrane Guidelines. In the future, in order to overcome these issues, prospective studies that control for these independent factors through high-quality medical research need to be encouraged.
Conclusions
The present study presents favorable clinical outcomes in terms of meniscus healing rates and perioperative complications in young patients. Furthermore, based on our results, both the all-inside and inside-out meniscal suture techniques can be equally effective in these patients. To strengthen our results, more high-quality clinical trials and RCTs are warranted.
Appendix 1. Electronic Search Strategy for Each Database
MEDLINE
“Menisci, Tibial”[Mesh] 6150
Menisci[tiab] OR meniscal[tiab] OR meniscus[tiab] 12783
1 OR 2 14102
((“Arthroscopy”[Mesh]) OR “Suture Techniques”[Mesh]) OR “Rupture”[Majr] 76936
repairs[tiab] OR tears[tiab] OR Arthroscopy[tiab] OR Arthroscopies[tiab] OR Arthroscopic[tiab] OR Rupture[tiab] OR Suture[tiab] OR repair[tiab] OR tear[tiab] OR Rupture[tiab] OR injury[tiab] OR injuries[tiab] 1016833
4 OR 5 1047348
3 AND 6 8475
7 NOT (“review”[Publication Type] OR “review literature as topic”[MeSH Terms]) 7463
8 AND (“Controlled clinical trial” [ptyp]) 275
EMBASE
‘knee meniscus’/exp 12026
Menisci:ab,ti OR meniscal:ab,ti OR meniscus:ab,ti 15538
1 OR 2 18213
‘knee meniscus rupture’/exp OR ‘knee arthroscopy’/exp OR ‘suturing method’/exp OR ‘suture’/de OR ‘meniscal repair’/exp OR ‘meniscal surgery’/de 68017
repairs:ab,ti OR tears:ab,ti OR Arthroscopy:ab,ti OR Arthroscopies:ab,ti OR Arthroscopic:ab,ti OR Rupture:ab,ti OR Suture:ab,ti OR repair:ab,ti OR tear:ab,ti OR Rupture:ab,ti OR injury:ab,ti OR injuries:ab,ti 1260152
4 OR 5 1288683
3 AND 6 11581
7 NOT (‘conference review’/it OR ‘review’/it) 10300
8 AND (‘controlled study’/it) 2377
COCHRANE
MeSH descriptor: [Menisci, Tibial] explode all trees 219
Menisci OR meniscal OR meniscus 702
1 OR 2 702
MeSH descriptor: [Arthroscopy] explode all trees 1443
MeSH descriptor: [Suture Techniques] explode all trees 1976
MeSH descriptor: [Rupture] this term only 615
repairs OR tears OR Arthroscopy OR Arthroscopies OR Arthroscopic OR Rupture OR Suture OR repair OR tear OR Rupture OR injury OR injuries 52836
4-7/OR 53028
3 AND 8 587
9/TRIALS 549
Web of Science (WOS)
TOPIC: (Menisci OR meniscal OR meniscus) OR TITLE: (Menisci OR meniscal OR meniscus) 15299
TOPIC: (repairs OR tears OR Arthroscopy OR Arthroscopies OR Arthroscopic OR Rupture OR Suture OR repair OR tear OR Rupture OR injury OR injuries) OR TITLE: (repairs OR tears OR Arthroscopy OR Arthroscopies OR Arthroscopic OR Rupture OR Suture OR repair OR tear OR Rupture OR injury OR injuries) 1218242
1 AND 2 7014
3 Refined by: [excluding] DOCUMENT TYPES: (REVIEW) 6576
SCOPUS
INDEXTERMS(“Menisci, Tibial”) 6972
TITLE-ABS(Menisci OR meniscal OR meniscus) 22154
1 OR 2 23706
INDEXTERMS(“Arthroscopy” OR “Suture Techniques” OR “Rupture”) 184410
TITLE-ABS(repairs OR tears OR Arthroscopy OR Arthroscopies OR Arthroscopic OR Rupture OR Suture OR repair OR tear OR Rupture OR injury OR injuries) 1383260
4 OR 5 1447468
3 AND 6 11082
7 AND ( EXCLUDE (DOCTYPE, “re”) ) 9937
8 AND (LIMIT-TO (DOCTYPE, “ar”)) 8869
Footnotes
Source of funding: This work was supported by the Korean Military Medical Research Project funded by the ROK Ministry of National Defense (ROK-MND-2017-KMMRP-025).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Hollis JM, Pearsall AW, 4th, Niciforos PG. Change in meniscal strain with anterior cruciate ligament injury and after reconstruction. Am J Sports Med. 2000;28:700–4. doi: 10.1177/03635465000280051401. [DOI] [PubMed] [Google Scholar]
- 2.Renstrom P, Johnson RJ. Anatomy and biomechanics of the menisci. Clin Sports Med. 1990;9:523–38. [PubMed] [Google Scholar]
- 3.Seedhom BB, Dowson D, Wright V. Proceedings: functions of the menisci: a preliminary study. Ann Rheum Dis. 1974;33:111. doi: 10.1136/ard.33.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Voloshin AS, Wosk J. Shock absorption of meniscectomized and painful knees: a comparative in vivo study. J Biomed Eng. 1983;5:157–61. doi: 10.1016/0141-5425(83)90036-5. [DOI] [PubMed] [Google Scholar]
- 5.Zimny ML, Albright DJ, Dabezies E. Mechanoreceptors in the human medial meniscus. Acta Anat (Basel) 1988;133:35–40. doi: 10.1159/000146611. [DOI] [PubMed] [Google Scholar]
- 6.Giuliani JR, Burns TC, Svoboda SJ, Cameron KL, Owens BD. Treatment of meniscal injuries in young athletes. J Knee Surg. 2011;24:93–100. doi: 10.1055/s-0031-1280877. [DOI] [PubMed] [Google Scholar]
- 7.Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: a preliminary report. Am J Sports Med. 1986;14:270–5. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 8.Renstrom P, Ljungqvist A, Arendt E, Beynnon B, Fukubayashi T, Garrett W, Georgoulis T, Hewett TE, Johnson R, Krosshaug T, Mandelbaum B, Micheli L, Myklebust G, Roos E, Roos H, Schamasch P, Shultz S, Werner S, Wojtys E, Engebretsen L. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;42:394–412. doi: 10.1136/bjsm.2008.048934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee SJ, Aadalen KJ, Malaviya P, Lorenz EP, Hayden JK, Farr J, Kang RW, Cole BJ. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006;34:1334–44. doi: 10.1177/0363546506286786. [DOI] [PubMed] [Google Scholar]
- 10.Xu C, Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2015;23:164–70. doi: 10.1007/s00167-013-2528-6. [DOI] [PubMed] [Google Scholar]
- 11.Haas AL, Schepsis AA, Hornstein J, Edgar CM. Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy. 2005;21:167–75. doi: 10.1016/j.arthro.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 12.Barber FA, Herbert MA. Meniscal repair devices. Arthroscopy. 2000;16:613–8. doi: 10.1053/jars.2000.4819. [DOI] [PubMed] [Google Scholar]
- 13.Albrecht-Olsen PM, Bak K. Arthroscopic repair of the bucket-handle meniscus: 10 failures in 27 stable knees followed for 3 years. Acta Orthop Scand. 1993;64:446–8. doi: 10.3109/17453679308993664. [DOI] [PubMed] [Google Scholar]
- 14.Farng E, Sherman O. Meniscal repair devices: a clinical and biomechanical literature review. Arthroscopy. 2004;20:273–86. doi: 10.1016/j.arthro.2003.11.035. [DOI] [PubMed] [Google Scholar]
- 15.Tsai AM, McAllister DR, Chow S, Young CR, Hame SL. Results of meniscal repair using a bioabsorbable screw. Arthroscopy. 2004;20:586–90. doi: 10.1016/j.arthro.2004.04.064. [DOI] [PubMed] [Google Scholar]
- 16.Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:664–70. doi: 10.1302/0301-620X.30B4.664. [DOI] [PubMed] [Google Scholar]
- 17.Jackson JP. Degenerative changes in the knee after meniscectomy. Br Med J. 1968;2:525–7. doi: 10.1136/bmj.2.5604.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jorgensen U, Sonne-Holm S, Lauridsen F, Rosenklint A. Long-term follow-up of meniscectomy in athletes: a prospective longitudinal study. J Bone Joint Surg Br. 1987;69:80–3. doi: 10.1302/0301-620X.69B1.3818740. [DOI] [PubMed] [Google Scholar]
- 19.Jurist KA, Greene PW, 3rd, Shirkhoda A. Peroneal nerve dysfunction as a complication of lateral meniscus repair: a case report and anatomic dissection. Arthroscopy. 1989;5:141–7. doi: 10.1016/0749-8063(89)90010-8. [DOI] [PubMed] [Google Scholar]
- 20.Bryant D, Dill J, Litchfield R, Amendola A, Giffin R, Fowler P, Kirkley A. Effectiveness of bioabsorbable arrows compared with inside-out suturing for vertical, reparable meniscal lesions: a randomized clinical trial. Am J Sports Med. 2007;35:889–96. doi: 10.1177/0363546506298582. [DOI] [PubMed] [Google Scholar]
- 21.Hantes ME, Zachos VC, Varitimidis SE, Dailiana ZH, Karachalios T, Malizos KN. Arthroscopic meniscal repair: a comparative study between three different surgical techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14:1232–7. doi: 10.1007/s00167-006-0094-x. [DOI] [PubMed] [Google Scholar]
- 22.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–21. [PubMed] [Google Scholar]
- 23.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 24.Spindler KP, McCarty EC, Warren TA, Devin C, Connor JT. Prospective comparison of arthroscopic medial meniscal repair technique: inside-out suture versus entirely arthroscopic arrows. Am J Sports Med. 2003;31:929–34. doi: 10.1177/03635465030310063101. [DOI] [PubMed] [Google Scholar]
- 25.Albrecht-Olsen P, Kristensen G, Burgaard P, Joergensen U, Toerholm C. The arrow versus horizontal suture in arthroscopic meniscus repair: a prospective randomized study with arthroscopic evaluation. Knee Surg Sports Traumatol Arthrosc. 1999;7:268–73. doi: 10.1007/s001670050162. [DOI] [PubMed] [Google Scholar]
- 26.Barber FA, Johnson DH, Halbrecht JL. Arthroscopic meniscal repair using the BioStinger. Arthroscopy. 2005;21:744–50. doi: 10.1016/j.arthro.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Choi NH, Kim TH, Victoroff BN. Comparison of arthroscopic medial meniscal suture repair techniques: inside-out versus all-inside repair. Am J Sports Med. 2009;37:2144–50. doi: 10.1177/0363546509339010. [DOI] [PubMed] [Google Scholar]
- 28.Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10:90–5. doi: 10.1177/036354658201000205. [DOI] [PubMed] [Google Scholar]
- 29.Rockborn P, Messner K. Long-term results of meniscus repair and meniscectomy: a 13-year functional and radiographic follow-up study. Knee Surg Sports Traumatol Arthrosc. 2000;8:2–10. doi: 10.1007/s001670050002. [DOI] [PubMed] [Google Scholar]
- 30.Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jäger A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38:1542–8. doi: 10.1177/0363546510364052. [DOI] [PubMed] [Google Scholar]
- 31.Hurel C, Mertens F, Verdonk R. Biofix resorbable meniscus arrow for meniscal ruptures: results of a 1-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2000;8:46–52. doi: 10.1007/s001670050010. [DOI] [PubMed] [Google Scholar]
- 32.Anderson K, Marx RG, Hannafin J, Warren RF. Chondral injury following meniscal repair with a biodegradable implant. Arthroscopy. 2000;16:749–53. doi: 10.1053/jars.2000.7672. [DOI] [PubMed] [Google Scholar]
- 33.Ganko A, Engebretsen L. Subcutaneous migration of meniscal arrows after failed meniscus repair. A report of two cases. Am J Sports Med. 2000;28:252–3. doi: 10.1177/03635465000280021801. [DOI] [PubMed] [Google Scholar]
- 34.Kurzweil PR, Tifford CD, Ignacio EM. Unsatisfactory clinical results of meniscal repair using the meniscus arrow. Arthroscopy. 2005;21:905. doi: 10.1016/j.arthro.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 35.Song EK, Lee KB, Yoon TR. Aseptic synovitis after meniscal repair using the biodegradable meniscus arrow. Arthros copy. 2001;17:77–80. doi: 10.1053/jars.2001.7800. [DOI] [PubMed] [Google Scholar]
- 36.Arnoczky SP, Lavagnino M. Tensile fixation strengths of absorbable meniscal repair devices as a function of hydrolysis time: an in vitro experimental study. Am J Sports Med. 2001;29:118–23. doi: 10.1177/03635465010290020201. [DOI] [PubMed] [Google Scholar]
- 37.Dervin GF, Downing KJ, Keene GC, McBride DG. Failure strengths of suture versus biodegradable arrow for meniscal repair: an in vitro study. Arthroscopy. 1997;13:296–300. doi: 10.1016/S0749-8063(97)90024-4. [DOI] [PubMed] [Google Scholar]
- 38.Harris JD, Brand JC, Cote MP, Dhawan A. Research pearls: the significance of statistics and perils of pooling. Part 3: pearls and pitfalls of meta-analyses and systematic reviews. Arthroscopy. 2017;33:1594–602. doi: 10.1016/j.arthro.2017.01.055. [DOI] [PubMed] [Google Scholar]