Abstract
Background
The purpose of this study was to comprehensively examine the association of a multitude of individual medical conditions, as well as multimorbidity, on work status among a national sample of U.S. adults.
Methods
The present study included 7 cycles (1999–2012) from the National Health and Nutrition Examination Survey (N = 28,119).
Results
In total, 26 medical conditions increased the odds of not working. Multimorbidity as well as having prevalent medical condition(s) within each of the Cumulative Index Rating Scale Morbidity Classes were associated with increased odds of not working. Few medical conditions were associated with higher odds of working part-time (vs. full-time) or unemployment (vs. working).
Conclusion
These findings underscore the importance of instating comprehensive worksite wellness health promotion policies, as well as providing individuals with resources to preserve and enhance personal health.
Keywords: Chronic disease, Employment, Epidemiology, Multimorbidity
INTRODUCTION
Work status is frequently considered a predictor of poor health, with non-working adults reporting lower self-worth, less self-confidence, and less social integration. Previous research has also shown that life expectancy is inversely associated with high unemployment rates in the U.S [1]. In this nationally representative study, heart disease, cancer, diabetes, and liver cirrhosis were among the variables shown to be related to reduced life expectancy. The authors suggest that evaluating the impact of employment status on health disparities is an exigent public policy concern [1]. We hypothesize that health status may also be linked with various employment outcomes, and that this bidirectional relationship warrants further investigation. Other work utilizing national-level data indicate a relationship between various comorbidities, including musculoskeletal conditions [2], depression [3], chronic pain [4], on working status. We propose that delineating the plausible linkage between multimorbidity and employment is of paramount importance, as chronic physical and psychological limitations may predict increased risk of early mortality [5]. Thus, identifying and addressing medical conditions which may increase the likelihood of not working remains a major national health issue. To our knowledge, this is the first population-based study utilizing NHANES data to investigate this relationship. To this end, the purpose of this investigation was to comprehensively examine the association between a multitude of medical conditions and work status among a national sample of U.S. adults.
We chose to partition work status into distinct categories, beyond employed versus unemployed, as recent work demonstrates the damaging effects of insufficient employment in the modern economic climate [6]. Individuals employed part-time, may receive lower hourly wages, or salary reductions. Therefore, full time versus part-time status were included as critical variables of interest. We also dichotomized individuals into not working/not actively seeking gainful employment (i.e. those unable to work), and unemployed individuals, who are expected to be physically and/or mentally able to actively seek employment. This is an important distinction, as the capacity for seeking employment is likely to contribute to temporary versus long-term absences from the workforce, as well as differential consequences of not working between these groups, which may include (but is not limited to) social risk factors, progression of chronic disease states, access to healthcare, socioeconomic status and eligibility for financial assistance.
Poverty has been shown to impact global health status [7]. This relationship may be bidirectional, meaning health status may also contribute to reduced ability to work, or work effectively and consistently when employed. Thus, more research is needed on this topic to evaluate the specific influences of physical and psychological health determinants on stable employment. Healthcare policies in the United States have traditionally highlighted the importance of providing treatment for acute conditions. Economic and public health resources are generally directed to clinical care, over behavioral and lifestyle interventions, an imbalance which may exacerbate the extent of population-based health disparity over time [8]. Exploring the linkages between chronic lifestyle conditions and the ability to remain productive in the workforce will underscore the need for targeted public health interventions to develop strategies promoting both stable heath and stable employment.
In addition to examining the impact of medical and behavioral conditions, we also examined the extent to which multimorbidity (combination of medical conditions) is associated with work status. Our work provides important nationally representative data regarding health-related factors which affect employment. Such information will facilitate the development, implementation, and evaluative efforts of targeted interventions to promote employment among those with chronic illness.
MATERIALS AND METHODS
1. Design and participants
Data was obtained from the National Health and Nutrition Examination Survey (NHANES). NHANES is an ongoing survey conducted by the CDC that uses a representative sample of non-institutionalized U.S. civilians, selected by a complex, multistage, stratified, clustered probability design. The present study included 7 NHANES cycles (1999–2012), totaling 28,119 U.S. adults age 20 to 64. We combined NHANES 1999–2000 and 2001–2002 survey years prior to computing our analyses. As these survey years are not directly comparable, we utilized the NCHS 4-year sample weights with the 2-year weights for 2003–2004, 2005–2006, 2007–2008, 2009–2010, and 2011–2012 to create a 14-year weight variable that sufficiently accounted for the difference in population estimates between the selected survey cycles.
The multistage design consists of 4 stages, including the identification of counties, segments (city blocks), random selection of households within the segments, and random selection of individuals within the households. During each cycle, participants were sampled across 15 different U.S. geographic areas. Participants were interviewed in their homes and then subsequently examined in a mobile examination center (MEC) by NHANES personnel. The self-report medical conditions (e.g., coronary artery disease) were obtained from the household interview, with the examination (e.g., peripheral neuropathy) and laboratory (e.g., cholesterol) data obtained during the MEC evaluation. The impact of medical conditions was examined across the cycles for which that medical condition was assessed (Table 1). Participants provided informed consent and the study was approved by the National Center for Health Statistics ethics committee.
Table 1.
NHANES cycles utilized and available data for each of the evaluated medical conditions*
| Medical/Health Condition | NHANES Cycles Evaluated | Unweighted Sample Size for Variable (n)a | Unweighted Sample Size for Having the Condition (n)b | Weighted Proportion (%) for Having the Conditionc | Age Range of Participants |
|---|---|---|---|---|---|
| Determined from Questionnaire | |||||
| Depression | 2005–2012 | 14,762 | 1,450 | 7.9 | 20–64 |
| Self-Report of Physician Diagnosis | |||||
| Arthritis | 1999–2012 | 28,119 | 4,946 | 17.3 | 20–64 |
| Asthma | 1999–2012 | 28,119 | 3,729 | 13.6 | 20–64 |
| Bronchitis | 1999–2012 | 28,119 | 1,457 | 5.5 | 20–64 |
| Cancer (of any type) | 1999–2012 | 28,119 | 1,316 | 5.5 | 20–64 |
| Congestive Heart Failure | 1999–2012 | 28,119 | 426 | 1.1 | 20–64 |
| Coronary Artery Disease | 1999–2012 | 28,119 | 512 | 1.6 | 20–64 |
| Diabetes | 1999–2012 | 28,119 | 2,185 | 5.7 | 20–64 |
| Emphysema | 1999–2012 | 28,119 | 307 | 1.1 | 20–64 |
| Liver Disease | 1999–2012 | 28,119 | 953 | 3.1 | 20–64 |
| Sleep Disorder | 2005–2012 | 17,136 | 1,289 | 7.7 | 20–64 |
| Stroke | 1999–2012 | 28,119 | 510 | 1.4 | 20–64 |
| Determined from Examination | |||||
| Age-Related Macular Degeneration | 2005–2008 | 3,633 | 119 | 3.1 | 40–64 |
| Visual Impairment | 1999–2008 | 17,033 | 146 | 0.7 | 20–64 |
| Cardiorespiratory Fitness | 1999–2004 | 3,300 | 550 | 15.4 | 20–49 |
| Chronic Obstructive Pulmonary Disease | 2007–2010 | 5,499 | 580 | 11.5 | 20–64 |
| Hearing Impairment | 1999–2010 | 4,510 | 1,395 | 31.3 | 20–64 |
| Non-Proliferative Retinopathy | 2005–2008 | 3,655 | 395 | 8.3 | 40–64 |
| Obesity | 1999–2012 | 26,593 | 9,511 | 33.4 | 20–64 |
| Underweight | 1999–2012 | 26,593 | 451 | 1.8 | 20–64 |
| Peripheral Arterial Disease | 1999–2004 | 4,063 | 541 | 11.4 | 40–64 |
| Peripheral Neuropathy | 1999–2004 | 4,701 | 514 | 9.0 | 40–64 |
| Physical Inactivity | 2003–2006 | 4,339 | 2,365 | 50.7 | 20–64 |
| Determined from Laboratory Assessment | |||||
| Chronic Kidney Disease | 1999–2012 | 25,247 | 515 | 1.8 | 20–64 |
| Elevated C-Reactive Protein | 1999–2010 | 21,532 | 8,480 | 35.1 | 20–64 |
| Elevated Fasting Glucose | 1999–2012 | 12,429 | 1,045 | 5.9 | 20–64 |
| Elevated LDL Cholesterol | 1999–2012 | 11,744 | 1,381 | 11.5 | 20–64 |
| Elevated Total Cholesterol | 1999–2012 | 25,304 | 3,772 | 14.6 | 20–64 |
| Elevated Triglycerides | 1999–2012 | 12,309 | 2,071 | 15.1 | 20–64 |
| Low HDL Cholesterol | 1999–2012 | 25,304 | 5,088 | 20.5 | 20–64 |
| Hypertension | 1999–2012 | 25,661 | 3,596 | 12.3 | 20–64 |
| Smoking (cotinine) | 2003–2012 | 18,778 | 5,937 | 31.5 | 20–64 |
Estimates in this table are after excluding participants with missing work status data and those between 20 and 74 years of age (only those 20 yrs and older were eligible for the medical condition survey).
Represents the unweighted sample size for the evaluated variable (e.g., 33,095 participants provided data for having arthritis [yes/no]) across the available NHANES cycles.
Represents the unweighted sample size for having the evaluated medical condition. For example, 7,342 had a physician diagnosis of arthritis. For medical conditions with multiple categories (e.g., no retinopathy, mild retinopathy, and moderate or greater retinopathy), this sample size estimate is the number of participants with any degree of the impairment/condition (e.g., mild or moderate+ retinopathy).
Represents the weighted proportion of column “c”, i.e., the proportion of Americans with any degree of the evaluated impairment/condition.
2. Assessment of medical conditions & work status
Evaluated conditions were based on self-report (e.g., survey-assessed depression), physician diagnosis (e.g., stroke), direct examination (e.g., peripheral neuropathy), and laboratory values (e.g., elevated cholesterol), with medical conditions categorized into Cumulative Index Rating Scale (CIRS) Morbidity Classes. Details regarding the assessment of self-report, physician-diagnosed, examination-determined, and laboratory-determined medical conditions are provided in the Table 2. Across the 1999–2012 cycles, 15 medical conditions were consistently evaluated across all ages, including arthritis, asthma, bronchitis, cancer, congestive heart failure, coronary artery disease, diabetes, emphysema, hypertension, kidney disease, obesity, weight status (defined via body mass index), liver disease, stroke, and dyslipidemia (i.e., elevated total cholesterol or low HDL cholesterol). As previously described, we used these 15 conditions to define participants with 0 (n = 6,775), 1 (n = 7,626), 2 (n = 5,134), 3 (n = 2,568), 4 (n = 1,074), and 5+ (n = 777) medical conditions; notably, these sample sizes don’t sum to 28,119 participants due to missing data for some of the morbidities used in the multimorbidity calculation.
Table 2.
Assessment and classification of the evaluated medical conditions
| Medical Condition | Description of Assessment | Definition of Categories |
|---|---|---|
| Determined from Questionnaire | ||
| Depression | Patient Health Questionnaire (PHQ-9) | Moderate or greater depression defined as PHQ-9 ≥ 10 |
| Determined from Examination | ||
| Age-Related Macular Degeneration | Canon Non-Mydratic Retinal Camera CR6-45NM | Early AMD: presence of drusen and/or pigmentary abnormalities; late AMD: presence of choroidal neovascularization and/or geographic atrophy; few participants had late AMD, so participants were classified as early/late AMD |
| Visual Impairment | ARK-760 autorefractor | Participants with presenting visual acuity of 20/40 or better in either eye were classified as having normal sight. Participants with presenting visual acuity worse than 20/40, but postrefraction visual acuity in either eye were 20/40 or better, were classified as having uncorrected refractive error. Participants with visual acuity worse than 20/40 after autorefraction, or who self-reported not being able to see light with both eyes open, were classified as having visual impairment. |
| Cardiorespiratory Fitness | Treadmill-based submaximal test. | Low fitness: < 20th percentile; moderate fitness: 20–59th percentile; high fitness ≥ 60th percentile for age and gender. |
| Chronic Obstructive Pulmonary Disease | Objective pulmonary function testing using Ohio 822/827 dry-rolling seal volume spirometers | GOLD classifications when FEV1/FVC < 0.70: Mild COPD: FEV1 ≥ 80% predicted; Moderate: 50% ≤ FEV1 < 80% predicted; Severe: 30% ≤ FEV1 < 50% predicted; Very severe: FEV1 < 30% predicted; few participants had very severe COPD, so classifications were mild, moderate, and severe COPD. |
| Hearing Impairment | Calculating the average of air conduction pure-tone thresholds; low pure-tone average (LPTA) and high pure-tone average (HPTA). | Hearing within normal limits (LPTA & HPTA ≤ 25 dB), mild hearing loss (LPTA or HPTA 26–40 dB) and moderate or greater hearing loss (LPTA or HPTA > 40 dB) |
| Non-Proliferative Retinopathy | Canon Non-Mydratic Retinal Camera CR6-45NM | No retinopathy, mild non-proliferative retinopathy, moderate-to-severe non-proliferative retinopathy; based on presence of 1 or more retinal microaneurysms or retinal blot hemorrhages using the Early Treatment Diabetic Retinopathy Study grading criteria. |
| Weight Status | Measured body mass index | Obesity defined as ≥ 30 kg/m2 Underweight defined as < 18.5 kg/m2 |
| Peripheral Arterial Disease | Ankle Brachial Index (ABI) from measured upper and lower extremity blood pressure assessment. | Normal ABI (1–1.4) and abnormal ABI (< 1 or > 1.4) |
| Peripheral Neuropathy | 5.07 Semmes-Weinstein nylon monofilament | Peripheral neuropathy defined as at least 1 insensate area in either foot. |
| Physical Inactivity | Accelerometry over a 7-day period, and only including those providing at least 4 days of 10+ hrs/day of monitoring. | Physical inactivity defined as engaging in < 150 min/wk of accelerometer-determined moderate-to-vigorous physical activity (1-min bouts). |
| Determined from Laboratory Assessment | ||
| Chronic Kidney Disease | Glomerular filtration rate was assessed from the CKD Epidemiology equation based on specified race, sex, and creatinine level. | < 60 mL/min per 1.73 m2 |
| Elevated C-Reactive Protein (CRP) | Latex-enhanced nephelometry. | > 0.3 mg/dL |
| Elevated Fasting Glucose | Hexokinase method | ≥ 126 mg/dL |
| Elevated LDL Cholesterol | Friedewald formula | ≥ 160 mg/dL |
| Elevated Total Cholesterol | Measured enzymatically in serum using the Roche Hitachi method. | > 240 mg/dL |
| Elevated Triglycerides | Measured enzymatically in serum. | ≥ 200 mg/dL |
| Low HDL Cholesterol | Measured enzymatically in serum. | < 40 mg/dL |
| Hypertension | Measured systolic and diastolic blood pressure; average of 3–4 measurements. | ≥ 140 mmHg systolic or ≥ 90 mmHg diastolic |
| Smoking (cotinine) | Serum cotinine, a biological measure of smoking status, was measured by an isotope dilution-high performance liquid chromatography/atmospheric pressure chemical ionization tandem mass spectrometry. | Serum cotinine levels of > 1.78 ng/mL for men and > 4.47 ng/mL for women were assessed to differentiate smokers from non-smokers |
As reported elsewhere, working is defined as working at an outside job or business within the last week; full time is defined as ≥ 35 hours/week; not working is defined as either not seeking work, nor on layoff; unemployed is defined as looking for work or on a layoff.
3. Data analysis
All statistical analyses were computed in Stata (v. 12), with analyses adjusted for the complex survey design employed by NHANES. Multivariable logistic regression models were used to determine if various medical conditions increased the odds of not working (vs. working), working part-time (vs. working full-time), and being unemployed (vs. working). As noted in the footnote of Table 3, all self-report of physician-diagnosed conditions were included in one model. The examination-determined variables were not all collected during the same cycles; therefore, separate models were computed for each of these examination-determined medical conditions. Separate models were also computed for each of the laboratory-determined variables, as not all laboratory variables were available for each cycle. Finally, models were computed to determine the impact of how work status varied with the number of prevalent medical conditions (as defined above). Age, gender (male/female), race-ethnicity (Mexican American, non-Hispanic white, non-Hispanic black, and other), education (< 9th grade, 9–11th grade, high school, some college, college or more) were included as covariates. Prevalence of health care utilization over the past 12 months and family income-to-poverty ratio were also included in sensitivity results to determine the additional impact these variables had on the association between chronic disease and employment. Results were similar when stratified by education status (data not shown), so education was included as a covariate instead of providing results stratified by education. Statistical significance was established as p < 0.05.
Table 3.
Multivariable logistic regression analyses* predicting odds of not working, working part-time, and being unemployed
| Medical/Health Condition Based on Cumulative Index Rating Scale (CIRS) Morbidity Classes | Not Working vs. Working† | Part Time vs. Full Time† | Unemployed vs. Working† | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| Entire Sample | Men | Women | Entire Sample | Entire Sample | ||||||
| Cardiac | ||||||||||
| Congestive Heart Failure vs. none | 2.14 | < 0.001 | 2.50 | < 0.001 | 1.72 | 0.01 | 1.09 | 0.73 | 1.02 | 0.94 |
| Coronary Artery Disease vs. none | 1.75 | < 0.001 | 1.57 | 0.003 | 1.86 | 0.01 | 1.06 | 0.81 | 1.36 | 0.27 |
| Vascular | ||||||||||
| Peripheral Arterial Disease vs none | 1.58 | < 0.001 | 1.41 | 0.03 | 1.64 | 0.002 | 0.87 | 0.52 | 1.72 | 0.02 |
| Hypertension vs none | 1.16 | 0.005 | 1.22 | 0.006 | 1.11 | 0.14 | 1.08 | 0.28 | 0.98 | 0.89 |
| Stroke vs. none | 2.83 | < 0.001 | 2.40 | < 0.001 | 3.24 | < 0.001 | 1.62 | 0.07 | 1.58 | 0.07 |
| Respiratory | ||||||||||
| Asthma vs. none | 1.00 | 0.86 | 1.10 | 0.27 | 0.97 | 0.67 | 1.07 | 0.19 | 1.01 | 0.90 |
| Bronchitis vs. none | 1.21 | 0.005 | 1.37 | 0.01 | 1.21 | 0.02 | 1.05 | 0.63 | 1.14 | 0.35 |
| Emphysema vs. none | 2.32 | < 0.001 | 2.56 | 0.001 | 1.91 | 0.005 | 1.37 | 0.30 | 1.46 | 0.35 |
| Chronic Obstructive Pulmonary Disease | ||||||||||
| Mild vs. no COPD | 1.17 | 0.26 | 1.13 | 0.53 | 1.19 | 0.51 | 1.47 | 0.01 | 0.84 | 0.56 |
| Moderate vs. no COPD | 1.36 | 0.06 | 1.40 | 0.10 | 1.28 | 0.30 | 1.22 | 0.40 | 1.01 | 0.97 |
| Severe vs. no COPD | 2.84 | 0.01 | 3.35 | 0.08 | 2.22 | 0.20 | 0.62 | 0.57 | 3.55 | 0.07 |
| Ophthalmological | ||||||||||
| Age-Related Macular Degeneration | ||||||||||
| Early/Late AMD vs. none | 1.12 | 0.69 | 0.83 | 0.66 | 1.43 | 0.37 | 1.37 | 0.45 | 1.88 | 0.07 |
| Non-Proliferative Retinopathy | ||||||||||
| Mild vs. none | 0.97 | 0.88 | 0.88 | 0.52 | 1.05 | 0.83 | 0.78 | 0.27 | 0.69 | 0.15 |
| Moderate/severe vs. none | 2.03 | 0.17 | 2.85 | 0.16 | 1.58 | 0.29 | 0.18 | 0.05 | 0.48 | 0.40 |
| Visual Impairment | ||||||||||
| Uncorrected refractive error vs. normal sight | 1.24 | 0.008 | 1.47 | 0.01 | 1.07 | 0.53 | 1.27 | 0.02 | 1.27 | 0.14 |
| Visual impairment vs. normal sight | 2.68 | < 0.001 | 1.53 | 0.28 | 4.49 | < 0.001 | 1.39 | 0.46 | 0.39 | 0.14 |
| Hepatic | ||||||||||
| Liver Disease vs. none | 1.47 | < 0.001 | 1.59 | < 0.001 | 1.32 | 0.03 | 0.96 | 0.81 | 1.27 | 0.23 |
| Renal | ||||||||||
| Chronic Kidney Disease vs. none | 1.87 | < 0.001 | 1.93 | < 0.001 | 1.88 | < 0.001 | 1.40 | 0.13 | 0.76 | 0.42 |
| Musculoskeletal | ||||||||||
| Arthritis vs. none | 1.55 | < 0.001 | 1.85 | < 0.001 | 1.41 | < 0.001 | 1.11 | 0.15 | 1.22 | 0.02 |
| Neurological | ||||||||||
| Hearing Impairment | ||||||||||
| Mild vs none | 1.19 | 0.17 | 1.33 | 0.15 | 1.17 | 0.37 | 1.03 | 0.85 | 1.47 | 0.10 |
| Moderate+ vs. none | 1.46 | 0.002 | 1.74 | 0.002 | 1.18 | 0.37 | 1.05 | 0.79 | 1.16 | 0.53 |
| Peripheral Neuropathy vs none | 1.38 | 0.04 | 1.44 | 0.11 | 1.25 | 0.29 | 1.45 | 0.03 | 0.61 | 0.12 |
| Endocrine/Metabolic | ||||||||||
| Diabetes vs. none | 1.53 | < 0.001 | 1.71 | < 0.001 | 1.39 | < 0.001 | 1.01 | 0.92 | 1.31 | 0.08 |
| Obesity vs not obese | 1.06 | 0.09 | 1.05 | 0.24 | 1.07 | 0.11 | 0.87 | 0.007 | 1.08 | 0.29 |
| Underweight vs. not underweight | 1.62 | 0.001 | 1.83 | 0.01 | 1.51 | 0.003 | 1.25 | 0.17 | 1.47 | 0.08 |
| Elevated C-Reactive Protein vs. not | 1.25 | < 0.001 | 1.35 | < 0.001 | 1.18 | < 0.001 | 1.02 | 0.70 | 1.04 | 0.56 |
| Elevated Glucose vs. not | 1.35 | 0.002 | 1.24 | 0.09 | 1.24 | 0.14 | 0.89 | 0.47 | 1.03 | 0.86 |
| Elevated LDL Cholesterol vs. not | 1.10 | 0.25 | 0.89 | 0.41 | 1.31 | 0.02 | 1.07 | 0.54 | 1.30 | 0.07 |
| Elevated Total Cholesterol vs. not | 1.18 | < 0.001 | 0.99 | 0.95 | 1.37 | < 0.001 | 1.11 | 0.09 | 1.35 | 0.002 |
| Elevated Triglycerides vs. not | 1.37 | < 0.001 | 1.14 | 0.18 | 1.70 | < 0.001 | 1.03 | 0.76 | 1.17 | 0.19 |
| Low HDL Cholesterol vs. not | 1.20 | < 0.001 | 1.10 | 0.12 | 1.40 | < 0.001 | 0.88 | 0.07 | 1.03 | 0.67 |
| Cancer (of any type) vs. not | 1.33 | 0.002 | 1.63 | < 0.001 | 1.22 | 0.07 | 1.00 | 0.94 | 1.31 | 0.10 |
| Psychiatric | ||||||||||
| Moderate+ Depression vs. Less Depression Symptoms | 3.12 | < 0.001 | 4.23 | < 0.001 | 2.60 | < 0.001 | 1.31 | 0.06 | 1.76 | < 0.001 |
| Behavioral | ||||||||||
| Sleep Disorder vs. none | 1.25 | 0.003 | 1.03 | 0.73 | 1.41 | 0.003 | 1.12 | 0.33 | 0.94 | 0.75 |
| Cardiorespiratory Fitness | ||||||||||
| Low vs. high | 1.09 | 0.48 | 1.13 | 0.59 | 1.13 | 0.45 | 0.83 | 0.31 | 1.06 | 0.74 |
| Moderate vs. high | 0.87 | 0.25 | 0.85 | 0.33 | 0.91 | 0.63 | 0.84 | 0.13 | 0.78 | 0.28 |
| Physical Activity | ||||||||||
| Inactive vs. active | 1.93 | < 0.001 | 2.62 | < 0.001 | 1.46 | 0.01 | 1.09 | 0.38 | 1.33 | 0.10 |
| Smoker vs. non-smoker | 1.39 | < 0.001 | 1.45 | < 0.001 | 1.33 | < 0.001 | 1.07 | 0.24 | 1.23 | 0.01 |
Separate logistic regression models were computed for employment status (not working vs. working; part-time vs. full-time; and unemployed vs. working).
For the self-report of physician diagnosis variables, 1 model was computed which included all conditions in the model, plus the covariates age, gender, and race-ethnicity. The exception to this was the sleep disorder variable because sleep disorder assessment did not occur across all NHANES cycles. Therefore, the ORs for the sleep variable is from a separate model that included sleep disorder plus the other medical conditions and covariates.
Separate models were computed for each of the laboratory-determined variables not all participants had data on all biomarkers. In each model covariates included age, gender, and race-ethnicity.
The examination-determined variables were not all collected during the same cycles; therefore, separate models were computed for each of these examination-determined medical conditions. Covariates age, gender, and race-ethnicity were included in each model.
Working is defined as working at an outside job or business within the last week; full time is defined as ≥ 35 hrs/wk; and unemployed is defined as looking for work or on a layoff.
RESULTS
Results are based on the following CIRS categorizes: cardiac, vascular, respiratory, ophthalmological, hepatic, renal, musculoskeletal, neurological, endocrine/metabolic, and psychiatric. An inclusion of this battery of conditions provides a more comprehensive assessment of individual health. Although not a CIRS morbidity class, the association between health-compromising behaviors (e.g., physical inactivity and smoking) and work status was also examined to further examine all relevant associations between health and work status.
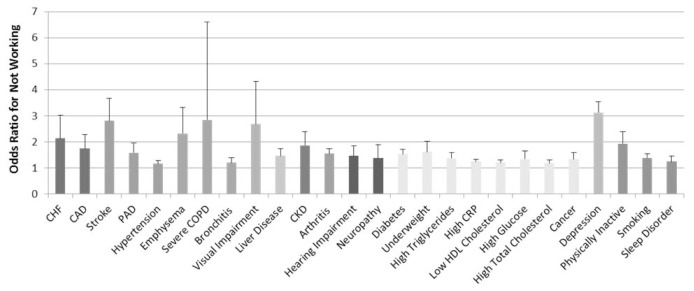
Twenty-six medical conditions were associated with significantly higher odds of not working (p < 0.05; shown in Fig. 1).
Fig. 1.
Conditions significantly associated with higher odds of not working. CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; CRP, C-reactive protein; PAD, peripheral arterial disease. Medical conditions organized based on Cumulative Index Rating Scale (CIRS) Morbidity Classes.
Table 3 reports the odds of not working, working part-time, and being unemployed for each of the evaluated medical conditions, with these findings summarized in following narrative.
1. Individual medical conditions associated with not working
A total of 26 medical conditions were associated with higher odds of not working, including at least one medical condition within each of the CIRS morbidity classes. (Fig. 1 and Table 2; ORrange = 1.16–3.12, p < 0.05 for all).
Amongst the individual medical conditions evaluated, depression (OR = 3.12, 95% CI: 2.74–3.55; p < 0.05), severe COPD (OR = 2.84, 95% CI: 1.22–6.61; p < 0.05), Stroke (OR = 2.83 95% CI: 2.16–3.71; p < 0.05) and visual impairment (OR = 2.68, 95% CI: 1.65–4.33; p < 0.05) demonstrated the greatest odds of not working.
The presence of cardiovascular conditions such as congestive heart failure (OR = 2.14, 95% CI: 1.51–3.03; p < 0.05), coronary artery disease (OR = 1.75, 95% CI: 1.33–2.29; p < 0.05), stroke (OR = 2.81, 95% CI: 2.15–3.67; p < 0.05), and peripheral arterial disease (OR = 1.58, 95% CI: 1.27–1.95; p < 0.05) all increased the odds of not working. Additionally, vascular and metabolic risk factors for cardiovascular conditions such as being underweight (OR = 1.62, 95% CI: 1.29–2.03; p < 0.05), hypertension (OR = 1.16, 95% CI: 1.05–1.29; p < 0.05), elevated total cholesterol (OR = 1.18, 95% CI: 1.07–1.31; p < 0.05), low HDL cholesterol (OR = 1.20, 95% CI: 1.11–1.31; p < 0.05), elevated C-reactive protein (OR = 1.25, 95% CI: 1.16–1.34; p < 0.05), and physical inactivity (OR = 1.93, 95% CI: 1.56–2.39; p < 0.05) were associated with a higher odds of not working. Similarly, respiratory conditions such as emphysema (OR = 2.32, 95% CI: 1.62–3.33; p < 0.05), severe COPD (OR = 2.84, 95% CI: 1.22–6.61; p < 0.05) and bronchitis (OR = 1.21, 95% CI: 1.06–1.39; p < 0.05) increased the odds of not working, as did behaviors associated with such respiratory disease such as smoking (OR = 1.39, 95% CI: 1.25–1.54; p < 0.05).
Several types of neurosensory dysfunction were associated with higher odds of not working, including visual impairment (OR = 2.68, 95% CI: 1.65–4.33; p < 0.05), moderate+ hearing loss (OR = 1.46, 95% CI: 1.15–1.86; p < 0.05), and peripheral neuropathy (OR = 1.38, 95% CI: 1.01–1.89; p < 0.05). Other classes of organ dysfunction associated with higher odds of not working included chronic kidney disease (OR = 1.87, 95% CI: 1.47–2.39; p < 0.05) and liver disease (OR = 1.47, 95% CI: 1.24–1.75; p < 0.05). Finally, psychiatric disease such as moderate+ depressive symptoms were associated with increased odds of not working (OR = 3.12, 95% CI: 2.74–3.55; p < 0.05).
When results were stratified by gender, similar results were generally observed for both men and women (Table 3).
2. Multiple medical conditions associated with not working
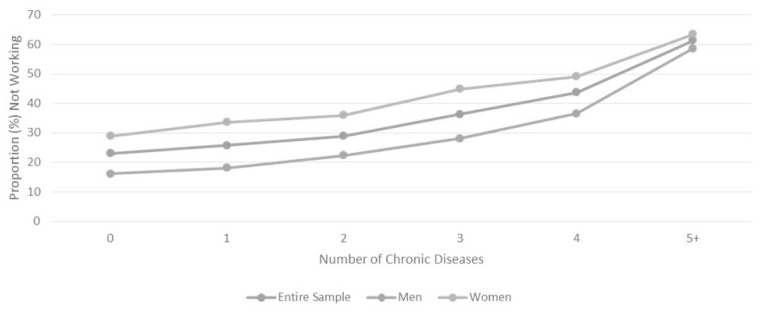
The weighted proportion of Americans with 0, 1, 2, 3, 4, and 5+ chronic diseases, respectively, was 29.3%, 32.4%, 21.1%, 10.2%, 4.3%, and 2.7%. Regarding being multimorbid (2+ diseases), 38.3% was multimorbid.
The proportion of Americans not working increased substantially as multimorbidity increased, with a similar trend observed across gender (Fig. 2). Similarly, the adjusted odds of not working increased substantially as multimorbidity increased, with the greatest change occurring between having 4 (vs. 0) and 5 (vs. 0) chronic diseases; compared to those with 0 morbidities, the odds ratio for those with 1, 2, 3, 4, and 5+ morbidities, respectively, was 1.14 (95% CI: 1.04–1.24; p < 0.05), 1.29 (95% CI: 1.15–1.44; p < 0.05), 1.72 (95% CI: 1.50–1.96; p < 0.05), 2.16 (95% CI: 1.83–2.55; p < 0.05), and 4.37 (95% CI: 3.44–5.55; p < 0.05).
Fig. 2.
Proportion of American adults not working based on the degree of multimorbidity.
After adjusting for age, gender, race-ethnicity and education, multimorbid (2+ morbidities) Americans had a 48% increased odds of not working (OR = 1.48, 95% CI: 1.37–1.59; p < 0.05) as compared to participants with 1 or fewer conditions. When adding the number of times they received healthcare in the past 12 months as a covariate, results were similar (OR changed from 1.48 [p < 0.05] to 1.33 [95% CI: 1.22–1.43; p < 0.05]). Additionally, when adding income-to-poverty ratio as a covariate, results were still statistically significant (OR = 1.22; 95% CI: 1.11–1.34; p < 0.001). Further, and after adjustments (age, gender, race-ethnicity, education and healthcare access), multimorbidity was associated with odds of not working among those 20–39 yrs (OR = 1.17, 95% CI: 1.03–1.32; p = 0.01) as well as those 40–64 yrs (OR = 1.42, 95% CI: 1.26–1.58; p < 0.001).
Given the relatively strong association between depression and odds of not working, additionally analyses were computed to examine the potential interaction effect of depression on the association between multimorbidity and odds of not working. A multiplicative interaction model was examined by creating a cross-product term of depression and multimorbidity along with their main effects and the covariates. Multiplicative interaction was present given that, after adjustments, multimorbidity (OR = 1.31; 95% CI: 1.16–1.48; p < 0.001), depression (OR = 2.13; 95% CI: 1.67–2.70; p < 0.001) and the interaction term between multimorbidity and depression (OR = 1.47; 95% CI: 1.09–1.98; p = 0.01) were all significant.
3. Odds of part time vs. full-time work
Mild COPD (OR = 1.47, 95% CI: 1.08–2.01; p < 0.05), uncorrected refractive error (OR = 1.27, p < 0.05), peripheral neuropathy (OR = 1.45, 95% CI: 1.02–2.06; p < 0.05) and obesity (OR = 0.87, 95% CI: 0.78–0.96; p < 0.05) were associated with working part-time vs. full-time. No other conditions increased the likelihood of part-time as compared to full-time work (p ≥ 0.05).
4. Odds of unemployed vs. working
Arthritis (OR = 1.22, 95% CI: 1.03–1.46; p < 0.05), elevated total cholesterol (OR = 1.35, 95% CI: 1.12–1.64; p < 0.05), smoking (OR = 1.23, 95% CI: 1.05–1.46; p < 0.05) and depression (OR = 1.76, 95% CI: 1.40–2.23; p < 0.05) were the only health parameters associated with increased odds of being unemployed vs. working. No other conditions increased the likelihood of unemployment as compared to full-time work (p ≥ 0.05).
DISCUSSION
Few population-based studies have examined the association between health and work status, with a recent study [9] demonstrating that those with worse vision have increased odds of not working. Our findings demonstrate that numerous medical conditions are strongly associated with higher likelihood of not working. The included medical conditions were less associated with higher odds of working part-time (vs. full-time) or unemployment (vs. working), suggesting that health deficits generally lead individuals to not work, as opposed to restricting their work hours. Evidence of a relationship between co-morbidity and employment status, as evidenced by few downstream medical conditions fails to illustrate a comprehensive picture of this public health issue. Experimental interventions aiming to promote or effectively sustain employment among patients with morbidities will be better informed by a broad range of selected medical conditions. Taken together, our inclusion of a variety of clinical indices, underscore the relationship between poor health status on likelihood of not working among a nationally representative sample of American adults. The cross-sectional nature of NHANES epidemiological surveillance data makes it impossible to discount the possibility that not working may increase morbidity due to less access to health care; however, when access to health care was included as a covariate, chronic disease was still highly associated with increased odds of not working. In addition, when we included sex as a covariate, similar results were generally observed for men and women. This is not to say models utilized in subsequent research should not stratify by gender, as cultural factors, social norms, educational status, or the wealth gap between sexes may confer statistically significant outcomes.
Among this national sample of U.S. adults, multimorbidity was prevalent, with 38.3% having 2 or more medical conditions and approximately 3.0% having 5 or more conditions, which is in alignment with other studies [10,11]. While several individual medical conditions increased the odds of not working, the likelihood of not working increased drastically with the degree of multimorbidity.
The association between morbidity and multimorbidity with work status is complex and likely influenced by a multitude of factors, including socioeconomic status (SES), and in particular, an individual’s income level [12]. For example, adults with lower SES are more likely to be multimorbid and individuals from lower SES groups have an increased risk of losing their jobs [13]. Not working, in turn, may further increase their risk of morbidity by, for example, reducing their income level and ultimately making it less likely that healthcare is sought (even if available), increasing medication non-compliance, and making it more difficult to adhere to healthy lifestyle habits (i.e. nutritious food and access to exercise resources, including equipment and trained exercise specialists) [14]. Such an effect may also precipitate other chronic diseases, such as depression, which can result in a vicious cycle inhibiting work status.
Recent work has shown that employment is associated with favorable physical and psychological health outcomes [15]. At a societal level, better methods are needed to facilitate employment amongst the chronically ill, particularly among those with multimorbidity. As the relationship between health and employment status appears to be bidirectional, promotion of favorable health among those with chronic ailments may, in turn, facilitate acquisition and retainment of employment over time [15]. The concurrent presence of multiple chronic diseases may render difficulty in working ability and attendance, possibly as a result of several comorbidity-induced mediators, such as fatigue [16], cognitive dysfunction [17], mobility limitations [18], and need for regular medical appointments. Our findings support the goals outlined by the United States Department of Health and Human Services for improving the health of individuals with multiple chronic conditions [19]. While programs to facilitate employment in the chronically ill may be expensive, the societal costs to support non-working individuals is also high at the government, family, and individual level [20]. The low, private cost of untaxed unemployment in the short-term, may actually increase the cost of permanent unemployment in the United States, as select individuals are fully covered by unemployment benefits for a brief period. The culture of acceptance of financial assistance has transformed within the modern social climate to promote reliance on these low-cost benefits among disadvantaged individuals. Disability insurance, food stamps and health insurance payments provide a sense of personal well-being and security, which may exponentiate the amount of national unemployment debt [21]. Unemployment is suggested to confer higher monetary costs than inflation, which increases the global economic burden, particularly among the elderly and least educated [22], who are at a higher risk of health disparity [23,24].
The strong link between multimorbidity and work status underscores the importance of holistically assessing and treating patients. Earlier work indicates that empathetic “care as usual,” coupled with cognitive-behavioral treatment, reduces the length of employee absenteeism among patients with adjustment disorders (compounding symptoms of stress and physical deterioration). The influence of holistic care should be evaluated across broader patient populations, as the risk of permanent disability and associated insurance costs may be ameliorated, in part, via best treatment practices [25]. Our findings also emphasize that physicians must be aware of the risks that illness poses to their patient’s employment, and ultimately their financial and emotional well-being. History taking regarding work status is frequently overlooked by modern-day physicians, and even when such a history is elicited, treatment strategies to facilitate working are generally not known [26]. Significant research is needed to understand what abilities allow patients to continue working in the context of illness, and how these abilities can be maximized by the healthcare team.
The observed association between morbidity and multimorbidity with work status should be interpreted in the context of the study’s limitations. The continuous NHANES is a series of cross-sectional assessments among a national sample of Americans, with this cross-sectional study design preventing the ability to render cause-and-effect. Although it is highly plausible that morbidity and multimorbidity may interfere with an individual’s ability to initiate and maintain work, it is also highly likely that not working may facilitate the development of select morbidities, such as depression, which further underscores the complex relationship between morbidity and work status. Even minor depression has been linked with loss of employee productivity and retention, highlighting the importance of mental health considerations relative to the morbidity-work capacity interaction [27,28]. Our observation of a statistically significant positive interaction between multimorbidity and depression further corroborates these assertions. Additionally, there is no gold standard method for calculating one’s comorbid load, such that our method of calculating multimorbidity may not be optimal. Further, the NHANES did not evaluate several work-related parameters (e.g., job loss history, duration of unemployment, and loss of opportunity to work), which should be taken into consideration with future work on this topic as these work-related parameters likely play an important role when defining the morbidity-work status relationship. Notable strengths of this study include the utilization of a large national sample of U.S. adults, and comprehensively (using questionnaire, direct examination, and laboratory assessments) examining the association of morbidity and multimorbidity with work status while employing numerous robust measures of health (e.g., pulmonary function-determined COPD, accelerometer-determined physical inactivity, and objectively assessed vision, hearing, and neuropathy).
In conclusion, multimorbidity and numerous individual morbidities including cardiac, vascular, respiratory, ophthalmological, hepatic, renal, musculoskeletal, neurological, endocrine/metabolic, and psychiatric medical conditions were associated with increased odds of not working among Americans. Further investigation is necessary to assess chronic effects of multimorbidity on employment status and quality of life, determine which interventions can effectively limit the impact of chronic disease on work status, and prevent the potential vicious cycle between morbidity and insecure employment.
Footnotes
CONFLICT OF INTERESTS
None to declare.
REFERENCES
- 1.Singh GK, Siahpush M. Inequalities in US life expectancy by area unemployment level, 1990–2010. Scientifica (Cairo) 2016;2016 doi: 10.1155/2016/8290435. 8290435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yelin E, Sonneborn D, Trupin L. The prevalence and impact of accommodations on the employment of persons 51–61 years of age with musculoskeletal conditions. Arthritis Care Res. 2000;13:168–76. doi: 10.1002/1529-0131(200006)13:3<168::AID-ANR6>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Zhao S, Blazer DG, Swartz M. Prevalence, correlates, and course of minor depression and major depression in the National Comorbidity Survey. J Affect Disord. 1997;45:19–30. doi: 10.1016/S0165-0327(97)00056-6. [DOI] [PubMed] [Google Scholar]
- 4.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290:2443–54. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- 5.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384:45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 6.Janlert U, Winefield AH, Hammarstrom A. Length of unemployment and health-related outcomes: A life-course analysis. Eur J Public Health. 2015;25:662–7. doi: 10.1093/eurpub/cku186. [DOI] [PubMed] [Google Scholar]
- 7.Feachem RG. Poverty and inequity: A proper focus for the new century. Bull World Health Organ. 2000;78:1–2. [PMC free article] [PubMed] [Google Scholar]
- 8.Adler NE, Cutler DM, Fielding JE, Galea S, Glymour MM, Koh HK, Satcher D. NAM Perspectives. Discussion Paper. National Academy of Medicine; Washington, DC: 2016. Addressing social determinants of health and health disparities: A vital directions for health and health care series. [DOI] [Google Scholar]
- 9.Sherrod CE, Vitale S, Frick KD, Ramulu PY. Association of vision loss and work status in the United States. JAMA Ophthalmol. 2014;132:1239–42. doi: 10.1001/jamaophthalmol.2014.2213. quiz 43–6. [DOI] [PubMed] [Google Scholar]
- 10.Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: Toward a more uniform methodology. Ann Fam Med. 2012;10:142–51. doi: 10.1370/afm.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83. doi: 10.1093/epirev/mxs009. [DOI] [PubMed] [Google Scholar]
- 12.Stronks K, van de Mheen H, van den Bos J, Mackenbach JP. The interrelationship between income, health and employment status. Int J Epidemiol. 1997;26:592–600. doi: 10.1093/ije/26.3.592. [DOI] [PubMed] [Google Scholar]
- 13.Arber S. Social class, non-employment, and chronic illness: Continuing the inequalities in health debate. Br Med J (Clin Res Ed) 1987;294:1069–73. doi: 10.1136/bmj.294.6579.1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mathes T, Jaschinski T, Pieper D. Adherence influencing factors - a systematic review of systematic reviews. Arch Public Health. 2014;72:37. doi: 10.1186/2049-3258-72-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Noordt M, HIJ, Droomers M, Proper KI. Health effects of employment: A systematic review of prospective studies. Occup Environ Med. 2014;71:730–6. doi: 10.1136/oemed-2013-101891. [DOI] [PubMed] [Google Scholar]
- 16.Fritschi C, Quinn L. Fatigue in patients with diabetes: A review. J Psychosom Res. 2010;69:33–41. doi: 10.1016/j.jpsychores.2010.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Boxtel MP, Buntinx F, Houx PJ, Metsemakers JF, Knottnerus A, Jolles J. The relation between morbidity and cognitive performance in a normal aging population. J Gerontol A Biol Sci Med Sci. 1998;53:M147–54. doi: 10.1093/gerona/53A.2.M147. [DOI] [PubMed] [Google Scholar]
- 18.Loprinzi PD, Sheffield J, Tyo BM, Fittipaldi-Wert J. Accelerometer-determined physical activity, mobility disability, and health. Disabil Health J. 2014;7:419–25. doi: 10.1016/j.dhjo.2014.05.005. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. Multiple chronic conditionss–A strategic framework: Optimum health and quality of life for individuals with multiple chronic conditions. U.S. Department of Health and Human Services; Washington, DC: 2010. [Google Scholar]
- 20.Feldstein MS. The private and social costs of unemployment. NBER Working Paper. 1977;(223) [Google Scholar]
- 21.Feldstein MS. The private and social costs of unemployment. Am Econ Rev. 1978;68:155–8. [Google Scholar]
- 22.Blanchflower DG. NBER Working Paper, No 13505. 2007. Is unemployment more costly than inflation? [Google Scholar]
- 23.Pincus T, Callahan LF. Associations of low formal education level and poor health status: Behavioral, in addition to demographic and medical, explanations? J Clin Epidemiol. 1994;47:355–61. doi: 10.1016/0895-4356(94)90156-2. [DOI] [PubMed] [Google Scholar]
- 24.Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O’Donnell M, Sullivan R, Yusuf S. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385:549–62. doi: 10.1016/S0140-6736(14)61347-7. [DOI] [PubMed] [Google Scholar]
- 25.van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Occup Environ Med. 2003;60:429–37. doi: 10.1136/oem.60.6.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Politi BJ, Arena VC, Schwerha J, Sussman N. Occupational medical history taking: How are today’s physicians doing? A cross-sectional investigation of the frequency of occupational history taking by physicians in a major US teaching center. J Occup Environ Med. 2004;46:550–5. doi: 10.1097/01.jom.0000128153.79025.e4. [DOI] [PubMed] [Google Scholar]
- 27.Beck A, Crain AL, Solberg LI, Unutzer J, Glasgow RE, Maciosek MV, Whitebird R. Severity of depression and magnitude of productivity loss. Ann Fam Med. 2011;9:305–11. doi: 10.1370/afm.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annu Rev Psychol. 2011;62:501–30. doi: 10.1146/annurev.psych.031809.130711. [DOI] [PMC free article] [PubMed] [Google Scholar]